Abstract
The advent of acoustically responsive nanodrugs that are specifically optimized for sonodynamic therapy (SDT) is a novel approach for clinical applications. Examining the therapeutic applications of sono-responsive drug delivery systems, understanding their dynamic response to acoustic stimuli, and their crucial role in enhancing targeted drug delivery are intriguing issues for current cancer treatment. Specifically, the suggested review covers SDT, a modality that enhances the cytotoxic activity of specific compounds (sonosensitizers) using ultrasound (US). Notably, SDT offers significant advantages in cancer treatment by utilizing US energy to precisely target and activate sonosensitizers toward deep-seated malignant sites. The potential mechanisms underlying SDT involve the generation of radicals from sonosensitizers, physical disruption of cell membranes, and enhanced drug transport into cells via US-assisted sonoporation. In particular, SDT is emerging as a promising modality for noninvasive, site-directed elimination of solid tumors. Given the complexity and diversity of tumors, many studies have explored the integration of SDT with other treatments to enhance the overall efficacy. This trend has paved the way for SDT-based multimodal synergistic cancer therapies, including sonophototherapy, sonoimmunotherapy, and sonochemotherapy. Representative studies of these multimodal approaches are comprehensively presented, with a detailed discussion of their underlying mechanisms. Additionally, the application of audible sound waves in biological systems is explored, highlighting their potential to influence cellular processes and enhance therapeutic outcomes. Audible sound waves can modulate enzyme activities and affect cell behavior, providing novel avenues for the use of sound-based techniques in medical applications. This review highlights the current challenges and prospects in the development of SDT-based nanomedicines in this rapidly evolving research field. The anticipated growth of this SDT-based therapeutic approach promises to significantly improve the precision of cancer treatment.
Keywords: sonodynamic therapy, ultrasound, synergistic therapy, sonosensitizer, nanomedicine, cancer treatment, acoustic audible wave
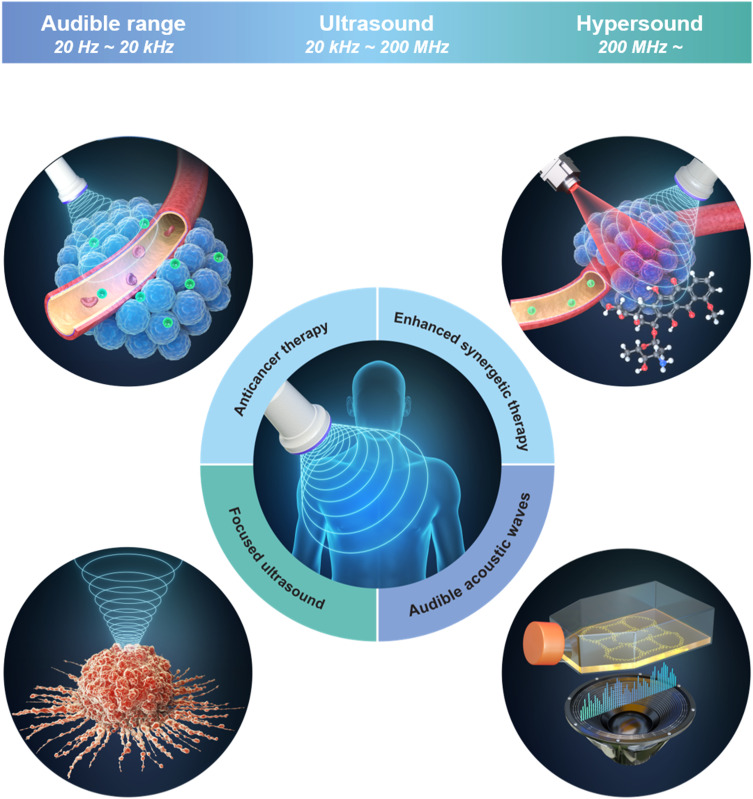
Graphical Abstract
Introduction
Cancer continues to pose a significant threat to human health and longevity, driving the ongoing search for more effective and less harmful treatments. Traditional cancer therapies, such as surgical tumor resection, chemotherapy, radiotherapy, and immunotherapy, remain essential pillars of oncological care.1,2 Although these treatments can be effective, they are often accompanied by substantial side effects that negatively impact a patient’s quality of life. For instance, surgery may lead to complications and disrupt the functioning of healthy organs, particularly in cases involving deep-seated or inoperable tumors.3 Moreover, the inability of surgery to eliminate microscopic residual tumor cells necessitates the adjunctive use of chemotherapy and radiotherapy. While these therapies target cancer cells, they also harm healthy tissues and may promote resistance in cancer cells.4 This resistance often leads to the survival and proliferation of cancer cells with mutations, making subsequent therapies less effective and contributing to disease recurrence or progression.5–9
Non-targeted agents used alongside chemotherapy and radiotherapy can also cause various adverse effects, which may range from acute symptoms such as nausea and hair loss to long-term consequences like organ damage and secondary cancer. Likewise, immunotherapies that aim to engage the immune system of the body in fighting cancer may trigger dysregulated immune responses, potentially resulting in autoimmune disorders or cytokine release syndrome.10–14
Given these challenges, there is growing interest in developing alternative therapeutic strategies that selectively target tumor cells while sparing healthy tissues. Among these approaches, photodynamic therapy (PDT), photothermal therapy (PTT), hyperthermia and radiotherapy have emerged as promising techniques. PDT uses photosensitizers and PTT employs photothermal agents, both of which are activated by specific wavelengths of light to induce localized tumor cell death through the production of reactive oxygen species (ROS) or heat.15–17 While PDT and PTT offer advantages such as reduced systemic toxicity and the ability to target specific tumor sites, their clinical applicability is limited by the shallow tissue penetration of light, restricting their use to superficial or endoscopically accessible tumors.18,19 Hyperthermia, which relies on localized heating to kill cancer cells, can be challenging to control, potentially damaging healthy tissues surrounding the tumor.20 Similarly, radiotherapy, though effective in inducing DNA damage to cancer cells, involves ionizing radiation that carries risks such as secondary cancers and long-term tissue damage.21 In contrast, SDT combines the production of ROS with acoustic cavitation, enabling more precise tumor targeting with deeper tissue penetration and fewer side effects. Moreover, SDT utilizes ultrasound waves, eliminating the radiation-related risks associated with radiotherapy. These unique attributes position SDT as a promising alternative to existing non-invasive cancer therapies, offering more versatility and safety in clinical applications.
The unique properties of ultrasound (US), a well-established tool in medical imaging and therapy, present a promising alternative for cancer treatment. Unlike light, US can penetrate deeper into tissues, potentially overcoming the limitations of phototherapy. Sonodynamic therapy (SDT) is an emerging technique that combines US with acoustically sensitive drugs to induce cytotoxic effects at tumor sites. By harnessing the cavitation effect of US, SDT can increase the permeability of cancer cell membranes, facilitating the targeted delivery and activation of therapeutic agents. Additionally, incorporating acoustically responsive nanomaterials into SDT enables precise control of drug release and activation, further minimizing collateral damage to healthy tissues.22,23
The synergistic combination of US and sonosensitizers in SDT not only enhances tumor treatment efficacy but also opens new possibilities for combination therapies. Integrating SDT with conventional therapies such as chemotherapy, photothermal therapy, and immunotherapy could overcome treatment resistance and lead to more comprehensive tumor eradication. Furthermore, the exploration of acoustically responsive nanomaterials within SDT presents a frontier for innovation, with the development of multifunctional nanoparticles capable of responding to US stimuli for targeted drug delivery and therapy activation.24–26
Despite the potential of SDT, several challenges remain unresolved. These include optimizing the design and synthesis of sonosensitizers for maximum efficacy, understanding the complex interactions between US, sonosensitizers, and biological tissues, and developing protocols for safe and effective clinical application of SDT. Addressing these challenges is essential for fully realizing the potential of SDT as a precise, targeted, and minimally invasive cancer treatment strategy.26–30
Therapeutic Mechanisms of SDT
SDT is a therapeutic approach that utilizes US and its interactions with chemical compounds known as sonosensitizers. The potential mechanisms of SDT include four primary concepts: direct US irradiation, cavitation, ROS generation, and thermal effects.31–34 Direct US irradiation damages or denatures the targeted cancer tissue through high-intensity US beams.31,32 Additionally, combining US with various sonosensitizers has been proposed as a strategy to inhibit tumor growth by inducing cell death via cavitation, ROS generation, and thermal effects. High-intensity focused US (HIFU) primarily operates within the frequency range of 0.8 to 3.3 MHz, using high-energy US to precisely target and treat tumor tissues with minimal collateral damage. Furthermore, SDT employing sonosensitizers typically operates within the frequency range of 0.5 to 3.0 MHz,33,34 which is effective for deep tissue penetration and the generation of ROS and heat, leading to efficient tumor treatment. Acoustically responsive nanoparticles can be engineered to undergo structural transformations or release their payload upon exposure to specific US frequencies and intensities, providing a highly targeted approach to cancer therapy. The release of drugs from acoustically responsive nanoparticles is primarily governed by cavitation and sonoporation. Stable cavitation involves the gentle oscillation of microbubbles at low frequencies, which enhances drug penetration through the tumor vasculature. In contrast, inertial cavitation results from the violent collapse of bubbles, generating mechanical forces that break apart the nanoparticle shell, releasing the encapsulated drug. Additionally, sonoporation temporarily increases the permeability of tumor cell membranes, allowing drugs to infiltrate the tumor tissue more effectively.
US-Direct Irradiation
HIFU therapy transmits energy in the form of US waves through intervening tissues to specific target points within body organs, thereby raising temperature or inducing other biological effects in a completely non-invasive manner. Therapeutic US uses higher energy and intensity compared to diagnostic US, although the fundamental principles of HIFU remain the same as those of conventional US.
The primary mechanisms of HIFU ablation are thermal and mechanical effects. HIFU generates heat by focusing US waves on a precise point within the tissue where the energy is concentrated. This focused energy leads to rapid molecular vibrations, producing frictional heat. The generated heat increases the tissue temperature to over 60 °C, causing coagulation necrosis, effectively destroying tumor cells. The Pennes bioheat transfer equation models the heat generation and transfer process in tissues subjected to HIFU. The equation is as follows:
 |
where the subscripts t and b relate to the tissue and blood phases, respectively. Additionally, ρ, C, k, and T represent the tissue density, specific heat, thermal conductivity, and temperature, respectively.  denotes the capillary bed perfusion rate, and T∞ is the temperature at a distant location from the transducer focal region (typically 37°C).35,36
denotes the capillary bed perfusion rate, and T∞ is the temperature at a distant location from the transducer focal region (typically 37°C).35,36
The mechanical effects of HIFU include microstreaming and cavitation.32,37 Microstreaming refers to the small-scale fluid flow induced by US waves as they travel through tissues, generating shear forces that damage cell structures and promote cell death. Cavitation involves the rapid formation and collapse of bubbles caused by US waves.38 The violent collapse of these bubbles generates high temperatures and pressures, producing strong mechanical shock waves that destroy cells and tissues.39 When the ultrasonic energy is precisely focused on the target area, minimal adverse biological effects are observed in the surrounding tissues. Specific ultrasonic energy levels vary depending on the application, typically determined by the frequency and intensity settings of the US equipment, ensuring energy is concentrated in the intended area to minimize collateral damage. Due to its non-invasive nature, this technology has gained widespread attention from clinicians, researchers, and companies worldwide as a promising, minimally invasive therapeutic tool (Figure 1a).
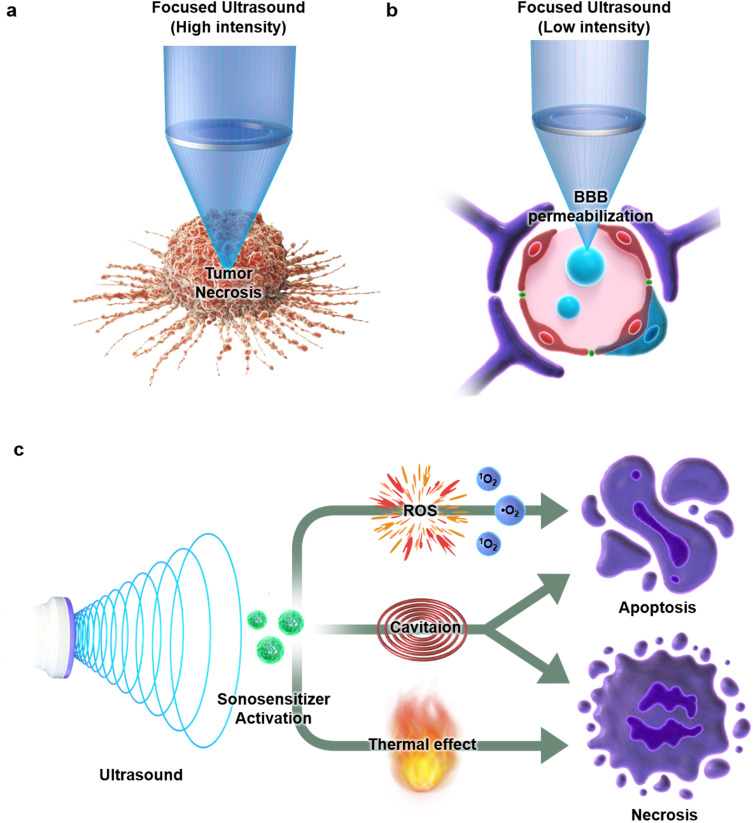
Figure 1.
Therapeutic strategies using ultrasound (US) in cancer treatment include the application of US alone (a and b) or in combination with sonosensitizers (c). The potential mechanisms of sonodynamic therapy (SDT) involve focused US, the production of reactive oxygen species (ROS), hyperthermic damage, and the cavitation effect.
A promising variation of focused US is low-intensity focused US (LIFU). LIFU is an innovative, non-invasive technique used to temporarily and reversibly open the blood-brain barrier (BBB).40–42 This magnetic resonance imaging-guided focused US (MRIgFUS) technique uses low-frequency US combined with gas-filled microbubbles (MBs) to specifically disrupt the BBB.43 MBs, typically composed of lipid-encapsulated carbon fluoride gas, range from 1 to 5 μm in diameter and are inherently echogenic.44,45 They are widely used as contrast agents in US imaging and help target and disrupt the BBB for therapeutic purposes.46 The pressure amplitude for opening the BBB with FUS is kept below 1.5–2 MPa, comparable to diagnostic US, ensuring its safety for use in humans.47 While US is believed to interact with brain tissue to open the BBB through stable and inertial cavitation, the exact mechanisms underlying LIFU-induced BBB opening remain unclear. Stable cavitation occurs when MBs rhythmically expand and contract in low-pressure environments, generating microflows in the surrounding fluid that apply mechanical forces on endothelial cells, temporarily disrupting tight junction proteins. In contrast, inertial cavitation occurs under high-pressure conditions, causing MBs to collapse violently, generating mechanical forces such as shock waves and microjets that perforate cell membranes and increase blood vessel permeability (Figure 1b).40
In summary, HIFU and LIFU are non-invasive therapeutic technologies that leverage US for various medical applications, utilizing high and low intensities, respectively.48 HIFU is primarily used in tumor treatments, involving high-intensity US energy, typically exceeding 1000 W/cm², directed at tumor tissue to increase its temperature and destroy it through a combination of thermal and mechanical effects. This method has demonstrated efficacy in treating several cancers, including prostate and liver cancers.31 In contrast, LIFU is used in neuroscience research and neuromodulation, applying lower intensities, generally below 3 W/cm². Additionally, LIFU facilitates drug delivery by temporarily opening the BBB, making it valuable for studying brain functions and treating neurological disorders.49 Ongoing research suggests that these technologies have broad potential for medical applications, promising significant advancements in non-invasive therapeutic methods.
SDT Induced by Sonosensitizers
Sonosensitizers optimize the therapeutic impact of US irradiation, playing a crucial role in SDT. These compounds absorb energy from US waves, converting it into localized ROS, which are vital in triggering apoptosis in cancer cells.29 ROS can disrupt cellular structures, damage DNA, and initiate biochemical cascades that lead to programmed cell death.50,51 In recent decades, sonosensitizers have been rapidly developed based on their role in SDT-induced cell apoptosis.
The development of effective sonosensitizers is essential for enhancing the therapeutic efficacy of SDT. Current research focuses on two main types of sonosensitizers: organic and inorganic. Organic sonosensitizers, often derived from natural compounds or synthetic analogs, are noted for their biocompatibility and efficient ROS generation.52,53 Conversely, inorganic sonosensitizers, such as metal-based nanoparticles, offer advantages including high stability, functionalization ease, and robust ROS production.54,55 Each type has distinct strengths and limitations, making the selection of the appropriate sonosensitizer crucial in optimizing SDT for cancer treatment.
Furthermore, choosing the appropriate sonosensitizer for SDT in cancer therapy is a major focus of current research. Comparing SDT with other treatment modalities, such as photodynamic therapy (PDT), underscores the importance of this selection. Unlike PDT, which relies on light-sensitive compounds and is limited by light penetration depth, SDT utilizes ultrasound waves that can penetrate deeper into tissues and are less dependent on oxygen levels. This characteristic makes SDT particularly effective in treating deep-seated and hypoxic tumors.56
The integration of these insights into the development and application of sonosensitizers in SDT highlights their potential for significant advancements in cancer therapy. This comprehensive approach enhances our understanding of the underlying mechanisms of SDT and paves the way for more effective and targeted cancer treatments (Figure 1c).
Fundamental Mechanisms of SDT
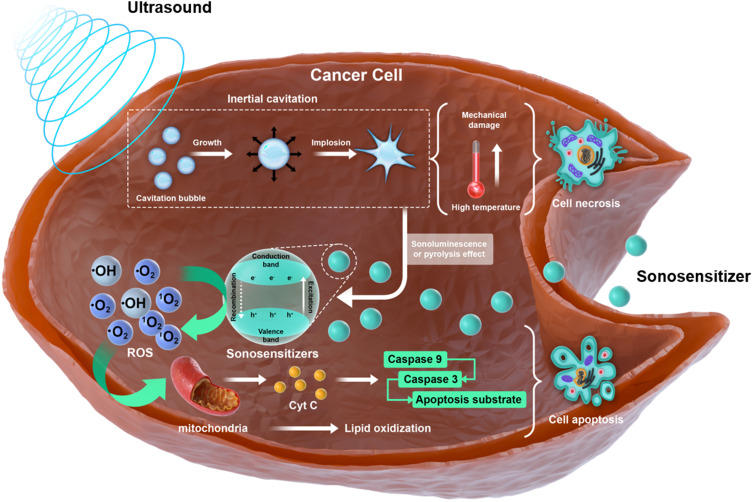
SDT employs a multifaceted approach that involves both biochemical and biophysical interactions to effectively treat cancer (Figure 2). One of the key theories is the oxygen radical theory, which suggests that the primary mechanism of SDT is the generation of ROS through cavitation or US activation of sonosensitizers. ROS, mainly produced by the collapse of US-induced cavitation bubbles, play a critical role in damaging cellular components such as DNA, proteins, and lipids, thereby inducing apoptosis in cancer cells.56 Furthermore, processes such as pyrolysis and sonoluminescence significantly enhance ROS production, further inhibiting tumor growth by promoting cellular oxidative stress. Pyrolysis involves the decomposition of materials due to localized heating generated by US waves, leading to the breakdown of chemical bonds and the formation of reactive radicals, which subsequently interact with oxygen to produce ROS.57 In contrast, sonoluminescence occurs during the collapse of microscopic gas bubbles formed by cavitation. The extreme conditions within these collapsing bubbles lead to the emission of light and the dissociation of molecules, generating additional ROS that contribute to oxidative damage in tumor cells.30 Simultaneously, the cavitation effect theory explains the physical phenomena triggered by US, emphasizing the dynamic process of cavitation, which involves the formation, growth, and implosion of bubbles within the liquid medium.23 This process includes two main types of gas oscillation: stable (non-inertial) cavitation and inertial (transient) cavitation. In stable cavitation, bubbles oscillate in size around an equilibrium radius over many cycles of US waves without collapsing, typically occurring at US frequencies ranging from 20 to several hundred kHz. In contrast, inertial cavitation involves bubbles growing significantly during the negative pressure phase and then collapsing violently during the positive pressure phase, usually at frequencies ranging from 20 kHz to several MHz. This activity not only supports ROS generation by creating the physical conditions necessary for cavitation but also directly disrupts cellular structures. The mechanical forces generated by rapid bubble collapse produce high temperatures and pressures, leading to mechanical damage to cell membranes and subsequent cell necrosis. Additionally, US-induced cavitation enhances drug penetration and distribution by disrupting adjacent cell membranes, thereby facilitating the therapeutic effects of co-administered drugs.58–60 Post-SDT morphological changes in cancer cells include the disappearance of microvilli, vacuolation of cell membranes, cell shrinkage, and cytoskeletal alterations. These changes align with the observed increase in apoptotic/necrotic ratios and significant post-treatment mitochondrial dysfunction, indicating the involvement of both ROS-mediated and mechanical damage pathways. ROS-induced damage leads to mitochondrial dysfunction, including the opening of the mitochondrial permeability transition pore (MPTP), which results in the release of cytochrome c into the cytosol. Cytochrome c binds to Apaf-1 and adenosine triphosphate (ATP), forming an apoptosome complex that activates pro-caspase-9. Activated caspase-9 then cleaves and activates caspase-3, a key executioner caspase responsible for the cleavage of various cellular substrates, leading to programmed cell death. Additionally, lipid peroxidation and the downregulation of antioxidant enzymes have been observed, illustrating the extensive impact of SDT on cellular functions.54,61–63
Figure 2.
Mechanisms underlying sonodynamic therapy (SDT) include: 1) cavitation effects induced by ultrasound (US) and 2) the generation of reactive oxygen species (ROS), as depicted in this figure. The predominant and widely accepted mechanism is ROS production, triggered by either pyrolysis or sonoluminescence.
Overall, SDT efficacy arises from a dual mechanism: the chemical effects mediated by ROS and the physical effects resulting from the mechanical forces of cavitation. Together, these effects lead to the comprehensive disruption of cancer cells through oxidative stress and direct physical damage, culminating in tumor regression and cell death. This integrated approach demonstrates that SDT is a potent therapeutic modality that leverages the synergistic effects of both biochemical and biophysical processes.64
Organic Sonosensitizer-Based SDT
Sonosensitizers can be classified as either inorganic or organic. Both types share the ability to be activated by US irradiation to generate ROS, a critical factor in the efficacy of SDT. However, they differ significantly in their properties and applications. Organic sonosensitizers, like their photosensitizer counterparts, are activated by US irradiation to generate ROS through sonoluminescence or sono-chemical pyrolysis.65,66 Generally, photosensitizers can also function as sonosensitizers, with the molecular design of the latter derived from the former.67 Compared to inorganic sonosensitizers, organic ones typically exhibit a higher capability to generate ROS when activated from the ground state to the excited state under US. This characteristic has made organic sonosensitizers widely utilized in SDT research.68 However, conventional organic sonosensitizers face limitations, such as poor water solubility, low chemical stability, and inadequate tumor targeting, which reduce their therapeutic efficacy and hinder SDT development. 69 Conversely, while inorganic sonosensitizers often demonstrate better chemical stability and water solubility, they may have different activation mechanisms and generally produce lower levels of ROS compared to their organic counterparts. Inorganic sonosensitizers may include materials like metal oxides, which can also be activated by US to generate ROS, albeit through different pathways, such as electron-hole pair generation.54,55,70
Organic sonosensitizers can be categorized into four types: porphyrin derivatives, cyanine derivatives, nanoliposomal sonosensitizers, and semiconducting polymer sonosensitizers. These compounds offer several advantages, including high biocompatibility, excellent biodegradability, strong tumor-targeting potential, and ease of metabolism by the liver or kidneys in living organisms, making them highly promising for biomedical applications.53,71
Porphyrin derivatives have been extensively used in SDT due to their strong activity under ultrasonic stimulation. Hematoporphyrin (HP), the first sonosensitizer identified among porphyrins, was found to synergistically inhibit tumor growth through the production of singlet oxygen (1O2) when ultrasonically activated. Since then, various porphyrins and their analogs, including hematoporphyrin monomethyl ether (HMME), protoporphyrin IX (PpIX), chlorin e6 (Ce6), sinoporphyrin sodium (DVDMS), tetra-α-(3-carboxyphenoxyl) zinc(II) phthalocyanine (ZnPcC4), and di-sulfo-di-phthalimidomethyl phthalocyanine zinc (ZnPcS2P2), have been utilized in SDT.72–75 Porphyrin-derived sonosensitizers possess an 18-π aromatic macrocycle carbon core structure and are highly effective at generating ROS under US irradiation. Nevertheless, their application in SDT is significantly limited by their poor water solubility, biosafety concerns, and low tumor-targeting efficiency, necessitating the development of porphyrin-based nanomedicines with enhanced circulation and targeting capabilities.67,76
Recently, cyanine-based organic sonosensitizers, including indocyanine green (ICG), IR780, trifluoromethyl-heptamethine cyanine, and platinum(II)-cyanine complexes, have been applied in cancer sono-immunotherapy.77–79 Heptamethine cyanine dyes are small organic molecules characterized by heterocyclic nitrogen atoms at both ends and a long conjugated methine chain, with strong absorption bands in the 700–900 nm range.68 Indocyanine green (ICG), the first heptamethine cyanine dye approved by the US Food and Drug Administration (FDA) for use in angiography, offers significant benefits for clinical diagnostics and scientific research.80 Moreover, newly developed heptamethine cyanine dyes, such as IR780, IR783, IR808, and MHI-148, exhibit a high molar absorption coefficient, strong fluorescence quantum yield, and excellent sonodynamic properties,81 making them highly promising in the development of sonosensitizers and photothermal agents (PTAs).82 However, due to poor biocompatibility, introducing trifluoromethyl groups, which enhance membrane permeability, metabolic stability, and bioavailability, may be necessary.83
Semiconducting polymer nanoparticles (SPNCs), a novel class of organic sonosensitizers derived from highly π-electron delocalized semiconducting polymers, exhibit high biocompatibility, significant chemical flexibility, and adjustable sizes.84 SPNCs have been studied for various biomedical applications, such as optical imaging,85 phototherapy, and biological regulation.86 An SPNC that synergistically enhances tumor penetration and alleviates tumor hypoxia has been reported for SDT in large solid tumors. This SPNC consists of a semiconducting polymer nanoparticle core coated with polyethylene glycol as a sonodynamic converter. Catalase, an oxygen-modulating enzyme, is efficiently conjugated to the nanoparticle surface via a coupling reaction. The smallest SPNC (SPNC1) efficiently penetrates tumor tissue, alleviates hypoxia, and generates sufficient singlet oxygen to eradicate tumor cells at deep tissue levels upon US irradiation, significantly improving antitumor efficacy.53,65,87,88
Nanoliposomes, often selected as carriers, are essential for improving the bioaccumulation and stability of sonosensitizers at target sites. Composed primarily of phospholipids with bilayer structures, nanoliposomes are efficient drug carriers. For instance, liposome-encapsulated artemether (LEA) has shown notable sonodynamic anticancer activity.89,90 Compared to artemether alone, SDT mediated by LEA demonstrated a stronger antiproliferative effect on HepG2 cells. In another innovative study, Li et al designed a liposome-microbubble complex loaded with the sonosensitizer DVDMS (DLMBs) to target breast cancer. Under US-induced cavitation, DLMBs released their payload, enhancing DVDMS cellular uptake and tumor penetration, thereby improving SDT efficacy.67,91 Table 1 outlines the various categories of organic sonosensitizers.
Table 1.
Categories of Organic Sonosensitizers
| Category | Sonosensitizer | Key Features | Limitations |
|---|---|---|---|
| Porphyrin Derivatives | Hematoporphyrin, HMME, PpIX, Ce6, DVDMS, ZnPcC4, ZnPcS2P2 | High ROS generation capability under ultrasound (US), 18-π aromatic macrocycles, excellent sonodynamic activity | Poor water solubility, high biosafety concerns, low tumor-targeted accumulation |
| Cyanine Derivatives | ICG, IR780, trifluoromethyl-heptamethine cyanine, platinum(II)–cyanine complex | Intense absorption bands in 700–900 nm, approved for clinical use, high molar absorption coefficient, good sonodynamic activity | Poor biocompatibility, need for modifications to improve membrane permeability and metabolic stability |
| Semiconducting Polymeric nanoparticles | SPNCs | High biocompatibility, high chemical flexibility, tunable sizes, efficient tumor penetration, alleviates tumor hypoxia | Complex synthesis process, need for optimization in clinical applications |
| Nanoliposome Sonosensitizers | LEA, DLMBs | Enhances bioaccumulation and stability of sonosensitive molecules, effective drug carriers, improved antiproliferative effect | Potential for immune response, stability of encapsulated drugs, scalability of production |
Abbreviations: HMME, hematoporphyrin monomethyl ether; PpIX, protoporphyrin IX; Ce6, Chlorin e6; DVDMS, sinoporphyrin sodium; ZnPcC4, tetra-α-(3-carboxyphenoxyl) zinc(II) phthalocyanine; ZnPcS2P2, di-sulfo-di-phthalimidomethyl phthalocyanine zinc; ICG, indocyanine green; IR780, trifluoromethyl-heptamethine cyanine; SPNCs, Semiconducting polymer nanoparticles; LEA, Liposome-encapsulated artemether; DLMBs, DVDMS-loaded microbubbles.
Inorganic Sonosensitizer-Based SDT
Inorganic materials demonstrate rapid metabolism, low toxicity, and high stability compared to organic materials. Their unique structures, compositions, and multifunctionality make inorganic micro- and nanomaterials a promising platform for SDT. Sonosensitizers are classified into two categories based on their primary components: metal-based and non-metallic.
TiO2 nanoparticles are widely used in food, cosmetic, energy, and environmental protection industries because of their semiconductor properties. Their narrow bandgap (3.2 eV) and excellent biocompatibility make them suitable for a variety of applications. When exposed to UV irradiation, electrons in the valence band of TiO2 nanoparticles are excited to the conduction band, where they interact with surrounding oxidizing agents (O2 and H2O) to generate reactive oxygen species (ROS), such as •OH, O2−, H2O2, or other active substances. This property has led to their use in tumor photodynamic therapy. However, TiO2 nanoparticles activated by UV irradiation have limited tissue penetration, restricting their photodynamic therapy applications. Recent studies have shown that TiO2 nanoparticles activated by US effectively kill tumor cells, resulting in extensive research into their use as key sonosensitizers.92 GNR-PEG, a commonly used photosensitizer, underscores the potential of TiO2 nanoparticles as sonosensitizers, as they are generally non-toxic to experimental cells or animals.93 However, bare TiO2 nanoparticles are unstable and tend to be cleared rapidly by the reticuloendothelial system, which limits their accumulation in tumor areas and reduces their therapeutic efficacy. To address this issue, surface modifications using high-polymer materials such as proteins, glucans, and polyionic complexes have been implemented to enhance their stability. Moreover, biomimetic cell membrane-based nanocomposite structures have been developed to improve both stability and tumor-targeting ability. By coating nanoparticles with cancer cell membranes (CM), a C-TiO2/TPZ@CM composite sonosensitizer was created, enabling tumor targeting through homologous binding via CM components.94
In addition to TiO2 nanoparticles, transition metal oxide nanomaterials can also serve as sonosensitizers when activated by US irradiation. Nanoparticles of transition metal oxides, such as Fe3O4 (magnetite) and Fe2O3 (maghemite), have garnered significant attention due to their superparamagnetic properties and role in Fenton reactions.95 To improve therapeutic outcomes, Shen et al developed a core-shell sonosensitizer comprising an Fe3O4 nanoparticle core and a TiO2 shell loaded with doxorubicin (DOX). The Fe3O4@TiO2-DOX nanoparticles generated substantial amounts of ROS for SDT.96 Under US irradiation, the nanostructure released DOX, which synergistically worked with SDT to destroy cancer cells. A recent study reported a sonosensitizer (MnWOx-PEG) that demonstrated highly efficient US-triggered production of 1O2 and •OH.97
Noble metal nanoparticles, such as Au, Ag, and Pt, have also gained attention as effective sonosensitizers due to their stability, water solubility, lack of skin photosensitivity, and inherent acoustic cavitation properties. Incorporating noble metals such as Au, Ag, and Cu into nanomaterials enhances SDT efficacy by reducing electron-hole recombination and increasing ROS production.98 Among these, Au nanoparticles are notable for their remarkable sonodynamic activity, biocompatibility, adjustable surface properties, and efficient photothermal conversion, making them a focus of sonosensitizer research.57,99 These metals naturally promote cavitation under US irradiation, with Au nanoparticles being particularly advantageous for cancer therapy due to their ease of synthesis and surface modifiability. Recent studies have highlighted the acoustic cavitation effects of Au nanoparticles on colon cancer, showing that the uneven surfaces of these nanoparticles act as nucleation sites for cavitation, reducing the cavitation threshold.100 Modifications of Au nanoparticles, such as functionalization with δ-aminolevulinic acid (ALA) or PPIX, have been shown to significantly boost therapeutic efficacy by increasing singlet oxygen production and enhancing the SDT effect through plasmon resonance and cavitation.101,102 The various categories of inorganic sonosensitizers are summarized in Table 2. Compared to organic sonosensitizers, inorganic alternatives offer enhanced biocompatibility, stability, and multifunctionality, with their distinct chemical and physical properties enabling synergistic combinations that significantly improve SDT effectiveness.
Table 2.
Categories of Inorganic Sonosensitizers
| Category | Sonosensitizer | Key Features | Limitations |
|---|---|---|---|
| Metal-based Sonosensitizers | TiO2 nanoparticles | High ROS generation under US, good biocompatibility, used in tumor photodynamic therapy | Limited tissue penetration under UV activation, easy electron-hole recombination, poor stability without surface modification |
| Transition metal oxides | Fe3O4, Fe2O3, MnWOx | Superparamagnetic properties, Fenton reaction, can be combined with other materials to enhance ROS production | Complex synthesis and stability issues, potential toxicity |
| Noble metal nanoparticles | Au, Ag, Pt, Cu-based nanoparticles | Exceptional stability, water solubility, intrinsic acoustic cavitation properties, high biocompatibility, efficient photothermal conversion | High cost, the potential for aggregation, requires surface modifications for optimal use |
Abbreviations: TiO2, titanium dioxide; Fe3O4, magnetite; Fe2O3, maghemite; MnWOx, Manganese oxide catalyst.
Therefore, developing biocompatible sonosensitizers with robust ROS generation capabilities remains essential. Innovations in sonosensitizer design aim to overcome current limitations by combining the strengths of both inorganic and organic materials, enhancing ROS production while improving stability, solubility, and tumor-targeting efficiency.
Organic-Inorganic Hybrid Sonosensitizer-Based SDT
The utilization of organic-inorganic hybrid sonosensitizers in SDT confers distinctive advantages, primarily due to their capacity to augment ROS generation, enhance biocompatibility, and maintain stability under physiological conditions. These hybrid materials are composed of both organic and inorganic components, offering a unique combination of properties. Organic sonosensitizers are typically renowned for their high biocompatibility and reduced systemic toxicity. However, they may exhibit limitations in ROS generation and stability. Inorganic components, such as metal-based nanoparticles, address these limitations by enhancing ROS production and improving the overall stability of the system. This combination enables a more controlled and efficient therapeutic response in cancer treatment. One experimental example of this approach is the use of metal-organic frameworks (MOFs), which have demonstrated promising results in enhancing the therapeutic efficacy of SDT. MOF-based hybrid sonosensitizers exploit the structural characteristics of inorganic metals to generate a substantial ROS response under US activation, while simultaneously benefiting from the biocompatibility of organic ligands. A study utilizing MOF sonosensitizers demonstrated enhanced ROS generation and prolonged retention in tumor tissues, resulting in improved tumor suppression in vivo models.103,104 Similarly, hollow mesoporous organosilica nanoparticles (HMONs) have also shown significant potential as organic-inorganic hybrid sonosensitizers. In one study, HMONs were loaded with protoporphyrin IX (PpIX) as the organic sonosensitizer and doxorubicin (DOX) as the chemotherapeutic agent. The hybrid system took advantage of the high surface area and mesoporous structure of HMONs, leading to enhanced ROS production under US irradiation. Furthermore, the organic components improved biocompatibility and responsiveness to the tumor microenvironment, while the inorganic silica matrix provided structural stability and controlled drug release. This combined approach resulted in synergistic effects in both in vitro and in vivo models, significantly improving tumor suppression through the dual action of SDT and chemotherapy.105 This demonstrates how hybrid materials not only bridge the gap between organic and inorganic sonosensitizers but also significantly enhance therapeutic outcomes in SDT applications. Table 3 outlines the comparing organic, inorganic, and organic-inorganic hybrid sonosensitizers with detailed focus on ROS generation capacity, biocompatibility, flexibility and toxicity.
Table 3.
Comparison of Organic, Inorganic, and Organic-Inorganic Hybrid Sonosensitizers
| Category | Organic Sonosensitizers | Inorganic Sonosensitizers | Organic-Inorganic Hybrid Sonosensitizers |
|---|---|---|---|
| ROS Generation Capacity | Moderate (limited ROS generation) | High (strong ROS generation from metal nanoparticles) | High (enhanced ROS from combined organic-inorganic components) |
| Biocompatibility | High (derived from natural molecules, low toxicity) | Moderate (metal-based nanoparticles, potential toxicity) | High (improved biocompatibility due to organic component) |
| Stability | Low (rapid degradation, poor stability in vivo) | High (chemically stable, slow degradation in the body) | High (enhanced stability from inorganic components) |
| System Design Flexibility | Limited (difficult to modify structure) | High (wide range of inorganic nanoparticle designs) | High (flexible design, enhanced functionality through combination) |
| Toxicity | Low (derived from natural materials, low systemic toxicity) | Moderate (potential toxic by some metal nanoparticles) | Moderate (toxicity from inorganic part, mitigated by organic component) |
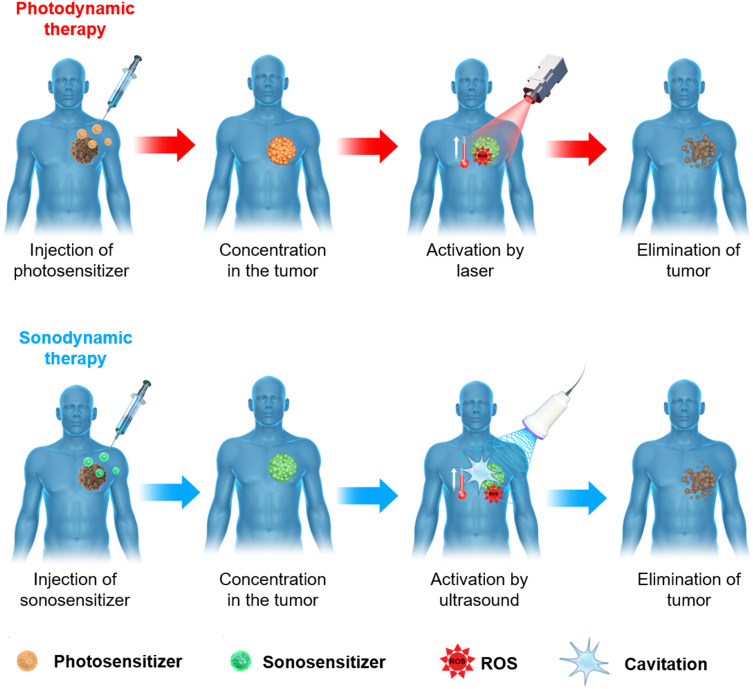
Comparison Between SDT and PDT
SDT and PDT are innovative cancer treatments that differ significantly in their mechanisms and applications. PDT relies on light activation to generate ROS, requiring direct light exposure and being heavily dependent on tissue oxygen levels.15,17,19,106 This dependence limits the effectiveness of PDT in treating deep-seated tumors and hypoxic tumor environments, where light penetration and oxygen are insufficient. In contrast, SDT uses US waves, which can penetrate deeper into tissues and are less reliant on oxygen, making it particularly effective in treating deep-seated and hypoxic tumors (Figure 3).107,108
Figure 3.
A general outline of photodynamic therapy (PDT) and sonodynamic therapy (SDT) in cancer treatment involves the administration of photo- and sonosensitizers, which can be delivered throughout the body or directly into the tumor. Activation occurs via laser for PDT and ultrasound for SDT, leading to the reduction or, ideally, complete elimination of cancerous tissue.
In SDT, US waves induce thermal effects through a process known as cavitation, where the rapid collapse of bubbles results in localized high temperatures and pressures, leading to cellular damage and necrosis. Similarly, PDT can also produce thermal effects; light-activated photosensitizers generate localized heat, along with ROS, both contributing to tumor cell destruction.109,110
Both PDT and SDT effectively destroy tumor cells through their distinct mechanisms.111 However, the ability of SDT to produce ROS with minimal oxygen dependence gives it a clear advantage in hypoxic tumor environments where PDT may be less effective. The combination of chemical damage (via ROS generation) and physical damage (through thermal and mechanical effects) makes SDT a highly adaptable and potent therapeutic option.112,113 Furthermore, SDT can be enhanced using targeted delivery systems to increase specificity and minimize side effects. Significant advancements have been made in developing sonosensitizers activated specifically by US.26 These sensitizers can be tailored to target tumor cells more accurately, optimizing therapeutic outcomes while reducing damage to healthy tissues. Although PDT also uses photosensitizers to target tumor cells, its efficacy is limited by the need for light exposure and adequate oxygen levels.114
In summary, while PDT is well-suited for treating superficial tumors via light activation, SDT offers a more versatile treatment approach that can penetrate deeper into tissues and function effectively in hypoxic conditions. Ongoing research and technological advancements are expected to refine SDT further, leading to improved patient outcomes and expanding the potential of this promising cancer therapy. The following sections explore combination therapy strategies and their potential to enhance cancer treatment by integrating the mechanisms of SDT and PDT. Leveraging their complementary strengths may yield a more comprehensive and effective cancer treatment approach, offering new hope for managing challenging tumor types.
SDT-Derived Synergistic Therapy
Cancer is a heterogeneous disease characterized by rapid and uncontrolled progression, making it difficult for SDT alone to effectively suppress tumors. Consequently, the approach to SDT-based cancer therapy has shifted from monotherapy to multimodal therapy to enhance treatment effectiveness.115 Comprehensive treatment strategies are being developed by combining SDT with chemotherapy, PTT, and immunotherapy, aiming to overcome the limitations of monotherapy and offer more effective, long-lasting cancer treatments (Table 4). The synergistic potential of these multimodal therapies shows great promise for improving clinical outcomes and enhancing the quality of life for cancer patients. Clinical trials have investigated the combination of SDT with these treatment modalities, yielding promising results in improving therapeutic efficacy and minimizing side effects. For example, the integration of SDT with chemotherapy has led to increased drug uptake and improved tumor reduction in preclinical models.116 Similarly, combining SDT with PTT has demonstrated synergistic effects in tumor ablation, while adding immunotherapy has been found to enhance the anti-tumor immune response, potentially leading to more sustained cancer control.117,118
Table 4.
Synergistic Effects of SDT-Derived Therapies with Chemotherapy, Photothermal Therapy, and Immunotherapy
| Synergistic Treatment | Mechanism of Action | Key Advantages | Unique Feature |
|---|---|---|---|
| Chemotherapy | Enhances drug delivery via sonoporation | Lowers drug dose and side effects | Overcomes drug resistance |
| Photothermal Therapy | Heat combined with SDT-induced ROS | Improves tumor destruction | Dual effect: Heat and ROS |
| Immunotherapy | Stimulates immune response with ROS | Boosts immune system activation | Supports long-term immune memory |
SDT Combination with Chemotherapy
Despite the significant benefits that many chemotherapeutic regimens have provided to patients in recent years, the increasingly recognized adverse effects resulting from the off-target actions of conventional chemotherapy have spurred the search for more effective treatment options. Even highly targeted molecular therapies have exhibited off-target effects that contribute to the development of drug resistance.119,120 SDT can enhance the uptake of chemotherapeutic drugs into cancer cells and promote their distribution throughout poorly vascularized solid tumors due to its sonoporation effect. As a result, SDT plays a crucial role in sensitizing tumors to chemotherapy, allowing for a reduced dose of the chemotherapeutic drug to achieve a cytotoxic effect.121
Liu et al designed multifunctional nanoparticles (HPDF) with a core-shell structure incorporating hematoporphyrin (HP, a sonosensitizer), doxorubicin (DOX), and pluronic F68 as the encapsulation agent.122 The hydrophobic components, HP and DOX, formed the core of the nanoparticles through π-π stacking, while the hydrophilic pluronic F68 created the shell. The average diameter of the HPDF nanoparticles was approximately 87.9 nm, enabling them to accumulate in tumors via enhanced permeability and retention (EPR) effects. Pluronic F68 inhibits the efflux activity of adenosine triphosphate (ATP)-binding cassette transporters by depleting ATP,123 which increases the sensitivity of multidrug-resistant HepG2 cells to DOX. Additionally, when combined with SDT, the resulting ROS damage the mitochondria, further reversing multidrug resistance by downregulating ATP levels.124 The viability of HepG2 cells was almost eliminated by the combined effects of DOX-induced DNA damage and ROS production from HP-mediated SDT. Consequently, the growth of HepG2-derived tumors in mice was significantly inhibited following intravenous injection of HPDF nanoparticles and subsequent US irradiation.52
O2-loaded microbubbles (O2MB) can act as carriers for delivering sonosensitizers (RB) and antimetabolic drugs (5-fluorouracil, 5-FU). Callan et al developed O2MB-RB and O2MB-5-FU using avidin-biotin binding interactions.125 The combined SDT and antimetabolite treatment produced significant cytotoxic effects in three different pancreatic cancer cell lines, with similar results observed in a xenograft mouse model. Therefore, O2MB-based therapy, when combined with antimetabolite drugs, may enhance the efficiency of SDT and reduce the side effects associated with systemic antimetabolite administration.
Gemcitabine, a widely used antineoplastic agent, is particularly effective in treating pancreatic cancer and is suitable for encapsulation within O2MB nanoparticles. Both in vitro and in vivo studies have demonstrated that chemo-SDT following the US-targeted microbubble destruction (UTMD) of O2MB-Gem and O2MB-RB serves as an effective and targeted approach for treating pancreatic cancer.126 Moreover, the biosafety of O2MB-Gem was assessed in a healthy mouse model, with no significant renal or hepatic damage observed. The inclusion of superparamagnetic iron oxide nanoparticles (MAG-Lipid) in the preparation of O2MB resulted in the creation of magnetically responsive microbubbles (MagO2MBs), which were used to deliver RB and 5-FU to pancreatic tumors. The application of an external magnetic field to the tumor site enhanced the accumulation of MagO2MB-RB and MagO2MB-5-FU in the tumor regions, further improving the therapeutic effect of the combined chemotherapy and SDT regimen.127
SDT Combination with PTT
NIR-responsive photosensitizers have been widely applied in PDT to address penetration depth issues; however, the efficiency of PDT in deep-seated tumors still requires improvement.128 For skin tumors, necrotic epidermis and deposited pigments can further reduce light penetration, diminishing the therapeutic efficacy of PDT.129 The combination of SDT and PDT can overcome these challenges by utilizing the deep penetration of US. When SDT is enhanced by catalysis and combined with photothermal effects, it nearly achieves complete tumor inhibition while maintaining a favorable biosafety profile.130 For example, combining SDT with PDT takes advantage of the deep tissue penetration of US and the surface-targeting abilities of light-based therapy, potentially addressing the limitations of each method when used alone.117 Innovative approaches, such as mesoporous silica nanoparticles activated by HIFU, are being developed to enhance US applications and generate substantial thermal effects for tumor ablation.131 Furthermore, recent studies have utilized biodegradable PLGA as a carrier to encapsulate ICG and HP, forming NPs with an average diameter of 200–270 nm for SDT and PDT. Cytotoxic effects of these NPs were observed both in vitro and in vivo, with spectrophotometric analysis confirming efficient HP and ICG encapsulation.132
There is growing recognition that combining SDT with PTT or PDT, which generates both toxic ROS and heat, can effectively lower the required concentration of sensitizers while enhancing tumor cytotoxicity. Studies have reported the initial combination of SDT and PTT using AuNPs as sensitizers, with tumor-bearing mice showing significantly longer survival times when treated with NIR, US, and Au nanoparticles, compared to those receiving only monotherapy (NIR or US).133,134 Encouraged by these promising results, numerous sonosensitizers with strong photothermal conversion capabilities have been developed over recent decades. Gao et al reported a TiO2-coated Au nanoplate (Au NPL@TiO2) for synergistic PTT/SDT therapy.135 Modifying TiO2 shells on the surface of 2D Au NPLs led to Au NPL@TiO2 nanoagents displaying a red shift in the optical window from the NIR I to the NIR II region, achieving a remarkable photothermal conversion efficiency of 42.05% under 1064 nm laser irradiation. These metal-semiconductor nanoagents created a charge transfer channel at the Au NPL@TiO2 interface, effectively suppressing the recombination of electrons (e−) and holes (h+) generated by TiO2 under US, thus significantly enhancing ROS production (1.5 W cm−2, 3 MHz). This synergistic anticancer treatment reduced cell viability to 20.3% in vitro and eliminated tumors in vivo.135 The combination of PTT and SDT has demonstrated superior anticancer efficacy under laser and US irradiation. Therefore, it is crucial to develop technologies that achieve the combined therapeutic effects of SDT and PTT while maintaining low toxicity, efficient targeting, and high photothermal-sonodynamic conversion.68
SDT-Enhanced Immunotherapy
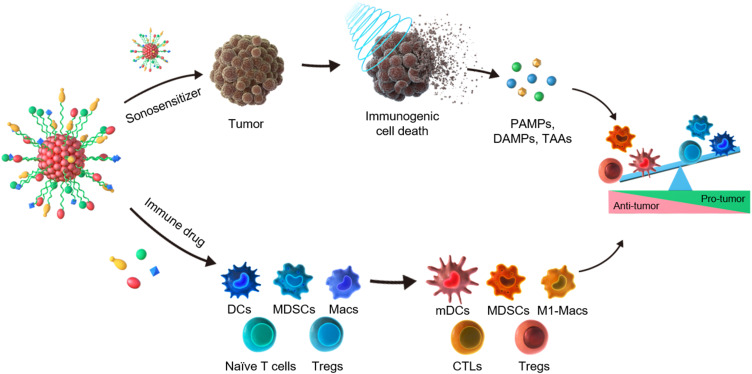
Emerging research has highlighted the immunomodulatory effects of SDT. By inducing localized tumor destruction and releasing tumor antigens, SDT has the potential to stimulate an immune response against the tumor, paving the way for its combination with immunotherapy to improve overall treatment outcomes (Figure 4).24 In immunotherapy, SDT can be leveraged as immune cells, including T lymphocytes, dendritic cells, and macrophages, play crucial roles in anti-tumor immunity through cellular immune mechanisms.136 Studies have demonstrated that SDT promotes the activation and proliferation of immune cells in three key ways. First, SDT enhances T cell activation and improves antigen presentation, leading to more effective recognition and elimination of cancer cells. Second, SDT induces dendritic cells (DCs) activation and strengthens the anti-tumor immune response. Finally, the tumor debris generated by SDT triggers immune and anti-inflammatory responses, promoting the transition of alternatively activated M2 macrophages to the pro-inflammatory M1 phenotype, thereby enhancing the immune response.137–139 These mechanisms primarily boost the immune system of the patients, aiding in the fight against cancer cells.
Figure 4.
The mechanism of cancer sono-immunotherapy involves two key processes: (i) sonosensitizer-mediated SDT, which induces immunogenic cell death (ICD) and the release of damage-associated molecular patterns (DAMPs), pathogen-associated molecular patterns (PAMPs), and tumor-associated antigens (TAAs); and (ii) immune-oncology drug-mediated remodeling of the tumor immune environment (TIEM), including dendritic cell (DC) maturation, activation of cytotoxic T lymphocytes (CTLs), inhibition of myeloid-derived suppressor cells (MDSCs), polarization of M1 macrophages (M1-Macs), and suppression of regulatory T cells (Tregs).
Research has confirmed that during SDT treatment, high levels of ROS are produced, which disrupt the mitochondrial membrane and reduce the mitochondrial membrane potential. In addition, ROS mediates apoptosis through the mitochondrial caspase pathway, releasing tumor antigens and promoting cytotoxic T lymphocyte (CTL) infiltration.54,61–63
Studies have shown that SDT enhances the immune response against tumors by inducing immunogenic cell death (ICD) and releasing tumor-associated antigens.140–142 ICD results from damage-associated molecular patterns (DAMPs), a group of highly immunostimulatory signals. These DAMPs interact with their respective receptors, leading to immune cell activation. For instance, extracellular ATP generates “find me” signals that promote the rapid recruitment of antigen-presenting cells (APCs) to apoptotic tumor cells. HMGB1 binds to Toll-like receptor 4, aiding APCs in presenting tumor antigens to T cells. Additionally, calreticulin (CRT) is transported to the surface of tumor cells, producing “eat me” phagocytic signals that prompt phagocytes, such as dendritic cells, to recognize and engulf cancer cells. ICD induced by SDT and the resulting tumor cell lysates can elicit a robust immune response.143–145
Application of Audible Sound waves in Biological Systems
US for SDT has primarily been studied in the frequency range above 20 kHz. However, there are limited reports on the use of sound waves within the audible frequency range for SDT. Researchers are increasingly exploring the potential of audible sound waves for various biological and biomaterial applications.146,147
Recent studies have shown that sound waves in the audible range can create temporal patterns and gradients in the domains of glucose oxidase (GOx) and horseradish peroxidase (HRP) in solution, thereby regulating cascade reaction networks.148 This approach can precisely position temporally formed supramolecular aggregates in solution, addressing a challenge that has largely remained elusive in out-of-equilibrium self-assembly and systems chemistry. Additionally, experimental results demonstrated that the formation and aggregation of gold nanoparticles (AuNPs) could be guided to desired locations within hydrogels using acoustic waves, promoting cell growth at specific sites. This suggests an innovative method for spatially and temporally controlling chemical reactions using acoustic waves.149
There have also been reports of audible sounds affecting cell-to-cell interactions. Surface acoustic waves (SAW) have been investigated for their ability to regulate intercellular interactions. In one study, HEK 293T cells were arranged in a linear array using the gap junctional coupling-forming calcein-AM dye. The findings revealed that the greater the number of cells, the longer it took for the dye to reach the terminal cells of the linearly arranged group, demonstrating that SAW can precisely control cell positioning to regulate intercellular distance and spatial arrangement.150,151
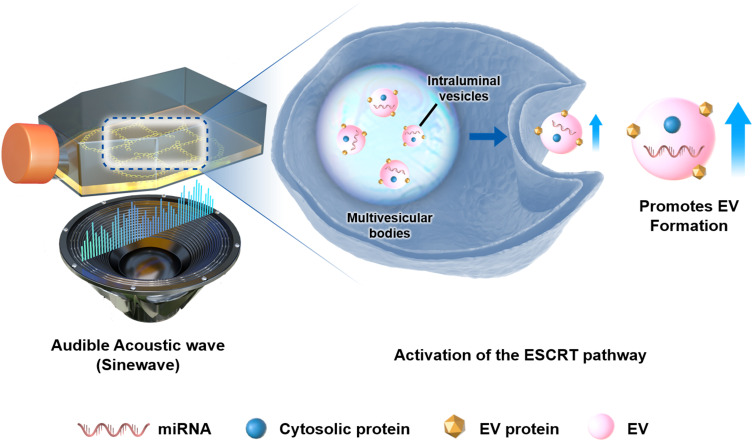
Research has shown that audible acoustic waves (AAWs) stimulate the formation and secretion of extracellular vesicles (EVs) in cancer cells. To verify the enhancement of EV formation under AAW conditions, we measured the relative expression of EV markers such as Calnexin, CD63, CD81, and TSG101. Our findings indicated that the size and distribution of EVs produced under AAW conditions were similar to those generated under static conditions. Additionally, AAWs increased EV production by promoting membrane fusion through the regulation of gene translation, particularly via the ESCRT (endosomal sorting complex required for transport) pathway and upregulation of membrane fusion-associated proteins. These EVs were found to contribute to cancer cell migration and invasion, providing new insights into cancer metastasis research.152 Another study found that high-frequency acoustic stimulation of cells promotes exosome release in a calcium-dependent manner. These results suggest that acoustic waves enhance exosome production, which is crucial for intercellular communication. This process involves the regulation of intracellular calcium levels, indicating that acoustic stimulation may be an effective method for manipulating exosome generation and influencing cellular communication and signaling pathways. Furthermore, research has demonstrated that audible sound stimulation can selectively suppress mechanosensitive genes depending on the cell type. Various sound parameters, including frequency, waveform, and sound pressure levels, were tested on different cell types. The study showed that ST2 stromal cells and C2C12 myoblasts exhibited strong responses to sound waves, while NIH3T3 fibroblasts and NB2a neuroblastoma cells showed partial or no responses. These findings suggest the potential of using audible sound as a non-invasive tool for the targeted modulation of gene expression and cellular functions (Figure 5).153,154
Figure 5.
The schematic diagram illustrates the methodology using audible acoustic waves (AAWs) to enhance extracellular vesicle (EV) production. The speaker emits audible acoustic waves that induce mechanical stimulation of the cells. The process of EV formation and secretion within the cell is depicted, showing that mechanical stimulation generated by AAWs promotes this process.
Integrating these findings illustrates that the application of sound waves in the audible range can significantly influence various biological processes, including EV formation, gene expression suppression, and exosome release. These insights offer promising avenues for further research and potential clinical applications in fields such as cancer treatment, gene therapy, and modulation of cellular communication.
Conclusion and Future Perspective
In summary, the integration of nanotechnology with US-based therapy represents a significant advance in both basic research and clinical applications.155,156 NP-associated sonosensitizers, particularly those incorporating valuable organic, inorganic and organic-inorganic hybrid sonosensitizers, have shown great promise in enhancing the efficacy of SDT due to their superior stability, solubility, and acoustic cavitation properties.66,67,157 These US-activated sonosensitizers can work synergistically with US waves to achieve targeted therapeutic effects with fewer side effects than conventional therapies. Furthermore, they can be combined with established cancer therapies such as chemotherapy, photothermal therapy, and immunotherapy to achieve synergistic effects.158–160 This review has highlighted the significant progress made in nanomedicine-enhanced US therapy, particularly the interplay between US applications and nanoscience, which has advanced our understanding of SDT mechanisms and its applications in disease treatment. Despite these advances, several issues still need to be addressed.67,161 One primary concern is the toxicity of certain sonosensitizers, particularly inorganic and hybrid nanomaterials, which can exhibit long-term cytotoxicity. Further evaluation of the biocompatibility and clearance mechanisms of these agents is essential to mitigate potential side effects. Additionally, the long-term stability of sonosensitizers in physiological conditions is crucial for ensuring sustained treatment efficacy, especially in chronic conditions. Another significant challenge lies in the translation from preclinical to clinical settings, as the success observed in animal models may not directly translate to human trials due to the complexity of the human tumor microenvironment. Optimizing treatment parameters such as ultrasound frequency, intensity, and exposure duration will be crucial for successful clinical translation. Moreover, developing more precise sonosensitizer delivery systems capable of deep tissue targeting remains a critical area of research.
To advance the clinical application of sonotherapy, the following points must be addressed. First, the long-term biological stability of SDT should be thoroughly evaluated.161 The results so far are preliminary, based on short-term toxicity data from mice, which are insufficient to predict outcomes in humans.158 A new standard evaluation protocol is needed to obtain comparable clinical data. Current US therapy equipment is complex, requiring hospital visits, and developing more user-friendly, precise systems remains a key challenge. Furthermore, a sonosensitizer that can be mass-produced while maintaining high quality is needed for realistic clinical applications.66 Production quality and cost control are also essential considerations for achieving large-scale clinical application.110 Moreover, the intrinsic mechanisms of US-responsive sonosensitizers in disease treatment remain poorly understood, complicating the regulation of SDT efficacy. Advances in biological, medical, and chemical research may optimize the performance of sonodynamic therapies and enhance their efficacy in treating diseases.162 In particular, research on nanomaterials that respond to sound waves within the audible frequency range, which is currently underexplored, may open new areas of SDT research in the future.163 Based on these considerations, efforts to complement and advance SDT for treating a wide range of intractable diseases, including cancer, will pave the way for breakthroughs that contribute to medical science and improve patient outcomes.
Acknowledgments
This work was supported by the Basic Science Research Program through the National Research Foundation of Korea (NRF- 2022M3A9G8018189, RS-2024-00414617), and by the Gachon University Research Fund of 2020 (GGU- 202008430004).
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Ali R, Mirza Z, Ashraf GMD, et al. New anticancer agents: recent developments in tumor therapy. Anticancer Res. 2012;32(7):2999–3005. [PubMed] [Google Scholar]
- 2.Urruticoechea A, Alemany R, Balart J, Villanueva A, Viñals F, Capellá G. Recent advances in cancer therapy: an overview. Curr Pharm Design. 2010;16(1):3–10. doi: 10.2174/138161210789941847 [DOI] [PubMed] [Google Scholar]
- 3.Retsky M, Demicheli R, Hrushesky W, Baum M, Gukas I. Surgery triggers outgrowth of latent distant disease in breast cancer: an inconvenient truth? Cancers. 2010;2(2):305–337. doi: 10.3390/cancers2020305 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Liu YP, Zheng CC, Huang YN, He ML, Xu WW, Li B. Molecular mechanisms of chemo- and radiotherapy resistance and the potential implications for cancer treatment. Medcomm. 2021;2(3):315–340. doi: 10.1002/mco2.55 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wu PJ, Gao W, Su M, et al. Adaptive mechanisms of tumor therapy resistance driven by tumor microenvironment. Front Cell Dev Biol. 2021;9:641469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Gonçalves AC, Richiardone E, Jorge J, et al. Impact of cancer metabolism on therapy resistance - clinical implications. Drug Resist Updat. 2021;59:100797. doi: 10.1016/j.drup.2021.100797 [DOI] [PubMed] [Google Scholar]
- 7.Qu Y, Dou B, Tan H, Feng Y, Wang N, Wang D. Tumor microenvironment-driven non-cell-autonomous resistance to antineoplastic treatment. Mol Cancer. 2019;18(1):69. doi: 10.1186/s12943-019-0992-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Sun Y. Tumor microenvironment and cancer therapy resistance. Cancer Lett. 2016;380(1):205–215. doi: 10.1016/j.canlet.2015.07.044 [DOI] [PubMed] [Google Scholar]
- 9.Wu P, Gao W, Su M, et al. Adaptive mechanisms of tumor therapy resistance driven by tumor microenvironment. Front Cell Dev Biol. 2021;9:641469. doi: 10.3389/fcell.2021.641469 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Rocha PHP, Reali RM, Decnop M, et al. Adverse radiation therapy effects in the treatment of head and neck tumors. Radiographics. 2022;42(3):806–821. doi: 10.1148/rg.210150 [DOI] [PubMed] [Google Scholar]
- 11.Stone HB, Coleman CN, Anscher MS, McBride WH. Effects of radiation on normal tissue: consequences and mechanisms. Lancet Oncol. 2003;4(9):529–536. doi: 10.1016/S1470-2045(03)01191-4 [DOI] [PubMed] [Google Scholar]
- 12.Dörr W, Hendry JH. Consequential late effects in normal tissues. Radiother Oncol. 2001;61(3):223–231. doi: 10.1016/S0167-8140(01)00429-7 [DOI] [PubMed] [Google Scholar]
- 13.Riva G, Cravero E, Pizzo C, et al. Sinonasal side effects of chemotherapy and/or radiation therapy for head and neck cancer: a literature review. Cancers. 2022;14(9):2324. doi: 10.3390/cancers14092324 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ibis B, Aliazis K, Cao C, Yenyuwadee S, Boussiotis VA. Immune-related adverse effects of checkpoint immunotherapy and implications for the treatment of patients with cancer and autoimmune diseases. Front Immunol. 2023;14. doi: 10.3389/fimmu.2023.1197364 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Overchuk M, Weersink RA, Wilson BC, Zheng G. Photodynamic and photothermal therapies: synergy opportunities for nanomedicine. Acs Nano. 2023;17(9):7979–8003. doi: 10.1021/acsnano.3c00891 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Pham TC, Nguyen VN, Choi Y, Lee S, Yoon J. Recent strategies to develop innovative photosensitizers for enhanced photodynamic therapy. Chem Rev. 2021;121(21):13454–13619. doi: 10.1021/acs.chemrev.1c00381 [DOI] [PubMed] [Google Scholar]
- 17.Cui XM, Ruan QF, Zhu XL, et al. Photothermal nanomaterials: a powerful light-to-heat converter. Chem Rev. 2023;123(11):6891–6952. doi: 10.1021/acs.chemrev.3c00159 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Jiang WQ, Liang MK, Lei QF, Li GZ, Wu S. The current status of photodynamic therapy in cancer treatment. Cancers. 2023;15(3):585. doi: 10.3390/cancers15030585 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Gunaydin G, Gedik ME, Ayan S. Photodynamic therapy-current limitations and novel approaches. Front Chem. 2021;9:691697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Chang MY, Hou ZY, Wang M, Li CX, Lin J. Recent advances in hyperthermia therapy-based synergistic immunotherapy. Adv Mater. 2021;33(4). doi: 10.1002/adma.202004788 [DOI] [PubMed] [Google Scholar]
- 21.Gong L, Zhang Y, Liu C, Zhang M, Han S. Application of radiosensitizers in cancer radiotherapy. Int J Nanomed. 2021;16:1083. doi: 10.2147/Ijn.S352169 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Alphandéry E. Ultrasound and nanomaterial: an efficient pair to fight cancer. J Nanobiotechnol. 2022;20(1). doi: 10.1186/s12951-022-01243-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Wang XW, Zhong XY, Gong F, Chao Y, Cheng L. Newly developed strategies for improving sonodynamic therapy. Mater Horiz. 2020;7(8):2028–2046. doi: 10.1039/d0mh00613k [DOI] [Google Scholar]
- 24.Yang YR, Huang J, Liu M, et al. Emerging sonodynamic therapy-based nanomedicines for cancer immunotherapy. Adv Sci. 2023;10(2):2204365. doi: 10.1002/advs.202204365 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Li JL, Yue ZY, Tang ML, et al. Strategies to reverse hypoxic tumor microenvironment for enhanced sonodynamic therapy. Adv Healthc Mater. 2024;13(1):2302028. doi: 10.1002/adhm.202302028 [DOI] [PubMed] [Google Scholar]
- 26.Gong ZR, Dai ZF. Design and challenges of sonodynamic therapy system for cancer theranostics: from equipment to sensitizers. Adv Sci. 2021;8(10). doi: 10.1002/advs.202002178 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Chen H, Zhou X, Gao Y, Zheng B, Tang F, Huang J. Recent progress in development of new sonosensitizers for sonodynamic cancer therapy. Drug Discov Today Apr. 2014;19(4):502–509. doi: 10.1016/j.drudis.2014.01.010 [DOI] [PubMed] [Google Scholar]
- 28.Pan X, Wang H, Wang S, et al. Sonodynamic therapy (SDT): a novel strategy for cancer nanotheranostics. Sci China Life Sci Apr. 2018;61(4):415–426. doi: 10.1007/s11427-017-9262-x [DOI] [PubMed] [Google Scholar]
- 29.Yan P, Liu LH, Wang P. Sonodynamic therapy (SDT) for cancer treatment: advanced sensitizers by ultrasound activation to injury tumor. ACS Appl Bio Mater. 2020;3(6):3456–3475. doi: 10.1021/acsabm.0c00156 [DOI] [PubMed] [Google Scholar]
- 30.Um W, EK KP, Lee J, Kim CH, You DG, Park JH. Recent advances in nanomaterial-based augmented sonodynamic therapy of cancer. Chem Commun. 2021;57(23):2854–2866. doi: 10.1039/d0cc07750j [DOI] [PubMed] [Google Scholar]
- 31.Al-Bataineh O, Jenne J, Huber P. Clinical and future applications of high intensity focused ultrasound in cancer. Cancer Treat Rev. 2012;38(5):346–353. doi: 10.1016/j.ctrv.2011.08.004 [DOI] [PubMed] [Google Scholar]
- 32.Zhou YF. High intensity focused ultrasound in clinical tumor ablation. World J Clin Oncol. 2011;2(1):8–27. doi: 10.5306/wjco.v2.i1.8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.van den Bijgaart RJE, Eikelenboom DC, Hoogenboom M, Fütterer JJ, den Brok MH, Adema GJ. Thermal and mechanical high-intensity focused ultrasound: perspectives on tumor ablation, immune effects and combination strategies. Cancer Immunol Immun. 2017;66(2):247–258. doi: 10.1007/s00262-016-1891-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Lafond M, Yoshizawa S, Umemura SI. Sonodynamic therapy: advances and challenges in clinical translation. J Ultras Med. 2019;38(3):567–580. doi: 10.1002/jum.14733 [DOI] [PubMed] [Google Scholar]
- 35.Mohammadpour M, Firoozabadi B. High intensity focused ultrasound (HIFU) ablation of porous liver: numerical analysis of heat transfer and hemodynamics. Appl Therm Eng. 2020;170:115014. doi: 10.1016/j.applthermaleng.2020.115014 [DOI] [Google Scholar]
- 36.Singh M. Modified Pennes bioheat equation with heterogeneous blood perfusion: a newer perspective. Int J Heat Mass Tran. 2024;218:124698. doi: 10.1016/j.ijheatmasstransfer.2023.124698 [DOI] [Google Scholar]
- 37.Kim Y-S, Rhim H, Choi MJ, Lim HK, Choi D. High-intensity focused ultrasound therapy: an overview for radiologists. Korean J Radiol. 2008;9(4):291–302. doi: 10.3348/kjr.2008.9.4.291 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Zhang P, Porter T. An study of a phase-shift nanoemulsion: a potential nucleation agent for bubble-enhanced HIFU tumor ablation. Ultrasound Med Biol. 2010;36(11):1856–1866. doi: 10.1016/j.ultrasmedbio.2010.07.001 [DOI] [PubMed] [Google Scholar]
- 39.Ohl SW, Klaseboer E, Khoo BC. Bubbles with shock waves and ultrasound: a review. Interface Focus. 2015;5(5):20150019. doi: 10.1098/rsfs.2015.0019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Burgess A, Shah K, Hough O, Hynynen K. Focused ultrasound-mediated drug delivery through the blood-brain barrier. Expert Rev Neurother. 2015;15(5):477–491. doi: 10.1586/14737175.2015.1028369 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Zhang SO, Zhang S, Luo SY, et al. Ultrasound-assisted brain delivery of nanomedicines for brain tumor therapy: advance and prospect. J Nanobiotechnol. 2022;20(1). doi: 10.1186/s12951-022-01464-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Dasgupta A, Liu M, Ojha T, Storm G, Kiessling F, Lammers T. Ultrasound-mediated drug delivery to the brain: principles, progress and prospects. Drug Discov Today Technol. 2016;20:41–48. doi: 10.1016/j.ddtec.2016.07.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Martinez P, Nault G, Steiner J, et al. MRI-guided focused ultrasound blood-brain barrier opening increases drug delivery and efficacy in a diffuse midline glioma mouse model. Neuro-Oncol Adv. 2023;5(1):vdad111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Phillips LC, Dhanaliwala AH, Klibanov AL, Hossack JA, Wamhoff BR. Focused ultrasound-mediated drug delivery from microbubbles reduces drug dose necessary for therapeutic effect on neointima formation-brief report. Arterioscl Throm Vas. 2011;31(12):2853–U264. doi: 10.1161/Atvbaha.111.238170 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Wang F, Dong L, Liang SM, et al. Ultrasound-triggered drug delivery for glioma therapy through gambogic acid-loaded nanobubble-microbubble complexes. Biomed Pharmacother. 2022;150:113042. [DOI] [PubMed] [Google Scholar]
- 46.Barzegar-Fallah A, Gandhi K, Rizwan SB, Slatter TL, Reynolds JNJ. Harnessing ultrasound for targeting drug delivery to the brain and breaching the blood-brain tumour barrier. Pharmaceutics. 2022;14(10):2231. doi: 10.3390/pharmaceutics14102231 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Arsiwala TA, Sprowls SA, Blethen KE, et al. Ultrasound-mediated disruption of the blood tumor barrier for improved therapeutic delivery. Neoplasia. 2021;23(7):676–691. doi: 10.1016/j.neo.2021.04.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Baek H, Lockwood D, Mason EJ, et al. Clinical intervention using Focused Ultrasound (FUS) Stimulation of the brain in diverse neurological disorders. Front Neurol. 2022;13. doi: 10.3389/fneur.2022.880814 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Gorick CM, Breza VR, Nowak KM, et al. Applications of focused ultrasound-mediated blood-brain barrier opening. Adv Drug Deliv Rev. 2022;191:114583. doi: 10.1016/j.addr.2022.114583 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Redza-Dutordoir M, Averill-Bates DA. Activation of apoptosis signalling pathways by reactive oxygen species. Bba-Mol Cell Res. 2016;1863(12):2977–2992. doi: 10.1016/j.bbamcr.2016.09.012 [DOI] [PubMed] [Google Scholar]
- 51.Villalpando-Rodriguez GE, Gibson SB. Reactive Oxygen Species (ROS) Regulates different types of cell death by acting as a rheostat. Oxid Med Cell Longev. 2021;2021(1). doi: 10.1155/2021/9912436 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Xing XJ, Zhao SJ, Xu T, et al. Advances and perspectives in organic sonosensitizers for sonodynamic therapy. Coordin Chem Rev. 2021;445:214087. doi: 10.1016/j.ccr.2021.214 [DOI] [Google Scholar]
- 53.Li D, Yang Y, Li DF, Pan J, Chu CC, Liu G. Organic sonosensitizers for sonodynamic therapy: from small molecules and nanoparticles toward clinical development. Small. 2021;17(42):2101976. [DOI] [PubMed] [Google Scholar]
- 54.Cao XS, Li MX, Liu QY, Zhao JJ, Lu XH, Wang JW. Inorganic sonosensitizers for sonodynamic therapy in cancer treatment. Small. 2023;19(42). doi: 10.1002/smll.202303195 [DOI] [PubMed] [Google Scholar]
- 55.He ZY, Du J, Miao YQ, Li YH. Recent developments of inorganic nanosensitizers for sonodynamic therapy. Adv Healthc Mater. 2023;12(22). doi: 10.1002/adhm.202300234 [DOI] [PubMed] [Google Scholar]
- 56.Liu RG, Zhang QY, Lang YH, Peng ZZ, Li LB. Sonodynamic therapy, a treatment developing from photodynamic therapy. Photodiagn Photodyn. 2017;19:159–166. doi: 10.1016/j.pdpdt.2017.06.003 [DOI] [PubMed] [Google Scholar]
- 57.Misík V, Riesz P. Free radical intermediates in sonodynamic therapy. Ann Ny Acad Sci. 2000;899(1):335–348. doi: 10.1111/j.1749-6632.2000.tb06198.x [DOI] [PubMed] [Google Scholar]
- 58.Qin D, Zou QQ, Lei S, Wang W, Li ZY. Cavitation dynamics and inertial cavitation threshold of lipid coated microbubbles in viscoelastic media with bubble-bubble interactions. Micromachines-Basel. 2021;12(9). doi: 10.3390/mi12091125 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Fabiilli ML, Haworth KJ, Fakhri NH, Kripfgans OD, Carson PL, Fowlkes JB. The role of inertial cavitation in acoustic droplet vaporization. Ieee T Ultrason Ferr. 2009;56(5):1006–1017. doi: 10.1109/Tuffc.2009.1132 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Ashokkumar M. The characterization of acoustic cavitation bubbles - An overview. Ultrason Sonochem. 2011;18(4):864–872. doi: 10.1016/j.ultsonch.2010.11.016 [DOI] [PubMed] [Google Scholar]
- 61.Li CH, Chang YC, Hsiao MC, Chan MH. Ultrasound and nanomedicine for cancer-targeted drug delivery: screening, cellular mechanisms and therapeutic opportunities. Pharmaceutics. 2022;14(6):1282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Jiang Q, Gao XR, Zhang W, Chen ZG. Recent progress in metal-organic framework-based sonosensitizers for sonodynamic tumor therapy. Biomater Sci. 2023;11(13):4452–4470. doi: 10.1039/d3bm00556a [DOI] [PubMed] [Google Scholar]
- 63.Canavese G, Ancona A, Racca L, et al. Nanoparticle-assisted ultrasound: a special focus on sonodynamic therapy against cancer. Chem Eng J. 2018;340:155–172. doi: 10.1016/j.cej.2018.01.060 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Rosenthal I, Sostaric JZ, Riesz P. Sonodynamic therapy - a review of the synergistic effects of drugs and ultrasound. Ultrason Sonochem. 2004;11(6):349–363. doi: 10.1016/j.ultsonch.2004.03.004 [DOI] [PubMed] [Google Scholar]
- 65.Zhang C, Pu KY. Organic sonodynamic materials for combination cancer immunotherapy. Adv Mater. 2023;35(51). doi: 10.1002/adma.202303059 [DOI] [PubMed] [Google Scholar]
- 66.Sun LH, Wang P, Zhang JX, et al. Design and application of inorganic nanoparticles for sonodynamic cancer therapy. Biomater Sci. 2021;9(6):1945–1960. doi: 10.1039/d0bm01875a [DOI] [PubMed] [Google Scholar]
- 67.Hu CT, Hou B, Xie SL. Application of nanosonosensitizer materials in cancer sono-dynamic therapy. Rsc Adv. 2022;12(35):22722–22747. doi: 10.1039/d2ra03786f [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Shi HR, Tan X, Wang P, Qin JL. A novel near-infrared trifluoromethyl heptamethine cyanine dye with mitochondria-targeting for integration of collaborative treatment of photothermal and sonodynamic therapy. Mater Today Adv. 2022;14:100251. [Google Scholar]
- 69.Liu WX, Dong A, Wang B, Zhang H. Current advances in black phosphorus-based drug delivery systems for cancer therapy. Adv Sci. 2021;8(5):2003033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Chen P, Zhang P, Shah NH, Cui YY, Wang YL. A comprehensive review of inorganic sonosensitizers for sonodynamic therapy. Int J Mol Sci. 2023;24(15):12001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Zhao PX, Deng YB, Xiang GY, Liu YN. Nanoparticle-assisted sonosensitizers and their biomedical applications. Int J Nanomed. 2021;16:4615–4630. doi: 10.2147/Ijn.S307885 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Yu Z, Cao WL, Han CY, et al. Biomimetic metal-organic framework nanoparticles for synergistic combining of sdt-chemotherapy induce pyroptosis in gastric cancer. Front Bioeng Biotech. 2022;10:796820. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Wang Q, Liu N, Hou ZY, Shi JP, Su XH, Sun XL. Radioiodinated persistent luminescence nanoplatform for radiation-induced photodynamic therapy and radiotherapy. Adv Healthc Mater. 2021;10(5):2000802. [DOI] [PubMed] [Google Scholar]
- 74.Zhong D, Wu HY, Wu YH, et al. Redox dual-responsive dendrimeric nanoparticles for mutually synergistic chemo-photodynamic therapy to overcome drug resistance. J Control Release. 2021;329:1210–1221. doi: 10.1016/j.jconrel.2020.10.048 [DOI] [PubMed] [Google Scholar]
- 75.Zhang YF, Wan YL, Chen YT, Blum NT, Lin J, Huang P. Ultrasound-enhanced chemo-photodynamic combination therapy by using albumin “nanoglue”-based nanotheranostics. Acs Nano. 2020;14(5):5560–5569. doi: 10.1021/acsnano.9b09827 [DOI] [PubMed] [Google Scholar]
- 76.Hachimine K, Shibaguchi H, Kuroki M, et al. Sonodynamic therapy of cancer using a novel porphyrin derivative, DCPH-P-Na(I), which is devoid of photosensitivity. Cancer Sci. 2007;98(6):916–920. doi: 10.1111/j.1349-7006.2007.00468.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Liu YL, Pan YX, Cao W, et al. A tumor microenvironment responsive biodegradable CaCO - based nanoplatform for the enhanced photodynamic therapy and improved PD-L1 immunotherapy. Theranostics. 2019;9(23):6867–6884. doi: 10.7150/thno.37586 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Chen SJ, Huang BY, Pei WJ, Wang L, Xu Y, Niu CC. Mitochondria-targeting oxygen-sufficient perfluorocarbon nanoparticles for imaging-guided tumor phototherapy. Int J Nanomed. 2020;15:8641–8658. doi: 10.2147/Ijn.S281649 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Liu XL, Dong X, Yang SC, et al. Biomimetic liposomal nanoplatinum for targeted cancer chemophototherapy. Adv Sci Apr. 2021;8(8):2003679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Zhang CQ, Zhao Y, Zhang H, et al. The application of heptamethine cyanine dye DZ-1 and indocyanine green for imaging and targeting in xenograft models of hepatocellular carcinoma. Int J Mol Sci. 2017;18(6). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Li W, Yang J, Luo LH, et al. Targeting photodynamic and photothermal therapy to the endoplasmic reticulum enhances immunogenic cancer cell death. Nat Commun. 2019;10:3349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Thomas RG, Jeong YY. NIRF heptamethine cyanine dye nanocomplexes for multi modal theranosis of tumors. Chonnam Med J. 2017;53(2):83–94. doi: 10.4068/cmj.2017.53.2.83 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Burriss A, Edmunds AJF, Emery D, Hall RG, Jacob O, Schaetzer J. The importance of trifluoromethyl pyridines in crop protection. Pest Manag Sci. 2018;74(6):1228–1238. doi: 10.1002/ps.4806 [DOI] [PubMed] [Google Scholar]
- 84.Cui D, Huang JG, Zhen X, Li JC, Jiang YY, Pu KY. A semiconducting polymer nano-prodrug for hypoxia-activated photodynamic cancer therapy. Angew Chem Int Edit. 2019;58(18):5920–5924. doi: 10.1002/anie.201814730 [DOI] [PubMed] [Google Scholar]
- 85.Zhen X, Zhang CW, Xie C, Miao QQ, Lim KL, Pu KY. Intraparticle energy level alignment of semiconducting polymer nanoparticles to amplify chemiluminescence for ultrasensitive imaging of reactive oxygen species. Acs Nano. 2016;10(6):6400–6409. doi: 10.1021/acsnano.6b02908 [DOI] [PubMed] [Google Scholar]
- 86.Lyu Y, Fang Y, Miao Q, Zhen X, Ding D, Pu K. Intraparticle molecular orbital engineering of semiconducting polymer nanoparticles as amplified theranostics for in vivo photoacoustic imaging and photothermal therapy. Acs Nano. 2016;10(4):4472–4481. doi: 10.1021/acsnano.6b00168 [DOI] [PubMed] [Google Scholar]
- 87.Wang X, Wu M, Li HZ, et al. Enhancing penetration ability of semiconducting polymer nanoparticles for sonodynamic therapy of large solid tumor. Adv Sci. 2022;9(6):2104125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Li JC, Luo Y, Zeng ZL, et al. Precision cancer sono-immunotherapy using deep-tissue activatable semiconducting polymer immunomodulatory nanoparticles. Nat Commun. 2022;13(1):4032. doi: 10.1038/s41467-022-31551-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Torchilin VP. Recent advances with liposomes as pharmaceutical carriers. Nat Rev Drug Discov. 2005;4(2):145–160. doi: 10.1038/nrd1632 [DOI] [PubMed] [Google Scholar]
- 90.Chen HJ, Huang XR, Zhou XB, Zheng BY, Huang JD. Potential sonodynamic anticancer activities of artemether and liposome-encapsulated artemether. Chem Commun. 2015;51(22):4681–4684. doi: 10.1039/c5cc00927h [DOI] [PubMed] [Google Scholar]
- 91.Zheng YL, Ye JX, Li ZY, Chen HJ, Gao Y. Recent progress in sono-photodynamic cancer therapy: from developed new sensitizers to nanotechnology-based efficacy-enhancing strategies. Acta Pharm Sin B. 2021;11(8):2197–2219. doi: 10.1016/j.apsb.2020.12.016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Harada Y, Ogawa K, Irie Y, et al. Ultrasound activation of TiO in melanoma tumors. J Control Release. 2011;149(2):190–195. doi: 10.1016/j.jconrel.2010.10.012 [DOI] [PubMed] [Google Scholar]
- 93.Lee HR, Kim DW, Jones VO, et al. Sonosensitizer-functionalized graphene nanoribbons for adhesion blocking and sonodynamic ablation of ovarian cancer spheroids. Adv Healthc Mater. 2021;10(13). doi: 10.1002/adhm.202001368 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Ning SP, Dai XL, Tang WW, et al. Cancer cell membrane-coated C-TiO2 hollow nanoshells for combined sonodynamic and hypoxia-activated chemotherapy. Acta Biomater. 2022;152:562–574. doi: 10.1016/j.actbio.2022.08.067 [DOI] [PubMed] [Google Scholar]
- 95.Yu H, Chen M, Rice PM, Wang SX, White RL, Sun SH. Dumbbell-like bifunctional Au-Fe nanoparticles. Nano Lett. 2005;5(2):379–382. doi: 10.1021/nl047955q [DOI] [PubMed] [Google Scholar]
- 96.Popova V, Poletaeva Y, Chubarov A, Dmitrienko E. pH-responsible Doxorubicin-Loaded Fe nanocomposites for cancer treatment. Pharmaceutics. 2023;15(3):771. doi: 10.3390/pharmaceutics15030771 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Gong F, Cheng L, Yang NL, et al. Ultrasmall oxygen-deficient bimetallic oxide mnwo nanoparticles for depletion of endogenous gsh and enhanced sonodynamic cancer therapy. Adv Mater. 2019;31(23). doi: 10.1002/adma.201900730 [DOI] [PubMed] [Google Scholar]
- 98.Lin XH, Song JB, Chen XY, Yang HH. Ultrasound-activated sensitizers and applications. Angew Chem Int Edit. 2020;59(34):14212–14233. doi: 10.1002/anie.201906823 [DOI] [PubMed] [Google Scholar]
- 99.Bhattacharyya S, Kudgus RA, Bhattacharya R, Mukherjee P. Inorganic nanoparticles in cancer therapy. Pharm Res-Dordr. 2011;28(2):237–259. doi: 10.1007/s11095-010-0318-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Sazgarnia A, Shanei A, Taheri AR, et al. Therapeutic effects of acoustic cavitation in the presence of gold nanoparticles on a colon tumor model. J Ultrasound Med. 2013;32(3):475–483. doi: 10.7863/jum.2013.32.3.475 [DOI] [PubMed] [Google Scholar]
- 101.Benito M, Martín V, Blanco MD, Teijón JM, Gómez C. Cooperative effect of 5-aminolevulinic acid and gold nanoparticles for photodynamic therapy of cancer. J Pharm Sci-Us. 2013;102(8):2760–2769. doi: 10.1002/jps.23621 [DOI] [PubMed] [Google Scholar]
- 102.Tewari KM, Eggleston IM. Chemical approaches for the enhancement of 5-aminolevulinic acid-based photodynamic therapy and photodiagnosis. Photoch Photobio Sci. 2018;17(11):1553–1572. doi: 10.1039/c8pp00362a [DOI] [PubMed] [Google Scholar]
- 103.Canaparo R, Foglietta F, Barbero N, Serpe L. The promising interplay between sonodynamic therapy and nanomedicine. Adv Drug Deliv Rev. 2022;189:114495. doi: 10.1016/j.addr.2022.114495 [DOI] [PubMed] [Google Scholar]
- 104.Cao J, Sun Y, Zhang C, et al. Tablet-like TiO nanoparticles. Nano Lett. 2005;5(2):379–382. doi: 10.1021/nl047955q [DOI] [PubMed] [Google Scholar]
- 105.Li ZL, Han J, Yu LD, et al. Synergistic sonodynamic/chemotherapeutic suppression of hepatocellular carcinoma by targeted biodegradable mesoporous nanosonosensitizers. Adv Funct Mater. 2018;28(26):1800145. [Google Scholar]
- 106.Kang Y, Xu LL, Dong JR, et al. Programmed microalgae-gel promotes chronic wound healing in diabetes. Nat Commun. 2024;15(1):1042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Shibaguchi H, Tsuru H, Kuroki M, Kuroki M. Sonodynamic cancer therapy: a non-invasive and repeatable approach using low-intensity ultrasound with a sonosensitizer. Anticancer Res. 2011;31(7):2425–2429. [PubMed] [Google Scholar]
- 108.Wan GY, Liu Y, Chen BW, Liu YY, Wang YS, Zhang N. Recent advances of sonodynamic therapy in cancer treatment. Cancer Biol Med. 2016;13(3):325–338. doi: 10.20892/j.issn.2095-3941.2016.0068 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Qian XQ, Zheng YY, Chen Y. Micro/nanoparticle-augmented sonodynamic therapy (SDT): breaking the depth shallow of photoactivation. Adv Mater. 2016;28(37):8097–8129. doi: 10.1002/adma.201602012 [DOI] [PubMed] [Google Scholar]
- 110.Liang YL, Zhang MZ, Zhang YJ, Zhang MX. Ultrasound sonosensitizers for tumor sonodynamic therapy and imaging: a new direction with clinical translation. Molecules. 2023;28(18):6484. doi: 10.3390/molecules28186484 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Yuan X, Kang Y, Dong JR, et al. Self-triggered thermoelectric nanoheterojunction for cancer catalytic and immunotherapy. Nat Commun. 2023;14(1). doi: 10.1038/s41467-023-40954-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Zhou Z, Song J, Nie L, Chen X. Reactive oxygen species generating systems meeting challenges of photodynamic cancer therapy. Chem Soc Rev. 2016;45(23):6597–6626. doi: 10.1039/c6cs00271d [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Liu Z, Xie Z, Li W, et al. Photodynamic immunotherapy of cancers based on nanotechnology: recent advances and future challenges. J Nanobiotechnology. 2021;19(1):160. doi: 10.1186/s12951-021-00903-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Correia JH, Rodrigues JA, Pimenta S, Dong T, Yang ZC. Photodynamic therapy review: principles, photosensitizers, applications, and future directions. Pharmaceutics. 2021;13(9):1332. doi: 10.3390/pharmaceutics13091332 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.McHale AP, Callan JF, Nomikou N, Fowley C, Callan B. Sonodynamic therapy: concept, mechanism and application to cancer treatment. Adv Exp Med Biol. 2016;880:429–450. doi: 10.1007/978-3-319-22536-4_22 [DOI] [PubMed] [Google Scholar]
- 116.Zhou Y, Gao YY, Yao NN, et al. Multi-modal triggered-release sonodynamic/chemo/phototherapy synergistic nanocarriers for the treatment of colon cancer. Front Bioeng Biotech. 2024;12. doi: 10.3389/fbioe.2024.1439883 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Xu MM, Zhou LQ, Zheng L, et al. Sonodynamic therapy-derived multimodal synergistic cancer therapy. Cancer Lett. 2021;497:229–242. doi: 10.1016/j.canlet.2020.10.037 [DOI] [PubMed] [Google Scholar]
- 118.Zhang Y, Zhang XQ, Yang HC, et al. Advanced biotechnology-assisted precise sonodynamic therapy. Chem Soc Rev. 2021;50(20):11227–11248. doi: 10.1039/d1cs00403d [DOI] [PubMed] [Google Scholar]
- 119.Mokuyasu S, Suzuki Y, Kawahara E, Seto T, Tokuda Y. High-sensitivity cardiac troponin I detection for 2 types of drug-induced cardiotoxicity in patients with breast cancer. Breast Cancer. 2015;22(6):563–569. doi: 10.1007/s12282-014-0520-8 [DOI] [PubMed] [Google Scholar]
- 120.Tonder M, Eisele G, Weiss T, et al. Addition of lomustine for bevacizumab-refractory recurrent glioblastoma. Acta Oncol. 2014;53(10):1436–1440. doi: 10.3109/0284186x.2014.920960 [DOI] [PubMed] [Google Scholar]
- 121.Nomikou N, Li YS, McHale AP. Ultrasound-enhanced drug dispersion through solid tumours and its possible role in aiding ultrasound-targeted cancer chemotherapy. Cancer Lett. 2010;288(1):94–98. doi: 10.1016/j.canlet.2009.06.028 [DOI] [PubMed] [Google Scholar]
- 122.Liu Y, Wan GY, Guo H, et al. A multifunctional nanoparticle system combines sonodynamic therapy and chemotherapy to treat hepatocellular carcinoma. Nano Res. 2017;10(3):834–855. doi: 10.1007/s12274-016-1339-8 [DOI] [Google Scholar]
- 123.Kabanov AV, Batrakova EV, Alakhov VY. An essential relationship between ATP depletion and chemosensitizing activity of Pluronic block copolymers. J Control Release. 2003;91(1–2):75–83. doi: 10.1016/S0168-3659(03)00211-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Wan GY, Liu Y, Shi SR, et al. Hematoporphyrin and doxorubicin co-loaded nanomicelles for the reversal of drug resistance in human breast cancer cells by combining sonodynamic therapy and chemotherapy. Rsc Adv. 2016;6(102):100361–100372. doi: 10.1039/c6ra22724d087 [DOI] [Google Scholar]
- 125.McEwan C, Kamila S, Owen J, et al. Combined sonodynamic and antimetabolite therapy for the improved treatment of pancreatic cancer using oxygen loaded microbubbles as a delivery vehicle. Biomaterials. 2016;80:20–32. doi: 10.1016/j.biomaterials.2015.11.033 [DOI] [PubMed] [Google Scholar]
- 126.Nesbitt H, Sheng YJ, Kamila S, et al. Gemcitabine loaded microbubbles for targeted chemo-sonodynamic therapy of pancreatic cancer. J Control Release. 2018;279:8–16. doi: 10.1016/j.jconrel.2018.04.018 [DOI] [PubMed] [Google Scholar]
- 127.Sheng YJ, Beguin E, Nesbitt H, et al. Magnetically responsive microbubbles as delivery vehicles for targeted sonodynamic and antimetabolite therapy of pancreatic cancer. J Control Release. 2017;262:192–200. doi: 10.1016/j.jconrel.2017.07.040 [DOI] [PubMed] [Google Scholar]
- 128.Sun BW, Rahmat JNB, Zhang Y. Advanced techniques for performing photodynamic therapy in deep-seated tissues. Biomaterials. 2022;291:121875. doi: 10.1016/j.biomaterials.2022.121875 [DOI] [PubMed] [Google Scholar]
- 129.Hasan N, Nadaf A, Imran M, et al. Skin cancer: understanding the journey of transformation from conventional to advanced treatment approaches. Mol Cancer. 2023;22(1). doi: 10.1186/s12943-023-01854-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Liang S, Deng XR, Chang Y, et al. Intelligent Hollow Pt-CuS Janus architecture for synergistic catalysis-enhanced sonodynamic and photothermal cancer therapy. Nano Lett. 2019;19(6):4134–4145. doi: 10.1021/acs.nanolett.9b01595 [DOI] [PubMed] [Google Scholar]
- 131.Blum NT, Gyorkos CM, Narowetz SJ, Mueller EN, Goodwin AP. Phospholipid-coated hydrophobic mesoporous silica nanoparticles enhance thrombectomy by high-intensity focused ultrasound with low production of embolism-inducing clot debris. Acs Appl Mater Inter. 2019;11(40):36324–36332. doi: 10.1021/acsami.9b11095 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Nomikou N, Sterrett C, Arthur C, McCaughan B, Callan JF, McHale AP. The effects of ultrasound and light on indocyanine-green-treated tumour cells and tissues. Chemmedchem. 2012;7(8):1465–1471. doi: 10.1002/cmdc.201200233 [DOI] [PubMed] [Google Scholar]
- 133.Kayani Z, Vais RD, Soratijahromi E, Mohammadi S, Sattarahmady N. Curcumin-gold-polyethylene glycol nanoparticles as a nanosensitizer for photothermal and sonodynamic therapies: in vitro and animal model studies. Photodiagn Photodyn. 2021;33:102139. doi: 10.1016/j.pdpdt.2020.102139 [DOI] [PubMed] [Google Scholar]
- 134.Xu XY, Zhang RY, Yang XF, et al. A Honeycomb-Like Bismuth/Manganese Oxide nanoparticle with mutual reinforcement of internal and external response for triple-negative breast cancer targeted therapy. Adv Healthc Mater. 2021;10(18). doi: 10.1002/adhm.202100518 [DOI] [PubMed] [Google Scholar]
- 135.Gao FL, He GL, Yin H, et al. Titania-coated 2D gold nanoplates as nanoagents for synergistic photothermal/sonodynamic therapy in the second near-infrared window. Nanoscale. 2019;11(5):2374–2384. doi: 10.1039/c8nr07188h [DOI] [PubMed] [Google Scholar]
- 136.Mukherjee AG, Wanjari UR, Namachivayam A, et al. Role of immune cells and receptors in cancer treatment: an immunotherapeutic approach. Vaccines-Basel. 2022;10(9):1493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Han LA, Huang RQ, Liu SH, Huang SX, Jiang C. Peptide-conjugated PAMAM for targeted doxorubicin delivery to transferrin receptor overexpressed tumors. Mol Pharm. 2010;7(6):2156–2165. doi: 10.1021/mp100185f [DOI] [PubMed] [Google Scholar]
- 138.Pardoll DM. The blockade of immune checkpoints in cancer immunotherapy. Nat Rev Cancer Apr. 2012;12(4):252–264. doi: 10.1038/nrc3239 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Wang T, Peng WR, Du M, Chen ZY. Immunogenic sonodynamic therapy for inducing immunogenic cell death and activating antitumor immunity. Front Oncol. 2023;13:1167105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Liu Z, Li JP, Jiang Y, Wang DD. Multifunctional nanocapsules on a seesaw balancing sonodynamic and photodynamic therapies against superficial malignant tumors by effective immune-enhancement. Biomaterials. 2019;218:119251. doi: 10.1016/j.biomaterials.2019.119251 [DOI] [PubMed] [Google Scholar]
- 141.Si YR, Yue J, Liu ZY, et al. Phase-transformation nanoparticle-mediated sonodynamic therapy: an effective modality to enhance anti-tumor immune response by inducing immunogenic cell death in breast cancer. Int J Nanomed. 2021;16:1913–1926. doi: 10.2147/Ijn.S297933 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Xie W, Zhu SY, Yang BY, et al. The destruction of laser-induced phase-transition nanoparticles triggered by low-intensity ultrasound: an innovative modality to enhance the immunological treatment of ovarian cancer cells. Int J Nanomed. 2019;14:9377–9393. doi: 10.2147/Ijn.S208404 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Arimoto KI, Miyauchi S, Liu MD, Zhang DE. Emerging role of immunogenic cell death in cancer immunotherapy. Front Immunol. 2024;15. doi: 10.3389/fimmu.2024.1390263 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Krysko DV, Garg AD, Kaczmarek A, Krysko O, Agostinis P, Vandenabeele P. Immunogenic cell death and DAMPs in cancer therapy. Nat Rev Cancer. 2012;12(12):860–875. doi: 10.1038/nrc3380 [DOI] [PubMed] [Google Scholar]
- 145.Tesniere A, Apetoh L, Ghiringhelli F, et al. Immunogenic cancer cell death: a key-lock paradigm. Curr Opin Immunol. 2008;20(5):504–511. doi: 10.1016/j.coi.2008.05.007 [DOI] [PubMed] [Google Scholar]
- 146.Guex AG, Di Marzio N, Eglin D, Alini M, Serra T. The waves that make the pattern: a review on acoustic manipulation in biomedical research. Mater Today Bio. 2021;10. doi: 10.1016/j.mtbio.2021.100110 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Greco G, Agostini M, Tonazzin I, Sallemi D, Barone S, Cecchini M. Surface-Acoustic-Wave (SAW)-driven device for dynamic cell cultures. Anal Chem. 2018;90(12):7450–7457. doi: 10.1021/acs.analchem.8b00972 [DOI] [PubMed] [Google Scholar]
- 148.Hwang I, Mukhopadhyay RD, Dhasaiyan P, et al. Audible sound-controlled spatiotemporal patterns in out-of-equilibrium systems. Nat Chem. 2020;12(9):808–813. doi: 10.1038/s41557-020-0516-2 [DOI] [PubMed] [Google Scholar]
- 149.Dhasaiyan P, Ghosh T, Lee HG, et al. Cascade reaction networks within audible sound induced transient domains in a solution. Nat Commun. 2022;13(1). doi: 10.1038/s41467-022-30124-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Deymier PA, Swinteck N, Runge K, Deymier-Black A, Hoying JB. Effect of sound on gap-junction-based intercellular signaling: calcium waves under acoustic irradiation. Phys Rev E. 2015;92(5). doi: 10.1103/PhysRevE.92.052711 [DOI] [PubMed] [Google Scholar]
- 151.Guo F, Li P, French JB, et al. Controlling cell-cell interactions using surface acoustic waves. Proc Natl Acad Sci. 2015;112(1):43–48. doi: 10.1073/pnas.1422068112 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Lei ZY, Jiang HW, Liu J, et al. Audible acoustic wave promotes EV formation and secretion from adherent cancer cells via mechanical stimulation. Acs Appl Mater Inter. 2023;15(46):53859–53870. doi: 10.1021/acsami.3c13845 [DOI] [PubMed] [Google Scholar]
- 153.Ambattu LA, Ramesan S, Dekiwadia C, Hanssen E, Li HY, Yeo L. High frequency acoustic cell stimulation promotes exosome generation regulated by a calcium- dependent mechanism. Biophys J. 2021;120(3):111a–111a. doi: 10.1016/j.bpj.2020.11.892 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Ambattu LA, Ramesan S, Dekiwadia C, Hanssen E, Li HY, Yeo LSY. High frequency acoustic cell stimulation promotes exosome generation regulated by a calcium-dependent mechanism. Commun Biol. 2020;3(1). doi: 10.1038/s42003-020-01277-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155.Qin Y, Geng X, Sun Y, et al. Ultrasound nanotheranostics: toward precision medicine. J Control Release. 2023;353:105–124. doi: 10.1016/j.jconrel.2022.11.021 [DOI] [PubMed] [Google Scholar]
- 156.Zhu Y, Liu YY, Khan K, et al. Ultrasound combined with nanomaterials for cancer therapy. Mater Today Adv. 2023;17:100330. [Google Scholar]
- 157.Yang F, Lv J, Ma W, Yang Y, Hu X, Yang Z. Engineering sonosensitizer-derived nanotheranostics for augmented sonodynamic therapy. Small. 2024;20(44):e2402669. doi: 10.1002/smll.202402669 [DOI] [PubMed] [Google Scholar]
- 158.Yang Y, Huang J, Liu M, et al. Emerging sonodynamic therapy-based nanomedicines for cancer immunotherapy. Adv Sci. 2023;10(2):e2204365. doi: 10.1002/advs.202204365 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159.Han HS, Choi KY. Advances in nanomaterial-mediated photothermal cancer therapies: toward clinical applications. Biomedicines. 2021;9(3):305. doi: 10.3390/biomedicines9030305 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Li C, Cheng Y, Li D, et al. Antitumor applications of photothermal agents and photothermal synergistic therapies. Int J Mol Sci. 2022;23(14). doi: 10.3390/ijms23147909 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.Gong Z, Dai Z. Design and challenges of sonodynamic therapy system for cancer theranostics: from equipment to sensitizers. Adv Sci. 2021;8(10):2002178. doi: 10.1002/advs.202002178 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.Ouyang J, Tang ZM, Farokhzad N, et al. Ultrasound mediated therapy: recent progress and challenges in nanoscience. Nano Today. 2020;35:100949. doi: 10.1016/j.nantod.2020.100949 [DOI] [Google Scholar]
- 163.Yang N, Li J, Yu S, et al. Application of nanomaterial-based sonodynamic therapy in tumor therapy. Pharmaceutics. 2024;16(5):603. doi: 10.3390/pharmaceutics16050603 [DOI] [PMC free article] [PubMed] [Google Scholar]