Abstract
Background
Rib fractures are common in trauma patients, often leading to complications such as pneumonia and prolonged hospitalization. Surgical Stabilization of Rib Fractures (SSRF) has become increasingly prevalent in treating severe cases. However, traditional approaches, like posterolateral thoracotomy, are invasive and cause significant muscle damage. Recently, muscle-sparing minimally invasive techniques have been introduced, yet they still require advanced reduction and fixation techniques to avoid complications. This study presents an “ultra” minimally invasive SSRF (uMI-SSRF) technique designed to minimize surgical wounds and soft tissue damage while maintaining the benefits of rib fixation.
Methods
This study involved 76 patients with multiple rib fractures treated using the uMI-SSRF technique between August 2021 and December 2023. Preoperative chest tomography with 3D reconstruction was used for surgical planning. The technique employed small incisions (3–5 cm), muscle-sparing approaches, and advanced fixation techniques. Data on patient demographics, intraoperative details, and postoperative outcomes were collected.
Results
The mean patient age was 58 years, with 66% being male. On average, patients had 6.4 fractured ribs, and 3.5 ribs with 3.88 plates were fixed per surgery, achieving a fixation/fracture ratio of 59%. The average wound length was 4.2 cm, with a mean operation time of 122 min. Most patients required only one incision (74%). The median hospital length of stay was 7 days, with a pneumonia rate of 5%. No wound infections or implant-related complications were observed.
Conclusions
The uMI-SSRF technique effectively reduces wound size and soft tissue damage in rib fracture stabilization while maintaining high fixation quality. This method shows promise for improving patient outcomes, reducing recovery time, and minimizing complications. Further studies with larger sample sizes and comparisons with other methods are warranted to verify the advantages of uMI-SSRF.
Supplementary Information
The online version contains supplementary material available at 10.1186/s13017-024-00566-3.
Keywords: Surgical stabilization of rib fractures, SSRF, Ultra minimally invasive surgery, Flail chest, Postoperative complications
Introduction
Rib fractures have been identified in as many as 39% of patients with blunt chest trauma and in up to 10% of all trauma admissions [1, 2]. Surgical Stabilization of Rib Fractures (SSRF) is becoming more common in treating these injuries. Properly performed SSRF can reduce the risk of pneumonia, tracheostomy rates, mechanical ventilation days, length of stays in intensive care units and hospitals, and mortality rates in patients with flail chest or multiple ribs fracture [3–7]. Flail segment is generally accepted as an indication for SSRF among different guidelines [8–11]. However, up to 80% of these patients may not have received the surgery, and rates of fixation among different hospitals ranged from 0–88% [12]. A possible reason may be the unfamiliarity of surgical exposures, fixation techniques, and instrumentation [13].
Traditionally, SSRF was performed using a posterolateral thoracotomy incision [14]. This extensive approach can damage soft tissue and compromise neurovascular due to muscle division. Postoperative muscle pain and dysfunction hinder the progress of fracture healing, as the benefits of the procedure may be reduced by morbidities iatrogenically produced from the large incision [15]. Recently, muscle-sparing minimally invasive techniques have been introduced to decrease morbidity [14–21]. Most technical papers have addressed the surgical exposures for SSRF, but only a handful have discussed reduction and fixation techniques [11, 16, 18]. Due to the extensiveness and complexity of rib fractures, without precise surgical planning and advanced reduction and fixation technique, a minimally invasive incision may need to be extended, ultimately resembling a thoracotomy incision. The benefits of fixation may therefore be compromised by the complications of the large wound.
Our paper focuses on novel and modified techniques that enables SSRF to be performed safely through a small incision and limited window. We introduce an “ultra” minimally invasive technique for SSRF(uMI-SSRF) to further reduce wound size and soft tissue damage while maintaining the benefits of SSRF.
Methods
Pre-operation and planning
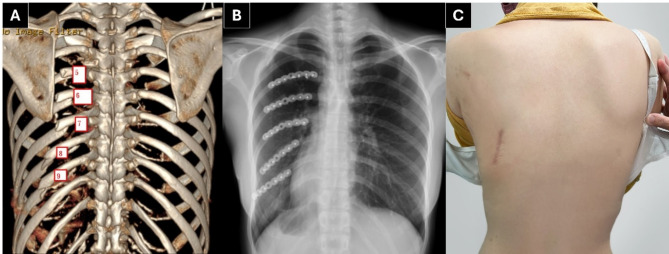
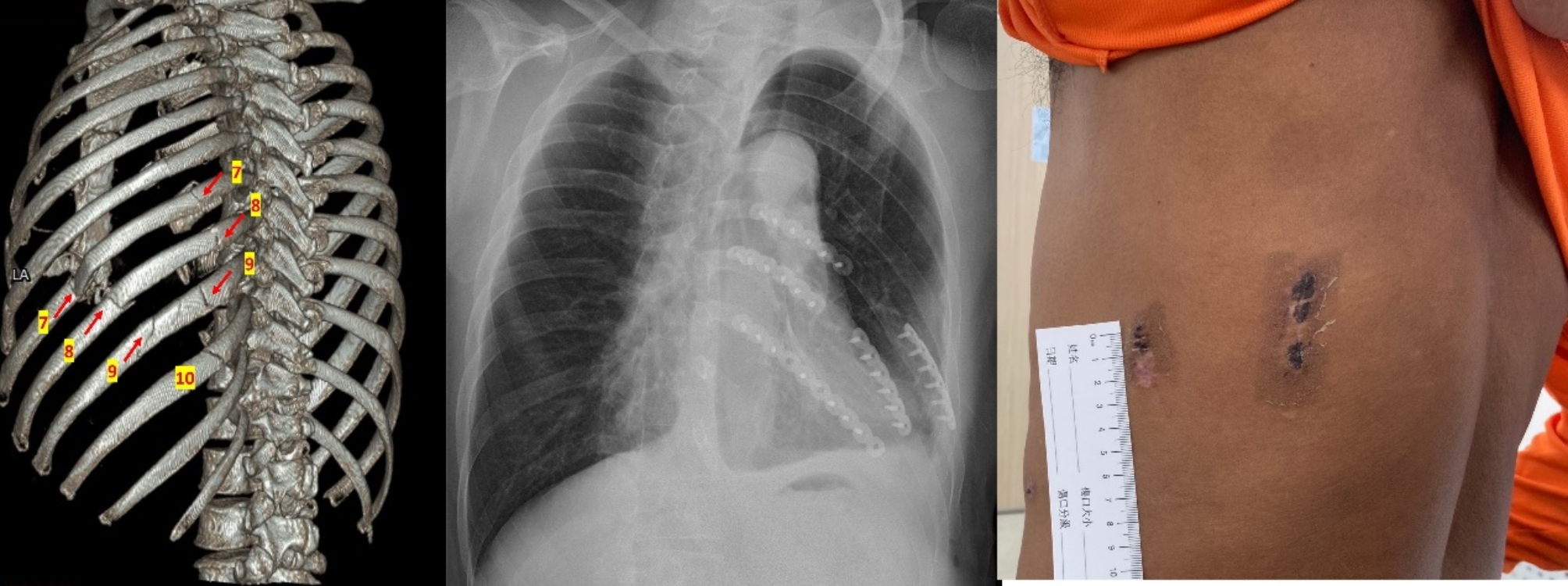
When a patient is preparing for Surgical Stabilization of Rib Fractures (SSRF), a routine chest tomography with three dimensional(3D) reconstruction of the ribs is obtained to help the surgeon identify the fracture sites and develop a clear operation plan (Fig. 1). The priority of surgical stabilization is given to fractures that most impact pulmonary function, typically those that are severely displaced between the 4th and 9th ribs. Fractures outside this range are less commonly operated on unless they are severely displaced or show clinical significance. In cases of flail segment, the site with the greatest displacement is prioritized for repair. Generally, a fixation ratio of over 50% of the fractured ribs is targeted to ensure adequate stabilization while balancing the risks and benefits of the surgery.
Fig. 1.
Surgical Stabilization of Rib Fractures (SSRF) of 5 consecutive ribs in 4.5 cm wound. A: Preoperative chest tomography with 3D reconstruction shows left posterolateral 5th to 9th ribs fracture with displacement B: Chest radiograph of post-surgical stabilization of the rib fractures(SSRF) C: Final incision wound of 4.5 cm
Patient positioning, video-assisted thoracoscopic surgery (VATS)
Under one-lung ventilation, the patient is placed in the lateral decubitus position with the affected side up and the arm abducted over the head. Video-Assisted Thoracoscopic Surgery (VATS) is performed when there is a suspicion of substantial hemothorax or lesions on the lung or diaphragm. It also allows us to check for lung entrapment at the fracture site and ensures proper lung deflation during the stabilization procedure. Initial hemothorax is evacuated, and the fracture site is confirmed intrathoracically.
Incision and exposure
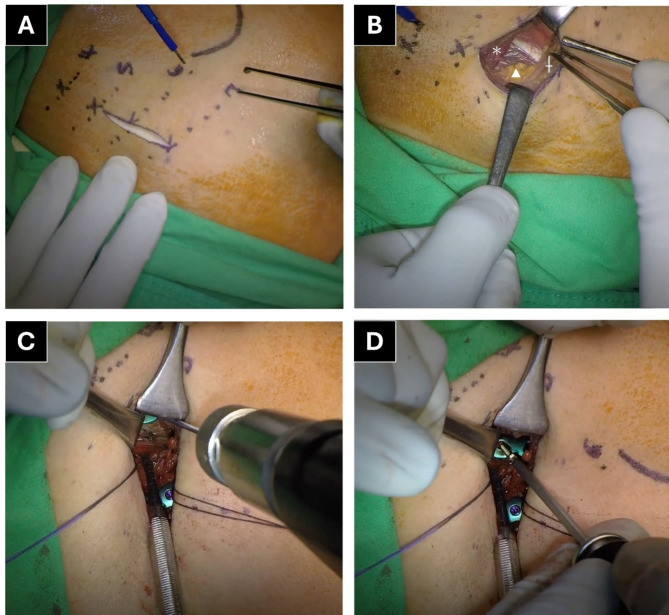
The edges of fractured ribs can cause skin tenting or create an indentation during chest wall palpation. The sites of the ribs planned for fixation are marked, and a longitudinal incision is made connecting these marks (Fig. 2A). A 3–5 cm incision is performed to fix up to 5 consecutive ribs, and the fascia is incised in line with skin incision.
Fig. 2.
The ultra Minimally Invasive Surgical Stabilization of Rib Fractures (uMI-SSRF) surgical technique. A: Dotted lines show the target ribs, “X” indicates the fracture edge, a longitudinal incision is made B:The Auscultation triangle, “*” stands for rhomboid muscle, "†"stands for latissimus dorsi muscle, "Δ"stands for Erector Spinae muscle. C: Free hand drilling of 4th rib after temporary reduction with level arm technique D: Compression nonlocking screw for pressing the plate to the bone
For posterolateral rib fractures, the incision should pass through the auscultation triangle (Fig. 2B). The fat or bursa at the auscultation triangle is separated transversely, parallel to the latissimus dorsi muscle below. A finger is inserted under the scapula to mobilize it, then the scapula is retracted laterally to widen the created window. This window is sufficient for fixing the 5th to 7th ribs. To fix the 3rd and 4th ribs, or the 8th and 9th ribs, perform a longitudinal transection of less than 3 cm on the rhomboid and latissimus dorsi muscles, respectively. Alternatively, when only the upper or lower ribs require fixation, a window can be created by dividing the muscle parallel to their fibers. When the fracture lies beneath the erector spinae muscle, elevate the muscle instead of transecting it.
For anterolateral rib fractures, the skin incision is designed by connecting the fracture marks. The serratus muscle window beneath is created parallel to the muscle fibers, which is sufficient for up to three fractured ribs. For more than four fractured ribs, two separate muscle windows within the same incision can be made.
When rib fractures occur in different regions, such as posterior and lateral, a double incision is made. This approach is also used when more than six consecutive ribs require fixation or when a long plate is necessary for specific fracture patterns (Fig. 3).
Fig. 3.
Double incision for Long plate placement in flail segment patient. Double incision for patients with flail segment and slide a long plate within two wounds
Bone reduction
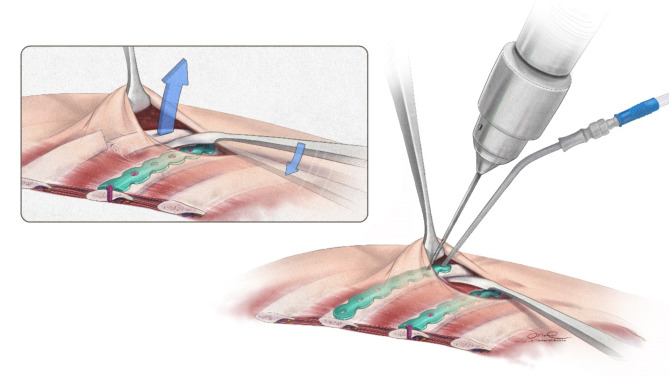
The cornerstone of fracture fixation, crucial for avoiding postoperative complications and achieving bone union, is the quality of the fracture reduction. One of three reduction techniques can be employed. First, bone reduction forceps or a towel clamp can directly pick up the bone. Second, the lever arm technique is used for ribs hidden under the skin flap or scapula. This involves sliding a mini-Hohmann retractor under the depressed bone segment and using the neighboring intact or fixed rib as a fulcrum to raise the bone (Fig. 4). When performing this technique, it is essential to ensure the quality of reduction and fixation in the neighboring fulcrum-fixed rib; otherwise, there is a risk of compromising the fixation. Finally, for osteoporotic or comminuted bones, a right angle forcep or mini-Langenbeck retractor is inserted from the rib’s upper end to lift it.
Fig. 4.
The Lever Arm Technique for temporary reduction. A mini Hohmann retractor is slid under the depressed bone segment, using a neighboring rib as a fulcrum to elevate the rib
Plate positioning and fixation
After achieving temporary reduction, a 6 or 7-hole short segment plate is carefully contoured and positioned centrally with three holes on each side of the fracture. Using an instrument, usually the suction tip, the plate is held in place. The second to the last hole on each side of the fracture is drilled without a drill guide (Fig. 2C). Compression nonlocking screws are used to firmly press the plate against the bone, ensuring perfect contouring and shortening the fracture gap. The axis of the screw should be perpendicular to the plate whenever possible. However, if the visible operational space is limited, the screw may be positioned obliquely to adapt to the constraints. An alternative to compression lag screws are cerclage wires, which are useful when the bone is osteoporotic or comminuted, and the compression effect of the screw fails. Sometimes, longer plates are necessary to bridge comminuted fracture patterns. After ensuring adequate plate positioning and fracture reduction, the remaining screw holes are filled with locking screws, with a minimum of three screws on each side of the fracture. The nonlocking screws are subsequently replaced with locking screws. If the screw’s axis is not perpendicular to the plate, the locking mechanism for the exchanged locking screw may fail. This can be easily corrected by redrilling the hole using the drill guide. An additional movie file shows this in more detail [see Additional file 1].
In remote areas, a 90-degree drill and screwdriver may be used for locking screw holes located beneath the scapula. Stab incisions can also be made for drill holes that are too far from the main wound. Self-drilling screws are suitable for use in anatomically sensitive areas, such as near vital organs like a hypertrophied heart, where the risk of injury is higher. Variable angle (VA) screws can be useful when plate positioning or contouring is suboptimal.
Final VATS examination
After properly fixing the fracture, ensure thorough irrigation and hemostasis before closing the wound. Perform VATS to validate the fixation intrathoracically, check for penetrated screws, remove any remaining hemothorax, and insert a 14 French pigtail or 28 French chest tube for drainage. Subcutaneous wound drains are not routinely placed.
Data collection and analysis
We recorded the following baseline characteristics: age, sex, body mass index (BMI), smoking status, injury mechanism, Injury Severity Score (ISS), presence of flail segment, time to surgery, and the side and number of fractures. During the operation, we recorded the total number of ribs fixed, operation time, blood loss, and the number and length of incision wounds. Each patient was routinely followed up at 1, 2, 4, and 8 weeks after discharge, with continued follow-ups for at least 6 months post-operation. All operative and postoperative outcomes, including mechanical ventilation days, intensive care unit (ICU) length of stay, and hospital length of stay, were recorded in this study. Complications included tracheostomy, pneumonia, wound infection, implant-related issues, and mortality. Implant-related complications were defined as implant breakage, dislodgment, or removal due to irritation. Approval was obtained from the Institutional Review Board (KMUHIRB-E(II)-20240265).Statistical analyses of the data were performed using SPSS version 23.0 (SPSS Inc., Chicago, IL, USA). Continuous data are described as means and standard deviations or as medians and interquartile ranges (IQR). Categorical data are presented as absolute and relative frequencies.
Result
From August 2021 through December 2023, our team performed Ultra Minimally Invasive Surgical Stabilization of Rib Fractures (uMI-SSRF) on 76 patients with multiple rib fractures. The indications for surgery included patients with flail segments, those with multiple (≥ 3) displaced fractures accompanied by pulmonary physiologic derangements, or patients who did not respond to multi-modal pain therapy. The characteristics of these patients are reported in Table 1. Among these patients, the mean age was 58 years, and 50 patients (66%) were men. The average Injury Severity Score (ISS) was 21.3 (range 9–36), and 40 patients (52.6%) had a flail segment. On average, the patients had 6.4 (range 3–14) fracture ribs, with 8.5 fracture sites (range 3–19). The location and displacement of the ribs were classified and recorded according to the consensus paper from World Society of Emergency Surgery (WSES) and the Chest Wall Injury Society (CWIS) [11].
Table 1.
Characteristics of the patients (N = 76) who received the Ultra minimally invasive Surgical stabilization of Rib fractures (uMI-SSRF)
| Characteristic | mean ± SD or n% | Range |
|---|---|---|
| N | 76 | |
| Age, mean ± SD | 58 ± 13.4 | 21–81 |
| Sex, n(%) | ||
| Male | 50 (66%) | |
| Female | 26 (34%) | |
| Body Mass Index, mean ± SD | 24.51 ± 3.42 | 17.3–32.5 |
| Smoking, n (%) | ||
| Nonsmoking | 57 (75%) | |
| Smoking | 17 (22%) | |
| Quit | 2 (3%) | |
| Injury Mechanism, n (%) | ||
| Motor-vehicle collision | 62 (82%) | |
| Fall from Heights | 5 (7%) | |
| Ground Fall | 5 (7%) | |
| Fall from Stairs | 3 (4%) | |
| Direct contusion (hit) | 1 (1%) | |
| Injury Severity Score (ISS), mean ± SD | 21.26 ± 6.17 | 9–36 |
| Intrathoracic lesions, n (%) | ||
| Hemothorax | 71 (93%) | |
| Lung entrapment | 3 (3.9%) | |
| Lung laceration | 4 (5.2%) | |
| Diaphragm rupture | 2 (2.6%) | |
| Flail Segment, n (%) | ||
| No | 36 (47%) | |
| Yes | 40 (53%) | |
| Rib Fracture Side, n (%) | ||
| Left | 44 (58%) | |
| Right | 28 (37%) | |
| Bilateral | 4 (5%) | |
| Rib Fractures by Location, mean ± SD | ||
| Posterior | 5.23 ± 2.25 | |
| Lateral | 4.17 ± 1.71 | |
| Anterior | 3.42 ± 1.86 | |
| Fib Fracture Displacement(n), mean ± SD | ||
| Severely Displaced | 2.53 ± 1.45 | |
| Displaced | 2.68 ± 1.68 | |
| Offset | 3.49 ± 2.37 | |
| Nondisplaced | 2.73 ± 1.70 | |
| Total Fracture, mean ± SD | 6.4 ± 2.1 | 3–14 |
| Total Fracture sites, mean ± SDa | 8.5 ± 3.63 | 3–19 |
| Time to surgery(hr), mean ± SD | 39 ± 30.1 | 4-152 |
aIf a single rib has 2 fractures, it is recorded as 2 fracture sites
The intraoperative results are listed in Table 2. An average of 3.5 ribs were fixed (range 2–6) with 3.88 plates (range 2–8), resulting in an average fixation-fracture ratio of 59% (range 29–100%). 89% (range 33–100%) of the severely displaced or displaced ribs were fixed. Of the 274 fracture sites that were fixed, 77% were severely displaced or displaced, the rest were offset fractures. 56 patients (74%) required one surgical incision for their fracture fixation, while the rest needed two or three separate incisions. The average wound length was 4.2 cm (range 2.5–5 cm). The average operation time for each surgery was 122 min (range 55–300 min), with an average time to fix each rib of 35 min (range 20–102 min).
Table 2.
Intraoperative results for the patients (N = 76) who received the Ultra minimally invasive Surgical stabilization of Rib fractures (uMI-SSRF)
| Intraoperative Results | Total | Range |
|---|---|---|
| N | 76 | |
| Fixed Ribs (n), mean ± SD | 3.5 ± 0.88 | 2–6 |
| Implants Used (n), mean ± SD | 3.88 ± 1.16 | 2–8 |
| Fixation Fracture Ratio (%), mean ± SD | 59 ± 17% | 29–100% |
| Fixation Displaced Ratio% a, mean ± SD | 89±18% | 33–100% |
| Total Fixed Fracture Sites, n (%) | 274 | |
| Severely Displaced | 83 (30.3%) | |
| Displaced | 129 (47.1%) | |
| Offset | 62 (22.6%) | |
| Wound Length Average(cm)b, mean ± SD | 4.2 ± 0.7 | 2.5-5.0 |
| Wound number | ||
| 1 | 56 (74%) | |
| 2 | 18 (24%) | |
| 3 | 2 (3%) | |
| Operation time(min), mean ± SD | 122 ± 50.3 min | 50–300 min |
| Operation Time/Rib(min), mean ± SD | 35 ± 13.7 min | 13.7–102 min |
| Blood loss(ml), mean ± SD | 40.6 ± 51.0ml | 5-200 ml |
aThe percentage of displaced and severely displaced fracture sites that were fixed
bIf a patient has two or more wounds, the wound length is the average of the wounds
The outcome results are listed in Table 3. The patients stayed in the hospital for a median of 7 days (range 2–37 days). Four patients (5%) acquired pneumonia, and one patient (1.3%) with the underlying disease of chronic obstructive pulmonary disease (COPD) expired within 3 months. No wound infections or implant-related complications were noted in this patient series.
Table 3.
Overall postoperative results for the patients (N = 76) who received the Ultra minimally invasive Surgical stabilization of Rib fractures (uMI-SSRF)
| Overall Results | Total | Range |
|---|---|---|
| N | 76 | |
| ICU patients, n (%) | 27 (36%) | |
| ICU Length of Stay, median (IQR) | 4 (2.0–6.0) days | 1-12 days |
| Hospital Length of Stay, median (IQR) | 7 (6.0–11.0) days | 2-37 days |
| Mechanical Ventilation, n (%) | 20 (26%) | |
| Mechanical Ventilation Days, median (IQR) | 2 (1.0-3.5) days | 1-23 days |
| Complications | ||
| Tracheostomy, n (%) | 0 (0) | |
| Pneumonia, n (%) | 4 (5%) | |
| Wound Infection, n (%) | 0 (0) | |
| Implant Related Complication, n (%) | 0 (0) | |
| Mortality, n (%) | 1 (1%) | |
| Any outcome | ||
| 0 | 72(95%) | |
| ≥1 | 4 (5%) |
Discussion
Surgical stabilization of rib fractures (SSRF) began in the 1950s with instruments like cerclage wires, intramedullary devices, and clamping devices. However, it became widely accepted and popular in chest wall trauma surgery only in the past 15 years with the introduction of anatomically precontoured plates with locking screws [13, 22].
We successfully performed uMI-SSRF in 76 patients, fixing an average of 4 ribs with an average wound length of 4.2 cm. A fixation-fracture ratio of 59% was achieved, demonstrating sufficient stability for chest wall injuries [23, 24]. The average surgery time was 122 min, or 35 min per rib.
Taylor et al. utilized thoracotomy approaches and performed SSRF on 21 patients with multiple ribs fracture. They fixed a mean of 4.7(range, 2–7)ribs for a mean of 6(range, 3–10) fractures. Estimated blood loss and operative time was 98.1mL and 160.2 min respectively. The patients stayed in the intensive care unit and hospital for an average of 5.2days and 14.6 days [14]. Zhang et al. recorded the wound length in their series of SSRF with the zoning method, the average incision length was 6.2 cm for an average number of 5.3 internal fixations [21]. In the series by Schulz-Drost et al., they were able to fix 4 ribs with an average wound length of 6 to 7 cm, both posteriorly and laterally. Their average operation time was 100 min [19]. We achieved equivalent rib fixation with a shorter surgical wound and comparable operation time.
Our surgical approach follows the general principles mentioned in previous studies, utilizing a longitudinal incision through the auscultation triangle or the serratus muscle window, and minimal dissection of the trapezius, rhomboid, or latissimus dorsi muscles [20, 21, 25]. We were able to minimize our wound length due to modified reduction and plate holding techniques including lever arm reduction technique, freehand drilling and plate compression screw technique.
The optimal approach for SSRF remains controversial and largely depends on the surgeon’s familiarity with the exposure techniques. Posterolateral thoracotomy incision is a common approach for SSRF, especially among thoracic and trauma surgeons, as it provides a large view of the complete chest wall. However, the extensive muscle dissection associated with this approach can result in significant morbidity. The introduction of muscle-sparing techniques has minimized damage to soft tissues. Nonetheless, due to the extensiveness and complexity of rib fractures, without precise surgical planning and meticulous technique, a minimally invasive incision may need to be extended, ultimately resembling a thoracotomy incision. This can compromise the benefits of fixation due to the complications of a large wound. Currently, several minimally invasive surgical instruments, including upright plate holding forceps, 90-degree drills and screwdrivers, and Alexis wound retractors (Applied Medical, Rancho Santa Margarita, CA, USA), have proven helpful in reducing wound size and soft tissue damage [18]. However, each of these instruments may have its own limitations. Therefore, we successfully modified current SSRF techniques by integrating common fracture reduction and fixation techniques from orthopedic procedures, which we named ‘ultra’ Minimally Invasive Surgical Stabilization of Rib Fractures (uMI-SSRF).
There is no standard incision length for minimally invasive SSRF; however, most studies regarding this technique indicate an incision wound length ranging from 6 to 10 cm for fixing 3 to 4 fractured ribs [16, 19, 21, 26]. Our results demonstrate that it is possible to fix the same number of ribs with an even shorter incision length. Additionally, our study includes the largest number of patients among similar studies, highlighting the feasibility and consistency of this technique.
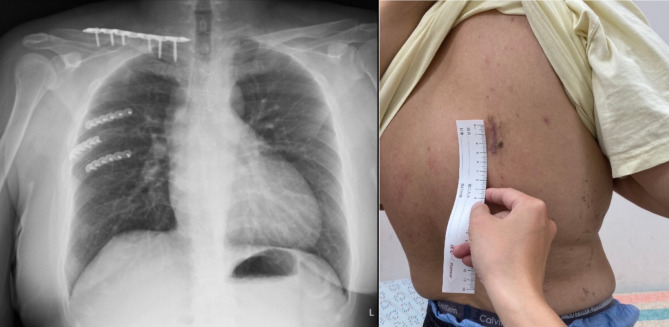
Obesity can influence surgical outcomes and affect the incision size necessary for a successful surgery [27]. Our technique can be successfully performed in patients with a body mass index (BMI) as high as 32.5 (Fig. 5). A 3 cm incision was sufficient to fix 3 posterolateral rib fractures. Langenbach et al. studied the accessible rib area with different wound lengths on cadavers and found that a minimum of 6 ribs can be accessed via a 5 cm wound through both posterior and lateral approaches [15], This provides strong evidence of the feasibility of our technique.
Fig. 5.
The ultra Minimally Invasive Surgical Stabilization of Rib Fractures (uMI-SSRF) performed in an obese patient. An obese patient (BMI 32.5) with fractured 5-7th ribs fixed in a 3 cm wound
A common technique for temporary fixation involves using plate holding forceps on both sides of the plate. This requires a larger incision to secure both ends of the plate simultaneously. The fixed angle nature of the clamps limits their effectiveness in small exposures. In osteoporotic bone, the compressive force of bone clamps may further shatter the fractured bone, leaving a more comminuted fracture pattern to fix. Additionally, they can potentially injure the intercostal artery and nerves while assessing either from the superior or inferior border of the rib. It is commonly understood that the intercostal artery runs inside the concave intercostal groove. However, in certain areas, such as 6 cm from the spinous process, the artery may not be shielded by the rib [28]. Routine clamping underneath the bone poses a threat to the underlying artery and nerves, potentially resulting in unnecessary blood loss and nerve damage.
Our article discusses three reduction techniques that can all hold the fracture in a reduced state while providing sufficient counterforce during drilling of screw holes in the bone. These techniques are minimally invasive to the intercostal space and underlying structures. The lever arm technique is particularly useful when the rib is well under the skin flap.
Many studies on minimally invasive techniques have addressed the use of a 90-degree drill and screwdriver [16, 18, 19]. We prefer performing freehand drilling instead. The ability to alter the drilling angle makes it more flexible in a small surgical exposure. A deviation of less than 30 degrees does not significantly affect the compression force of the screw [29]. A potential drawback of using a 90-degree drill is the lack of clear sensation when penetrating the cortical bone during drilling. Locking screws can be secured to the plate regardless of whether they are fully within the bone, therefore screw misplacement is a common technical error with this technique.
Freehand drilling without a threaded drill guide poses the risk of penetrating underlying vital organs. However, bi-cortical drilling is a well-established technique in orthopedic procedures. With sufficient practice, a surgeon can perform this technique with minimal risk to underlying organs. In our series, no complications from penetration were encountered. In specific anatomical areas requiring special attention, such as ribs near the heart, diaphragm, or liver, using a drilling guide or self-drilling screws can minimize the risk of critical complications.
Ribs, though classified as ‘flat’ bones, are typically curved in anatomy, with inconsistent curvature radii. The outer surface of the rib is also not uniformly flat and smooth, becoming more convex to triangular posterior to the costal angle. These unique features make contouring and positioning the plate more challenging. A short segment plate reduces the effort required for contouring, particularly in addressing the ‘frowning’ or ‘smiling’ in-plane curvature. Even when plate positioning is suboptimal, using variable angle screws can improve screw purchase and, consequently, increase construct stability.
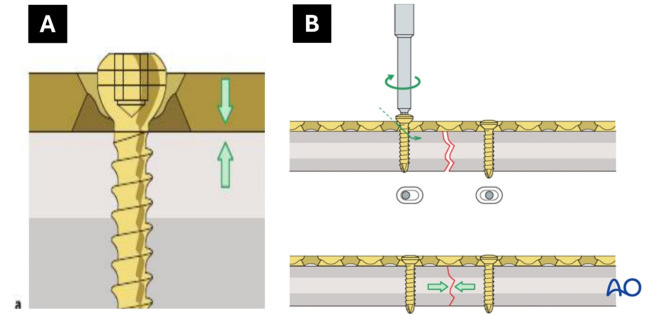
Conventional non-locking screws (Fig. 6) offer three benefits in uMI-SSRF. First, the smooth screw head presses the plate down to the bone, indirectly elevating the depressed bone. Second, the compression effect further contours the flexible titanium plate to perfection. Third, by inserting the screw eccentrically to the fracture site, it provides a dynamic compression effect. Together with the curved plate placed on the tension side of the rib, this acts as a tension band construct, shortening the fracture gap, increasing stability, and decreasing the chance of nonunion [30].
Fig. 6.
Benefits of plate compression with nonlocking screws and fracture gap reduction with eccentric screw placement. A. Nonlocking screws presses the plate against the bone, indirectly reduces the depressed bone to the plate. B. Inserting 2 nonlocking screws eccentrically at both side of the fracture further shortens the fracture gap, increases stability. From AO Surgery Reference, https://surgeryreference.aofoundation.org, with copyright by AO Foundation, Switzerland [31].
There are several limitations to our study. First, this is a single center study which may affect the generalizability of the results to other settings or surgical teams with different levels of expertise. Second, the absence of a control group makes it difficult to assess whether the uMI-SSRF technique offers superior outcomes compared to traditional or other minimally invasive methods. Further studies with larger sample sizes and comparisons with other methods are warranted to verify the advantages of uMI-SSRF.
Conclusion
In conclusion, uMI-SSRF is an effective, safe, and feasible technique for treating patients with rib fractures. It effectively reduces wound size and soft tissue damage in rib fracture stabilization while maintaining high fixation quality. This method shows promise for improving patient outcomes, reducing recovery time, and minimizing complications in rib fracture patients who require surgery.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplementary Material 1: Additional file 1: a detailed video of the Ultra Minimally Invasive Surgical Stabilization of Rib Fractures(uMI-SSRF).
Acknowledgements
We would like to acknowledge Monal MEDillustration for their illustration of Fig. 4.
Author contributions
HLL, DLT, CKL initiated the conception and design of study. HLL, DLT, CKL, JYL acquired the data. HLL, DLT, JYL, OYL, CCL, and SYL analyzed and interpreted the data. HLL drafted the manuscript primarily, DLT, CCL, SYL and OYL contributed. HLL, SYL, DLT, CCL, JYL, OYL helped revising the manuscript critically for important intellectual content. All authors reviewed the manuscript and agreed for publication.
Funding
Not applicable.
Data availability
No datasets were generated or analysed during the current study.
Declarations
Ethical approval
Approval for patient data was obtained from the Kaohsiung Medical University Institutional Review Board(KMUHIRB-E(II)-20240265).
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Dong-Lin Tsai and Sung-Yen Lin contributed equally to this work.
Contributor Information
Dong-Lin Tsai, Email: anakin711112@gmail.com.
Sung-Yen Lin, Email: tony8501031@gmail.com.
References
- 1.Lafferty PM, Anavian J, Will RE, Cole PA. Operative treatment of chest wall injuries: indications, technique, and outcomes. J Bone Joint Surg Am. 2011;93(1):97–110. [DOI] [PubMed] [Google Scholar]
- 2.Ziegler DW, Agarwal NN. The morbidity and mortality of rib fractures. J Trauma. 1994;37(6):975–9. [DOI] [PubMed] [Google Scholar]
- 3.Choi J, Gomez GI, Kaghazchi A, Borghi JA, Spain DA, Forrester JD. Surgical stabilization of Rib fracture to mitigate pulmonary complication and mortality: a systematic review and bayesian Meta-analysis. J Am Coll Surg. 2021;232(2):211–e92. [DOI] [PubMed] [Google Scholar]
- 4.Craxford S, Owyang D, Marson B, Rowlins K, Coughlin T, Forward D, et al. Surgical management of rib fractures after blunt trauma: a systematic review and meta-analysis of randomised controlled trials. Ann R Coll Surg Engl. 2022;104(4):249–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Sawyer E, Wullschleger M, Muller N, Muller M. Surgical Rib fixation of multiple Rib fractures and flail chest: a systematic review and Meta-analysis. J Surg Res. 2022;276:221–34. [DOI] [PubMed] [Google Scholar]
- 6.Ferreira ROM, Pasqualotto E, Viana P, Schmidt PHS, Andrighetti L, Chavez MP, et al. Surgical versus non-surgical treatment of flail chest: a meta-analysis of randomized controlled trials. Eur J Trauma Emerg Surg. 2023;49(6):2531–41. [DOI] [PubMed] [Google Scholar]
- 7.Hisamune R, Kobayashi M, Nakasato K, Yamazaki T, Ushio N, Mochizuki K, et al. A meta-analysis and trial sequential analysis of randomised controlled trials comparing nonoperative and operative management of chest trauma with multiple rib fractures. World J Emerg Surg. 2024;19(1):11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kasotakis G, Hasenboehler EA, Streib EW, Patel N, Patel MB, Alarcon L, et al. Operative fixation of rib fractures after blunt trauma: a practice management guideline from the Eastern Association for the surgery of Trauma. J Trauma Acute Care Surg. 2017;82(3):618–26. [DOI] [PubMed] [Google Scholar]
- 9.Pieracci FM, Majercik S, Ali-Osman F, Ang D, Doben A, Edwards JG, et al. Consensus statement: Surgical stabilization of rib fractures rib fracture colloquium clinical practice guidelines. Injury. 2017;48(2):307–21. [DOI] [PubMed] [Google Scholar]
- 10.Kong LW, Huang GB, Yi YF, Du DY. Consensus expert g. The Chinese consensus for surgical treatment of traumatic rib fractures 2021 (C-STTRF 2021). Chin J Traumatol. 2021;24(6):311–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sermonesi G, Bertelli R, Pieracci FM, Balogh ZJ, Coimbra R, Galante JM, et al. Surgical stabilization of rib fractures (SSRF): the WSES and CWIS position paper. World J Emerg Surg. 2024;19(1):33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hylands M, Gomez D, Tillmann B, Haas B, Nathens A. Surgical stabilization of rib fractures for flail chest: analysis of center-based variability in practice and outcomes. J Trauma Acute Care Surg. 2024;96(6):882–92. [DOI] [PubMed] [Google Scholar]
- 13.Fitzpatrick DC, Denard PJ, Phelan D, Long WB, Madey SM, Bottlang M. Operative stabilization of flail chest injuries: review of literature and fixation options. Eur J Trauma Emerg Surg. 2010;36(5):427–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Taylor BC, French BG, Fowler TT. Surgical approaches for rib fracture fixation. J Orthop Trauma. 2013;27(7):e168–73. [DOI] [PubMed] [Google Scholar]
- 15.Langenbach A, Oppel P, Grupp S, Krinner S, Pachowsky M, Buder T, et al. Reduced invasive and muscle-sparing operative approaches to the posterolateral chest wall provide an excellent accessibility for the operative stabilization! Minimized approaches to the posterolateral chest wall. Eur J Trauma Emerg Surg. 2018;44(3):471–81. [DOI] [PubMed] [Google Scholar]
- 16.Pieracci FM, Rodil M, Stovall RT, Johnson JL, Biffl WL, Mauffrey C, et al. Surgical stabilization of severe rib fractures. J Trauma Acute Care Surg. 2015;78(4):883–7. [DOI] [PubMed] [Google Scholar]
- 17.Sarani B, Schulte L, Diaz JJ. Pitfalls associated with open reduction and internal fixation of fractured ribs. Injury. 2015;46(12):2335–40. [DOI] [PubMed] [Google Scholar]
- 18.Bemelman M, van Baal M, Yuan JZ, Leenen L. The role of minimally invasive plate osteosynthesis in Rib fixation: a review. Korean J Thorac Cardiovasc Surg. 2016;49(1):1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Schulz-Drost S, Grupp S, Pachowsky M, Oppel P, Krinner S, Mauerer A, et al. Stabilization of flail chest injuries: minimized approach techniques to treat the core of instability. Eur J Trauma Emerg Surg. 2017;43(2):169–78. [DOI] [PubMed] [Google Scholar]
- 20.Greiffenstein P, Tran MQ, Campeau L. Three common exposures of the chest wall for rib fixation: anatomical considerations. J Thorac Dis. 2019;11(Suppl 8):S1034–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Zhang D, Zhou X, Yang Y, Xie Z, Chen M, Liang Z, et al. Minimally invasive surgery rib fracture fixation based on location and anatomical landmarks. Eur J Trauma Emerg Surg. 2022;48(5):3613–22. [DOI] [PubMed] [Google Scholar]
- 22.Bottlang M, Helzel I, Long WB, Madey S. Anatomically contoured plates for fixation of rib fractures. J Trauma. 2010;68(3):611–5. [DOI] [PubMed] [Google Scholar]
- 23.Marasco S, Liew S, Edwards E, Varma D, Summerhayes R. Analysis of bone healing in flail chest injury: do we need to fix both fractures per rib? J Trauma Acute Care Surg. 2014;77(3):452–8. [DOI] [PubMed] [Google Scholar]
- 24.Nickerson TP, Thiels CA, Kim BD, Zielinski MD, Jenkins DH, Schiller HJ. Outcomes of complete Versus partial Surgical stabilization of flail chest. World J Surg. 2016;40(1):236–41. [DOI] [PubMed] [Google Scholar]
- 25.Marasco S, Saxena P. Surgical rib fixation - technical aspects. Injury. 2015;46(5):929–32. [DOI] [PubMed] [Google Scholar]
- 26.Hasenboehler EA, Bernard AC, Bottiggi AJ, Moghadamian ES, Wright RD, Chang PK, et al. Treatment of traumatic flail chest with muscular sparing open reduction and internal fixation: description of a surgical technique. J Trauma. 2011;71(2):494–501. [DOI] [PubMed] [Google Scholar]
- 27.Liu YF, Chen TL, Tseng CH, Wang JY, Wang WC. Impact of obesity on outcomes after surgical stabilization of multiple rib fractures: evidence from the US nationwide inpatient sample. PLoS ONE. 2024;19(2):e0299256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Helm EJ, Rahman NM, Talakoub O, Fox DL, Gleeson FV. Course and variation of the intercostal artery by CT scan. Chest. 2013;143(3):634–9. [DOI] [PubMed] [Google Scholar]
- 29.Kuzma AL, Luo TD, De Gregorio M, Coon GD, Danelson K, Halvorson JJ, et al. Biomechanical Evaluation of Interfragmentary Compression of lag Screw Versus positional screw at different angles of fixation. J Orthop Trauma. 2019;33(5):e183–9. [DOI] [PubMed] [Google Scholar]
- 30.Warner S, Sommer C, Zderic I, Woodburn W, Castle R, Penman J, et al. Lateral rim variable angle locked plating versus tension band wiring of simple and complex patella fractures: a biomechanical study. Arch Orthop Trauma Surg. 2024;144(5):2131–40. [DOI] [PubMed] [Google Scholar]
- 31.Reference AS. https://surgeryreference.aofoundation.org
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary Material 1: Additional file 1: a detailed video of the Ultra Minimally Invasive Surgical Stabilization of Rib Fractures(uMI-SSRF).
Data Availability Statement
No datasets were generated or analysed during the current study.