Abstract
Background
This study aims to analyse the clinical characteristics of different types of odontogenic jawbone cysts (OJCs) and to provide a theoretical basis for prevention and clinical treatment.
Methods
Data from 1,038 patients with OJCs were collected, and relevant information, such as sex, age, clinical symptoms and signs, imaging data, number of lesions, lesion location, pathological diagnosis, clinical treatment and prognosis, was statistically analysed.
Results
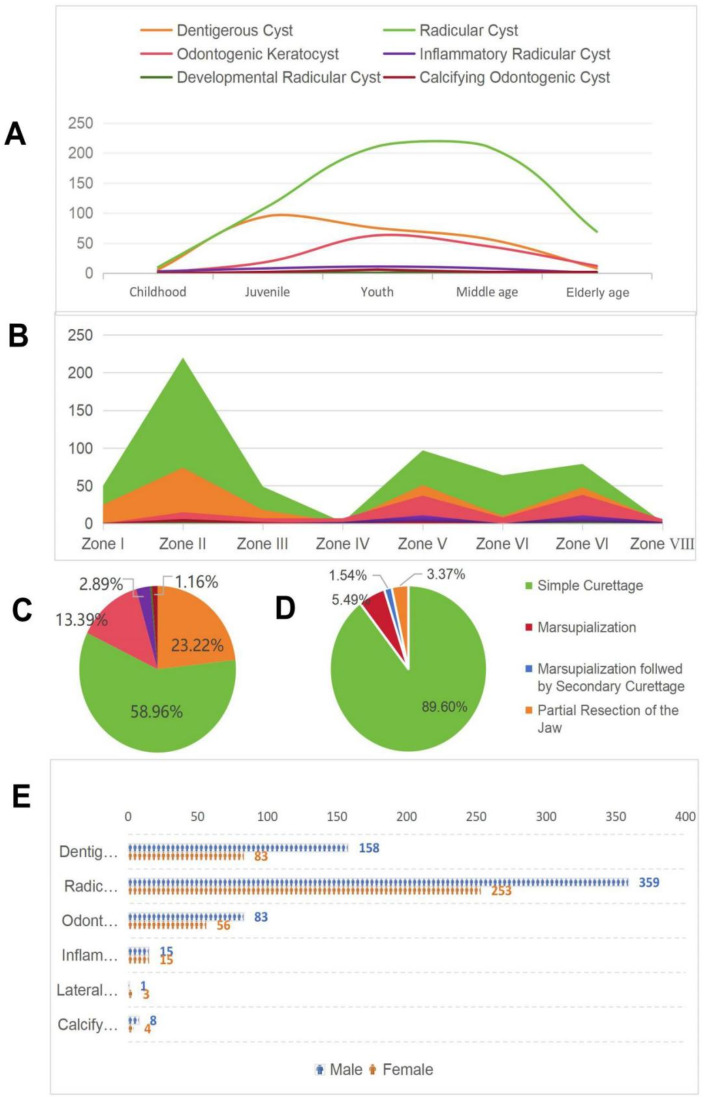
According to the World Health Organization (WHO) classification of OJCs in 2022, the highest incidence rate was observed for radicular cysts (RCs), accounting for 58.96% of the total number of cases, followed by dentigerous cysts (DCs), accounting for approximately 23.22% of cases. lateral periodontal cysts (LPCs) and calcifying odontogenic cysts (COCs) comprised the lowest number of cases. The age distribution of patients was between 4 and 89 years, and the high incidence age group was youth and middle age, accounting for 66.67% of the total number of cases. The male-to-female ratio of patients was 1.51:1, and there was a statistically significant difference between the sexes(p < 0.05).In terms of the site of incidence, odontogenic keratocysts (OKCs) were prevalent in the mandibular molar region. In addition, mandibular ramus, inflammatory collateral cysts (ICCs) and dentigerous cysts (DCs) were more common in the mandibular third molar, and radicular cysts (RCs) and calcifying odontogenic cysts (COCs) were prevalent in the maxillary anterior region. On imaging, 955 (92.0%) lesions were solitary, and 83 (8.0%) were multiple. The treatment included four types of surgery, including simple curettage, marsupialization, marsupialization followed by secondary curettage, and partial resection of the jaw, and a total of 921 patients were followed up, with a recurrence rate of 2.82%.
Conclusions
OJCs are more common in males than in females, and a statistically significant difference is observed in the most prevalent types of cysts occurring at different ages and in various regions of the jawbone (p < 0.05). Early diagnosis should be made with the help of X-rays, age, location, and clinical symptoms. In addition, appropriate treatment methods should be selected, and long-term follow-up observation is needed.
Keywords: Odontogenic cysts, Retrospective study, Clinicopathological classification
Background
The special anatomy of the oral and maxillofacial region and the complexity of the embryonic development process leads to the occurrence of cysts in the oral and maxillofacial region, with the jawbone being the most prevalent site for cysts in the human skeleton [1]. Jaw cysts can be divided into odontogenic and nonodontogenic cysts according to their tissue origin, among which odontogenic cysts comprise a group of cysts originating from the epithelium and epithelial remnants of tooth-forming organs, accounting for up to 90% of the cysts in the jawbone [2]. In an overall study of odontogenic jawbone cysts, Sharifian et al. explored the effects of special dental positions on cyst occurrence [3], but research on the distribution characteristics of cysts throughout the jaws is lacking. Several scholars, such as Ansari [4], have used every ten years as a criterion for the division of age ranges for the study of the correlation between lesions and age. However, this method of dividing ages does not coincide with the cycle of growth and development of the human body and has limitations. According to the 2022 World Health Organization (WHO) classification of odontogenic jawbone cysts (OJCs), these lesions can be categorised into radicular cysts (RCs), odontogenic keratocysts (OKCs), dentigerous cysts (DCs), calcifying odontogenic cysts (COCs), lateral periodontal cysts (LPCs), and inflammatory collateral cysts (ICCs) [5]. There are few studies based on this classification, and long-term observations of its efficacy are lacking. On the basis of the anatomical characteristics, combined with the characteristics of the occurrence of jawbone cysts, the group proposed the ‘eight-zone method of the jaw’ to partition the maxilla and mandible and to explore the relationships between different types of cysts and different jawbone zones. According to the characteristics of human growth and development and the replacement of erupted deciduous and permanent teeth, we divided the whole lifecycle into five stages and explored the relationships between different growth and development stages and different types of cysts. In addition, on the basis of the study by Tamiolakis and others’ studies combining pathological and demographic data [6], the group further included treatment methods and postoperative follow-up to conduct a comprehensive analysis of cysts to serve as a reference for cyst prevention, early identification, and the development of effective treatment plans.
Subjects and methods
Study subjects
A total of 1,038 files of patients with odontogenic jawbone cysts who presented at the First Affiliated Hospital of Bengbu Medical University from January 2017 to December 2023 were collected.
Inclusion criteria
1, Meeting the diagnostic criteria for odontogenic jawbone cysts; 2, receiving surgical treatment; 3, having complete clinical data; and 4, always undergoing follow up and treatment at our stomatology department according to the doctor’s prescription after surgery.
Exclusion criteria
1, Combination of abnormal bone metabolism system diseases; 2, case diagnosis of solid tumorous diseases such as central jaw cancer; 3, pregnancy and lactation; and 4, cognitive impairment or poor treatment adherence.
Clinical data collection
We collected data from 1,038 OJCs files and compiled clinically relevant data, such as patient sex, age of onset, clinical symptoms and signs, imaging data, number of lesions, location of lesions, pathologic results and other clinically relevant data. Preoperatively, the cystic lesion was clearly demonstrated via orthopantomogram (OPG) or cone-beam computed tomography (CBCT; technical parameters: tube voltage, 90 kV; tube current, 10 mA). Each patient was required to stand upright and bite down with the upper and lower front teeth in the grooves of the occlusal guide. During this process, the head was in a fixed position, and the centre line of the face was perpendicular to the ground. Images were recorded in digital imaging and communication (DICOM) format. The patients were followed up regularly within 3–6 months after the operation and at least once a year after 1 year, and any recurrence was recorded. The collection of patient data involved in this study was approved by the Biomedical Ethics Committee of the First Affiliated Hospital of Bengbu Medical University (ethics approval number: 201410).
Statistical analysis of data
The data were analysed via IBM SPSS Statistics (version 27). Data on sex, site distribution, and age of prevalence of patients with jaw cysts were statistically analysed. For the count data, a cross-cardinality analysis was performed, in which significant results were compared two by two via the Bonferroni correction and reported in the form of counts and percentages. Quantitative data are expressed as xˉ±s, and independent samples t tests were used to analyse differences for variables that met a normal distribution and were grouped into two groups. One-way analysis of variance (ANOVA) was used for variables that met a normal distribution and were grouped into three or more groups. Nonparametric tests were used for variables that did not meet the normal distribution of the indicators were used to analyse the variables and are reported in the form of the median (p25th quartile and p75th quartile). A test level of p < 0.05 was considered statistically significant.
Results
Pathologic typing of OJCs
According to the pathological diagnosis of tissue sections, combined with imaging data and clinical manifestations, 1,038 OJCs were classified into different pathological types: RCs accounted for 58.96%; DCs accounted for 23.22%; OKCs accounted for 13.39%; LPCs accounted for 0.39%; ICCs accounted for 2.89%; and COCs accounted for 1.16% (Table 1).
Table 1.
Classification and gender ratio of odontogenic jawbone cysts
| Male | Female | Subtotal | Composition Ratio | Chi-square | p-value | ||||
|---|---|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | ||||
| Dentigerous Cyst | 158 | 0.040 | 83 | 0.020 | 241 | 0.030 | 1.90: 1 | 37.089 | 0.000 |
| Radicular Cyst | 359 | 0.080 | 253 | 0.050 | 612 | 0.060 | 1.42: 1 | 39.445 | 0.000 |
| Odontogenic Keratocyst | 83 | 0.020 | 56 | 0.010 | 139 | 0.010 | 1.48: 1 | 10.506 | 0.001 |
| Inflammatory Collateral Cyst | 15 | 0.000 | 15 | 0.000 | 30 | 0.000 | 1:1 | 0.192 | 0.661 |
| Lateral Periodontal Cyst | 1 | 0.000 | 3 | 0.000 | 4 | 0.000 | 0.33: 1 | 0.711 | 0.399 |
| Calcifying Odontogenic Cyst | 8 | 0.000 | 4 | 0.000 | 12 | 0.000 | 2:1 | 2.061 | 0.151 |
| Total | 442,553 | 100.000 | 519,301 | 100.000 | 961,854 | 100.000 | 0.85: 1 | ||
Sex ratio of OJCs
A total of 961,854 patients were hospitalised in our hospital from January 2017 to December 2023, with a male to female ratio of 1:1.17. Among them, the male to female ratio of patients with OKCs was 1.48:1; the DC ratio was 1.90:1; the RC ratio was 1.42:1; the LPC ratio was 0.33:1; the ICC ratio was 1:1; and the COC ratio was 2:1 (Fig. 1E). The chi-square test for different subtypes of odontogenic jawbone cysts revealed that the differences between the male and female incidence rates of DCs, RCs, and OKCs were statistically significant (p < 0.05), whereas the differences between the male and female incidence rates of LPCs, ICCs, and COCs were not statistically significant (p > 0.05; Table 1).
Fig. 1.
(A) Age distribution of odontogenic jawbone cysts. (B) Location distribution of odontogenic jawbone cysts. (C) Percentages of different subtypes of odontogenic jawbone cysts. (D) Percentages of different types of surgery for odontogenic jawbone cysts. (E) Sex distribution of odontogenic jawbone cysts
Age division of OJCs
The characteristics of the onset of OJCs in patients at different stages of growth and development differ based on the cyclic patterns of human growth and development. Our group referred to the “2022 NBS age division standards” to categorise the cysts into five age groups: (1) Childhood: 0–6 years old; (2) Juvenile: 7–17 years old; (3) Youth: 18–40 years old; (4) Middle age: 41–65 years old; and (5) Elderly age: 66 years old and above. The most common age category of OJCs was youth, followed by middle-aged individuals and juveniles. A cross‒square comparison revealed a statistically significant difference in the prevalence of DCs, RCs, OKCs, ICCs, and COCs across the different age categories (p < 0.05), and a difference in the prevalence of different types of cysts across childhood, juvenile, middle-aged, and elderly age groups was observed (p < 0.05). In childhood, RCs are most commonly found. In Juvenile, both RCs and DCs are prevalent. Among individuals in the youth category, various types of diseases are commonly seen. Whereas in middle age and elderly age, RCs are the most predominant (Table 2; Fig. 1A).
Table 2.
Case analysis *age group cross-tabulation
| Childhood (0–6 years old) | Juvenile (7–17 years old) | Youth (18-40years old) | Middle age (41-65years old) | Elderly age (66years old and above) | Subtotal | ||
|---|---|---|---|---|---|---|---|
| Dentigerous Cyst | Count | 6 | 95 | 75 | 57 | 8 | 241 |
| Percentage of Pathological Types | 2.50% | 39.40% | 31.10% | 23.70% | 3.30% | 100.00% | |
| Percentage by Age Group | 31.60% | 40.30% | 20.40% | 17.50% | 8.80% | 23.20% | |
| Percentage of the Total | 0.60% | 9.20% | 7.20% | 5.50% | 0.80% | 23.20% | |
| Radicular Cyst | Count | 10 | 111 | 211 | 211 | 69 | 612 |
| Percentage of Pathological Types | 1.60% | 18.10% | 34.50% | 34.50% | 11.30% | 100.00% | |
| Percentage by Age Group | 52.60% | 47.00% | 57.50% | 64.90% | 75.80% | 59.00% | |
| Percentage of the Total | 1.00% | 10.70% | 20.30% | 20.30% | 6.60% | 59.00% | |
| Odontogenic Keratocyst | Count | 0 | 19 | 63 | 45 | 12 | 139 |
| Percentage of Pathological Types | 0.00% | 13.70% | 45.30% | 32.40% | 8.60% | 100.00% | |
| Percentage by Age Group | 0.00% | 8.10% | 17.20% | 13.80% | 13.20% | 13.40% | |
| Percentage of the Total | 0.00% | 1.80% | 6.10% | 4.30% | 1.20% | 13.40% | |
| Inflammatory Collateral Cyst | Count | 3 | 8 | 11 | 8 | 0 | 30 |
| Percentage of Pathological Types | 10.00% | 26.70% | 36.70% | 26.70% | 0.00% | 100.00% | |
| Percentage by Age Group | 15.80% | 3.40% | 3.00% | 2.50% | 0.00% | 2.90% | |
| Percentage of the Total | 0.30% | 0.80% | 1.10% | 0.80% | 0.00% | 2.90% | |
| Lateral Periodontal Cyst | Count | 0 | 1 | 1 | 2 | 0 | 4 |
| Percentage of Pathological Types | 0.00% | 25.00% | 25.00% | 50.00% | 0.00% | 100.00% | |
| Percentage by Age Group | 0.00% | 0.40% | 0.30% | 0.60% | 0.00% | 0.40% | |
| Percentage of the Total | 0.00% | 0.10% | 0.10% | 0.20% | 0.00% | 0.40% | |
| Calcifying Odontogenic Cyst | Count | 0 | 2 | 6 | 2 | 2 | 12 |
| Percentage of Pathological Types | 0.00% | 16.70% | 50.00% | 16.70% | 16.70% | 100.00% | |
| Percentage by Age Group | 0.00% | 0.80% | 1.60% | 0.60% | 2.20% | 1.20% | |
| Percentage of the Total | 0.00% | 0.20% | 0.60% | 0.20% | 0.20% | 1.20% | |
| Total | Count | 19 | 236 | 367 | 325 | 91 | 1038 |
| Percentage of Pathological Types | 1.80% | 22.70% | 35.40% | 31.30% | 8.80% | 100.00% | |
| Percentage by Age Group | 100.00% | 100.00% | 100.00% | 100.00% | 100.00% | 100.00% | |
| Percentage of the Total | 1.80% | 22.70% | 35.40% | 31.30% | 8.80% | 100.00% |
Distribution of different sites of OJCs
To more accurately describe the complexity of jawbone lesions, the group further conducted a detailed zoning study of the jawbone on the basis of the nomenclature system of the International Federation of Dentistry (FDI) for dental sites. Through careful observation and analysis of the anatomical features of the jawbone, we divided the jawbone into eight different regions in a clockwise direction. This partitioning method considers not only the anatomical differences and variations in the exercise of functions but also the special characteristics of each region in the process of disease occurrence and treatment. We named this new division method the “eight-zone method of the jawbone” (Fig. 2). The jawbone is divided into the following zones: Zone I, the portion of the jawbone corresponding to the 14–18 dental positions; Zone II, the portion of the jawbone corresponding to the 13–23 dental positions; Zone III, the portion of the jawbone corresponding to the 24–28 dental positions; Zone IV, the left mandibular ramus; Zone V, the portion of the jawbone corresponding to the 34–38 dental positions; Zone VI, the portion of the jawbone corresponding to the 33–43 dental positions; Zone VII, the jawbone corresponding to the 44–48 dental positions; and Zone VIII, the right mandibular ramus.
Fig. 2.
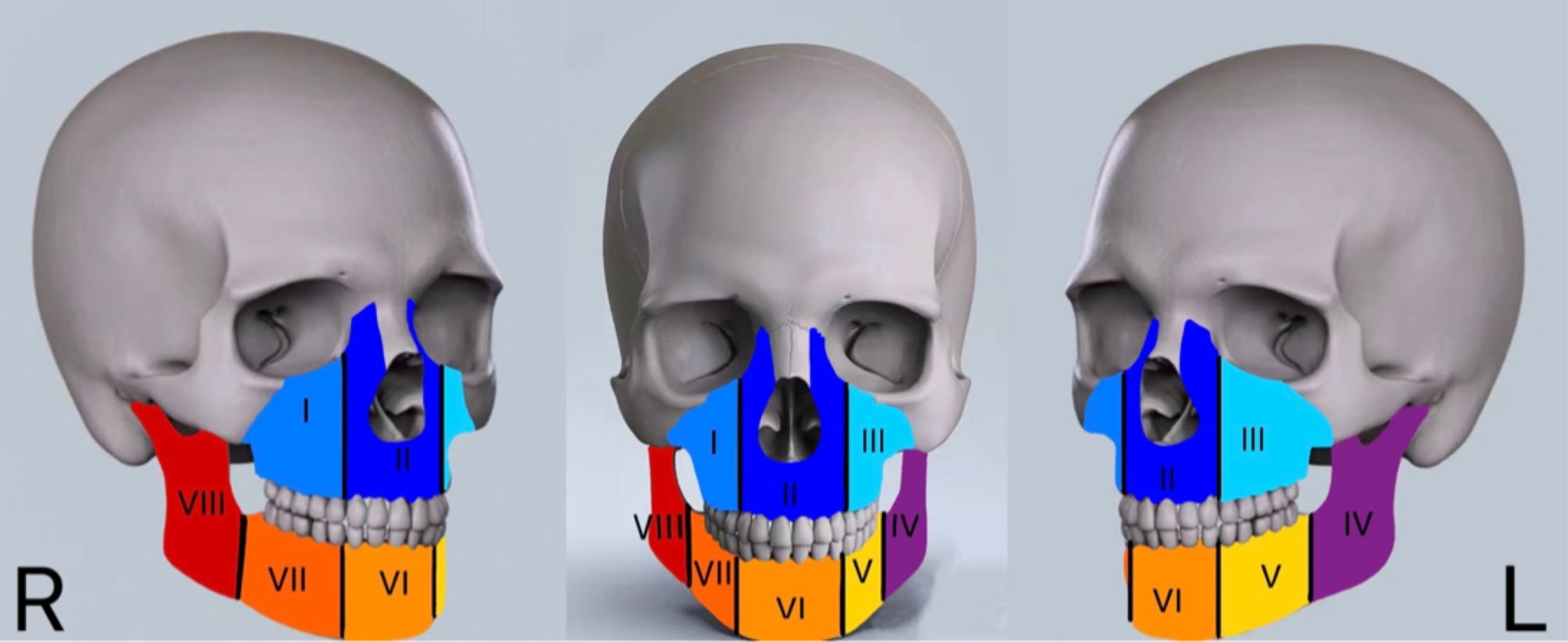
Eight-zone method of the jaw
Our statistical analysis revealed 955 cases of solitary OJCs (Table 3). Statistical analysis of the prevalent cysts in each region revealed a significant difference in the distribution of cyst types (p < 0.05). Dividing the maxilla and mandible into eight zones was statistically significant for studying the characteristics of OJC development. Further analysis revealed a significant difference in the distribution of prevalent regions for each cyst type (p < 0.05). Specifically, the incidence of OKCs in the mandible was significantly greater than that in the maxilla, and OKCs were prevalent in Zones IV, VIII, V and VII, accounting for 74.58% of the total incidence. The incidence of RCs was 56.66% in the maxilla, with zone II being the most common, accounting for 39.08% of the total incidence.DCs were found in Zones II, V, and VII, accounting for 74.89% of the total incidence, and the highest prevalence was noted in the maxillary cuspid region. Its percentage in the corresponding area of the mandibular third molar(MTM) region is 73.73% of that of zones V and VII.The sample sizes of ICCs and LPCs were too small. The former predominantly occurred in Zones V and VII, especially in the MTM, and the latter were most easily found in Zones II and VII. COCs are prevalent in Zone II. There were 83 multifocal OJCs (8.00%), including 21 OKCs, 10 DCs, 49 RCs, and 3 ICCs.
Table 3.
Central location distribution in different types of odontogenic jaw cysts
| Zone I | Zone II | Zone III | Zone IV | Zone V | Zone VI | Zone VII | Zone VIII | Total | |
|---|---|---|---|---|---|---|---|---|---|
| Dentigerous Cyst | 25 | 74 | 18 | 2 | 51 | 10 | 48 | 3 | 231 |
| Radicular Cyst | 50 | 220 | 49 | 2 | 97 | 64 | 79 | 2 | 563 |
| Odontogenic Keratocyst | 0 | 15 | 7 | 7 | 37 | 8 | 38 | 6 | 118 |
| Inflammatory Collateral Cyst | 0 | 0 | 1 | 2 | 11 | 0 | 11 | 2 | 27 |
| Lateral Periodontal Cyst | 0 | 2 | 0 | 0 | 0 | 0 | 2 | 0 | 4 |
| Calcifying Odontogenic Cyst | 1 | 6 | 2 | 0 | 3 | 0 | 0 | 0 | 12 |
| Total | 76 | 317 | 77 | 13 | 199 | 82 | 178 | 13 | 955 |
Note: If an OJC spans more than one zone, the position of the centre of the cyst is used to assign it to a specific zone
Surgical modalities of OJCs
For OJCs, four surgical procedures are typically used: simple curettage, marsupialization, marsupialization followed by secondary curettage, and partial resection of the jaw. Through the OPG and CBCT, for large jaw cysts, priority is given to marsupialization and wearing cyst plugs to prevent the window from closing. Moreover, 6–18 months after marsupialization, marsupialization is performed in combination with second-stage curettage, as appropriate, for those cysts whose cystic cavity shrinkage slows down and has not completely disappeared. Partial maxillectomy for lesions with high frequency of recurrence and malignant tendency.Among the patients in this group, 930 underwent simple curettage, accounting for 89.60%; 57 underwent open marsupialization, accounting for 5.49%; 16 underwent marsupialization followed by secondary curettage, accounting for 1.54%; and 35 underwent partial resection of the jaw, accounting for 3.37% Table 4).
Table 4.
Various surgical approaches for treating odontogenic jawbone cysts
| Odontogenic Jaw Cyst | Simple Curettage | Marsupialization | Marsupialization followed by Secondary Curettage | Partial Resection of the Jaw | subtotal |
|---|---|---|---|---|---|
| Dentigerous Cyst | 209 | 23 | 3 | 6 | 241 |
| Radicular Cyst | 563 | 24 | 7 | 18 | 612 |
| Odontogenic Keratocyst | 117 | 6 | 6 | 10 | 139 |
| Inflammatory Collateral Cyst | 26 | 4 | 0 | 0 | 30 |
| Lateral Periodontal Cyst | 3 | 0 | 0 | 1 | 4 |
| Calcifying Odontogenic Cyst | 12 | 0 | 0 | 0 | 12 |
| Total | 930 | 57 | 16 | 35 | 1038 |
Postoperative follow-up of OJCs
Postoperative follow-up ranged from 6 months to 7 years, with a total of 921 patients followed up and 26 (2.82%) recurrences. No recurrence was noted after marsupialization or partial resection of the jaw alone, and some patients experienced recurrence after curettage and after marsupialization followed by secondary curettage. In 823 follow-up cases after curettage, 22 (2.67%) patients experienced recurrence, of which 10 were OKCs, accounting for 45.45% of the recurrences after curettage, and 7 were RCs (31.81%). Among the 16 patients who underwent marsupialization followed by secondary curettage, 4 (25%) experienced recurrence, of which 2 were OKCs. Notably, 15 of the 1,038 patients with a history of inpatient surgery (before 2017) were readmitted for recurrence after curettage. Among these patients, 6 patients experienced recurrence 4 years after surgery, 2 patients experienced recurrence 10 years after surgery, and 2 patients experienced recurrence 6 years after surgery. The recurrence intervals for the remaining 5 patients were 11, 9, 5, 3 and 1 year, respectively. These findings demonstrate that OJCs can recur after a long latency period after curettage. This included 8 cases of OKCs, 5 cases of RCs and 2 cases of DCs.
Discussion
Diagnosis of OJCs
The histopathology of OJCs is usually considered the “gold standard” for diagnosis. However, in terms of histopathological features, the different types of odontogenic jawbone cysts presented some common features. Specifically, the epithelial lining of OKCs, DCs, and LPCs was thin and had a uniformly thick squamous epithelium without epithelial pegs. The epithelial lining of coinfected OKCs, RCs, and ICCs is a squamous epithelium of variable thickness with irregularly elongated epithelial pegs. The walls of the cysts are infiltrated with inflammatory cells, and cholesterol crystals are observed in the walls of the cysts [7, 8], which makes the diagnosis of cyst type on the basis of histology alone difficult in some cysts. Therefore, the diagnosis of OJCs should consider the clinical manifestations and imaging and histological features of the cyst. We have shown the imaging characteristics of cystic lesions by means of OPGs, which are more suitable for routine examination of OJCs. CBCT can provide three-dimensional images of cysts. CBCT images provide important information on the presence and extent of bone and tooth resorption, cortical expansion, calcification, tooth displacement and anatomical structure involvement. These imaging methods are used to observe the presence or absence of root resorption and its characteristics, whether the cysts are compartmentalised, the presence of a surrounding radiopaque line, the presence of notching, whether the cysts contain teeth and the condition of those teeth, and whether the density is homogeneous, among other features (Fig. 3). By combining the patient’s clinical manifestations, such as the presence of dental or pulp diseases, or by distinguishing the contents of the cyst, we can further clarify the diagnosis [9].
Fig. 3.
Imaging manifestations of odontogenic jawbone cysts. (a) Inflammatory Radicular Cyst (b) Dentigerous Cyst (c) Odontogenic Keratocyst. (d) Radicular Cyst (e) Calcifying Odontogenic Cyst (f) Inflammatory Radicular Cyst
Relationships between the pathologic type of OJCs and sex
Our data revealed that RCs accounted for the highest percentage of OJCs (58.96%), which was slightly greater than that reported by Tamiolakiss (57.0%) [6]. DCs accounted for 23.22%, which was slightly greater than that reported by Ansaris (22.1%) [4]. OKCs accounted for 13.39%, which was slightly lower than that reported by Kammer (15.02%) [10]. The male to female ratio in our inpatient population was close to 1:1, but the prevalence of OJCs was 1.51:1 in males and females, which is in agreement with the results of the study by Tamiolakis (1.6:1) [6]. We found that the prevalence of DCs was 1.90 times greater in males than in females; 1.48 times greater in OKCs; and 1.42 times greater in DCs, with a statistically significant difference in prevalence (p < 0.05). This can be attributed to certain lifestyle differences, such as smoking and drinking, between men and women [11]; differences in hormone levels between men and women, where androgens may play a specific role in the development of teeth and jaws, thus affecting the formation of cysts ; and differences in dental development, such as delayed eruption of teeth in males. In addition, certain occupations with increased exposure risks for substances that are harmful to oral health are dominated predominantly by males. These previously noted reasons may contribute to the higher incidence of odontogenic jawbone cysts in males than in females.
Relationships between OJCs and different age groups
Based on the characteristics of human growth and development and taking into full consideration the process of eruption and replacement of deciduous and permanent teeth, we classified our patients according to their life cycle into five age groups: Childhood, Juvenile, Youth, Middle age and Elderly age. Childhood is the period of deciduous dentition; children have poor brushing habits and prefer sweets, and the incidence of dental caries is greater. The lack of coordination of motor function in childhood and the vulnerability of the anterior deciduous teeth to trauma may increase the risk of RCs [12]. RCs account for 52.63% of the total number of cases of childhood morbidity, suggesting that children should be actively prevented from experiencing caries, and RCs should be prevented through on-time reassessments after dental trauma. Jun Pei et al. suggested that the incidence of RCs is lower in deciduous teeth [13]. This is due to the smaller age range of childhood and fewer cases of cysts. In fact, the incidence of RCs is greater than that of other cysts in children if OJCs occur. The juvenile period is characterized by a mixed dentition stage, during which young permanent teeth erupt and the apical foramen gradually closes. The incidence of DCs was greater in this period, accounting for 40.25% of the total number of cases in the juvenile study population. The sudden increase in the incidence of DCs compared with the previous childhood period is because the juveniles at this stage are in the mixed dentition period. In addition, the decay and retention of deciduous teeth may prevent the normal eruption of permanent teeth and cause problems in the periapical tissues of the deciduous teeth. Moreover, the late eruption of permanent teeth and crowding of the teeth, as well as the pressure and movement during orthodontic treatment, may cause some teeth to fail to erupt normally and form DCs. The presence of supernumerary teeth may also cause DCs, and hidden jaw cysts are often found when the patient addresses the aforementioned conditions. Therefore, it is suggested that patients should undergo early X-ray examination to exclude ambulatory teeth, supernumerary teeth and cysts if the number of teeth erupted during the replacement period is not consistent with their age. Among individuals in the youth category, the apical foramen is closed at this stage, and it is the time when wisdom teeth start to erupt (18–25 years old), and DCs occur due to improper positioning of the teeth or insufficient space in the jaws for normal eruption. This is in complete agreement with the age group (21.5 ± 14.5) reported by Sharifian as the prevalent age group for DCs [3], which coincides with the full stage of juveniles and youth, reflecting the intuitive and easy nature of this age classification. OJCs in young individuals are also associated with genetic factors, hormonal changes, hygiene habits and past medical history, and their clinical features are diverse. In middle-aged and Elderly-aged individuals, along with the wear and damage to teeth, cysts can be triggered by common oral diseases, such as pulpitis, apical periodontitis, and periodontal disease. In addition, chronic systemic diseases, such as diabetes mellitus, can affect the ability to heal and resist infections; thus, the cysts of this period predominantly RCs, which is consistent with the conclusions drawn by Kanipakam [14] after an in-depth discussion of the aetiology of RCs and the pathogenesis of the cysts. In addition, 64.92% and 75.82% of the participants were middle-aged and older, respectively. Problems in the dental tissues of middle-aged and elderly people should be addressed promptly.
Relationships between OJCs and different regions of the jawbone
In the study of OJCs, we found significant differences in their distributions at different sites (p < 0.05). Some researchers have studied jawbone cysts from the perspective of characteristics of individual teeth [3], but there are limitations because the development of cysts is not only related to teeth but also closely related to the anatomical structure of the jawbone. On the basis of the unique anatomical characteristics of different jawbone regions and the naming of tooth positions by FDI, zoning different parts of the jawbone can help to pinpoint each region and analyse the characteristics of the entire jawbone in a systematic manner. Using the position of the centre of OJCs as the basis for regional positioning can solve the problem of determining the location assignment of large cysts involving multiple tooth positions. This approach can be used not only to count the types of cysts and their incidence in different regions but also to explore the causes of the pathogenesis of different anatomical regions and define a reasonable method to address them. Zones II to VI comprise the area of the jawbone corresponding to the anterior teeth. Zone II is close to the nasal cavity, and the anterior teeth are susceptible to trauma, which makes them prone to RCs. This finding suggests regular follow-up and imaging after anterior tooth trauma. The region between maxillary cuspids often has supernumerary teeth, and it is more common to find DCs here. Less dental trauma is noted in Zone VI, and the incidence of supernumerary teeth is lower than that in Zone II [12], so the incidence of all types of maxillary cysts is lower in Zone VI. Owing to the presence of the maxillary sinus in Zones I and III, OJCs are often closely related to the maxillary sinus and should be protected during surgery to prevent excessive force from penetrating the maxillary sinus [15]. Owing to the low bone density and thin bone cortex in this region, cysts develop faster [16] and should be treated promptly after cyst occurrence. Mandibular premolar teeth, molar teeth and inferior alveolar nerve canals are present in Zones V and VII, and the onset of OJCs can affect the inferior alveolar nerve. The appropriate surgical procedure should be based on the location and size of the cystic cavity, and the appropriate procedure should be selected to reduce damage to the nerve. Mandibular molars usually have multiple roots and tortuous root canals, which increases the difficulty of root canal treatment [17]. Treatment should be as thorough as possible; otherwise, it may lead to the development of DCs. Wisdom teeth often do not erupt completely because of an abnormal position or insufficient bone mass. This can easily lead to the development of DCs, and the percentage of MTM with DCs is 73.73% in Zones V and VII. The molar region is subjected to greater masticatory pressure, which may lead to microinjuries to the teeth and surrounding structures, increasing the risk of cysts. Long-term tooth wear or injury may lead to pulp damage, which subsequently results in the development of cysts. Zones V and VII are the most common areas for many types of cysts. In addition to COCs, RCs, DCs, and OKCs have a much greater incidence in Zones V and VII than in Zones I and II, and the incidence of these cysts in the mandibular premolar and molar regions is much greater than that in the same region of the maxilla (Fig. 1B). Zones IV and VIII are mandibular ramus segments, and cysts may form in this zone due to ectopic, impacted, or supernumerary teeth. Their corresponding treatments have less impact on occlusal function. However, the mandibular ramus is connected to the temporomandibular joint, and large jaw cysts may affect the condyle and the temporomandibular joint; if accompanied by infection, the patient’s opening and closing of the mouth may have a certain impact.
Postoperative follow-up of patients with OJCs
The recurrence rate after curettage of OJCs in our group was relatively low, much lower than the recurrence rate reported by Gonçalves et al. for curettage [18]. The main reason for this is that the procedure removes the cyst wall completely by physical means, reducing the possibility of residual diseased tissue. With improvements in surgical techniques in recent years, influenced by Hisaki Aiba [19], we have used endoscopic techniques during the scraping of some cysts. This method improves the accuracy of the procedure and reduces the recurrence rate. After curettage, the recurrence rate of OKCs was high, and the time of recurrence could be up to 7 years after surgery. This finding is consistent with Titinchi’s conclusion [20], suggesting that patients should be followed up for a long time after surgery. In minors, marsupialization is less invasive and has less impact on jaw development. Allon’s study also supports marsupialization as a conservative treatment for minors [21]. Marsupialization not only significantly reduces the size of the cyst but also reduces damage to healthy bone tissue and maintains the integrity of the jaw. The jaws of minors are still in the developmental stage, and their bone regeneration capacity is significantly greater than that of adults. However, the reason for the significant increase in the recurrence rate after marsupialization followed by secondary curettage remains unclear. The possible reasons are that this procedure is indicated for large maxillary cysts. Some of these cysts have multiple compartments that can be easily missed. Most of these cysts are located in the jawbone distal to the posterior teeth or in the ascending mandibular ramus, with limited intraoperative manipulation and difficulty in reaching all parts of the cystic cavity with instruments, resulting in incomplete scraping. Postoperative formation of new bone may cover or hide the cyst wall remnants or even encapsulate the cyst wall, leading to cyst recurrence. Wuelling, M. et al. also suggested that MSCs differentiate into chondrocytes or osteoblasts depending on the local environment during bone repair, allowing the bone to integrate in a complex manner with other tissues during growth [22]. Nevertheless, these results should be interpreted with caution due to the small sample size of recurrences.
In addition, we found that in patients with OJCs, recurrence can occur after a relatively long interval following curettage surgery. Recurrence can still occur 4 years or even up to 11 years postoperatively. Alberto reported that most glandular odontogenic cysts recur within 5 years after surgery, but recurrence may occur up to 21 years after surgery [23]. This finding shows that, in addition to glandular odontogenic cysts, OJCs also exhibit this characteristic. Titinchi et al. reported that the low recurrence rate of inflammatory cysts is because inflammatory cysts are more likely to be completely removed by surgery than other cysts are [24]. However, we found that recurrence of RCs can occur in the short term after curettage, and recurrence was still observed in some patients with RCs 4–10 years after surgery. Although the overall recurrence rate of inflammatory cysts is lower than that of other types of cysts, local infection or residual lesions may lead to recurrence. Owing to individual patient differences, cyst types and postoperative management, some patients may still experience recurrence after a long interval and require long-term follow-up.
Limitations
There are several limitations in this study. First, some patients did not have timely postoperative follow-up, and telephone follow-up could not accurately assess the recovery of patients without the help of auxiliary examinations (OPG, CBCT). In particular, some patients choose to visit other hospitals for treatment after recurrence for work or personal reasons, resulting in incomplete follow-up data. Second, the small number of cases of certain types of OJCs, such as LPCs and COCs, causes underrepresented. Thus, further case collection and validation are still needed. In addition, failure to fully control for confounding factors such as patients’ health status and lifestyle habits may have had some impact on the accuracy of the study results. In future studies, we will adopt methods to overcome these limitations, such as improving data collection methods, expanding the sample size, and designing more refined follow-up procedures.
Conclusion
In summary, the prevalent types of OJCs differ in terms of sex, age group and jaw region, and these characteristics are fundamental for the early diagnosis and personalised treatment of OJCs. Moreover, due to multiple complex factors, some cysts have long recurrence intervals, suggesting that the follow-up period should be extended. In the future, we will further explore the mechanisms of action of OJCs and improve the prognosis of patients by optimising the treatment plan and clinical operation.
Acknowledgements
Not applicable.
Abbreviations
- DC
Dentigerous cyst
- RC
Radicular cyst
- OKC
Odontogenic keratocyst
- ICC
Inflammatory collateral cyst
- LPC
Lateral periodontal cyst
- COC
Calcifying odontogenic cyst
- OJC
Odontogenic jaw cyst
- WHO
World health organization
- MTM
mandibular third molar
Author contributions
K.Z, L.L, C.D: Conceptualization, Methodology, Investigation, Supervision, Project Administration; C.D, Z,W, R.Z: Data Curation, Formal Analysis; C.D, D.L, D.W: Visualization, Software; H.W, C.W: Investigation; T.G, R.H: Validation. All authors had access to the study data and reviewed and approved the final manuscript.
Funding
This research was supported by Scientific Research Foundation of Education Department of Anhui Province of China, China under grant number gxbjZD2021058.
Data availability
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Declarations
Ethics approval and consent to participate
This study protocol was performed in accordance with the Declaration of Helsinki and approved by the Ethics Committee of The First Affiliated Hospital of Bengbu Medical University (No. (2014)10). Ethics Committee for the Application of Clinical Technology of the First Affiliated Hospital of Bengbu Medical University evaluated and approved this study.
Consent for publication
Not applicable.
Informed consent
was obtained from all the participants including both patients and the legal guardians of children involved in the present study.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Liang Liu, Email: dclhhhh@163.com.
Kai Zhang, Email: zk29788@163.com.
References
- 1.Li T, editor. Clinical Pathology diagnosis and Differential diagnosis—oral and maxillofacial diseases. People’s Medical Publishing House; 2020.
- 2.Franklin JRB, Vieira EL, Brito LNS, Castro JFL, Godoy GP. Epidemiological evaluation of jaw cysts according to the new WHO classification: a 30-year retrospective analysis. Braz Oral Res. 2021;35:e129. 10.1590/1807-3107bor-2021.vol35.0129. [DOI] [PubMed] [Google Scholar]
- 3.Sharifian MJ, Khalili M. Odontogenic cysts: a retrospective study of 1227 cases in an Iranian population from 1987 to 2007. J Oral Sci. 2011;53(3):361–7. 10.2334/josnusd.53.361. [DOI] [PubMed] [Google Scholar]
- 4.Ansari MK, Alam S, Meraj F, Ahmad SS. Clinicopathological analysis of 847 odontogenic cysts examined over 10 years period: a retrospective study. J Dent Med Sci. 2021;20(3):58–64. 10.9790/0853-2003055864. [Google Scholar]
- 5.Vered M, Wright JM. Update from the 5th Edition of the World Health Organization Classification of Head and Neck tumors: odontogenic and maxillofacial bone tumours. Head Neck Pathol. 2022;16(1):63–75. 10.1007/s12105-021-01364-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Tamiolakis P, Thermos G, Tosios KI et al. Demographic and Clinical Characteristics of 5294 Jaw Cysts: A Retrospective Study of 38 Years. Head and Neck Pathol 2019;13, 587–596. https://doi.org/10.1007/s12105-019-01011-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Uddin N, Zubair M, Abdul-Ghafar J, et al. Orthokeratinized odontogenic cyst (OOC): Clinicopathological and radiological features of a series of 10 cases. Diagn Pathol. 2019;14(1):28. 10.1186/s13000-019-0801-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Akutsu JI, Iwahashi T, Nariai Y. Fenestration is a logical and effective treatment for a large primordial cyst with cholesterol granuloma: a case report. J Int Med Res. 2022;50(6):3000605221104185. 10.1177/03000605221104185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Luo JF, Zhou H, Wei Z, et al. Clinical and pathological characteristics analysis of odontogenic jaw cysts. J Pract Hosp Clin. 2021;18(3):104–7. [Google Scholar]
- 10.Kammer PV, Mello FW, Rivero ERC. Comparative analysis between developmental and inflammatory odontogenic cysts: retrospective study and literature review. Oral Maxillofac Surg. 2020;24:73-84.https://doi.org/10.1007/s10006-019-00816-8. [DOI] [PubMed] [Google Scholar]
- 11.Perez A, Lenoir V, Lombardi TD. Cysts with Diverse Radiological Presentation Highlighting Diagnostic Challenges. Diagnostics.2022;12(8):2006. 10.3390/diagnostics12082006 [DOI] [PMC free article] [PubMed]
- 12.Agrawal, N, Singh, V, & Manandhar, A Interdisciplinary approach to treat a large trauma-induced chronic periapical pathology: A clinical report. International Journal of Advanced Research, 2014; 2(5): 211–217. [Google Scholar]
- 13.Pei J, Zhao S, Chen H, Wang J. Management of radicular cyst associated with primary teeth using decompression: aretrospective study. BMC Oral Health. 2022;22:560. 10.1186/s12903-022-02638-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kumaravelu R, Jude NJ, Sathyanarayanan R. Radicular Cyst: A Case Report. J Sci Dent. 2021;11(1):23–25. https://doi.org/10.5005/jp-journals-10083-0939 [Google Scholar]
- 15.AlRowis RM, Alzahrani AH, Alzuhair SH et al. Assess the Association Between Periodontitis and Maxillary Sinusitis: A Cross-Sectional Cone-Beam Computerized Tomography (CBCT) Study. Cureus.2023;15(11):e48587. 10.7759/cureus.48587 [DOI] [PMC free article] [PubMed]
- 16.Boyle RL, Psoter KJ, Merlo CA, et al. Prevalence and risk factors for low bone Mineral density in adults with cystic fibrosis. JBMR Plus. 2022;6(11):e10666. 10.1002/jbm4.10666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.AL-Rammahi HM, Chai WL, Nabhan MS, et al. Root and canal anatomy of mandibular first molars using micro-computed tomography: a systematic review. BMC Oral Health. 2023;23:339. 10.1186/s12903-023-03036-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Gonçalves TOF, Rangel RMR, Marañón-Vásquez GA et al. Management and recurrence of the odontogenic keratocyst: an overview of systematic reviews. Oral Maxillofac Surg. 2024 Jul. 10.1007/s10006-024-01277-4. PMID: 38954313. [DOI] [PubMed]
- 19.Aiba H, Kobayashi M, Waguri-Nagaya Y, et al. Treatment of aneurysmal bone cysts using endoscopic curettage. BMC Musculoskelet Disord. 2018;19:268. https://doi.org/10.1186/s12891-018-2176-6. [DOI] [PMC free article] [PubMed]
- 20.Titinchi F. Novel recurrence risk stratification of odontogenic keratocysts: A systematic review. Oral Diseases. 2021;27(8): https://doi.org/10.1111/odi.13931. [DOI] [PubMed]
- 21.Allon DM, Allon I, Anavi Y, Kaplan I, Chaushu G. Decompression as a treatment of odontogenic cystic lesions in children. J Oral Maxillofac Surg. 2015;73(4):649–54. 10.1016/j.joms.2014.10.010. [DOI] [PubMed]
- 22.Wuelling M, Vortkamp A. A newly discovered stem cell that keeps bones growing. Nature. 2019;566(7744):639–40. 10.1038/d41586-019-00692-w. [DOI] [PubMed] [Google Scholar]
- 23.Peraza Labrador A. Glandular odontogenic cysts: recurrence patterns and long-term follow-up. Head Neck Pathol. 2023;17(1):292–9. 10.1007/s12105-022-01410-9.37184731 [Google Scholar]
- 24.Titinchi F, Morkel J. Residual cyst of the jaws: A clinico-pathologic study of this seemingly inconspicuous lesion. PLOS ONE, 2020;15(12), e0244250. https://doi.org/10.1371/journal.pone.0244250. [DOI] [PMC free article] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.