Abstract
Purpose
Good initial fixation of glenoid component for reverse total shoulder arthroplasty (RTSA) relies on component placement and screw purchase in the scapula bone. This is especially difficult in an Asian population with small glenoid geometry. Optimal glenoid component roll angle and screw angulation to achieve the longest screws for best fixation has not been defined in the current literature.
Methods
Computer 3D modelling of 133 scapulas with RTSA performed were analyzed to determine patient specific optimal glenoid roll angle (GRA) for the longest bi-cortical screws attainable. The cranial-caudal angle (CCA), anterior-posterior angle (APA) and lengths for the superior and inferior screws were measured. Validation testing using calculated average (CA) angles and rounded average (RA) angles to the nearest 5 degree were recomputed for each case to determine the bi-cortical screw lengths achievable. The CA and RA screw lengths were compared against patient specific modelling using paired-sample t-tests.
Results
Average GRA was − 1.6°, almost perpendicular to the long axis of the glenoid and achieves an average bi-cortical screw length of 51.3 mm and 45.5 mm for the superior and inferior screws respectively. The CCA and APA were 9.1° cranial and 6.5° posterior for the superior screw and screw angulation of 11.2° caudal and 0.7° anterior for the inferior screw. Validation testing shows statistically shorter screw lengths in the CA and RA models compared to patient specific modelling (p < 0.01).
Conclusion
Validation testing with average angles for GRA, CCA and APA demonstrates strong patient heterogeneity and anatomical variation. Despite this, screw lengths attainable in the RA group were > 38 mm with good safety profile. Surgeons may consider the additional use of navigation-assisted, or 3D printed patient specific instrumentation to optimize baseplate and screw configuration for RTSA.
Supplementary Information
The online version contains supplementary material available at 10.1007/s00264-024-06340-z.
Keywords: Reverse shoulder arthroplasty, Glenoid fixation, Screw length, Patient specific instrumentation, 3D modelling
Introduction
Reverse Total Shoulder Arthroplasty (RTSA) is indicated for irreparable massive rotator cuff tear, severe rotator cuff arthropathy, glenohumeral arthritis, and non-reconstructable proximal humerus fractures in elderly individuals [1]. However, a notable concern associated with this procedure is the potential loosening of the glenoid component, stemming from incorrect positioning and inadequate anchorage within the scapular bone [2]. In addition to ensuring the proper orientation of the glenoid base plate and preserving high-quality subchondral bone, augmenting the quantity and length of screws for the glenoid component has been proven to enhance biomechanical fixation [3–6]. It is crucial to direct each screw through the glenoid vault to the area of most bone, with the superior screw aimed towards the scapular spine confluence and inferior screw towards the scapular body to achieve maximal screw length. Stronger screw purchase hopes to achieve superior immediate implant stability and allow bony ingrowth to prolong the implant longevity [3–5].
There are various challenges in glenoid component placement for RTSA. Gender and ethnicity influence significant morphological and size variations of the glenoid, sometimes resulting in glenoid dimensions smaller than the available glenoid base plate, particularly evident in populations such as the Japanese, where the mean AP glenoid dimension is studied to be of an average of only 23.4 mm [7]. The naturally small and thin scapular bone in the Asian population makes the insertion of anterior and posterior screws impractical due to lack of bone. Secondly, there is a higher risk of iatrogenic fracture associated with 4 screw insertion without additional biomechanical advantage [8]. As a result, insertion of only the superior and inferior screws for the glenoid component during RTSA in small glenoid geometry is common practice. Thus, a greater accuracy for screw insertion is required. Pre-operative 3D planning with patient-specific instrumentation (PSI), computer navigation assisted surgery and robotic assisted surgery have been used to improve accuracy albeit with logistical issues, time consumption and operative costs [9–14].
This study seeks to establish a guide for the optimal rotation of the glenoid component and screw trajectory to facilitate the longest bi-cortical superior and inferior screw length to be used in small-sized glenoids for centers lacking the ancillary technology or with financial constraints. To date, there is no current literature describing optimal screw placement angular trajectory and glenoid roll.
Materials and methods
A retrospective review of all CT scapula data obtained from a university hospital 3D printing facility where in-house patient-specific instrumentation (PSI) jig fabrication for RTSA is routinely practiced. All patients from 2020 to 2023, greater than 18 years old and planned for RTSA for any indication were included in this study. Informed consent was obtained for all patients and ethics approval was obtained (HKU/HA HKW IRB Reference number: UW 21–111). Delta Xtend Reverse Shoulder System (DePuy Synthes, Raynham, Massachusetts, USA) was used in all cases. The metaglene (baseplate-peg-screw complex) has a 27 mm diameter with an 8 mm central peg and allows for four variable angle-locking screws. Patients with severe bone loss defined as Walch classification grade B2, B3 and C type were excluded from the study [15]. Native excessive glenoid surface superior tilt > 10 degrees or retroversion > 10 degrees, revision or conversion surgeries from hemi-arthroplasty were also excluded. Patient demographic information and fine-cut CT scans with ≤ 1.00 mm cuts were obtained from all patients. 3D reconstruction for glenoid geometry measurements, glenoid component roll angle and screw angulation for superior and inferior variable angle screws within 15 degrees were used. The dimensional assessments were calculated using Autodesk-Meshmixer software, version 3.5.474 (Autodesk, San Rafael, CA, USA).
Outcome measures
Glenoid anterior-posterior (AP) diameter and cranial-caudal (CC) dimensions were recorded (Fig. 1). Placement of metaglenes with a tilt angle nominal to the native glenoid surface was planned to minimize reaming while also avoiding superior tilt and retroversion more than 5 degrees (Fig. 2). All metaglenes were placed at the most inferior position with its inferior margin flush to the inferior margin of the native glenoid (Fig. 3). Subsequently, rotation of the metaglene is adjusted to optimize for the longest superior screw length, ensuring its placement into the dense bone through the glenoid vault corridor congruent with the base of the scapular spine6. The inferior screw is adjusted to maximize bi-cortical screw length within the scapula body. The glenoid roll angle (GRA) was defined as the angle between a line drawn from the supraglenoid tubercle through the glenoid component center (glenoid axis) and a line drawn through the center of the superior and inferior screw holes (metaglene axis) as show in Fig. 3. An anterior GRA was described as positive while posterior GRA described as negative. Superior and inferior screw trajectories were referenced in relation to the central pin. Cranial-caudal angles (CCA) and anterior-posterior angles (APA) were recorded for both screws. The APA angles were described as positive and negative in the posterior and anterior direction respectively. The maximal length of bi-cortical screws were also recorded.
Fig. 1.
Glenoid geometrical measurements. Orange line: Cranial-caudal diameter of glenoid fossa. Purple line: Anterior-posterior width of glenoid fossa
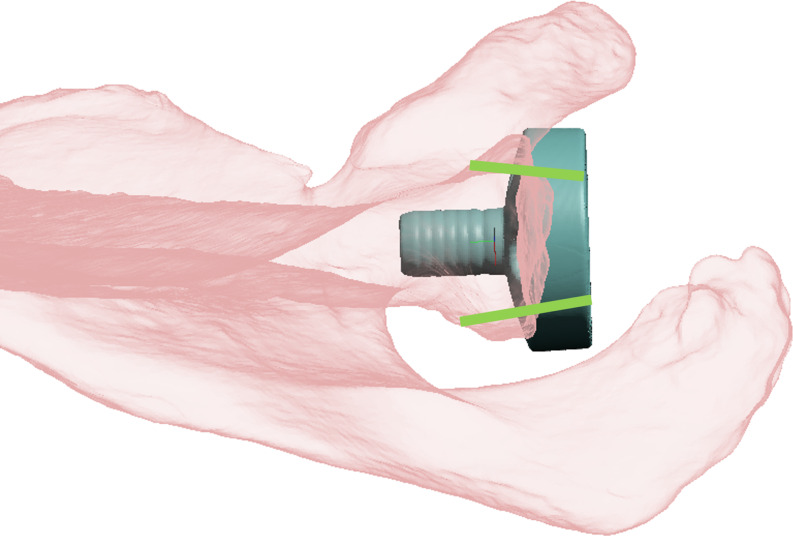
Fig. 2.
Patient specific modelling with metaglene placed nominal to the glenoid surface. Small glenoids in Asian population have inadequate or no bony purchase for anterior and/or posterior screws (green lines)
Fig. 3.
Glenoid Roll Angle (GRA) is the angle between the supraglenoid tubercle and center of metaglene line (orange) and a line intersecting the center of the superior and inferior screw holes of the metaglene representing the metaglene axis (purple)
Hypothesis testing and statistical analysis
To validate and investigate patient variation; the calculated averages (CA) for GRA, the superior screw angles (sCCA and sAPA), inferior screw angles (iCCA and iAPA) were re-inputted into a computer model for all cases and maximal screw lengths were recorded. These screw lengths were compared with their initial optimal screw lengths from PSI modelling using paired student t-test (SPSS version 27, Chicago, IL, USA). However, pragmatic replication of an accurate angle intra-operatively would be unrealistic. A pragmatic adaptation using rounded averages to the nearest 5 degrees for GRA, CCA and APA were also computed for each case to obtain maximal screw lengths. Statistical comparison with rounded averages (RA) screw length and initial PSI optimal screw lengths was performed using paired student t-test.
Results
A total of 171 cases fulfilled inclusion criteria. However, 38 cases were excluded due to significant glenoid defect, revision surgery or inadequate CT scan. Analysis was performed on 133 cases. There were 99 females (74.4%) and 34 were males (24.6%). The average age was 73.6 ± 7.6 years old (range: 51–92). Most cases (62.1%) were performed for four part proximal humerus fractures. While osteoarthritis accounted for 23.4% of cases and rotator cuff arthropathy in 13.7% of cases.
In this Asian population, the glenoid geometry measurements showed an average anterior-posterior diameter of 28.2 ± 4.5 mm (range: 18.2–47.8) and a craniocaudal diameter of 38.0 ± 4.6 mm (range: 30.3–53.4). The mean glenoid version is posteriorly tilted with a mean angle of -4.13°±4.6 (range: -16.8-8.8) relative to the scapula body. Significant differences between male and female in age, AP and CC diameters as shown in Table 1 with males having larger glenoid AP and CC diameters.
Table 1.
Patient demographics and glenoid geometrical measurements
| Female (n = 99) | Male (n = 34) | p-value | Combined average | |
|---|---|---|---|---|
| Age (years ± SD) | 74.6 ± 0.7 | 69.0 ± 1.3 | < 0.01 | 73.5 ± 7.6 |
| Glenoid A-P width (mm ± SD) | 27.5 ± 3.9 | 31.1 ± 5.2 | < 0.01 | 28.2 ± 4.5 |
| Glenoid C-C diameter (mm ± SD) | 37.1 ± 4.3 | 41.1 ± 4.3 | < 0.01 | 38.0 ± 4.6 |
| Glenoid Version (degree ± SD) | -4.3 ± 4.5 | -3.3 ± 4.7 | 0.33 | -4.1 ± 4.6 |
With patient specific modelling, the average GRA value was − 1.6°±5.3 (range: -15.7-13), representing its rotation in the anterior direction. The optimal superior screw placement showed an average sCCA of 9.1°±4.0 (range: -2-19) cranial and an average sAPA of 6.5°±4.8 (range: -11.2-17.6) angulated posteriorly as shown in Fig. 4. For the inferior screw, optimal iCCA was 11.2°±4.0 (range: 3.5–24.7) caudal and iAPA of ---0.7°±5.6 (range: -11.8-16.0) as shown in Fig. 5. The optimal bi-cortical screw lengths obtained were on average 51.3 ± 21.4 mm (range: 22.7–118) and 48.5 ± 8.6 mm (range: 24.9–84.5) for the superior and inferior screws respectively. There was a positive Pearson correlation between glenoid anterior-posterior diameter with both superior (R = 0.249, p < 0.01) and inferior screw lengths (R = 0.215 p = 0.02). Screw lengths and age did not have statistically significant correlation. No statistically significant differences were observed between gender and glenoid roll angle nor superior and inferior screw angles except the superior screw cranial angle, with males being 11.7°±3.52 and females 8.11°±3.65 (p < 0.01). However, the differences amounted to the same rounded average scenario for validation testing.
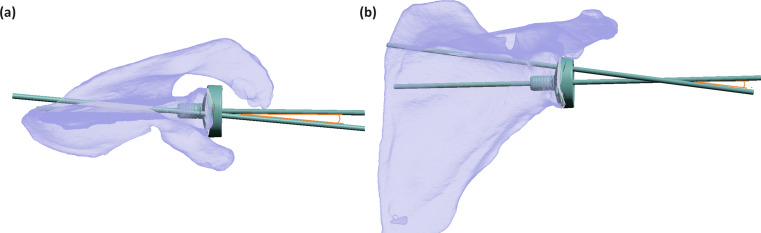
Fig. 4.
(a) Three-Dimensional view from above of the superior glenoid vault demonstrating the posterior orientation (6.5 degrees) in the optimal trajectory of the superior screw (blue), attributable to the relative posterior position of the scapular spine to the glenoid and slight glenoid retroversion relative to the scapular body. (b) AP view showing the optimal cranial angle of the superior screw (9.1 degrees)
Fig. 5.
Three-Dimensional view from below of the inferior glenoid vault demonstrating the slight anterior orientation (0.7 degrees) of the optimal trajectory of the inferior screw (green) due to the retroversion of the glenoid relative to the scapular body. (b) AP view showing the optimal caudal angle of the superior screw (11.2 degrees)
Computational modeling using the CA for all angles in each case yielded an average screw length of 40.6 ± 18.4 mm (range: 16.9–98.3) and 38.2 ± 10.9 mm (range: 13.4–90.8) for superior and inferior screws respectively. Paired sample t-test comparing to PSI optimal screw lengths was statistically significant (p-value < 0.01) as shown in Table 2 and summary. With RA computational modelling, maximal screw lengths were on average 40.5 ± 18.1 mm (range: 15.1-103.3) and 39.4 ± 9.7 mm (range: 17.2–71.7) for superior and inferior screws respectively. Paired sample t-test comparing RA and PSI modelling showed statistical significance with a p-value < 0.01. No statistical significance was found between the CA and RA modeling superior and inferior screw lengths (p = 0.89, p = 0.05 respectively). All re-computation modeling of screw trajectories in the CA and RA groups did not perforate the suprascapular notch nor the spinoglenoid notch predisposing to suprascapular nerve injury.
Table 2.
Mean maximal bi-cortical screw lengths attained from patient specific modelling compared to validation testing using calculated averages and rounded averages computer modelling
| Patient specific model | Calculated average model | Rounded average model | ANOVA test p-value | |||
|---|---|---|---|---|---|---|
| GRA (degrees) | PS | -1.6° | 0° | - | ||
| Superior Screw Angles (degrees) | PS | sCCA: 9.1° | sAPA: 6.5° |
sCCA: 10° |
sAPA: 5° |
- |
| Average Superior screw length (mm ± SD) | 51.3 ± 21.4 | 40.6 ± 18.3 | 40.5 ± 18.1 | < 0.01 | ||
| Inferior Screw Angles (degrees) | PS | iCCA: 11.2° | iAPA: -0.7° | iCCA: 10° | iAPA: 0° | - |
| Average inferior screw length (mm ± SD) | 48.5 ± 8.6 | 38.2 ± 10.9 | 39.4 ± 9.7 | < 0.01 | ||
*PS: Patient specific, sCCA: Superior screw cranial angle, sAPA: Superior screw anterior-posterior angle (posterior as positive value), iCCA: Inferior screw caudal angle, iAPA: Inferior screw anterior-posterior angle (anterior as negative value)
Discussion
The reverse shoulder arthroplasty developed by Grammont is a semi-constrained prosthesis with an increased deltoid fulcrum [16]. High stresses at the bone-prosthesis interface have led to catastrophic early failures. Obtaining strong early baseplate fixation is complicated by heterogenous glenoid geometry with different sizes and morphology. Data in Asian countries have shown an average glenoid width to often be less than the minimal metaglene diameter of various manufacturers (25–28 mm) especially in females [7, 14, 17]. A combined average of 28.2 ± 4.5 mm of glenoid diameter was found in our study population, comparable to Western anatomy as demonstrated by Mathews et al. [18]. However, in contrast our population included more proportion of males and pathological glenoid morphologies with 23.4% and 13.7% of the cases having osteoarthritis and rotator cuff arthropathy respectively. Osteophyte and glenoid erosion may lead to an overestimation of glenoid diameter in our study population. Axial glenoid morphology have been described to have different configurations offsetting anterior or posterior screws resulting in little to or no bony purchase [19]. Roche et al. demonstrated that only two screws for baseplate fixation conferred more implant displacement [20]. However, longer screw lengths showed better fixation irrespective of screw quantity – highlighting the importance of attaining maximal screw length in glenoid baseplate fixation.
A previous cadaveric study investigated glenoid baseplate rotation and screw length comparing baseplate rotation at 12 o’clock and 20 degrees rotation anterior or posterior [21]. The screw lengths obtained in a perpendicular angle and variable angle with baseplate rotation in these 3 positions were assessed. Results showed rotation at neutral (12 o’clock) and rotation anteriorly provided the longest screw lengths. However, the optimal degree of rotation and screw angulation were not measured. In this study utilizing 3D model computation – we can accurately define the best glenoid baseplate angular rotation (GRA) and screw angulation in two planes (CCA and APA) for maximizing bi-cortical screw length.
However, validation testing of the calculated angles against patient specific measurements, demonstrated statistically shorter screw lengths attainable. This illustrates the substantial patient anatomical variation and heterogeneity. Therefore, the use of ancillary operative technology to help improve accuracy is of great importance in RTSA. This has been shown in navigation assisted RTSA with improved baseplate and screw configurations [13, 22–24]. As well as in 3D planning with patient specific instrumentation, which has been shown to be reproducible and accurate with minimal deviation from pre-operative planning [25–27]. Studies on the outcomes of robotic assistance in reverse shoulder arthroplasty is also on the horizon [28].
The limitation of this study includes the use of a computational model specifically with circular metaglene systems and variable angle screws located directly superior and inferior to the central peg. We did not evaluate the screw lengths of implant designs using screws perpendicular to baseplate. Further biomechanical studies are required to determine the minimal length of screws required to limit micromotion and allow stable initial fixation. A previous study compared 18 mm and 36 mm screw lengths which showed significant difference in micromotion for the anterior, superior and inferior screws in a poor density bone model [29]. Micromotion in the 18 mm screw trials exceeded 150 μm required for bone ingrowth. However, differing screw lengths for floor and ceiling effects were not investigated.
Conclusion
In conclusion, the optimal average glenoid baseplate rotation was − 1.6°, close to perpendicular to the glenoid long axis. While optimal superior screw angulation was 9.1° cranial and 6.5° posterior. Inferior screw angulation of 11.2° caudal and 0.7° anterior, close to perpendicular to the glenoid plane. However, validation shows strong patient heterogeneity and anatomical variation. Nonetheless, as demonstrated from the pragmatic, rounded averages simulation – long screw lengths of > 38 mm for both superior and inferior screws were attainable with a good safety profile. Surgeons may consider the additional use of navigation-assisted, or 3D printed patient specific instrumentation to optimize baseplate and screw configuration in reverse shoulder arthroplasty.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Acknowledgements
The Tam Shiu Anatomical Modeling and 3D Printing Laboratory at the University of Hong Kong.
Author contributions
All authors contributed to the study conception and design. Data measurement and collection were performed by Martin Shun Sing Cheng, Samuel De Hoi Wong, Christopher Chun Hei Yip, Issac Jun Ren Khoo, Tsoi Wan Karen Wong. The data analysis was performed by Martin Shun Sing Cheng, Colin Shing-Yat Yung, Christian Fang. The first draft of the manuscript was written by Martin Shun Sing Cheng, Colin Shing-Yat Yung and Christian Fang and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Funding
Open access funding provided by The University of Hong Kong.
Data availability
Not applicable.
Declarations
Ethical approval
This study was performed in line with the principles of the Declaration of Helsinki. Approval was granted by the Ethics Committee of University of Hong Kong (HKU/HA HKW IRB Reference number: UW 21–111).
Informed consent
Informed consent was obtained from all individual participants included in the study.
Consent for publication
All authors consented for publication. Our manuscript did not contain any individual person’s data in any form.
Conflict of interest
The authors declare they have no conflicts of interests including no relevant financial or non-financial interests to disclose.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Familiari F, Rojas J, Nedim Doral M, Huri G, McFarland EG (2018) Reverse total shoulder arthroplasty. EFORT Open Rev 3(2):58–69 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Boileau P (2016) Complications and revision of reverse total shoulder arthroplasty. Orthop Traumatol Surg Res 102(1 Suppl):S33–43 [DOI] [PubMed] [Google Scholar]
- 3.DiStefano JG, Park AY, Nguyen TQ, Diederichs G, Buckley JM, Montgomery WH 3rd (2011) Optimal screw placement for base plate fixation in reverse total shoulder arthroplasty. J Shoulder Elb Surg 20(3):467–476 [DOI] [PubMed] [Google Scholar]
- 4.Chebli C, Huber P, Watling J, Bertelsen A, Bicknell RT, Matsen F 3rd (2008) Factors affecting fixation of the glenoid component of a reverse total shoulder prothesis. J Shoulder Elb Surg 17(2):323–327 [DOI] [PubMed] [Google Scholar]
- 5.Humphrey CS, Kelly JD 2nd, Norris TR (2008) Optimizing glenosphere position and fixation in reverse shoulder arthroplasty, part two: the three-column concept. J Shoulder Elb Surg 17(4):595–601 [DOI] [PubMed] [Google Scholar]
- 6.Codsi MJ, Bennetts C, Powell K, Iannotti JP (2007) Locations for screw fixation beyond the glenoid vault for fixation of glenoid implants into the scapula: an anatomic study. J Shoulder Elbow Surg 16(3):S84–S9 [DOI] [PubMed] [Google Scholar]
- 7.Matsuki K, Sugaya H, Hoshika S, Ueda Y, Takahashi N, Tokai M et al (2019) Three-dimensional measurement of glenoid dimensions and orientations. J Orthop Sci 24(4):624–630 [DOI] [PubMed] [Google Scholar]
- 8.James J, Allison MA, Werner FW, McBride DE, Basu NN, Sutton LG et al (2013) Reverse shoulder arthroplasty glenoid fixation: is there a benefit in using four instead of two screws? J Shoulder Elb Surg 22(8):1030–1036 [DOI] [PubMed] [Google Scholar]
- 9.Cabarcas BC, Cvetanovich GL, Gowd AK, Liu JN, Manderle BJ, Verma NN (2019) Accuracy of patient-specific instrumentation in shoulder arthroplasty: a systematic review and meta-analysis. JSES Open Access 3(3):117–129 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Dallalana RJ, McMahon RA, East B, Geraghty L (2016) Accuracy of patient-specific instrumentation in anatomic and reverse total shoulder arthroplasty. Int J Shoulder Surg 10(2):59–66 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Gomes NS (2016) Patient-specific instrumentation for total shoulder arthroplasty. EFORT Open Rev 1(5):177–182 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Heylen S, Van Haver A, Vuylsteke K, Declercq G, Verborgt O (2016) Patient-specific instrument guidance of glenoid component implantation reduces inclination variability in total and reverse shoulder arthroplasty. J Shoulder Elbow Surg 25(2):186–192 [DOI] [PubMed] [Google Scholar]
- 13.Kircher J, Wiedemann M, Magosch P, Lichtenberg S, Habermeyer P (2009) Improved accuracy of glenoid positioning in total shoulder arthroplasty with intraoperative navigation: a prospective-randomized clinical study. J Shoulder Elb Surg 18(4):515–520 [DOI] [PubMed] [Google Scholar]
- 14.Yung CS, Fang C, Fang E, Siu YC, Yee DKH, Wong KK et al (2023) Surgeon-designed patient-specific instrumentation improves glenoid component screw placement for reverse total shoulder arthroplasty in a population with small glenoid dimensions. Int Orthop 47(5):1267–1275 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Walch G, Badet R, Boulahia A, Khoury A (1999) Morphologic study of the glenoid in primary glenohumeral osteoarthritis. J Arthroplasty 14(6):756–760 [DOI] [PubMed] [Google Scholar]
- 16.Boileau P, Watkinson D, Hatzidakis AM, Hovorka I (2006) Neer Award 2005: the Grammont reverse shoulder prosthesis: results in cuff tear arthritis, fracture sequelae, and revision arthroplasty. J Shoulder Elbow Surg 15(5):527–540 [DOI] [PubMed] [Google Scholar]
- 17.Mizuno N, Nonaka S, Ozaki R, Yoshida M, Yoneda M, Walch G (2017) Three-dimensional assessment of the normal Japanese glenoid and comparison with the normal French glenoid. Orthop Traumatology: Surg Res 103(8):1271–1275 [DOI] [PubMed] [Google Scholar]
- 18.Slocum AMY, Siu YC, Ma CM, Lui TH (2021) The study of 2-dimensional computed tomography scans of the glenoid anatomy in relation to reverse shoulder arthroplasty in the Southern Chinese population. JSES Int 5(4):714–721 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Roche C, DiGeorgio C, Yegres J, VanDeven J, Stroud N, Flurin PH et al (2019) Impact of screw length and screw quantity on reverse total shoulder arthroplasty glenoid fixation for 2 different sizes of glenoid baseplates. JSES Open Access 3(4):296–303 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Parsons BO, Gruson KI, Accousti KJ, Klug RA, Flatow EL (2009) Optimal rotation and screw positioning for initial glenosphere baseplate fixation in reverse shoulder arthroplasty. J Shoulder Elb Surg 18(6):886–891 [DOI] [PubMed] [Google Scholar]
- 21.Hones KM, King JJ, Schoch BS, Struk AM, Farmer KW, Wright TW (2021) The in vivo impact of computer navigation on screw number and length in reverse total shoulder arthroplasty. J Shoulder Elb Surg 30(10):e629–e35 [DOI] [PubMed] [Google Scholar]
- 22.Sprowls GR, Wilson CD, Stewart W, Hammonds KAP, Baruch NH, Ward RA et al (2021) Intraoperative navigation and preoperative templating software are associated with increased glenoid baseplate screw length and use of augmented baseplates in reverse total shoulder arthroplasty. JSES Int 5(1):102–108 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Velasquez Garcia A, Abdo G (2023) Does computer-assisted navigation improve baseplate screw configuration in reverse shoulder arthroplasty? A systematic review and meta-analysis of comparative studies. J Orthop 36:29–35 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Lilley BM, Lachance A, Peebles AM, Powell SN, Romeo AA, Denard PJ et al (2022) What is the deviation in 3D preoperative planning software? A systematic review of concordance between plan and actual implant in reverse total shoulder arthroplasty. J Shoulder Elb Surg 31(5):1073–1082 [DOI] [PubMed] [Google Scholar]
- 25.Marcoin A, Nerot C, Lestra T, Blasco L, Ferrier A, Siboni R et al (2020) The precision of patient-specific instrumentation guides for the positioning of the glenoid component in total reverse shoulder arthroplasty: an in vivo scanographic study. Int Orthop 44(9):1761–1766 [DOI] [PubMed] [Google Scholar]
- 26.Kwak JM, Jeon IH, Kim H, Choi S, Lee H, Koh KH (2022) Patient-specific instrumentation improves the reproducibility of preoperative planning for the positioning of baseplate components with reverse total shoulder arthroplasty: a comparative clinical study in 39 patients. J Shoulder Elb Surg 31(7):1488–1498 [DOI] [PubMed] [Google Scholar]
- 27.Zeng GJ, Sheng X, Lie DTT (2023) Short- to medium-term outcomes and future direction of reverse shoulder arthroplasty: current concepts. J Isakos 8(6):398–403 [DOI] [PubMed] [Google Scholar]
- 28.Lung TS, Cruickshank D, Grant HJ, Rainbow MJ, Bryant TJ, Bicknell RT (2019) Factors contributing to glenoid baseplate micromotion in reverse shoulder arthroplasty: a biomechanical study. J Shoulder Elb Surg 28(4):648–653 [DOI] [PubMed] [Google Scholar]
- 29.Mathews S, Burkhard M, Serrano N, Link K, Häusler M, Frater N, Franke I, Bischofberger H, Buck FM, Gascho D, Thali M, Steffen Serowy, Magdalena Müller-Gerbl, Gareth Harper, Ford Qureshi, Thomas Böni, Bloch H-R, Ullrich O, Rühli F-J (2017) & Elisabeth Eppler Glenoid morphology in light of anatomical and reverse total shoulder arthroplasty: a dissection- and 3D-CT-based study in male and female body donors: BMC Musculoskeletal Disorders 18, Article number: 9 [DOI] [PMC free article] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Not applicable.