Abstract
Although rare, internal hernias have an increased incidence of development in patients who have undergone Roux-en-Y gastric bypass. They are difficult to diagnose given their non-specific presentation and lack of externally visible findings, and most cases develop within a few months of the original procedure. In this case report, we present a patient with recent weight loss who developed an internal hernia decades post-bariatric surgery with computed tomography findings showing the classic “mesenteric swirl” sign.
Keywords: bariatric surgery, internal hernia, mesenteric internal hernia, mesenteric swirl, rou-en-y, roux-en-y complication, roux-en-y gastric bypass (rygb)
Introduction
In the United States, more than a third of the population is obese [1,2]. Bariatric surgery is well-regarded as one of the most effective treatments, with Roux-en-Y gastric bypass (RYGB) being one of the most common types performed [1,3]. Mesenteric defects formed in the process of creating the bypass predispose patients to develop rare and clinically ambiguous internal hernias [4,5]. If unrecognized, internal hernias can have serious consequences, including incarceration, strangulation, and death [5,6]. We report an internal hernia case with classic findings on computed tomography (CT) in a patient with a remote history of RYGB.
Case presentation
A 66-year-old woman with a history of suboxone-treated IV drug use, chronic back pain, laparoscopic RYGB, and laparoscopic cholecystectomy presented to the emergency department with two days of intermittent, colicky pain in the upper abdomen with associated nausea, epigastric fullness, and vomiting. During this time, she continued to have normal flatus and regular, formed bowel movements. She denied having previous issues or revisional procedures for her RYGB, which was created using the antecolic technique 20 years ago. Per the patient's report, her pre-procedural weight was 320 lbs, and her post-procedural weight was 220 lbs. However, she also had an unintentional 30 lbs weight loss in the last six months.
Her vital signs at the presentation were stable. On physical exam, her abdomen was soft and distended with epigastric tenderness but without guarding or rebound tenderness. Lab results were unremarkable (Table 1). Abdominal ultrasound was negative for acute pathology. The chest X-ray was also unremarkable aside from a small hiatal hernia at the right cardiac border.
Table 1. The patient's lab results at presentation.
Bolded text are values in the abnormal range.
MCV: mean corpuscular volume; MCH: mean corpuscular hemoglobin; MCHC: mean corpuscular hemoglobin concentration; RDW: red cell distribution width; MPV: mean platelet volume; eGFR: estimated glomerular filtration rate
| Component | Value | Normal range |
| Complete blood count | ||
| White blood cell count | 9.4 | 4.5-11.0 k/mm3 |
| Red blood cell count | 4.71 | 4.00-5.20 m/mm3 |
| Hemoglobin | 12.8 | 12.0-16.0 g/dL |
| Hematocrit | 39.4 | 36.0-46.0% |
| MCV | 83.8 | 80.0-100.0 fL |
| MCH | 27.3 | 27.0-33.0 pg |
| MCHC | 32.5 | 32.0-36.0% |
| RDW | 14.9 | 0.0-14.7% |
| MPV | 8.8 | 6.8-10.0 fL |
| Platelet count | 206 | 130-400 k/mm3 |
| Basic metabolic panel | ||
| Sodium | 140 | 136-145 mmol/L |
| Potassium | 4.3 | 3.4-5.1 mmol/L |
| Chloride | 103 | 98-107 mmol/L |
| Carbon dioxide total | 25 | 22-29 mmol/L |
| Anion gap | 12 | 7-15 mmol/L |
| Urea nitrogen, blood (BUN) | 15 | 6-20 mg/dL |
| Creatinine serum | 0.59 | 0.51-1.17 mg/dL |
| Glucose | 140 | 74-109 mg/dL |
| Calcium | 9.7 | 8.6-10.0 mg/dL |
| e-GFR creatinine (female) | 7.4 | >30 mL/min/1.73m*2 |
| Urinalysis | ||
| Collection | Clean catch | |
| Color | Yellow | None/yellow |
| Clarity | Clear | Clear |
| pH Urine | 5 | 4.8-7.8 |
| Occult blood urine | Negative | Negative |
| Bilirubin urine | Negative | Negative |
| Ketones | 80 | Negative |
| Glucose urine | Negative | Negative |
| Protein urine | Negative | Negative |
| Urobilinogen | Negative | Negative |
| Nitrite urine | Negative | Negative |
| Leukocyte esterase | Negative | Negative |
| Microscopic | Not indicated | Not indicated |
| Urine culture | Not indicated | Not indicated |
| Hepatic function panel | ||
| Protein | 7.4 | 6.6-8.7 g/dL |
| Albumin | 4.3 | 4.0-4.9 g/dL |
| Alkaline phosphatase (ALP) | 78 | 35-129 U/L |
| Aspartate transaminase (AST) | 14 | ≤41 U/L |
| Bilirubin total | 0.5 | 0.0-0.3 mg/dL |
| Alanine transferase (ALT) | 10 | ≤33 U/L |
| Bilirubin direct | 0.2 | 0.0-0.3 mg/dL |
| Other | ||
| Lipase | 14 | 13-60 U/L |
| Troponin T | <6 | ≤19 ng/L |
| Lactic acid | 0.9 | 0.5-2.2 mmol/L |
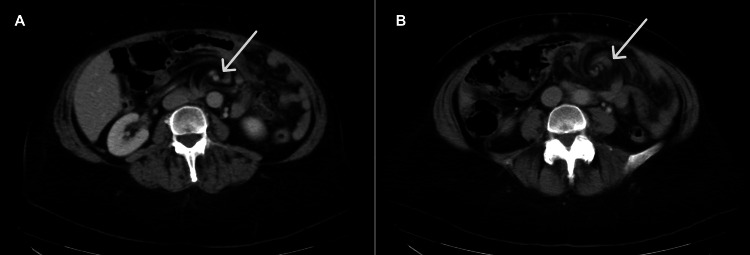
CT abdomen with contrast showed mesenteric edema stranding and swirling in the left upper abdomen, which was concerning for mesenteric volvulus (Figure 1). Notably, there was a distorted course and caliber of multiple vessels and bowel loops. The superior mesenteric vein was distorted below the pancreaticoduodenal vein with multiple occluded colic branches. There were no definite signs of small bowel obstruction.
Figure 1. CT abdomen and pelvis (axial). The mesenteric swirl sign, indicative of mesenteric edema and distortion of vessels and bowel loops, can be seen at the arrow in two slices (A: superior; B: inferior).
The patient was diagnosed with an internal hernia and subsequently taken to surgery for a diagnostic laparoscopy and internal hernia repair. Intraoperatively, the jejunojejunostomy was noted to have twisted on itself, with a portion of the common channel herniated through the jejunojejunostomy mesenteric defect. After untwisting, all segments of the bowel were still viable, and the hernia was reduced with the closure of the defect with a non-absorbable 0-Surgidac running suture. The patient tolerated the procedure well, and she was discharged two days post-operation with no complications.
Discussion
RYGB patients represent a unique population that is at increased risk of developing internal hernias given their surgically modified anatomy. Internal hernias are rare, with an overall incidence of less than 1% in the general population and between 0.2% and 9% in bariatric surgery patients, but they cause nearly half of all bowel obstructions in post-RYGB patients [5,7]. In present literature, they have been reported to commonly occur 6 to 24 months post-procedure, which is during the period of greatest expected weight loss [8,9]. Weight loss allows defects in the mesentery to reopen despite intraoperative closure, increasing the risk of internal hernias [10]. Our case study exemplifies that there is still a possibility of presentation even as far as 20 years out from the original procedure. In our patient, her risk was likely magnified by her recent, unintentional, and significant weight loss.
The creation of the bypass results in three potential sites of weakness: the transmesocolon mesentery, jejunojejunostomy mesentery, and Petersen’s space [4-8]. A defect in the transmesocolon mesentery is only formed when using the retrocolic technique of joining the Roux limb with the gastric pouch, and these hernias are the most common type [5,7,8,11]. An antecolic technique and surgical standards to take care to close mesenteric defects during the procedure may decrease the overall risk of internal hernias [8,11].
Internal hernias are notoriously difficult to diagnose given their non-specific and variable presentations. Patients with reducible hernias are often asymptomatic, but complications such as strangulation and incarceration can develop and lead to increased mortality if recognition is delayed [5,6]. Common symptoms include epigastric or periumbilical abdominal pain (described as postprandial, vague, or colicky), nausea, and vomiting [5,7,11]. It was reassuring that our patient remained hemodynamically stable and continued to have regular bowel function leading up to the procedure. The absence of laboratory and radiographic signs of bowel obstruction and ischemia further supported a less severe presentation, but surgical treatment was still indicated to minimize further complications.
CT has been the most useful in diagnosis given its ability to offer clarity of anatomic structures compared to plain abdominal radiographs. One of the best predictors is the presence of a “mesenteric swirl” formed from distorted mesenteric fat and vessels [4,7,12,13], as seen in our patient. When seen in conjunction with small bowel obstruction, the sensitivity and specificity can reach up to 96% and 87%, respectively [13]. Other helpful CT signs have been identified, including the mushroom sign, superior mesenteric vein beaking, hurricane eye, criss-cross appearance, small bowel behind superior mesenteric artery, weeping mesentery, and right-sided anastomosis [4,5]. Treatment is surgery to repair the hernia [11].
Conclusions
We present in this case study a unique internal hernia case that developed 20 years after RYGB, likely complicated by our patient's unexpected weight loss outside of the typical period of post-RYGB weight loss. Internal hernias are notoriously difficult to diagnose given their non-specific presentation and, as exemplified in this case, should be considered in the differential even if patients are years out from their bowel revision surgery. CT is the most reliable modality in work-up, and signs of mesenteric swirling and small bowel obstruction are most predictive of the presence of an internal hernia.
Disclosures
Human subjects: Consent was obtained or waived by all participants in this study.
Conflicts of interest: In compliance with the ICMJE uniform disclosure form, all authors declare the following:
Payment/services info: All authors have declared that no financial support was received from any organization for the submitted work.
Financial relationships: All authors have declared that they have no financial relationships at present or within the previous three years with any organizations that might have an interest in the submitted work.
Other relationships: All authors have declared that there are no other relationships or activities that could appear to have influenced the submitted work.
Author Contributions
Concept and design: Katherine Liu, Michael C. Larson
Acquisition, analysis, or interpretation of data: Katherine Liu, Lyanne Lu, Brandon Wong
Drafting of the manuscript: Katherine Liu
Critical review of the manuscript for important intellectual content: Katherine Liu, Michael C. Larson, Lyanne Lu, Brandon Wong
Supervision: Katherine Liu, Michael C. Larson
References
- 1.US national trends in bariatric surgery: a decade of study. Alalwan AA, Friedman J, Park H, Segal R, Brumback BA, Hartzema AG. Surgery. 2021;170:13–17. doi: 10.1016/j.surg.2021.02.002. [DOI] [PubMed] [Google Scholar]
- 2.Overweight & obesity statistics - NIDDK. [ Feb; 2024 ]. https://www.niddk.nih.gov/health-information/health-statistics/overweight-obesity https://www.niddk.nih.gov/health-information/health-statistics/overweight-obesity
- 3.Examining the rates of obesity and bariatric surgery in the United States. Altieri MS, Irish W, Pories WJ, Shah A, DeMaria EJ. Obes Surg. 2021;31:4754–4760. doi: 10.1007/s11695-021-05628-y. [DOI] [PubMed] [Google Scholar]
- 4.Internal hernias: a difficult diagnostic challenge. Review of CT signs and clinical findings. Monica ML, Antonella M, Gloria A, et al. Acta Biomed. 2019;90:20–37. doi: 10.23750/abm.v90i5-S.8344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Review of internal hernias: radiographic and clinical findings. Martin LC, Merkle EM, Thompson WM. Am J Roentgenol. 2006;186:703–717. doi: 10.2214/AJR.05.0644. [DOI] [PubMed] [Google Scholar]
- 6.Internal hernia complications of gastric bypass surgery in the acute setting: spectrum of imaging findings. Patel RY, Baer JW, Texeira J, Frager D, Cooke K. Emerg Radiol. 2009;16:283–289. doi: 10.1007/s10140-008-0781-7. [DOI] [PubMed] [Google Scholar]
- 7.CT scan reliability in detecting internal hernia after gastric bypass. Farukhi MA, Mattingly MS, Clapp B, Tyroch AH. JSLS. 2017;21 doi: 10.4293/JSLS.2017.00054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Laparoscopic antecolic Roux-En-Y gastric bypass with closure of internal defects leads to fewer internal hernias than the retrocolic approach. Steele KE, Prokopowicz GP, Magnuson T, Lidor A, Schweitzer M. Surg Endosc. 2008;22:2056–2061. doi: 10.1007/s00464-008-9749-7. [DOI] [PubMed] [Google Scholar]
- 9.Assessment of weight change patterns following Roux en Y gastric bypass, one anastomosis gastric bypass and sleeve gastrectomy using change-point analysis. Boustani P, Sheidaei A, Mokhber S, Pazouki A. Sci Rep. 2024;14:17416. doi: 10.1038/s41598-024-68480-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Failure of mesenteric defect closure after Roux-en-Y gastric bypass. Hope WW, Sing RF, Chen AY, Lincourt AE, Gersin KS, Kuwada TS, Heniford BT. JSLS. 2010;14:213–216. doi: 10.4293/108680810X12785289144151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Internal hernia after laparoscopic Roux-en-Y gastric bypass. Obeid A, McNeal S, Breland M, Stahl R, Clements RH, Grams J. J Gastrointest Surg. 2014;18:250–256. doi: 10.1007/s11605-013-2377-0. [DOI] [PubMed] [Google Scholar]
- 12.Internal hernia after gastric bypass: Sensitivity and specificity of seven CT signs with surgical correlation and controls. Lockhart ME, Tessler FN, Canon CL, et al. Am J Roentgenol. 2007;188:745–750. doi: 10.2214/AJR.06.0541. [DOI] [PubMed] [Google Scholar]
- 13.Internal hernia after laparoscopic roux-en-Y gastric bypass: optimal CT signs for diagnosis and clinical decision making. Dilauro M, Mcinnes MDF, Schieda N, et al. Radiology. 2017;282:752–760. doi: 10.1148/radiol.2016160956. [DOI] [PubMed] [Google Scholar]