Abstract
Objective
To develop an evidence- and consensus-based Digital Healthcare Equity Framework (the Framework) that guides users in intentionally considering equity in healthcare solutions that involve digital technologies.
Materials and Methods
We conducted an environmental scan including a scoping review of the literature and key informant interviews with health equity and digital healthcare technology thought leaders and convened a technical expert panel (TEP).
Results
We grouped similar concepts from the scoping review and key informant interviews, synthesized them into several primary domains and subdomains, and presented the composite list of domains and subdomains to the TEP for their input. From those, we derived the following domains for the Framework: (1) Patient and Community Characteristics, (2) Health System Characteristics, and (3) Health Information Technology Characteristics. We structured the Framework around the following 5 phases of the digital healthcare lifecycle: planning, development, acquisition, implementation/maintenance, and monitoring/improvement/equity assessment.
Discussion
The proposed Framework is designed to specify the aspects that need to be considered in a systematic and intentional approach to ensure digital healthcare solutions improve, and not exacerbate, healthcare inequities.
Conclusion
The proposed Framework serves as a tool to help users and other stakeholders assess whether their healthcare solutions that involve digital technologies are equitable at every phase of the digital healthcare lifecycle.
Keywords: Digital Healthcare, Health Equity, consensus-based framework
Introduction
Digital technologies are an increasingly important means of gaining access to employment, housing, education, and social networks.1 Their role in healthcare delivery is growing and includes both patient-facing solutions and clinician-facing solutions. In particular, individuals in communities who currently experience sub-optimal and timely access to high-quality healthcare could benefit the most from enhanced digital healthcare solutions that help address the health and well-being challenges they now experience.2,3
Despite the considerable opportunities that digital healthcare technologies provide, substantial disparities due to race, ethnicity, and socioeconomic status still exist in access to and utilization of digitally supported healthcare services.4–6 The positive impact of digital technologies on individual and population health will be limited if the unique characteristics, needs, and capabilities of all patient groups are not considered at each phase of the digital healthcare lifecycle, the process used in technology development aligned with quality improvement approaches such as the “Deming Wheel” and the Institute for Healthcare Improvement’s (IHI’s) model of “Plan, Do, Study, Act.”7–9 Considerations ranging from a lack of patient digital literacy to a lack of broadband access—which is collectively often referred to as the digital divide—may impact the viability (eg, implementation and successful use across different communities) of healthcare solutions that involve digital technologies and tools.10–12
Growing concerns over the digital divide and their impact on the application of healthcare technologies in the United States and across the world has created a demand for an approach to serve as a core framework to intentionally consider equity throughout the lifecycle of digital healthcare solutions.13–15 This systematic approach is essential to consider the unique needs and capabilities (eg, a patient’s digital literacy) of all applicable patient groups, as well as social determinants, social risks, and social needs in the built environment, where they live, work, or socialize (eg, a patient’s broadband access). The first step of such a process is the development of a digital healthcare equity framework to specify the aspects that need to be considered when creating, planning, and assessing the performance of equitable healthcare solutions that involve digital technologies.
This article aims to present a Digital Healthcare Equity Framework (the Framework), an evidence- and consensus-based framework that guides users in intentionally considering equity in healthcare solutions that involve digital technologies. The Framework is accompanied by an implementation guide that contains key steps and recommendations to help users implement the Framework (the guide is presented in a separate article). This development process involved extensive input from a diverse and varied national advisory group from across the United States (a technical expert panel; TEP) and was supported by the Agency for Healthcare Research and Quality of the U.S. Department of Health and Human Services.16
The Framework is designed as a tool to help users and other stakeholders (in the United States and potentially globally) intentionally consider equity during each phase of the digital healthcare lifecycle: the planning and development phases (eg, for digital healthcare developers and vendors), the acquisition phase (eg, for healthcare provider/payer organizations), and the implementation/maintenance and the monitoring/improvement/equity assessment phase (eg, for health systems or clinician practices). The Framework is intended to apply to both patient-/consumer-facing and clinician-/provider-facing digital healthcare solutions and address the accessibility, purpose, security, privacy features, usability, and safety concerns applying to those digital solutions (refer to Table S1 for the definitions we developed and applied for key terms and concepts that were central to this development process).
Materials and methods
The development of the Framework was informed by an environmental scan, which included a scoping literature review and key informant interviews, engagement of the national TEP in various manners, and reviews by a panel of internal and external advisors. The development process took place over 2 years starting in 2021 and ending in 2023 (refer to Figure S1 for a summary of the key project phases and timeline).
As a first step in developing the Framework, an environmental scan was conducted to identify existing related frameworks and best practices for designing equitable healthcare solutions that involve digital technologies. The scan included 2 components: a scoping literature review and interviews with key informants.
Environmental scan—scoping review
The scoping review aimed to identify existing US and international digital healthcare equity frameworks and literature reporting on the development or implementation of the frameworks. The details of the environmental scan’s search strategy are available in a published report.17 Articles that both described a framework and those that offered recommendations on developing a framework or implementing it in different settings were identified. Thus, PubMed, CINAHL, and PsycINFO database searches were conducted, as well as a hand search of reference lists of included articles and relevant systematic reviews, selected health informatics journals, and gray literature on relevant websites. Two reviewers independently screened each abstract. Articles promoted to round 2 screening underwent a full-text review by 2 independent reviewers. The selected literature was organized according to frameworks addressing either digital healthcare solutions or those addressing healthcare equity.
Environmental scan—key informant interviews
The key informant interview component of the scoping review included discussions with health equity and digital technology thought leaders about their experiences and perspectives on intentionally integrating healthcare equity into healthcare solutions involving digital technologies and products. Nine thought leaders and experts in health equity or digital healthcare with an array of experiences in researching, planning, and implementing health equity initiatives or digital healthcare technologies were interviewed. Individuals with a leadership role within an organization or department that was accountable for health equity and/or digital health were targeted. Key informants from organizations serving underrepresented populations, or who identified themselves with an underrepresented population, including rural, racial/ethnic underrepresented populations, patients with disabilities, and sexual minority populations were prioritized. Steps were taken to ensure informants represented a mix of geographies and organization sizes (see Table S2 for the list of key informants, their organizational background, and expertise). A semi-structured interview guide was used to facilitate individual, hour-long interviews. Questions focused on developing both an understanding of the key informant’s specific experiences and background related to digital healthcare or health equity and on soliciting input on best practices that could inform our framework (see Table S3 for the interview guide).
Technical expert panel review and survey
A 31-member TEP comprised of digital healthcare and health equity experts was convened to ascertain their perspectives on the development of the evidence- and consensus-based digital healthcare equity framework (see Table S4 for the list of diverse and nationally representative TEP members and their organizations). The TEP members included thought leaders representing health plans, healthcare delivery systems, digital healthcare or health equity researchers, public health experts, digital healthcare developers and health IT vendors, and patient advocates. The TEP members comprised diverse expertise in research, planning, and implementation of health equity initiatives and/or digital health technologies. Additionally, the TEP members were targeted if they possessed a leadership role within an organization or department accountable for promoting health equity or supporting digital healthcare tool development. Through different expert panel engagements (2 meetings with all panel members, 2 small group discussion sessions with a subset of panel members, and a survey to all panel members), feedback was sought on how to best address equity issues in healthcare solutions that involve digital technologies. The feedback from the TEP members focused on reviewing the Framework and the proposed list of domains and subdomains that were drafted (see Supplementary Material S5 for the details about the group discussion sessions and the TEP survey).
Results
General findings from the scoping review
As part of the scoping review, we identified 124 published articles that met the inclusion criteria, of which 60 targeted health equity, 51 targeted digital healthcare, and 13 targeted both digital healthcare and health equity (refer to the environmental scan report17 for more details). The majority of the proposed frameworks were developed by independent researchers/experts, and in only a few instances were frameworks developed by a national (eg, National Academy of Medicine,18 Diabetes Wellness and Prevention Coalition)19 or international organization (eg, Dutch Center for Consumer Experiences in Healthcare,20 World Health Organization’s [WHO’s] regional and Country office in Ghana).21 Other approaches for framework development included engaging key informants, performing a literature review, using surveys and focus groups, and participatory research.
About one-third of the articles identified health systems as their target audience. Furthermore, most frameworks did not specify an applicable patient population and very few proposed concepts were specifically applicable to groups of special interest, such as the elderly patients or the medically underserved. The scoping review identified only a few frameworks that focused specifically on digital healthcare equity,22,23 despite a wealth of frameworks that focused on social determinants, needs, and risk factors. Only a few frameworks covered the concepts applicable to both health equity and digital technologies. In the digital healthcare space, frameworks have been proposed to understand how evolving digital technologies are applied in healthcare. Most of the proposed frameworks for the design of healthcare solutions that involve digital technologies lacked equity intentionality in their recommendations, guidelines, and best practices.18,22,24,25
Key features of exemplar frameworks addressing digital healthcare equity
Only a few of the articles we identified proposed frameworks that addressed both healthcare solutions that involve digital technologies and equity concepts. For example, the Digital Health Equity Framework (DHEF)22 identified the digital determinants of health and their interaction with other intermediate health factors, such as psychosocial stressors, preexisting health conditions, health-related beliefs, and behaviors. Hughes et al26 used the Health Equity Impact Assessment (HEIA),27 a flexible and practical assessment tool capable of identifying potential unintended positive or negative impacts of a policy, program, or initiative on disadvantaged or marginalized groups. They proposed the Telehealth Equity Impact Assessment (TEIA) Tool26 as an overarching framework to assess digital healthcare equity in the context of the rapid telehealth expansion due to the COVID-19 pandemic. Moreover, Were et al28 adapted the HEIA framework to the digital healthcare landscape and recommended a framework with 5 steps addressing (1) scope, (2) impacts, (3) mitigation, (4) monitoring, and (5) dissemination strategies for digital healthcare equity assessments. Other notable findings included the recommendations by Rodriguez et al29 to bring equity to patient-facing digital healthcare tools including recommendations for government agencies, vendors, healthcare institutions, clinical providers, and patients.
Domains identified in the scoping review
After reviewing concepts related to digital healthcare equity from identified articles within the scoping review, we grouped similar concepts and categorized them into several primary domains and subdomains. For articles that addressed health equity, we identified 7 primary domains and then from 3 to 7 subdomains for each. For example, some articles presented concepts such as a lack of health insurance coverage or inadequate internet access as potential barriers to equitable use of healthcare solutions involving digital technologies. We synthesized such concepts under the domain of Access to Care and the subdomain of Access to Services.
From articles addressing either digital healthcare alone or a combination of digital healthcare and health equity, we identified 7 primary domains with 4 to 7 subdomains for each domain. For example, some articles presented concepts such as the potential to build in automatic interpretation and active recognition, as well as addressing the barriers to using technology as important factors related to equitable access to digital healthcare solutions involving digital technologies. We synthesized such concepts under the domain of General Characteristics of Digital Healthcare Solutions and the subdomain of Equitable Access.
For health equity frameworks, the most referenced concepts were related to Access to Care. This finding was expected, as the main focus of many equity frameworks was the challenge of access to care for marginalized patient populations, including digital barriers, health literacy, and access to insurance. In frameworks related to either digital healthcare alone or combined digital healthcare-health equity, the most referenced concepts were Patient/Caregiver Characteristics and Technical Characteristics of Healthcare Solutions that involve digital technologies. The focus on patient/caregiver characteristics was promising and highlighted a trend to integrate patient-centered approaches in frameworks addressing the design, development, and implementation of healthcare solutions that involve digital technologies (refer to Tables S3 and S4 in the environmental scan report17 for more details on the domains, subdomains, and examples of the identified concepts).
Contributions from key informant interviews
We identified 4 primary domains based on the concepts that emerged from the key informant interviews: Digital Determinants of Health, Inclusive and Diverse Product Development, Digital Healthcare Technology, and Implementing and Monitoring Digital Healthcare Technologies (refer to Table S7 in the environmental scan report17 for more details on the domains and subdomains identified from the key informant interviews). The identified domains highlighted several barriers and facilitators to health equity. These interrelated structural (eg, policy), environmental, and individual factors may each be relevant to specific phases or multiple phases of the digital healthcare technology lifecycle. For instance, some key informants highlighted the importance of participatory design, community engagement, and considerations related to end-users experiences as major factors to be considered for equitable healthcare solutions that involve digital technologies. We categorized these concepts under the Inclusive and Diverse Product Development domain. These factors may be more critical to be considered during the planning and development of such solutions. Thus, a technology lifecycle approach would help identify critical factors and where they would have the most impact.
Domain and subdomain synthesis
We synthesized the domains and subdomains identified in the scoping review and key informant interviews. While different terminologies were used to describe the different domains and subdomains, there were several conceptual overlaps. To better understand how these domains and subdomains compared to each other, we performed a side-by-side comparison of the different domains and subdomains.
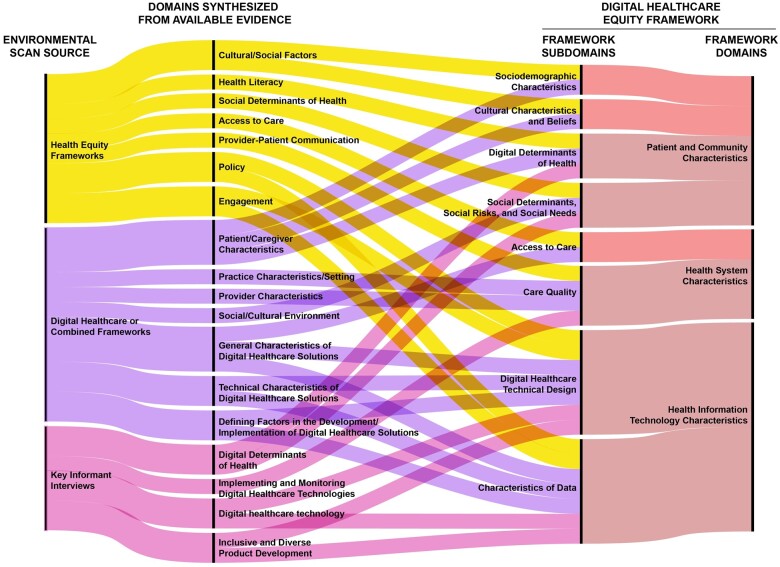
Figure 1 presents the areas of congruence between domains and subdomains identified in health equity frameworks, digital healthcare or combined frameworks, and key informant interviews (left), the synthesized domains from the available evidence (center), and the proposed domains and subdomains in the Framework (right) (also refer to Table S6 for more details on the comparison of synthesized domains and subdomains from the environmental scan). The alignment of domains and subdomains was guided by the specific examples identified in the environmental scan. For example, the subdomain Care Continuity included examples such as “cultural misunderstandings” and “identification of decision options and their implications” derived from health equity framework concepts. These examples matched closely with the Approachability and Appropriateness subdomain, which included examples such as “culturally sensitive services” and “access to care resources” found in digital healthcare frameworks.
Figure 1.
Comparison of synthesized domains and subdomains from environmental scan for the development of the Digital Healthcare Equity Framework.
Several domains and subdomains from the health equity frameworks and digital healthcare frameworks overlapped. For example, the Access to Care domain from health equity frameworks and the General Characteristics of Digital Healthcare Solutions domain from digital healthcare frameworks had overlaps across several subdomains. We also found overlapping domains and subdomains between the key informant interviews and the health equity and digital healthcare frameworks. Notable overlaps in subdomains included: adapting technology to stakeholders’ needs, community engagement, co-creating health solutions with patients, health literacy, and digital determinants of health. Few synthesized subdomains were unique to one component of the environmental scan. These were primarily related to the digital healthcare frameworks and included: user-friendliness, adaptation to other health technologies, interoperability, scalability, and rigorous evaluation and assessment.
Framework contributions from technical expert panel
We presented the composite list of domains and subdomains to the TEP members. Panel members supported the need for a framework and lauded the extensive content gathered during the environmental scan. They suggested improving the clarity and usefulness of the Framework and indicated strong interest in working with the team to address these opportunities to improve the Framework (refer to Supplementary Material S7 for the details of the recommendations from different TEP engagements).
Approach to and an overview of the framework and domains/subdomains
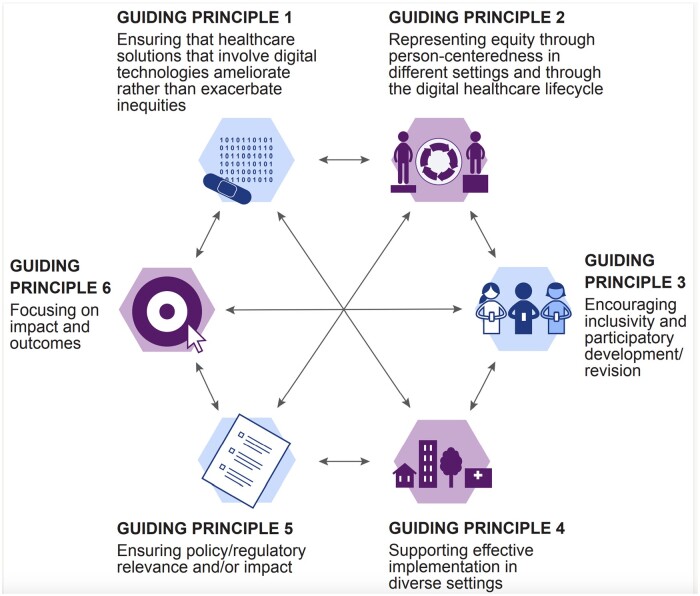
Six principles guided the development of the Framework to ensure equity intentionality across the digital healthcare lifecycle (Figure 2). These principles were based on TEP recommendations as well as the synthesis of the evidence from the environmental scan.
Figure 2.
Guiding principles to ensure equity intentionality across digital healthcare lifecycle.
Framework overview
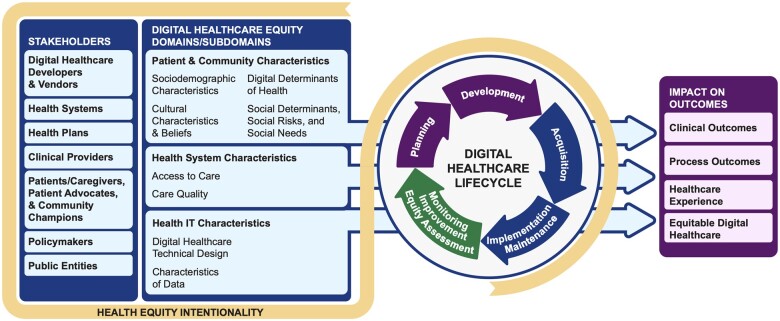
Figure 3 presents an overview of the digital healthcare equity framework developed by the comprehensive process we described in this article. The Framework is intended to guide equity assessment across the digital healthcare lifecycle. While the users of the Framework reflected a smaller subgroup, it specifically called for the engagement of multiple stakeholders. The Framework is designed to improve a range of critical patient outcomes and to provide equitable digital healthcare. Accordingly, it provided definitions of both the specific domains and subdomains and their interactions that users would need to intentionally consider throughout the digital healthcare lifecycle to achieve the desired outcomes.
Figure 3.
Framework for assessing and advancing equity for healthcare solutions that involve digital technologies.
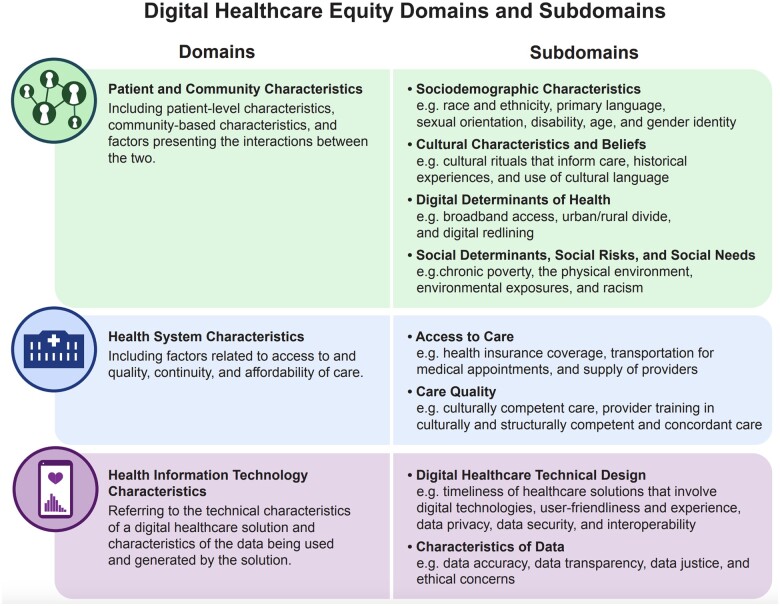
Domains and subdomains
The proposed domains and subdomains were synthesized from the concepts identified in the scoping review, the key informant interviews, and feedback from the TEP members. As noted in the large blue box in Figure 3 (second from the left), 3 overarching domains were identified for intentionally considering equity in digital healthcare solutions, including Patient and Community Characteristics, Health System Characteristics, and Health Information Technology Characteristics, with several relevant subdomains for each domain. Given the central and unique aspect of this component of the framework, we further expanded the domains and subdomains in Figure 4 and defined each domain and specific examples describing each subdomain.
Figure 4.
Domains and subdomains of the Digital Healthcare Equity Framework.
Addressing equity across the digital healthcare lifecycle
Equity intentionality in the context of digital healthcare solutions requires the involvement of different stakeholders at different stages of the development and utilization of such solutions. Thus, the Framework was organized around the digital healthcare lifecycle, a process used in technology development.7 The lifecycle included planning, development, acquisition, implementation/maintenance, and monitoring/improvement/equity assessment of healthcare solutions that involve digital technologies. The lifecycle also aligned with quality improvement approaches such as the “Deming Wheel” and the IHI’s model of “Plan, Do, Study, Act.”8,9
The planning and development phases of the lifecycle were aligned with the “Plan” phase of the IHI model, the acquisition and implementation/maintenance phase was aligned with the “Do” phase, and the monitoring/improvement/equity assessment phase was aligned with the “Study and Act” phases of the IHI model. The framework acknowledged that different stakeholders may enter this process at different points, and each phase of the lifecycle offered opportunities for stakeholders to intentionally consider equity (eg, a stakeholder might enter the Implementation phase of the lifecycle). To ensure equity intentionality during this process, an equity assessment should be completed at each phase of the lifecycle. This equity assessment at each phase of the lifecycle would help identify whether equity could be achieved through a digital healthcare solution alone and when certain populations may need a non-digital alternative solution to address their needs.
Engagement with stakeholders
Stakeholders and their roles in the digital healthcare lifecycle should be considered in developing healthcare solutions that intentionally consider equity. While the users of the Framework would most likely be digital healthcare developers and vendors, health systems, health plans, and clinical providers (eg, clinicians and pharmacists), other key stakeholders (eg, patients, caregivers, patient advocates, community champions, policymakers, and public entities such as public health departments) would be important collaborators in improving health equity. The users of the Framework should provide different opportunities for their contributions in the process.
Impact on outcomes
An intentional approach to considering equity throughout the digital healthcare lifecycle aimed to promote improvement in clinical outcomes (eg, mortality, morbidity, and health/quality of life), process outcomes (eg, care continuity, care coordination, and care quality), and healthcare experiences (eg, patient satisfaction/engagement and provider satisfaction/engagement). It also sought to achieve equitable access to and equity in the quality of healthcare solutions involving digital technologies.
Discussion
The use of digital technologies in healthcare delivery is growing, including both patient-facing and clinician-facing solutions. However, despite the considerable opportunities that these digital healthcare technologies provide, substantial disparities still exist in access to and utilization of healthcare services.4–6 Moreover, the existing digital divide may impact the viability of these digital healthcare tools if consideration is not given to the culture, physical environment (eg, home or workplaces), and social context (eg, communities) of digital health technology users the quality of digital healthcare will suffer and digital healthcare equity will be impacted.10–12 The effectiveness of a given digital healthcare solution will also be diminished if developers are not mindful of these factors in creating institutional digital healthcare strategies or in providing funding and remuneration models for clinical providers.22
To achieve digital healthcare equity, a systematic approach is required to intentionally consider equity throughout the lifecycle of digital healthcare solutions. Digital healthcare equity should be monitored by providers, institutions, insurers, healthcare regulators, and government leaders and should be a key focus of their respective quality efforts. The digital healthcare equity framework will help move from a superficial description of factors to an ecologically comprehensive approach that considers the multitude of sociodemographic, cultural, and economic factors and their interactions that impact health and well-being.22,23
Limitations of available frameworks in the digital healthcare space
Despite the growing concerns over the digital divide and its impact on the application of healthcare technologies and the need for a systematic approach to intentionally consider equity throughout the lifecycle of digital healthcare solutions, the evidence on digital healthcare equity frameworks is scarce. Our scoping review identified very few frameworks that focused specifically on digital healthcare equity.17,22,23 Most frameworks lacked equity intentionality in their recommendations, guidelines, and best practices. For example, while the WHO’s Global Strategy on Digital Health30 report presented several health equity-related approaches throughout, there was no formulated and explicit plan to address digital healthcare equity within the WHO implementation plan.1 Another example was the Evidence Standards Framework for Digital Health Technologies by the UK’s National Institute for Health and Care Excellence (NICE).24 The document described “an evidence standards framework for digital health technologies…that should be available, or developed, for digital health technologies to demonstrate their value in the UK health and care system.”24 The framework proposed a very limited equity analysis as one component of an economic analysis and recommended including subgroup analyses to show the relevant economic impact if there were good clinical data to show that the effects differed by demographic factors. In the United States, Mathews et al25 proposed a pragmatic framework for an objective, transparent, and standards-based evaluation of digital healthcare products across technical, clinical, usability, and cost domains. Although the framework aimed to address the current limitations in the marketplace and to bring greater clarity to the market, it failed to address digital healthcare equity.
The scarcity of frameworks from national or international organizations limited the generalizability of digital healthcare equity concepts because most frameworks developed by independent researchers did not spread beyond their organization and only reached a limited readership if published. In terms of the development process for a framework, only a few articles identified in our scoping review reported a consensus-based approach, and very few identified the health systems as their target audience.17 Furthermore, most frameworks did not specify an applicable patient population, which could help determine the needs to address when proposing different concepts for a framework.17
The DHEF by Crawford and Serhal22 was one of the few examples available in the literature addressing factors relevant to health equity and digital healthcare. However, it was developed by independent researchers in Toronto and was not consensus-based, which may have limited the generalizability of the proposed concepts. The TEIA Tool for Telehealth Equity Impact Assessment by Hughes et al26 was developed with an eye toward real-world implementation to address telehealth equity. Thus, the framework may be limited to a specific digital healthcare solution but still provide practical approaches for implementation in similar settings.
Reviewing the available evidence revealed a lack of schemas that provided a process for intentionally addressing equity in the context of healthcare solutions that involve digital technologies.17 Furthermore, the available frameworks did not adequately acknowledge that there was a process involved in the technology development10 and use, which included different phases such as planning, development, acquisition, implementation/maintenance, and monitoring/improvement/equity assessment. Additionally, the frameworks did not address how health equity should be considered as a critical part of each phase of the process.17 Our environmental scan also highlighted an absence of formal guidelines or common approaches that could inform how healthcare solutions that involve digital technologies could better serve patient populations who have historically been excluded from access to such technologies that have the potential to improve their health.17
Even with the limitation of the existing literature, we were able to identify a set of potentially useful domains and subdomains from the scoping review that informed our proposed Framework and how digital healthcare equity should be planned, structured, and implemented. We built on this with input from the key informant interviews to come up with potential ideas for how we could advance the field by developing and implementing the new Framework presented in this article.
Strengths of the proposed framework
In the development of the Framework, we applied a comprehensive approach that bridged the 2 well-developed distinct concepts of digital healthcare and health equity. In doing so, we sought to find linkages between social determinants, needs, and risk factors relevant to health equity and the implementation of the digital healthcare lifecycle. We intended to focus on the endpoint of digital healthcare equity at the patient and community levels and to suggest actions such as planning and measurement by key stakeholders, including clinicians, delivery systems, IT vendors, health plans, and government agencies.22 This approach also recognized health equity as an essential domain of the quality of digital healthcare, alongside other critical end-points such as person-centeredness, safety, timeliness, effectiveness, and efficiency.31,32
Moreover, our approach acknowledged that to ensure equity intentionality for certain populations, non-digital solutions may need to stand alongside digital ones. For instance, in the context of COVID-19 vaccination, many initial technologies used for vaccination signups relied on internet access and familiarity with digital forms, which was a disadvantage for those who lacked those capabilities. Furthermore, if a digital healthcare solution was designed explicitly for a portion of the patient population needing the solution, it should be labeled accordingly. Entities implementing such a solution could consider best practice alternatives when creating an overarching solution to fit the needs of their entire patient population. Health systems, for example, should not eliminate vaccination signups through patient portals but should offer viable alternatives for patients better served by these analog approaches.
Our proposed Framework was designed to specify key aspects that need to be considered in the systematic and intentional approach to digital healthcare equity. The targeted users of the Framework include digital healthcare developers and vendors, health systems, health plans, and clinical providers. While these supply-side stakeholder groups were considered the primary users of the Framework, other demand-side stakeholders were considered essential collaborators in improving health equity (eg, patients, caregivers, community champions). Thus, users of the Framework are encouraged to include other stakeholders in opportunities to contribute throughout the digital healthcare lifecycle.
The quality improvement approaches for addressing equity gaps proposed in the Framework build on existing approaches for addressing any important identified gaps in quality.32–34 Moreover, the digital healthcare lifecycle is aligned with quality improvement approaches such as the “Deming Wheel” and the IHI’s model of “Plan, Do, Study, Act.”8,9
Conclusion
The proposed Digital Healthcare Equity Framework serves as an evidence- and consensus-based tool to help users such as digital healthcare developers and vendors, health systems, health plans, clinical providers, and other stakeholders assess whether their healthcare solutions that involve digital technologies are equitable at every phase of the digital healthcare lifecycle, including planning, development, acquisition, implementation, and monitoring.
Supplementary Material
Acknowledgments
We would like to acknowledge the following individuals who have contributed their time, knowledge, and expertise to this project: Johns Hopkins University: Karen Robinson, PhD, Smisha Agarwal, PhD, Renee Wilson, MS, Elyse Lasser, DrPH, Allen Zhang, BS, Yvonne Commodore-Mensah, PhD, Shannon Cole, PhD, Christine Holzmueller, BLA, Jeff Day, MD, MA, Jordan Derk, MPH, Meghan Walrath, MA, Phillip Joslin, BS, Preeti Joshi, MBBS, MPH, Karen Klinedinst, BFA, and Courtney Weber, MFA. National Committee for Quality Assurance: Carrie Mills, PhD, Theresa Hwee, MPH, and Kevin Wiley, PhD, MPH. Agency for Healthcare Research and Quality, U.S. Department of Health and Human Services: Kevin Chaney, MGS, Sheena Patel, MPH, and Chris Dymek PhD.
We would also like to acknowledge the contributions of our key informants and technical expert panel, who generously shared their time, experiences, and ideas to make this work meaningful and useful (more information on the key informants and panel members is available in Tables S2 and S4).
Contributor Information
Elham Hatef, Division of General Internal Medicine, Department of Medicine, Johns Hopkins School of Medicine, Baltimore, MD 21205, United States; Center for Population Health Information Technology, Johns Hopkins Bloomberg School of Public Health, Baltimore, MD 21205, United States.
Sarah Hudson Scholle, National Committee for Quality Assurance, Washington, DC 20005, United States.
Bryan Buckley, National Committee for Quality Assurance, Washington, DC 20005, United States.
Jonathan P Weiner, Center for Population Health Information Technology, Johns Hopkins Bloomberg School of Public Health, Baltimore, MD 21205, United States.
John Matthew Austin, Johns Hopkins Armstrong Institute for Patient Safety and Quality, Johns Hopkins Medicine, Baltimore, MD 21202, United States.
Author contributions
Conceptualization: Elham Hatef and John Matthew Austin. Data Curation: Elham Hatef and John Matthew Austin. Investigation and Validation: Elham Hatef, Sarah Hudson Scholle, and John Matthew Austin. Methodology: Elham Hatef, Sarah Hudson Scholle, Bryan Buckley, Jonathan P. Weiner, and John Matthew Austin. Writing - original draft: Elham Hatef and John Matthew Austin. Writing - review & editing: Elham Hatef, Sarah Hudson Scholle, Bryan Buckley, Jonathan P. Weiner, and John Matthew Austin.
Supplementary material
Supplementary material is available at JAMIA Open online.
Funding
This work was funded under contract number 75Q80120D00015 from the Agency for Healthcare Research and Quality (AHRQ), U.S. Department of Health and Human Services (HHS). The authors are solely responsible for the findings and conclusions, which do not necessarily represent the views of AHRQ or HHS. Readers should not interpret any statement in this paper as an official position of position of AHRQ or HHS.
Conflicts of interest
None of the authors have any affiliation or financial involvement that conflicts with the material presented in this framework.
Data availability
The data underlying this article will be shared on reasonable request to the corresponding author.
References
- 1. Baum F, Newman L, Biedrzycki K.. Vicious cycles: digital technologies and determinants of health in Australia. Health Promot Int. 2014;29:349-360. [DOI] [PubMed] [Google Scholar]
- 2.Consumers and Health Information Technology: A National Survey. California Health Care Foundation; 2010. Accessed April 11, 2024. https://www.chcf.org/wp-content/uploads/2017/12/PDF-ConsumersHealthInfoTechnologyNationalSurvey.pdf
- 3.National Healthcare and Disparities Report. Rockville, MD: Agency for Healthcare Research and Quality; 2012. Accessed April 11, 2024. https://www.ahrq.gov/sites/default/files/wysiwyg/research/findings/nhqrdr/nhdr11/nhdr11.pdf
- 4. Pu J, Chewning B.. Racial difference in diabetes preventive care. Res Social Adm Pharm. 2013;9:790-796. [DOI] [PubMed] [Google Scholar]
- 5. Zhang P, Too G, Irwin KL.. Utilization of preventive medical services in the United States: a comparison between rural and urban populations. J Rural Health. 2000;16:349-356. [DOI] [PubMed] [Google Scholar]
- 6. Johnson-Jennings MD, Tarraf W, Xavier Hill K, et al. United States colorectal cancer screening practices among American Indians/Alaska natives, blacks, and non-Hispanic whites in the new millennium (2001 to 2010). Cancer. 2014;120:3192-3299. [DOI] [PubMed] [Google Scholar]
- 7.Technology Development Life Cycle Processes. Albuquerque, NM and Livermore, CA: Sandia National Laboratories. Accessed April 11, 2024. https://www.osti.gov/servlets/purl/1089868
- 8. Best M, Neuhauser D.. Walter a Shewhart, 1924, and the Hawthorne factory. Qual Saf Health Care. 2006;15:142-143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Quality Improvement 102: The Model for Improvement: Your Engine for Change Summary Sheet. The Institute for Healthcare Improvement. Accessed April 11, 2024. https://www.ihi.org/education/ihiopenschool/Courses/Documents/QI102-FinalOnePager.pdf
- 10.Merriam-Webster Dictionary. Accessed April 11, 2024. https://www.merriam-webster.com/dictionary/digital%20divide
- 11. Scheerder A, van Deursen A, van Dijk J.. Determinants of Internet skills, uses and outcomes. A systematic review of the second-and third-level digital divide. Telemat Inform. 2017;34:1607-1624. [Google Scholar]
- 12.2016 Broadband Progress Report. Federal Communications Commission; 2016. Accessed April 11, 2024. https://www.fcc.gov/reports-research/reports/broadband-progress-reports/2016-broadband-progress-report
- 13.The White House Executive Order. Advancing Equity and Racial Justice through the Federal Government. Accessed April 11, 2024. https://www.whitehouse.gov/equity/
- 14.Advancing Equity at the U.S. Department of Health and Human Services. Accessed April 11, 2024. https://www.hhs.gov/equity/index.html
- 15.The U.S. Department of Health and Human Services. The Biden-Harris Administration Takes Action to Improve Health and Wellbeing by Addressing Social Determinants of Health. Accessed April 11, 2024. https://www.hhs.gov/about/news/2023/11/16/biden-harris-administration-takes-action-improve-health-and-wellbeing-addressing-social-determinants-health.html
- 16. Evidence- and Consensus-Based Digital Healthcare Equity Framework. (Prepared by Johns Hopkins University under Contract No. 75Q80120D00015.) AHRQ Publication No. 24-0020-1-EF. Rockville, MD: Agency for Healthcare Research and Quality; February 2024.
- 17. Hatef E, Austin JM, Mills C, et al. Environmental Scan to Determine the Current State of Existing, Related Frameworks and Best Practices for Creating Equitable Healthcare Solutions Involving Digital Technologies. (Prepared by Johns Hopkins University under Contract No. 75Q80120D00015). AHRQ Publication No. 23-0028. Rockville, MD: Agency for Healthcare Research and Quality; June 2023.
- 18. Wetta RE, Severin RD, Gruhler H.. An evidence-based strategy to achieve equivalency and interoperability for social-behavioral determinants of health assessment, storage, exchange, and use. Health Informatics J. 2020;26:1477-1488. [DOI] [PubMed] [Google Scholar]
- 19. Surbhi S, Brooks IM, Shuvo SA, et al. A mid-South chronic disease registry and practice-based research network to address disparities. Am J Manag Care. 2020;26:e211-e218. [DOI] [PubMed] [Google Scholar]
- 20. Thijssing L, Tensen E, Jaspers M.. Patient's perspective on quality of teleconsultation services. Stud Health Technol Inform. 2016;228:132-136. [PubMed] [Google Scholar]
- 21. Olu O, Muneene D, Bataringaya JE, et al. How can digital health technologies contribute to sustainable attainment of universal health coverage in Africa? A perspective. Front Public Health. 2019;7:341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Crawford A, Serhal E.. Digital health equity and COVID-19: the innovation curve cannot reinforce the social gradient of health. J Med Internet Res. 2020;22:e19361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Dover DC, Belon AP.. The health equity measurement framework: a comprehensive model to measure social inequities in health. Int J Equity Health. 2019;18:36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Evidence standards framework for Digital Health Technologies. United Kingdom National Institute for Health and Care Excellence; 2019. Accessed April 11, 2024. https://www.nice.org.uk/Media/Default/About/what-we-do/our-programmes/evidence-standards-framework/digital-evidence-standards-framework.pdf
- 25. Mathews SC, McShea MJ, Hanley CL, et al. Digital health: a path to validation. NPJ Digit Med. 2019;2:38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Hughes HK, Hasselfeld BW, Cooper LA, et al. A process for developing a telehealth equity dashboard at a large academic health system serving diverse populations. J Health Care Poor Underserved. 2021;32:198-210. [Google Scholar]
- 27. Ontario Ministry of Health. Health Equity Impact Assessment (HEIA) tool. Hamilton, ON: National Collaborating Centre for Methods and Tools (NCCMT); 2020. Accessed April 11, 2024. https://www.nccmt.ca/knowledge-repositories/search/146
- 28. Were MC, Sinha C, Catalani C.. A systematic approach to equity assessment for digital health interventions: case example of mobile personal health records. J Am Med Inform Assoc. 2019;26:884-890. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Rodriguez JA, Clark CR, Bates DW.. Digital health equity as a necessity in the 21st century Cures Act era. JAMA. 2020;323:2381-2382. [DOI] [PubMed] [Google Scholar]
- 30. Global Strategy on Digital Health 2020-2025. Geneva: World Health Organization; 2021. License: CC BY-NC-SA 3.0 IGO. Accessed April 11, 2024. https://www.who.int/publications/i/item/9789240020924
- 31. Crossing the Quality Chasm: A New Health System for the 21st Century. Washington, DC: Institute of Medicine Committee on Quality of Health Care in America; 2001.
- 32. Austin JM, Weeks K, Pronovost PJ.. Health system leaders' role in addressing racism: time to prioritize eliminating health care disparities. Jt Comm J Qual Patient Saf. 2021;47:265-267. [DOI] [PubMed] [Google Scholar]
- 33. Lion KC, Raphael JL.. Partnering health disparities research with quality improvement science in pediatrics. Pediatrics. 2015;135:354-361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Chin MH. Quality improvement implementation and disparities: the case of the health disparities collaborative. Med Care. 2010;48:668-675. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data underlying this article will be shared on reasonable request to the corresponding author.