Abstract
Objectives:
The diagnosis of infertility affects between 8–12% of couples of childbearing age worldwide. It is difficult to manage infertility, which often generates anxiety and depression.
Material and methods:
We conducted a study that included women of childbearing age who were unsuccessful in getting pregnant. Our research was based on a questionnaire distributed online via social media and it was carried out over a period of two months. The questionnaire comprised 35 questions and intended to highlight the psychological impact of infertility diagnosis on the female participants in the present study.
Results:
A total of 486 women with a diagnosis of infertility responded to the online questionnaire. Subjects had an average age between 31 and 40 years (58.4%) and most of them (80.2%) came from urban areas. It was found that 38.1% of patients experienced a very high level of stress generated by their infertility diagnosis and 54.7% stated that their greatest fear was that they would never get pregnant; 41.4% of these patients claimed that their quality of life was affected and 31.7% indicated a negative impact even on their couple life. Of all participants to the questionnaire, 96.6% stated that the costs of treatments or even assisted reproduction procedures were an additional stress and 73.7% believed that religion played an important moral role.
Conclusions:
The women who were enrolled in the current study recognized the negative impact of their infertility diagnosis on both themselves and their couple's lives. At the same time, they believed in Divine help and looked optimistically to the future in terms of achieving pregnancy.
Keywords:
infertility, psychological impact, religion, costs, couple life.
Introduction
Infertility has been defined as the impossibility of achieving pregnancy after six or 12 months of unprotected sexual intercourse, depending on the age of the partners; it has been estimated that about 8% to 12% of couples of childbearing age worldwide experience this diagnosis (1). It was established that 85% of all causes of infertility were known, while 15% of couples had infertility with no identified cause (2).
There has been a significant decline in the number of births over the last half century, which has been linked to economic and behavioral factors as well as biological aspects (3). The inability to achieve pregnancy, especially in young couples, or failure to complete a pregnancy is a major health problem (4). There has been evidence of a decrease in the number of abortions on demand, which was also associated with a descendant trend in overall conception (5).
Several research articles have claimed that infertility could be a real challenge for couples, most commonly dealing with depression and anxiety (6). According to a recent study, these symptoms affected on average between 25 and 53% of women just before the start of medical treatment or assisted reproduction techniques (7) and between 40 and 75% of women undergoing treatment (8). The diagnosis of infertility was complex and ambiguous, and the condition itself could exacerbate feelings of anxiety in already affected patients (9).
A study conducted on 160 married couples who were in the process of infertility treatments. It was found that women had higher levels of anxiety and depression compared to men (10). Comparing with the general population, both women and men of infertile couples were about twice as affected by anxiety and depression (11).
Another study conducted in Japan in 2021 used a web-based questionnaire involving 254 women who received treatment for infertility and concluded that infertile women experienced stigma and were mostly anxious and depressed (12) or believed their identity was threatened (13). The results of the study indicated that psychoeducation or cognitive therapy may significantly ameliorate these perceptions (14).
The focus of the present study was to demonstrate the psychological impact of infertility on Romanian women, the associated treatment cost barrier and how they and their partner consider the fertility outcome.
MATERIAL AND METHODS
The prospective study was conducted over a period of two months (20 January – 25 March 2024) by distributing a questionnaire using social media. The questionnaire targeted women with infertility who lived in the south area of Romania and had an above middle economic status educational level; it included 35 questions aimed at highlighting the psychological impact of infertility on the female respondents. The recruitment process was conducted through social media by distributing an online questionnaire to be completed by the study participants. All subjects answered the question "Are you experiencing a diagnosis of infertility?", and those who answered "no" ended their participation and were excluded from the questionnaire-based study.
Inclusion criteria were as follows: women’s age over 18 years, impossibility of conception for a period of minimum six months, women with a stable marital status or a stable relationship who have already been diagnosed with infertility or were even undergoing treatment to achieve pregnancy.
Questionnaire items included age, origin, height and weight, personal pathological history, tobacco use, paraclinical methods of diagnosis or treatment and the impact of infertility on participants through questions such as "How strongly does the diagnosis of infertility affect you?", "Do you consider the future optimistic for your family?", "How many hours do you sleep per night?", "How do you evaluate the level of stress induced by the infertility diagnosis (rated from 1 to 5)?", etc.
Exclusion criteria were male infertility (without female pathology) and age of partners less than 18 years.
Data were statistically analysed using IBM SPSS Statistics 21 program, p≤0.05 values were considered statistically. The statistical tests used for data analysis were Chi-Square, Mann-Whitney U, Spearman correlation indicator and Phi correlation coefficient.
RESULTS
RESULTS
The present study included 486 women who accomplished the inclusion criteria. Regarding the age of patients, it was found that 0.8% of subjects were less than 20 years old (n=4), 29.4% between 21 and 30 years old (n=143), 58.4% between 31 and 40 years old (n=284), and 11.3% (n=55) over 41 years old.
Of the total number of women included in the study, 80.2% (n=390) lived in urban areas, and 19.8% (n=96) in rural areas.
In terms of body weight, 10.3% of patients mentioned that they weighed less than 50 kg (n=50), 15.0% between 71 kg and 80 kg (n=73), and 13.2% more than 81 kg (n=64). It was not possible to calculate the body mass index (BMI) because no correlation could be made between the weights and heights of participants.
Regarding consumption of tobacco, 29.0% (n=141) of all patients responded they were smokers, and 71.0% (n=345) non-smokers. 55.3% (n=269) of respondents denied any personal pathology. Of the total of 44.7% (n=217) who stated that they had health problems, the most frequently reported ones included endometriosis (34.4%, n=167), followed by autoimmune thyroiditis (30.9%, n=67), micropolycystic ovaries (19.5%, n=95), hypertension (7.8%, n=17), and type 2 diabetes mellitus (2.3%, n=5). Breast pathology, uterine malformations, psychiatric pathology, and adenomyosis or fibromatous uterus were also mentioned by a minority of patients.
In terms of obtaining a pregnancy, 58.6% (n=285) of all respondents stated that they never had either spontaneously or through assisted reproduction techniques. 5.8% of them had only one ectopic pregnancy in the past (n=28), and 11.5% (n=56) experienced a miscarriage.
Of all study participants, 70.8% (n=344) were diagnosed with primary or secondary infertility, 52.3% (n=254) were evaluated by hysteroscopy, and 62.1% (n=301) underwent hysterosalpingography or hysterosonography. Patients claimed that 44.4% (n=216) had undergone assisted reproductive techniques, and 35.2% (n=171) indicated that their partners had modified spermograms associated.
Regarding stress, it was found that 38.1% (n=185) of patients experienced a very high level of stress generated by their infertility diagnosis. Furthermore, 54.7% (n=266) stated that their greatest fear was that they would never get pregnant; 41.4% (n=201) reported that major stress affected their quality of life and 31.7% (n=154) claimed a negative impact on their couple life.
Of all participants, 33.5% (n=163) stated that they were able to carry out their physical activity as before their infertility diagnosis and only 10.5% (n=51) claimed that their daily activity was significantly negatively affected.
Patients responding to the questionnaire stated that the cost of treatment was an additional stress factor in 96.6% of cases (n=387). In 6.8% of services (n=33), patients were not satisfied with the doctor's attitude in terms of identifying and treating the cause of infertility, while 46.9% (n=228) found that the doctor was empathetic, interested and willing to answer questions and find solutions.
DISCUSSIONS
Of the total number of 486 patients who responded to questionnaires, the largest group included women aged between 31 and 40 (58.4%) and the fewest were aged under 20 (0.8%). A previous study published in 2023 included patients aged between 20 and 40 years, and those diagnosed with infertility had an average age of 32 years (15). Infertility had multiple causes but the increased risk of infertility has most often been associated with low ovarian reserve and accelerates after the age of 30 (16).
Numerous studies in the literature have shown that obesity had a major negative impact on women's fertility, and its management may contribute to infertility diagnosis (17). Among women included in our study, only 28.2% of subjects weighed over 71 kg, with 13.2% having a body weight of more than 81 kg.
The negative impact of nicotine use on fertility has been widely discussed. A study conducted on 3,665 women aged 18 to 45 showed that the risk of infertility increased by 41.8% among smokers compared to never smokers (18). In the current study, 71.0% of participants denied cigarette smoking.
In most patients, the diagnosis of infertility was associated with severe physical, psychological, and financial stress (19). A study of 352 women with infertility showed that 56.5% were depressed and 75.9% had anxiety. Failure to achieve pregnancy after long periods of effort and pregnancy loss were also correlated with increased diagnoses of depression and anxiety (21, 22). A Danish study of 42,000 women with infertility showed that 35% were diagnosed with depression (23). A different study, that included 51,222 Danish women, showed that the risk of suicide was twice as significant among women who were unsuccessful in getting pregnant compared to those who had at least one child (24). The findings of the present study were similar to those published in the literature; most of the women who responded to the questionnaire stated that infertility had a negative impact on both themselves and their conjugal life.
A study published in 2022 found that mental disorders were on the rise in women diagnosed with infertility (25) but argued that this type of disorder could be easily overlooked (26, 27). Diagnosing and supporting these women (28) and getting them the necessary therapies could positively influence their infertility diagnosis (29).
In terms of daily activities, only one tenth of patients reported that they were strongly affected by the infertility diagnosis, while one third of them stated that this diagnosis did not affect their daily activities and their performance status was similar to the pre-diagnosis one. Studies have revealed the inverse association of the quality of life with stress generated by infertility diagnosis (30) as well as the association with sadness, quality of couple life (31), and quality of sleep (32).
A study published in 2019 claimed that monthly household income and causes of infertility were significantly related to the quality of life. Stress related to infertility diagnosis was negatively correlated with participants' quality of life; in general, women interviewed had relatively low quality of life scores (33).
Hoping has given women perspective in their fight against infertility. In a study that included 100 women of childbearing age with infertility diagnosis, it was found that 57% of them stated they would continue to do whatever was necessary until they succeeded (34).
The costs of investigations and assisted reproduction techniques for infertile couples were defined as substantial (35), which had a considerable emotional impact as it was a factor generating stress in both women and men (36). 96.6% of the women who responded to the questionnaire considered the costs of treatments to achieve pregnancy as an additional major stress factor.
Psychological interventions have been shown to be helpful for infertility patients; their efficiency has been directly associated with stress management and coping skills training as well as the ability to optimistically regard the future (37). Concerning the results of the questionnaire completed by participants in our study, only 16.9% of subjects admitted they used to sleep less than six hours a night. It was noticed that religion was very important for most of our respondents. Previously published studies have equally pointed out that religious faith was a protective factor for psychological distress in infertile couples (38).
Conversely, culture and religion have historically been obstacles to the early acceptance of assisted reproductive techniques, particularly in the Middle East and to a lesser extent in Europe, due to cultural and religious differences. As the development of assisted reproductive technologies progressed, public opinion has varied considerably around the world (39). Conservative Protestants and more religious people were found to be more likely to disapprove of ART (40). Religion has historically played an important role in mediating the difficulties experienced by infertile women. A study of 168 women with infertility aimed to support the relationship between coping mechanisms through religion and adaptation in the situation of infertility diagnosis (41).
Our study limitation consists in a heterogeneity of the respondents’ economic and educational level. Although the population included in the present study was living in the highest income region of the country, with good medical infrastructure and access to medical facilities, including infertility clinics, there would be interesting to further evaluate which group of patients would be more exposed to psychoemotional and financial stress related to infertility in terms of education, marital status, or economic income.
Another limitation is the fact that respondents could not be divided into groups who either benefitted from government financial endorsement of ART procedures or had to pay by themselves. In Romania, there is a governmental support for one in vitro fertilization procedure for the couples who meet some conditions. Moreover, in the region where we conducted the study, the local administration offered some financial support for that particular service, which could alleviate some of the financial and psychoemotional burden.
We intend to extend the study and evaluate a profile of women who are prone to be very susceptible to that kind of burden and advance a system of support for such persons in their journey toward a successful pregnancy.
CONCLUSIONS
Women enrolled in the present study recognized the negative impact of their infertility diagnosis on both themselves and their couple's lives. At the same time, they believed in Divine help and looked optimistically to the future in terms of achieving pregnancy.
It was helpful that their doctor also recommended psychological counselling, which played an important role in managing the emotions related to the infertility diagnosis in addition to treatments to cure the pathology.
The moral support of women diagnosed with infertility could also be improved by increasing government funding for infertility treatments as well as by adopting increased psychological assistance programs. There are still considerable financial concerns for women around the world who have been diagnosed with infertility. Therefore, financial and psychological support would most likely improve the situation for these women.
Conflicts of interest: none declared.
Financial support: none declared.
FIGURE 1.
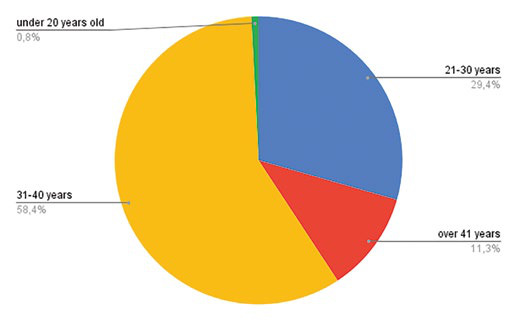
Age distribution of respondents
TABLE 1.
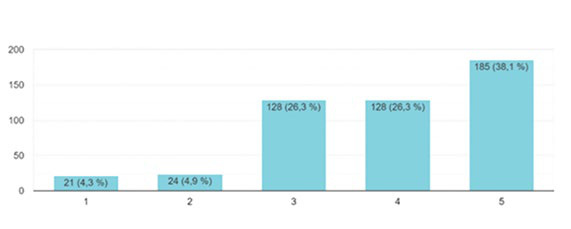
Level of stress induced by infertility diagnosis (1= insignificant, 5=major impact)
FIGURE 2.
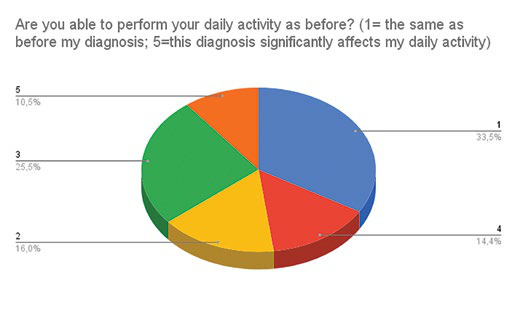
The impact of infertility diagnosis on daily activities
TABLE 2.
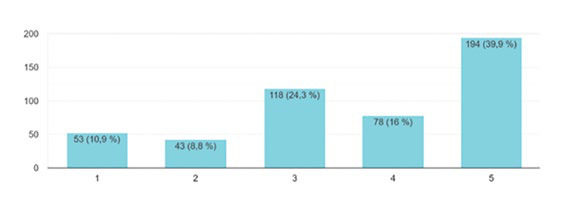
How optimistic respondents were about getting pregnant in the next 12 months (1=pessimistic; 5=optimistic)
Contributor Information
Cristina Diana POPESCU, Department PhD, IOSUD, “Carol Davila” University of Medicine and Pharmacy, Bucharest, Romania.
Romina Marina SIMA, Department of Obstetrics and Gynaecology, “St John” Hospital, “Bucur” Maternity, Bucharest, Romania; “Carol Davila” University of Medicine and Pharmacy, Bucharest, Romania.
Denisa Oana BALALAU, Department of Obstetrics and Gynaecology, “St John” Hospital, “Bucur” Maternity, Bucharest, Romania; “Carol Davila” University of Medicine and Pharmacy, Bucharest, Romania.
Mihaela AMZA, Department of Obstetrics and Gynaecology, “St John” Hospital, “Bucur” Maternity, Bucharest, Romania; “Carol Davila” University of Medicine and Pharmacy, Bucharest, Romania.
Delia BOGHEANU, Department of Obstetrics and Gynaecology, “St John” Hospital, “Bucur” Maternity, Bucharest, Romania.
Liana PLES, Department of Obstetrics and Gynaecology, “St John” Hospital, “Bucur” Maternity, Bucharest, Romania; “Carol Davila” University of Medicine and Pharmacy, Bucharest, Romania.
References
- 1.Vander Borght M, Wyns C. Fertility and infertility: Definition and epidemiology. Clin Biochem. 2018;62:2–10. doi: 10.1016/j.clinbiochem.2018.03.012. [DOI] [PubMed] [Google Scholar]
- 2.Carson SA, Kallen AN. Diagnosis and Management of Infertility: A Review. JAMA. 2021;326:65–76. doi: 10.1001/jama.2021.4788. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Skakkebæk NE, Lindahl-Jacobsen R, Levine H, et al. Environmental factors in declining human fertility. Nat Rev Endocrinol. 2022;18:139–157. doi: 10.1038/s41574-021-00598-8. [DOI] [PubMed] [Google Scholar]
- 4.Zegers-Hochschild F, Adamson GD, Dyer S, et al. The International Glossary on Infertility and Fertility Care, 2017. Hum Reprod. 2017;32:1786–1801. doi: 10.1093/humrep/dex234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Vollset SE, Goren E, Yuan CW, et al. Fertility, mortality, migration, and population scenarios for 195 countries and territories from 2017 to 2100: a forecasting analysis for the Global Burden of Disease Study. Lancet. 2020;396:1285–1306. doi: 10.1016/S0140-6736(20)30677-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wdowiak A, Makara-Studzińska M, Raczkiewicz D, Cyranka K. Reproductive problems and intensity of anxiety and depression in women treated for infertility. Psychiatr Pol. 2022;56:153–170. doi: 10.12740/PP/125885. [DOI] [PubMed] [Google Scholar]
- 7.Clifton J, Parent J, Seehuus M, et al. An internet-based mind/body intervention to mitigate distress in women experiencing infertility: A randomized pilot trial. PLoS One. 2020;15:e0229379. doi: 10.1371/journal.pone.0229379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Pasch LA, Holley SR, Bleil ME, et al. Addressing the needs of fertility treatment patients and their partners: are they informed of and do they receive mental health services? Fertil Steril. 2016;106:209–215. doi: 10.1016/j.fertnstert.2016.03.006. [DOI] [PubMed] [Google Scholar]
- 9.Meyers AJ, Domar AD. Research-supported mobile applications and internet-based technologies to mediate the psychological effects of infertility: a review. Reprod Biomed Online. 2021;42:679–685. doi: 10.1016/j.rbmo.2020.12.004. [DOI] [PubMed] [Google Scholar]
- 10.Kumar R, Dhillon HS, Hashim U, et al. Anxiety and depression among couples undergoing treatment for infertility with assisted reproductive techniques at an Indian centre. Natl Med J India. 2023;36:286–290. doi: 10.25259/NMJI_170_21. [DOI] [PubMed] [Google Scholar]
- 11.Hasanpoor-Azghdy SB, Simbar M, Vedadhir A. The emotional-psychological consequences of infertility among infertile women seeking treatment: Results of a qualitative study. Iran J Reprod Med. 2014;12:131–138. [PMC free article] [PubMed] [Google Scholar]
- 12.Anderson K, Norman RJ, Middleton P. Preconception lifestyle advice for people with subfertility. Cochrane Database Syst Rev 1010. [DOI] [PubMed]
- 13.Yokota R, Okuhara T, Okada H, et al. Association between Stigma and Anxiety, Depression, and Psychological Distress among Japanese Women Undergoing Infertility Treatment. Healthcare (Basel) 2022. [DOI] [PMC free article] [PubMed]
- 14.Ishihara O, Jwa SC, Kuwahara A, et al. Assisted reproductive technology in Japan: A summary report for 2017 by the Ethics Committee of the Japan Society of Obstetrics and Gynecology. Reprod Med Biol. 2019;19:3–12. doi: 10.1002/rmb2.12307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Popescu CD, Sima RM, Amza M, et al. Hysteroscopy for Infertility in Young Women – Our Experience. Maedica (Bucur) 2023. [DOI] [PMC free article] [PubMed]
- 16.Lee Y, Bohlin J, Page CM, et al. Associations between epigenetic age acceleration and infertility. Hum Reprod. 2022;37:2063–2074. doi: 10.1093/humrep/deac147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Wen Z, Li X. Association between weight-adjusted-waist index and female infertility: a population-based study. Front Endocrinol (Lausanne) 2023. [DOI] [PMC free article] [PubMed]
- 18.He S, Wan L. Associations between smoking status and infertility: a cross-sectional analysis among USA women aged 18-45 years. Front Endocrinol (Lausanne) 2023. [DOI] [PMC free article] [PubMed]
- 19.Holley SR, Pasch LA, Bleil ME, et al. Prevalence and predictors of major depressive disorder for fertility treatment patients and their partners. Fertil Steril. 2015;103:1332–1339. doi: 10.1016/j.fertnstert.2015.02.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Rooney KL, Domar AD. The relationship between stress and infertility. Dialogues Clin Neurosci. 2018;20:41–47. doi: 10.31887/DCNS.2018.20.1/klrooney. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Pasch LA, Holley SR, Bleil ME, et al. Addressing the needs of fertility treatment patients and their partners: are they informed of and do they receive mental health services? Fertil Steril. 2016;106:209–215. doi: 10.1016/j.fertnstert.2016.03.006. [DOI] [PubMed] [Google Scholar]
- 22.Jannink T, Bordewijk EM, Aalberts J, et al. Anxiety, depression, and body image among infertile women with and without polycystic ovary syndrome. Hum Reprod. 2024;39:784–791. doi: 10.1093/humrep/deae016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Sejbaek CS, Hageman I, Pinborg A, et al. Incidence of depression and influence of depression on the number of treatment cycles and births in a national cohort of 42,880 women treated with ART. Hum Reprod. 2013;28:1100–1109. doi: 10.1093/humrep/des442. [DOI] [PubMed] [Google Scholar]
- 24.Kjaer TK, Jensen A, Dalton SO, et al. Suicide in Danish women evaluated for fertility problems. Hum Reprod. 2011;26:2401–2407. doi: 10.1093/humrep/der188. [DOI] [PubMed] [Google Scholar]
- 25.Szigeti F J, Sexty RE, Szabó G, et al. The SCREENIVF Hungarian version is a valid and reliable measure accurately predicting possible depression in female infertility patients. Sci Rep. 2024;14:12880. doi: 10.1038/s41598-024-63673-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Hazlina NHN, Norhayati MN, Bahari SI, et al. Worldwide prevalence, risk factors and psychological impact of infertility among women: a systematic review and meta-analysis. BMJ Open. 2022;12:e057132. doi: 10.1136/bmjopen-2021-057132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Zhang H, Hua L, Liu D, et al. Effects of physical activity on infertility in reproductive females. Reprod Biol Endocrinol. 2024;22:62. doi: 10.1186/s12958-024-01234-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Ling S, Dai Y, Weng R, et al. Epidemiologic and genetic associations of female reproductive disorders with depression or dysthymia: a Mendelian randomization study. Sci Rep. 2024;14:5984. doi: 10.1038/s41598-024-55993-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Larsen U. Research on infertility: which definition should we use? Fertil Steril. 2005;83:846–852. doi: 10.1016/j.fertnstert.2004.11.033. [DOI] [PubMed] [Google Scholar]
- 30.Thanscheidt CL, Wischmann T. Systematic Review: Risk Factors of Anxiety, Depressiveness, and (Lack of) Social Support in Women and Men Prior to Assisted Reproduction. Geburtshilfe Frauenheilkd. 2023;83:1350–1360. doi: 10.1055/a-2166-4374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Choi Y, Moon SH. Types and Characteristics of Stress Coping in Women Undergoing Infertility Treatment in Korea. Int J Environ Res Public Health. 2023;20:2648. doi: 10.3390/ijerph20032648. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Kiesswetter M, Marsoner H, Luehwink A, et al. Impairments in life satisfaction in infertility: Associations with perceived stress, affectivity, partnership quality, social support and the desire to have a child. Behav Med. 2020;46:130–141. doi: 10.1080/08964289.2018.1564897. [DOI] [PubMed] [Google Scholar]
- 33.Li Y, Zhang X, Shi M, et al. Resilience acts as a moderator in the relationship between infertility-related stress and fertility quality of life among women with infertility: a cross-sectional study. Health Qual Life Outcomes. 2019;17:38. doi: 10.1186/s12955-019-1099-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Abramov M, Shalom-Paz E, Benyamini Y. Persevering in Fertility Treatments Despite Failures: Unrealistic Optimism and the Reality of a Pronatalist Culture. Int J Behav Med. 2022;29:209–219. doi: 10.1007/s12529-021-10001-5. [DOI] [PubMed] [Google Scholar]
- 35.Le KD, Vuong LN, Ho TM, et al. A cost-effectiveness analysis of freeze-only or fresh embryo transfer in IVF of non-PCOS women. Hum Reprod. 2018;33:1907–1914. doi: 10.1093/humrep/dey253. [DOI] [PubMed] [Google Scholar]
- 36.Braam SC, Ho VNA, Pham TD, et al. In-vitro maturation versus IVF: a cost-effectiveness analysis. Reprod Biomed Online, 2021. [DOI] [PubMed]
- 37.Cousineau TM, Domar AD. Psychological impact of infertility. Best Pract Res Clin Obstet Gynaecol. 2007;21:293–308. doi: 10.1016/j.bpobgyn.2006.12.003. [DOI] [PubMed] [Google Scholar]
- 38.Jurić Vukelić D, Kušević Z, Vuksan-Ćusa B. The Role of Religiosity in Coping with Infertility Treatment. Psychiatr Danub 2021. [PubMed]
- 39.Serour GI, Serour AG. The impact of religion and culture on medically assisted reproduction in the Middle East and Europe. Reprod Biomed Online. 2021;43:421–433. doi: 10.1016/j.rbmo.2021.06.002. [DOI] [PubMed] [Google Scholar]
- 40.Adamczyk A, Suh B, Lerner L. Analysis of the relationship between religion, abortion, and assisted reproductive technology: Insights into cross-national public opinion. Soc Sci Res. 2024;120:103012. doi: 10.1016/j.ssresearch.2024.103012. [DOI] [PubMed] [Google Scholar]
- 41.Demirel G, Taskin Yilmaz F, Yenicesu AG. The Relation Between Religious Coping, Adjustment to Fertility, Being Affected by Infertility, and Satisfaction with Life in Turkish Women with Infertility. J Relig Health. 2021;60:4264–4277. doi: 10.1007/s10943-021-01319-1. [DOI] [PubMed] [Google Scholar]


