Abstract
Background
Coronoid fractures often occur with complex elbow dislocations, accounting for 15% of elbow fractures. The effectiveness of open reduction internal fixation (ORIF) versus arthroscopic-assisted reduction internal fixation (ARIF) surgeries for coronoid fractures remains uncertain. This study aimed to compare the outcomes of these two surgical approaches in treating varus posteromedial injuries.
Methods
This study was conducted and reported following the Preferred Reporting Items for Systematic Reviews and Meta-Analyses guidelines. The study protocol was registered with PROSPERO. The primary outcomes assessed in this study were the functional outcomes measured by the Mayo Elbow Performance Score (MEPS) and the complications associated with each surgical approach.
Results
Analysis of the data from 759 patients included in this study revealed that the mean postoperative MEPS score was higher in the ARIF group compared to the ORIF group (97.5 Vs. 90.7), with the mean improvement in MEPS was 16.6 points (19 for ORIF and 14.3 for ARIF). The complication rate in the ORIF group was 24.6%, while the ARIF group reported a complication rate of 6%.
Conclusion
This study suggests that ARIF surgery can yield comparable and promising outcomes to ORIF surgery for coronoid fractures.
Level of evidence
IV
Keywords: coronoid, coronoid fracture, elbow instability, elbow dislocation, elbow arthroscopy
Introduction
Coronoid fractures are mostly associated with complex elbow dislocation and accounted for up to 15% of elbow fractures. The traditional belief is that a coronoid fracture involves more than 50% of the coronoid process (Regan–Morrey Type III) requires fixation. 1 Understanding the Mayo classification (O'Driscoll Classification), which categorizes coronoid fractures based on their characteristics, is also crucial to determine the best approach. Each type (tip, anteromedial fracture, and base) has different implications for stability and potential complications, with the base and anteromedial fracture often require fixation. 2 However, some studies have shown that elbow instability may occur with smaller avulsion fractures.3,4 The tight insertion of the capsule that attaches closely to the tip may account for these smaller fracture fragments.5,6
More concern has been raised regarding the complexity of injury in The Regan–Morrey type I and II fractures. A recent consensus has agreed to fix all coronoid fractures associated with elbow instability. 7 Both arthroscopic-assisted reduction internal fixation (ARIF) and open reduction internal fixation (ORIF) may be performed for the coronoid fracture fixation. However, there is a lack of evidence comparing ORIF and ARIF regarding their outcomes in the same surgical indication.
Our study aimed to compare the surgical outcome of coronoid fixation in varus posteromedial injury treated with ARIF and ORIF by evaluating functional outcome and possible complications.
Methods
Search strategy
This study was conducted and reported in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses Guidelines. 8 The references to the included studies were also reviewed for cross-referencing. The study protocol was registered in the PROSPERO International Prospective Register of Systematic Reviews (CRD42022385094). The PICO of this study were as follows: P (Population): coronoid fracture; I (Intervention): arthroscopic fixation; C (Comparison): open fixation; O (Outcome): functional outcome and complications.
A thorough literature search was performed on PubMed, Medline (via EBSCO), ProQuest, and ScienceDirect in September 2022 with the following search string combination: “coronoid fracture,” “fixation,” “operative,” “surgery,” and “outcome.”
Our literature search in PubMed use these specific string: (((“coronoid"[All Fields] OR “coronoids"[All Fields]) AND (“fractur"[All Fields] OR “fractural"[All Fields] OR “fracture s"[All Fields] OR “fractures, bone"[MeSH Terms] OR (“fractures"[All Fields] AND “bone"[All Fields]) OR “bone fractures"[All Fields] OR “fracture"[All Fields] OR “fractured"[All Fields] OR “fractures"[All Fields] OR “fracturing"[All Fields]) AND (“fixate"[All Fields] OR “fixated"[All Fields] OR “fixates"[All Fields] OR “fixating"[All Fields] OR “fixation"[All Fields] OR “fixational"[All Fields] OR “fixations"[All Fields] OR “fixator"[All Fields] OR “fixator s"[All Fields] OR “fixators"[All Fields])) OR ((“coronoid"[All Fields] OR “coronoids"[All Fields]) AND (“fractur"[All Fields] OR “fractural"[All Fields] OR “fracture s"[All Fields] OR “fractures, bone"[MeSH Terms] OR (“fractures"[All Fields] AND “bone"[All Fields]) OR “bone fractures"[All Fields] OR “fracture"[All Fields] OR “fractured"[All Fields] OR “fractures"[All Fields] OR “fracturing"[All Fields]) AND (“operability"[All Fields] OR “operable"[All Fields] OR “operate"[All Fields] OR “operated"[All Fields] OR “operates"[All Fields] OR “operating"[All Fields] OR “operation s"[All Fields] OR “operational"[All Fields] OR “operative"[All Fields] OR “operatively"[All Fields] OR “operatives"[All Fields] OR “operator"[All Fields] OR “operator s"[All Fields] OR “operators"[All Fields] OR “surgery"[MeSH Subheading] OR “surgery"[All Fields] OR “operations"[All Fields] OR “surgical procedures, operative"[MeSH Terms] OR (“surgical"[All Fields] AND “procedures"[All Fields] AND “operative"[All Fields]) OR “operative surgical procedures"[All Fields] OR “operation"[All Fields])) OR ((“coronoid"[All Fields] OR “coronoids"[All Fields]) AND (“fractur"[All Fields] OR “fractural"[All Fields] OR “fracture s"[All Fields] OR “fractures, bone"[MeSH Terms] OR (“fractures"[All Fields] AND “bone"[All Fields]) OR “bone fractures"[All Fields] OR “fracture"[All Fields] OR “fractured"[All Fields] OR “fractures"[All Fields] OR “fracturing"[All Fields]) AND (“surgical procedures, operative"[MeSH Terms] OR (“surgical"[All Fields] AND “procedures"[All Fields] AND “operative"[All Fields]) OR “operative surgical procedures"[All Fields] OR “surgical"[All Fields] OR “surgically"[All Fields] OR “surgicals"[All Fields]) AND (“outcome"[All Fields] OR “outcomes"[All Fields])))
Study selection
All included studies in this investigation contained original data published in English within the past 20 years. The studies that were included focused on investigating the outcomes of coronoid fixation using either an arthroscopic or open approach for coronoid fractures, with or without posteromedial rotatory injuries. The following type of studies were excluded from the investigation: studies published before 2002, studies not in English, studies specifically related to terrible triad injury, trans-olecranon fracture, radial head arthroplasty, elbow fracture involving more than three columns of the elbows as described by Ring et al., 9 studies involving associated musculoskeletal procedures at the time of surgery (lateral or medial ligament repair or reconstruction, capsule plication, or bony procedures such as radial head), and animal studies.
Quality appraisal and risk of bias assessment
Two independent authors (orthopedic surgery resident and intern) were responsible for the identification, selection, data extraction, and quality assessment processes. In case of conflicting opinions between the reviewers, reassessment and discussion with another author were conducted to reach a resolution. The quality analysis of the literature was evaluated using the methodologic index for non-randomized studies (MINORS). The MINORS includes a 12-item checklist for assessing methodological quality, consisting of eight common items and four additional items. 10 Each item is scored on a scale from 0 to 2, with a maximum score of 16 points for non-comparative studies and 24 points for comparative studies. Since there is no specific cutoff point for scoring, we considered a study to be high quality if scored >60% (9 out of 16). The level of evidence was determined using the Oxford Centre for Evidence-Based Medicine Guideline 2011. 11
Data extraction and analysis
Data were extracted from the text, figures, tables, and associated supplementary files of each included study. These data encompassed the following aspects: (a) article and demographic characteristics (number of patients, number of elbows, mean age, and gender), (b) surgical characteristics, (c) functional outcomes, (d) complications, and (e) rate of return to activities. The primary clinical outcome focused on the functional scores for the ARIF group compared to the ORIF group. Subgroup analysis was performed within the ORIF group to assess surgical approaches and fixation techniques.
Statistical analysis was conducted using the OpenMeta-Analyst software to obtain combined results. The I2 value was used to assess heterogeneity between studies. A random effects model was employed to assess the outcomes in this meta-analysis. Forest plots were utilized for data visualization and outcome identification. Significance was determined as p-values < 0.05.
Results
Study selection
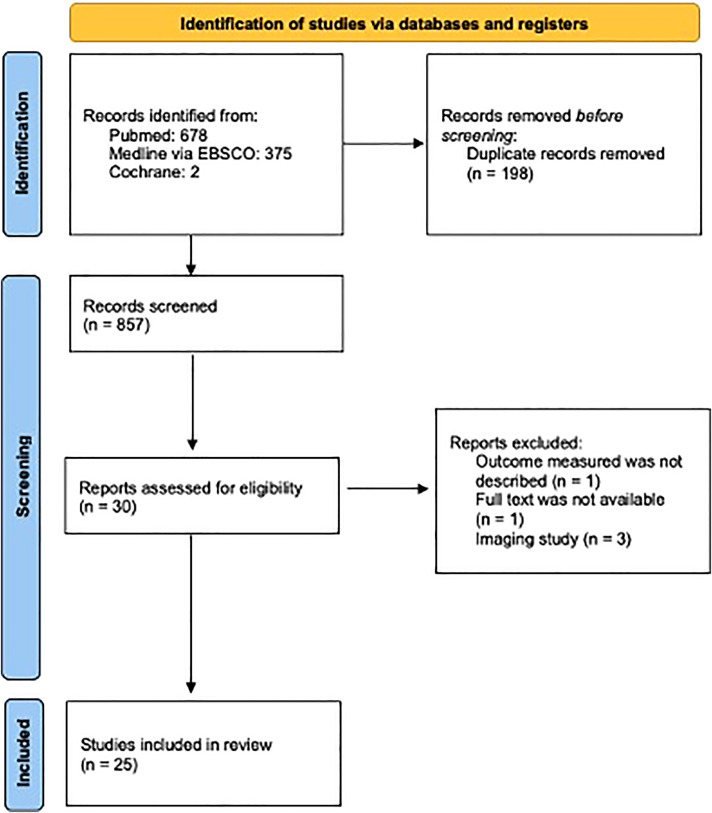
A total of 1055 studies were initially retrieved during the screening process (Figure 1). After excluding duplicates, 859 studies remained. Subsequently, 827 records were removed based on abstract screening. Out of the remaining 31 studies, one article did not provide a description of the outcome measures, 12 one article was without full text, 13 and three articles only focused on imaging analysis.14–16 The search strategy is summarized in Figure 1.
Figure 1.
PRISMA flow chart. PRISMA: Preferred Reporting Items for Systematic Reviews and Meta-Analyses.
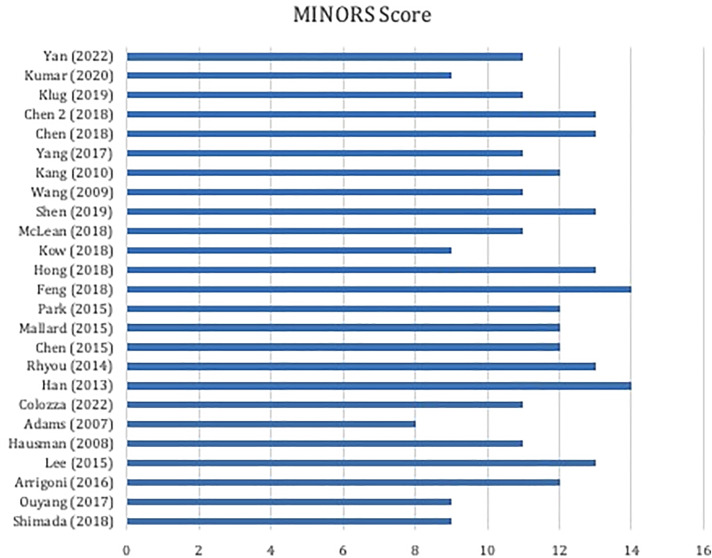
Quality assessment of the study
The level of evidence was assessed using the Oxford Centre for Evidence-Based Medicine Guideline 2011, which found levels 3–4 of evidence in the included studies. 11 The MINORS quality criteria from studies are described in Figure 2. Among the included studies, there were seven articles describing the ARIF approach and 18 articles describing the ORIF approach.
Figure 2.
Distribution of MINORS scores and the range of studies considered high quality. MINORS: methodologic index for non-randomized studies.
Demographic characteristics
The characteristics of twenty-five studies included in our study are presented in Tables 1 and 2. A total of 759 patients (66 ARIF patients and 693 ORIF patients) were included in the current study. The selected studies were published between 2007 and 2022. The postoperative range of motion was found to be higher in the ARIF group (142.0 ± 6.8 (124–150)) than in the ORIF group 115.1 ± 12.5 (94.4–135).
Table 1.
Demographic characteristics of the studies.
| ARIF Group | ORIF Group | |
|---|---|---|
| Number of patients | 66 | 693 |
| Average waiting time (days) | 9 ± 2.2 (5–12) | 4.3 ± 0.5 (2.5–7) |
| Mean follow-up (months) | 23.6 ± 6.8 (10–31.8) | 16.3 ± 9.4 (9.47–68.4) |
| Average age (years) | 43.2 ± 7.0 (26.6–49.9) | 38.5 ± 5.3 (23–47.7) |
ORIF: open reduction internal fixation; ARIF: arthroscopic-assisted reduction internal fixation.
Table 2.
Post-operative characteristics of the studies.
| ARIF Group | ORIF Group | |
|---|---|---|
| Post-operative motion arc (degree) | 142.0 ± 6.8 (124–150) | 115.1 ± 12.5 (94.4–135) |
| Mean union time (months) | 19.7 ± 5.7 (12–24) | 11.9 ± 1.8 (7.8–16.3) |
| Return to activities (%) | 94.3 ± 11.8 | 97.2 ± 3.8 |
ORIF: open reduction internal fixation; ARIF: arthroscopic-assisted reduction internal fixation.
Functional outcomes
The Mayo Elbow Performance Score
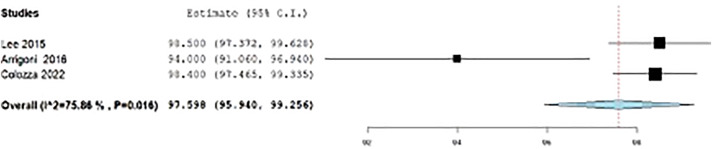
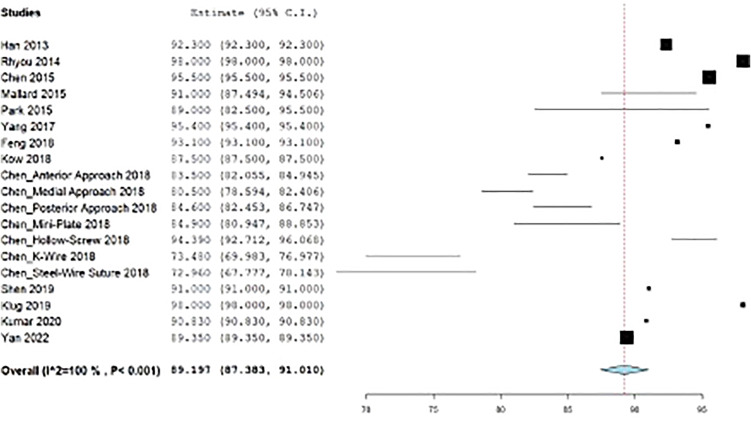
The mean improvement in Mayo Elbow Performance Score (MEPS) was 16.6 points (19 for ORIF and 14.3 for ARIF) as shown in table 3. There were no details regarding the time patients were evaluated. The mean postoperative MEPS was found to be higher in the ARIF group (97.5, 95% CI: 95.9, 99.2, I2 = 85.86%, p = 0.016) (Figure 3) compared to the ORIF group (90.7, 95% CI: 88.7, 92.7, I2 = 100%, p < 0.001) (Figure 4).
Table 3.
The comparison of MEPS between ARIF and ORIF groups.
| ORIF Group | ARIF Group | |
|---|---|---|
| Preoperative MEPS | 87 | 97.5 |
| Postoperative MEPS | 82 | 90.7 |
ORIF: open reduction internal fixation; ARIF: arthroscopic-assisted reduction internal fixation; MEPS: Mayo Elbow Performance Score.
Figure 3.
The Mayo Elbow Performance Score (MEPS) of ARIF group. ARIF: arthroscopic-assisted reduction internal fixation.
Figure 4.
The Mayo Elbow Performance Score (MEPS) of the ORIF group. ORIF: open reduction internal fixation.
Complications
Out of the 759 patients included in the study, a total of 176 complications were observed. These complications were classified into several categories, including joint symptoms (such as heterotopic ossification (HO), stiffness/contracture, persistent instability, and posttraumatic arthritis/degenerative changes), bone healing impairment (including delayed union, malunion, and non-union), infection, nerve symptoms, hardware issues (such as fixation failure/loosening and prominence), and other complications.
In the ORIF group, 172 complications were reported (24.8% of patients), encompassing joint symptoms, bone healing impairment, infection, nerve symptoms, hardware issues, and other complications (Table 4). On the other hand, the ARIF group had four complications (6% of patients), consisting of joint symptoms and nerve symptoms.
Table 4.
The complication rate between ARIF and ORIF groups.
| ORIF Group (%) | ARIF Group (%) | |
|---|---|---|
| No complication | 75.2 | 94 |
| Joint symptoms | 13.8 | 3.2 |
| Joint stiffness | 18.4 | - |
| Heterotopic ossification | 40 | 100 |
| Persistent instability | ||
| Degenerative changes | 16.6 | - |
| 25 | - | |
| Bone-healing impairments | 4.2 | - |
| Infection | 0.3 | - |
| Nerve symptoms | 1.2 | 3.2 |
| Hardware issues | 3.6 | - |
| Others | 1.9 | - |
ORIF: open reduction internal fixation; ARIF: arthroscopic-assisted reduction internal fixation.
Discussion
The current meta-analysis demonstrates that surgical fixation for coronoid fracture using ARIF leads to better surgical outcomes compared to ORIF. The meta-analysis reveals that ARIF is associated with greater postoperative range of motion, superior functional scores, and a lower complication rate in comparison to ORIF for coronoid fracture fixation.
Surgical fixation of coronoid fractures that cause ulnohumeral joint instability or subluxation is recommended to facilitate early motion and prevent elbow stiffness. 17 Both arthroscopic-assisted and open reduction approaches can be utilized for surgical treatment of coronoid fractures. However, surgical management of coronoid fractures poses challenges due to limited surgical accessibility. Literatures have described favorable outcomes with ORIF of coronoid fractures.4,6,18–33 Arthroscopic-assisted surgery for coronoid fractures provides excellent intraarticular visualization and is a minimally invasive procedure that minimize extensive soft tissue dissection. 34 Previous reports have indicated that large flaps and additional skin incisions are associated with complications such as neurovascular injuries, seromas, hematomas, or skin necrosis.35,36
Previous reports have demonstrated good to excellent functional outcomes with arthroscopic fixation for coronoid fractures in four patients. 37 Lee et al. conducted a study on 10 patients and reported excellent MEPS scores within a short follow-up time of 12 weeks. 38 Domos et al. observed MEPS scores of 79 in a group of 22 patients. 39 Additionally, Oh et al. found that patients treated with ARIF had higher MEPS scores (93 vs. 91) and experienced fewer complications compared to those treated with ORIF. 34 In line with these findings, the current meta-analysis indicates a higher MEPS score in the ARIF group (97.5) compared to the ORIF group (90.7). The pre-operative MEPS were found to be higher in the ARIF group since mostly, the time of injury of patients in ARIF group was more recent (Acute to sub-acute) compared to that of patients in the ORIF group. It was also found that patients in the ORIF group sustained the severest injury (based on the Regan–Morrey Classification) compared to those of in the ARIF group. Therefore, the mean improvement was found to be lower in the ARIF group. We also hypothesize that this improvement can be attributed to the reduced surgical dissection of the soft tissues surrounding the elbow during arthroscopic procedures, leading to minimized pain and enhanced postoperative rehabilitation.
Early mobilization is advantageous in order to avoid poor outcomes such as persistent stiffness, pain, and loss of function, as observed in individuals with prolonged immobilization (over 3–4 weeks). 7 The decision to prescribe early mobilization to patients is determined by the stability of the fixation and the extent of soft tissue dissection during surgery. Oh et al. compared ARIF versus ORIF for coronoid fractures and found that elbow flexion was greater in the arthroscopic group (140° vs. 130°; p = 0.04), despite similar outcomes at the 2-year follow-up. 34 In the current meta-analysis, a greater postoperative range of motion was observed following coronoid fixation with ARIF (142°) compared to the ORIF group (115°). In terms of soft tissue preservation, ARIF may provide additional benefits as it allows fixation of the coronoid without major insult to the anterior capsule. The advantage of avoiding extensive surgical approaches and unnecessary damage to surrounding soft tissues facilitates early motion and contributes to reduced pain, enabling early rehabilitation. 40 A retrospective study by Choi et al. reported that patients treated with the ARIF approach were able to initiate range of motion exercises earlier due to the shorter recovery time compared to the ORIF approach. 41
The fracture union time is significantly shorter in the ORIF group compared to the ARIF group (11.9 vs. 19.7 months), with no cases of non-union reported in either group. In our study, plate and screw fixation were predominantly used in the ORIF group, while the ARIF group utilized cannulated screws and Kirschner wire augmented with suture fixation. The main goals of coronoid fixation surgery are to achieve anatomic reduction and stable fixation. The use of more stable fixation techniques in the ORIF group, such as plate and screw, may contribute to the shorter union time. 27 Chen et al. have described plate and screw fixation as superior options that provide rigid fixation, which is crucial for promoting bone healing. 30 However, it is important to note that the bone healing process is influenced by multiple factors and cannot solely rely on the type of fixation used. Patient-related factors such as age, comorbidities, and lifestyle, as well as injury-related factors such as fracture type, severity, and timing of injury, also play significant roles in fracture healing. 42
The return to activities rate in the current study showed no statistical difference between the ORIF group (97.2%) and the ARIF group (94.3%). However, there was insufficient data available regarding the duration of returning to activities since not all studies provided this information. The timing of return to activities is typically determined by the surgeon's discretion, which often takes into account factors such as the type of surgery performed and the functional and radiological outcomes. The shorter union time observed in the ORIF group may contribute to a higher rate of return to activities compared to the ARIF group. Klug et al. reported excellent return to activities rates in 24 patients who underwent open surgery using a pre-formed buttress plate, with 90% of patients returning to their pre-traumatic activities. Only one patient experienced postoperative ulnar dysesthesia, which fully resolved within 3 months. 31
Complications
Heterotopic ossification
HO remains a challenging complication following elbow trauma and surgery. While certain risk factors for the development of HO, such as central nervous system injury and severe burn injuries, have been identified, surgical intervention has also been implicated in HO formation. Direct trauma to the soft tissues surrounding the elbow joint can induce the formation of HO by upregulating inflammatory markers. Therefore, extensive soft tissue injury caused by surgery further increases the risk of HO development. 43 In our study, joint complications related to HO were significantly higher in the ORIF group (13.8%) compared to the ARIF group (3.2%). Agarwal et al. found that the incidence of HO increases in patients who undergo more invasive surgeries, which is directly related to the extent of soft tissue insult.44,45 Conversely, arthroscopic-assisted coronoid fixation procedures have been associated with a lower incidence of HO formation. Xu et al. and Sorkin et al. reported zero incidences of HO following arthroscopic surgery for coronoid fixation.46,47 Adams et al. also concluded that one in seven patients who underwent arthroscopic fixation for coronoid fractures experienced HO. 37
Recurrent instability
The humeral-ulnar articulation, along with the radial head and the medial collateral ligament, plays a crucial role in maintaining elbow stability, with the anterior buttress provided by the coronoid process being particularly important. According to Morrey's classification, the coronoid process acts as one of the elbow stabilizers. Therefore, achieving adequate reduction and fixation in cases of coronoid fracture is imperative for restoring elbow stability.48,49 Karbach et al. also emphasized the significant role of the joint capsule in elbow joint stability. 50 Preserving the integrity of the joint capsule is likely more achievable through arthroscopic-assisted fracture fixation surgery compared to an open approach. In our current study, there were six cases in the ORIF group (16.6%) 51 that experienced recurrent instability following coronoid fracture, while there were no cases of recurrent instability in the ARIF group. Agarwal et al. also noted that although plate and screws provide more stable and adequate fixation, the less invasive nature of arthroscopically assisted surgery could reduce the extent of soft tissue damage, including damage to the joint capsule. 44
As mentioned earlier, due to the limited number of patients and the variability in fracture types, we cannot definitively conclude whether one procedure is superior to another. However, Lanzerath et al. found no significant difference in functional outcomes between different techniques used in the surgical treatment of coronoid fractures. 3 Considering the similar radiological findings observed in both the open and arthroscopic groups, the arthroscopic technique offers advantages in terms of lower complication rates and shorter post-surgical recovery time. On the other hand, the open technique may be more suitable for more complex cases or when there is concomitant injury to the elbow joint that requires additional extra-articular reconstruction.52–56
It is important to note that arthroscopic surgery is considered more technically demanding and requires a surgeon with advanced skills and experience to achieve optimal results and minimize arthroscopic-related complications.27,34
Strength and limitations
As the first meta-analysis comparing ARIF and ORIF in coronoid fixation, our study has several strengths. We conducted a comprehensive literature search using three large databases and included 26 studies in our analysis, providing a comprehensive overview of the available evidence. We structured the data from the included articles in a systematic manner, enhancing the reliability and clarity of our findings. However, it is important to acknowledge the limitations of our study. We had a relatively small number of patients included, with a total of 430 elbows analyzed (68 in the arthroscopic group and 362 in the open group). This small sample size may limit the generalizability of our results and the statistical power to detect small differences between the groups. One possible reason for the limited number of patients in the arthroscopic group is the technical complexity associated with arthroscopic procedures, leading to a lower frequency of their performance compared to the open approach. Furthermore, the heterogeneity in surgical fixations and approaches across the included studies also poses a challenge in making direct comparisons and determining the superiority of each technique. The variability in surgical techniques and fixation methods may introduce additional confounding factors that could impact the outcomes. There was also no detail regarding the timing of examination in the included article. To address these limitations, future studies should aim to have a higher level of evidence in the coronoid fixation approach and a larger sample size. Conducting well-designed prospective studies with standardized protocols and larger patient cohorts comparing open and arthroscopic techniques will provide more robust evidence to guide clinical decision-making in the management of coronoid fractures.
Conclusion
This meta-analysis study demonstrates that arthroscopically assisted coronoid fixation yields comparable surgical outcomes to open surgery fixation.
Supplemental Material
Supplemental material, sj-docx-1-sel-10.1177_17585732241229636 for Surgical outcomes and complication rates of arthroscopic-assisted fixation versus open fixation for coronoid fractures: A systematic review and meta-analysis by Erica Kholinne, Hua Liu, Leonard Christianto Singjie, Maria Anastasia, Jae-Man Kwak and In-Ho Jeon in Shoulder & Elbow
Footnotes
Contributorship: EK: conception, design of the study, interpretation of data, critically revising for important intellectual content, and final approval. HL: conception, design of the study, acquisition of data, and drafting the article. LCS: acquisition of data, analysis, interpretation of data, drafting the article, and revising it critically for important intellectual content. MA: acquisition of data, interpretation of data, drafting the article, and revising it critically for important intellectual content. JMK: conception, design of the study, and final approval of the version to be submitted. IHJ: final approval of the version to be submitted.
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The authors received no financial support for the research, authorship, and/or publication of this article.
Guarantor: EK
ORCID iDs: Erica Kholinne https://orcid.org/0000-0002-4326-8205
In-Ho Jeon https://orcid.org/0000-0002-9289-9193
Supplemental Material: Supplemental material for this article is available online.
References
- 1.Thayer MK, Swenson AK, Hackett DJ, et al. Classifications in brief: Regan-Morrey classification of coronoid fractures. Clin Orthop Relat Res 2018; 476: 1540–1543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.O’Driscoll SW. Elbow instability. Hand Clin 1994; 10: 405–415. [PubMed] [Google Scholar]
- 3.Lanzerath F, Hackl M, Wegmann K, et al. The treatment of anteromedial coronoid facet fractures: a systematic review. J Shoulder Elbow Surg 2021; 30: 942–948. [DOI] [PubMed] [Google Scholar]
- 4.Kumar D, Sodavarapu P, Kumar K, et al. Functional outcome of surgically treated isolated coronoid fractures with elbow dislocation in young and active patients. Cureus 2020; 12: e10883. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.de Klerk HH, Ring D, Boerboom L, et al. Coronoid fractures and traumatic elbow instability. JSES Int 2023; 7: 2587–2593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Park SM, Lee JS, Jung JY, et al. How should anteromedial coronoid facet fracture be managed? A surgical strategy based on O’Driscoll classification and ligament injury. J Shoulder Elbow Surg 2015; 24: 74–82. [DOI] [PubMed] [Google Scholar]
- 7.Wells J, Ablove RH. Coronoid fractures of the elbow. Clin Med Res 2008; 6: 40–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Page MJ, McKenzie JE, Bossuyt PM, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. Syst Rev 2021; 10: 1–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ring D, Jupiter JB. Fracture-dislocation of the elbow. Hand Clin 2002; 18: 55–63. [DOI] [PubMed] [Google Scholar]
- 10.Slim K, Nini E, Forestier D, et al. Methodological index for non-randomized studies (MINORS): development and validation of a new instrument. ANZ J Surg 2003; 73: 712–716. [DOI] [PubMed] [Google Scholar]
- 11.Howick J, Chalmers I, Lind J, et al. Oxford Centre for Evidence-Based Medicine 2011 Levels of Evidence, http://www.cebm.net/index.aspx?o=5653 (accessed 11 January 2023).
- 12.Doornberg JN, Ring D. Coronoid fracture patterns. J Hand Surg 2006; 31: 45–52. [DOI] [PubMed] [Google Scholar]
- 13.Liu G, Hu J, Ma W, et al. Surgical treatment for terrible triad injury of the elbow with anteromedial coronoid fracture through a combined surgical approach. J Int Med Res 2018; 46: 3053–3064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Rausch V, Neugebauer S, Leschinger T, et al. Injuries to the coronoid process of the ulna with involvement of the lesser sigmoid notch. Z Orthop Unfall 2022; 160: 35–39. [DOI] [PubMed] [Google Scholar]
- 15.Morellato J, Louati H, Desloges W, et al. Fixation of anteromedial coronoid facet fractures: a biomechanical evaluation of plated versus screw constructs. J Orthop Trauma 2018; 32: e451–e456. [DOI] [PubMed] [Google Scholar]
- 16.Budoff JE, Meyers DN, Ambrose CG. The comparative stability of screw versus plate versus screw and plate coronoid fixation. J Hand Surg Am 2011; 36: 238–245. [DOI] [PubMed] [Google Scholar]
- 17.Manidakis N, Sperelakis I, Hackney R, et al. Fractures of the ulnar coronoid process. Injury 2012; 43: 989–998. [DOI] [PubMed] [Google Scholar]
- 18.Han SH, Yoon HK, Rhee SY, et al. Anterior approach for fixation of isolated type III coronoid process fracture. Eur J Orthop Surg Traumatol 2013; 23: 395–405. [DOI] [PubMed] [Google Scholar]
- 19.Rhyou IH, Kim KC, Lee JH, et al. Strategic approach to O’Driscoll type 2 anteromedial coronoid facet fracture. J Shoulder Elbow Surg 2014; 23: 924–932. [DOI] [PubMed] [Google Scholar]
- 20.Mallard F, Hubert L, Steiger V, et al. An original internal fixation technique by tension band wiring with steel wire in fractures of the coronoid process. Orthop Traumatol Surg Res 2015; 101: S211–S215. [DOI] [PubMed] [Google Scholar]
- 21.Chen H, Wang Z, Li J, et al. Treatment of the coronoid process fractures with anteromedial approach: a case report. Int J Clin Exp Med 2015; 8: 19607–19611. [PMC free article] [PubMed] [Google Scholar]
- 22.Feng D, Zhang X, Jiang Y, et al. Plate fixation through an anterior approach for coronoid process fractures. Medicine (Baltimore) 2018; 97: e12041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Yang X, Chang W, Chen W, et al. A novel anterior approach for the fixation of ulnar coronoid process fractures. Orthop Traumatol Surg Res 2017; 103: 899–904. [DOI] [PubMed] [Google Scholar]
- 24.Chen HW, Teng XF. A comparative study on the validity and reliability of anterior, medial, and posterior approaches for internal fixation in the repair of fractures of the coronoid process of the ulna. Eur J Med Res 2018; 23: 40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.McLean J, Kempston MP, Pike JM, et al. Varus posteromedial rotatory instability of the elbow: injury pattern and surgical experience of 27 acute consecutive surgical patients. J Orthop Trauma 2018; 32: e469–e474. [DOI] [PubMed] [Google Scholar]
- 26.Kow RY, Zakaria ZM, Khan ESKM, et al. Isolated Regan-Morrey type III fracture of the ulnar coronoid process: a report of two cases. J Orthop Case Rep 2018; 8: 65–67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Chen ACY, Weng CJ, Chou YC, et al. Anteromedial fractures of the ulnar coronoid process: correlation between surgical outcomes and radiographic findings. BMC Musculoskelet Disord 2018; 19: 248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Wang Y, Meng Q, Wu J, et al. Treatment of fractures of the ulnar coronoid process. Orthop Surg 2009; 1: 269–274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Kang LQ, Ding ZQ, Sha M, et al. A minimally invasive anterior approach to reduction and screw fixation of coronoid fractures. J Hand Surg Eur Vol 2010; 35: 224–227. [DOI] [PubMed] [Google Scholar]
- 30.Chen HW, He HH, Gao BL. Efficacy of internal fixation with mini plate and internal fixation with hollow screw for Regan-Morrey type II and III ulna coronoid fractures. BMC Musculoskelet Disord 2018; 19: 194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Klug A, Buschbeck S, Gramlich Y, et al. Good outcome using anatomically pre-formed buttress plates for anteromedial facet fractures of the coronoid—a retrospective study of twenty-four patients. Int Orthop 2019; 43: 2817–2824. [DOI] [PubMed] [Google Scholar]
- 32.Shen JJ, Qiu QM, Gao YB, et al. Direct anterior approach for mini plate fixation of Regan–Morrey type II comminuted ulnar coronoid process fracture. J Orthop Surg 2019; 27: 230949901882522. [DOI] [PubMed] [Google Scholar]
- 33.Yan R, Wu Y, Xiang Z, et al. A novel suture-preset spring plate system (SSPS) for comminuted coronoid process fracture in the elbow. Orthop Surg 2022; 14: 2580–2590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Oh WT, Do WS, Oh JC, et al. Comparison of arthroscopy-assisted vs. open reduction and fixation of coronoid fractures of the ulna. J Shoulder Elbow Surg 2021; 30: 469–478. [DOI] [PubMed] [Google Scholar]
- 35.Dowdy P, Bain G, King G, et al. The midline posterior elbow incision. An anatomical appraisal. J Bone Joint Surg Br 1995; 77: 696–699. [PubMed] [Google Scholar]
- 36.Englert C, Zellner J, Koller M, et al. Elbow dislocations: a review ranging from soft tissue injuries to complex elbow fracture dislocations. Adv Orthop 2013; 2013: 1–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Adams JE, Merten SM, Steinmann SP. Arthroscopic-assisted treatment of coronoid fractures. Arthroscopy 2007; 23: 1060–1065. [DOI] [PubMed] [Google Scholar]
- 38.Lee JM, Yi Y, Kim JW. Arthroscopically assisted surgery for coronoid fohractures. Orthopedics 2015; 38: 742–746. [DOI] [PubMed] [Google Scholar]
- 39.Domos P, Ascione F, Wallace AL. Arthroscopic Bankart repair with remplissage for non-engaging Hill-Sachs lesion in professional collision athletes. Shoulder Elbow 2019; 11: 17–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Fournier M, Corning E, Witt A, et al. Arthroscopically assisted fixation of terrible triad variant injuries of the elbow with small-bore needle arthroscopy. Arthrosc Tech 2021; 10: e1469–e1474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Choi CH, Seok HG, Park SG. Arthroscopic reduction and fixation of coronoid fractures with bending K-wire: a new technique. J Clin Med 2022; 11: 4964. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Mills LA, Aitken SA, Simpson AHRW. The risk of non-union per fracture: current myths and revised figures from a population of over 4 million adults. Acta Orthop 2017; 88: 434–439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Shukla DR, Pillai G, McAnany S, et al. Heterotopic ossification formation after fracture-dislocations of the elbow. J Shoulder Elbow Surg 2015; 24: 333–338. [DOI] [PubMed] [Google Scholar]
- 44.Agarwal S, Loder S, Brownley C, et al. Inhibition of Hif1α prevents both trauma-induced and genetic heterotopic ossification. Proc Natl Acad Sci 2016; 113: E338–E347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Meyers C, Lisiecki J, Miller S, et al. Heterotopic ossification: a comprehensive review. JBMR Plus 2019; 3: e10172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Xu Y, Huang M, He W, et al. Heterotopic ossification: clinical features, basic researches, and mechanical stimulations. Front Cell Dev Biol 2022; 10: 770931. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Sorkin M, Huber AK, Hwang C, et al. Regulation of heterotopic ossification by monocytes in a mouse model of aberrant wound healing. Nat Commun 2020; 11: 722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Sanchez-Sotelo J, Morrey M. Complex elbow instability: surgical management of elbow fracture dislocations. EFORT Open Rev 2016; 1: 183–190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Pugh DMW, Wild LM, Schemitsch EH, et al. Standard surgical protocol to treat elbow dislocations with radial head and coronoid fractures. J Bone Joint Surg Am 2004; 86: 1122–1130. [DOI] [PubMed] [Google Scholar]
- 50.Karbach LE, Elfar J. Elbow instability: anatomy, biomechanics, diagnostic maneuvers, and testing. J Hand Surg Am 2017; 42: 118–126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Hausman MR, Klug RA, Quereshi S, et al. Arthroscopically assisted coronoid fracture fixation: a preliminary report. Clin Orthop Relat Res 2009; 466: 3147–3315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Arrigoni P, D’Ambrosi R, Cucchi D, et al. Arthroscopic fixation of coronoid process fractures through coronoid tunnelling and capsular prication. Joints 2016; 4: 153–158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Ouyang K, Wang D, Lu W, et al. Arthroscopic reduction and fixation of coronoid fractures with and exchange rod-a new technique. 2017; 12: 9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Shimada N, Shirakilt K, Saita K. Arthroscopic osteosynthesis for the treatment of coronoid process fractures: a case series. Case Rep Orthop 2018; 19: 8512963. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Colozza A, Menozzi M, Perna L, et al. Results of arthroscopically assisted reduction and fixation of anteromedial facet coronoid fractures at short-term follow-up. J Shoulder Elbow Surg 2022; 31: 1890–1897. [DOI] [PubMed] [Google Scholar]
- 56.Chen HW, Huang MS. Risk factors of efficacy for patients receiving surgical treatment following terrible triad of the elbow joint: a comparative study. Medicine (Baltimore) 2019; 98: 13836. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-docx-1-sel-10.1177_17585732241229636 for Surgical outcomes and complication rates of arthroscopic-assisted fixation versus open fixation for coronoid fractures: A systematic review and meta-analysis by Erica Kholinne, Hua Liu, Leonard Christianto Singjie, Maria Anastasia, Jae-Man Kwak and In-Ho Jeon in Shoulder & Elbow