Abstract
Background
The community-based social healing (CBSH) model, developed by Ubuntu Centre for Peace, aims to support individuals with traumatic experiences and mental health challenges in achieving better mental health. CBSH combines BREATH-BODY-MIND™ (BBM) practices with collective narrative and rituals, facilitated by Community Healing Assistants in therapeutic groups. A previous pilot study involving 1889 Rwandan CBSH participants showed significant mental health improvements, including reductions in depression, anxiety, and PTSD, along with enhanced work productivity, and decreased intimate partner violence. The trial investigates the CBSH model’s impact on Ubuntu and mental health. Ubuntu, a concept that encompasses humanness, compassion, and interconnectedness, is deeply rooted in the African philosophy.
Methods/design
This cluster randomized controlled trial will involve 54 villages randomly selected in the Kirehe district, with 1080 participants randomly allocated equally to the CBSH intervention or a wait-list control group. While the trial will be conducted at the village (cluster) level, both primary and secondary outcomes will be measured individually for participants within each cluster. The Primary outcome “Ubuntu” will be measured using a context-adapted Ubuntu measurement scale. Secondary outcomes include psychosocial indicators which will be assessed through standardized tools such as the Patient Health Questionnaire for depression (PHQ-9), Generalized Anxiety Disorder-7 (GAD-7), Posttraumatic Stress Disorder Checklist for DSM-5 (PCL-5), Warwick-Edinburgh Mental Wellbeing scale (WEMWS), Connor-Davidson Resilience scale (CD-RISK-10), Somatic Symptom Severity Scale (PHQ-15), Revised Conflict Tactics scale (CTS2S), and Adapted Social Capital Assessment Tool (SASCAT).
Conclusion
This trial aims to evaluate the CBSH model’s impacts on Ubuntu, mental health, and social functioning among trauma-affected Rwandans, including those impacted by the 1994 Genocide against the Tutsi, mass killings, sexual abuse, and domestic violence. The findings could be of value to the Ubuntu Centre for Peace, policymakers, healthcare practitioners, and other stakeholders, by highlighting the significance of promoting Ubuntu as a foundation for addressing mental health challenges and the consequences of psychosocial trauma.
Trial registration
ISRCTN ISRCTN17659369. Registered on February 09, 2024.
Supplementary Information
The online version contains supplementary material available at 10.1186/s13063-024-08632-6.
Keywords: Community-based, Social healing, Post-traumatic stress, Ubuntu, Mental health, Mind–body, Breath-based, Africa, Genocide
Introduction
Mental health, a key aspect of human well-being, influences thoughts, emotions, and the ability to deal with life’s challenges. Globally, 1 in 8 people is affected by mental illnesses, with depression and anxiety disorders being the most common [1]. Factors such as poverty, conflict, economic insecurity, political wars, urbanization, and climate change contribute to both physical and mental ill-health [2]. Between 2000 and 2015, Africa observed a 52% increase in years lost to disability due to mental and substance use disorders [3]. Tragically, mental healthcare services delivery and utilization are scarce across the African continent. The region has approximately 99% fewer mental health consultations and 85% fewer mental healthcare workers than the global average [3]. In Africa, mental health care is hindered by a lack of government funding, a scarcity of professionally trained providers, and stigmatization linked to traditional beliefs.
Thirty years have passed since Rwanda endured the atrocities of the 1994 Genocide against the Tutsis, which have damaged the social structure leaving behind psychosocial problems such as chronic fear and mistrust, social isolation and discrimination, guilt, collective angst, victimhood, and shame [4]. Genocide survivors experience more than double the rates of mental health disorders compared to the general population, with significantly higher prevalence rates of depressive disorders (35% vs 12%) and posttraumatic stress disorder (PTSD) (27.9% vs 3.6%) [5]. Additionally, ex-prisoner genocide perpetrators face social and family rejection, loss of social and professional identity due to long periods of incarceration, emotional suppression, and feelings of hopelessness [4]. Although 62% of the population are aware of available mental healthcare services, only 5.3% utilize them [5]. This low level of mental healthcare-seeking behavior results from numerous barriers including lack of awareness, financial constraints, geographic inaccessibility, and cultural stigma [6].
Western paradigms of mental health treatment focus primarily on the individual’s traumas, often overlooking communal, socio-cultural, and historical factors [7, 8]. In contrast, the socio-ecological model of mental health addresses six levels of influence on human behavior: individual, relationships, organizations, communities, policy, and society [9]. This model aligns with the World Health Organization’s definition of mental health, which emphasizes not only the absence of mental illness but also the person’s capacity to manage stress, reach their full potential, and maintain emotional and social well-being, resilience, and the ability to work effectively, thereby contributing to their community [10]. The socio-ecologic model is consistent with the Pan-African philosophy of Ubuntu, which underscores the authenticity of an individual as inherently connected to a larger relational, communal, societal, environmental, and spiritual network [11].
Ubuntu is a fundamental moral and relational ethic in African culture that promotes right actions, values fellowship, reconciliation, friendliness, harmony, reciprocity, mutual caring, and dignity, all in service of communality and justice [12]. The Ubuntu way of living improves mental health by fostering social support, nurturing environments, and peaceful coexistence [13]. The quality of social relationships and support, which increases resilience to stress, has been shown to significantly reduce symptoms of depression and decrease the likelihood of developing PTSD [14, 15]. Additional factors contributing to mental healing within social cooperation include empathy, emotional contagion, emotion regulation, compassion, and consoling behavior [16–18]. The African philosophy of Ubuntu, a culturally sensitive approach to the emotional and relational dimensions of healing, could help bridge the mental healthcare gap in Rwanda and Africa, where current systems are often limited to Western approaches.
Community-based social healing (CBSH) model is a holistic intervention developed by the Ubuntu Centre for Peace to promote psychosocial healing and support individuals experiencing mental health conditions resulting from traumatic events including genocide, mass killings, sexual abuse, domestic abuse, and other forms of violence. The CBSH combines Breath-Body-Mind practices with collective narrative and rituals, facilitated by Community Healing Assistants within therapeutic groups. A pre and post-evaluation of the CBSH pilot project, conducted from July 1, 2020, to June 30, 2021, for 1889 participants, revealed significant reductions in rates of depression, anxiety, and PTSD. The intervention also led to improvements in work productivity and reductions in intimate partner violence [19]. CBSH addresses trauma, mental health conditions, and relationships within families and communities [19].
Breath-body-mind (BBM) practices help restore autonomic balance, improve emotion regulation, and alleviate trauma-related symptoms through various mechanisms, as described by Drs. Gerbarg and Brown [16, 17, 20, 21]. These mechanisms likely include the use of voluntary, regulated breathing techniques that activate parasympathetic pathways, decrease the sympathetic nervous system overactivity, promote the release of inhibitory neurotransmitter gamma-aminobutyric acid (GABA), inhibit excessive activity in the amygdala (responsible for emotion processing), and enhance activity in the brain’s higher centers, which mediate safety assessment, executive functions, decision-making, and interoceptions (perceptions of internal bodily states) [16]. Evidence suggests that BBM practices increase awareness of feelings, emotions, and thoughts by focusing attention and stimulating the brain’s interoceptive pathways [20]. Additionally, they may stimulate pro-social neurophysiological processes, increasing empathy, love, and social engagement. The overall effect is a positive shift in the psycho-neurophysiological state from one of defensive fear, anger, isolation, and mistrust to a state characterized by feelings of safety, calmness, connectedness, flexibility, cooperation, and compassion [16, 17, 21].
Breath-Body-Mind was selected for the CBSH model due to its demonstrated benefits for anxiety, depression, and PTSD in previous studies and fieldwork, including in South Sudan, Uganda, and Rwanda [22, 23]. It has shown positive effects even among individuals with extreme trauma [22, 23].
The CBSH model also incorporates local rituals, such as singing, dancing, and drumming, to create a safe space for authentic storytelling and attentive listening [24]. Sharing personal narratives in a secure group setting allows participants to reinterpret their life stories, restoring their sense of belonging, self-worth, purpose, and hope [25]. The stories shared by therapeutic group members influence and inspire one another, challenging unhealthy perspectives and perceptions, and facilitating transformation into healthier ones.
The CBSH model aligns with Ubuntu African philosophy, which fosters individual wellbeing within a collective environment, supportive relationships, personal and societal healing, and economic growth. Nevertheless, the relationship between the improvements in Ubuntu and mental health, along with other positive outcomes associated with the CBSH model have not yet been evaluated. Additionally, there is currently no validated and reliable Ubuntu measurement tool that reflects the nuances of Rwandan culture and language. Consequently, this study aims to culturally adapt and validate a psychometrically validated and reliable scale for measuring Ubuntu. This study investigates the effects of CBHS on Ubuntu, mental health (depression, anxiety, PTSD, mental wellbeing, resilience, and psychosomatic symptoms), and psychosocial outcomes (intimate partner violence and social capital) in post-genocide Rwanda.
Study objectives
To culturally adapt, translate, and rigorously test the reliability and validity of an existing Ubuntu scale in the Rwandan context.
To assess the impact of the community-based social healing (CBSH) model on Ubuntu in Rwandan participants.
To evaluate the effects of the CBSH model on mental health outcomes, including depression, anxiety, post-traumatic stress, mental well-being, resilience, and psychosomatic symptoms among Rwandan participants.
To investigate the CBSH model’s impact on psychosocial functioning, focusing on outcomes such as intimate partner violence and social capital within the Rwandan community context.
To explore the extent to which Ubuntu mediates the effects of the CBSH on mental health and psychosocial functioning, determining how changes in Ubuntu influence improvements in these areas for Rwandan participants.
Study hypotheses
Participation in the CBSH model will be associated with significant improvements in Ubuntu compared to a control group receiving no intervention.
CBSH participation will be associated with significant improvements in mental health, demonstrated by reductions in depression, anxiety, post-traumatic stress, and psychosomatic symptoms, along with improvements in mental wellbeing and resilience, compared to a control group receiving no intervention.
CBSH participation will be associated with significant improvements in psychosocial functioning, characterized by reduced intimate partner violence and increased social capital, compared to a control group receiving no intervention.
Improvements in Ubuntu will correlate positively with improvements in mental health and psychosocial functioning.
Trial design
For this cluster randomized controlled trial, participants will be recruited from randomly selected villages, which will be randomly assigned to either the intervention group (receiving the CBSH intervention) or the wait-list control group (awaiting the intervention). Randomization will be conducted using Microsoft Excel to allocate village clusters to either the intervention or control group. No placebo or alternative active treatment will be provided to the control group; however, participants in both groups will have access to treatment as usual through their primary healthcare providers. This trial design and report follows the Standard Protocol Items: Recommendations for Interventional Trials (SPIRIT) 2013 statement [26].
Methods
Study setting
This trial will be conducted from December 2023 to January 2025 in 54 randomly selected villages in the Kirehe district, Eastern Province, Rwanda. Kirehe district has high rates of mental health conditions (22.1%) and suicidality [27, 28]. Moreover, there are no Non-Governmental Organizations, community-based social healing, or mental health organizations working in that region.
Selection of eligible study villages
For this study, 54 villages will be randomly selected from the 612 villages in Kirehe district, as listed by the Ubuntu Center for Peace. The village list will be stored in an Excel file containing four columns: A (District), B (Sector), C (cell), and D (Village), organized alphabetically. Using Microsoft Excel, the external research team from the University of Rwanda will generate a column of randomized values for each village, Column E, using the command = Rand(), and then paste these values into a new column to fix them. The fixed random values will be ranked from highest to lowest and the 54 top-ranked villages will be chosen for the study.
To prevent spillover or crossover effects, we will ensure that the selected villages are at least 1 km apart. The Ubuntu Centre for Peace will review village proximities; If two selected villages are too close, the lower-ranked one will be replaced by the next eligible village on the ranked list.
Community Healing Assistant (CHA) selection and participant recruitment
The recruitment of trial participants was conducted by Community Healing Assistants (CHAs), who will be community members selected from the 54 villages included in the study. CHAs will be organized in pairs, with each pair responsible for two villages: one being their own and the other an additional paired village. In total, 27 pairs of CHAs will be selected from 27 villages, which will be randomly chosen from the 54 villages in the study.
Participants will be recruited by Community Healing Assistants (CHAs) in close collaboration with local village leaders. This partnership will enable CHAs to leverage local knowledge and identify individuals who are most in need of psychosocial support. Local leaders recommended participants based on observed signs of distress and who are in need of an intervention such as the CBSH program. The selection was guided by variables related to the study’s aims, specifically targeting genocide survivors, ex-prisoner genocide perpetrators, individuals experiencing family conflicts or intimate partner violence, single mothers, and those facing extreme poverty. These criteria are consistent with the study’s objectives, focusing on mental health and psychosocial outcomes, such as depression, anxiety, PTSD, resilience, and social capital.
After receiving recommendations, CHAs will visit potential participants at their homes to explain the program and invite them to join. CHAs will be trained to follow the intervention selection criteria, providing accurate information to each participant. Each CHA pair will recruit a total of 20 participants per village. Ultimately, all CHAs will enroll a total of 1080 participants across the 54 villages. This approach will allow for a targeted and community-informed recruitment process, closely aligned with the study’s intended measures.
Participants’ eligibility criteria
Inclusion criteria for intervention and control groups
Individuals aged 18 years and older.
Residing in the Kirehe district during the study period.
Individuals identified by village leaders and/or CHAs as having mental health or psychosocial difficulties, including signs or symptoms of being depressed, suicidal, withdrawn, fearful, mistrustful, overly reactive, aggressive, violent, combative, abusive (to partner, children, or others); unable to work reliably; misuse or abuse of substances; recurring psychosomatic symptoms, for example, sleep problems, chronic headaches, or chronic backaches.
Exclusion criteria for intervention and control groups
Individuals unable to communicate due to hearing and/or speech disability without an available translator.
Individuals who are mentally or intellectually incapacitated to the extent that they cannot comprehend or respond to questions.
Previous participation in the CBSH intervention or a similar program.
Ethical considerations
This trial has received ethical approval from the Institutional Review Board of the College of Medicine and Health Sciences at the University of Rwanda (No 111/CMHS IRB/2024). The trial has been registered with ISRCTN (ID: ISRCTN1765936, registered on February 09, 2024). Informed consent will be obtained by trained data collectors, all of whom are clinical psychologists. These data collectors will provide participants with comprehensive information about the study, including its objectives, and the voluntary nature of their participation. Candidates will be assured that they have the right to withdraw from the study at any point without any repercussions.
Participants assigned to the wait-list control group will have the opportunity to engage in the intervention after the final round of data collection.
To maintain confidentiality, each participant will be assigned a unique identification code, which will be used on all test measure documents. The participants’ names will not appear on any data sheets or test measures; only the Principal Investigator will have access to the master list linking names to identification codes. All data collected will be anonymized and securely stored on a password-protected computer, accessible only to the research team, thereby safeguarding participants’ confidentiality. The Ethical Committee has full rights to oversee the study, including the power to review and monitor trial conduct and confidentiality procedures.
Randomization
Village allocation to intervention and control
The randomization and allocation process will be managed by an external research team from the University of Rwanda to ensure objectivity and impartiality, with no influence from Community Healing Assistants (CHAs) or village leaders involved in the recruitment phase. The University of Rwanda team (SJ, AN, JN), will be solely responsible for generating the allocation sequence and assigning villages to either the intervention or control group, using a structured approach in Microsoft Excel. Each pair of CHAs will be assigned two villages: their own village and an additional paired village. For each pair, a random value will be generated using the = Rand () function, which produces values between 0 and 1.
To determine allocation, the random value will be adjusted by subtracting 0.5. If the result is positive, indicating a random value above 0.5, the CHA’s own village will be allocated to the intervention group and the paired village will be assigned to the control group. Conversely, if the result is negative, indicating a random value of 0.5 or below, the CHA’s paired village will be allocated to the intervention group, and their own village to the control group. This approach provides an equal probability of assignment for each village, balancing the allocation across intervention and control groups. The process will continue until all 54 villages are assigned, resulting in 27 villages in each group. By involving the University of Rwanda’s external research team, the study will uphold methodological rigor and minimize potential bias.
The intervention
Explanation of the comparators
Trial participants in the intervention group receive CBSH, while those in the control group are on a waiting list. This is done to compare the impact of CBSH on Ubuntu and the secondary outcomes with a non-intervention wait-list control. In compliance with ethical standards, the participants assigned to the waiting list (control group) will be given the opportunity to participate in the CBSH after the final evaluation of the trial. While waiting to participate in the CBSH, both the intervention group and the control group will have access to their usual care through their existing primary healthcare services (care as usual).
Intervention description
The community-based social healing (CBSH) model is a scalable, culturally sensitive, non-stigmatizing, accessible, cost-effective community mental health approach. This model is being implemented by the Ubuntu Center for Peace, a Non-profit Organization that strives to bring people living with the consequences of traumatic experiences and common mental health conditions to a more flourishing life.
The CBSH model includes a manualized program of BREATH-BODY-MIND™ (BBM) practices, sharing of individual narratives in a safe group setting, and engagement in local social rituals. Group sessions are provided by Community Healing Assistants (CHAs) who are members of the same community as the participants (i.e., village), and who are recruited by the Ubuntu Center for Peace. The CHAs receive a 6-week training that covers breath-body-mind techniques and a theory of emotional anatomy that describes childhood traumatic experiences associated with sacrificing one’s authenticity and adapting to situations to keep connections to the caretaker, and how these traumas and adaptations affect individuals as they grow. They learn about trauma, Post-Traumatic Stress Disorder (PTSD), depression, and anxiety disorders, Sexual and Gender-based Violence (SGBV), non-violent communication, five love languages, JOHARI windows, Tree of Life, evolving from trauma to wholeness, social entrepreneurship, and how to recruit participants affected by trauma and common mental conditions. Additionally, they learn how to collect data and are equipped with smartphones as well as with group facilitation skills. CHAs then facilitate healing practices through therapeutic groups. They are supervised and mentored by professional psychologists.
Each therapeutic group is comprised of 18–20 people who meet once a week for 2–3 h, over a period of 15 weeks. They then transition to long-term support or self-help groups and create additional socio-economic activities including lending circles, solidarity work, and business or farming cooperatives to sustain healing, health, and resilience.
Setting, principles, and processes of the healing practices
Participants sit in the circle at a participant’s home, local church, office, or school and set up principles that they all abide by including confidentiality, equal participation, democracy, mutual respect, and dignity. The setting and principles create a feeling of belonging and connection and a sense of equality. They enable a smooth process in the healing journey as described below.
The session begins with local rituals, dancing, and/or singing followed by group sharing (checking in). Participants talk about what they experienced during the week. The theme for the day is introduced. Next, the group does a breath-body-mind sequence for 40 min followed by a structured group-sharing process related to the theme of the day. The session ends with coherent breathing.
Breath-body-mind sequence
- Activating practices:
- Body tapping or shaking with or without music. No more than 5 min.
- Two forms of Ha breath—arm movements while making a loud “Ha” sound for one or two rounds of 10 breaths performed at 20 breaths per minute (bpm).
- Balancing and calming practices using arm movements synchronized with breathing:
- 4–4–6–2 breath (inhale 4 counts, hold breath 4 counts, exhale 6 counts, hold 2 counts) with synchronized Qigong arm movements.
- Balancing and calming practices using arm movements synchronized with coherent breathing at 5 bpm
- Either 4–4 breath (inhale 4 counts, exhale 4 counts) with arm circles or
- Painting the waterfall with arm movements and visualization.
- Weeks 6 or 7 introduce sky and earth Qigong movements synchronized with coherent breathing (5 bpm).
Open joints (joint mobility exercises) sessions #1, #6, and optionally as needed.
Group sharing process
- Coherent breathing is performed after the group sharing processes:
- Starts with two deep relaxing breaths: slow inhale and long exhale with deep sighing sound
- Top-down muscle relaxation
- Coherent (or resonant) breathing is gentle, natural breathing at 5 bpm, in and out through the nose with equal duration of the inspiratory and expiratory phases. This technique is practiced at the end of the healing session, before participants go home. The length of coherent breath practice starts with 7–8 min and increases gradually up to 20 min.
- Ends with a bottom-up body scan.
Group sharing processes
Week 1–4: Creation of a safe space for the therapeutic groups. CHAs help the healing or therapeutic groups create group safety contracts, for example, all participants agree to maintain the confidentiality of the other participants. They employ methodologies and relevant exercises that help participants become more aware of their fears and identify situations that prevent them from feeling safe and emotionally vulnerable. This phase helps participants create bonds between them in their healing journey.
Week 5–7: Enhancing trust and emotional vulnerability amongst participants through specialized exercises and practices, becoming more aware of and progressively sharing their deep emotional traumas that led to guilt, shame, resentment, fear, denial, and doubt.
Week 8: Introduction of the Tree of Life as a tool to help structure storytelling/ personal narratives and to provide a metaphor for healing. Different parts of the tree symbolize key aspects of our lives: roots symbolize our historical background; the trunk symbolizes our current lives; branches symbolize our families and friends, leaves symbolize how we nourish ourselves—physically, emotionally, mentally, and spiritually; ripe fruits symbolize our accomplishments; green fruits symbolize our hopes and dreams; and thorns symbolize our challenges and barriers to healing and self-actualization.
Week 9–13: Participants tell and retell their stories in smaller groups of 4–6 people each, using the symbolism of the Tree of Life. As they share their personal narratives, they reinterpret the meaning of their traumatic events, feel seen, heard, and acknowledged, listen to one another with empathy, learn from one another, humanize one another, and feel part of a secondary family with a new vision.
Week 14–15: Group participants focus on the future, discussing the transition to a self-help group. They start exploring socio-economic activities that they want to integrate in their healing journey, such as cooperatives, solidarity work, lending circles, and more, to sustain healing, health, and resilience. They are empowered with basic leadership skills to manage their self-help groups effectively.
Graduation ceremony and transition to self-help groups
At the completion of 15 weeks, participants celebrate together, but family members who were not part of the healing program are not invited. They invite government authorities and other dignitaries. During the graduation celebration, they practice BBM and share testimonials. With a candle ceremony, participants make commitments for what they will do through the long-term support group.
Supportive supervision and mentorship
At least once a month, a psychologist supervises the CHAs while they are facilitating healing sessions in their groups. In addition, psychologists provide a 1-day refresher training with feedback from all CHAs, every 4 weeks.
Criteria for discontinuing or modifying allocated interventions
The CBSH has been implemented in different regions in Rwanda and both qualitative and quantitative data were collected with good evidence that this intervention causes no harm. Participants in the intervention can always end their participation by their own free choice. A participant can be removed from a therapeutic group by the group leaders, if he or she does not adhere to the rules and regulations of the group, for example breaching confidentiality. However, for this study, the participation of those assigned to the intervention will only be discontinued if the participant requests to withdraw from the study (as our main analysis is based on the intention-to-treat principle).
Strategies to improve adherence to intervention
During the weeks of intervention, participants are encouraged to adhere to the group sessions by the CHAs. There is a protocol implemented by CHAs with the support of psychologists who supervise them. If a participant does not show up for one session, the CHA contacts the person to find out why they did not come and encourages them to come to the next session. They note the reason underlying the participant’s absence and share this information with the supervisor. If the person does not show up for more than one session, the CHA visits them and finds out why they did not come. The CHA responds based on guidance from the supervisor. CHAs’ supervisors call them weekly and visit them monthly to ensure quality monitoring and retention strategy. A participant is considered to have fully participated in a CBSH group if he/she attended a minimum number of sessions. Active participants continue to engage in the healing group practices and complete the 15-week-long program.
Relevant concomitant care permitted or prohibited during the trial
There are no planned concomitant interventions that will take place in the area where the CBSH intervention will be conducted. The participants will be free to participate in any other intervention program that may arise during the trial period without requiring permission from the CHAs. To ensure control over co-intervention bias, we will monitor whether the participants are involved in similar group therapy programs [29].
Provisions for post-trial care
This study poses no risk to the participants, except the risk of potential discomfort due to discussing their personal matters. In addition, clinical psychologists are available to provide psychological support in case any crises occur during the intervention. Participants will not receive any monetary compensation. Those in the control group will be on the waiting list and will have the opportunity to participate in the CBSH intervention after the final evaluation. Participants in the intervention groups will continue receiving support through the long-term CBSH group activities. They will also have access to their usual local primary care providers.
Outcome measures
Socio-demographic characteristics will be collected using the sociodemographic questionnaire.
Primary outcome measures
Ubuntu as assessed using the Ubuntu measurement scale developed by Itayi Mutsonziwa’s (PhD thesis), which includes three indicators: humanness, interconnectedness, and compassion, comprised of 6, 5, and 8 items, respectively [30]. Additionally, the 9-item Ubuntu scale by Terblanché-Greeff and Nel will be used for convergent validity testing [31].
Secondary outcome measures
Depression as measured with the Patient Health Questionnaire (PHQ-9) for depression [32].
Anxiety as measured with the Generalized Anxiety Disorder assessment (GAD-7) [33].
Posttraumatic stress disorder as assessed using the PTSD Checklist for DSM-5 (PCL-5) [34].
Mental wellbeing as evaluated with the Warwick-Edinburgh Mental Wellbeing scale (WEMWS) [35].
Resilience as assessed with the 10-item Connor-Davidson Resilience scale (CD-RISK-10) [36].
Psychosomatic symptoms as measured with the 15-item Somatic Symptom Severity Scale (PHQ-15) [37].
Intimate partner violence as assessed using the Revised Conflict Tactics scale short form (CTS2S) [38].
Social capital as measured with the Adapted Social Capital Assessment Tool (SASCAT) [39].
Participant timeline
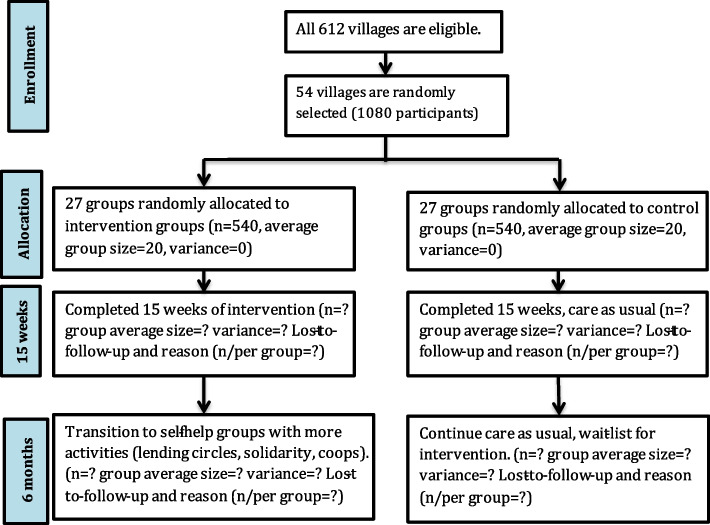
The schematic chart and study schedule are shown in Fig. 1 and Table 1.
Fig. 1.
The schematic chart
Table 1.
The community-based social healing (CBSH) trial work plan
| Study period | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| Time point | Enrollment | Allocation | Post-allocation | ||||||
| Enrollment: | Dec-2023 | Jan-24 | Feb-24 | Mar-24 | Apr-24 | May-24 | June-24 | Jul-24 | Jan-25 |
| Screening | Dec 13–Jan 26 | ||||||||
| Informed consent | Jan 29–Feb 7 | ||||||||
| Allocation | Feb 7 | ||||||||
| Interventions: | |||||||||
| CBSH | March 1–June 23 | ||||||||
| Assessments: | |||||||||
| Baseline tests | Jan 29–Feb 7 | ||||||||
| 15-week tests | June 24–July 10 | ||||||||
| Final tests | Jan 6–17 | ||||||||
Figure 1 shows when the test measures will be obtained from both groups. The baseline data is collected at T1 after villages are randomly selected and participants recruited, but before they are randomly allocated to either intervention or control group. The endline data is collected at T2, immediately after the intervention, and at T3, the follow-up data collection is collected 6 months after the intervention.
Table 1 shows the protocol schedule starting with participant enrollment in the community-based social healing (CBSH) intervention and ending with the final assessments.
Sample size
The objective of the sample calculation for this proposal is to determine the required total sample size and cluster size considering the cluster randomized controlled trial (cRCT) design. The research aims to investigate the effect of the intervention, considering an intra-cluster correlation coefficient (ICC) of 0.13, which was based on previous pilot study data. Each cluster was designed to contain 20 individuals, and an effect size of 0.2 was considered. This effect size was chosen to ensure the study’s sensitivity in detecting even small effects if they exist, reflecting the research team’s commitment to robustly evaluate the intervention’s impact. An expectation of two individuals to be lost to follow-up in each cluster is included in the calculation, based on previous experiences with the implementation of the intervention. Using standard statistical formulas, the study determined that a total sample size of approximately 1,080 individuals will be necessary to achieve the desired statistical power of 0.80 and a significance level of alpha = 0.05 while accounting for attrition. To evenly distribute participants between the control and intervention groups, an allocation of 27 clusters to each group is proposed, ensuring a balanced study design. This calculation highlighted the importance of incorporating real-world experiences and statistical rigor into the design of this study, especially in the context of cluster randomized trials.
Assignment of interventions: randomized allocation
Sequence generation
All computer-generated randomization sequence numbers were generated using Microsoft Excel. The random selection of 54 villages in Kirehe is detailed in the “ Selection of eligible study villages” section. The allocation of villages to intervention or control groups is detailed in the “ Randomization” section.
Concealment mechanism
The allocation of villages to intervention and control will be performed after the baseline data collection. The allocations will be concealed from the CHAs until the beginning of the intervention to avoid biased selection of participants and from the participants to avoid the influence of knowledge of the group they would belong to [39].
Assignment of interventions: blinding
Due to the nature of mind–body interventions in this study, it is not feasible to blind participants or Community Healing Assistants (CHAs) to the intervention. Also, there is no placebo activity for the control group. However, to reduce potential bias, all data will be anonymized by removing identifying information and using participant numbers instead of names. This anonymization process ensures that data collectors remain blind to the group assignments throughout the study. Since data collectors will not have knowledge of which participants are in the intervention or control groups, no further unblinding procedures are necessary.
Data collection and management
Plans for assessment and collection of outcomes
The Ubuntu measurement scales will be validated through translation and back-translation and content reviewed by subject matter experts and CBSH beneficiaries. Through two focus group discussions, they determined that the scales were appropriate culturally for Rwanda and did not make any changes. Trial data will be collected using a team of 16 data collectors who will have trained for 2 days about study objectives, ethical considerations, data quality, and the questionnaires. They use standardized questionnaires on mental health, social capital, resilience, intimate partner violence, and somatic symptoms. Prior to the actual data collection, questionnaires will be tested by data collectors for clarity and data accuracy. Data collections will take about 1 h per participant.
Plans to promote participant retention and complete follow-up
There is a participant retention protocol that will be implemented by CHAs with the support of psychologists who supervise them. These plans and protocols are detailed in the “ Strategies to improve adherence to intervention” section.
Data management
Detailed notes will be taken during qualitative preparatory data collection and will be accessible to the research team. Quantitative data will be collected in the Kobo toolbox, an electronic data management system, and will be extracted for statistical analysis. The data will be managed by a researcher who will check the quality of the data during and after data collection as well as clean it. All files related to the research such as attendance list, ID logs, and informed consent forms will be kept in a secure place throughout the research. All data and information will be stored in a password-protected computer, only accessible to the research team.
Confidentiality
All qualitative and quantitative data and other documents related to the study will be anonymized and stored in a password-protected computer only accessible to the research team. In addition, confidentiality is a vital component of the principles of the intervention. In the first therapeutic group session, participants commit themselves to respecting and preserving one another’s confidentiality for their safety.
Data collection
Both qualitative and quantitative data will be collected. First, qualitative data will be collected for content validation of the Ubuntu measurement scales. The tools will be translated into Kinyarwanda and back translated. A team of three people (two translators and one back-translator) will meet to review the questionnaire and come to a consensus, which culminated in the final Ubuntu scales in the Kinyarwanda language. The translated tools will then be used at preparatory workshops. One workshop will be attended by the community-based social healing (CBSH) Subject Matter Experts (SMEs) including academics and senior staff of the Ubuntu Center for Peace; the other workshop will be with CBSH beneficiaries. Content validity will be tested in terms of understandability, relevance, and comprehensiveness of the proposed measurement tools for examining the relevance of indicators and item-by-item evaluation. This will ensure effective contextualization of the Ubuntu measurement tools in Rwanda.
For the quantitative data, a team of 16 data collectors will be recruited and trained for 2 days on the ethics of human research, research objectives, questionnaire content, and electronic data capture. This will be followed by practical sessions to ensure accurate, reliable, and consistent collection of data. Quantitative data will be collected and analyzed using an electronic data management system (Kobo toolbox). After training, a one-day questionnaire testing will be done, in which each data collector interviews two participants. This will ensure that data collectors are comfortable with the questionnaires and that the questions are understandable to the participants. It will also enable us to correct any mistakes in the questionnaire design and/or setup in the electronic data management system. The interviews will last approximately 1 h. Data collection will be done prior to the first group sessions, followed by one endline (immediately after the intervention) and one follow-up (6 months after the intervention).
Statistical methods
Psychometric testing
Confirmatory Factor Analysis (CFA) will be conducted on the Ubuntu measurement tool to assess factorial validity using the entire baseline sample. The model fit will be evaluated using multiple fit indices, including chi-square (non-significant), Goodness-of-Fit Index (GFI), Comparative Fit Index (CFI), and Tucker-Lewis Index (TLI) with values of 0.95 or greater, and root mean square error of approximation (RMSEA) with values close to or below 0.8, the magnitude of the factor loadings, and correlations among the latent variables will also be examined. Discriminant and convergent validity will be calculated to ensure construct validity. Cronbach’s alpha (a) and mean inter-item correlation (MIIC) will be used to evaluate the tools’ internal consistency. Items with factor loadings below 0.4, low item-total correlations (less than 0.3), or high cross-loadings will be considered for removal. Additionally, items that negatively impact Cronbach’s alpha or have mean inter-item correlations outside the acceptable range (0.15 to 0.50) will also be candidates for removal to improve the scale’s reliability.
Baseline characteristics
To verify balance across the intervention and control groups, baseline characteristics will be evaluated at both the village cluster level (such as group size and village location) and the individual level (including variables like age, gender, marital status, education, occupation, and social category). These characteristics will be organized into cross-tabulations based on group assignments, providing a detailed summary of the study population. For continuous variables with normal distributions, descriptive statistics such as mean, standard deviation, and range will be presented. For continuous variables with skewed distributions, the median, interquartile range, and range will be reported. Categorical variables will be summarized by calculating frequencies and percentages for each category within the groups.
While this baseline analysis will allow us to characterize the population and confirm that randomization has resulted in balanced groups, we do not intend to perform formal statistical tests to compare baseline characteristics between the intervention and control groups. Instead, these baseline metrics will provide descriptive insights into the initial equivalency of the groups.
Primary analysis
Pearson correlation analyses will be conducted to examine the strength of associations between Ubuntu and secondary outcomes, addressing multicollinearity concerns. We will employ a linear mixed-effects model to assess the treatment effect. The model will include fixed effects for intervention and random effects for village-specific variations, adjusting for participants’ age, gender, and location.
Age will be treated as a continuous fixed effect, so it will be z-scored in the models. By accounting for interdependence within clusters, this model will assess the intervention’s influence on the primary outcome (Ubuntu) and secondary outcomes (mental health and psychosocial functioning).
Both the main effects and interaction effects for age, gender, and location will be analyzed. The Akaike information criterion (AIC) will guide model selection by identifying models with the lowest AIC score. Additionally, mediation analyses (simple mediation, multiple parallel mediation models, and Structural Equation Models [SEM]) will be used to explore the potential mediating effects of Ubuntu on secondary outcomes using the MPlus software. Finally, since we regard this study as discovery research, we will also analyze in an exploratory fashion whether the model fit of SEM models is better when we reverse the mediation relationship by considering the main outcome to be Ubuntu and the mediating variables to be mental health (depression, anxiety, PTSD, mental wellbeing, resilience, and psychosomatic symptoms) and psychosocial functioning (intimate partner violence and social capital).
Subgroup analyses
Exploratory analyses will be conducted to assess whether the effects of the CBSH intervention differ across specific subgroups, including genocide survivors, ex-prisoners, and youth. These analyses will incorporate interaction terms between the intervention group and each subgroup within a linear mixed-effects model. Given the potential limitations in statistical power for detecting subgroup-specific effects, the results will be interpreted with caution. All subgroup analyses will adhere to the intention-to-treat principle. To mitigate the increased risk of false positives due to multiple comparisons, a Bonferroni correction will be applied where appropriate.
Interim analysis
No interim analysis will be conducted for primary and secondary outcomes. Data will be continuously monitored to ensure accuracy and consistency across baseline, endline, and follow-up data collections.
Qualitative data analysis
The qualitative data analysis will focus on adapting the Ubuntu scale through insights gained from focus group discussions (FGDs) with both beneficiaries and intervention experts. These FGDs will explore how Ubuntu is understood and experienced in the context of the CBSH intervention and within the broader Rwandan cultural framework.
The FGDs will be audio-recorded, and the recordings will be transcribed verbatim. The transcripts will be analyzed in Kinyarwanda to ensure that the nuances of the language and culture are accurately captured. The transcription files will be reviewed by the research team to ensure accuracy and consistency.
A thematic analysis approach will be used to analyze the qualitative data. A team of three researchers will independently code the transcripts, using a systematic process to identify key themes and sub-themes that emerge from the data. Thematic analysis will involve multiple stages, including open coding, axial coding, and selective coding. This process will ensure that the themes developed reflect the participants’ experiences and perceptions of Ubuntu, as well as any adjustments needed for the measurement tool.
Emerging themes will be organized into broader categories that capture the essential components of Ubuntu, while sub-themes will highlight finer distinctions, such as differences in how Ubuntu is perceived by beneficiaries versus intervention experts. The themes and sub-themes will be discussed among the research team to reach consensus on the final coding structure. This iterative process of coding and theme development will guide the adaptation of the Ubuntu scale to align with the cultural and contextual realities of the study population.
The qualitative findings will inform revisions to the Ubuntu measurement scale, adding culturally relevant items where necessary and refining the tool to better capture the concept of Ubuntu in this context. The analysis will provide a comprehensive understanding of how the intervention affects Ubuntu as a psychosocial construct, which will enhance the overall validity of the tool.
Methods in analysis to handle protocol non-adherence and missing data
To account for protocol non-adherence, an intention-to-treat (ITT) approach will be applied, ensuring that all participants are analyzed in the groups to which they were initially assigned, regardless of their adherence to the intervention protocol. This approach maintains the integrity of randomization and reflects real-world conditions, thus enhancing the study's generalizability.
For managing missing data, we will document and report specific reasons for any missing values. If the extent of missing data is less than 5%, we will address it using multiple imputation techniques in SPSS version 29. This method is chosen to minimize the potential bias that missing data could introduce and to ensure robust statistical analysis.
Plans for accessing the full protocol, anonymized participant-level data, and statistical code
The public will access the full protocol upon publication. Upon reasonable request, the principal investigator will provide the participant-level anonymized dataset and statistical codes to promote transparency and further research.
Adverse event reporting and harms
The interventions in this study have been developed to minimize the risks of harm or adverse reactions, including in traumatized populations. Nevertheless, responding to questions related to one’s personal life could cause a participant to feel uncomfortable or to experience some emotional distress. Furthermore, when people engage in mind–body practices that are relaxing, especially in settings that feel safe, their customary defenses may be lowered, such that feelings and emotion-laden memories that are usually suppressed may emerge into consciousness. Consequently, sad (or other) feelings may arise. Usually, these are brief and easily managed by the individual and the group. Often they are accompanied by feelings of relief. However, if they become too intense or prolonged, the individual may need additional support. Psychological support and referrals can be provided by a clinical psychologist as part of the protocol. Data collectors will record adverse events that might occur and report them to the researchers in the field, using an adapted standardized stress protocol that has been used in similar studies by the research team.
Plans for communicating important protocol amendments to relevant parties
All amendments made to the protocol will be reported to the Institutional Review Board of the College of Medicine and Health Sciences for review and approval. The approved amendments will be signed and dated by the Principal Investigator before implementation. Deviations from the protocol will be documented in participant files.
Dissemination plans
The results of this study will be submitted for publication in peer-reviewed journals and presented at local and international conferences to disseminate the findings to a broad academic and professional audience. Locally, the study’s outcomes will be shared at the community level, with detailed feedback provided to the Ubuntu Centre for Peace and relevant policy stakeholders in Rwanda. Furthermore, we aim to engage with the broader Rwandan community through dissemination efforts that include workshops, public forums, and collaborations with local health and social organizations. Detailed feedback will be given to the Ubuntu Centre for Peace.
Trial status
This is the original version of the protocol, issued in February 2024. The recruitment phase started in December 2023 and ended in January 2024. Any changes or protocol amendments will be accounted for in the public study record available on ClinicalTrials.gov with ID: sISRCTN17659369.
Discussion
This study is the first to examine the effect of the CBSH model on Ubuntu among its participants, including those who have experienced psychological traumas such as genocide, mass killings, sexual abuse, and domestic abuse. The previous CBSH program, a pilot study of 1899 Rwandans showed significant improvements in depression, anxiety, and PTSD [19]. Moreover, this model demonstrated substantial improvements in family relationships and work productivity [19]. The improvements associated with participation in the CBSH align with the Ubuntu way of living. Ubuntu fosters individual wellbeing in a collective environment, thereby creating a support system for the person and their society. This study will permit us to explore Ubuntu in the Rwandan context and psychometrically validate the adapted measurement tools.
One limitation of this study is that validated diagnostic measurements and criteria will not be used in the selection process. Therefore, the study population will not be characterized by documented specific diagnoses. Most participants will never have been seen by mental health professionals and therefore they will not already have formal mental health diagnoses. The selection process will rely on the judgment of village elders and briefly trained CHAs. Although the CHA training will include information about anxiety, depression, and PTSD, they will not be trained to diagnose specific disorders. However, the baseline testing will include measures of depression, anxiety, and PTSD which will help to characterize the participants. In addition, unlike drug studies wherein one can administer a placebo or comparator substance contained in capsules identical to the drug being studied, trials of mind–body interventions cannot be blinded. Another limitation of the study is the use of a non-intervention wait-list control. Without an active control, the study will not account for the effects of the attention from the CHAs and from the other participants.
The above limitations can be understood in the context of doing large field studies in countries like Rwanda with scarce mental health services, especially in rural areas. It is extremely important to do intervention trials in such settings to develop effective, inexpensive treatments that can be delivered by CHAs who may not have professional degrees in mental health, but who can extend services into remote villages with people in serious need of mental health treatment and psychosocial support.
Our hypothesis is that, compared to the control group, the intervention group receiving the CBSH will have significantly greater improvements in Ubuntu, mental health, and psychosocial functioning. The results of this study could be valuable for the Ubuntu Centre for Peace in implementing the CBSH and to policymakers, healthcare practitioners, and other stakeholders. This study could strengthen the evidence base that supports the importance of fostering Ubuntu by integrating breath-centered mind–body methods, and communal group processes to address and heal the psychosocial consequences of trauma. The quantitative and qualitative data generated by this work will provide a rich source of information to guide the adaptation of this CBSH model to the diverse people of Africa and other continents where interventions are sorely needed to cope with and recover more effectively from numerous natural and man-made disasters.
Supplementary Information
Additional file 2. Appendix A: Participant information and consent form.
Additional file 3. Appendix B: Translated partcipant information and consent form.
Acknowledgements
Not applicable.
Authors’ contributions
SJ, JBN, and PLG are the trial’s principal investigators who conceptualized the study and its objectives and designed its methods. JBN designed and provided background on the CBSH methodology; PLG and RPB designed and provided background and methodology of the Breath-Body-Mind intervention. EP determined the sample size and he is the data analyst along with JN. AN and JN drafted the manuscript. JN, EP, and SJ developed the data analysis plan. All authors revised and reviewed the manuscript and contributed to the final approval of the manuscript. All authors will fulfill authorship eligibility guidelines according to the International Committee of Medical Journal Editors (ICMJE).
Funding
This study was funded by the Trauma Research Foundation (TRF) and Ubuntu Centre for Peace.
The Trauma Research Foundation did not play a role in study design; collection, management, analysis, interpretation of data; or writing of the report. The terms of the TRF grant agreement with the Ubuntu Center for Peace include submission of the report for publication. Ubuntu Center for Peace contributed to deciding on the objectives of the study and providing background on the CBSH methodology and the decision to submit the report for publication.
Data availability
Upon reasonable request from the corresponding author, the final anonymized data set for the proposed study will be provided.
Declarations
Ethics approval and consent to participate
The Institutional Review Board of the College of Medicine and Health Sciences at the University of Rwanda has granted ethical approval to this trial (No 111/CMHS IRB/2024). The trial has already been registered with ISRCTN (ISRCTN17659369, registered on February 09, 2024). Eligible participants will be given an explanation of the study, including potential risks and benefits, and will sign informed consent forms prior to participating.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.WHO. World Health Organization. 2022. Mental disorders. Available from: https://www.who.int/news-room/fact-sheets/detail/mental-disorders. Cited 2023 Dec 13.
- 2.Ras I, Kaduyu lNuwagaba M. ISS Africa. 2023. Rethinking the language of mental healthcare in Africa. Available from: https://issafrica.org/iss-today/rethinking-the-language-of-mental-healthcare-in-africa. Cited 2023 Dec 13.
- 3.Sankoh O, Sevalie S, Weston M. Mental health in Africa. Lancet Glob Health. 2018;6(9):e954–5. [DOI] [PubMed] [Google Scholar]
- 4.Interpeace. Interpeace. 2021. Rwanda: new findings and protocols to improve mental health and social cohesion. Available from: https://www.interpeace.org/2021/09/rwanda-new-findings-and-protocols-to-improve-mental-health-and-social-cohesion-in-rwanda/. Cited 2023 Dec 12.
- 5.Kayiteshonga Y, Sezibera V, Mugabo L, Iyamuremye JD. Prevalence of mental disorders, associated co-morbidities, health care knowledge and service utilization in Rwanda – towards a blueprint for promoting mental health care services in low- and middle-income countries? BMC Public Health. 2022;22(1):1858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Muhorakeye O, Biracyaza E. Exploring Barriers to mental health services utilization at Kabutare District Hospital of Rwanda: perspectives from patients. Front Psychol. 2021;22(12):638377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Andermahr S. “Decolonizing trauma studies: trauma and postcolonialism”—Introduction. Humanities. 2015;4(4):500–5. [Google Scholar]
- 8.Bemme D, Kirmayer LJ. Global mental health: interdisciplinary challenges for a field in motion. Transcult Psychiatry. 2020;57(1):3–18. [DOI] [PubMed] [Google Scholar]
- 9.University of Minnesota. Mental health and well-being ecological model. 2020. Available from: https://mch.umn.edu/resources/mhecomodel/. Cited 2023 Dec 12.
- 10.WHO. Mental health. 2022. Available from: https://www.who.int/news-room/fact-sheets/detail/mental-health-strengthening-our-response. Cited 2023 Dec 18.
- 11.Mugumbate JR, Chereni A. Editorial: Now, the theory of Ubuntu has its space in social work. J R. 2020;10(1).
- 12.Ewuoso C, Hall S. Core aspects of ubuntu: a systematic review. South Afr J Bioeth Law. 2019;12(2):93. [Google Scholar]
- 13.Chigangaidze RK. Defending the African philosophy of ubuntu and its place in clinical social work practice in mental health: the biopsychosocial and ecological systems perspectives. Soc Work Ment Health. 2021;19(4):276–88. [Google Scholar]
- 14.Alegría M, NeMoyer A, Falgas I, Wang Y, Alvarez K. Social determinants of mental health: where we are and where we need to go. Curr Psychiatry Rep. 2018;20(11):95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ozbay F, Johnson DC, Dimoulas E, Morgan CA, Charney D, Southwick S. Social support and resilience to stress. Psychiatry Edgmont. 2007;4(5):35–40. [PMC free article] [PubMed] [Google Scholar]
- 16.Brown R, Gerbarg P, Muench F. Breathing practices for treatment of psychiatric and stress-related medical conditions. Psychiatr Clin North Am. 2013;1(36):121–40. [DOI] [PubMed] [Google Scholar]
- 17.Gerbarg P, Brown R, Streeter C, Katzman M, Vermani M. Breath practices for survivor and caregiver stress, depression, and post-traumatic stress disorder: connection, co-regulation. Compassion OBM Integr Complement Med. 2019;4(3):1–31. [Google Scholar]
- 18.Kohrt BA, Ottman K, Panter-Brick C, Konner M, Patel V. Why we heal: the evolution of psychological healing and implications for global mental health. Clin Psychol Rev. 2020;82:101920. [DOI] [PubMed] [Google Scholar]
- 19.Ubuntu Centre for Peace. Ubuntu Center for Peace. 2022. Reports and studies. Available from: https://ubuntucenterforpeace.org/reports. Cited 2023 Dec 18.
- 20.Geisler FCM, Kubiak T, Siewert K, Weber H. Cardiac vagal tone is associated with social engagement and self-regulation. Biol Psychol. 2013;93(2):279–86. [DOI] [PubMed] [Google Scholar]
- 21.Porges SW. The polyvagal perspective. Biol Psychol. 2007;74(2):116–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Chioneso NA, Hunter CD, Gobin RL, McNeil Smith S, Mendenhall R, Neville HA. Community healing and resistance through storytelling: a framework to address racial trauma in africana communities. J Black Psychol. 2020;46(2–3):95–121. [Google Scholar]
- 23.Murphy J. The role of community in meaning making: storytelling in expressive arts therapy with narrative and traumatic memory in domestic violence and sexual assault. Expressive therapies capstone theses. 2021:420.
- 24.Chan AW, Tetzlaff JM, Altman DG, Laupacis A, Gøtzsche PC, Krleža-Jerić K, et al. SPIRIT 2013 Statement: Defining Standard Protocol Items for Clinical Trials. Ann Intern Med. 2013;158(3):200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Hakizimana J paul. IGIHE. 2023. Kirehe: Buri kwezi abarenga 2200 bivuza uburwayi bwo mu mutwe. Available from: https://igihe.com/ubuzima/article/kirehe-buri-kwezi-abarenga-2200-bivuza-uburwayi-bwo-mu-mutwe. Cited 2024 Jan 9.
- 26.Magnifique M. Vuga Ukire. 2022. ABATURAGE BASAGA MILIYONI 2 BAFITE INDWARA ZO MU MUTWE MU RWANDA. Available from: https://www.vugaukire.com/post/abaturage-basaga-miliyoni-2-bafite-indwara-zo-mu-mutwe-mu-rwanda. Cited 2024 Jan 9.
- 27.Sackett DL. Clinician-trialist rounds: 5. cointervention bias – how to diagnose it in their trial and prevent it in yours. Clin Trials. 2011;8(4):440–2. [DOI] [PubMed] [Google Scholar]
- 28.Mutsonziwa I. Ubuntu: development and validation of a scale to measure African humanism. 2020;
- 29.Terblanché-Greeff AC, Nel P. Measuring context-specific collectivism: the Metzian Ubuntu Inventory. South Afr J Philos. 2022;41(4):401–14. [Google Scholar]
- 30.Kroenke K, Spitzer RL, Williams JBW. The PHQ-9: Validity of a brief depression severity measure. J Gen Intern Med. 2001;16(9):606–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Spitzer RL, Kroenke K, Williams JBW, Löwe B. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch Intern Med. 2006;166(10):1092. [DOI] [PubMed] [Google Scholar]
- 32.Blevins CA, Weathers FW, Davis MT, Witte TK, Domino JL. The posttraumatic stress disorder checklist for DSM-5 (PCL-5): Development and Initial Psychometric Evaluation. J Trauma Stress. 2015;28(6):489–98. [DOI] [PubMed] [Google Scholar]
- 33.Tennant R, Hiller L, Fishwick R, Platt S, Joseph S, Weich S, et al. The Warwick-Edinburgh Mental Well-being Scale (WEMWBS): development and UK validation. Health Qual Life Outcomes. 2007;5(1):63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.De Silva MJ, Harpham T, Tuan T, Bartolini R, Penny ME, Huttly SR. Psychometric and cognitive validation of a social capital measurement tool in Peru and Vietnam. Soc Sci Med. 2006;62(4):941–53. [DOI] [PubMed] [Google Scholar]
- 35.Nartova-Bochaver S, Korneev A, Bochaver K. Validation of the 10-item connor-davidson resilience scale: the case of Russian Youth. Front Psychiatry. 2021;10(12):611026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Straus MA, Douglas EM. A short form of the revised conflict tactics scales, and typologies for severity and mutuality. Violence Vict. 2004;19(5):507–20. [DOI] [PubMed] [Google Scholar]
- 37.Kroenke K, Spitzer RL, Williams JBW. The PHQ-15: validity of a new measure for evaluating the severity of somatic symptoms. Psychosom Med. 2002;64(2):258–66. [DOI] [PubMed] [Google Scholar]
- 38.Raudenbush SW. Statistical analysis and optimal design for cluster randomized trials. Psychol Methods. 1997;2(2):173–85. 10.1037/1082-989X.2.2.173.
- 39.Dettori J. The random allocation process: two things you need to know. Evid-Based Spine-Care J. 2010;1(3):7–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Additional file 2. Appendix A: Participant information and consent form.
Additional file 3. Appendix B: Translated partcipant information and consent form.
Data Availability Statement
Upon reasonable request from the corresponding author, the final anonymized data set for the proposed study will be provided.