Abstract
Background
The lack of training for professionals on how to manage suicide risk is an important barrier to effective intervention. Dialectical Behavior Therapy Intensive Training™ (DBT-IT) includes specific training for suicide and has shown promising results to enhance implementation of DBT. To our knowledge, no published studies have evaluated the effect of DBT-IT on therapists’ attitudes towards treating suicide risk and among Spanish-speaking mental health professionals. The main aim of this study was to evaluate the effect of DBT-IT on therapists’ attitudes regarding treating suicide risk and its relationship with the implementation of DBT before and after receiving DBT-IT.
Methods
A total of 242 mental health workers (76.4% women, mean age 35.38, SD = 9.17; 77.7% from Latin America; 22.3% from Spain) who had received a DBT-IT participated in the study. Self-efficacy (Efficacy in Assessing and Managing Suicide Risk Scale) and concerns (Concerns about Treating Suicidal Clients Scale) in treating suicide, perceived burnout (Copenhagen Burnout Inventory), confidence in applying DBT (Behavioral Anticipation and Confidence Questionnaire), barriers to implementation (Barriers to Implementation Inventory), implementation of DBT and reach were measured via online survey at parts 1 (pre-training) and 2 (post-training, after 9 months of implementation) of the DBT-IT.
Results
Differences between pre-training and post-training (n = 61) indicated statistically significant improvements in self-efficacy, concerns about the lack of training and competence in treating suicide, and confidence in applying DBT. Statistically significant increases in the rates of DBT treatment modes implementation (except for individual therapy) and mindfulness practice, as well as the number of team members and consultation team hours, were also found. Findings also indicated statistically significant positive correlations between burnout and concerns about treating suicidal clients, as well as with structural and administrative implementation barriers, and between self-efficacy in managing suicide, confidence in applying DBT and implementation of DBT treatment modes. Participants with more implementation barriers reported lower rates of consultation team meetings and phone coaching implementation.
Conclusions
DBT-IT could be an adequate training model to increase self-efficacy and confidence in treating suicide risk as well as to facilitate implementation of DBT treatment modes by Spanish-speaking mental health professionals.
Clinical trial number
Not applicable.
Keywords: Mental health professionals, Suicide, Burnout, Self-efficacy, Dialectical behavior therapy, DBT intensive training, Implementation
Background
Therapists’ attitudes to treating suicide risk and need for training
Worldwide, suicide is the fourth leading cause of death in the population aged 15–29, causing more than 700,000 deaths annually [1]. Therefore, suicide prevention becomes “a global imperative” [2]. One of the key factors for a comprehensive approach to suicide is the role of the mental health professionals who work daily with people who present suicidal ideation and/or risk of suicide [3]. Recent efforts to identify strategies to prevent suicide have pointed out the importance of training professionals who treat suicide risk (e.g., 4). Two fundamental barriers to achieving this goal have been suggested: the lack of adequate and specialized training in the assessment and management of suicide risk and the low level of willingness of the clinicians to work with this population [5].
Findings from a meta-analysis have warned that healthcare providers report high emotional exhaustion when treating suicide risk [6] and other studies have shown that therapists’ burnout has been associated with an increased likelihood of unsafe self-care, unprofessional behaviors, and low patient satisfaction [7, 8]. Research has also shown that greater perceived training in working with suicide risk is related to lower professionals’ anxiety regarding the suicide risk of their patients and higher self-efficacy, attitudes, knowledge, and confidence in managing suicide risk (e.g., [9, 10, 11]). Despite the need for adequate training for professionals (e.g.,, specialized training in the assessment and management of suicidal behavior is generally not included in postgraduate training or certification programs [10] and the accredited graduate programs that require suicide-specific training typically lack guidelines on the content, focus, or timing of such training [12, 13]. All these findings suggest a lack of access and quality of specialized training to treat suicide risk.
Dialectical behavior therapy intensive training
Linehan’s Dialectical Behavior Therapy (DBT; [14, 15]) is an integrative intervention that combines acceptance and change strategies using dialectics. DBT standard consists of 4 modes of treatment: individual therapy, group skills training (mindfulness, emotion regulation, stress tolerance, interpersonal effectiveness), telephone coaching between sessions and consultation team meetings for therapists which aim to work the following functions respectively: (1) improve client´s motivation to change and engage in treatment; (2) enhance individual’s capability by increasing skillful behavior; (3) ensure generalization of change and restructuring or changing individual’s environment; (4) enhance therapist motivation to deliver effective treatment [16]. Furthermore, therapists’ own mindfulness practice has been proposed as a requisite in order to ensure that mindfulness skills would be taught both from an experiential and intellectual knowledge. Although no formal practice is required, mindfulness exercises are practiced during the consultation team meetings and therapists are required to practice particular mindfulness exercises prior to using them with clients [17].
Traditionally, DBT has been recommended as a first-line treatment for people with Borderline Personality Disorder (BPD) [18], a problem that it is often associated with an increased risk of presenting any of the symptoms of suicidal behavior: active (thoughts about taking steps to end one’s own life) and passive (thoughts about death, or wanting to be dead) suicidal ideation, self-injury (self-injurious behavior without intent to die), suicide attempts (potentially self-injurious behavior associated with at least some intent to die) and completed suicide [19, 20]. To improve clinicians’ ability to assess and manage suicidal behaviors, Linehan’s team developed the Linehan Risk Assessment and Management Protocol (LRAMP; 16), which has shown good acceptability and usability results and improvements in providers’ concerns and self-efficacy in managing suicide [5].
The LRAMP is included in the DBT Intensive Training (DBT-IT), which is considered one of the most successful dissemination efforts undertaken by those developing evidence-based psychological treatments [21]. The DBT Intensive Training™ Model (DBT-ITM) is the standard training method for obtaining DBT knowledge or certification and is designed to train mental health professionals for them to be successful in implementing a comprehensive DBT program. The training consists of two 5-day workshops separated by a 6-month period devoted to self-study and implementation of DBT [22]. The effectiveness of the DBT-IT to help implement DBT in clinical practice has shown promising results.
Effectiveness of DBT-IT on the implementation of DBT
The treatment modes, the core elements of the DBT program, were selected as the variable by which the success of DBT implementation is assessed because each mode demonstrates a function of DBT (e.g., conducting intersession telephone coaching allows the generalization of patient skills learned in therapy). It is assumed that the more DBT modes implemented, the higher the level of DBT adoption [23]. There are currently very promising findings on the effectiveness of DBT-ITM for increasing the implementation of a DBT program after training. In the largest study, of 105 intensively trained teams in the United Kingdom (UK), 62.8% were still actively running DBT programs 2–15 years after receiving training [24]. Subsequently, different studies assessed adoption rates of DBT treatment modes. For example, two large studies in the United States (US) found high adoption rates (above 75–87% across all modes; 22, 23), being individual therapy and group skills training the most adopted modes and phone coaching and consultation team meetings the least adopted. Other studies also indicated promising reach rates (average 118 clients treated) after training [25]. A different study in US Veterans Health Administration (VHA) facilities (n = 59) showed that, while 42% of the facilities offered all four DBT modalities, the skills group was the most frequently implemented; 59% offered telephone coaching in any form, although only 11% of them offered 24-hour coaching [27]. The findings from these studies suggest a need to continue working on implementing less frequent treatment modes such as phone coaching and consultation team meetings.
Although adoption rates of DBT are promising, it has been suggested that further research is needed to evaluate different aspects that may influence the implementation of DBT, such as therapist and organizational factors [12]. An important therapist factor to consider when applying DBT is burnout. Two studies have found that receiving DBT training decreases therapist burnout and the stress associated with applying DBT [25, 26]. However, to our knowledge, no studies have specifically evaluated the effect DBT-IT has on practitioners’ concerns and self-efficacy when treating suicidal patients and its relationship with the implementation of DBT.
Regarding other factors that may influence implementation, several studies have focused on exploring barriers and facilitators encountered by professionals. The most reported reason for DBT program “death” in the UK study was the lack of organizational support [30]. Two more studies showed similar barriers to the implementation of DBT in public health systems with clinicians [29] and administrators [31]. Another study [24] also encountered lack of peer support and staff turnover as the main barriers in a large study in the UK. Finally, Flynn et al. [32], in a study conducted in Ireland, suggested the lack of system support for the phone coaching mode and logistical challenges as the main barriers. Regarding facilitators, a study in the US [12] found that lower training and program needs, fewer clinicians with an undergraduate level of education, and greater prior DBT experience predicted adoption of more DBT modes. In this line, two more studies showed that therapist skills, attitudes, willingness, and training on DBT [24], as well as effective leadership and the possibility of being supervised [32], facilitated the implementation of DBT.
Considering all these findings, receiving specialized training may help increase self-efficacy and reduce burnout of professionals who treat suicidal behavior, and it could be a facilitator for the implementation of DBT in routine clinical practice. Previous research also indicates successful implementation of DBT across English-speaking countries. However, to our knowledge, there are no published studies that have evaluated the implementation of DBT in Spanish-speaking mental health professionals, the fourth most spoken language in the world. Therefore, the main aims of this study were to evaluate: (1) differences between parts 1 (pre-training) and 2 (post-training) of DBT-IT in the level of implementation of DBT treatment modes and reach (numbers of patient treated) as well as therapist attitudes related to suicide risk treatment, (2) associations between the therapist attitudes and DBT treatment modes and barriers to implementation in Spanish-speaking practitioners.
Methods
Participants
A total of 274 mental health professionals from Spain or Latin America who enrolled on an online DBT-IT through the training agency DBT Iberoamérica (affiliated to Behavioral Tech Institute) from 2020 to 2022 were invited to participate in the study. The inclusion criteria for participation in the study were: (1) Be at least 18 years old; (2) Be enrolled in an online DBT-IT; (3) Understand the Spanish language; (4) Sign the informed consent. Exclusion criteria were (1) Not interested in taking part of the study during the DBT-IT and (2) Not attending any of the two parts of the DBT-IT in which they were enrolled. Sociodemographic data of the sample can be seen in the results section.
Measures
Participants sociodemographic and implementation of DBT
Professionals information survey
adapted into Spanish from Navarro et al. [25] to collect demographic information, type of discipline practiced, theoretical orientation and population treated, as well as DBT experience and level of training (hours of DBT training) and practitioners’ mindfulness practice. This survey also included items to evaluate level of implementation of DBT (individual therapy, group skills training, phone coaching and consultation team meetings modes applied), reach (number of patients treated). This section corresponds with the first 4 items of the Program Elements of Treatment Questionnaire (PETQ; [28]), which has been adapted to evaluate DBT adoption (e.g., 21).
Concerns and self-efficacy about treating suicidal patients
Concerns about treating suicidal clients scale
(CATSP; 5). It consists of 22 items generated from the empirical literature which assess concerns about treating suicidal patients. The scale has 4 subscales: Concerns about Clinical Errors (CE), Legal Consequences (LC), Lack of Knowledge and Training (LT) and Emotional Impact (EI) and has shown good psychometric properties [5]. For our sample, the Cronbach’s alpha reliability values for this instrument showed acceptable internal consistency (α = 0.93 and 0.83, 0.75, 0.74 and 0.81 for each subscale respectively).
Self-efficacy in assessing and managing suicide risk scale
(SETSP-S; 5). This 8-item scale was developed to mirror the suicide risk assessment and management process of the LRAMP protocol used in DBT [16]. The scale showed good psychometric properties [5]. In the study sample, the Cronbach’s alpha value for this instrument also showed good reliability (α = 0.89).
Burnout
Copenhagen burnout inventory
(CBI; [34]). The validated Spanish version of this instrument was used [35]. This 19-item scale assesses burnout (defined as physical and psychological fatigue and exhaustion) in three areas: (1) personal (2), work, and (3) dealing with clients. It presents good scores in the internal consistency of the three scales [35]. In our study sample, the Cronbach’s alpha values for this instrument showed good results (α = 0.91 and 0.88, 0.80 and 0.83 for personal, work and dealing with client’s subscales, respectively).
Confidence and motivation in applying DBT
Behavioral anticipation and confidence questionnaire
(BAQ; [33]). A version with 16 items adapted by Linehan’s team [25] was used to assess professionals’ confidence in their ability and motivation to apply different DBT strategies. Items were averaged to create two subscales: Confidence (participants’ confidence in their ability to use DBT) and motivation (practitioners’ motivation to apply different aspects of DBT). The questionnaire showed good internal consistency [36]. In this study sample, the reliability Cronbach’s alpha values for this instrument were 0.85 for the total scale and 0.87 and 0.76 for each subscale, respectively.
Barriers to implementation of DBT
Barriers to implementation inventory
(BTI; Behavioral Tech, LLC. (n.d), unpublished instrument). The 39-item inventory consists of a list of barriers that teams may encounter when implementing DBT. Barriers are structured by the following domains: Administrative problems (AD): refers to problems related to the day-to-day organization of therapy implementation (e.g. “productivity demands”). Team problems (TE): problems among professionals implementing therapy (e.g. “not attending DBT meetings”). Philosophical problems (PH): problems related to the content and theoretical basis implied by the DBT model (e.g. “not possessing a cognitive-behavioral orientation”) and structural problems (ST): problems concerning the organization and structure of the working center (e.g. “too many patients or referrals”). The internal reliability of this instrument was good [36]. In the study sample, the overall Cronbach’s alpha reliability value for this instrument was 0.74 (α = 0.71, 0.67, 0.64 and 0.49 for each subscale respectively). In the study sample, the overall Cronbach’s alpha reliability value for this instrument was 0.74 (α = 0.71, 0.67, 0.64 and 0.49 for each subscale respectively).
Design and procedure
This design consists of a quasi-experimental study with two assessment time points, at Part 1 (pre-training) and at Part 2 (post-training) of the DBT-IT.
DBT-IT is organized in two parts: part 1 (knowledge acquisition) and part 2 (expert consultation for practice improvement and sustainability), each of which lasts 5 days. Between the two parts, the trainees have an implementation period of around 6–9 months (with 5 sessions of mentoring) with a total of 120 h of training. An important characteristic of this training is that participants are required to attend in teams (see more information: [23]). In this case, the training was conducted online.
Participants were recruited by sending an invitation email to the mailing lists of the health professionals enrolled on a DBT-IT via the training agency. Participants had previously given their authorization in accordance with Personal Data Protection Policies. In the email text, there was a link (via Qualtrics® platform: https://www.qualtrics.com/es/) to access the study information and informed consent form. Once they agreed to participate in the study, participants accessed an online survey with a series of questionnaires (explained above in the description of the measures) via Qualtrics® platform at part 1 (pre-training) and 2 (post-training) of the DBT-IT. Part 1 of the online DBT-IT took place over 5 Saturdays and trainees completed the survey questionnaires during the first week. Part 2 of the online DBT-IT was also carried out over 5 Saturdays and participants completed part 2 survey questionnaires during the last week.
Statistical analysis
First, normality tests were performed using the Kolmogorov-Smirnov test for all variables. Then, descriptive statistics were carried out to analyze the characteristics of the participants in the study. After that, mean comparison analyses were conducted (using the chi-square test for categorical and those with a non-normal distribution variables and Student’s t-test and analysis of variance [ANOVA] for continuous variables) in order to analyze differences in sociodemographic characteristics and variables under study between participants from Spain and Latin America as well as differences according to gender, marital status, profession, qualification, primary work setting, psychotherapeutic orientation and experience in applying DBT treatment modes (individual therapy, group skills training, phone coaching and consultation team) before training. We created a new variable, i.e., DBT treatment mode implementation, to measure the combined score of all four DBT treatment modes.
Next, Student’s t-test for related samples were carried out to analyze the changes produced in the variables under study between pre-training and post-training. Also, Pearson’s R correlations were used to establish relationships between the variables under study in part 2. All statistical analyses were carried out using the statistical software SPSS version 25.0 [37].
Results
Attrition and baseline sociodemographic characteristics
A total of 274 mental health professionals were registered to receive the DBT-IT and were invited to participate in the study. The total sample attended part 1 and 2 of the DBT-IT. Only participants who completed part 1 (pre-training) survey were asked to participate in the part 2 (post-training) survey. Of the 274 mental health professionals registered, 242 (88.32%) completed the pre-training survey and, of these, 61 (25.21%) completed also the post-training survey.
The sociodemographic results of the professionals and the differences between the participants from Spain and Latin America can be found in Table 1. In terms of sample characteristics, participants had a mean age of 35.38 (SD = 9.17), 76.4% of them were women (n = 188), 77.7% were from Latin American countries (n = 188; Colombia (15.8%); Costa Rica (5.5%); Argentina (3.3%); Uruguay (3%); Peru (5.1%); Chile (15.8%); Paraguay (3.3%); Puerto Rico (0.6%); Panama (1.5%); Bolivia (0.6% ); Mexico (12.9%); Dominican Republic; (1.2%); Guatemala (1.2%); Ecuador (2.1%); only reported “LATAM” (5%)) and 22.3% from Spain (n = 54).
Table 1.
Sociodemographic characteristics of the participants
| Spain | Latin America | Total | Difference of distributions | |||||
|---|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | X 2 | p | |
| Profession/discipline | 8.9 | 0.175 | ||||||
| Psychologists | 43 | 79.6 | 124 | 66 | 176 | 69.0 | ||
| Psychiatrists | 8 | 14.8 | 56 | 29.8 | 64 | 26.4 | ||
| Mental health counselor/therapist or technician | 1 | 1.9 | 4 | 2.1 | 5 | 2.1 | ||
| Substance abuse therapist | 0 | 0.0 | 1 | 0.5 | 1 | 0.4 | ||
| Other | 2 | 3.7 | 3 | 1.5 | 5 | 2.1 | ||
| Highest degree | 21.9 | < 0.001 | ||||||
| University degree | 4 | 7.5 | 58 | 30.8 | 62 | 11,6 | ||
| Masters | 28 | 51.9 | 61 | 32.4 | 89 | 36.8 | ||
| PhD | 6 | 11.1 | 4 | 2.1 | 10 | 4.1 | ||
| Major in medicine/nursing/psychology | 16 | 29.6 | 65 | 34.6 | 81 | 33.5 | ||
| Primary work setting | 32.6 | < 0.001 | ||||||
| Private practice | 11 | 20.4 | 92 | 48.9 | 103 | 42.6 | ||
| Outpatient treatment facility | 14 | 25.9 | 21 | 3.2 | 35 | 14.5 | ||
| Day treatment facility | 8 | 14.8 | 7 | 1.7 | 15 | 6.2 | ||
| Inpatient treatment facility | 4 | 7.4 | 15 | 8.0 | 19 | 7.9 | ||
| Residential treatment facility | 2 | 3.7 | 0 | 0.0 | 2 | 0.8 | ||
| Correctional/forensic facility | 0 | 0.0 | 1 | 0.5 | 1 | 0.4 | ||
| University | 4 | 7.4 | 11 | 5.9 | 15 | 6.2 | ||
| Public Health | 6 | 11.1 | 22 | 11.7 | 28 | 8.6 | ||
| Welfare/ Social Services | 0 | 0.0 | 7 | 3.7 | 7 | 2.9 | ||
| Other | 5 | 9.3 | 12 | 6.4 | 17 | 7.0 | ||
| Therapeutic Orientations | 14.4 | 0.155 | ||||||
| CBT | 30 | 55.6 | 99 | 52.5 | 129 | 53.3 | ||
|
Client-Centered Therapy /Humanist |
1 | 1.9 | 2 | 1.8 | 3 | 1.2 | ||
| DBT | 6 | 11.1 | 26 | 13.7 | 32 | 13.2 | ||
| Psychodynamic interventions | 1 | 1.9 | 9 | 4.9 | 10 | 4.1 | ||
| Psychoanalysis | 0 | 0.0 | 2 | 1.2 | 2 | 0.8 | ||
| Gestalt | 0 | 0.0 | 5 | 2.7 | 5 | 2.1 | ||
| Interpersonal therapy | 1 | 1.9 | 0 | 0.0 | 1 | 0.4 | ||
| Rehabilitation model | 0 | 0.0 | 2 | 1.1 | 2 | 0.8 | ||
| Systemic approach | 1 | 1.9 | 13 | 6.9 | 14 | 5.8 | ||
| ACT | 6 | 11.1 | 20 | 10.6 | 26 | 10.7 | ||
| Other | 8 | 14.8 | 10 | 5.3 | 18 | 7.4 | ||
Note: In bold p-values < 0.05. CBT: Cognitive Behavior Therapy; DBT: Dialectical Behavior Therapy; ACT: Acceptance and Commitment Therapy; PhD: Doctor of Philosophy
As shown in Table 1, participants had been working in their current job for an average of 5.99 years (SD = 7.26. range 0–40) and had previously received an average of 50.21 h (SD = 91.6, range 0-600) of DBT training (20.2% had not received any training and 41.7% had received less than 10 h). They were mostly psychologists by profession (69.0%), with a master’s degree (36.8%), working in a private clinic (42.6%) and reported a cognitive-behavioral psychotherapeutic orientation (73.2%). The results of the Chi square test showed significant differences in the distribution of the sociodemographic variables “highest degree” and “primary work setting” between participants from Spain and those from Latin America. Specifically, participants from Latin America had a lower level of education and a higher proportion of work in private clinical settings than those from Spain. All variables presented a normal distribution (p > .05) except for two of the categorical variables: individual therapy and skills group modes of treatment implementation.
Descriptive statistics and baseline differences at pre-training of the DBT-IT
Regarding the descriptive statistics for the study outcomes at pre-training on Behavioral Anticipation and Confidence (BAQ), Efficacy in Assessing and Managing Suicide Risk (SETSP-S), Concerns about Treating Suicidal Clients (CATSP) and Burnout (CBI), the variables can be found in Table 2.
Table 2.
Mean instruments differences between part 1 and part 2
| Part 1 | Part 2 | Mean differences | ||||
|---|---|---|---|---|---|---|
| n = 242 | n = 61 | |||||
| M | SD | M | SD | t | p | |
| Practitioners’ attitudes | ||||||
| SETSP-S | 45.50 | 6.75 | 46.63 | 4.67 | 3.88 | 0.000 |
| CATSP | 3.91 | 1.03 | 3.84 | 1.02 | 1.88 | 0.065 |
| CATSP_EI | 4.48 | 1.30 | 4.50 | 1.33 | 1.56 | 0.124 |
| CATSP_LC | 4.19 | 1.06 | 4.20 | 1.13 | 0.49 | 0.624 |
| CATSP_LT | 3.63 | 1.20 | 3.40 | 1.11 | -3.21 | 0.002 |
| CATSP_CE | 4.19 | 1.06 | 3.27 | 1.17 | 1.13 | 0.262 |
| CBI | 46.94 | 10.88 | 48.48 | 10.08 | − 0.40 | 0.690 |
| CBI_CLIENTS | 14.41 | 3.95 | 15.14 | 3.24 | 1.64 | 0.108 |
| CBI_WORK | 18.08 | 4.12 | 18.52 | 3.935 | 0.41 | 0.684 |
| CBI_PERSONAL | 14.45 | 3.88 | 14.82 | 3.89 | 0.09 | 0.928 |
| BAQ | 66.54 | 5.23 | 66.39 | 5.91 | 0.18 | 0.860 |
| BAQ_CONFIDENCE | 3.92 | 0.44 | 4.02 | 0.47 | -1.53 | 0.002 |
| BAQ_MOTIVATION | 4.46 | 0.33 | 4.32 | 0.36 | 2.66 | 0.076 |
| DBT experience | ||||||
| Implementation of DBT treatment modes | 1.57 | 1.72 | 3.19 | 0.97 | 8.58 | 0.000 |
| No. patients treated with DBT | 3.75 | 7.48 | 7.46 | 11.3 | -0.99 | 0.33 |
| No. DBT skills groups conducted | 0.65 | 1.85 | 1.02 | 1.64 | 0.34 | 0.74 |
| No. hours consultation team meetings | 18.01 | 49.12 | 32.78 | 47.45 | 2.92 | 0.008 |
| No. DBT team members | 2.51 | 3.81 | 5.43 | 2.37 | 2.51 | 0.021 |
| No. hours mindfulness practice | 2.57 | 2.62 | 2.69 | 2.21 | -1.20 | 0.240 |
Note: In bold = p < .05; SETSP-S: Efficacy in Assessing and Managing Suicide Risk scale, CBI: Copenhagen Burnout Inventory; CATSP: Concerns About Treating Suicidal Clients Scale; EI: Emotional Impact Subscale; L: Legal Consequences subscale; LT: Lack of training and competence subscale; CE: Clinical Errors Subscale; BAQ: Behavioral Anticipation and Confidence Questionnaire
Taking into account sociodemographic information at baseline, results showed statistically significant differences according to gender in “concerns about legal consequences” about treating suicide risk (CATSP_LC; t = -2.22, p = .028) with higher scores in women (M = 4.32; SD = 1.01; vs. man M = 3.48; SD = 1.36). And in self-efficacy in assessing and managing suicide risk (SETSP-S; t = -3.66; p = .001) between psychologists (M = 45.20; SD = 4.31) and psychiatrists (M = 49.82; SD = 4.59), with higher scores in psychiatrists. No differences were found on any other scale with any other sociodemographic or experience in applying DBT treatment modes before training.
Differences between pre- and post-training of the DBT-IT
As seen in Table 2, results of the differences between pre-training and post-training of DBT-IT showed a statistically significant decrease in “concerns about lack of training and competence” in treating suicide risk (CATSP_LT; t = -3.21; p = .002), a statistically significant increase in self-efficacy to assess and manage suicide risk (SETSP-S; t = 3.88; p < .001), in confidence in applying DBT (BAQ_C; t = -1.53; p = .002) and in the implementation of DBT treatment modes (t = 8.58; p < .001). In addition, the number of hours dedicated to DBT consultation team at post-training (t = 2.92; p = .008) and the number of members who were part of it (t = 2.51; p = .021) statistically and significantly increased. No differences were found in the remaining variables between pre-training and post-training.
The aforementioned higher concerns about legal consequences when treating suicide risk among women professionals at pre-training persisted also at post-training (t = -2.22; p = .028) and the same held true for the higher self-efficacy of psychiatrists vs. psychologists (t = -2.32; p = .009) regarding treatment of suicidal ideation/attempts.
In terms of barriers to the implementation of DBT (BTI) at post-training, participants reported an average of 7.67 barriers (SD = 4.48, range = 0–16); 6.7% did not find any barriers when implementing DBT. The most common barriers were equipment (77.1% had encountered at least one and 32.4% had encountered at least four of the 15 equipment barriers described) and structural barriers (77.1% reported at least one structural barrier and 2.9% at least four of the nine structural barriers described). The most commonly encountered barriers related to team problems were: “difficulty in meeting with each other/sporadic attendance at consultation meetings; lack of reinforcers at team meetings; team members leaving, and no formal commitment to learn and implement DBT from some team members”. The most frequent barriers related to structural problems were the “lack of individual therapists and too many patients or referrals”. Fifty-one point four per cent of the participants found at least one philosophical barrier and 50% had at least one administrative barrier.
Student’s t-test showed also statistically significant differences in motivation and confidence in applying DBT (BAQ, t = 2.26; p = .025); between participants who completed the pre-training assessment (M = 68.51; DT = 6.1) and both pre and post training assessments (M = 66.54; DT = 5.23) and in self-efficacy to assess and manage suicide risk (SETSP; t = 3.27; p = .001; M pre-training = 46.24 DT = 6.20; M pre and post training assessments = 43.05; DT = 7.25), with higher scores for those who completed pre-training only. Moreover, findings indicated statistically significant differences in concerns about the lack of training (CATSP_LT; t=-2.47; p = .015; M pre assessment = 3.44; DT = 1.27; M pre and post assessments = 3.89; DT = 0.96) and emotional impact (CATSP_EI; t = 0.60; p = .009; M pre assessment = 4.21 DT = 1.32; M both assessments = 4.75; DT = 1.22), with lower scores for those who completed pre-training only.
Implementation of DBT treatment modes
Additionally, as shown in Table 3, a statistically significant increase was found in the application of DBT group skills training (χ2 = 3.94; p = .047), consultation team (χ2 = 4.39; p = .036), phone coaching (χ2 = 5.65; p = .017) and treatment modes, as well as mindfulness practice (χ2 = 12.74; p < .001), from part 1 to part 2. No differences were found in the implementation of individual therapy. Accounting for sociodemographic characteristics of the sample, a statistically significant higher implementation of the DBT group skills training mode was found for men (χ2 = 4.81; p = .049) compared to women and for Latin American participants (χ2 = 10.02; p = .003) compared to the Spanish. No other differences were found regarding the rest of the sociodemographic data.
Table 3.
Number and percentage distribution of variables regarding DBT treatment modes and mindfulness practice and difference of chi-square distributions
| PART 1 | PART 2 | Difference of distributions χ2 | ||||
|---|---|---|---|---|---|---|
| n = 242 | n = 61 | |||||
| Individual therapy | n | % | Individual therapy | n | % | χ2 = 0.94; p = .332 |
| Yes | 101 | 31.1% | Yes | 65 | 89.0% | |
| No | 224 | 68.9% | No | 8 | 11.0% | |
| Group Skills training | Group skills training | χ2 = 3.94;p = .047 | ||||
| Yes | 101 | 31.1% | Yes | 64 | 87.7% | |
| No | 224 | 68.9% | No | 9 | 12.3% | |
| Consultation team | Consultation team | χ2 = 4.39;p = .036 | ||||
| Yes | 58 | 17.8% | Yes | 52 | 71.2% | |
| No | 267 | 82.2% | No | 21 | 28.8% | |
| Phone Coaching | Phone Coaching | χ2 = 5.65;p = .017 | ||||
| Yes | 118 | 36.3% | Yes | 51 | 69.9% | |
| No | 207 | 66.7% | No | 22 | 30.1% | |
| Mindfulness | Mindfulness | χ2 = 12.74;p = < 0.001 | ||||
| Yes | 198 | 60.9% | Yes | 58 | 79.5% | |
| No | 127 | 39.1% | No | 15 | 20.5% | |
Note: * = In bold p < .05
Considering the differences in self-reported measures regarding the implementation of DBT treatment modes, a statistically significant increase was found in the number of barriers (BTI, t = 3.23; p = .033) reported by those who did not apply phone coaching (M = 71.24; SD = 4.80) compared to those who applied it (M = 60. 94; SD = 20.57), and in the number of team problems reported (BTI_TE subscale; t = -2.41; p = .022) by those who did not apply DBT consultation team meetings (M = 5.33; SD = 2.06) compared to those who did (M = 2.82; SD = 2.36). Except for implementation barriers, no further differences were found in the rest of the variables under study according to the DBT application modes.
Associations between implementation of DBT and therapists’ attitudes
Finally, based on Pearson’s correlations, statistically significant moderate positive correlations were found between barriers to implementation (BTI) and burnout (CBI) (r = .37; p = .023). Significant moderate negative correlations were encountered between implementation of DBT treatment modes and structural barriers (r = − .33; p = .042), and between burnout (CBI) and structural (BTI_ST r = .50, p = .002) and administrative (BTI_AD; r = .43, p = .008) barriers.
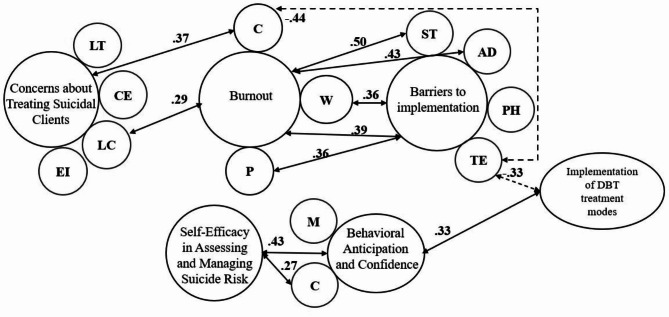
Statistically significant positive moderate correlations were also found between therapist confidence in applying DBT (BAQ-C) and perceived self-efficacy in assessing and managing suicide risk (SETSP-S) (r = .43; p = .001), and between motivation and confidence to apply DBT (BAQ) and implementation of DBT treatment modes (r = .33; p = .009). A statistically significant negative moderate correlation was found between average number of clients treated per month and the implementation of DBT treatment modes after training (r = − .33; p = .009). The remaining correlations performed between the instruments, their subscales and application of DBT treatment modes after training can be found in Table 4. A representation of the main correlations can be seen in Fig. 1.
Table 4.
Correlations between concerns, self-efficacy in treating suicide risk and burnout and factors related to the implementation of DBT (adoption of DBT treatment modes, confidence-BAQ and barriers-BTI)
| 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 | BTI_ TOTAL |
BTI_ST | BTI_TE | BTI_PH | BTI_AD | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. BAQ_TOTAL | − 0.20 | − 0.23 | − 0.21 | − 0.12 | − 0.14 | − 0.11 | − 0.09 | − 0.0 | − 0.11 | 0.33 | 0.43 | − 0.16 | − 0.07 | 0.02 | − 0.29 | − 0.07 |
| 2.BAQ_CONFIDENCE | -,10 | -,06 | − 0.09 | − 0.05 | − 0.17 | − 0.06 | 0.01 | 0.02 | 0.02 | 0.24 | 0.27 | 0.01 | 0.01 | 0.01 | 0.04 | 0.12 |
| 3.BAQ_MOTIVATION | − 0.10 | − 0.21 | − 0.15 | 0.02 | 0.06 | − 0.13 | − 0.01 | − 0.19 | − 0.02 | 0.18 | 0.12 | 0.04 | 0.01 | − 0.09 | 0.08 | 0.06 |
| 4. CATSP_TOTAL | 0.29 | 0.17 | 0.37 | 0.25 | − 0.07 | − 0.23 | 0.12 | 0.20 | − 0.23 | 0.05 | 0.23 | |||||
| 5. CATSP_EI | 0.28 | 0.17 | 0.39 | 0.22 | − 0.10 | − 0.17 | 0.13 | 0.12 | − 0.24 | 0.06 | 0.28 | |||||
| 6. CATSP_LC | 0.29 | 0.17 | 0.39 | 0.24 | − 0.04 | − 0.23 | 0.05 | 0.20 | − 0.35 | 0.10 | 0.13 | |||||
| 7. CATSP_LT | 0.19 | 0.08 | 0.26 | 0.18 | − 0.03 | − 0.20 | 0.02 | 0.08 | − 0.17 | − 0.04 | 0.13 | |||||
| 8. CATSP_CE | 0.25 | 0.17 | 0.25 | 0.25 | − 0.09 | − 0.22 | 0.24 | 0.32 | − 0.02 | 0.04 | 0.23 | |||||
| 9. CBI_TOTAL | 0.04 | − 0.09 | 0.37 | 0.50 | − 0.30 | 0.23 | 0.43 | |||||||||
| 10. CBI_WORK | 0.04 | − 0.08 | 0.36 | 0.50 | − 0.28 | 0.19 | 0.41 | |||||||||
| 11. CBI_CLIENTS | 0.12 | − 0.11 | 0.29 | 0.46 | − 0.44 | 0.31 | 0.32 | |||||||||
| 12. CBI_PERSONAL | − 0.06 | − 0.05 | 0.36 | 0.39 | − 0.13 | 0.14 | 0.42 | |||||||||
| 13. Implementation of DBT treatment modes | − 0.04 | − 0.29 | − 0.06 | − 0.33 | − 0.29 | − 0.97 | ||||||||||
| 14. SETSP-S_TOTAL | − 0.19 | − 0.09 | − 0.06 | − 0.26 | − 0.94 |
Note: In bold = p < .05;CBI: Copenhagen Burnout Inventory; CATSP: Concerns About Treating Suicidal Clients Scale; EI: Emotional Impact Subscale; L: Legal Consequences subscale; LT: Lack of training and competence subscale; CE: Clinical Errors Subscale; BAQ: Behavioral Anticipation and Confidence Questionnaire; BTI: Barriers to implementation Questionnaire; TE: Team problems subscale; ST: Structural problems subscale: Philosophical problems subscale; AD: Administrative problems subscale; SETSP-S: Efficacy in Assessing and Managing Suicide Risk. Scale
Fg. 1.
Statistically significant correlations between study variables. Caption: Note: Dashed lines for negative correlations and solid lines for positive correlations
Discussion
The main aims of this study were to analyze: (1) differences in therapist burnout, concerns and self-efficacy in treating suicide and confidence in applying DBT as well as in the level of implementation of DBT treatment modes, mindfulness practice and the number of patients treated at the beginning (pre-training) and at the end (post-training) of a DBT-IT; (2) the relationships between therapist attitudes regarding suicide risk treatment and the implementation of DBT treatment modes as well as barriers to implement DBT in clinical practice.
Regarding the first aim, the results of the study showed a statistically significant increase in professionals’ confidence in applying DBT and in self-efficacy in assessing and managing suicide risk between pre-training and post-training of the DBT-IT. These findings correspond with a study with young professionals in Argentina, in which, after a brief training in Safety Planning Intervention, a significant increase in their perception of self-efficacy in the management of suicide risk was found and even maintained two months after the training [36]. These results are relevant because unwillingness and low perceived self-efficacy are precisely one of the main barriers found among professionals who prefer not to work with clients with suicide risk [5, 9, 10]. Therefore, DBT-IT could help increase therapists’ motivation and self-efficacy and thus increase the likelihood that more clients might be treated.
Furthermore, a statistically significant reduction in professionals’ concerns about their lack of competence and training to address suicidal behavior was also found. The lack of qualified training in working with suicide risk represents another major barrier to work with this population. In general, studies noted a widespread lack of access to and quality of specialized training to address suicide risk [4, 5, 12, 13]. However, DBT-IT appears to achieve an initial significant reduction in professionals’ concerns about their lack of competence and training for treating suicide, which suggests that including DBT-IT training as part of the accredited programs might be a good solution to reduce professionals’ worries regarding training to treat suicide risk.
Concerning the implementation of DBT, statistically significant increases in the implementation of the DBT treatment modes (sum of all modes) and in the number of hours devoted to the consultation team among professionals and the number of DBT team members between pre-training and post-training were found. In addition to the training content, as suggested by Flynn et al. [32], the possibility of attending supervisions/mentoring by practitioners during the process of implementation between part 1 and 2 of these DBT-IT could be a facilitator for the successful implementation of DBT.
When analyzing implementation of each mode, the most frequently implemented mode was individual therapy (89%), followed by group skills training (87.7%) and consultation meetings (71,2%). The least implemented mode was phone coaching (69.9%). These findings show similar rates (above 75–87% across all modes) of implementation of DBT treatment modes to studies conducted with professionals from the US and UK after DBT-IT [24, 25, 27], being individual therapy and group skills training the most implemented modes and phone coaching and consultation team meetings the least implemented. These results contribute to the existing evidence on the effectiveness of DBT-IT to increase implementation of DBT, in this case by Spanish-speaking professionals.
Findings of the study also showed a significant increase in the implementation of each of the treatment modes, except for individual therapy, between pre-training and post-training. This result could be related to the fact that individual therapy is the least demanding mode in terms of human resources and it was already used largely by the professionals before the intensive training. Moreover, a significant increase in mindfulness practice among professionals was found. This result may have a positive effect on the subsequent implementation of DBT since results of other studies have shown that mindfulness practice is associated with decreases in burnout among health professionals (e.g. 38). Additionally, significantly higher implementation of the DBT group skills training mode was found for Latin American participants. A possible interpretation is that most professionals from Latin America were working on private practice so more opportunities to carry out group skills training may be available.
Exploring therapist variables that could influence the implementation of DBT treatment modes, findings indicated a greater general number of implementation barriers detected among professionals who had not implemented phone coaching mode compared to those who had applied it. On the other hand, a higher number of barriers related to “team problems” (e.g. “team members left”, “no real commitment to learn and implement DBT”, “lack of reinforcers in team meetings”) among professionals who did not implement the consultation team meeting mode. In this regard, other studies [24, 29] have found similar barriers to implementing telephone coaching (having to work outside working hours or not having funding for this work) and the standard model of DBT (time commitment and balance of other functions, and staff resources such as attrition). Interestingly, results found by Landes et al. [27] indicate that the three barriers rated as unable to be overcome by the highest percentage of public centers that had received DBT training were related to the implementation of telephone coaching.
As discussed by Flynn et al. [32], the lower implementation rates of phone coaching may have to do with the requirement for extended patient care time outside working hours. Therefore, as suggested by Chapman [39], considering other strategies to improve implementation of phone coaching mode such as using more remotely means (via text, email, etc.) to contact therapist or other ways to ensure skills generalization (e.g. homework assignments) might be an important target during DBT-IT to help practitioners overcome this barrier. On the other hand, and although DBT-IT is a team focused training [23], a possible solution to overcome this implementation barrier may be to explore team problems more in depth during supervision/mentoring meetings and finding strategies to increase team members commitment and as well to figure it out possible reinforcers (e.g. validation, recognize achievements, etc.) during consultation team meetings.
Except for implementation barriers, no further differences regarding therapist variables were found in the rest of the study variables regarding treatment modes implementation.
To our knowledge, no previous studies have related barriers to the level of implementation of each specific treatment modality. The results of this study illustrate the relationship between professional-reported barriers and implementation of DBT treatment modes. Thus, if successful implementation of the telephone coaching and consultation team modes are to be achieved, it will be necessary to address important barriers such as team commitment and other organizational barriers. Findings of this study may also allow to evaluate the suitability of different implementation strategies before carrying them out in a specific system and suggest that training programs should include strategies to overcome barriers to implementation. These results are also in line with the existing knowledge of the selection tasks prior to the training such as the recommendations published by Swales [40] where important aspects to ensure a successful implementation of DBT are pointed out, such as the selection of staff capable of delivering an effective treatment, the reallocation of clinician time and the strategies for achieving team and organizational commitment.
Moreover, correlation analyses showed significant positive relationships between confidence in applying DBT and self-efficacy to work with patients with suicidal behavior, and between motivation and confidence in applying DBT and the implementation of all modes of treatment. These findings correspond to some studies in which lower training needs, greater previous DBT experience [12, 24] and therapist skills were identified as facilitators for the implementation of DBT [24].
Significant positive correlations were also found between the total implementation barriers and burnout. Specifically, burnout was associated with higher administrative and structural barriers and the latter with lower DBT implementation. These results are similar to previous studies such as the one by Carmel et al. [29] in which burnout appears to be related to many of the barriers that impede the implementation of new evidence-based psychological treatments. Therefore, therapists’ burnout may be another important variable to decrease in order to improve the implementation of DBT.
Finally, regarding reach after DBT-IT, DBT was implemented to a lesser extent by those professionals with the highest patient load. In this study, “too many patients” was also one of the most reported barriers. These findings could be related to all the other findings already cited, such as burnout, barriers related to time commitment and balance of other practitioner roles and lack of staff resources. Therefore, it would be interesting to evaluate these factors as potential predictors of implementation of DBT.
Considering these findings, implications for mental health practice and policies should be taken into account for therapist treating people with risk of suicide. Organizations may consider the need of providing strategies to reinforce phone coaching outside office hours for therapists to help their patients generalize skills outside the health system, as well as to reduce patient load for therapist applying DBT standard, which requires more time to be applied. Enhancing supervision may help overcome team barriers regarding consultation team meetings. Implementing DBT for BPD has been related with reduced costs for mental health systems mainly due to the reduced use of inpatient services [41] and therefore, overcoming barriers of DBT implementation may help increase its adoption more widely.
Limitations and future directions.
Although promising, the findings of this study must be considered in light of their limitations. First, despite the research team’s efforts to increase participants response rates, completion rate for the survey from post-training was lower than expected. Results comparing participants who completed only pre-training survey versus those who completed pre- and post-training surveys indicated that the ones who completed only baseline were significantly less concerned and perceived more confidence and self-efficacy to manage and treat suicide risk. Therefore, a possible interpretation is that a subset of the sample might not be needed/interested in continuing providing information at post-training. The generalizability of these data may also be affected by the existence of an unequal distribution in the variable “country”, with a greater number of participants from Latin America than from Spain. Another important limitation is that no follow-up was conducted after training and no group comparison was included in this study. Future longitudinal research with bigger samples and experimental designs are needed to confirm these results. On the other hand, it is also hoped further research with Spanish-speaking professionals will be carried out. Finally, factors influencing less frequently implemented DBT implementation modes, like phone coaching and consultation team, may need to be further investigated.
Conclusions
To conclude, findings of this study suggest that DBT-IT seems to be a suitable training model to increase self-efficacy in the treatment of suicide risk and confidence in applying DBT, as well as to facilitate the implementation of DBT, in Spanish-speaking mental health professionals. Participants with more implementation barriers reported lower rates of consultation team and implementation of phone coaching. It will be very important to address team barriers to achieve a successful implementation of the consultation team mode and other barriers for implementing the telephone coaching mode. If DBT can be brought into clinical practice in Spanish-speaking countries, it could contribute to suicide prevention.
Acknowledgements
We would like to acknowledge the collaboration of the agency DBT Iberoamérica for facilitating the dissemination of the study among the DBT-IT participants.
Author contributions
Design M.V.N-H. and P.G.; conceptualization M.V.N-H., A.G.-P., P.G. and J.O.; methodology M.V.N-H., O.P-B., J.O. and A.G.-P.; investigation M.V.N-H. and P.G.; resources M.V.N-H; writing - original draft preparation M.V.N-H., A.A. and O.P-B.; writing - review and editing J.O., A.G.-P., P.G. and D.R.; project administration M.V.N-H. All authors participated in the review and revision of the manuscript and have approved the final manuscript to be published.
Funding
This study was funded by Fundación Ibercaja- University of Zaragoza (Spain) as part of their “Convocatoria: 2021 “Proyectos de Investigación, Desarrollo e Innovación para Jóvenes Investigadores” (grant number: JIUZ-2021-SOC-11) and it was also supported by Gobierno de Aragon (Departamento de Ciencia, Universidad y Sociedad del Conocimiento; Research team: S31_23R).
Data availability
The datasets generated and/or analyzed during the current study are not publicly available but are available from the corresponding author upon reasonable request.
Declarations
Ethics approval and consent to participate
This study follows the standards of the Declaration of Helsinki and existing guidelines in Spain and the European Union for the protection of patients in clinical trials. The study procedure was subject to the approval of the Clinical Research Ethics Committee of Aragón (CEICA), maintaining the explicit commitments of the Organic Law 5/1992 of October 20, 1992, which was approved by the CEICA in September 2020 (Register code: PI20/454).
Consent for publication
Not applicable.
Competing interests
M.V.N-H., D.R. and P.G. are compensated for providing training in DBT. The remaining authors declare that they have no competing interests.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.World Health Organization. Suicide. https://www.who.int/news-room/fact-sheets/detail/suicide
- 2.Geneva. World Health Organization. Suicide worldwide in 2019: global health estimates. 2021. Licence: CC BY-NC-SA 3.0 IGO.
- 3.Roush JF, Brown SL, Jahn DR, Mitchell SM, Taylor NJ, Quinnett P, et al. Mental Health professionals’ suicide risk Assessment and Management practices: the impact of fear of suicide-related outcomes and Comfort Working with suicidal individuals. Crisis Jan. 2018;1(1):55–64. [DOI] [PubMed] [Google Scholar]
- 4.Van Der Feltz-Cornelis CM, Sarchiapone M, Postuvan V, Volker D, Roskar S, Grum AT, et al. Best practice elements of multilevel suicide Prevention Strategies: a review of systematic reviews. Crisis Nov. 2011;1(6):319–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Harned MS, Lungu A, Wilks CR, Linehan MM. Evaluating a Multimedia Tool for suicide risk Assessment and Management: the Linehan suicide safety net. J Clin Psychol Mar. 2017;73(3):308–18. [DOI] [PubMed] [Google Scholar]
- 6.O’Connor K, Muller Neff D, Pitman S. Burnout in mental health professionals: a systematic review and meta-analysis of prevalence and determinants. Eur Psychiatry Sept. 2018;53:74–99. [DOI] [PubMed] [Google Scholar]
- 7.Salyers MP, Bonfils KA, Luther L, Firmin RL, White DA, Adams EL, et al. The relationship between Professional Burnout and Quality and Safety in Healthcare: a Meta-analysis. J Gen Intern Med Apr. 2017;32(4):475–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Panagioti M, Geraghty K, Johnson J, Zhou A, Panagopoulou E, Chew-Graham C, et al. Association between Physician Burnout and Patient Safety, Professionalism, and patient satisfaction: a systematic review and Meta-analysis. JAMA Intern Med Oct. 2018;1(10):1317. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 9.Mitchell SM, Taylor NJ, Jahn DR, Roush JF, Brown SL, Ries R, et al. Suicide-related training, Self-Efficacy, and Mental Health Care Providers’ reactions toward suicidal individuals. Crisis Sept. 2020;41(5):359–66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Smith AR, Silva C, Covington DW, Joiner TE. An assessment of suicide-related knowledge and skills among health professionals. Health Psychol. 2014;33(2):110–9. [DOI] [PubMed] [Google Scholar]
- 11.Rothes I, Henriques M. Health professionals facing suicidal patients: what are their clinical practices? Int J Environ Res Public Health Jun. 2018;8(6):1210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Beidas RS, Kendall PC. Training therapists in evidence-based practice: a critical review of studies from a systems-contextual perspective. Clin Psychol Sci Pract Mar. 2010;17(1):1–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Binkley EE, Leibert TW. Prepracticum Counseling Students’ perceived preparedness for suicide response. Couns Educ Superv Jun. 2015;54(2):98–108. [Google Scholar]
- 14.Linehan M. Cognitive-behavioral treatment of borderline personality disorder. 3. print. New York: Guilford Pr; 1993. 558 p. (Diagnosis and treatment of mental disorders).
- 15.Linehan M. DBT skills training manual. Second edition. New York London: The Guilford Press; 2015. 504 p.
- 16.Linehan MM, Comtois KA, Ward-Ciesielski EF. Assessing and managing risk with suicidal individuals. Cogn Behav Pract May. 2012;19(2):218–32. [Google Scholar]
- 17.Dimidjian S, Linehan MM. Mindfullness practice. In: Fisher JE, O’Donohue WT, editores. Cognitive Behavior Therapy: Applying Empirically Supported Techniques in Your Practice. 2nd ed. Hoboken, New Jersey; 2008. pp. 327 – 36.
- 18.Calati R, Courtet P. Is psychotherapy effective for reducing suicide attempt and non-suicidal self-injury rates? Meta-analysis and meta-regression of literature data. J Psychiatr Res Aug. 2016;79:8–20. [DOI] [PubMed] [Google Scholar]
- 19.Turecki G, Brent DA. Suicide and suicidal behaviour. Lancet Mar. 2016;387(10024):1227–39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Chesney E, Goodwin GM, Fazel S. Risks of all-cause and suicide mortality in mental disorders: a meta-review. World Psychiatry Jun. 2014;13(2):153–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.McHugh RK, Barlow DH. The dissemination and implementation of evidence-based psychological treatments: a review of current efforts. Am Psychol. 2010;65(2):73–84. [DOI] [PubMed] [Google Scholar]
- 22.Landes SJ, Linehan M. Dissemination and implementation of dialectical behavior therapy: an intensive training model. In: Dissemination and implementation of evidence-based psychological interventions. New York, NY: Oxford University Press; pp. 187–208.
- 23.DuBose A, Navarro-Haro MV, Linehan M. Evidence-based training: the intensive model of training in dialectical behaviour therapy. In: The Oxford Handbook of Dialectical Behavior Therapy. New York, NY: Oxford University Press; pp. 965–79.
- 24.King JC, Hibbs R, Saville CWN, Swales MA. The survivability of dialectical behaviour therapy programmes: a mixed methods analysis of barriers and facilitators to implementation within UK healthcare settings. BMC Psychiatry Dec. 2018;18(1):302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Navarro-Haro MV, Harned MS, Korslund KE, DuBose A, Chen T, Ivanoff A, et al. Predictors of Adoption and Reach following Dialectical Behavior Therapy Intensive Training™. Community Ment Health J Jan. 2019;55(1):100–11. [DOI] [PubMed] [Google Scholar]
- 26.Ditty MS, Landes SJ, Doyle A, Beidas RS. It takes a village: a mixed method analysis of inner setting variables and dialectical behavior therapy implementation. Adm Policy Ment Health Ment Health Serv Res Nov. 2015;42(6):672–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Landes SJ, Rodriguez AL, Smith BN, Matthieu MM, Trent LR, Kemp J, et al. Barriers, facilitators, and benefits of implementation of dialectical behavior therapy in routine care: results from a national program evaluation survey in the Veterans Health Administration. Transl Behav Med Dec. 2017;7(4):832–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Perseius K, Kåver A, Ekdahl S, Åsberg M, Samuelsson M. Stress and burnout in psychiatric professionals when starting to use dialectical behavioural therapy in the work with young self-harming women showing borderline personality symptoms. J Psychiatr Ment Health Nurs Oct. 2007;14(7):635–43. [DOI] [PubMed] [Google Scholar]
- 29.Carmel A, Fruzzetti AE, Rose ML. Dialectical Behavior Therapy Training to reduce clinical burnout in a public behavioral Health System. Community Ment Health J Jan. 2014;50(1):25–30. [DOI] [PubMed] [Google Scholar]
- 30.Swales MA, editor. The Oxford handbook of dialectical behavior therapy. paperback edition. New York, NY: Oxford University Press; 2020.
- 31.Herschell AD, Kogan JN, Celedonia KL, Gavin JG, Stein BD. Understanding Community Mental Health administrators’ perspectives on dialectical behavior therapy implementation. Psychiatr Serv Jul. 2009;60(7):989–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Flynn D, Joyce M, Gillespie C, Kells M, Swales M, Spillane A, et al. Evaluating the national multisite implementation of dialectical behavior therapy in a community setting: a mixed methods approach. BMC Psychiatry Dec. 2020;20(1):235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Schmidt IH, Ivanoff A, Korslund K, Linehan MM. Program elements of treatment questionnaire. Seattle: Research & Therapy Clinics; 2008. [Google Scholar]
- 34.Kristensen TS, Borritz M, Villadsen E, Christensen KB. The Copenhagen Burnout Inventory: a new tool for the assessment of burnout. Work Stress Jul. 2005;19(3):192–207. [Google Scholar]
- 35.Molinero Ruiz E, Basart Gómez-Quintero H, Moncada Lluis S. Fiabilidad Y validez del Copenhagen Burnout Inventory para su uso en España. Rev Esp Salud Pública Apr. 2013;87(2):165–79. [DOI] [PubMed] [Google Scholar]
- 36.Dimeff LA, Harned MS, Woodcock EA, Skutch JM, Koerner K, Linehan MM. Investigating Bang for your training Buck: a randomized controlled trial comparing three methods of Training clinicians in two core strategies of Dialectical Behavior Therapy. Behav Ther May. 2015;46(3):283–95. [DOI] [PubMed] [Google Scholar]
- 37.IBM SPSS Statistics. IBM Corp. New York: Armonk; 2021. [Google Scholar]
- 38.Luken M, Sammons A. Systematic review of mindfulness practice for reducing Job Burnout. Am J Occup Ther Mar. 2016;1(2):p70022500201–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Chapman AL. Phone coaching in dialectical behavior therapy. New York London: The Guilford Press; 2019. p. 214. (Guilford DBT® practice series). [Google Scholar]
- 40.Swales MA. Implementing DBT: selecting, training and supervising a team. Cogn Behav Ther Jun. 2010;3(2):71–9. [Google Scholar]
- 41.Wagner T, Fydrich T, Stiglmayr C, Marschall P, Salize HJ, Renneberg B, et al. Societal cost-of-illness in patients with borderline personality disorder one year before, during and after dialectical behavior therapy in routine outpatient care. Behav Res Ther Oct. 2014;61:12–22. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets generated and/or analyzed during the current study are not publicly available but are available from the corresponding author upon reasonable request.