Abstract
Background
The use of the multistate Markov chain model is a valuable tool for studying child undernutrition. This allows us to examine the trends of children's transitions from one state to multiple states of undernutrition.
Objectives
In this study, our objective was to estimate the median duration for a child to first transition from one state of undernutrition to another as well as their first recurrence of undernutrition and also to analyze the typical duration of undernourishment. This involves understanding the central tendency of these transitions and durations in the context of longitudinal data.
Methods
We used a longitudinal dataset from the Young Lives cohort study (YLCS), which included approximately 1997 Ethiopian children aged 1–15 years. These children were selected from five regions and followed through five survey rounds between 2002 and 2016. The surveys provide comprehensive health and nutrition data and are designed to assess childhood poverty. To analyze this dataset, we employed a Markov chain regression model. The dataset constitutes a cohort with repeated measurements, allowing us to track the transitions of individual children across different states of undernutrition over time.
Results
The findings of our study indicate that 46% of children experienced concurrent underweight, stunting, and wasting (referred to as USW). The prevalence of underweight and stunted concurrent condition (US) was 18.7% at baseline, higher among males. The incidence density of undernutrition was calculated at 22.5% per year. On average, it took 3.02 months for a child in a wasting state to transition back to a normal state for the first time, followed by approximately 3.05 months for stunting and 3.89 months for underweight. It is noteworthy that the median duration of undernourishment among children in the US (underweight and stunted concurrently) state was 48.8 months, whereas those concurrently underweight and wasting experienced a median of 45.4 months in this state. Additionally, rural children (HR = 1.75; 95% CI: 1.53–1.97), those with illiterate fathers (HR = 1.50; 95% CI: 1.38–1.62) and mothers (HR = 1.45; 95% CI: 1.02–3.29), and those in households lacking safe drinking water (HR = 1.70; 95% CI: 1.26–2.14) or access to cooking fuel (HR = 1.95; 95% CI: 1.75–2.17) exhibited a higher risk of undernutrition and a slower recovery rate.
Conclusions
This study revealed that rural children, especially those with illiterate parents and households lacking safe drinking water but cooking fuels, face an increased risk of undernutrition and slower recovery.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12874-024-02399-9.
Keywords: Lifetime Undernourished Period, Median First Passage Time, Median Recurrence Time, Transition Intensities, Transition Probability, Young Lives Data
Introduction
The prevalence of undernutrition has shown a decline in Asia from 33% to 27%, in Latin America from 33% to 22%, and in Europe from 20% to 16% [1–3]. However, chronic hunger continues to be an issue in Africa, impacting approximately 50% of children under the age of five. Notably, half of all undernourished children are found in seven specific countries: Nigeria, the Democratic Republic of the Congo (DRC), Ethiopia, India, Pakistan, Bangladesh, and China [2, 4, 5].
The under5 mortality rate is a global concern, with sub-Saharan Africa (sSA) having the highest rate of 1 child out of 13 deaths before the fifth birthday [6]. sSA and central and southern Asia accounted for more than 80% of the under5 deaths in 2019, with half occurring in five countries: Nigeria, India, Pakistan, the Netherlands, and Ethiopia [7]. DRC has a high stunting rate (42% of children under five) in sSA, with undernutrition being the primary cause of nearly half of these deaths [8]. Child undernutrition is a serious health concern in Ethiopia, a developing nation in Africa's Horn [7, 9, 10]. Moreover, a lack of nutrients has an impact on a child's growth, development, and overall health. For several years, Ethiopia has struggled with high rates of child undernutrition [11].
Child undernutrition is a significant issue that has severe consequences, such as increased morbidity, mortality risk, impaired cognitive development, reduced school performance, and decreased productivity in adulthood [7, 10, 12]. Factors contributing to this risk include inadequate dietary intake, poor feeding practices, low household income, food insecurity, limited healthcare access, inadequate sanitation, and lack of education. This long-term issue perpetuates poverty and underdevelopment in communities and nations [9, 12].
The World Health Organization (WHO) [13] defines severe thinness in children as a body mass index (BMI) less than 16 kg/m2 or a Z score less than -3, indicating low undernourishment. Undernourished individuals had Z scores between -3 and -2 (SD) or a BMI between 16 kg/m2 and 18.49 kg/m2.
Ethiopia's child undernutrition is a significant issue due to high rates of stunting (38–57%), wasting (10–17%), and underweight (22–38%) in children under five years of age [14–16].
Traditional statistical models, such as multivariate logistic regression [17], spatial [18], longitudinal [19] and many others, have limitations in predicting future disease states based on the current state and fail to account for the complexity of state transitions. They typically do not account for crucial factors such as the duration of stay, periods of undernourishment, and key metrics like Median First Passage Time (the median time until the first transition into a specific state) and Median First Recurrence Time (the median time until returning to a specific state after leaving it). These limitations highlight the need for advanced models that can better capture the dynamic nature of state transitions in predicting disease progression.
However, the multistate Markov chain model improves disease prediction by quantifying transition probabilities and identifying median transit and recurrence times required for first-time transitions between states. Additionally, it considers influencing factors, which improves risk factor identification and enables targeted interventions to improve child nutritional outcomes [20, 21]. It accurately estimates transition probabilities, aiding in understanding patient progress, intervention effectiveness, and developing nutritional status strategies, especially in developing countries.
In recent years, the study of child undernutrition has increasingly focused on understanding the dynamics of state transitions. Key to this understanding are metrics such as median first passage time, which provides insights into how quickly children transition into undernourished states for the first time [22–26], and median recurrence time, which helps to understand the average time until a child returns to a previous health state after leaving it [27–29]. Additionally, the duration of undernourishment indicates the length of time children remain in these vulnerable states [30]. Together, these measures offer a comprehensive view of the dynamics of undernutrition, enabling researchers to identify critical intervention points and the factors that influence these transitions.
Therefore, this study used a multistate Markov chain model to analyze child undernutrition in Ethiopia, focusing on state transitions (such as normal, underweight, stunted, wasted, and their combinations). It identifies critical periods of transition and the factors influencing them, including socioeconomic, demographic, maternal and caregiving factors. The model estimates transition probabilities between undernutrition states, providing insights into children's health outcomes over time.
The primary goal of this research is to investigate the transitions between different states of nutritional deficiency in children. Specifically, we aim to understand how children move between various nutritional states over time by analyzing the median transit and recurrence times between these states. Additionally, we seek to quantify the median duration that children spend in undernourished states and determine the median duration of these states. We also seek to identify covariates that play significant roles in these transitions. By examining these metrics, we aim to gain insights into the complex patterns of nutritional transitions and to identify key covariates that significantly influence these transitions. This study contributes to enhancing our understanding of the factors affecting child nutrition and informs strategies for intervention and prevention.
This study is the first to examine the median transit and recurrence times between undernourished states, as well as the median duration a child spends in undernourished states, and the identification of covariates significantly associated with these transitions in Ethiopia.
Methods
Data source and study participants
The Young Lives cohort study (YLCS) evaluates the impact of poverty reduction policies and interventions on children's lives in low- and middle-income countries, including Ethiopia. Using an observational cohort design, the cohort included approximately 12,000 boys and girls aged from infancy to adulthood from India, Peru, Vietnam, and Ethiopia. There were two cohorts, a young cohort (aged 1 to 15) and an old cohort (aged 8 to 22) in the survey in all countries. However, for this study, we used only young cohort data collected from Ethiopia [31]. In this cohort, 1997 Ethiopian children were admitted to the study. The children were selected from five regions (Amhara, Oromiya, Tigray, SNNP (Southern Nations, Nationalities, and Peoples' Region), and Addis Ababa CA (city administration)), including urban and rural areas, and followed them longitudinally.
Variables in the study
The data provider used WHO standards to standardize Z scores for each observation and defined children's anthropometric status as underweight, stunted, or wasted as outcome variables. We proceeded with the analysis after cleaning and making necessary adjustments to the dataset. Therefore, the state variables are shown in Table 1 and are classified as follows: normal, underweight only, stunted only, wasted only, underweight and stunted, underweight and wasted, stunted and wasted, and underweight, stunted and wasted concurrently [32]. Children who have a height-for-age Z-score (HAZ), a weight-for-height z-score (WHZ), and weight for age z-score (WAZ) which is below two are defined as having stunting, wasting and underweight respectively [33–35].
Table 1.
Classification and percentage of child undernutrition over time in Ethiopia
| Group | Description of the group | Definition | Underweight | Stunting | Wasting | 2002 | 2006 | 2009 | 2013 | 2016 |
|---|---|---|---|---|---|---|---|---|---|---|
| N | Normal | All WAZ, HAZ, & WHZ > -2SD | No | No | No | 46.2% | 58.1% | 54.1% | 39.6% | 49.9% |
| U | Underweight only | WAZ < -2SD | Yes | No | No | 2.0% | 3.5% | 6.5% | 4.5% | 2.5% |
| S | Stunting only | HAZ < -2SD | No | Yes | No | 16.5% | 15.1% | 4.1% | 1.6% | 1.0% |
| W | Wasting only | WHZ < -2SD | No | No | Yes | 3.2% | 3.0% | 6.8% | 6.6% | 7.3% |
| US | Underweight and stunting | WAZ & HAZ < -2SD | Yes | Yes | No | 18.7% | 14.7% | 13.6% | 13.1% | 10.2% |
| UW | Underweight and wasting | WHZ & WAZ < -2SD | Yes | No | Yes | 6.1% | 4.1% | 11.0% | 20.5% | 14.6% |
| SW | Stunting and wasting | HAZ & WHZ < -2SD | No | Yes | Yes | 0.0% | 0.0% | 0.1% | 0.2% | 0.1% |
| USW | Underweight, stunting, and wasting | All WHZ, WAZ, & HAZ < -2SD | Yes | Yes | Yes | 7.4% | 1.5% | 3.9% | 13.9% | 14.3% |
| Underweight | U + US + UW + USW | 34.2% | 23.8% | 35.0% | 52.0% | 41.6% | ||||
| Stunting | S + US + SW + USW | 42.6% | 31.3% | 21.7% | 28.8% | 25.6% | ||||
| Wasting | W + UW + SW + USW | 16.7% | 8.6% | 21.8% | 41.2% | 36.3% |
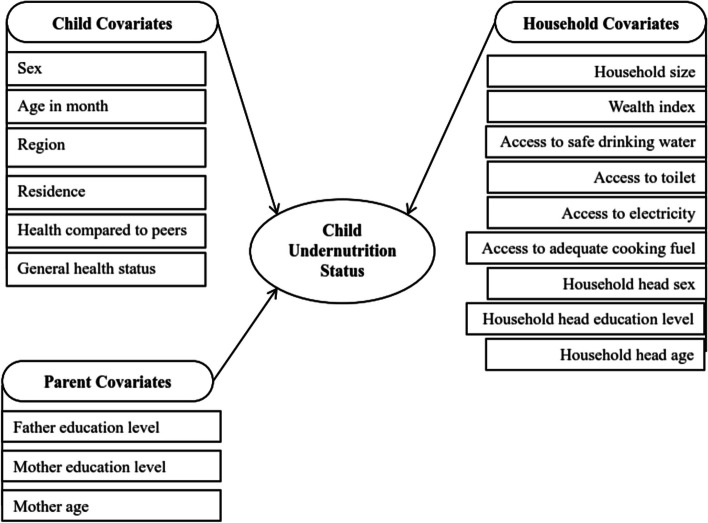
The following figure clearly demonstrates the study's covariates and their connection with the state variable (Fig. 1). However, it is important to note that certain variables widely discussed in literature, such as breastfeeding duration, parental smoking habits, access to prenatal care, exposure to indoor air pollution, maternal employment status, and availability of childcare services, were not included in the dataset.
Fig. 1.
Classifications of covariates in the study associated with child undernutrition
Statistical analysis
This paper utilized a multistate Markov chain model with a set of discrete nutritional states observed at different discrete time points (t = 2002, 2006, 2009, 2013, and 2016) [36].
The Markov chain model is mathematically explained by considering a child's nutritional state at time t (Xt) and transition probability (pij = P(Xt+1 = sj | Xt=si), where P = [pij], 1≤i, j≤8.
In the transition probability matrix P, which is an 8×8 square matrix, each element pij represents nonnegativity, and the row sums to one while transitioning from nutritional state si to sj.
| 1 |
| 2 |
The undernutrition status (N, U, S, W, US, UW, SW, and USW) of the children at each time point was recorded as an outcome variable in the dataset called the state (Fig. 2). A child's condition can be classified into one state if they fall into the normal, underweight, stunted, or wasted category; two states if they experience both conditions simultaneously; and three states if they are simultaneously affected by all three conditions. Therefore, subjects with multiple states at a time are treated using the multistate Markov chain model.
Fig. 2.

State transition diagram
The undernutrition status (N, U, S, W, US, UW, SW, and USW) of the children at each time point was recorded as an outcome variable in the dataset called the state (Fig. 2). A child's condition can be classified into one state if they fall into the underweight, stunted, or wasted categories; into two states if they experience both conditions simultaneously; and into three states if they are simultaneously affected by all three conditions (underweight, stunting, and wasting). The inclusion of the Normal (N) state reflects both the overall health status of children in the dataset and serves as a reference category for comparing undernutrition states. This approach enables a comprehensive assessment of nutritional outcomes and health dynamics within the studied population. Therefore, subjects with multiple states at a time are treated using the multistate Markov chain model.
Median First Passage Time (MFPT) and Median First Recurrence Time (MFRT)
The median is particularly useful in scenarios where the distribution of times may be skewed or when outliers could disproportionately influence the mean. The Median First Passage Time (MFPT), denoted as , represents the median time it takes for a child to transition from nutritional state to state for the first time. This can be computed by identifying the point at which 50% of the transition times from to occur, effectively capturing the typical experience of a child navigating nutritional states.
| 3 |
where, represents the probability that the time to transition from state to is less than or equal to the median value .
Similarly, the Median First Recurrence Time (MFRT), denoted as quantifies the median time required for a child to return to a specific nutritional state after its initial visit. This measure accounts for the recurrence dynamics, reflecting the state’s stability and the likelihood of relapse into previous nutritional states. The calculation involves determining the median of the times taken to return to state across all relevant transitions.
| 4 |
where, is the probability that the time to return to state is less than or equal to the median recurrence time .
Lifetime Undernourished Period (LUP)
The LUP measures the duration spent in undernourished states (U, S, W, US, UW, SW, and USW) over time, considering all possible sequences leading to undernourished periods. It is calculated by summing the probabilities of transitioning to an undernourished state at each time point [30].
| 5 |
where,
is the nutritional state at time t.
represents the undernourished state.
is the probability of transitioning to an undernourished state at time t, given that the nutritional state at time t-1 is not the undernourished state .
is an indicator function that equals 1 if the nutritional state at time t is and 0 otherwise.
Markov regression
The multistate Markov chain model is a statistical technique that analyzes transitions between undernutrition states over time, providing a comprehensive understanding of child undernutrition. It captures the dynamics and an interrelationship among undernutrition states; an estimate transition probability between different combinations of undernutrition states and identifies patterns and determinants of transitions. One key advantage of the model is its ability to estimate transition probabilities between different combinations of under nutritional states, identifying patterns and determinants of transitions [36–39].
Markov regression using transition probabilities is a method that considers the current-state response as an additional covariate alongside usual risk factors and expresses conditional probability as a function of both factors (1-normal, 2-underweight only, 3-stunting only, 4-wasted only, 5-underweight and stunted, 6-underweight and wasted, 7- stunted and wasted, and 8-underweight, stunted and wasted).
| 6 |
The model can be written as follows:
| 7 |
This logistic model considers the current state of child undernutrition and the interaction between and risk factors, allowing us to determine whether a specific risk factor affects response probability.
With a first-order Markov model, the contribution to the likelihood for the ith subject can be written as
| 8 |
The conditional distribution of Yit in a Markov model of order q is
| 9 |
Therefore, the likelihood contribution for the ith subject becomes
| 10 |
The logistic case does not determine from the GLM assumption, and the full likelihood is unavailable. An alternative is to estimate β and α by maximizing the conditional likelihood.
| 11 |
In addition, multistate Markov chain models are governed by transition intensity functions, which represent the instantaneous incidence rate of moving from one state to another state at time t [37].
| 12 |
where Y(t) is the state occupied at time t. This transition intensity is the (j, k) entry of the transition intensity matrix denoted by Λ, the rows of which sum to zero. The model is time homogeneous, which means that or all t. The diagonal entries of Λ are defined by convention as the sum of off diagonal entries with negative magnitude [37].
| 13 |
The model includes other risk factors; hence, the model is where l is the number of risk factors (l = 1, 2, …., L).
For a given random sample of n individuals, the likelihood function for θ is calculated using the number of individuals in state j at t-1 and k at t by the distribution of individuals among states at t0;
| 14 |
When the time is homogeneous, yields the log likelihood
| 15 |
The data analysis utilized two prominent R packages, msm [40] and markovchain [41].
Results
The study showed that US was prevalent at a baseline level of 18.7%, with male children having a greater incidence of undernutrition (19.9%) than female children (17.3%). In rural areas, the prevalence was 11.6%, while in urban areas, it was greater (22.5%). The prevalence of US, UW, and USW was found to be greater for children with illiterate fathers (22.5%, 8.0%, and 9.6%, respectively), and mothers (22.3%, 7.0%, and 9.8%, respectively) than for those with literate families (Table 2).
Table 2.
Prevalence of child nutritional status at baseline (2002) across sociodemographic characteristics
| Variables | Category | N | U | S | W | US | UW | SW | USW | Total |
|---|---|---|---|---|---|---|---|---|---|---|
| n(%) | n(%) | n(%) | n(%) | n(%) | n(%) | n(%) | n(%) | n | ||
| Gender | Male | 433 (41.4) | 17 (1.6) | 195 (18.6) | 38 (3.6) | 208 (19.9) | 65 (6.2) | 0 (0) | 91 (8.7) | 1047 |
| Female | 489 (51.6) | 22 (2.3) | 134 (14.1) | 26 (2.7) | 164 (17.3) | 56 (5.9) | 0 (0) | 56 (5.9) | 947 | |
| Residence | Urban | 413 (59.2) | 12 (1.7) | 128 (18.3) | 23 (3.3) | 81 (11.6) | 17 (2.4) | 0 (0) | 24 (3.4) | 698 |
| Rural | 509 (39.3) | 27 (2.1) | 201 (15.5) | 41 (3.2) | 291 (22.5) | 104 (8) | 0 (0) | 123 (9.5) | 1296 | |
| Father’s Edu | Illiterate | 407 (38.9) | 21 (2) | 166 (15.9) | 33 (3.2) | 235 (22.5) | 84 (8) | 0 (0) | 100 (9.6) | 1045 |
| Literate | 516 (54.4) | 18 (1.9) | 163 (17.2) | 31 (3.3) | 137 (14.4) | 37 (3.9) | 0 (0) | 47 (5) | 949 | |
| Mother’s Edu | Illiterate | 474 (39.8) | 22 (1.8) | 193 (16.2) | 36 (3) | 266 (22.3) | 84 (7) | 0 (0) | 117 (9.8) | 1192 |
| Literate | 448 (55.9) | 17 (2.1) | 136 (17) | 28 (3.5) | 106 (13.2) | 37 (4.6) | 0 (0) | 30 (3.7) | 802 | |
| Access to Safe Drink Water | No | 364 (39.4) | 23 (2.5) | 139 (15) | 28 (3) | 215 (23.2) | 77 (8.3) | 0 (0) | 79 (8.5) | 925 |
| Yes | 558 (52.2) | 16 (1.5) | 190 (17.8) | 36 (3.4) | 157 (14.7) | 44 (4.1) | 0 (0) | 68 (6.4) | 1069 | |
| Access to Toilet | No | 466 (37.6) | 28 (2.3) | 207 (16.7) | 35 (2.8) | 291 (23.5) | 96 (7.7) | 0 (0) | 116 (9.4) | 1239 |
| Yes | 456 (60.4) | 11 (1.5) | 122 (16.2) | 29 (3.8) | 81 (10.7) | 25 (3.3) | 0 (0) | 31 (4.1) | 755 | |
| Access to Electricity | No | 498 (38.7) | 27 (2.1) | 205 (15.9) | 42 (3.3) | 294 (22.8) | 100 (7.8) | 0 (0) | 121 (9.4) | 1287 |
| Yes | 424 (60) | 12 (1.7) | 124 (17.5) | 22 (3.1) | 78 (11) | 21 (3) | 0 (0) | 26 (3.7) | 707 | |
| Access to Cooking Fuel | No | 815 (44.7) | 34 (1.9) | 290 (15.9) | 60 (3.3) | 358 (19.6) | 120 (6.6) | 0 (0) | 145 (8) | 1822 |
| Yes | 107 (62.2) | 5 (2.9) | 39 (22.7) | 4 (2.3) | 14 (8.1) | 1 (0.6) | 0 (0) | 2 (1.2) | 172 | |
| Overall | 922 (46.2) | 39(1.96) | 329(16.5) | 64(3.2.) | 372(18.7) | 121(6.1) | 0(0) | 147(7.4) | 1994 | |
Similarly, in Table 2: children with unsafe drinking water in their household experienced higher levels of US (23.2%) than did those with safe water at baseline (14.7%). Likewise, children without toilet access in households at baseline were more affected by US (23.5%), UW (7.7%) and USW (9.4%) than were those with toilet access (10.7%, 3.3% and 4.1%, respectively). In addition, children in households without electricity access were more affected by the US (22.8%), the UW (7.8%) and the USW (9.4%) than were those with electricity access (11%, 3%, and 3.7%, respectively). Finally, children in households with cooking fuel access at baseline had higher rates of experiencing US (19.6%), UW (6.6%), and USW (8%) than did those without cooking fuel (8.1%, 0.6%, and 1.2%, respectively). The zero values in the SW column indicate that there were no children concurrently affected by stunting and wasting at baseline.
The study revealed changes in the prevalence of various nutritional states over the years. The study revealed that the prevalence of normal nutritional status increased from 922 in 2002 to 1110 in 2006 and 1019 in 2009 but decreased to 741 in 2013 and 906 in 2016. The lowest incidence of underweight was 39 at baseline, followed by 46 in 2016, 67 in 2006, 84 in 2013, and 123 in 2009. The highest incidence of UW was 383 in 2013, and the lowest was 78 in 2006. The prevalence of both stunted and wasted children was extremely low. Similarly, the prevalence of both stunted and wasted children was extremely low. Finally, the prevalence of children who were USW increased from 147 thousand in 2002 to 260 thousand in 2016 (Table 3).
Table 3.
Prevalence of child nutritional status at each time-point
| Variables | 2002 Year | 2006 Year | 2009 Year | 2013 Year | 2016 Year | |||||
|---|---|---|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | n | % | n | % | |
| Undernutrition State | ||||||||||
| N | 922 | 46.2 | 1110 | 58.1 | 1019 | 54.1 | 741 | 39.6 | 906 | 49.9 |
| U | 39 | 2 | 67 | 3.5 | 123 | 6.5 | 84 | 4.5 | 46 | 2.5 |
| S | 329 | 16.5 | 289 | 15.1 | 77 | 4.1 | 30 | 1.6 | 18 | 1 |
| W | 64 | 3.2 | 57 | 3 | 129 | 6.8 | 123 | 6.6 | 133 | 7.3 |
| US | 372 | 18.7 | 282 | 14.7 | 256 | 13.6 | 246 | 13.1 | 185 | 10.2 |
| UW | 121 | 6.1 | 78 | 4.1 | 207 | 11 | 383 | 20.5 | 265 | 14.6 |
| SW | 0 | 0 | 0 | 0 | 1 | 0.1 | 4 | 0.2 | 2 | 0.1 |
| USW | 147 | 7.4 | 29 | 1.5 | 73 | 3.9 | 261 | 13.9 | 260 | 14.3 |
Table 4 revealed that almost half 2269(48.3%) of male children were normal, 177(49.3%) were underweight, 443 (59.6%) were stunted, 255(50.4%) were wasted, 752(56.1%) were US, 597 (56.6%) were UW, 3(42.9%) were SW, and 502(65.2%) were USW while 182(50.7%) of females were underweight, 300(40.4%) stunted, 251(49.6%) wasted, 589(43.9%) US, 457(43.4%) UW, 4(57.1%) SW, and 268(34.8%) were USW. The majority of children in the normal, underweight and stunted states were from the SNNP region (25.4%, 28.7%, and 23.3%, respectively), while the majority wasted children were from the Amhara region (115; 22.7%). Similarly, the majority of children affected by US were diagnosed with SNNP 361 (26.9%). However, the majority of the children affected by UW, SW, or USW were from the Amhara region (286; 27.1%), (4; 57.1%), and (237; 30.8%), respectively.
Table 4.
Distribution of sociodemographic and biosocial characteristics of children by nutrition states in Ethiopia
| Variables | Category | N | U | S | W | US | UW | SW | USW |
|---|---|---|---|---|---|---|---|---|---|
| n(%) | n(%) | n(%) | n(%) | n(%) | n(%) | n(%) | n(%) | ||
| Gender | Male | 2269 (48.3) | 177 (49.3) | 443 (59.6) | 255 (50.4) | 752 (56.1) | 597 (56.6) | 3 (42.9) | 502 (65.2) |
| Female | 2429 (51.7) | 182 (50.7) | 300 (40.4) | 251 (49.6) | 589 (43.9) | 457 (43.4) | 4 (57.1) | 268 (34.8) | |
| Region | Tigray | 884 (18.8) | 77 (21.4) | 135 (18.2) | 108 (21.3) | 275 (20.5) | 265 (25.1) | 2 (28.6) | 174 (22.6) |
| Amhara | 713 (15.2) | 82 (22.8) | 155 (20.9) | 115 (22.7) | 292 (21.8) | 286 (27.1) | 4 (57.1) | 237 (30.8) | |
| Oromiya | 1021 (21.7) | 62 (17.3) | 168 (22.6) | 77 (15.2) | 315 (23.5) | 157 (14.9) | 0 (0.0) | 139 (18.1) | |
| SNNP | 1191 (25.4) | 103 (28.7) | 173 (23.3) | 101 (20.0) | 361 (26.9) | 245 (23.2) | 1 (14.3) | 197 (25.6) | |
| Addis Ababa CA | 889 (18.9) | 35 (9.7) | 112 (15.1) | 105 (20.8) | 98 (7.3) | 101 (9.6) | 0 (0.0) | 23 (3.0) | |
| Residence | Urban | 2041 (43.4) | 93 (25.9) | 274 (36.9) | 234 (46.2) | 308 (23.0) | 282 (26.8) | 2 (28.6) | 144 (18.7) |
| Rural | 2657 (56.6) | 266 (74.1) | 469 (63.1) | 272 (53.8) | 1033 (77) | 772 (73.2) | 5 (71.4) | 626 (81.3) | |
| Mother's level of education | Illiterate | 1884 (40.1) | 176 (49.0) | 407 (54.8) | 202 (39.9) | 782 (58.3) | 538 (51.0) | 3 (42.9) | 435 (56.5) |
| Literate | 2814 (59.9) | 183 (51.0) | 336 (45.2) | 304 (60.1) | 559 (41.7) | 516 (49.0) | 4 (57.1) | 335 (43.5) | |
| Father's level of education | Illiterate | 1328 (28.3) | 128 (35.7) | 316 (42.5) | 149 (29.4) | 579 (43.2) | 349 (33.1) | 1 (14.3) | 256 (33.2) |
| Literate | 3370 (71.7) | 231 (64.3) | 427 (57.5) | 357 (70.6) | 762 (56.8) | 705 (66.9) | 6 (85.7) | 514 (66.8 | |
| Access to safe drinking water | Yes | 1627 (34.6) | 165 (46.0) | 285 (38.4) | 173 (34.2) | 659 (49.1) | 506 (48.0) | 4 (57.1) | 380 (49.4) |
| No | 3071 (65.4) | 194 (54.0) | 458 (61.6) | 333 (65.8) | 682 (50.9) | 548 (52.0) | 3 (42.9) | 390 (50.6) | |
| Access to sanitation | Yes | 1490 (31.7) | 133 (37.0) | 388 (52.2) | 142 (28.1) | 663 (49.4) | 358 (34.0) | 3 (42.9) | 305 (39.6) |
| No | 3208 (68.3) | 226 (63.0) | 355 (47.8) | 364 (71.9) | 678 (50.6) | 696 (66.0) | 4 (57.1) | 465 (60.4) | |
| Access to electricity | Yes | 1949 (41.5) | 221 (61.6) | 429 (57.7) | 199 (39.3) | 888 (66.2) | 605 (57.4) | 4 (57.1) | 491 (63.8) |
| No | 2749 (58.5) | 138 (38.4) | 314 (42.3) | 307 (60.7) | 453 (33.8) | 449 (42.6) | 3 (42.9) | 279 (36.2) | |
| Access to cooking fuels | Yes | 4082 (86.9) | 336 (93.6) | 672 (90.4) | 439 (86.8) | 1271 (94.8) | 998 (94.7) | 7 (100.0) | 741 (96.2) |
| No | 616 (13.1) | 23 (6.4) | 71 (9.6) | 67 (13.2) | 70 (5.2) | 56 (5.3) | 0 (0.0) | 29 (3.8) | |
| Total | 4698 | 359 | 743 | 506 | 1341 | 1054 | 7 | 770 | |
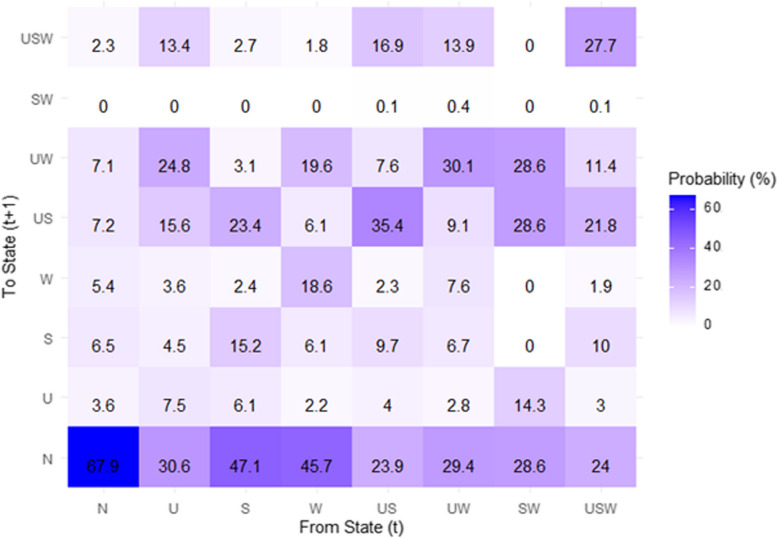
The study showed that the probability of children being in a normal state at time t + 1 was 0.68. The probability of transitioning from underweight to normal was 0.31, while the probability of transitioning from underweight to a UW state was 0.25. Similarly, the probability of recovering from stunting to normal was 0.47, and a higher transition of 0.23 was to the SW state. Finally, children in a wasting state at time t had a probability of 0.46 of recovering to the normal state and had a higher probability of transitioning to UW (0.20) (Fig. 3).
Fig. 3.
State transition probability (%) matrix. NB: the diagonal elements representing the probability of remaining in a state and off-diagonal elements showing transition probabilities between states
Children who were facing US simultaneously had a 0.24 chance of recovering to normal, with a higher probability of 0.35 remaining in the same state at time t + 1. Similarly, children in the UW state at time t had a 0.29 chance of recovering and 0.30 chance of remaining in the same state at time t + 1. Likewise, children who were affected by SW had a probability of 0.29 moving to a normal state, with a greater likelihood of 0.29 moving to both the UW and the US. Finally, children in all USW states concurrently had a 0.24 chance of recovering, with a decreased transition to SW. Generally, the transitions from any state to concurrent stunting and wasting states were relatively fewer (near zero) (Fig. 3).
Finally, the probability of children being in a state varied, with normal children having the highest probability (0.68), followed by US (0.35), UW (0.30), USW (0.28), wasting (0.19), stunting (0.15), and underweight children (0.08) (Fig. 3).
Figure 3 includes the normal state, providing a comprehensive view of nutritional states among the children in the study. Understanding its transition probabilities is crucial for assessing nutritional outcomes and serves as a baseline for comparing transitions into and out of states like underweight, stunting, wasting, and their combinations (US, UW, SW, and USW).
There was a greater incidence of US in male children (16%) than in female children (14.6%). In rural areas, the cumulative incidence of UWs was 10.3%, while in urban areas, it was lower (6.5%). Children in households without safe drinking water experienced greater incidences of US, UW, SW and USW (15.7%, 9.2%, 0.1% and 6.7%, respectively) than did those with safe drinking water. Similarly, children without access to toilets in households face greater incidents of stunting, US and USW (13.7%, 20.7%, and 7.4%, respectively) than do those who have access to toilets. Similarly, children in households without access to electricity experienced higher incidences of underweight, stunting, US, UW, and USW (4.2%, 11.7%, 20%, 10% and 8.2%, respectively) than did the other children. Finally, children in families without cooking fuel access were more likely to be underweight or stunted and to have experienced incidents of US and UW (3.7%, 10.7%, 16.1%, and 9.4%, respectively) than were those with access to cooking fuel (Table 5).
Table 5.
Cumulative incidence of child undernutrition at the end of the survey in 2016
| Variables | Category | N | U | S | W | US | UW | SW | USW | Total |
|---|---|---|---|---|---|---|---|---|---|---|
| n(%) | n(%) | n(%) | n(%) | n(%) | n(%) | n(%) | n(%) | |||
| Gender | Male | 7140 (47.0) | 516 (3.4) | 1853 (12.2) | 684 (4.5) | 2431 (16.0) | 1443 (9.5) | 0 (0) | 1124 (7.4) | 15191 |
| Female | 6813 (53.9) | 493 (3.9) | 1176 (9.3) | 581 (4.6) | 1846 (14.6) | 1049 (8.3) | 0 (0) | 670 (5.3) | 13641 | |
| Residence | Urban | 6219 (61.0) | 275 (2.7) | 1132 (11.1) | 581 (5.7) | 989 (9.7) | 663 (6.5) | 0 (0) | 347 (3.4) | 10195 |
| Rural | 8275 (44.4) | 764 (4.1) | 1976 (10.6) | 727 (3.9) | 3448 (18.5) | 1920 (10.3) | 0 (0) | 1510 (8.1) | 18637 | |
| Mother’s Edu | Illiterate | 6293 (43.3) | 552 (3.8) | 1715 (11.8) | 567 (3.9) | 2791 (19.2) | 1410 (9.7) | 0 (0) | 1177 (8.1) | 14534 |
| Literate | 8207 (57.4) | 500 (3.5) | 1358 (9.5) | 743 (5.2) | 1644 (11.5) | 1158 (8.1) | 0 (0) | 672 (4.7) | 14298 | |
| Father’s Edu | Illiterate | 4785 (43.0) | 423 (3.8) | 1380 (12.4) | 456 (4.1) | 2215 (19.9) | 1046 (9.4) | 0 (0) | 824 (7.4) | 11129 |
| Literate | 9719 (54.9) | 620 (3.5) | 1735 (9.8) | 850 (4.8) | 2213 (12.5) | 1522 (8.6) | 18 (0.1) | 1027 (5.8) | 17703 | |
| Access to Safe Drink Water | No | 4472 (36.8) | 413 (3.4) | 1021 (8.4) | 413 (3.4) | 1908 (15.7) | 1118 (9.2) | 12 (0.1) | 814 (6.7) | 12153 |
| Yes | 10,675 (64.0) | 634 (3.8) | 2202 (13.2) | 951 (5.7) | 2502 (15.0) | 1451 (8.7) | 0 (0) | 1034 (6.2) | 16679 | |
| Access to Toilet | No | 5308 (42.5) | 450 (3.6) | 1711 (13.7) | 425 (3.4) | 2585 (20.7) | 1087 (8.7) | 0 (0) | 924 (7.4) | 12490 |
| Yes | 9184 (56.2) | 588 (3.6) | 1405 (8.6) | 882 (5.4) | 1847 (11.3) | 1487 (9.1) | 0 (0) | 931 (5.7) | 16342 | |
| Access to Electricity | No | 6720 (42.1) | 670 (4.2) | 1868 (11.7) | 591 (3.7) | 3193 (20.0) | 1596 (10.0) | 0 (0) | 1309 (8.2) | 15963 |
| Yes | 7773 (60.4) | 373 (2.9) | 1248 (9.7) | 721 (5.6) | 1235 (9.6) | 965 (7.5) | 0 (0) | 540 (4.2) | 12869 | |
| Access to Cooking Fuel | No | 12,812 (48.7) | 973 (3.7) | 2815 (10.7) | 1184 (4.5) | 4236 (16.1) | 2473 (9.4) | 0 (0) | 1815 (6.9) | 26308 |
| Yes | 1689 (60.3) | 64 (2.3) | 289 (10.3) | 140 (5.0) | 193 (6.9) | 101 (3.6) | 0 (0) | 325 (11.6) | 2801 | |
| Overall | 14,495(34.9) | 14,495(34.9) | 1046(2.5) | 3110(7.5) | 1314(3.2) | 4433(10.7) | 2569(6.2) | 13(0.0) | 41475 | |
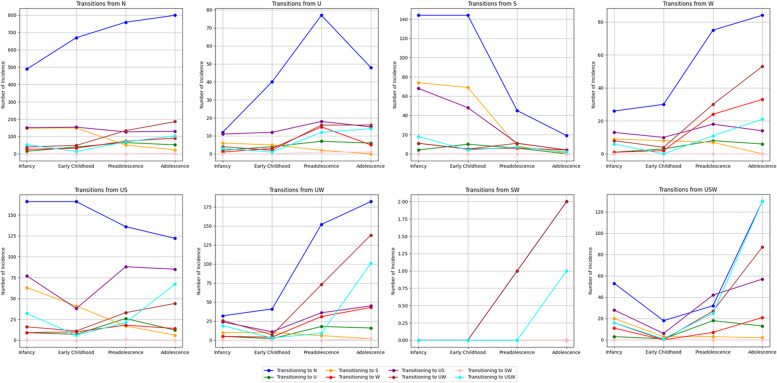
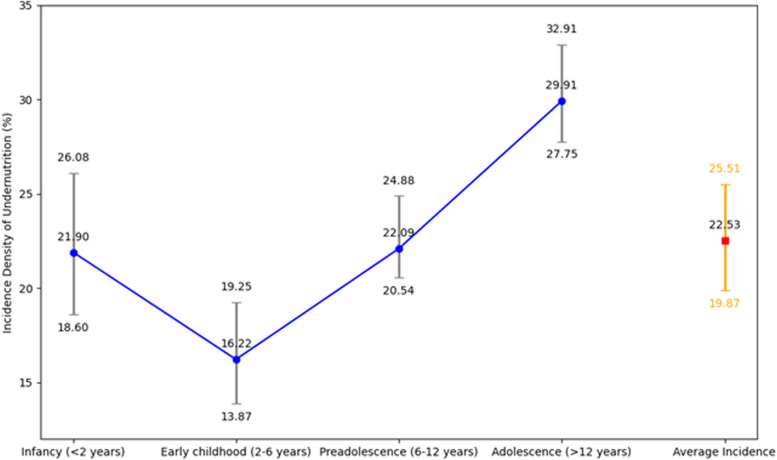
The incidence trends of transitions between the eight distinct nutritional statuses of children across their developmental stages are displayed in Fig. 4. This figure tracks how children move from one nutritional status to another at each stage of development, with incidence rates reported per 100 children. The study finds varying rates of undernutrition prevalence, with the highest incidence observed in adolescence (29.91 per 100 children) and the lowest in early childhood (16.22 per 100 children). For instance, in infancy (< 2 years), the incidence rate is 21.90 per 100 children, while in early childhood (2–6 years) it decreases to 16.22 per 100 children. Conversely, preadolescence (6–12 years) shows an increase to 22.09 per 100 children, and adolescence (> 12 years) exhibits the highest incidence at 29.91 per 100 children (Fig. 5). These figures provide a comprehensive overview of undernutrition incidence across different developmental stages, highlighting notable variations in vulnerability among children (Figs. 4 and 5).
Fig. 4.
Incidence trends of transitions in child nutritional status across their developmental stages in Ethiopia
Fig. 5.
Trend of incidence density of undernutrition by child developmental stages with 95% confidence intervals in Ethiopia
Accordingly, the study revealed that a child initially in a USW takes approximately a median of 13.90 months to make the first transition to the normal state, 24 months or two years to underweight, and 21.50 months to stunt. The transition period for a child initially in US, UW, and USW to experience SW for the first time is relatively lengthy. According to Table 6, initially, individuals spent a median of 24 months or two years transitioning from a healthy state to underweight, followed by 22 months to stunted, 17.9 months to USW, 17.5 months to wasted, 13.75 months to US, and 9.5 months to UW. The zero values (not exactly zero but near to zero) in the SW column indicate that the median time to transition from another nutritional state to SW is extremely short or negligible. Lastly, underweight children had a median recurrence period of 23.4 months, followed by 19.8 months for stunted, 14.5 months for wasted, 8 months for US, 6.5 months for UW, and 9.8 months for USW states (Table 6).
Table 6.
Median first passage time and median first recurrence time of child undernutrition in Ethiopia
| To time (t + 1) | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| Median First Passage Time and Median First Recurrence Time (95% CI) (in months) | |||||||||
| N | U | S | W | US | UW | SW | USW | ||
| From time (t) | N | 11.5 (10.8, 12.2) | 24.0 (19.5, 28.5) | 22.0 (18.0, 26.0) | 17.5 (13.0, 22.0) | 13.8 (11.5, 15.0) | 9.5 (7.5, 11.5) | 0 | 17.9 (15.8, 20.0) |
| U | 12.8 (12.0, 13.5) | 23.4 (18.0, 29.0) | 22.5 (19.0, 26.0) | 18.5 (14.0, 23.0) | 11.5 (9.5, 13.0) | 7.5 (5.5, 9.5) | 0 | 14.1 (11.5, 16.5) | |
| S | 12.5 (11.8, 13.2) | 23.9 (19.0, 28.5) | 19.8 (15.0, 24.0) | 18.8 (15.0, 22.0) | 10.6 (8.0, 12.0) | 10.0 (8.0, 12.0) | 0 | 16.5 (14.0, 19.0) | |
| W | 12.6 (11.9, 13.3) | 24.5 (20.0, 29.0) | 23.5 (19.0, 28.0) | 14.5 (10.0, 18.0) | 13.5 (11.0, 16.0) | 7.5 (5.5, 9.5) | 0 | 17.0 (14.0, 20.0) | |
| US | 13.2 (12.0, 14.0) | 24.4 (19.0, 29.5) | 20.5 (16.0, 25.0) | 19.5 (16.0, 23.0) | 8.0 (6.0, 10.0) | 9.4 (7.0, 11.0) | 41 (39, 43) | 12.8 (10.5, 15.0) | |
| UW | 13.0 (12.0, 14.0) | 24.8 (20.0, 29.5) | 22.6 (18.0, 27.0) | 17.0 (13.0, 21.0) | 12.6 (10.5, 14.0) | 6.5 (4.5, 8.5) | 43 (40, 46) | 13.5 (11.0, 16.0) | |
| SW | 13.6 (12.5, 14.5) | 20.5 (16.0, 25.0) | 23.5 (20.0, 27.0) | 19.0 (15.0, 23.0) | 10.7 (8.0, 12.5) | 6.0 (4.0, 8.0) | 0 | 15.5 (13.0, 18.0) | |
| USW | 13.9 (13.0, 14.8) | 24.0 (19.0, 29.0) | 21.5 (17.0, 25.0) | 19.2 (15.0, 23.0) | 9.5 (7.0, 11.0) | 8.8 (6.5, 10.5) | 34 (31, 37) | 9.8 (7.0, 12.0) | |
NB: The diagonal entries in the above table represent MFRT, indicating the median time taken for children to return to a specific state after initially transitioning away from it. The off-diagonal entries denote MFPT, showing the median time for children to transition from one nutritional state to another for the first time during the study period
Furthermore, the study showed that underweight children had a shorter lifetime undernourished period (LUP) of approximately 15.3 months, while those with stunting had a LUP of nearly 23 months. Those with wasting had a median LUP of 30.4 months. The combined category of underweight and stunted children (US) had a higher LUP of approximately 48.8 months, while those with USW had a median LUP of approximately 45.4 months. However, a child experiencing SW had a LUP of nearly five months, implying a shorter duration of undernutrition in this state (Table 7).
Table 7.
Median and IQR of the Lifetime Undernourished Period (LUP) of a children in Ethiopia
| States | Median LUP (months) | Inter Quartile Range (IQR) of LUP |
|---|---|---|
| N | 83.6 | 10.5 |
| U | 15.3 | 5.0 |
| S | 23.0 | 7.5 |
| W | 30.4 | 6.0 |
| US | 48.8 | 8.0 |
| UW | 45.4 | 4.5 |
| SW | 5.2 | 2.0 |
| USW | 48.1 | 9.0 |
Additionally, in Table 8: males had a median LUP of approximately 89.7 months, while females had a lower median LUP of approximately 75.4 months. Regionally, children living in the Amhara region had the highest median LUP, nearly 94.5 months; followed by those living in the Tigray region, 87.2 months; and those living in the SNNP region, 82.3 months. In the Oromia region, the median LUP was approximately 78.1 months. Finally, the Addis Ababa City Administration had the lowest median LUP among the regions, occurring at 55.7 months. Similarly, rural children had the highest median LUP of approximately 89.3 months. Children from illiterate mothers had a greater LUP 68.5 months than did those from literate mothers. Children from households without access to safe water, electricity, or cooking fuel had higher LUPs (52.1 months, 67.5 months, and 70.8 months, respectively (see Table 8).
Table 8.
Median and IQR of the Lifetime Undernourished Period (LUP) in Ethiopia
| Variables | Category | Median LUP (months) | IQR of LUP (months) |
|---|---|---|---|
| Gender | Male | 89.7 | 12.5 |
| Female | 75.4 | 10.4 | |
| Region | Tigray | 87.2 | 15.8 |
| Amhara | 94.5 | 8.7 | |
| Oromiya | 78.1 | 6.5 | |
| SNNP | 82.3 | 9.3 | |
| Addis Ababa CA | 55.7 | 5.5 | |
| Residence | Urban | 60.4 | 7.6 |
| Rural | 89.3 | 11.3 | |
| Father's level of education | Illiterate | 52.3 | 9.5 |
| Literate | 56.9 | 7.1 | |
| Mother's level of education | Illiterate | 68.5 | 6.4 |
| Literate | 57.3 | 5.5 | |
| Access to safe drinking water | Yes | 48.3 | 6.3 |
| No | 52.1 | 5.7 | |
| Access to toilet | Yes | 45.2 | 4.8 |
| No | 43.8 | 3.5 | |
| Access to electricity | Yes | 40.7 | 8.4 |
| No | 67.5 | 10.2 | |
| Access to cooking fuels | Yes | 25.1 | 5.5 |
| No | 70.8 | 12.1 |
The Markov regression analysis revealed that a previous state of undernutrition was the main risk factor for current undernutrition. Other risk factors include rural residence, child's health compared to peers, education of mother and father, access to safe drink water, and cooking fuel. Children from rural areas were 70% (95% CI: 1.40, 2.06) more likely to be undernourished than were those from urban residences. Compared to their peers, children with worse health conditions were 80% (95% CI: 1.40, 2.30) more likely to be undernourished. Children with illiterate fathers (OR = 1.85: 1.45, 2.42) and mothers (OR = 1.40; 95% CI: 1.24, 1.56) had greater odds of wasting than did those with literate mothers. Children who did not drink safe water had greater odds (OR = 1.60; 95% CI = 1.21, 2.04) of experiencing undernutrition. Children with access to cooking fuel were 50% more likely to be undernourished, irrespective of previous undernutrition, than were those without access to cooking fuel (OR = 1.50; 95% CI: 1.40, 1.61). These findings highlight the importance of addressing undernutrition in children's lives (Table 9).
Table 9.
Factors influencing childhood undernutrition risk in Ethiopia
| Variables | Category | OR | Robust SE | 95% CI | P value | |
|---|---|---|---|---|---|---|
| LCL | UCL | |||||
| Residence | Urbana | |||||
| Rural | 1.70 | 0.110 | 1.395 | 2.059 | 0.010 | |
| Previous state of Undernutrition | 92.00 | 0.280 | 50.500 | 160.00 | < 0.001 | |
| Residence*Previous State | 1.85 | 0.107 | 1.480 | 2.360 | 0.015 | |
| Child's health compared to peers | Samea | 1.00 | ||||
| Better | 1.55 | 0.450 | 0.620 | 3.940 | 0.950 | |
| Worse | 1.80 | 0.135 | 1.400 | 2.300 | 0.003 | |
| Previous state of Undernutrition | 102.00 | 0.290 | 57.04 | 182.41 | < 0.001 | |
| Child’s health*Previous State | 1.15 | 0.075 | 1.010 | 1.320 | 0.750 | |
| Father's level of education | Illiterate | 1.85 | 0.130 | 1.450 | 2.420 | 0.004 |
| Literatea | 1.00 | |||||
| Previous state of Undernutrition | 90.00 | 0.055 | 80.201 | 100.04 | < 0.001 | |
| level of education *Previous State | 1.70 | 0.250 | 1.030 | 2.830 | 0.040 | |
| Mother's level of education | Illiterate | 1.40 | 0.055 | 1.240 | 1.560 | 0.010 |
| Literatea | 1.00 | |||||
| Previous state of Undernutrition | 85.00 | 0.295 | 45.04 | 150.81 | < 0.001 | |
| level of education *Previous State | 1.25 | 0.030 | 1.170 | 1.340 | 0.030 | |
| Access to safe drinking water | Yesa | |||||
| No | 1.60 | 0.140 | 1.210 | 2.040 | 0.015 | |
| Previous state of Undernutrition | 95.00 | 0.120 | 75.50 | 115.04 | < 0.001 | |
| Safe drink water *Previous State | ||||||
| Access to cooking fuel | Yes | 1.50 | 0.002 | 1.400 | 1.610 | 0.020 |
| Noa | ||||||
| Previous state of Undernutrition | 105.00 | 0.310 | 58.15 | 190.74 | < 0.001 | |
| Cooking fuel *Previous State | ||||||
aDenotes the reference category
*The asterisks represent interaction effects rather than statistical significance
The Markov regression analysis using transition intensity revealed that children in rural areas with undernutrition had a 1.75 (95% CI: 1.53, 1.67) greater risk of being undernourished and a 0.63% (95% CI: 1.57, 1.69) slower recovery from undernutrition to normal status than did those in urban areas. This finding suggested that the probability of a child recovering from undernutrition to normal was less than the probability of progression. Children with illiterate fathers (HR = 1.50; 95% CI: 1.38, 1.62) and mothers (HR = 1.45; 95% CI: 1.02, 3.29) transitioned faster from normal to undernutrition, while those with illiterate mothers 1.81 (95% CI: 1.01, 3.24) recovered to normal. Additionally, children in households without safe drinking water (HR = 1.70; 95% CI: 1.26, 2.14) were more likely to transition from normal to undernutrition than were those with access to safe water. Children with access to cooking fuel also had a faster (HR = 1.95; 95% CI: 1.75, 2.17) transition from normal to undernutrition, while those with fuel-based families had a slower recovery rate. These findings highlight the importance of accessing safe drinking water and cooking fuel for children's health (Table 10). However, due to the complexity and volume of transition intensity data across multiple states (U, S, W, US, UW, SW, and USW), these categories were combined into a single Undernourished category in Table 10 for clarity and simplicity of presentation.
Table 10.
Transition intensity analysis of childhood undernutrition risk factors in Ethiopia
| Variables | Category | From time (t) | To time (t + 1) | |||
|---|---|---|---|---|---|---|
| Normal | Undernourished | |||||
| Hazard Ratio | 95% CI | Hazard Ratio | 95% CI | |||
| Sex of child | Male | Normal | 1.75 | 1.53, 1.67 | ||
| Undernutrition | 1.63 | 1.57, 1.69 | ||||
| Femalea | Normal | 1.00 | ||||
| Undernutrition | 1.00 | |||||
| Residence | Urban | Normal | 1.42 | 1.40, 1.44 | ||
| Undernutrition | 0.42 | 0.40, 0.44 | ||||
| Rurala | Normal | 1.00 | ||||
| Undernutrition | 1.00 | |||||
| Father's level of education | Illiterate | Normal | 1.50 | 1.38, 1.62 | ||
| Undernutrition | 1.34 | 0.59, 2.91 | ||||
| Literatea | Normal | 1.00 | ||||
| Undernutrition | 1.00 | |||||
| Mother's level of education | Illiterate | Normal | 1.45 | 1.02, 3.29 | ||
| Undernutrition | 1.81 | 1.01, 3.24 | ||||
| Literatea | Normal | 1.00 | ||||
| Undernutrition | 1.00 | |||||
| Access to safe drinking water | Yesa | Normal | 1.00 | |||
| Undernutrition | 1.00 | |||||
| No | Normal | 1.70 | 1.26, 2.14 | |||
| Undernutrition | 0.35 | 0.33, 0.37 | ||||
| Access to cooking fuel | Yes | Normal | 1.95 | 1.75, 2.17 | ||
| Undernutrition | 0.64 | 0.50, 0.84 | ||||
| Noa | Normal | 1.00 | ||||
| Undernutrition | 1.00 | |||||
aDenotes the reference category
Discussion
One study showed that the prevalence of stunting and underweight was greater than 20% [42]. The present study reported that the incidences of stunting and US were above 16.5% and 18.7%, respectively, which were similar to the findings of previous studies. Furthermore, the study revealed that male children have a longer median lifetime undernourished period (89.7 months) than female children (75.4 months). The present study showed that male children had a greater risk of undernutrition than female children did.
This finding was similar to the finding from the NHFS-3 data [43]. A case‒control study from Bangladesh found no significant difference in all undernutrition states (underweight, stunting, or wasting) among male and female children [44]. The present study revealed that urban children have better health status and immunization rates, while rural children have a greater risk of undernutrition. This finding is supported by a Ugandan study that revealed that residence significantly impacts nutritional health [45].
The Markov chain principle states that the current state is dependent on the previous state, allowing for the calculation of the first median transition time. This time is used to estimate the median duration for underweight, stunted or wasted children to reach normalcy and to identify the factors affecting this time. This type of time has not been reported in longitudinal studies. The present study reported the probability of transition from one state at the previous time to the current state of undernutrition, providing valuable insights for appropriate intervention. This information is crucial for understanding the progression of undernourished children and their needs.
In many studies involving multistate Markov chain modeling with follow-up times, mean and standard deviation (SD) are commonly reported as summary statistics [31, 46, 47]. However, since follow-up times are typically skewed, the use of mean and SD may not accurately represent the data's distribution. In this study, we opted for the median and IQR as more appropriate summary statistics, as they provide a clearer picture of central tendency and variability while reducing the impact of outliers. This approach offers a more accurate representation of follow-up durations in skewed data.
The study showed that children in the USW state required an average of 14.63 months to transition to normal health, those in the stunting state took an average of 13.05 months, and those in the underweight state took an average of 13.89 months. However, a study by [37] revealed that it takes an average of 2.73 years (about 33 months) to transition from a wasting state to normal undernutrition and 1.97 years (about 24 months) to transition from stunting to normal undernutrition.
This study examined the risk factors for undernutrition on the Markovian property. The authors found that area of residence where the children lived in rural areas, having worse health conditions than their peers, illiterate parents, lack of safe drinking water, and access to cooking fuels were significant factors associated with wasting, regardless of previous undernutrition. The interaction effect of these covariates with the previous state was also statistically significant. This study highlights the importance of addressing these factors to improve nutritional outcomes.
The study revealed that children in rural areas with undernutrition face a greater risk of undernutrition and slower recovery from undernutrition than urban children. Likewise, children with illiterate fathers and mothers experienced faster transitions from normal to undernutrition. In addition, these findings also indicate that children living in households without safe drinking water but with access to cooking fuels are at a greater risk of transitioning from a normal to an undernutrition state rather than from undernutrition to a normal state.
Conclusions
In conclusion, our study highlights on critical factors influencing transition of child undernutrition in Ethiopia. Children facing USW take an average of 14.63 months to return to normal health, with male children taking a relatively longer time to become undernourished. Our findings underscore the increased risk among children in rural areas, those with illiterate parents, and those lacking access to safe drinking water and cooking fuel, who experience worse health conditions compared to their peers. Addressing these disparities is crucial for improving child health outcomes. Public health efforts should focus on targeted nutritional interventions, enhancing access to basic amenities, and promoting educational programs to empower families. These initiatives, supported by robust policy frameworks, are essential for reducing the duration of undernutrition and recurrence of child undernutrition and fostering healthier communities in Ethiopia.
Supplementary Information
Acknowledgements
The authors express their gratitude to the Young Lives Study teams for providing access to the data files.
Authors’ contributions
GBB: Contributed to the conceptualization, conducted the formal analysis, shaped the methodology, performed the data analysis, engaged in the writing of the report, and authored the original draft.TZ: Provided insights into conceptualization and guided methodology, reviewed and edited the manuscript, and contributed to the data analysis. HMF: Contributed to the methodology, played a key role in creating the original draft, and conducted the data analysis.
Funding
The authors have no support or funding to report.
Data availability
The dataset used in this study was obtained from the Young Lives Study. Access to the data can be obtained either by completing the form available at https://www.younglives.org.uk/use-our-data-form, selecting the dataset “Young Lives: Rounds 1-5 constructed files, 2002-2016” (used in this study), or by creating a user account through the https://ukdataservice.ac.uk/, subject to their terms and conditions. Additionally, the survey questionnaires for each round (Rounds 1-5) are available through the following link: https://www.younglives.org.uk/round-1-questionnaires. By adjusting the round number in the URL or navigating through the menu on the Young Lives website, users can access the questionnaires for each respective round.
Declarations
Ethics approval and consent to participate
Ethics approval for this study was not required since the data are secondary and available in the public domain.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Khan AA, Bano N, Salam A. Child malnutrition in South Asia: a comparative perspective. South Asian Survey. 2007;14(1):129–45. [Google Scholar]
- 2.UNICEF. Progress for children: a report card on nutrition. Unicef; 2006. https://data.unicef.org/resources/progress-for-children-a-report-card-on-nutrition/.
- 3.Meerman J, Carisma B, Thompson B. Global, regional and subregional trends in undernourishment and malnutrition. SOFA FOA. 2012;1:1–33. https://www.fao.org/fileadmin/user_upload/agn/pdf/SOFA_2013global.regional.subregional.trends.pdf.
- 4.Watkins K. The state of the world's children 2016: a fair chance for every child. 2016. ERIC.
- 5.Rudan I, et al. Epidemiology and etiology of childhood pneumonia. Bull World Health Organ. 2008;86:408-416B. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Agarwal M, Banerjee A. Prospects for achieving the sustainable development goals. In: ECONOMICS OF G20: A World Scientific Reference Vol 2: How Developing Countries can Achieve Sustainable Development Goals. Singapore: World Scientific; 2020. p. 65–99.
- 7.Black RE, et al. Maternal and child undernutrition and overweight in low-income and middle-income countries. Lancet. 2013;382(9890):427–51. [DOI] [PubMed] [Google Scholar]
- 8.Organization WH. UNICEF-WHO low birthweight estimates: levels and trends 2000–2015. Geneva: World Health Organization; 2019.
- 9.Victora CG, et al. Maternal and child undernutrition: consequences for adult health and human capital. Lancet. 2008;371(9609):340–57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Fenta SM, Fenta HM, Ayenew GM. The best statistical model to estimate predictors of under-five mortality in Ethiopia. J Big Data. 2020;7(1):1–14. [Google Scholar]
- 11.Woldeyohannes M, et al. Ethiopia national food and nutrition survey to inform the Ethiopian national food and nutrition strategy: a study protocol. BMJ Open. 2023;13(4):e067641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lassi ZS, et al. Systematic review of complementary feeding strategies amongst children less than two years of age. Karachi City, Pakistan: Division of Women and Child Health, The Aga Khan University; 2013. [Google Scholar]
- 13.WHO. WHO, Global strategy on diet, physical activity and health. In: fifty-seventh world health assembly. 2004. https://www.who.int/publications/i/item/9241592222. [DOI] [PubMed]
- 14.Berhe K, et al. Risk factors of stunting (chronic undernutrition) of children aged 6 to 24 months in Mekelle City, Tigray Region, North Ethiopia: an unmatched case-control study. PLoS ONE. 2019;14(6):e0217736. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Mengistu K, Alemu K, Destaw B. Prevalence of malnutrition and associated factors among children aged 6–59 months at Hidabu Abote District, North Shewa, Oromia Regional State. J nutr disorders ther. 2013;1(1):2161–509. [Google Scholar]
- 16.Wondimagegn ZT. Magnitude and determinants of stunting among children in Africa: a systematic review. Curr Res Nutr Food Sci J. 2014;2(2):88–93. [Google Scholar]
- 17.Tesfaw LM, Fenta HM. Multivariate logistic regression analysis on the association between anthropometric indicators of under-five children in Nigeria: NDHS 2018. BMC Pediatr. 2021;21(1):1–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Fenta HM, Zewotir T, Muluneh EK. Spatial data analysis of malnutrition among children under-five years in Ethiopia. BMC Med Res Methodol. 2021;21(1):1–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Takele K, Zewotir T, Ndanguza D. Understanding correlates of child stunting in Ethiopia using generalized linear mixed models. BMC Public Health. 2019;19(1):1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Zheng X, et al. Multistate Markov model application for blood pressure transition among the Chinese elderly population: a quantitative longitudinal study. BMJ Open. 2022;12(7): e059805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Matsena Zingoni Z, et al. Hiv disease progression among antiretroviral therapy patients in Zimbabwe: a multistate Markov model. Front Public Health. 2019;7:326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Belan S. Median and mode in first passage under restart. Phys Rev Res. 2020;2(1):013243. [Google Scholar]
- 23.Warr RL, Woodfield TB. Bayesian nonparametric estimation of first passage distributions in semi-Markov processes. Appl Stoch Model Bus Ind. 2020;36(2):237–50. [Google Scholar]
- 24.Eisler Z, et al. Diffusive behavior and the modeling of characteristic times in limit order executions. Quant Finance. 2009;9(5):547–63. [Google Scholar]
- 25.Schwarz W. Small steps at high speed: the diffusion limit. In: Random Walk and Diffusion Models: An Introduction for Life and Behavioral Scientists. Cham: Springer; 2022. p. 55–70.
- 26.Mermoud, G. Model-Based Real-Time Control. In: Stochastic Reactive Distributed Robotic Systems. Springer Tracts in Advanced Robotics, vol 93. Cham: Springer; 2014. 10.1007/978-3-319-02609-1_12.
- 27.Suit H, Wette R, Lindberg R. Analysis of tumor-recurrence times. Radiology. 1967;88(2):311–21. [DOI] [PubMed] [Google Scholar]
- 28.Huang R, et al. A retrospective analysis of the risk factors affecting recurrence time in patients with recurrent glioblastoma. Ann Palliat Med. 2021;10(5):5391399–5399. [DOI] [PubMed] [Google Scholar]
- 29.Guraya SY. Pattern, stage, and time of recurrent colorectal cancer after curative surgery. Clin Colorectal Cancer. 2019;18(2):e223–8. [DOI] [PubMed] [Google Scholar]
- 30.Owoeye SM, Oseni BM, Gayawan E. Estimating lifetime malnourished period and its statistics based on the concept of Markov chain with reward. Heliyon. 2020;6(5):e04073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Lives Y. A guide to Young Lives research. Lives Y, editor. Oxford; 2017. https://www.younglives.org.uk/sites/default/files/migrated/GuidetoYLResearch_0.pdf.
- 32.Fenta HM, Zewotir T, Muluneh EK. Disparities in childhood composite index of anthropometric failure prevalence and determinants across Ethiopian administrative zones. PLoS One. 2021;16(9):e0256726. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Khan S, Zaheer S, Safdar NF. Determinants of stunting, underweight and wasting among children< 5 years of age: evidence from 2012–2013 Pakistan demographic and health survey. BMC Public Health. 2019;19:1–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Gupta AK, Borkotoky K. Exploring the multidimensional nature of anthropometric indicators for under-five children in India. Indian J Public Health. 2016;60(1):68–72. [DOI] [PubMed] [Google Scholar]
- 35.Kassie GW, Workie DL. Exploring the association of anthropometric indicators for under-five children in Ethiopia. BMC Public Health. 2019;19:1–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Simegnew M. Modeling the Progression of Neonatal Hypothermia Disease Progression Using Data on New Borns at Dilla University Referral Hospital Application of Multi State Hidden Markov Model. 2022, HU.
- 37.Visalakshi J. Estimation of mean transition time using markov model and comparison of risk factors of malnutrition using Markov regression to generalized estimating equations and random effects model in a longitudinal study. The Tamilnadu Dr. Chennai: MGR Medical University; 2012. [Google Scholar]
- 38.Dong H, et al. Multi-state analysis of the impact of childhood starvation on the healthy life expectancy of the elderly in China. Front Public Health. 2021;9: 690645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Moreira C, et al. A multistate Model for analyzing transitions between body mass index categories during childhood: the Generation XXI Birth Cohort Study. Am J Epidemiol. 2019;188(2):305–13. [DOI] [PubMed] [Google Scholar]
- 40.Jackson C. Multi-state models for panel data: the msm package for R. J Stat Softw. 2011;38:1–28. [Google Scholar]
- 41.Spedicato G, Signorelli M. The markovchain Package: A Package for Easily Handling Discrete Markov Chains in R. 2014.
- 42.Kain J, et al. Trends in height and BMI of 6-year-old children during the nutrition transition in Chile. Obes Res. 2005;13(12):2178–86. [DOI] [PubMed] [Google Scholar]
- 43.International Institute for Population Sciences (IIPS) and ORC Macro, MEASURE/DHS+, National Family Health Survey (NFHS-2), 1998-99: India, vol. 1. International Institute for Population Sciences; 2000.
- 44.Nahar B, et al. Risk factors associated with severe underweight among young children reporting to a diarrhoea treatment facility in Bangladesh. J Health Popul Nutr. 2010;28(5):476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Kikafunda JK, et al. Risk factors for early childhood malnutrition in Uganda. Pediatrics. 1998;102(4):e45–e45. [DOI] [PubMed] [Google Scholar]
- 46.Wang W. Multi-state Markov models with fixed and random effects. UCL (University College London); 2022.
- 47.Abner EL. Multistate Markov chains and their application to the Biologically Resilient Adults in Neurological Studies cohort. University of Kentucky; 2013.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The dataset used in this study was obtained from the Young Lives Study. Access to the data can be obtained either by completing the form available at https://www.younglives.org.uk/use-our-data-form, selecting the dataset “Young Lives: Rounds 1-5 constructed files, 2002-2016” (used in this study), or by creating a user account through the https://ukdataservice.ac.uk/, subject to their terms and conditions. Additionally, the survey questionnaires for each round (Rounds 1-5) are available through the following link: https://www.younglives.org.uk/round-1-questionnaires. By adjusting the round number in the URL or navigating through the menu on the Young Lives website, users can access the questionnaires for each respective round.