Abstract
Introduction Hand amputation at the wrist level is severely disabling, especially when bilateral. It is paramount to restore the hand function to the best possible level for the patient's daily living activities, as well as optimal social and occupational rehabilitation. There are various options for restoration of function after amputation at wrist and distal forearm levels including Krukenberg's operation, variations of toe transfers, hand allotransplantation, and prosthesis. Krukenberg's procedure and the reconstruction using toe transfer like Vilkki's procedure or two-toe transfers, restore only the pinch. Hand allotransplantation, although it gives excellent function, has limitations due to the complications of immunosuppression. Functional hand prosthesis, though superior in cosmetic appearance, have again limitations in function, and the cost is prohibitive for most patients in our country.
Materials and Methods We present the unique case of a bilateral hand amputation at the wrist level reconstructed with three toes and free anterolateral thigh (ALT) flap in a single-stage surgery for each hand. In two stages, the patient had six toes transferred to both hands.
Result All transferred toes and all three free (two ALT and one thoracodorsal artery perforator) flaps survived completely. Three-finger grip (tripod pinch) was thus restored in each hand. The hook grip was also restored well by the reconstructed two fingers. Within 3 months after surgery, the patient could perform all activities of daily living. He resumed his original job with some modification of his work within 6 months postinjury.
Conclusion Hand reconstruction using three toes and a free flap is an excellent option for functional restoration for amputation at the wrist and distal forearm level. It allows an early return to function and good social and professional integration of the patient. This procedure is a potential alternative to expensive prosthesis and allotransplantation for a bilateral hand amputation.
Keywords: toe transfer, great toe, combined second and third toe, bilateral amputation, ALT flap, TDAP flap
Introduction
Amputation of the thumb and fingers at various levels leads to degrees of mutilation and significant loss of function. The mutilating hand injuries and guidelines for their reconstructive options are classified by del Piñal and Wei et al. 1 2 Different sets of toe transfers have been described in the literature for the restoration of amputated thumb and fingers done in multiple stages with prior skin cover of the stump. 1 For reconstruction of the bilateral metacarpal hand, Wei et al have advised transferring three toes to the dominant hand and two toes to the nondominant hand as a multistaged procedure. 2 Pisarek was the first to transfer six toes in three stages in a patient with bilateral metacarpal hand due to frostbite. 3 Jones et al have described the reconstruction of bilateral metacarpal hands in a child with postburn deformity, using six-toe transfers in four stages of surgery, three for each hand with a good functional result. 4
While reconstructing a metacarpal hand by toe transfer can give an excellent result, the same does not hold true if the amputation is at the wrist level. 5 Functional restoration for a patient with amputation at the wrist level can be achieved by reconstruction or by prosthesis. 6 7 The reconstructive options described for unilateral amputation at the wrist level are hand transplantation, 8 9 Krukenberg's operation, 10 11 or various sets of toe transfers as described by Vilkki and Kotkansalo 12 or by del Piñal. 1
We present the unique case of a bilateral hand amputation at the wrist level reconstructed with three toes and a free flap in one stage for each hand at a time. We intended to give three-finger grip for each hand for better functional results.
Materials and Methods
A 28-year-old male presented with bilateral hand crush injury while working in a factory. The right hand was completely amputated at the wrist level, whereas the left hand was hanging on the limb with small skin tags at the wrist level. Distal parts of the hand were crushed to the extent that salvage or replantation was not feasible. Amputation in both hands was at the transcarpal level with intact proximal row of carpal bones ( Fig. 1 ).
Fig. 1.
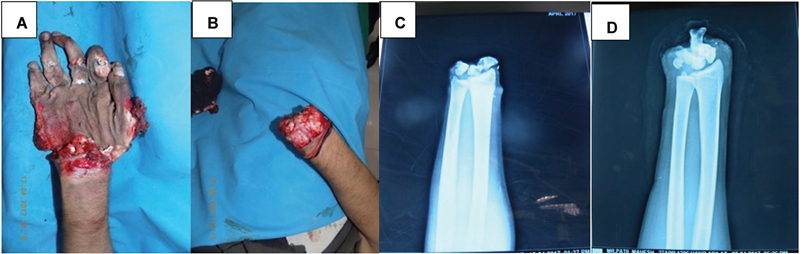
Bilateral hand crush injury at presentation and preop X-rays. ( A ) Right hand, ( B ) left hand, ( C ) right hand, and ( D ) left hand.
Various options for reconstruction of both hands, including fitting of prostheses were discussed with the patient and his relatives. Prosthesis fitting was considered functionally and financially nonviable. Allotransplantation in the acute setting was out of consideration. To rehabilitate him early, we planned the reconstruction of both hands in two stages, that is, one hand at a time with an interval of 1 week.
The aim of reconstruction was to give pinch on the right hand and wide grasp on the left hand so that both hands complement each other for better function. The right hand was reconstructed using the ipsilateral three toes and contralateral anterolateral thigh skin flap, in the following manner:
Fig. 2.

Right hand reconstruction. ( A ) Amputation stump. ( B ) Incisions for toes harvest. ( C ) Plantar incision. ( D ) Harvested right great toe and combined 2nd and 3rd toes. ( E ) Resultant defect after toe transfers. ( F ) Harvested anterolateral thigh (ALT) skin flap. ( G ) On table postop result.
Table 1. Surgical plan and technical details.
| Surgical plan for reconstruction of right and left hand | |||||
|---|---|---|---|---|---|
| Arterial anastomosis | Venous anastomoses | Nerve reconstruction | Flexor tendon reconstruction | Extensor tendon reconstruction | |
| Thumb reconstruction using great toe | Dorsalis pedis artery to radial artery | Dorsalis pedis Vena-comitans and medial arch vein to cephalic vein and radial artery Vena-comitantes | Plantar digital nerves to median nerve | FHL to FPL | EHL to EDL of index finger |
| Fingers reconstruction using combined 2nd and 3rd toes | Plantar common digital artery to ulnar artery | Dorsal vein and the lateral arch vein to ulnar artery vena-comitantes | Plantar digital nerves to ulnar nerve | FDL of the toes to FDPs of middle and ring fingers | EDL of the toes to EDL of middle and ring fingers |
| ALT flap cover | Descending branch of lateral circumflex femoral artery to radial artery end to side | Vena-comitantes to cephalic vein and its tributary | – | – | – |
| TDAP for left hand | Thoracodorsal artery to ulnar artery end to side | Vena-comitans to basilic vein | – | – | – |
Abbreviations: ALT, anterolateral thigh; EDL, extensor digitorum longus; EHL, extensor hallucis longus; FDL, flexor digitorum longus; FDP, flexor digitorum profundus; FHL, flexor hallucis longus; FPL, flexor pollicis longus; TDAP, thoracodorsal artery perforator.
Surgical plan and technical details:
The thumb was reconstructed by using the great toe distal to the level of the metatarsophalangeal joint.
Two fingers were reconstructed by the ipsilateral combined 2nd and 3rd toes.
Positioning of the toes: To restore three-finger grip (tripod pinch) in the hand, it is essential that the toe used for the thumb can oppose to those for the fingers. The great toe was positioned in pronated manner by proximal phalanx fixation on the scaphoid to aid motion at the radiocarpal joint. This was intended to increase the range of motion of the transferred toe and achieve some palmar grip rather than the straight pincer grip ( Fig. 3 ). Combined second and third toes were fixed on the triquetrum and distal ulna in a manner that on flexion they would receive the opposing thumb to restore the palmar grip. Bone fixation was achieved by interosseous wires and oblique Kirschner wires (K-wires).
The resultant soft tissue defect in the web space and the circumferential defect over the base of the toes and that on the wrist was covered using the contralateral anterolateral thigh skin flap at the same time.
Fig. 3.

Reconstructed palmar grip like normal palmar grip.
At the end of surgery for 14.5 hours all the three toes and the flap had good circulation and patient withstood the procedure well.
After 1 week when the reconstruction was stable with good circulation, the reconstruction of the left hand was planned as follows ( Fig. 4A–F , Table 1 ).
Fig. 4.

Left hand reconstruction. ( A ) Amputation stump. ( B ) Harvested left great toe and combined 2nd and 3rd toes. ( C ) Primary closure of the foot defect. ( D ) Resultant defect after toe transfers. ( E ) Harvested anterolateral thigh (ALT) skin flap. ( F ) On table postop result. ( G ) Harvested thoracodorsal artery perforator (TDAP) flap. ( H ) TDAP flap inset complete.
An exactly similar plan of transfer was used for the left hand using ipsilateral three toes and the contralateral anterolateral skin flap, except that the bony fixation and tendon balancing which were done to create a wider grasp. It took 11 hours for the reconstruction of the left hand. On the first postop day after left hand reconstruction, transferred combined second and third toes developed loss of arterial blood flow. Immediate reexploration revealed anastomotic thrombosis, which was revised with a vein graft harvested from the dorsum of the foot. As wound closure was not possible over the pedicle due to edema, a small thoracodorsal artery perforator flap, harvested from the right side, was used as cover ( Fig. 4G and H , Table 1 ).
The postoperative period after that was uneventful. Hand therapy and rehabilitation were started after 3 weeks in a graded manner by an experienced physiotherapist. The K-wires were removed after 4 weeks of surgery.
Results
Video 1 Drinking water.
Video 2 Eating with spoon.
Video 3 Combing hair.
Video 4 Using mobile phone.
Video 5 Walking.
Video 6 Cycling.
Video 7 Writing.
All the transfers were successful and the patient was discharged within 3 weeks of admission after all the wounds had healed ( Fig. 5 ).
Fig. 5.
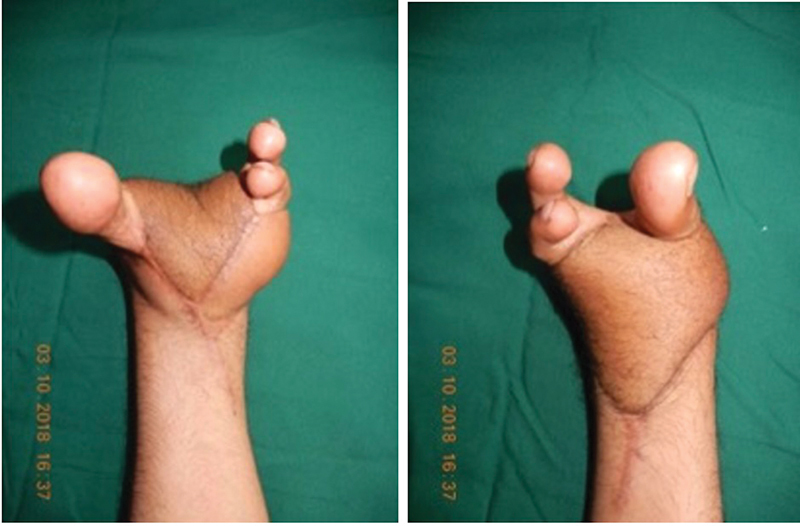
Late postop results of bilateral hand reconstruction.
The patient did not have any limitation in walking or in his daily activities, though the donor site deformity of the feet was unaesthetic ( Fig. 6 ).
Fig. 6.

Donor site deformity of the feet.
The patient was followed up every week initially for the first 2 months and then every month for next 1 year. After a period of 1 year the progress in the function plateaued. 13 At the end of 1 year hand function was evaluated using the Tamai score for activities of daily living 14 ( Fig. 7 , Videos 1 2 3 4 5 6 7 ).
Fig. 7.
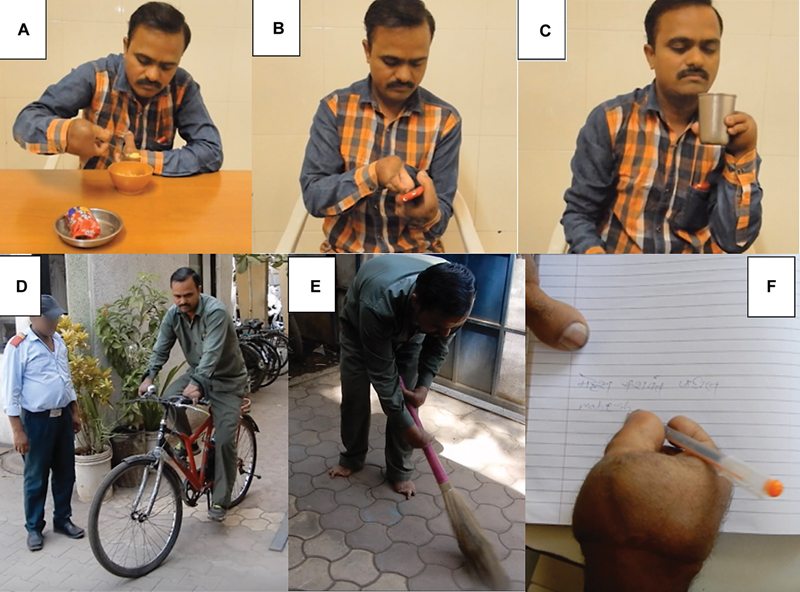
Postop function with different activities.
Discussion
Bilateral hand amputation at the wrist level is a great challenge for reconstruction, as there is complete loss of all the functional components of the hand. The following options have been suggested in the literature for the restoration of hand function in such patients:
Krukenberg's operation
Vilkki's procedure of toe to antebrachial stump transplantation
Hand prosthesis
Hand allotransplantation
Various sets of toe transfers
Krukenberg's procedure was described in the literature in 1930 for amputation at the wrist and distal forearm level leading to optimum restoration of grip function. 15 16
Vilkki's procedure to restore pinch function by transferring the second toe onto the radial aspect of the distal forearm using muscle tendon units in the forearm was designed by the author in 1981, first performed in 1983.The long-term results were published in 2007 showing good function. 12 None of these procedures achieved tripod pinch which is recommended since it offers lateral stability in key pinch, provides stronger hook grip, and a wider grasp compared to a single-digit reconstruction. 17 Despite advances in upper extremity prosthetics, sensate hand reconstructions or transferred toes have better functional outcomes unmatched by the prosthetic hand. 18
The worthiness of hand allotransplantation is still being debated due to the costs involved, the risk of rejection, and the need for lifelong immunosuppression with its possible risks to the patient. 19 20 Therefore, though hand transplantation is a clinical reality, it has not yet become the “standard of care” for bilateral amputees in the acute setting. 8
Pisarek was the first to transfer six toes for reconstruction of bilateral metacarpal hand in three surgeries using three toes on each side. 3 Later, Tan et al suggested using three toes on the dominant hand and two toes for the other hand for reconstruction of bilateral metacarpal hands. 21 Similar combinations of toe transfers for reconstruction after amputation at the wrist level can be classified as follows:
Two-toe transfers: one for thumb and other for finger
Three-toe transfer: one for thumb and double toe for fingers
For the unilateral amputation at the wrist level, a two-toe transfer to achieve pinch can achieve optimum function as the opposite hand is normal. In case of the bilateral hand amputation at the wrist level, there is increased demand on the reconstruction wherein reconstructing a three-finger pinch/grasp achieves better function. 12 20
The fixation of the toes in flexed position over the wrist to achieve palmar grip simulates the palmar grip by thumb and fingers in the normal hand. It has definite advantage in function over the straight positioning of the toes in line with the forearm which gives only the straight pincer pinch.
On functional evaluation, the shortcomings of the reconstruction at the wrist level are evident like the short length of the reconstructed thumbs and fingers, moderately poor cosmetic appearance, and lack of power grasp and strength. Because of these, total Tamai score for activities of daily living was 8 out of 20. Though the score seems poor, the patient is completely independent for activities of daily living. He has also retained his job in the same company with some modification and earns for his family.
Conclusion
The evidence in this case demonstrates that three toes transfer and free flap cover in one stage surgery as a viable option for the restoration of function in hand amputation at the wrist level. This kind of reconstruction is not for the faint hearted. It should be attempted only by microsurgeons or centers which have a long experience in complex microsurgical reconstructions. It involves technically demanding intense surgery, long surgical time, a setup geared for close monitoring, and emergency reexplorations to salvage a failing flap or toe. However, it involves much less cost than allotransplantation, no chances of rejection, and no immunosuppression and complications related to it. Wei et al has clearly explained the superiority of the hand reconstruction over the bilateral hand transplantation in select situations and need for hybrid approach for better functional restoration. 20
Considering all these factors, we are of the opinion that three toes transfer and a flap cover is the best treatment option for patients with bilateral amputation at the wrist level.
Footnotes
Conflict of Interest None declared.
References
- 1.del Piñal F. Severe mutilating injuries to the hand: guidelines for organizing the chaos. J Plast Reconstr Aesthet Surg. 2007;60(07):816–827. doi: 10.1016/j.bjps.2007.02.019. [DOI] [PubMed] [Google Scholar]
- 2.Wei F C, Coessens B, Ganos D. Multiple microsurgical toe-to-hand transfer in the reconstruction of the severely mutilated hand. A series of fifty-nine cases. Ann Chir Main Memb Super. 1992;11(03):177–187. doi: 10.1016/s0753-9053(05)80367-9. [DOI] [PubMed] [Google Scholar]
- 3.Pisarek W. Transfer of the third, fourth and fifth toes for one-stage reconstruction of the thumb and two fingers. Br J Plast Surg. 1990;43(02):244–246. doi: 10.1016/0007-1226(90)90170-5. [DOI] [PubMed] [Google Scholar]
- 4.Jones N F, Graham D, Au K. Bilateral metacarpal hands: reconstruction with 6 toe transfers. Hand (N Y) 2020;15(04):465–471. doi: 10.1177/1558944718810844. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Zelken J, Lin C H. Evolution from toe-to-hand transfer to hand transplantation. Transl Res Biomed. 2016;5:45–54. [Google Scholar]
- 6.Ovadia S A, Askari M. Upper extremity amputations and prosthetics. Semin Plast Surg. 2015;29(01):55–61. doi: 10.1055/s-0035-1544171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Geethanjali P. Myoelectric control of prosthetic hands: state-of-the-art review. Med Devices (Auckl) 2016;9:247–255. doi: 10.2147/MDER.S91102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Brandacher G, Gorantla V S, Lee W PA. Hand allotransplantation. Semin Plast Surg. 2010;24(01):11–17. doi: 10.1055/s-0030-1253243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Alolabi N, Augustine H, Thoma A. Hand transplantation: current challenges and future prospects. Transpl Res Risk Manag. 2017;9:23–29. [Google Scholar]
- 10.Jha R, KC B R, Chand P. The Krukenberg procedure: a surgical option for the treatment of bilateral hand amputees. Med J Shree Birendra Hosp. 2006;8:48–50. [Google Scholar]
- 11.Williamson J S, Manktelow R T, Kelly L, Marcuzzi A, Mahabir R C. Toe-to-finger transfer for post-traumatic reconstruction of the fingerless hand. Can J Surg. 2001;44(04):275–283. [PMC free article] [PubMed] [Google Scholar]
- 12.Vilkki S K, Kotkansalo T. Present technique and long-term results of toe-to-antebrachial stump transplantation. J Plast Reconstr Aesthet Surg. 2007;60(07):835–848. doi: 10.1016/j.bjps.2007.02.018. [DOI] [PubMed] [Google Scholar]
- 13.Sabapathy S R, Venkatramani H, Bhardwaj P. Reconstruction of the thumb amputation at the carpometacarpal joint level by groin flap and second toe transfer. Injury. 2013;44(03):370–375. doi: 10.1016/j.injury.2013.01.012. [DOI] [PubMed] [Google Scholar]
- 14.Fleming J, Africa Marcus Castro Ferreira S, Frederick Finseth Bet al. Report of Subcommittee on Replantation 1983Accessed July 29, 2019 at:https://www.jhandsurg.org/article/S0363-5023(83)80257-3/pdf
- 15.Sinaki M, Dobyns J H, Kinnunen J M. Krukenberg's kineplasty and rehabilitation in a blind, bilateral full-hand amputee. Clin Orthop Relat Res. 1982;(169):163–166. [PubMed] [Google Scholar]
- 16.Yu Z J, Huang Y C, Yu S, Sui S P. Thumb reconstruction in a bilateral upper extremity amputee: an alternative to the Krukenburg procedure. J Hand Surg Am. 1999;24(01):194–197. doi: 10.1053/jhsu.1999.jhsu24a0194. [DOI] [PubMed] [Google Scholar]
- 17.Kotkansalo T.Post-traumatic grip reconstruction with toe transfers 2014. Accessed June 25, 2025 at:https://trepo.tuni.fi/bitstream/10024/96131/1/978-951-44-9572-4.pdf
- 18.Zlotolow D A, Kozin S H. Advances in upper extremity prosthetics. Hand Clin. 2012;28(04):587–593. doi: 10.1016/j.hcl.2012.08.014. [DOI] [PubMed] [Google Scholar]
- 19.Dubernard J M, Owen E, Herzberg G et al. Human hand allograft: report on first 6 months. Lancet. 1999;353(9161):1315–1320. doi: 10.1016/S0140-6736(99)02062-0. [DOI] [PubMed] [Google Scholar]
- 20.Wei F C, Al Deek N F. the battle ground between two giants: toe transfer and hand allotransplantation. J Reconstr Microsurg. 2018;34(09):678–680. doi: 10.1055/s-0038-1639513. [DOI] [PubMed] [Google Scholar]
- 21.Tan B K, Wei F C, Lutz B S, Lin C H.Strategies in multiple toe transplantation for bilateral type II metacarpal hand reconstruction Hand Clin 199915607–612., viii [PubMed] [Google Scholar]


