Abstract
Background
This study investigated the prevalence and predictors of episiotomy among puerperal women accessing postnatal care in the Kumasi Metropolis.
Methods
A cross-sectional survey was conducted among 1750 postnatal mothers who had spontaneous vaginal using a questionnaire. Descriptive statistics were conducted to show the rate of episiotomy. Chi-square and binary logistic regression analyses were conducted using Jamovi software version 2.5.3.
Results
The prevalence of episiotomy among the study population was 49.7% compared to the 10% of all deliveries recommended by World Health Organisation (WHO). Among those who had an episiotomy, 88.5% gave consent, and 77.6% required repairs. In the bivariate analysis educational status, age, perineal tearing, marital status, household monthly income, spontaneous vaginal deliveries and previous episiotomy had a significant association with episiotomy risk. In the multivariate analysis, married women, lower education levels, moderate household incomes, grand multiparous women, spontaneous vaginal delivery (SVD), instrumental deliveries, longer second stages of labour, and attending more antenatal care (ANC) sessions were all associated with a reduced likelihood of episiotomy. Higher one-minute Apgar scores and anemia also lowered the odds. Conversely, hypertensives, women with four or more previous vaginal deliveries, and those with a history of episiotomy were more likely to undergo the procedure.
Conclusion
Episiotomies conducted was high, indicating potential overuse compared to WHO’s recommendations. Antenatal attendance and timing should be prioritised to improve maternal preparation and outcomes. Policy interventions to reduce unnecessary episiotomies are needed. Midwifery education must also emphasise the importance of respectful maternity care.
Keywords: Episiotomy, Prevalence, Predictors, Puerperal women, Africa
Background
Maternal health remains a critical concern despite concerted efforts to improve healthcare access and outcomes in sub-Saharan Africa [1]. Puerperal women, particularly those accessing postnatal care, represent a vulnerable demographic requiring focused attention due to the complexities surrounding childbirth-related complications [2]. An episiotomy is a surgical incision made in the perineum, the area between the vagina and the anus, during childbirth [3].
Historically, episiotomy procedures have been employed as a preventive measure against severe perineal tears and trauma, aiming to facilitate the childbirth process and reduce maternal complications such as pelvic floor dysfunction and urinary or faecal incontinence [4]. This incision is typically made either mediolaterally (towards the side) or midline, depending on obstetric practices and provider preference [5]. By creating a controlled incision, episiotomy aims to facilitate the childbirth process and reduce the risk of extensive tearing [6]. Episiotomy was first reported in the 18th Century [7]. It was once considered a routine intervention in obstetric care, especially in situations where augmentation of labour was deemed necessary or when instrumental births, such as forceps or vacuum extraction, were anticipated [8]. However, over the past few decades, the routine use of episiotomy has come under scrutiny due to emerging evidence suggesting potential risks, including increased maternal perineal pain, prolonged wound healing times, and an elevated risk of perineal trauma compared to spontaneous perineal tearing [9].
Globally, episiotomy rates exhibit significant variability, with high-income countries witnessing substantial declines, often plummeting to rates as low as 10% or even less, with the adoption of evidence-based obstetric practices [10]. Notably, a contrast exists between the routine performance of episiotomies in Sub-Saharan Africa and high-income European countries [11]. In lower-middle-income countries (LMICs), such as Burkina Faso (22%) [12] and in Nigeria (62%) [13]. Higher episiotomy rates are higher due to limited access to obstetric care and the scarcity of alternative interventions and skilled birth attendants [14]. Evidence suggests that delayed second stage of labour, presence of face presentation, birth weight exceeding 4000 g, use of instrumental delivery, and primiparity among women were identified as obstetric factors linked to episiotomy [15].
Several factors influence episiotomy rates, including cultural practices and beliefs [7, 16]. Depending on the cultural beliefs surrounding childbirth and perineal health, episiotomy may be viewed as either necessary or unnecessary, thus influencing its prevalence [17]. Cultural attitudes towards pain management and endurance during childbirth can affect the acceptance of interventions like episiotomy. For instance, in cultures where women are expected to endure pain stoically during childbirth, healthcare providers may be more inclined to perform episiotomies to expedite childbirth and minimise perceived suffering [18]. In some cultures, female elders or traditional birth attendants play a significant role in guiding childbirth practices. Their knowledge and beliefs about perineal health and the necessity of interventions like episiotomy can influence healthcare-seeking behaviour and decision-making during childbirth [2, 19]. Cultural beliefs in the efficacy of herbal remedies or traditional healing techniques to promote perineal healing and prevent complications may influence the acceptance or avoidance of episiotomy. Sub-Saharan Africa, with its diverse cultural landscape and healthcare systems, presents a unique context for exploring the prevalence and predictors of episiotomy among puerperal women accessing postnatal care.
Ghana, like many LMICs, continues to have episiotomy performed unabated [10]. Cultural norms and beliefs surrounding childbirth, including episiotomy, may be influenced by a blend of traditional practices, modern healthcare interventions, and sociocultural factors [2]. The period following childbirth continues to be the most vulnerable time for the mother and her infant [20]. In the context of the Kumasi Metropolis, despite episiotomy being a commonly practised obstetric intervention, there is a lack of comprehensive data on its prevalence and the factors influencing its performance in this urban centre. Therefore, this study sought to investigate the prevalence and predictors of episiotomy among puerperal women accessing postnatal care in the Kumasi Metropolis.
Methods
Design and participants
This cross-sectional survey was conducted among 1750 postnatal mothers who had spontaneous vaginal delivery in the Kumasi Metropolis. Thus, 1750 represented a response rate of approximately 83%. The study sites include five hospitals within the Kumasi Metropolis: Suntreso Government Hospital, Ashanti Regional Regional Hospital, Manhyia Government Hospital, Tafo Government Hospital and Maternal and Child Health Hospital. These hospitals were purposively selected for their optimal geographical locations and to ensure accessibility to a diverse population within the metropolis. These hospitals serve as key healthcare centres catering to a wide range of patients from various socio-economic backgrounds and residential areas.
Additionally, these hospitals were identified for their high capacity to provide postnatal care (PNC) services and their significant attendance rates for delivery services. Mothers who had recently given birth (within the past six weeks before data collection) were included in this study. Postnatal mothers who were sick were excluded.
Data collection instrument
A survey questionnaire was developed based on items used in previous studies [21, 22]. The items were adapted to ensure cultural and contextual relevance. The survey questionnaire had two sections: Section A comprised five questions on the socio-demographic background of postnatal mothers, including age, educational level, marital status, occupation, and monthly income. Section B comprised 22 items addressing obstetric history and facility factors supplemented by essential information from the maternal record book provided by the Ghana Health Service.
Data collection procedure
Postnatal mothers who had received PNC services or were on break were conveniently sampled so as not to disrupt the clinical duties of the healthcare providers. Participants received an informed consent document detailing the study’s purpose, duration, and potential risks. Only postnatal mothers who voluntarily agreed and provided consent were included in this study. Five trained Research Assistants (RAs) conducted face-to-face survey interviews. The survey questionnaire was translated into Twi, the most widely spoken local dialect in Kumasi, and then back into English to ensure translation accuracy. Clear communication was maintained about the study’s significance. Participants completed the survey interviews in 10 to 20 min. No compensations were provided to prevent undue influence. Data collection spanned two months (March 1 2024 to May 5, 2024). Ethical considerations were paramount, with participants informed of their voluntary participation, the right to withdraw without penalty, the right to skip survey interview items and the assurance of anonymity and confidentiality.
Data analysis
Descriptive statistics using frequency and percentages were presented to show the episiotomy rate among postnatal mothers. A bivariate analysis using the Chi-square test of distribution was conducted to determine the independent variables (socio-demographic, obstetric history, and facility factors) associated with the dependent variable (occurrence of episiotomy). Independent variables that were significant in the bivariate phase were moved into the multivariate phase. Episiotomy occurrence was dichotomised (reported no episiotomy (0) and reported episiotomy [1]. Hence, a binary logistic regression was conducted. Jamovi statistical software version 2.5.3 was used in the statistical analysis.
Results
Prevalence of episiotomy
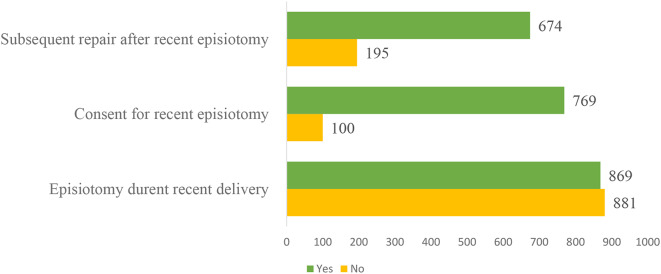
The table presents data on episiotomies performed during recent deliveries, including consent and subsequent repairs. Out of the total puerperal mothers (1750), 869 (49.7%) women underwent an episiotomy, while 881 (50.3%) did not. Thus, approximately 1 out of 2 puerperal mothers who recently delivered experienced episiotomy. Among those who had an episiotomy, 769 (88.5%) provided consent, whereas 100 (11.5%) did not. Additionally, of the women who had an episiotomy, 674 (77.6%) required subsequent repairs, and 195 (22.4%) did not require subsequent repairs. See Fig. 1 for the details.
Fig. 1.
Prevalence of recent episiotomy, consent and repair after episiotomy
Risk factors for episiotomy among puerperal women
Bivariate association
Table 1 provides insights into the bivariate correlation between several main variables and the risk of episiotomy during delivery, as determined by Chi-square tests. Age demonstrated a significant association (X² = 67.9, p < 0.001), with the risk of episiotomy varying across different age groups. Marital status also showed significance (X² = 50.2, p < 0.001), highlighting varying episiotomy rates among different marital statuses. Educational status exhibited a substantial correlation (X² = 84.7, p < 0.001), indicating differences in episiotomy likelihood based on educational background. Household monthly income displayed significance (X² = 40.2, p < 0.001), suggesting an association between income levels and the risk of episiotomy. Previous pregnancies (X² = 58.5, p < 0.001) and vaginal deliveries (X² = 20.4, p < 0.001) were strongly correlated with episiotomy risk. Additionally, previous episiotomy (X² = 7.93, p = 0.005) and perineal tearing (X² = 67, p < 0.001) were associated with an increased likelihood of episiotomy in subsequent deliveries. Delivery-related factors such as the type of delivery (X² = 20.6, p < 0.001) and the attending healthcare provider (X² = 23.2, p < 0.001) also demonstrated significant correlations with episiotomy risk. Neonatal health indicators, including Apgar score at one minute (X² = 25.4, p < 0.001) and birth weight (X² = 8.94, p = 0.011), were associated with the conduct of episiotomy. Furthermore, pre-existing medical conditions (X² = 18.8, p < 0.001) and factors related to antenatal care, such as the number of ANC attendances (X² = 25.4, p < 0.001) and the trimester for the first ANC visit (X² = 11.7, p = 0.003), showed significant correlations with episiotomy risk. All significant variables presented were included in the multivariate regression model presented in Table 2.
Table 1.
Bivariate correlation (Chi-square distribution) between factors and risk of episiotomy
| Variables | Categories | No Episiotomy | Episiotomy | X2 | P-value | ||
|---|---|---|---|---|---|---|---|
| Frequency | Percentage (%) | Frequency | Percentage (%) | ||||
| Age | 14–19 years | 34 | 1.9% | 102 | 5.8% | 67.9 | 0.000 |
| 20–34 years | 655 | 37.4% | 670 | 38.3% | |||
| 35–40 years | 176 | 10.1% | 94 | 5.4% | |||
| ≥ 41 years | 16 | 0.9% | 3 | 0.2% | |||
| Marital status | Single | 253 | 14.5% | 368 | 21.0% | 50.2 | 0.000 |
| Married | 628 | 35.9% | 501 | 28.6% | |||
| Educational status | No education | 70 | 4% | 83 | 4.7% | 84.7 | 0.000 |
| Basic education | 366 | 20.9% | 222 | 12.7% | |||
| Secondary education | 337 | 19.3% | 327 | 18.7% | |||
| Tertiary education | 108 | 6.2% | 237 | 13.5% | |||
| Household monthly income | ≤ 500 GHS | 535 | 30.6% | 528 | 30.2% | 40.2 | 0.000 |
| 501–1000 GHS | 148 | 8.5% | 87 | 5% | |||
| 1001–2000 GHS | 119 | 6.8% | 199 | 11.4% | |||
| ≥ 2001 GHS | 79 | 4.5% | 55 | 3.1% | |||
| Previous pregnancies | 1 pregnancy | 128 | 7.3% | 214 | 12.2% | 58.5 | 0.000 |
| 2–4 pregnancies | 636 | 36.3% | 614 | 35.1% | |||
| ≥ 5 pregnancies | 117 | 6.7% | 41 | 2.3% | |||
| Previous vaginal deliveries | 1 vaginal delivery | 224 | 12.8% | 299 | 17.1% | 20.4 | 0.000 |
| 2–3 vaginal deliveries | 606 | 34.6% | 541 | 30.9% | |||
| ≥ 4 vaginal deliveries | 51 | 2.9% | 29 | 1.7% | |||
| Previous CS deliveries | No CS delivery | 738 | 42.2% | 776 | 44.3% | 42.3 | 0.000 |
| 1 CS delivery | 102 | 5.8% | 93 | 5.3% | |||
| ≥ 2 CS deliveries | 41 | 2.3% | - | - | |||
| Previous episiotomy | No | 426 | 24.3% | 362 | 20.7% | 7.93 | 0.005 |
| Yes | 455 | 26% | 507 | 29% | |||
| Previous perineal tearing | No | 367 | 21% | 532 | 30.4% | 67 | 0.000 |
| Yes | 514 | 29.4% | 337 | 19.3% | |||
| Types of current delivery | Breech delivery | 818 | 46.7% | 835 | 47.7% | 20.6 | 0.000 |
| SVD | 35 | 2% | 6 | 0.3% | |||
| Instrumental delivery | 28 | 1.6% | 28 | 1.6% | |||
| Who did recent delivery | Midwife | 797 | 45.5% | 832 | 47.5% | 23.2 | 0.000 |
| Rotation midwife | 43 | 2.5% | 27 | 1.5% | |||
| Others | 41 | 2.3% | 10 | 0.6% | |||
| Apgar score at one minute | ≤ 4 | 9 | 0.5% | 15 | 0.9% | 25.4 | 0.000 |
| 5–7 | 297 | 17% | 389 | 22.2% | |||
| ≥ 8 | 575 | 32.9% | 465 | 26.6% | |||
| Birth weight | < 2.5 kg | 25 | 1.4% | 26 | 1.5% | 8.94 | 0.011 |
| 2.5–4 kg | 836 | 47.8% | 838 | 47.9% | |||
| > 4 kg | 20 | 1.1% | 5 | 0.3% | |||
| Pre-existing medical condition | None | 767 | 43.8% | 780 | 44.6% | 18.8 | 0.000 |
| Anemia | 74 | 4.2% | 38 | 2.2% | |||
| Asthma/heart disease | 9 | 0.5% | 3 | 0.2% | |||
| diabetes | 9 | 0.5% | 18 | 1% | |||
| Hypertension | 22 | 1.3% | 30 | 1.7% | |||
| Duration of second stage of labour | ≤ 30 min | 659 | 37.7% | 707 | 40.4% | 18.8 | 0.000 |
| 31–60 min | 198 | 11.3% | 157 | 9% | |||
| ≥ 61 min | 24 | 1.4% | 5 | 0.3% | |||
| ANC attendance | ≤ 3 ANC attendance | 16 | 0.9% | 23 | 1.3% | 25.4 | 0.000 |
| 4–8 ANC attendance | 411 | 23.5% | 502 | 28.7% | |||
| ≥ 9 ANC attendance | 454 | 25.9% | 344 | 19.7% | |||
| Trimester for first ANC | First trimester | 631 | 36.1% | 682 | 39% | 11.7 | 0.003 |
| Second trimester | 228 | 13% | 166 | 9.5% | |||
| Third trimester | 22 | 1.3% | 21 | 1.2% | |||
Table 2.
Binary logistic regression of factors associated with risk of episiotomy
| Variables | Categories | 95% Confidence Interval | ||||||
|---|---|---|---|---|---|---|---|---|
| Estimate | SE | Z-score | p-value | AOR | Lower | Upper | ||
| Intercept | 4.9256 | 0.832 | 5.9235 | < 0.001 | 137.7730 | 26.99962 | 703.025 | |
| Age | 14–19 years | Ref | Ref | Ref | Ref | Ref | Ref | Ref |
| 20–34 years | -1.3281 | 0.267 | -4.9664 | < 0.001 | 0.2650 | 0.15689 | 0.448 | |
| 35–40 years | -1.6402 | 0.318 | -5.1585 | < 0.001 | 0.1939 | 0.10399 | 0.362 | |
| ≥ 41 years | -2.8611 | 1.046 | -2.7342 | 0.006 | 0.0572 | 0.00736 | 0.445 | |
| Marital status | Single | Ref | Ref | Ref | Ref | Ref | Ref | Ref |
| Married | -0.9186 | 0.143 | -6.4174 | < 0.001 | 0.3991 | 0.30145 | 0.528 | |
| Educational status | No education | Ref | Ref | Ref | Ref | Ref | Ref | Ref |
| Basic education | -1.0507 | 0.231 | -4.5464 | < 0.001 | 0.3497 | 0.22230 | 0.550 | |
| Secondary education | -0.5667 | 0.231 | -2.4560 | 0.014 | 0.5674 | 0.36095 | 0.892 | |
| Tertiary education | 0.6935 | 0.276 | 2.5151 | 0.012 | 2.0007 | 1.16541 | 3.435 | |
| Household monthly income | ≤ 500 GHS | Ref | Ref | Ref | Ref | Ref | Ref | Ref |
| 501–1000 GHS | -0.9952 | 0.193 | -5.1575 | < 0.001 | 0.3696 | 0.25324 | 0.540 | |
| 1001–2000 GHS | 0.4151 | 0.201 | 2.0623 | 0.039 | 1.5145 | 1.02080 | 2.247 | |
| ≥ 2001 GHS | -0.5857 | 0.251 | -2.3366 | 0.019 | 0.5567 | 0.34060 | 0.910 | |
| Previous pregnancies | 1 pregnancy | Ref | Ref | Ref | Ref | Ref | Ref | Ref |
| 2–4 pregnancies | 0.0607 | 0.260 | 0.2332 | 0.816 | 1.0625 | 0.63818 | 1.769 | |
| ≥ 5 pregnancies | -1.2951 | 0.433 | -2.9885 | 0.003 | 0.2739 | 0.11712 | 0.640 | |
| Previous vaginal deliveries | 1 vaginal delivery | Ref | Ref | Ref | Ref | Ref | Ref | Ref |
| 2–3 vaginal deliveries | -0.1170 | 0.227 | -0.5154 | 0.606 | 0.8896 | 0.57015 | 1.388 | |
| ≥ 4 vaginal deliveries | 1.0295 | 0.497 | 2.0700 | 0.038 | 2.7997 | 1.05624 | 7.421 | |
| Previous CS deliveries | No CS delivery | Ref | Ref | Ref | Ref | Ref | Ref | Ref |
| 1 CS delivery | -0.0920 | 0.214 | -0.4305 | 0.667 | 0.9121 | 0.59985 | 1.387 | |
| ≥ 2 CS deliveries | -17.5858 | 298.781 | -0.0589 | 0.953 | 2.3008 | 1.10262 | 4.8246 | |
| Previous episiotomy | No | Ref | Ref | Ref | Ref | Ref | Ref | Ref |
| Yes | 1.1300 | 0.148 | 7.6393 | < 0.001 | 3.0956 | 2.31650 | 4.137 | |
| Previous perineal tearing | No | Ref | Ref | Ref | Ref | Ref | Ref | Ref |
| Yes | -1.2764 | 0.146 | -8.7149 | < 0.001 | 0.2791 | 0.20942 | 0.372 | |
| Types of current delivery | Breech delivery | Ref | Ref | Ref | Ref | Ref | Ref | Ref |
| SVD | -1.9982 | 0.706 | -2.8306 | 0.005 | 0.1356 | 0.03399 | 0.541 | |
| Instrumental delivery | -0.8579 | 0.362 | -2.3686 | 0.018 | 0.4241 | 0.20851 | 0.862 | |
| Who did recent delivery | Midwife | Ref | Ref | Ref | Ref | Ref | Ref | Ref |
| Rotation midwife | -0.6496 | 0.308 | -2.1094 | 0.035 | 0.5223 | 0.28559 | 0.955 | |
| Others | 0.8552 | 0.517 | 1.6545 | 0.098 | 2.3518 | 0.85393 | 6.477 | |
| Apgar score at one minute | ≤ 4 | Ref | Ref | Ref | Ref | Ref | Ref | Ref |
| 5–7 | -0.3505 | 0.489 | -0.7172 | 0.473 | 0.7044 | 0.27031 | 1.835 | |
| ≥ 8 | -1.1489 | 0.487 | -2.3601 | 0.018 | 0.3170 | 0.12208 | 0.823 | |
| Birth weight | < 2.5 kg | Ref | Ref | Ref | Ref | Ref | Ref | Ref |
| 2.5–4 kg | 0.2636 | 0.354 | 0.7451 | 0.456 | 1.3017 | 0.65060 | 2.604 | |
| > 4 kg | 0.7267 | 0.669 | 1.0862 | 0.277 | 2.0683 | 0.55732 | 7.676 | |
| Pre-existing medical condition | None | Ref | Ref | Ref | Ref | Ref | Ref | Ref |
| Anemia | -0.6289 | 0.253 | -2.4828 | 0.013 | 0.5332 | 0.32455 | 0.876 | |
| Asthma/heart disease | -1.3330 | 0.790 | -1.6882 | 0.091 | 0.2637 | 0.05610 | 1.239 | |
| diabetes | 3.4656 | 0.837 | 4.1391 | < 0.001 | 31.9943 | 6.19978 | 165.108 | |
| Hypertension | 0.7703 | 0.396 | 1.9430 | 0.042 | 2.1604 | 0.99331 | 4.699 | |
| Duration of second stage of labour | ≤ 30 min | Ref | Ref | Ref | Ref | Ref | Ref | Ref |
| 31–60 min | -0.5551 | 0.160 | -3.4797 | < 0.001 | 0.5740 | 0.41988 | 0.785 | |
| ≥ 61 min | -2.5283 | 0.760 | -3.3281 | < 0.001 | 0.0798 | 0.01800 | 0.354 | |
| ANC attendance | ≤ 3 ANC attendance | Ref | Ref | Ref | Ref | Ref | Ref | Ref |
| 4–8 ANC attendance | -1.1679 | 0.485 | -2.4097 | 0.016 | 0.3110 | 0.12030 | 0.804 | |
| ≥ 9 ANC attendance | -1.7370 | 0.500 | -3.4725 | < 0.001 | 0.1760 | 0.06605 | 0.469 | |
| Trimester for first ANC | First trimester | Ref | Ref | Ref | Ref | Ref | Ref | Ref |
| Second trimester | -0.8643 | 0.161 | -5.3643 | < 0.001 | 0.4214 | 0.30726 | 0.578 | |
| Third trimester | -0.8464 | 0.511 | -1.6553 | 0.098 | 0.4289 | 0.15745 | 1.169 | |
Multivariate associations
The independent variables in the binary regression model explained 38.7% of the variance in risk of episiotomy (Nagelkerke’s R2 = 0.387). Maternal age plays a crucial role, with women aged 20–34 years being 73.5% less likely to undergo an episiotomy (AOR = 0.27, 95% CI: 0.16, 0.45, p < 0.001), those aged 35–40 years being 80.6% less likely (AOR = 0.19, 95% CI: 0.10, 0.36, p < 0.001), and women aged ≥ 41 years being 94.3% less likely (AOR = 0.06, 95% CI: 0.01, 0.45, p = 0.006) compared to those aged 14–19 years. Marital status also shows significant differences, with married women being 60.1% less likely to have an episiotomy compared to single women (AOR = 0.40, 95% CI: 0.30, 0.53, p < 0.001). Educational status demonstrates a notable impact. Women with basic education are 65.0% less likely to undergo an episiotomy compared to those with no education (AOR = 0.35, 95% CI: 0.22, 0.55, p < 0.001). Those with secondary education are 43.3% less likely (AOR = 0.57, 95% CI: 0.36, 0.89, p = 0.014). Interestingly, women with tertiary education are twice as likely to have an episiotomy compared to those with no education (AOR = 2.00, 95% CI: 1.17, 3.44, p = 0.012). Women with household monthly incomes of 501–1000 GHS are 63.0% less likely to have an episiotomy compared to those with incomes of ≤ 500 GHS (AOR = 0.37, 95% CI: 0.25, 0.54, p < 0.001). Women whose incomes range between 1001 and 2000 GHS are 1.5 times more likely to undergo an episiotomy (AOR = 1.51, 95% CI: 1.02, 2.25, p = 0.039). Women with household incomes ≥ 2001 GHS are 44.3% less likely to have an episiotomy than the lowest income group (AOR = 0.56, 95% CI: 0.34, 0.91, p = 0.019).
Women with five or more previous pregnancies are 72.6% less likely to have an episiotomy compared to those with only one previous pregnancy (AOR = 0.27, 95% CI: 0.12, 0.64, p = 0.003). No significant association was found for women with 2–4 previous pregnancies (AOR = 1.06, 95% CI: 0.64, 1.77, p = 0.816). Women with four or more previous spontaneous vaginal deliveries are 2.8 times more likely to undergo an episiotomy compared to those with only one previous spontaneous vaginal delivery (AOR = 2.80, 95% CI: 1.06, 7.42, p = 0.038). There was no significant difference for women with 2–3 previous spontaneous vaginal (AOR = 0.89, 95% CI: 0.57, 1.39, p = 0.606).
There was no significant association between previous cesarean section (CS) births and the likelihood of episiotomy for women with one previous CS (AOR = 0.91, 95% CI: 0.60, 1.39, p = 0.667). The AOR for women with two or more previous CS deliveries was higher but statistically non-significant (AOR = 2.30, 95% CI: 1.10, 4.82, p = 0.953), suggesting variability in the data. Women who had a previous episiotomy are 3.1 times more likely to undergo an episiotomy in subsequent deliveries (AOR = 3.10, 95% CI: 2.32, 4.14, p < 0.001). Women with a history of previous perineal tearing are 72.1% less likely to have an episiotomy compared to those without such a history (AOR = 0.28, 95% CI: 0.21, 0.37, p < 0.001).
Women who had a spontaneous vaginal delivery (SVD) are 86.4% less likely to have an episiotomy compared to those who had a breech delivery (AOR = 0.14, 95% CI: 0.03, 0.54, p = 0.005). Women with an instrumental delivery are 57.6% less likely to undergo an episiotomy than those with a breech delivery (AOR = 0.42, 95% CI: 0.21, 0.86, p = 0.018). Women whose recent delivery was performed by a rotation midwife are 47.8% less likely to have an episiotomy than those performed by a regular midwife (AOR = 0.52, 95% CI: 0.29, 0.96, p = 0.035). There was no significant difference for deliveries performed by other healthcare providers compared to those performed by regular midwives (AOR = 2.35, 95% CI: 0.85, 6.48, p = 0.098).
Women whose babies had an Apgar score of 5–7 at one minute are less likely to have an episiotomy compared to those whose babies had a score of ≤ 4 (AOR = 0.70, 95% CI: 0.27, 1.84, p = 0.473). However, women whose babies had an Apgar score of ≥ 8 are less likely to undergo an episiotomy compared to those with a score of ≤ 4 (AOR = 0.32, 95% CI: 0.12, 0.82, p = 0.018). There is no significant association between birth weight and the likelihood of episiotomy. Women whose babies weighed 2.5–4 kg had an AOR of 1.30 (95% CI: 0.65, 2.60, p = 0.456) compared to babies weighing ≤ 2.4 kg. Similarly, women whose babies weighed ≥ 4.1 kg had an AOR of 2.07 (95% CI: 0.56, 7.68, p = 0.277). Women with anaemia are 46.7% less likely to have an episiotomy than those without pre-existing medical conditions (AOR = 0.53, 95% CI: 0.32, 0.88, p = 0.013). Those with asthma or heart disease are 73.6% less likely to undergo an episiotomy, though this finding is not statistically significant (AOR = 0.26, 95% CI: 0.06, 1.24, p = 0.091). Conversely, women with diabetes are significantly more likely to have an episiotomy, with an AOR of 31.99 (95% CI: 6.20, 165.11, p < 0.001). Women with hypertension showed a marginally significant increased likelihood of episiotomy (AOR = 2.16, 95% CI: 0.99, 4.70, p = 0.042).
Women whose second stage of labour lasted 31–60 min are 42.6% less likely to have an episiotomy compared to those whose labour lasted ≤ 30 min (AOR = 0.57, 95% CI: 0.42, 0.79, p < 0.001). Women whose second stage of labour lasted ≥ 61 min are 92.0% less likely to undergo an episiotomy compared to those with the shortest labour duration (AOR = 0.08, 95% CI: 0.02, 0.35, p < 0.001). Women who attended 4–8 ANC sessions are 69.0% less likely to have an episiotomy compared to those who attended ≤ 3 sessions (AOR = 0.31, 95% CI: 0.12, 0.80, p = 0.016). Those who attended ≥ 9 ANC sessions are 82.4% less likely to have an episiotomy (AOR = 0.18, 95% CI: 0.07, 0.47, p < 0.001). Women who began ANC in the second trimester are 57.9% less likely to undergo an episiotomy than those who started in the first trimester (AOR = 0.42, 95% CI: 0.31, 0.58, p < 0.001). For those who started ANC in the third trimester, there is no significant association with the likelihood of episiotomy (AOR = 0.43, 95% CI: 0.16, 1.17, p = 0.098).
Discussion
Summary of findings
Out of 1750 puerperal mothers, 49.7% underwent an episiotomy, while 50.3% did not. Among those who had an episiotomy, 88.5% gave consent, and 77.6% required repairs. Older women were significantly less likely to undergo episiotomy. Married women had a lower likelihood compared to single women. Lower educational levels were associated with reduced episiotomy rates, except for tertiary education, which showed higher rates. Moderate household incomes were linked to lower episiotomy likelihood, while higher incomes showed mixed results. Grand multiparous women (5 or >) with previous pregnancies had a significantly reduced likelihood of episiotomy compared to those with one previous pregnancy. Women with four or more previous vaginal deliveries were more likely to undergo an episiotomy. Previous CS deliveries were not significantly associated with episiotomy. Women with a history of episiotomy were more likely to undergo the procedure again, while those with a history of perineal tearing were less likely. SVD was associated with a lower likelihood of episiotomy than breech delivery, and instrumental deliveries also showed a reduced likelihood. Deliveries by rotation midwives had a lower likelihood of episiotomy compared to regular midwives. Higher infant Apgar scores at one minute decreased the likelihood of episiotomy. Birth weight was not significantly associated with episiotomy. Anaemia reduced the likelihood, while diabetes and hypertension increased it. Longer second stages of labour and attending more ANC sessions reduced the likelihood of episiotomy, with starting ANC in the second trimester also having a significant effect.
Prevalence, consent and subsequent repair of episiotomy
The data on episiotomies performed during recent deliveries among 1750 puerperal mothers offers several insights into clinical practices, patient consent, and post-procedural outcomes. Approximately 49.7% of the puerperal mothers underwent an episiotomy. This means that nearly half of the mothers in this sample experienced this surgical procedure during childbirth. This finding shows a relatively high prevalence of episiotomy compared with a previous study in Ghana in 2004 that reported a prevalence of 17.4% [23]. This suggests an increase in medical intervention during childbirth over the past two decades. This increase is consistent with a trend observed in some other lower- and middle-income countries where institutional birth and medical interventions during childbirth have become more common over time [7, 24–26]. Moreover, the current episiotomy rate is significantly higher than the World Health Organization’s (WHO) recommended rate of 10% [27], suggesting potential overuse and a deviation from global best practices.
The result of this study indicates that out of the 869 women who underwent an episiotomy, 769 (88.5%) provided consent, while 100 (11.5%) did not. This high rate of consented procedures highlights a generally positive trend towards patient involvement and informed decision-making in childbirth interventions. However, the fact that over one in ten women did not provide consent is a significant concern, suggesting gaps in communication and ethical practice within the healthcare system. The current finding is different from the finding from Brazil where 40.79% did not provide consent. However, some qualitative studies have shown that healthcare providers involved in episiotomy do not seek consent before the procedure in Iran [17] and London [28]. The act of not obtaining consent before performing a procedure is contrary to WHO standards, which emphasise the importance of informed consent in all medical procedures, including episiotomies, to ensure respect for patient autonomy and rights [27]. Furthermore, the issue of consent is fundamentally linked to the concept of respectful maternity care (RMC), which emphasises women’s dignity, privacy, and autonomy during childbirth [29]. Therefore, the rate of non-consensual episiotomies (11.5%) observed in this study highlights a breach in respectful maternity care, highlighting the need for improvement in how maternal care is delivered and perceived.
Additionally, among the women who had an episiotomy, 77.6% required subsequent repairs, while 22.4% did not. The need for subsequent repairs in such a high percentage of cases suggests that the practice of routine episiotomy may not be achieving its intended purpose of controlled perineal trauma [30]. Hence, this could contribute to complications such as infections, hemorrhage, incontinence, sexual dysfunction, prolonged healing, and potential long-term perineal pain necessitating further medical care [31, 32]. These complications are associated with subsequent repairs of episiotomy, maternal morbidity, increasing healthcare costs and the burden on healthcare systems [33]. Furthermore, while episiotomy-related deaths are rare, severe complications arising from poorly managed repairs, such as infections and hemorrhage can increase the risk of maternal mortality [33]. Therefore, the high rate of post-episiotomy repairs observed in this study and the associated complications that could arise may directly impact maternal morbidity and mortality, which are critical indicators for achieving SDG 3 since Ghana’s maternal mortality rate remains high, with postpartum hemorrhage and infections being key contributors [34]. Consequently, ensuring high standards of care during and after episiotomy procedures is crucial for minimising risks associated with subsequent repairs after the procedure. Additionally, promoting more restrictive episiotomy practices as recommended by the WHO should be encouraged since countries such as Sweden and the UK which utilise episiotomy judiciously, reported lower rates of post-procedural complications [30, 35].
Risk factors for episiotomy
Older maternal age was significantly less likely to experience episiotomy during childbirth compared to adolescent mothers. This finding aligns with previous studies suggesting that younger women are predisposed to episiotomies due to less tissue elasticity and higher rates of assisted deliveries [35, 36]. Furthermore, better perineal tissue management by experienced healthcare providers, comprehensive birth plans, informed decision-making in childbirth, and increased awareness of episiotomy risks among older women contribute to these findings [26]. The notably lower episiotomy rates in women aged 41 years and above, who were 94.3% less likely to undergo the procedure, indicate the importance of individualised care [37]. This trend suggests a shift towards prioritising natural birth processes and minimising unnecessary surgical interventions, leading to better postpartum recovery and maternal health outcomes. However, contrasting evidence from Muraca et al. [38] indicates that episiotomies are more common in older women due to larger babies, which indicates the need for further research into age-related factors influencing episiotomy rates.
Married women were also found to be less likely to have an episiotomy compared to single women. This study corroborates findings in American Samoa, where unmarried women were more likely to undergo episiotomy [39]. This maybe because episiotomies have been associated with future poorer sexual capabilities and damage to the Bartholin’s gland which are reported to contribute to dyspareunia and insufficient lubrication [22]. Consequently, midwives promoting normal birth devoid of episiotomy among married women could be a protective strategy to promote sexual health following childbirth.
Antenatal care (ANC) attendance and timing significantly influenced the likelihood of episiotomy, underscoring the importance of comprehensive ANC in improving obstetric outcomes. Women attending 4–8 ANC sessions had a 69% lower likelihood of undergoing an episiotomy compared to those attending three or fewer sessions. Furthermore, attending nine or more ANC sessions reduced the likelihood by 82.4%. Starting ANC in the second trimester was associated with a 57.9% lower likelihood of episiotomy, while initiating ANC in the third trimester showed no significant association. These findings emphasise the critical role of timely and frequent ANC in optimising maternal outcomes during childbirth, with implications for maternal well-being and birth experiences. These findings align with previous studies [22, 40]. The reduced likelihood of episiotomy with increased ANC attendance suggests that thorough prenatal care can better prepare women for childbirth, promoting less invasive delivery methods [41].
The type of childbirth also significantly affected the likelihood of episiotomy. These findings highlight the clinical implications for obstetric care, suggesting that SVD and instrumental deliveries may involve less need for surgical intervention. This is supported by Bączek et al. [42] and Frenette et al. [43], who also identified the type of childbirth as a significant predictor of episiotomy rates. The lower likelihood of episiotomy among women with SVB and instrumental births, compared to breech births, suggests the need for nuanced clinical assessment and support during labor and childbirth, promoting safer and less invasive delivery methods.
Neonatal health indicators, such as the Apgar score of 8 and above reduced the likelihood of episiotomy in this setting. This finding emphasised the influence of fetal and neonatal health on maternal interventions during childbirth. This finding aligns with previous studies [44, 45]. The reduced likelihood of episiotomy among women whose babies had higher Apgar scores suggests that better neonatal outcomes may reduce the need for surgical interventions, promoting a more natural birthing process.
The study also found no significant association between episiotomy and birth weight. The high prevalence of episiotomy across birthweights suggests that the clinical judgment underscoring episiotomy could have been due to fetal factors such as distress or maternal factors such as maternal previous history of lower genital tract surgeries or other [46]. This could imply that episiotomy is performed routinely without following the WHO protocols and guidelines [10].
Previous medical conditions also played a role in the likelihood of episiotomy. Women with anemia demonstrated a surprising 46.7% lower likelihood of undergoing an episiotomy compared to those without any previous medical conditions. The association between anemia and reduced episiotomy rates might be due to cautious management by healthcare providers to avoid additional stress on anemic patients. Also, pregnant women with anemia are likely to attend regular prenatal check-ups where their iron levels are monitored, and adjustments to diet or supplementation are made as necessary. Women with diabetes mellitus and hypertension were significantly more likely to have an episiotomy. These findings explain the complex relationship between maternal health conditions and obstetrical outcomes, with implications for maternal well-being and birth experiences. The findings align with previous studies [22, 40], highlighting maternal health conditions’ influence on birth interventions.
The duration of the second stage of labour was also found to influence episiotomy likelihood. Women whose second stage of labor lasted 31–60 min had a 42.6% lower likelihood of undergoing an episiotomy compared to those with shorter labor durations. Moreover, a second stage lasting 61 min or more was associated with a 92% lower likelihood of episiotomy. These findings highlight the importance of labor progression in episiotomy decision-making, suggesting that prolonged labor may allow for better management and less need for surgical intervention. Therefore, aligns with research by Brown et al. [47], which similarly highlighted the influence of labor duration on obstetric interventions. The reduced episiotomy rates with longer labor durations suggest that patience and careful monitoring during labor can promote safer and less invasive delivery methods.
Implications for policy, practice and midwifery education
The high prevalence of episiotomies at 49.7% suggests a potential overuse of the procedure compared to WHO recommendations of 10%, highlighting the need for stricter adherence to evidence-based guidelines. Addressing this involves policy interventions aimed at reducing unnecessary episiotomies through national protocols and guidelines that promote judicious use based on clinical indications rather than routine practice. Enhancing midwifery education to emphasise the importance of respectful maternity care and informed consent is crucial, as evidenced by the 11.5% rate of non-consensual episiotomies observed. This highlights the necessity for ongoing professional training in communication skills and ethical practices to ensure patient autonomy and dignity during childbirth. Furthermore, optimising ANC attendance and timing, and starting ANC earlier in pregnancy, should be prioritised through public health campaigns and healthcare system reforms to improve maternal preparation and outcomes. Addressing specific risk factors such as maternal age, type of delivery, and medical conditions like diabetes and hypertension through tailored clinical guidelines and continuous quality improvement initiatives can help mitigate episiotomy rates and improve overall maternal health and safety outcomes.
Study limitations and suggestions for future studies
The limitations of this study include its cross-sectional design, which precludes the establishment of causality between variables. Convenience sampling from selected hospitals in the Kumasi Metropolis introduces potential sampling bias, limiting the generalizability of findings. Moreover, reliance on self-reported data may have introduced recall and social desirability biases regarding episiotomy experiences. Translation efforts, language and cultural factors could have influenced participant responses. Future research should employ longitudinal designs to track episiotomy practices over time and explore causal relationships. Additionally, incorporating qualitative methods to delve into cultural beliefs and perceptions surrounding episiotomy could provide deeper insights. These approaches would enhance the validity and applicability of findings, informing more effective maternal health strategies and policies in similar contexts.
Conclusion
Data from this study suggest a high episiotomy prevalence of 49.7%, indicating potential overuse compared to WHO recommendations. While 88.5% of procedures were consented to, the occurrence of 11.5% non-consensual episiotomies highlights gaps in respectful maternity care. Subsequent repairs were required in 77.6% of cases, suggesting potential complications and healthcare burdens. Factors such as maternal age, ANC attendance and timing, type of delivery, neonatal health, and maternal medical conditions significantly influenced episiotomy likelihood. There is a need for evidence-based guidelines, improved patient communication, and enhanced midwifery education to promote judicious use of episiotomy and optimise maternal health outcomes. Addressing these aspects could mitigate risks associated with episiotomy and advance maternal healthcare practices in similar settings in Ghana. Future research should employ longitudinal and qualitative methods to explore these dynamics further and inform comprehensive maternal health strategies.
Acknowledgements
The authors express their appreciation to the research assistants that helped in the collection of data. We are also grateful to the administration of the five facilities included in the study and to all the study participants for their collaboration.
Author contributions
Conceptualization: MA & PFD; Data collection: MA, PFD, TDA, GO & SAA; Data analysis: MA; Draft of initial manuscript: PFD, TDA, GO; Writing of final manuscript: GO, PFD & TDA; Review: SAA, PFD & MA.
Funding
This study did not receive funding.
Data availability
The dataset used and analysed is available from the corresponding author upon reasonable request. The dataset has been registered at Open Science Framework: https://archive.org/details/osf-registrations-jmv9a-v1.
Declarations
Ethics approval and consent to participate
To protect the rights of all participants, we rigorously followed the Declaration of Helsinki in both the design and execution of the research. This study received approval from the Ghana Health Services Ethics Review Committee (ERC) in Accra (ID: GHS-ERC: 031/02/24). Participants were fully informed about the purpose of the study, the voluntary nature of their involvement, the confidentiality of their data, and their right to withdraw at any time. All methods were conducted in compliance with pertinent guidelines and regulations. All participants provided oral consent for their participation. Also, trained research assistants translated the consent forms into the native languages of participants with no or lower levels of education. Afterwards, they obtained written informed consent from all participants before the face-to-face interviews.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Woldearegay EA, Amevor E, Steeves HL. Participatory and intersectionality approaches for gender equity and maternal health promotion in sub-saharan Africa. Handb Commun Dev. 2021;285–301.
- 2.Minckas N, Gram L, Smith C, Mannell J. Disrespect and abuse as a predictor of postnatal care utilisation and maternal-newborn well-being: a mixed-methods systematic review. BMJ Glob Heal. 2021;6(4):1–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Mittal M. Episiotomy. In: Labour Room Emergencies. 2020. pp. 271–81.
- 4.Rotstein E. Pelvic Floor Dysfunction After Childbirth - Symptoms, Diagnosis, Treatment [Internet]. Karolinska Institutet; 2022. https://openarchive.ki.se/xmlui/bitstream/handle/10616/48302/Thesis_Emilia_Rotstein.pdf?sequence=1&isAllowed=y
- 5.Schmidt PC, Fenner DE. Repair of episiotomy and obstetrical perineal lacerations (first–fourth). Am J Obstet Gynecol [Internet]. 2024 Mar 1 [cited 2024 Jun 24];230(3):S1005–13. http://www.ajog.org/article/S0002937822005415/fulltext [DOI] [PubMed]
- 6.Kalis V, Rusavy Z, Prka M, Episiotomy. Childbirth Trauma [Internet]. 2017 Jul 29 [cited 2024 Jun 24];69–99. https://link.springer.com/chapter/10.1007/978-1-4471-6711-2_6
- 7.Clesse C, Lighezzolo-Alnot J, De Lavergne S, Hamlin S, Scheffler M. Socio-historical evolution of the episiotomy practice: a literature review. Women Health. 2019;59(7):760–74. [DOI] [PubMed] [Google Scholar]
- 8.Falagario M, Greco F, Padova M, Morena M, Palieri T, D’Antonio F et al. The Role of Episiotomy in Emergency Delivery. In: Practical Guide to Simulation in Delivery Room Emergencies. 2023. pp. 893–914.
- 9.Childs C, Sandy-Hodgetts K, Broad C, Cooper R, Manresa M, Verdú-Soriano J. Risk, Prevention and Management of Complications After Vaginal and Caesarean Section Birth. J Wound Care [Internet]. 2020 Nov 1 [cited 2024 Jun 24];29(Sup11a):S1–48. https://pubmed.ncbi.nlm.nih.gov/33170077/ [DOI] [PubMed]
- 10.Gazari T, Atanuriba GA, Anagbe, Gariba P. Exploring the perceptions and preparedness for Episiotomy Amongpost Partum Mothers in Northern Ghana: a qualitative study. J Gynecol Reprod Med. 2023;7(3):1–15. [Google Scholar]
- 11.van der Pijl MSG. Learning from childbirth experiences: The importance of respectful care and consent during labour and birth [Internet]. Vrije Universiteit, Amsterdam; 2023 [cited 2024 Jun 24]. https://research.vu.nl/en/publications/learning-from-childbirth-experiences-the-importance-of-respectful
- 12.Adama O, Natacha LB, Smaila O, Alexis SY, Francoise MT, Charlemagne OM, et al. Episiotomy: epidemiological aspects, indications and prognosis in the Bogodogo Health District. Open J Obstet Gynecol. 2018;08(13):1354–63. [Google Scholar]
- 13.Howells IE, Abasi IJ. Episiotomy Repair in Poor Resource Settings, is It Justifiable to Recommend the Fast Absorbing Polyglactin 910 Suture (Vicryl Rapide) as the Suture of Choice ? – A Randomized Controlled Trial. Asian Res J Gynaecol Obstet [Internet]. 2020;4(2):30–42. https://journalarjgo.com/index.php/ARJGO/article/view/55
- 14.Lissu CA, Volgsten H, Mazuguni F, Maro E, Proportion. Characteristics and Maternal Outcome of women referred for childbirth to a tertiary hospital in northern Tanzania – A descriptive retrospective study based on a hospital birth registry. Sex Reprod Healthc [Internet]. 2021;29(July):100646. 10.1016/j.srhc.2021.100646 [DOI] [PubMed]
- 15.Deyaso ZF, Chekole TT, Bedada RG, Molla W, Uddo EB, Mamo TT. Prevalence of episiotomy practice and factors associated with it in Ethiopia, systematic review and meta-analysis. Women’s Heal. 2022;18. [DOI] [PMC free article] [PubMed]
- 16.Hussein SAAA, Dahlen HG, Duff M, Schmied V. The barriers and facilitators to evidence-based episiotomy practice in Jordan. Women Birth. 2016;29(4):321–9. [DOI] [PubMed] [Google Scholar]
- 17.Ghiasvand M, Nahidi F, Mobarakabadi SS, Nia HS, Majd HA. The perception of episiotomy among Iranian women: a qualitative study. Br J Midwifery [Internet]. 2021;13(1):30–40. https://api.semanticscholar.org/CorpusID:245561513
- 18.Navarro-Prado S, Sánchez-Ojeda M, Marmolejo-Martín J, Kapravelou G, Fernández-Gómez E, Martín-Salvador A. Cultural influence on the expression of labour-associated pain. BMC Pregnancy Childbirth [Internet]. 2022;22(1):1–9. 10.1186/s12884-022-05173-1 [DOI] [PMC free article] [PubMed]
- 19.Alex-Ojei C. The sociocultural influences on maternal healthcare utilisation among adolescent mothers in Nigeria: a pooled data analysis [Internet]. University of the Witwatersrand, Johannesburg; 2020. https://wiredspace.wits.ac.za/bitstreams/f18da3f2-4c39-4dfe-b358-572920b10169/download
- 20.Enos JY, Amoako RD, Enos SK, Hayford B, Tette EM. Perspective Chapter: Challenges to Postnatal Care in Sub-Saharan Africa – A Review. Intech [Internet]. 2016;11(tourism):13. https://www.intechopen.com/books/advanced-biometric-technologies/liveness-detection-in-biometrics
- 21.Pebolo F, Judith A, Kabonge Dan K. Prevalence and factors associated with episiotomy practice among primiparous women in mulago national referral hospital Uganda. Int J Pregnancy Child Birth. 2019;5(5):197–201. [Google Scholar]
- 22.Woretaw E, Teshome M, Alene M. Episiotomy practice and associated factors among mothers who gave birth at public health facilities in Metema district, northwest Ethiopia. Reprod Health [Internet]. 2021;18(1):1–11. 10.1186/s12978-021-01194-9 [DOI] [PMC free article] [PubMed]
- 23.Morhe ESK, Sengretsi S, Danso KA. Episiotomy in Ghana. Int J Gynecol Obstet. 2004;86(1):46–7. [DOI] [PubMed] [Google Scholar]
- 24.Aguiar BM, da Silva TPR, Pereira SL, Sousa AMM, Guerra RB, de Souza KV et al. Factors associated with the performance of episiotomy. Rev Bras Enferm. 2020;73(October). [DOI] [PubMed]
- 25.Clesse C, Lighezzolo-Alnot J, De Lavergne S, Hamlin S, Scheffler M. Statistical trends of episiotomy around the world: comparative systematic review of changing practices. Health Care Women Int. 2018;39(6):644–62. [DOI] [PubMed] [Google Scholar]
- 26.Graham ID, Carroli G, Davies C, Medves JM. Episiotomy rates around the world: an update. Birth [Internet]. 2005 [cited 2024 Jun 24];32(3):219–23. https://pubmed.ncbi.nlm.nih.gov/16128977/ [DOI] [PubMed]
- 27.WHO. WHO recommendation on episiotomy policy [Internet]. 2018 [cited 2024 Jun 24]. https://extranet.who.int/rhl/topics/preconception-pregnancy-childbirth-and-postpartum-care/care-during-childbirth/care-during-labour-2nd-stage/who-recommendation-episiotomy-policy-0
- 28.Djanogly T, Nicholls J, Whitten M, Lanceley A. Choice in episiotomy – fact or fantasy: a qualitative study of women’s experiences of the consent process. BMC Pregnancy Childbirth [Internet]. 2022;22(1):1–7. 10.1186/s12884-022-04475-8 [DOI] [PMC free article] [PubMed]
- 29.Bohren MA, Tunçalp Ö, Miller S. Transforming intrapartum care: Respectful maternity care. Best Pract Res Clin Obstet Gynaecol [Internet]. 2020;67:113–26. https://www.sciencedirect.com/science/article/pii/S1521693420300328 [DOI] [PubMed]
- 30.WHO. WHO recommendations Intrapartum care for a positive childbirth experience Executive summary [Internet]. 2018. https://creativecommons.org/licenses/by-nc-sa/3.0/igo). WHO/RHR/18.12. [PubMed]
- 31.Jiang DH, Fan YJ, Huang CJ, Zhang Y, Pan YL. Clinical effects of different anesthesia methods in lateral episiotomy. Ann Ital Chir [Internet]. 2021;92:190–5. https://annaliitalianidichirurgia.it/index.php/aic/article/view/1161 [PubMed]
- 32.Carroli G, Mignini L. Episiotomy for vaginal birth. Cochrane Database Syst Rev. 2009;(1):1–53. [DOI] [PMC free article] [PubMed]
- 33.Ye J, Chen Y, Yang H, Chen Q, Huang Y, Zhao J et al. A nationwide cross-sectional survey of episiotomy practice in China. Lancet Reg Heal - West Pacific [Internet]. 2022;19:100345. 10.1016/j.lanwpc.2021.100345 [DOI] [PMC free article] [PubMed]
- 34.Acquaye J, Nimako B, Arkoh R, Quarshie EL, Assim AO, Acquaye J et al. Factors Affecting Maternal Mortality at the Komfo Anokye Teaching Hospital Using the Audit Committee Report. Open Access Libr J [Internet]. 2021 Jun 30 [cited 2024 Jun 24];8(7):1–17. http://www.scirp.org/journal/PaperInformation.aspx?PaperID=110903
- 35.Hartmann K, Viswanathan M, Palmieri R, Gartlehner G, Thorp J, Lohr KN. Outcomes of Routine Episiotomy. JAMA. 2005;293(17):2141. [DOI] [PubMed] [Google Scholar]
- 36.Althabe F, Colomar M, Belizan M, Tosti E, Fortunato A, Settimi A. Interventions to improve the implementation of evidence based practices in Women Care. Curr Womens Health Rev. 2006;2(3):173–9. [Google Scholar]
- 37.Macleod M, Strachan B, Bahl R, Howarth L, Goyder K, Van De Venne M, et al. A prospective cohort study of maternal and neonatal morbidity in relation to use of episiotomy at operative vaginal delivery. BJOG Int J Obstet Gynaecol. 2008;115(13):1688–94. [DOI] [PubMed] [Google Scholar]
- 38.Muraca GM, Liu S, Sabr Y, Lisonkova S, Skoll A, Brant R, et al. Episiotomy use among vaginal deliveries and the association with anal sphincter injury: a population-based retrospective cohort study. CMAJ. 2019;191(42):E1149–58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Howells M, Ah Ching J, Bender R. Does maternal marital status indirectly influence use of medical interventions during delivery in american Samoa? Pac J Reprod Heal. 2016;1(3).
- 40.Bantas K, Aryastuti N, Gayatri D. The relationship between antenatal care with childbirth complication in Indonesian’s mothers (data analysis of the Indonesia demographic and health survey 2012). J Epidemiol Kesehat Indones. 2018;2(2):61. [Google Scholar]
- 41.Worku EB, Woldesenbet SA. Factors that influence teenage Antenatal Care utilization in John Taolo Gaetsewe (JTG) District of Northern Cape Province, South Africa: underscoring the need for tackling Social determinants of Health. Int J Matern Child Heal AIDS. 2016;5(2):134–45. [PMC free article] [PubMed] [Google Scholar]
- 42.Bączek G, Rychlewicz S, Sys D, Rzońca P, Teliga-Czajkowska J. Episiotomy for Medical Indications during Vaginal Birth—Retrospective Analysis of Risk Factors Determining the Performance of This Procedure. J Clin Med. 2022, Vol 11, Page 4334 [Internet]. 2022 Jul 26 [cited 2024 Jun 24];11(15):4334. https://www.mdpi.com/2077-0383/11/15/4334/htm [DOI] [PMC free article] [PubMed]
- 43.Frenette P, Crawford S, Schulz J, Ospina MB. Impact of Episiotomy during Operative Vaginal Delivery on Obstetrical Anal Sphincter injuries. J Obstet Gynaecol Can. 2019;41(12):1734–41. [DOI] [PubMed] [Google Scholar]
- 44.Basu M, Smith D. Long-term outcomes of the Stop Traumatic OASI Morbidity Project (STOMP). Int J Gynecol Obstet. 2018;142(3):295–9. [DOI] [PubMed] [Google Scholar]
- 45.Jones K, Webb S, Manresa M, Hodgetts-Morton V, Morris RK. The incidence of wound infection and dehiscence following childbirth-related perineal trauma: a systematic review of the evidence. Eur J Obstet Gynecol Reprod Biol. 2019;240:1–8. [DOI] [PubMed] [Google Scholar]
- 46.Barjon K, Vadakekut ES, Mahdy H, StatPearls. 2024. Episiotomy. https://www.ncbi.nlm.nih.gov/books/NBK546675/ [PubMed]
- 47.Brown O, Luchristt D, Miller ES, Pidaparti M, Geynisman-Tan J, Kenton K, et al. Is there an Association between Vaginal Birth after Cesarean Prediction and Obstetric Anal Sphincter Injury? Am J Perinatol. 2022;39(7):750–8. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The dataset used and analysed is available from the corresponding author upon reasonable request. The dataset has been registered at Open Science Framework: https://archive.org/details/osf-registrations-jmv9a-v1.