Abstract
Study Design
Cross-sectional Cohort Study.
Objective
To determine the cervicothoracic inflection point in an asymptomatic, adult population.
Introduction
The cervicothoracic inflection point (CTIP) is an important sagittal marker to understand for patients with cervical deformities. We aimed to identify the CTIP and understand the relationship to other sagittal alignment markers.
Methods
468 adult asymptomatic volunteers (18-80 years) from 5 countries (United States, France, Japan, Singapore, Tunisia). All volunteers underwent standing full body, low dose stereo radiographs. The CTIP was identified by measuring the cervical sagittal angle (CSA) and thoracic kyphosis maximum angle (TKMax), using the end vertebra concept. The CTIP was defined as the vertebra or disc between the lower end vertebra of the CSA and upper end vertebra of TKMax. A correlation matrix was utilized to identify the relationship between the CTIP and spinopelvic sagittal parameters of interest.
Results
The most common CTIP value was the T1 vertebra. CTIPs ranged from C5 to T4, respectively. CTIP showed a weak positive correlation to age (r = 0.10, P = 0.03) and negative correlation to BMI (r = −0.11, P = 0.04). Additionally, CTIP had a minor positive correlation with OC2-CL, C7 slope, T1 slope, T1PA, T1-T12 TK, and T4-T12 TK, all statistically significant. Linear regression demonstrated increased cervical lordosis and increased TK was associated with more caudal CTIP segments.
Conclusion
CTIP segments ranged from C5 to T4, with the most common segment being T1. Understanding the relationship of the CTIP to other sagittal variables is critical to patients with CD.
Keywords: adult cervical deformity, inflection point, cervical spine, cervical deformity, cervicothoracic deformity
Keywords: 3
Introduction
Understanding sagittal alignment is key for optimal spinopelvic correction in adult spinal deformity (ASD) surgery. Classically, cervical lordosis (CL), thoracic kyphosis (TK), lumbar lordosis (LL), pelvic incidence (PI), the C7-sagittal vertical axis (SVA), and T1 pelvic angle (TPA) have been lauded as parameters of interest related to sagittal alignment. Recent literature has explored the importance of the inflection point in the thoracolumbar spine.1-3 The thoracolumbar inflection point (TLIP) is described as the transitional vertebra or intervertebral disc depicting the change from kyphosis to lordosis.1,4 According to the Roussouly Classification, the TLIP is an important marker of sagittal spinopelvic alignment, 4 which is believed to be anatomically located between T12-L1. 5 This finding was corroborated by Malka and colleagues 1 , who reported that the mean TLIP was located between T12-L1. Interestingly, younger study subjects had a TLIP at L1 and older individuals had a TLIP at T12, suggesting cranial migration of the TLIP with increased age. Clinically, increased distance from the TLIP and LL apex has been associated with junctional complications. 6 Although recent studies have evaluated the relationship between TLIP, sagittal alignment, and patient outcomes, a dearth of information still exists. Even less is understood about the inflection point in the cervicothoracic spine.
The cervicothoracic inflection point (CTIP) is the theoretical segment (vertebra or intervertebral disc) depicting the curvature transition from the cervical sagittal angle (CSA) to TK. Several studies have suggested that the CTIP may exist between C7-T2 in most people.7-9 Yet, CTIP ranges can exist in more distal segments of the spine such as T3-T5. 8 Identification of the CTIP has been shown to be valuable for restoration of alignment in adult cervical deformity (ACD) patients and patients with cervical spondylotic radiculopathy.8,10
The purpose of this study was to identify the CTIP in a cohort of multiethnic, asymptomatic volunteers. Furthermore, the relationship between the CTIP and other cervicothoracic sagittal parameters was investigated to thoroughly understand how the CTIP relates to optimal global sagittal alignment. Additionally, CTIP was stratified by age, sex, and ethnicity.
Methods
A total of 468 asymptomatic adult volunteers were recruited to form the multi-ethnic asymptomatic normative study (MEANS) cohort. Volunteers from 5 countries, including France, Japan, Singapore, Tunisia, and the United States, were enrolled to garner a greater understanding of global and regional spinopelvic alignment. Full ethical approval and informed consent was obtained from each volunteer at each participating site. The institutional review board approval number from Washington University at St. Louis was IRB 201812144. The MEANS database remains the largest adult multi-ethnic cohort with asymptomatic volunteers. Volunteers ages ranged from 18-80 years of age without significant back, neck, or spinal related pain. The Visual Analog Scale (VAS) and Oswerty Disability Index (ODI) was utilized to screen for significant back/neck pain.
Inclusion criteria for this study included: 1) adult patients (18-80 years), 2) no present neck/back pain (VAS ≤2), 3) no known spinal pathology, 4) no past medical/surgical history for spinal-related pathologies. Exclusion criteria included 1) the presence of a coronal Cobb angle greater than 20°, 2) aberrant vertebral anatomy (ie, lumbosacral transitional vertebrae), and ODI scores greater than 20.
Additionally, demographics such as age, sex, body mass index (BMI), and ethnicity were obtained. All study participants underwent full-length, bi-planar, low dose stereoradiographic imaging. All radiographic measurements were conducted by experienced X-ray technicians and clinical researchers with a 2D/3D sterEOS® modeling software (EOS imaging, Paris, France), specifically EOS 3D service.
The CTIP was identified by measuring the cervical sagittal angle (CSA) and thoracic kyphosis (TK) using the end vertebra concept, respectively. Due to large morphologic variation in the cervical spine, we avoided the term “cervical lordosis.” Instead, we measured the CSA, which was defined as the sagittal cobb angle from the inferior end plate of C2 to the lower end plate of the most tilted caudal end vertebra in the lower cervical or upper thoracic spine. The CTIP was defined as the vertebra or disc between the lower end vertebra of the CSA and upper end vertebra of the thoracic kyphosis (Figures 1 and 2).
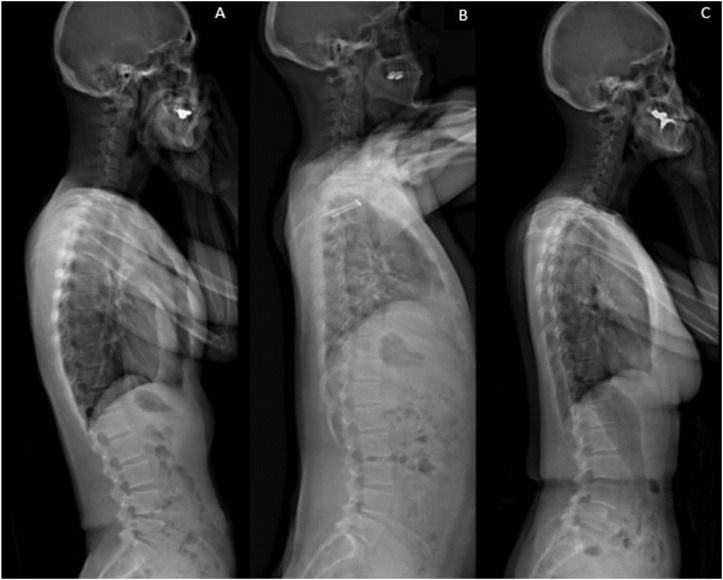
Figure 1.
Asymptomatic Volunteers with varying CTIP segments. (A) C7-T1 CTIP, (B) C6-C7 CTIP, (C) T3 CTIP.
Figure 2.
Method demonstrating the cervicothoracic inflection point (CTIP) at the C7-T1 disc. The CTIP was determined based on the end vertebra concept. The CTIP is the vertebra or disc between the lower end vertebra of the cervical sagittal Cobb angle (CSA) and the upper end vertebra of thoracic kyphosis (TK).
A numbering system of the vertebrae and intervertebral discs was created for CTIP identification and analysis: C1 was given the numerical value of 1, T1 was 8, L1 was 20, and S1 was 25. Intervertebral discs were assigned numerical values as such: the C2-C3 disc was assigned 2.5 the T1-T2 disc was assigned 8.5, the L1-L2 disc was assigned 20.5 and so on. Full ethical approval was provided by all participating institutions.
Results
CTIP by Population Stratification
A total of 468 patients were included in the MEANS cohort analysis with a mean age of 40.4 ± 14.8 years. Table 1 presents the frequency distribution of CTIP among the MEANS cohort. The most commonly occurring CTIP was T1, comprising 24.1% of the total, followed by C6 (13.9%), C5-C6 (13.2%), and C7-T1 (16.9%). Less frequent CTIPs included C5, C6-C7, T2-T3, T3, T4. Table 2 provides a stratification of CTIP by various demographic factors. Overall, the mean CTIP was 7.13, approximately corresponding to C7 (an example of which is shown in Figure 1) with a median of 7.5 (C7-T1) and a mode of 8 (T1). The range spanned from C5 to T4 with a standard deviation of 1.11 and a 95% confidence interval of (7.03-7.24).
Table 1.
CTIP Frequency.
| CTIP | Frequency | % of Total |
|---|---|---|
| C5 | 8 | 1.7 |
| C5-C6 | 62 | 13.2 |
| C6 | 65 | 13.9 |
| C6-C7 | 35 | 7.5 |
| C7 | 50 | 10.7 |
| C7-T1 | 79 | 16.9 |
| T1 | 113 | 24.1 |
| T1-T2 | 26 | 5.6 |
| T2 | 20 | 4.3 |
| T2-T3 | 7 | 1.5 |
| T3 | 1 | 0.2 |
| T4 | 1 | 0.2 |
| N/A | 1 | 0.2 |
| Total | 468 | 100.0 |
Table 2.
Stratification of CTIP by Demographics.
| Variable | Mean | Median | Mode | Range | SD | 95% CI | P-value | |
|---|---|---|---|---|---|---|---|---|
| Overall | 7.13 | 7.5 | 8 | C5 to T4 | 1.11 | (7.03-7.24) | ||
| Sex | Female | 7.07 | 7.5 | 8 | C5 to T2T3 | 1.14 | (6.94-7.20) | 0.12 |
| Male | 7.23 | 7.5 | 8 | C5 to T4 | 1.05 | (7.08-7.39) | ||
| Ethnicity | Asian | 7.06 | 7.5 | 8 | C5 to T2T3 | 1.08 | (6.9-7.22) | 0.01* |
| Caucasian | 7.29 | 7.5 | 8 | C5 to T4 | 1.11 | (7.12-7.45) | ||
| Arabo-Bèrbère | 7.16 | 7 | 8 | C5C6 to T2T3 | 1.1 | (6.92-7.41) | ||
| Others (including black, Indian) | 6.57 | 6 | 5.5 | C5C6 to T1T2 | 1.1 | (6.14-7.01) | ||
| 29-37 | 7.12 | 7.5 | 8 | C5 to T2T3 | 1.08 | (6.90-7.33) | ||
| 38-50 | 7.17 | 7.5 | 8 | C5 to T4 | 1.16 | (6.96-7.37) | ||
| 51-64 | 7.25 | 7.5 | 7.5 | C5C6 to T2T3 | 1.1 | (7.0-7.5) | ||
| 65 and above | 7.29 | 7.5 | 7.5 | C5 to T2T3 | 1.03 | (6.95-7.63) |
*P-value <.05 ANOVA. P < 0.01 indicates statistical significance.
When considering sex, males had a slightly higher mean CTIP of 7.23 compared to females with 7.07 with both corresponding approximately to C7, although this was not statistically significant. Among ethnic groups, Caucasians had the most caudal mean CTIP at 7.29 (approximately C7-T1), while “Others” (Black and Indian individuals), had a cranial CTIP at 6.57, correlating to the C6-C7 disc. Moreover, Tukey’s post-hoc analysis demonstrated that a significant difference was only noted between Caucasian and Other ethnic groups (P = .01). Although the ranges of the CTIP vary across different population groups, the average and median intersection point remained consistently close to the C7 vertebra or the C7-T1 disc.
Correlations of Demographic and Spinal Variables with the CTIP
A general correlation matrix was made to explore the relationships between the CTIP and demographics/cervicothoracic definition variables (Table 3). The CTIP demonstrated a weak positive correlation (caudal migration) with age (r = 0.10, P = 0.03) and a weak negative correlation (cranial migration) with BMI (r = −0.11, P = 0.04).
Table 3.
Correlation of CTIP to Demographics.
| Parameter | CTIP (r) | P-value |
|---|---|---|
| CTIP | 1.00 | - |
| Age | 0.10 | 0.03 |
| BMI | −0.11 | 0.04 |
P < 0.01 indicates statistical significance.
A second correlation matrix (Table 4) highlights several relationships between other sagittal spinopelvic parameters with the CTIP. The CTIP displays a weak negative correlation with OC2-cervical lordosis (r = −0.21, P < 0.00001), cervical sagittal vertical axis (cSVA) (r = 0.26, P < 0.001). A moderately positive correlation with TK (°) (r = 0.32, P < 0.001) was observed. Furthermore, CTIP exhibits positive correlations with other parameters such as T1 Slope (r = 0.33, P < 0.001), C7 slope (r = 0.25, P < 0.001), T4T12 kyphosis (r = 0.33, P < 0.001), and C2C7 angle (r = 0.38, P < 0.001), with moderate correlations in each circumstance. However, the CTIP does not correlate significantly with the lumbar lordosis (r = 0.04, P = 0.37). For pelvic parameters of interest, the CTIP does not have significant correlations with sacral slope, pelvic tilt, or pelvic incidence.
Table 4.
Correlation of CTIP to Regional and Global Alignment Parameters.
| Parameter | CTIP (r) | P-value |
|---|---|---|
| CTIP | 1.00 | - |
| OC2-Cervical lordosis (°) | 0.21 | <.00001 |
| C2C7 lordosis (°) | 0.38 | <.0001 |
| C7 slope angle (°) | 0.25 | <.00001 |
| T1 slope angle (°) | 0.33 | <.00001 |
| Cervical sagittal vertical axis; cSVA (mm) | −0.26 | <.00001 |
| T1 pelvic angle (°) | 0.12 | 0.01 |
| T1-T12 Kyphosis (°) | 0.26 | <.0001 |
| T4-T12 Kyphosis (°) | 0.33 | <.0001 |
| Thoracic kyphosis (°) | 0.32 | <.00001 |
| Lumbar lordosis (°) | −0.04 | 0.37 |
| Sagittal vertical axis; SVA (mm) | 0.25 | <.00001 |
| Global sagittal alignment (°) | 0.17 | <.001 |
| Sacral slope (°) | −0.03 | 0.46 |
| Pelvic tilt (°) | 0.04 | 0.39 |
| Pelvic incidence (°) | 0.00 | 0.98 |
P < 0.01 indicates statistical significance.
Lastly, stepwise linear regression demonstrated that the more lordotic the cervical spine was (as depicted by the C2C7), the more caudal the inflection point. The CTIP was positively correlated with all thoracic kyphosis angle measurements (Table 3), suggesting caudal CTIPs to be found in thoracic spines with increased kyphosis. Cervical spines with kyphotic shapes would be expected to have more cranial CTIPs and a reduction in thoracic kyphosis.
Discussion
To our knowledge, this is the largest study to date to investigate the CTIP in a large, asymptomatic, multi-ethnic, cross-sectional cohort. In our analysis, we identified the most common CTIP segment to be at T1. These findings align with what has been previously reported in the literature.7,11 Park et al 7 reported that the most common CTIP was the T1 vertebra, followed by the T2 vertebra. Additionally, the authors found the CTIP to remain static across the lifespan. Interestingly, Bortz and colleagues 8 found that the CTIP can change postoperatively, with a caudal migration of inflection point. Our observations showed a slight caudal migration of the CTIP across the lifespans of asymptomatic individuals which varies from the previous findings by Park and colleagues. 7 Moreover, we observed a large distribution of CTIP ranges in our cohort, with the most cranial CTIP being the C5 vertebra and the most caudal being the T4 vertebra. This range is much wider than previously reported in the literature.7-9 We speculate that this may be attributed to age related anatomical changes in the spine.
Our analysis found the CTIP to be weakly positively correlated with age and negatively correlated with BMI. When evaluating other sagittal alignment parameters, the C2C7 Cobb angle, C7 slope, T1 slope, T1 pelvic angle, T1T12 kyphosis, T4T12 kyphosis, and SVA were positively correlated with the CTIP, meaning the CTIP was more caudal. While other parameters, such as OC2-CL and cSVA, were negatively correlated, meaning the CTIP was more cranial.
The CTIP can help spine surgeons better understand cervical and upper thoracic sagittal alignment. Lamas et al 12 identified the lower arch of cervical curvature shape as occurring from the curve’s apex to the CTIP, the most distal point of the lower arch. The authors also demonstrated that patients with degenerative spinal deformities had higher lordotic curves in their cervical curvature’s lower arch than an asymptomatic reference group. Additionally, including the inflection point into fusion constructs resulted in superior post-surgical horizontal gaze and cervical alignment in ACD patients. 8 This is a vital finding as patients with cervical and cervicothoracic deformities have been shown to have difficulty maintaining horizontal gaze, which may lead to compensatory alignment mechanisms. 13
There are several limitations to note to our study. Firstly, we studied the inflection point in an asymptomatic population. Our findings may not be observed in symptomatic cohorts. Further study is warranted in this area. Secondly, the cross-sectional nature of this study may introduce the possibility of selection bias. Thirdly, our cohort does not include many older volunteers above the age of 80 years of age. Aging is associated with increased spine degeneration, which can inadvertently alter alignment.
There are several strengths to our study as well. First, all volunteers underwent bi-planar full body and full spine stereoradiographs using 2D/3D sterEOS® modeling software (EOS imaging, Paris, France). Second, our study investigated the largest asymptomatic dataset to identify the anatomical presence of the CTIP.
It should be noted that further investigation is warranted in ACD patients. The inclusion of the CTIP in fusion constructs should be evaluated for surgical efficacy in patients with long term follow-up. Mechanical complications, revision rates, and sagittal alignment should be assessed and related to the CTIP. We speculate that the CTIP may play an important role Moreover, the CTIP should be studied in patients with isolated cervical and cervicothoracic deformities as there may be anatomical differences according to varying deformities. We speculate that further knowledge on the role of CTIP may play an important role in our current understanding of junctional complications in patients with cervical and cervicothoracic deformities. We encourage researchers to continue to study this sagittal variable and its role in ACD.
Conclusion
In conclusion, the inflection point between cervical spine curvature and thoracic kyphosis may be a useful sagittal marker for spine surgeons treating patients with cervical and cervicothoracic deformities. Further investigation is warranted to understand the role that the CTIP plays in cervical and cervicothoracic deformities. In our study, CTIP values ranged from C5-T4, respectively. We noticed slight caudal migration in CTIP segments in older volunteers. This study aids spinal surgeons in identifying the CTIP in patients with cervical and cervicothoracic deformities, which can be used to study caudal cervical alignment and provide clinical benefit by including the CTIP segment in fusion constructs.
Acknowledgments
EOS imaging supported the multi-centric collaborative group by providing a web-based solution for image review. Authors did not receive any funding from EOS imaging relative to this work.
Footnotes
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Device Status/Drug Statement: The manuscript submitted does not contain information about medical device(s)/drug(s).
Ethics Statement
Ethical Approval
The research conducted in this study received institutional review/ethics board approval at all sites.
ORCID iDs
Justin L. Reyes https://orcid.org/0000-0001-6596-6488
Matan Malka https://orcid.org/0009-0001-1470-3335
Josephine Coury https://orcid.org/0000-0002-4511-1172
Yong Shen https://orcid.org/0000-0002-4866-838X
Hwee Weng Dennis Hey https://orcid.org/0000-0002-2012-9835
References
- 1.Malka M, Sardar ZM, Czerwonka N, et al. The thoracolumbar inflection point in a population of asymptomatic volunteers: a multi-ethnic alignment normative study cohort study. Global Spine J 2023. doi: 10.1177/21925682231193619 [DOI] [PubMed] [Google Scholar]
- 2.Pan C, Anouar B, Li Y, et al. Predicting thoracic kyphosis morphology and the thoracolumbar inflection point determined by individual lumbar lordosis in asymptomatic adults. Eur Spine J 2023;33. doi: 10.1007/s00586-023-07983-z [DOI] [PubMed] [Google Scholar]
- 3.Charles YP, Marchand PL, Tuzin N, Steib JP. Thoracic kyphosis and lumbar lordosis distribution after idiopathic scoliosis correction using posterior hybrid versus screw instrumentation. Clin Spine Surg. 2021;34(6):E354-E363. doi: 10.1097/BSD.0000000000001171 [DOI] [PubMed] [Google Scholar]
- 4.Roussouly P, Gollogly S, Berthonnaud E, Dimnet J. Classification of the normal variation in the sagittal alignment of the human lumbar spine and pelvis in the standing position. Spine. 2005;30(3):346-353. doi: 10.1097/01.brs.0000152379.54463.65 [DOI] [PubMed] [Google Scholar]
- 5.Roussouly P, Nnadi C. Sagittal plane deformity: an overview of interpretation and management. Eur Spine J. 2010;19(11):1824-1836. doi: 10.1007/s00586-010-1476-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Mir JM, Passias PGMD, Lewis , et al. MD; gum, jeffrey lynn MD; protopsalt, themistocles. 371 the impact of thoracolumbar inflection point on outcomes and complications in adult spinal deformity. Neurosurgery. 2024;70(Supplement_1):111. [Google Scholar]
- 7.Park MS, Moon S-H, Kim T-H, et al. Sagittal alignment based on inflection point and its differences according to age groups. J Orthop Surg. 2020;28(1). [DOI] [PubMed] [Google Scholar]
- 8.Bortz C, Passias PG, Pierce KE, et al. Radiographic benefit of incorporating the inflection between the cervical and thoracic curves in fusion constructs for surgical cervical deformity patients. J Craniovertebral Junction Spine. 2020;11(2):131-138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Passias PGMD, Williamson TK, Doa B, et al. The importance of incorporating proportional alignment in adult cervical deformity corrections relative to regional and global alignment: steps toward development of a cervical-specific score. Spine. 2024;49(2):116-127. [DOI] [PubMed] [Google Scholar]
- 10.Park MS, Moon SH, Kim YW, et al. The effect of cervical fusion on functional sagittal spinal alignment based on the inflection point: case series study. Global Spine J. 2023;13(3):643-650. doi: 10.1177/21925682211001795 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Roscop C, Mathio P, Gajny L, Kouyoumdjian P, Skalli W, Gille O. Analysis of apex and transitional vertebra of the spine according to pelvic incidence using orientation and position parameters. Eur Spine J. 2021;30(9):2514-2519. doi: 10.1007/s00586-021-06908-y [DOI] [PubMed] [Google Scholar]
- 12.Lamas V, Chapon R, Prost S, et al. Variation of cervical sagittal alignment parameters according to age and pelvic incidence in degenerative spinal deformity patients. Eur Spine J. 2023;32:3624-3633. [DOI] [PubMed] [Google Scholar]
- 13.Merrill RK, Clohisy JC, Albert TJ, Qureshi SA. Concepts and techniques to prevent cervical spine deformity after spine surgery: a narrative review. Neurospine. 2023;20(1):221-230. doi: 10.14245/ns.2244780.390 [DOI] [PMC free article] [PubMed] [Google Scholar]