Abstract
Varicella-zoster virus (VZV) can lead to rare complications such as cutaneous vasculitis. We present a unique case of post-zoster cutaneous vasculitis in an 82-year-old male, occurring alongside acute calcium pyrophosphate deposition disease (CPPD), a previously undocumented association. The patient initially presented with a painful zoster rash and hand swelling, treated with oral acyclovir. Persistent swelling led to a diagnosis of CPPD in the wrist, managed with prednisone and colchicine. A biopsy of purplish discoloration at the zoster site confirmed vasculitis, which resolved after treatment. This case underscores the importance of recognizing post-zoster vasculitis, even in immunocompetent individuals, and suggests a potential link with CPPD that warrants further investigation.
Keywords: acute calcium pyrophosphate deposition disease, infection, vasculitis, vzv vasculopathy, zoster
Introduction
Herpes zoster primarily affects older adults, but immunocompromised individuals are at increased risk for atypical and diverse cutaneous manifestations. These may present as ecthymatous, chronic, verrucous, painless, or vasculitic forms, which are rarely seen in the general population [1,2]. Although most cases resolve without major complications, some patients may develop severe sequelae, including postherpetic neuralgia, bacterial superinfection, myelopathy, and meningoencephalitis [3]. While cerebral vasculopathies involving large- and medium-sized vessels have been reported following herpes zoster infection [4], cutaneous vasculitis remains a rare and underreported complication. Cutaneous vasculitis is characterized by inflammation of the blood vessels in the skin, leading to vascular damage and cutaneous manifestations such as palpable purpura, ulcers, and necrosis. The pathophysiology of post-zoster cutaneous vasculitis remains poorly understood but is believed to involve an immune-mediated response to varicella-zoster virus (VZV) reactivation, leading to vascular inflammation and tissue damage [4]. While previous studies have reported rare cases of post-zoster cutaneous vasculitis [1-10], the concurrent occurrence of this condition with acute calcium pyrophosphate deposition disease (CPPD) remains undocumented in the literature. This case report presents a unique clinical scenario, highlighting the potential association between these two conditions. By contributing this case to the limited existing literature, we aim to enhance the understanding of the rare complications associated with varicella-zoster virus infection.
Case presentation
An 82-year-old male, with a medical history of controlled hypertension, diabetes mellitus, coronary artery disease (status post two stents in 2001 and 2024), and pacemaker implantation, presented to the dermatology clinic. The patient described an onset of burning pain in the posterior neck 2-3 days prior to presentation, which subsequently radiated to the left arm. He reported that the pain was followed by the appearance of red papules and blisters on his left arm, accompanied by swelling in the left hand, which began around the same time. Although the patient has a history of atopic dermatitis, it was well-managed at the time of presentation. He denied any exposure to sick contacts and confirmed a childhood varicella infection but lacked immunization against shingles. He also denied any known immunodeficiency, had a history of occasional alcohol use, and was a non-smoker. Physical examination revealed erythematous papules and vesicles on the patient's left shoulder and forearm (C5/C6 dermatome) (Figure 1) accompanied by erythema, warmth, and swelling in the left hand.
Figure 1. Clinical presentation at initial evaluation showing erythematous papules, vesicles, and bullae localized to the C5 and C6 dermatomes of the left arm.
Despite these symptoms, his vital signs were normal, without fever or hypotension. A clinical diagnosis of herpes zoster (shingles) was established. The patient was initiated on oral acyclovir 800 mg five times daily for a duration of seven days, along with acetaminophen for pain management. Given the swelling, warmth, and redness in the left hand, cellulitis was suspected, and the patient was empirically treated with amoxicillin/clavulanate for seven days. The patient was advised to return to the emergency department if he experienced fever, chills, or clinical deterioration. However, as the hand swelling and erythema did not improve with antibiotics, he was referred to rheumatology. Arthrocentesis and synovial fluid analysis confirmed a diagnosis of calcium pyrophosphate deposition disease (CPPD) in the left wrist. The patient was managed with oral prednisone, initiated at 20 mg per day for two weeks followed by a tapering schedule, alongside colchicine. One week later, he presented to the dermatology clinic with a resolving zoster eruption, characterized by residual erythematous macules and post-inflammatory hyperpigmentation (Figure 2).
Figure 2. Gradual resolution of the zoster eruption, with residual erythematous macules and post-inflammatory hyperpigmentation.
One month later, the patient exhibited a unique clinical presentation with a purplish transformation of his zoster rash. Physical examination revealed purpuric macules and patches with crusted erosions in the same area previously affected by zoster (Figure 3) alongside improvement in hand swelling following treatment for acute CPPD.
Figure 3. Progression to purpuric macules and patches with crusted erosions in the same area previously affected by zoster.
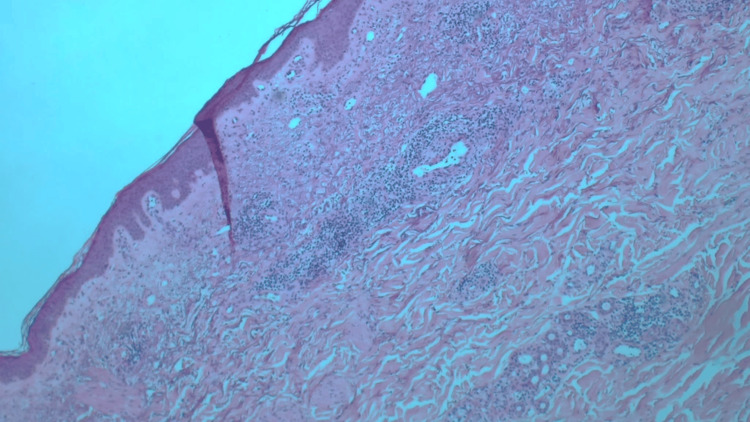
To rule out a post-zoster lichenoid reaction, a punch biopsy of a purple macule on the left arm was performed. Histopathologic examination with hematoxylin and eosin staining showed keratotic epidermis and perivascular inflammation in the upper and mid-dermis, primarily composed of small lymphocytes and some neutrophils with occasional necrotizing vasculitis (Figure 4).
Figure 4. Histopathology of a skin biopsy from the left arm revealing a keratotic epidermis and perivascular inflammation in the upper and mid-dermis, primarily composed of small lymphocytes and some neutrophils with occasional necrotizing vasculitis (hematoxylin and eosin stain).
Based on the clinical presentation of zoster followed by vasculitis on biopsy, a diagnosis of post-zoster cutaneous vasculitis was established. The patient had already received the recommended treatment of oral acyclovir and pain management. Given the asymptomatic nature of the vasculitis and its limited cutaneous involvement, the patient was reassured and monitored closely. The rash subsequently resolved without complications.
Discussion
Our patient initially presented with classic herpes zoster symptoms, including pain, erythema, vesicles, and bullae, which subsequently crusted over. However, one month later, the patient developed cutaneous vasculitis, a rare complication associated with herpes zoster infection. Although the varicella-zoster virus (VZV) is well-known for its association with a range of vascular complications, particularly those affecting the central nervous system and retina [11], its involvement in the pathogenesis of cutaneous vasculitis remains less clearly defined [2,6]. Post-zoster cutaneous vasculitis can emerge as a complication of herpes zoster, either following the characteristic vesicular rash or, interestingly, preceding the rash with no accompanying pain, as reported by Burgard et al. [3] and Erhard et al. [1]. The study of postherpetic cutaneous vasculitis continues to evolve, particularly concerning its pathophysiology and the connection between herpes zoster reactivation and subsequent vasculitis. Recent literature has underscored the complexity of this condition, with various studies suggesting that leukocytoclastic vasculitis (LCV) can occur as a complication of herpes zoster. For instance, Furuoka et al. (2023) documented a case of segmental cutaneous LCV associated with herpes zoster, which suggests a potential link between viral reactivation and the development of vasculitis [12].
Most reported cases of post-zoster cutaneous vasculitis have been observed in immunocompromised patients, including those receiving treatment for T-cell lymphoma [1] and systemic sarcoidosis [8]. These individuals are particularly susceptible due to the compromised state of their immune systems [1,4,7]. However, our patient was not immunocompromised. This raises the question of whether the prescribed 20 mg prednisone for managing acute CPPD led to transient immunosuppression, thereby facilitating an unusual progression of shingles into cutaneous vasculitis. This possibility is consistent with other case reports linking short-term immunosuppression to such complications [1,4]. In patients with CPPD, short-term immunosuppression significantly increases the risks associated with herpes virus reactivation. Immunosuppressive therapies can impair the host's ability to control latent infections, elevating the likelihood of complications such as postherpetic neuralgia and cutaneous vasculitis following herpes zoster reactivation [13].
Interestingly, our patient's post-zoster cutaneous vasculitis occurred concurrently with acute CPPD in the same extremity, which has not been described previously in the literature. This highlights the potential association between these two conditions. A plausible hypothesis suggests that VZV infection may act as a trigger for the onset or exacerbation of CPPD. Acute herpes zoster is linked to increased levels of pro-inflammatory cytokines, such as IL-1, IL-6, and TNF-α, which are also central to the development of CPPD [14,15]. The release of these cytokines during viral infection could promote localized inflammation and immune activation in surrounding tissues, potentially aggravating preexisting CPPD or triggering a new episode in predisposed individuals. Early recognition of post-zoster cutaneous vasculitis is crucial to prevent severe complications, including ulceration, necrosis, and secondary infections [8,10]. The condition can be easily misdiagnosed due to its similarity to other skin disorders such as leukocytoclastic vasculitis and pyoderma gangrenosum [9], emphasizing the need for prompt and accurate diagnosis.
Conclusions
In conclusion, postherpetic cutaneous vasculitis presents a complex interplay of viral infections, immune responses, and therapeutic interventions. Recent advancements in understanding its pathophysiology and treatment, alongside the implications of calcium pyrophosphate deposition disease (CPPD) and immunosuppression, highlight the importance of ongoing research and clinical vigilance in effectively managing this condition. Further studies are essential to enhance our understanding and improve patient outcomes.
Disclosures
Human subjects: Consent was obtained or waived by all participants in this study.
Conflicts of interest: In compliance with the ICMJE uniform disclosure form, all authors declare the following:
Payment/services info: All authors have declared that no financial support was received from any organization for the submitted work.
Financial relationships: All authors have declared that they have no financial relationships at present or within the previous three years with any organizations that might have an interest in the submitted work.
Other relationships: All authors have declared that there are no other relationships or activities that could appear to have influenced the submitted work.
Author Contributions
Concept and design: Marwa Hallal
Acquisition, analysis, or interpretation of data: Marwa Hallal, Zeina Tannous
Drafting of the manuscript: Marwa Hallal
Critical review of the manuscript for important intellectual content: Marwa Hallal, Zeina Tannous
Supervision: Zeina Tannous
References
- 1.Atypical varicella-zoster virus infection in an immunocompromised patient: result of a virus-induced vasculitis. Erhard H, Rünger TM, Kreienkamp M, Müller J, Müller-Hermelink HK, Bröcker EB. J Am Acad Dermatol. 1995;32:908–911. doi: 10.1016/0190-9622(95)91560-5. [DOI] [PubMed] [Google Scholar]
- 2.Education and imaging: gastrointestinal: herpes vasculitis in an ulcerative colitis patient. Wong JM, Huang PH, Wei SCh. J Gastroenterol Hepatol. 2013;28:586. doi: 10.1111/jgh.12093. [DOI] [PubMed] [Google Scholar]
- 3.Small vessel vasculitis in herpes zoster-discussion of current aspects of varicella zoster virus vasculopathy. Burgard B, Smola S, Vogt T, Müller CS. Am J Dermatopathol. 2018;40:602–604. doi: 10.1097/DAD.0000000000001134. [DOI] [PubMed] [Google Scholar]
- 4.Segmental leukocytoclastic vasculitis in herpes zoster. Wollina U, Schönlebe J. Int J Dermatol. 2012;51:1351–1352. doi: 10.1111/j.1365-4632.2011.05167.x. [DOI] [PubMed] [Google Scholar]
- 5.Herpes zoster associated with cutaneous small-vessel vasculitis: a rare case report with review of literature. Afacan E, Öğüt B, Erdem Ö, Adışen E. Indian J Dermatol. 2022;67:626. doi: 10.4103/ijd.ijd_1001_21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Leukocytoclastic vasculitis associated with cutaneous infection by herpesvirus. Cohen C, Trapuckd S. Am J Dermatopathol. 1984;6:561–565. doi: 10.1097/00000372-198412000-00008. [DOI] [PubMed] [Google Scholar]
- 7.Varicella-zoster virus vasculitis: a case of recurrent varicella without epidermal involvement. Uhoda I, Piérard-Franchimont C, Piérard GE. Dermatology. 2000;200:173–175. doi: 10.1159/000018359. [DOI] [PubMed] [Google Scholar]
- 8.Herpes zoster presenting as unilateral vasculitis. Clark AK, Dhossche J, Korcheva VB, Keller JJ. https://pubmed.ncbi.nlm.nih.gov/30695979/ Dermatol Online J. 2018;24:13030–13035. [PubMed] [Google Scholar]
- 9.Atypical herpes vasculitis in a leukemic patient: an unusual presentation. Cury-Martins J, Bellesso M, Sotto MN, Sanches JA. Hematol Transfus Cell Ther. 2019;41:95–98. doi: 10.1016/j.htct.2018.07.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Severe gangrene accompanied by varicella zoster virus-related vasculitis mimicking rheumatoid vasculitis. Tanaka A, Hayaishi N, Kondo Y, Kurachi K, Tanemura A, Katayama I. Case Rep Dermatol. 2014;6:103–107. doi: 10.1159/000360979. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Varicella zoster virus vasculopathy: the expanding clinical spectrum and pathogenesis. Nagel MA, Jones D, Wyborny A. J Neuroimmunol. 2017;308:112–117. doi: 10.1016/j.jneuroim.2017.03.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Segmental cutaneous leukocytoclastic vasculitis associated with herpes zoster: a case report and literature review. Furuoka K, Fukumoto T, Masuda Y, Tanigawa A, Kosaka H, Nagano T. Dermatol Reports. 2023;15:9709. doi: 10.4081/dr.2023.9709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Clinical features of varicella-zoster virus infection. Kennedy PG, Gershon AA. Viruses. 2018;10 doi: 10.3390/v10110609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Calcium pyrophosphate deposition disease. Pascart T, Filippou G, Lioté F, Sirotti S, Jauffret C, Abhishek A. Lancet Rheumatol. 2024 doi: 10.1016/S2665-9913(24)00122-X. [DOI] [PubMed] [Google Scholar]
- 15.Immunobiology of varicella-zoster virus infection. Laing KJ, Ouwendijk WJ, Koelle DM, Verjans GM. J Infect Dis. 2018;218:0–74. doi: 10.1093/infdis/jiy403. [DOI] [PMC free article] [PubMed] [Google Scholar]