Abstract
Background
Opioids are important medications that are used to control postoperative pain. The enhanced recovery after surgery (ERAS) program has reduced opioid use after surgery. In a surgical practice with a robust ERAS program, we wanted to determine if there was a relationship between in-hospital opioid use and postoperative complications.
Methods
We performed a retrospective nested case-control study of patients who underwent thoracic surgical intervention at the Houston Methodist Hospital (HMH) between 11/2020 and 11/2021 from the thoracic surgery database with hospital morphine milligram equivalent (MME) information, comparing patients who did and did not experience postoperative complications. We determined the total MME and average daily MME patients received during their hospitalization. We performed receiver operating characteristic (ROC) curve analysis with the Youden index to determine the optimal cutoff points for total MME and daily MME. We performed univariable and multivariable logistic regression analyses of the factors associated with postoperative complications.
Results
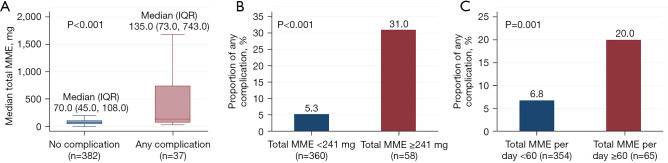
A total of 419 patients were included who were mostly female (59%) and white (75%). Most patients underwent either foregut surgery (52%) or lung surgery (25%). Of the patients, 160 (38%) were on home pain medication before surgery, and 52 (12.4%) were on opioid pain medication before surgery. The median total MME during hospitalization was 73 mg, with a median average daily MME of 30 mg. There were 37 patients (8.8%) who experienced postoperative complications. Patients who had complications had a significantly higher median total MME of 135 [interquartile range (IQR) 73.0, 743.0] vs. 70 (IQR 45, 108) mg; P<0.001. Patients with a total MME ≥241 mg were more than four times more likely to have postoperative complications than those with an MME <241 mg (31.0% vs. 5.3%; P<0.001). Patients who received daily MME ≥60 mg had significantly more postoperative complications (20.0% vs. 6.8%; P=0.001). Multivariate logistic regression analysis showed that Hispanic ethnicity [odds ratio (OR) 4.33; 95% confidence interval (CI): 1.63, 11.51; P=0.003], operation duration (OR 1.01; 95% CI: 1.00, 1.01; P=0.01), and total MME (OR 1.001; 95% CI: 1.00, 1.002; P<0.001) were associated with postoperative complications.
Conclusions
Hospital opioid use was associated with complications after thoracic surgical procedures. The amount of opioid medication received during hospitalization was an independent risk factor for postoperative complications in our patient population. Efforts to decrease the amount of opioid medication used with multimodal non-opioid medications may help improve surgical outcomes.
Keywords: Opioid, thoracic surgery, postoperative complications
Highlight box.
Key findings
• High in-hospital opioid use was associated with more post-operative complications in thoracic surgery.
What is known and what is new?
• Opioid medications have harmful side effect profiles. In orthopedic patient populations, there is a relationship between post-operative opioid use and post-operative complications.
• The above findings are also applicable to the thoracic surgery population.
What is the implication, and what should change now?
• Further effort(s) should be made to decrease in-hospital opioid use via other non-narcotic modalities to help improve surgical outcomes.
Introduction
Opioid-related overdose deaths in the United States totaled 80,411 in 2021. A total of 16,706 deaths were caused by prescribed opioids (1). From a surgeon’s perspective, it is imperative to minimize the risk of postoperative opioid dependency and to avoid opioid side-effect profiles (i.e., nausea and vomiting, bradycardia, hypotension, respiratory depression, central nervous system depression, delirium, etc.) that can negatively impact patients’ postoperative course. Enhanced recovery after surgery (ERAS) protocols have become prevalent in several surgical subspecialties. A common theme among such protocols is the recommendation for multimodal pain regimens that help reduce the amount of opioid medication required to treat postoperative pain (2). Curtailing the need for opioids can be a unique challenge for patients undergoing thoracic surgery.
Thoracic procedures often require surgery near the intercostal nerves, which patients can expect to contend with incisional pain postoperatively. Opioids play an important role in achieving adequate pain control after thoracic surgery to prevent postoperative pulmonary complications secondary to splinting and respiratory insufficiency (3). In such patient populations, the benefits of opioid analgesia in facilitating adequate pulmonary hygiene must be weighed against the risks of opioid-related complications. At our institution, the Division of Thoracic Surgery has implemented a modified version of the ERAS Society and the European Society of Thoracic Surgeons (ESTS) protocol for postoperative pain control, which includes a non-narcotic analgesic (acetaminophen), gamma-aminobutyric acid (GABA) analog (gabapentin), muscle relaxant (methocarbamol), topical anesthetic (lidocaine patches), and non-steroidal anti-inflammatory drugs (NSAID) (naproxen) in addition to as-needed rescue opioids for breakthrough pain (2). Opioids used on thoracic surgery service included tramadol, oxycodone, morphine, and hydromorphone. Multimodal pain regimens have been shown to decrease the need for outpatient opioid prescriptions after foregut and lung surgeries (4,5). We wanted to determine if there was a relationship between opioid use in the hospital and post-surgical complications. This article is presented in accordance with the STROBE reporting checklist (available at https://jtd.amegroups.com/article/view/10.21037/jtd-24-825/rc).
Methods
The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by the institutional review board of the Houston Methodist Research Institute (No. Pro00013680), and the requirement for individual consent for this retrospective analysis was waived. We performed a retrospective review of a single-institutional database developed from patients operated on by physicians of the Division of Thoracic Surgery at Houston Methodist Hospital. We performed a nested case-control study to determine if there was a relationship between thoracic surgical interventions and complications after surgery. The inclusion criteria were patients who underwent a thoracic surgical intervention between 11/1/2020 and 11/1/2021. We excluded patients who underwent outpatient procedures, such as endoscopy, flexible bronchoscopy, endobronchial ultrasound, endoscopic ultrasound, and transbronchial lung biopsy. The compiled data included basic demographic information (age, sex, race/ethnicity), body mass index (BMI), medical comorbidities, type of surgery, American Society of Anesthesiologists (ASA) classification, complications, operation duration, and opioid use data. Patient data including complications were identified and recorded in the institutional database at the time of discharge. The type of surgery was based on anatomical structures (foregut, lung, mediastinum, esophagus, etc.). Home pain medication prior to surgery was defined as prescribed or over-the-counter pain medication that the patient was taking at the time of the operation (i.e., acetaminophen, cyclophosphamide, and gabapentin). Opioid use data included history of opioid use at home prior to surgery. We obtained data on opioid use in the operating room, recovery, floor, and intensive care unit (ICU), if applicable. We converted the opioids to morphine milligram equivalent (MME) and calculated the total MME for hospital stay as well as the average daily MME. Complications were identified individually as well as Clavien-Dindo classification (6). The primary outcome of this study was the postoperative complications in patients undergoing thoracic surgical procedures.
Statistical analysis
Demographic and clinical data were reported as frequencies and proportions for categorical variables and as median and interquartile range (IQR) for continuous variables. Differences between groups were compared using the Chi-square or Fisher’s exact test for categorical variables and the Wilcoxon rank-sum test for continuous variables, as appropriate. Receiver operating characteristic (ROC) curve analysis with the Youden index (7) was used to identify the optimal cutoff points for total MME and total MME per day in predicting postoperative complications. Bar charts and box plots were used to visualize the distribution of postoperative complications. Logistic regression modeling was performed to determine the characteristics associated with outcomes (postoperative complications). Variables for the multivariable models were selected based on their clinical importance and Stata’s lasso technique with the cross-validation (CV) selection option (8,9). Model discrimination was determined using area under the ROC curve (AUC). Model calibration was assessed using the Hosmer-Lemeshow goodness-of-fit test, with a non-significant P value indicating good calibration. All analyses were performed using Stata version 18.5 (StataCorp LLC, College Station, TX, USA). Statistical significance was set at P value <0.05.
Results
Four hundred nineteen patients met the inclusion criteria. The median age of the patients in the study was 64 (IQR 54, 71) years. Two hundred forty-five patients were female (58.5%). A total of 316 patients were identified as White (75.4%), 48 patients were identified as Black/African American (11.5%), 35 patients were identified as Hispanic (8.4%), 18 patients were identified as Asian (4.3%), and 2 patients were identified as other (0.5%). The four most common comorbidities observed among the patients were hypertension (254 patients, 60.6%), diabetes mellitus (78 patients, 18.6%), coronary artery disease (43 patients, 10.3%), and chronic obstructive pulmonary disease (50 patients, 11.9%). The median ASA score was 3 (IQR 3, 3) (Table 1). The four most common anatomical locations of surgical procedures performed were the foregut (218 cases, 52%), lungs (103 cases, 24.6%), mediastinum (26 cases, 6.2%), and esophagus (18 cases, 4.3%). Except for chest wall procedures, all patients underwent robotic minimally invasive surgery. All patients received general anesthesia, and none of the patients received epidural anesthesia. Patients who had a chest incision received an intercostal nerve block with liposomal bupivacaine, and patients who had an abdominal incision received liposomal bupivacaine in the incisions. Patients were administered multimodal non-opioid pain medication after surgery, including acetaminophen, gabapentin, methocarbamol, a lidocaine patch, and selective use of ketorolac. The patient was administered tramadol for breakthrough pain and intravenous (IV) hydromorphone, if tramadol was insufficient. If the patient required additional opioids despite IV hydromorphone, the patient was placed on IV hydromorphone patient-controlled anesthesia.
Table 1. Characteristics of thoracic surgery patients.
| Characteristics | Value (N=419) |
|---|---|
| Age at surgery (years), median (IQR) | 64.0 (54.0, 71.0) |
| Female, n (%) | 245 (58.5) |
| Race/ethnicity, n (%) | |
| White | 316 (75.4) |
| Black | 48 (11.5) |
| Hispanic | 35 (8.4) |
| Asian | 18 (4.3) |
| Other | 2 (0.5) |
| Body mass index (kg/m2), median (IQR) | 27.3 (23.8, 31.1) |
| Comorbidities, n (%) | |
| Hypertension | 254 (60.6) |
| Diabetes | 78 (18.6) |
| Coronary artery disease | 43 (10.3) |
| COPD | 50 (11.9) |
| Surgery type, n (%) | |
| Foregut | 218 (52.0) |
| Lung | 103 (24.6) |
| Mediastinum | 26 (6.2) |
| Esophagus | 18 (4.3) |
| Pleura | 17 (4.1) |
| Diaphragm | 15 (3.6) |
| Chest wall | 13 (3.1) |
| Feeding tube | 9 (2.1) |
| ASA score, median (IQR) | 3.0 (3.0, 3.0) |
| Any home pain medication before surgery, n (%) | 160 (38.2) |
| Any home opioid medication before surgery, n (%) | 52 (12.4) |
| Operation duration (min), median (IQR) | 224.0 (186.0, 284.0) |
| MME (mg) | |
| Total MME, median (IQR) | 73.0 (45.0, 118.0) |
| Total MME per day, median (IQR) | 30.0 (18.3, 46.5) |
IQR, interquartile range; COPD, chronic obstructive pulmonary disease; ASA, American Society of Anesthesiologists; MME, morphine milligram equivalent.
A history of home pain medication use before surgery was reported in 160 (38.2%) patients. Fifty-two patients (12.4%) reported a history of home opioid pain medication within one month before surgery. There was a trend toward significance in higher postoperative complication rates in patients with preoperative home opioid use than in those without (15.4% vs. 7.9%, respectively, P=0.08). The median total MME during patient hospitalization was 73.0 mg (IQR 45.0, 118.0 mg). The median daily MME during patient hospitalization was 30.0 mg (IQR 18.3, 46.5 mg, Table 1). Median post-operative length of stay was 1.0 day (IQR 1.0, 2.0 days). Thirty-seven (8.8%) patients experienced postoperative complications. The most common postoperative complications were pneumothorax (n=8, 21.6%), pneumonia (n=4, 10.8%), dysphagia (n=3, 8.1%), respiratory insufficiency with new oxygen requirement at discharge (n=3, 8.1%), urinary retention (n=2, 5.4%), pulmonary embolism (n=2, 5.4%), new atrial fibrillation (n=2, 5.4%), postoperative bleeding (n=2, 5.4%), and urinary tract infection (n=2, 5.4%). The Clavien-Dindo classification of patient complications was as follows: class 1, 3 patients (0.7%); class 2, 13 patients (3.1%); class 3, 18 patients (4.3%); and class 4, 3 patients (0.7%, Table 2).
Table 2. Outcome after thoracic surgery procedures.
| Outcome | Value (N=419) |
|---|---|
| Any post-operative event, n (%) | 37 (8.8) |
| Post-operative event, n (%) | |
| None | 382 (91.2) |
| Minor | 9 (2.1) |
| Major | 28 (6.7) |
| Clavien-Dindo classification, n (%) | |
| 0 | 382 (91.2) |
| 1 | 3 (0.7) |
| 2 | 13 (3.1) |
| 3 | 18 (4.3) |
| 4 | 3 (0.7) |
| Post-operative LOS (days), median (IQR) | 1.0 (1.0, 2.0) |
| 30-day mortality, n (%) | 0 (0) |
LOS, length of stay; IQR, interquartile range.
Patients who suffered complications had significantly higher total MME (median 135.0; IQR 73.0, 743.0) vs. (median 70.0; IQR 45.0, 108.0) mg (P<0.001, Figure 1A). A ROC curve analysis with the Youden index determined that patients who had a total MME ≥241 mg had significantly higher complication rates than patients who had a total MME <241 mg (31.0% vs. 5.3%, respectively; P<0.001, Figure 1B). Similarly, patients who had a daily MME of ≥60 mg had significantly higher complication rates than those who had a daily MME of <60 mg (20.0% vs. 6.8%, respectively; P=0.001, Figure 1C). Multivariable logistic regression analysis demonstrated that the following subgroups were associated with higher odds of having any complications after surgery: Hispanic ethnicity [odds ratio (OR) 4.33, 95% confidence interval (CI) 1.63, 11.51; P=0.003], longer operation duration (OR 1.01; 95% CI: 1.00, 1.01; P=0.01), and total MME (OR 1.001; 95% CI: 1.00, 1.002; P<0.001) (Table 3).
Figure 1.
Relationship between MME and complication. (A) Patients with any complication had significantly higher total MME compared to patients who did not have a complication. (B) Total MME ≥241 mg had complication rate of 31% vs. 5.3% (P<0.001). (C) Total MME per day ≥60 had significantly higher complication rate of 20% vs. 6.8% (P=0.001). MME, morphine milligram equivalent; IQR, interquartile range.
Table 3. Multivariable logistic regression analysis for having any complication.
| Variable | OR (95% CI) | P |
|---|---|---|
| Hispanic | 4.33 (1.63, 11.51) | 0.003 |
| Hypertension | 1.85 (0.79, 4.36) | 0.16 |
| Operation duration (min) | 1.01 (1.00, 1.01) | 0.01 |
| Total MME | 1.001 (1.00, 1.002) | <0.001 |
OR, odds ratio; CI, confidence interval; MME, morphine milligram equivalent.
Discussion
There is likely a bidirectional relationship between the observed association between postoperative opioid use and complications after thoracic surgery. The side effect profiles of opioids can cause respiratory depression, altered mental status, dizziness, nausea, and vomiting amongst other side effects, all of which can hinder postoperative mobilization (10). Poor mobilization after surgery subsequently results in complications, such as venous thromboembolism, nosocomial pneumonia, and physical deconditioning (11). Conversely, many of the postoperative complications related to thoracic surgery and the requisite treatment of these complications can cause significant pain. Chest tubes of varying sizes, image-guided drains, nosocomial pneumonia, pulmonary emboli, surgical site infections, and anastomotic leaks are known complications of thoracic surgery and may increase the postoperative opioid requirement.
Multiple studies focusing on ERAS have demonstrated that a multimodal pain regimen decreases the overall need for postoperative opioid pain medication postoperatively (12-14). The ERAS Society and European Society of Thoracic Surgeons in 2019 published guidelines strongly recommend multimodal analgesia to help reduce overall opioid requirements in the postoperative phase. In a related note to our findings, Memtsoudis et al. found that patients managed on a multimodal pain regimen after orthopedic surgery experienced significantly fewer postoperative opioid-related complications than those managed with opioids alone (15). Cozowicz et al. demonstrated that postoperative opioid use was associated with greater postoperative complication rates in patients undergoing orthopedic surgery (16).
To our knowledge, no previous studies have evaluated the relationship between postoperative opioid requirements and postoperative complications in thoracic surgeries. We found that greater opioid use in the immediate postoperative period was associated with higher complication rates after thoracic surgical procedures. The amount of opioid medication received during hospitalization was an independent risk factor for postoperative complications. Efforts to decrease the amount of opioid medication used with multimodal non-opioid medication have the potential to improve surgical outcomes.
No studies have evaluated complication rates in a patient population similar to that being treated at our institution (i.e., comprising majority foregut pathology followed by lung, mediastinal, and esophageal pathology, respectively). For patients undergoing minimally invasive hiatal hernia repair, our complication rates were comparable to those reported in the literature (17,18). For patients undergoing minimally invasive lung resection, our complication rates were lower than those reported in the literature (19-21).
In our patient population, Hispanic ethnicity was found to be an independent risk factor for higher postoperative complication rates. Studies have demonstrated conflicting findings regarding the influence of Hispanic ethnicity on postoperative morbidity and mortality (22). Further studies are needed to identify the etiology of our findings. Longer operative time was also identified as an independent risk factor for postoperative complications. We posit that in more technically challenging cases (i.e., those with abnormal/aberrant anatomy or reoperative cases) requiring longer operative times, there may also be a greater risk of both intraoperative and postoperative complications.
Chronic opioid use has been shown to have a detrimental effect on postoperative outcomes. In the orthopedic population, chronic opioid use is associated with an increased length of stay, greater postoperative opioid requirement, and more frequent emergency department visits, readmissions, and early revision (23,24). In patients undergoing bariatric surgery, chronic opioid use has been associated with greater rates of postoperative complications, increased length of hospital stay, and the need for a reoperation (25,26). We did not observe similar findings in our patient population.
The limitations of this study were that it was a retrospective nested case-control study, and no causative relationship could be proven. There was also the potential for recall bias as the data regarding post-operative complications were gathered based on the inpatient team’s determination at a weekly service meeting of whether a postoperative complication occurred. This is most concerning in patients with long and complex hospital stays, in whom not all postoperative complications may have been identified. We have checked these cases and found that there were no complications that were missed. The generalizability of our findings is limited to patients who underwent thoracic surgery. In conclusion, we have demonstrated that increased postoperative opioid requirements are associated with greater postoperative complications after thoracic surgery, and we strongly support the widespread implementation of the ERAS protocol in the management of postoperative pain, which has been shown to decrease both perioperative and post-discharge opioid requirements. Further studies are needed to understand how postoperative opioid use can be decreased to mitigate its effects on postoperative complications. There is also an additional opportunity to investigate which specific postoperative complications are associated with a higher degree of postoperative opioid use in thoracic surgery.
Conclusions
An increased postoperative opioid requirement was independently associated with an increased risk of postoperative complications in patients undergoing thoracic surgery. These findings, in conjunction with existing knowledge of the adverse side-effect profiles of narcotic medications, provide further support for the need to find effective strategies for moderating post-operative opioid use.
Supplementary
The article’s supplementary files as
Acknowledgments
Funding: None.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by the institutional ethics board of the Houston Methodist Research Institute (No. Pro00013680), and the requirement for individual consent for this retrospective analysis was waived.
Footnotes
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at https://jtd.amegroups.com/article/view/10.21037/jtd-24-825/rc
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://jtd.amegroups.com/article/view/10.21037/jtd-24-825/coif). M.P.K. serves as an unpaid editorial board member of Journal of Thoracic Disease from September 2022 to August 2024. M.P.K. received royalties or licenses for VATS lobectomy video from Medtronic, honoria for teaching other surgeons on the use of technology from Medtronic and Intuitive Surgical. He has also consulted for Olympus. The other authors have no conflicts of interest to declare.
Data Sharing Statement
Available at https://jtd.amegroups.com/article/view/10.21037/jtd-24-825/dss
References
- 1.Services, U.S.D.o.H.a.H. Drug overdose death rates. 2023 September 25, 2023]; Available online: https://nida.nih.gov/research-topics/trends-statistics/overdose-death-rates
- 2.Batchelor TJP, Rasburn NJ, Abdelnour-Berchtold E, et al. Guidelines for enhanced recovery after lung surgery: recommendations of the Enhanced Recovery After Surgery (ERAS®) Society and the European Society of Thoracic Surgeons (ESTS). Eur J Cardiothorac Surg 2019;55:91-115. 10.1093/ejcts/ezy301 [DOI] [PubMed] [Google Scholar]
- 3.Rogers FB, Larson NJ, Rhone A, et al. Comprehensive Review of Current Pain Management in Rib Fractures With Practical Guidelines for Clinicians. J Intensive Care Med 2023;38:327-39. 10.1177/08850666221148644 [DOI] [PubMed] [Google Scholar]
- 4.Kim MP, Godoy C, Nguyen DT, et al. Preemptive pain-management program is associated with reduction of opioid prescriptions after benign minimally invasive foregut surgery. J Thorac Cardiovasc Surg 2020;159:734-744.e4. 10.1016/j.jtcvs.2019.06.056 [DOI] [PubMed] [Google Scholar]
- 5.Del Calvo H, Nguyen DT, Meisenbach LM, et al. Pre-emptive pain management program is associated with reduction of opioid prescription after minimally invasive pulmonary resection. J Thorac Dis 2020;12:1982-90. 10.21037/jtd-20-431 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg 2004;240:205-13. 10.1097/01.sla.0000133083.54934.ae [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.YOUDEN WJ . Index for rating diagnostic tests. Cancer 1950;3:32-5. [DOI] [PubMed] [Google Scholar]
- 8.Hastie T, Tibshirani R, Wainwright M. Statistical Learning with Spasity: The Lasso and Generalizations. 2015, Boca Raton, FL: CRC Press. [Google Scholar]
- 9.StataCorp, Stata Lasso. Stata Reference Manual. Vol. Release 16. 2019, College Station, TX. [Google Scholar]
- 10.Benyamin R, Trescot AM, Datta S, et al. Opioid complications and side effects. Pain Physician 2008;11:S105-20. 10.36076/ppj.2008/11/S105 [DOI] [PubMed] [Google Scholar]
- 11.Castelino T, Fiore JF, Jr, Niculiseanu P, et al. The effect of early mobilization protocols on postoperative outcomes following abdominal and thoracic surgery: A systematic review. Surgery 2016;159:991-1003. 10.1016/j.surg.2015.11.029 [DOI] [PubMed] [Google Scholar]
- 12.Clark IC, Allman RD, Rogers AL, et al. Multimodal Pain Management Protocol to Decrease Opioid Use and to Improve Pain Control After Thoracic Surgery. Ann Thorac Surg 2022;114:2008-14. 10.1016/j.athoracsur.2022.03.059 [DOI] [PubMed] [Google Scholar]
- 13.Tan WH, Ford J, Kindel T, et al. Implementation of a standardized multimodal pain regimen significantly reduces postoperative inpatient opioid utilization in patients undergoing bariatric surgery. Surg Endosc 2023;37:3103-12. 10.1007/s00464-022-09482-6 [DOI] [PubMed] [Google Scholar]
- 14.Petrikovets A, Sheyn D, Sun HH, et al. Multimodal opioid-sparing postoperative pain regimen compared with the standard postoperative pain regimen in vaginal pelvic reconstructive surgery: a multicenter randomized controlled trial. Am J Obstet Gynecol 2019;221:511.e1-511.e10. 10.1016/j.ajog.2019.06.002 [DOI] [PubMed] [Google Scholar]
- 15.Memtsoudis SG, Poeran J, Zubizarreta N, et al. Association of Multimodal Pain Management Strategies with Perioperative Outcomes and Resource Utilization: A Population-based Study. Anesthesiology 2018;128:891-902. 10.1097/ALN.0000000000002132 [DOI] [PubMed] [Google Scholar]
- 16.Cozowicz C, Olson A, Poeran J, et al. Opioid prescription levels and postoperative outcomes in orthopedic surgery. Pain 2017;158:2422-30. 10.1097/j.pain.0000000000001047 [DOI] [PubMed] [Google Scholar]
- 17.Klock JA, Walters RW, Nandipati KC. Robotic Hiatal Hernia Repair Associated with Higher Morbidity and Readmission Rates Compared to Laparoscopic Repair: 10-Year Analysis from the National Readmissions Database (NRD). J Gastrointest Surg 2023;27:489-97. 10.1007/s11605-022-05548-x [DOI] [PubMed] [Google Scholar]
- 18.Mertens AC, Tolboom RC, Zavrtanik H, et al. Morbidity and mortality in complex robot-assisted hiatal hernia surgery: 7-year experience in a high-volume center. Surg Endosc 2019;33:2152-61. 10.1007/s00464-018-6494-4 [DOI] [PubMed] [Google Scholar]
- 19.Swanson SJ, Miller DL, McKenna RJ, Jr, et al. Comparing robot-assisted thoracic surgical lobectomy with conventional video-assisted thoracic surgical lobectomy and wedge resection: results from a multihospital database (Premier). J Thorac Cardiovasc Surg 2014;147:929-37. 10.1016/j.jtcvs.2013.09.046 [DOI] [PubMed] [Google Scholar]
- 20.Louie BE, Farivar AS, Aye RW, et al. Early experience with robotic lung resection results in similar operative outcomes and morbidity when compared with matched video-assisted thoracoscopic surgery cases. Ann Thorac Surg 2012;93:1598-604; discussion 1604-5. 10.1016/j.athoracsur.2012.01.067 [DOI] [PubMed] [Google Scholar]
- 21.Boffa DJ, Dhamija A, Kosinski AS, et al. Fewer complications result from a video-assisted approach to anatomic resection of clinical stage I lung cancer. J Thorac Cardiovasc Surg 2014;148:637-43. 10.1016/j.jtcvs.2013.12.045 [DOI] [PubMed] [Google Scholar]
- 22.Upfill-Brown A, Paisner N, Sassoon A. Racial disparities in post-operative complications and discharge destination following total joints arthroplasty: a national database study. Arch Orthop Trauma Surg 2023;143:2227-33. 10.1007/s00402-022-04485-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Jain N, Brock JL, Malik AT, et al. Prediction of Complications, Readmission, and Revision Surgery Based on Duration of Preoperative Opioid Use: Analysis of Major Joint Replacement and Lumbar Fusion. J Bone Joint Surg Am 2019;101:384-91. 10.2106/JBJS.18.00502 [DOI] [PubMed] [Google Scholar]
- 24.Brock JL, Jain N, Phillips FM, et al. Postoperative opioid cessation rates based on preoperative opioid use: analysis of common orthopaedic procedures. Bone Joint J 2019;101-B:1570-7. 10.1302/0301-620X.101B12.BJJ-2019-0080.R2 [DOI] [PubMed] [Google Scholar]
- 25.Skogar ML, Sundbom M. Preoperative chronic opioid use and its impact on early complications in bariatric surgery: a Swedish nationwide cohort study of 56,183 patients. Surg Obes Relat Dis 2021;17:1256-62. 10.1016/j.soard.2021.04.008 [DOI] [PubMed] [Google Scholar]
- 26.Tian C, Maeda A, Okrainec A, et al. Impact of preoperative opioid use on health outcomes after bariatric surgery. Surg Obes Relat Dis 2020;16:768-76. 10.1016/j.soard.2020.02.008 [DOI] [PubMed] [Google Scholar]