Abstract
Background
The various systems of diagnosis and classification of mental disorders underline the need to evaluate the interference caused by the different disorders in a person’s daily life. The Maladjustment Inventory (MI) evaluates the impairment in the individual’s functioning in a brief and self-applied way, through six items. The objective of this research was to explore the psychometric properties of the MI scores through two studies, one with a Spanish clinical sample (Study 1) and another with a Spanish university students’ sample (Study 2).
Methods
The total sample was made up of 928 participants (81.1% women, n = 495 clinical sample). Descriptive analyses, exploration of internal structure and reliability, exploratory and confirmatory factor analyses, relationship with other variables (quality of life, anxiety, depression, neuroticism and extraversion), and percentiles and T-scores were performed.
Results
The results showed good psychometric properties of the MI, with a good fit model for one factor solution in both samples, Cronbach’s alpha coefficient of 0.84–88, and evidence of validity based on the relationship with other variables.
Conclusion
The good psychometric properties of the MI, together with its brevity, make it a recommended instrument for the evaluation of interference in both clinical and research contexts.
Supplementary Information
The online version contains supplementary material available at 10.1186/s40359-024-02133-6.
Keywords: Interference, Maladjustment, Dimensional assessment, Inventory, Clinical significance
Background
The World Health Organization defines mental health as “A state of well-being in which the individual realizes their own abilities, can cope with the normal stresses of life, can work productively and fruitfully, and is able to make a contribution to their community” [1]. From a clinical psychology categorical approach, in addition to the presence of symptoms and other related diagnostic criteria (i.e., temporary criterion), clinicians should evaluate the “clinical significance”, that is, the disorder must cause clinically significant distress or impairment in social, occupational or important areas in the individual’s functioning [2]. But how can clinicians evaluate this construct?
Methods for assessing maladjustment construct are not very clear, so it is often neglected in public health services or in research and interventions [3]. The fourth edition of the diagnostic and statistical manual for mental disorders (DSM-IV; [4]) included the “Global Assessment of Functioning (GAF)” [5]. Studies reveal that those people who have less general functioning evaluated by means of the GAF present higher scores in general psychopathology [6]. Despite the GAF appearing to be a moderately reliable and valid measure, it is not widely used due to its various limitations [7]. One of these, for example, is that it requires specific training for its use and, therefore, its reliability depends on the degree of experience of the clinician [3]. In the fifth revised edition of the DMS, clinical significance should be evaluated too, although the DSM-5 working group decided to exclude the GAF due to lack of conceptual clarity and questionable psychometrics. In this edition, within Section III, it is recommended to consider emerging measures; for example, the Disability Assessment Schedule (WHODAS 2.0; [8]) evaluates the disability of any disorder in six different domains (cognition, mobility, self-care, getting along, life activities, and participation) through 36 items. This scale also has different limitations, such as not having normative values or comparative studies that indicate the interpretation of a specific value [9]. For these reasons, despite considering functional impairment in vital areas for diagnosis, the DSM-5-TR explicitly highlights that the process of its evaluation constitutes an intrinsically difficult clinical judgment [2], as there are no specific measures.
The assessment of functional impairment defined as impairment in social, occupational or important areas in the individual’s functioning [2], is also relevant for psychological treatment purposes. In fact, one of the most well-known psychological transdiagnostic interventions for emotional disorders, the Unified Protocol (UP; [10]) recommends that clinicians carry out a case formulation which includes the patient’s current problems, then encourages clinicians to explore which vital areas are affected due to their intense emotional experiences. This information is collected qualitatively through functional assessment [10] because there are no specific tools to assess this construct quantitatively. In addition, the UP includes the assessment of depressive and anxiety symptoms over the course of the intervention through two brief validated measures, the OASIS [11] and ODSIS [12] (e.g [13]). Both measures include two items related to impairment. The Spanish validation of these scales in a clinical sample showed positive, moderate-high and statistically significant correlations with the Maladjustment Inventory (MI; [14]). One of the OASIS and ODSIS limitations is that they only assess functional impairment in three areas (work, academia and social life) and for two specific groups of symptoms (anxiety and depression).
The MI [15] is a brief self-applied Spanish scale which evaluates among six items the degree to which the current problems produce alterations in daily life (i.e., interference) in different vital areas: work/studies (“Due to my current circumstances, my performance at work has been affected”), social life (“Due to my current circumstances, my usual social life [friendship with other people] has been affected”), free time (“Due to my current circumstances, my usual leisure activities [going out, eating out, days out, holidays, playing sports…] have been affected”), relationship with partner (“Due to my current circumstances, the relationship with my partner [or the possibility of finding one] has been affected”), family life (“Due to my current circumstances, the overall relationship with my family has been affected”), and at a global level (“Due to my current circumstances, overall, my life has been affected”). The person must answer using the following scores: 0 = “Not at all”, 1 = “Rarely”, 2 = “Occasionally”, 3 = “Frequently”, 4 ="Considerably” or 5 = “Extremely” [15].
This measure has various advantages, such as being brief and easy to apply, being suitable to be applied to different clinical conditions, not requiring specialization or subjective judgment by the clinician or researcher who applies it, and overcoming the limitations of other scales that evaluate this same variable.
The original validation study was carried out with two Spanish samples: a clinical sample of 222 patients with diverse clinic pathologies (social anxiety, posttraumatic stress disorder, pathological gambling, violent behavior at home); and a normative sample of 100 subjects chosen randomly but with a similar age range and sex distribution as the clinical sample. In the study conducted on the MI, it showed adequate reliability and validity characteristics, with satisfactory internal consistency and significant positive correlations with neuroticism, anxiety, and depressive symptoms and negative correlations with extraversion and quality of life, both in clinical and non-clinical samples [14]. Likewise, in the validation article, authors explained that it was sensitive to therapeutic change [15].
Since the development and publication of the MI in 2000, it has been used in various investigations in Spain, but there are no other studies exploring its psychometric properties. Therefore, the present study aims to extend the preliminary psychometric results with two samples (Study 1: Spanish clinical sample; Study 2: Spanish university sample), including internal structure analyses (not performed in the original), in addition to estimating the reliability of the MI scores and obtaining evidence of validity based on the relationship with other variables.
The following hypotheses were proposed: (1) to obtain, through exploratory and confirmatory analysis, a unifactorial internal structure of the MI for the two subsamples; (2) acceptable internal consistency will be obtained in both samples; and finally, (3) convergent and discriminant validity will be established through positive correlations with the variables of depression, anxiety and neuroticism, and negative correlations with the variables that evaluate extraversion and quality of life.
Methods
Instruments
Sociodemographic data questionnaire (ad hoc). Using five items, it collects data about age, sex, educational level, marital status, and job status.
Semi-structured Interview Schedule for Anxiety Disorders Lifetime version (ADIS-IV-L; [16, 17]. It is a semi-structured interview for the evaluation of anxiety and depressive disorders according to the DSM-IV criteria [4]. Cohen’s Kappa inter-rater reliability ranged between values of 0.67 and 0.86 [18].
Maladjustment Inventory (MI; [15]. It evaluates the impairment or maladjustment for the individual’s current situation through six items that refer to six vital areas: 1) Work/Studies; 2) Social life; 3) Free time; 4) Relationship with partner; 5) Family life, and 6) Global. The response options are 6-point Likert-type, from 0 (Not at all) to 5 (Extremely). The total score is calculated by adding up the scores for all the items, and range between 0 and 30. Higher scores indicate greater maladjustment or impairment. We have added the Spanish original version and the translated English version of the MI following guidelines recommendations [19] (to facilitate its understanding and promote its use internationally), respectively, in the supplementary material.
Overall Depression Severity and Impairment Scale (ODSIS; [12, 14]) and Overall Anxiety Severity and Impairment Scale (OASIS; [11, 14]). These scales assess the frequency, intensity and impairment of depressive and anxious symptomatology in the past week. It is composed of five items with a 5-point Likert-type response scale from 0 (I did not feel depressed/anxious during the past week/little or not at all) to 4 (Constant/extremely depressed/anxious). Higher scores indicate greater severity and interference of depressive/anxious symptomatology.
Neuroticism and extraversion subscales of the NEO Five-Factor Inventory (NEO-FFI; [20]). We administered these two subscales of the NEO-FFI, which consists of 12 items each one. The response scale was Likert-type ranging from 0 (Strongly disagree) to 4 (Strongly agree). In the students’ sample, a Cronbach’s Alpha of 0.88 was obtained for the neuroticism and extraversion dimensions, while in the clinical sample a Cronbach’s Alpha of 0.76 was obtained for neuroticism and 0.81 for extraversion.
Quality of life. The quality of life was evaluated in the clinical sample through the Quality of Life Index (QLI; [21]). This questionnaire evaluates self-perceived quality of life through 10 items, using a Likert-type response scale ranging from 0 (Poor) to 10 (Excellent). In the case of the students’ sample, this was assessed through the Visual Analog Scale of the EuroQol-5D questionnaire [EQ-VAS: 22, 23] which evaluates the self-perceived general state of health, ranging from 0 (worst imaginable state of health) to 100 (best imaginable state of health).
Procedure
Study 1
The participants in Study 1 were patients with a main diagnosis of an ED who were part of a multicenter randomized clinical trial, carried out in public mental health units in Spain [24]. The recruitment of the clinical sample was done between March 2018 and December 2019. The inclusion criteria were: presenting a principal diagnosis of ED [25], being over 18 years old, understanding Spanish language and signing the informed consent form, and as exclusion criteria: presenting a severe mental disorder (organic mental disorder, schizophrenia or bipolar disorder), current risk of suicide or substance abuse in the last three months, and having received, in the last 5 years, 8 or more sessions of psychological treatment. The participants of the clinical sample filled out the questionnaires using the paper-and-pencil method in the first session with the clinician. This study has the approval of the ethics committee of H. Comarcal de Vinaròs; USM La Milagrosa; H. U. Río Hortega; CSM Ansoain; CSM Donostia-Egia; CSM Tarazona; H.U. Santa María; CSM Font Sant Lluís; H.G.U. de Alicante, and H.U. Reina Sofía.
Study 2
The participants in Study 2 were university students recruited through a snowball sampling method, which was carried out in 26 Spanish universities (e.g., Universidad de Zaragoza; Universitat Jame I; Universitat de València; Universidad Autónoma de Madrid; Universidad de Málaga; Universidad Alfonso X El Sabio; Universidad Complutense de Madrid; Universidad Autónoma de Barcelona; Universidad Pública de Navarra; Universidad de Oviedo, among others) starting in March 2020. For this purpose, an advertisement was disseminated through the different communication channels of the universities, as well as in social networks, to request the collaboration of university students to complete a series of questionnaires online (Qualtrics platform). The inclusion criteria were being over 18 years of age, being a student at a Spanish university, an excellent understanding of the Spanish language and signing the informed consent form; the exclusion criterion was being in receipt of psychological or psychiatric treatment at the time of evaluation. The study has been approved by the research ethics committee of Aragon.
Participants
The total sample involved 928 participants, divided into two studies: Study 1 consisted of a clinical sample of 495 participants, patients of the Spanish Public Mental Health System, with a main diagnosis of an emotional disorder (ED, which includes anxiety, depressive and related disorders [25]). The mean age was 42.34 (SD = 12.71, range 18–77) and 77.2% of the participants were women. Participants were recruited using purposive sampling. Study 2 consisted of 433 university students with a mean age of 23.02 (SD = 5.73, range 18–55), 85.7% of which were women, enrolled through the snowball sampling method. The remaining sociodemographic information for both studies can be found in Table 1.
Table 1.
Socio-demographic characteristics of the samples
| Study 1 (Clinical sample, n = 495) |
Study 2 (University students’ sample, n = 433) |
Comparison | Total (N = 928) |
||
|---|---|---|---|---|---|
| M (SD) | M (SD) | t | p | M (SD) | |
| Age | 42.34 (12.71) | 23.02 (5.73) | 30.13 | < 0.001 | 33.22 (13.92) |
| n (%) | n (%) | χ2 | p | n (%) | |
| Educational level | 401.28 | < 0.001 | |||
| University studies | 115 (23.2) | 433 (100.0) | 548 (59.1) | ||
| Primary studies or less | 112 (22.6) | — | 112 (12.1) | ||
| Secondary studies | 94 (19.0) | — | 94 (10.1) | ||
| Vocational training | 121 (24.0) | — | 121 (13.0) | ||
| High school | 53 (10.7) | — | 53 (5.7) | ||
| Marital status | 138.49 | < 0.001 | |||
| Married/living with partner | 260 (52.5) | 142 (32.8) | 402 (43.3) | ||
| Single | 152 (30.7) | 285 (65.8) | 437 (47.1) | ||
| Separated/Divorced | 70 (14.1) | 6 (1.4) | 76 (8.2) | ||
| Widowed | 13 (2.6) | — | 13 (1.4) | ||
| Job status | 270.99 | < 0.001 | |||
| Working | 212 (42.8) | 141 (32.6) | 353 (38.0) | ||
| Not working | 283 (57.2) | 292 (67.4) | 575 (62.0) | ||
| Unemployed | 108 (21.8) | — | 108 (11.6) | ||
| Sick leave | 97 (19.6) | — | 97 (10.4) | ||
| Home-maker | 26 (5.3) | — | 26 (2.8) | ||
| Student | 37 (7.5) | — | 37 (4.0) | ||
| Retired | 15 (3.0) | — | 15 (1.6) | ||
Data analysis
First, the sociodemographic characteristics of the participants were explored in both studies through descriptive statistics. To evaluate the internal structure, each of the samples were randomly and equally divided into two subsamples for exploratory (subsample 1) and confirmatory (subsample 2) factor analyses. Prior to the exploratory factor analysis, the Kaiser-Meyer-Olkin index (KMO) and Bartlett’s test of sphericity were calculated as indicators of the adequacy of the correlation matrix to the factor analysis. Likewise, in order to evaluate the number of factors, a scree plot was performed. The estimation method was principal axis factoring with oblimin rotation since a multivariate normal distribution of the data was not assumed with the Mardia Test (p < .001). Subsequently, with the data from subsample 2, a confirmatory factor analysis (CFA) was applied to corroborate the structures obtained in the exploratory factor analyses. The estimation method was Diagonally Weighted Least Squares (DWLS), a method recommended when the data are ordinal and/or non-normal. To evaluate the model fit in the CFA, the Comparative Fit Index (CFI), the Tucker-Lewis Index (TLI), the Root Mean Square Error Approximation (RMSEA) and the Standardized Root Mean Square Residual (SRMR) were used. A good fit in the CFA is considered when the SRMR and RMSEA values are less than 0.08 and 0.06, respectively. Similarly, values above 0.95 for the CFI and TLI indicate an adequate model fit [26]. The reliability was also analyzed through Cronbach’s Alpha reliability coefficients and Omega coefficients.
Next, validity tests based on the relationship with other variables were analyzed. For this purpose, the scores obtained in each study variable were compared (normality tests: p < .05, so non-parametric tests were performed) between the two samples and by sex in each of the two samples. In this sense, measurement invariance tests were performed for the MI instrument between groups and by gender. For this purpose, the Configural, Metric, Scalar, Strict and Structural invariance was analyzed. Chi-square/gl values equal to 2 and 3, ΔCFI ≤ 0.01 and ΔRMSEA ≤ 0.015 were used as reference for an adequate model fit in the analysis of measurement invariance [27].
Spearman correlation analyses were also performed to analyze MI scores with related variables, expecting positive associations between MI scores and ODSIS, OASIS and neuroticism scores, and negative associations with extraversion and quality of life scores. Finally, Percentiles and T-scores (M = 50; SD = 10) were also calculated to provide a clinically useful scale as recommended by the literature [28], based on the scores for both studies.
All statistical analyses were carried out using the IBM SPSS Statistics version 23 statistical package [29] and CFA analyses and measurement invariance testing through JASP software, version 0.9 [30].
Results
Descriptive results
The mean scores and Cronbach’s Alpha on each of the instruments used in each of the studies can be seen in Table 2. The mean score obtained on the MI in the clinical sample was 18.55 (SD = 6.45, range 0–30) and 8.56 (SD = 6.98, range 0–28) in the students’ sample. Likewise, the mean scores for each of the items (vital areas) that conform the MI in each sample can be found in Table 3.
Table 2.
Means, standard deviations, and evidence of validity based on the relationship of the MI with other variables in both studies
| M | SD | Cronbach’s Alpha |
Skewness
z |
Kurtosis
z |
Spearman’s correlation coefficient (rs) | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| 2 | 3 | 4 | 5 | 6 | |||||||
|
Study 1 (Clinical sample, n = 495) |
1. MI | 18.55 | 6.46 | 0.84 | − 0.64 | − 0.18 | 0.61** | 0.55** | 0.46** | − 0.40** | − 0.64** |
| 2. ODSIS | 10.16 | 5.25 | 0.94 | − 0.43 | − 0.77 | 0.68** | 0.47** | − 0.41** | − 0.64** | ||
| 3. OASIS | 11.09 | 4.35 | 0.87 | − 0.55 | − 0.03 | 0.46** | − 0.35** | − 0.55** | |||
| 4. Neuroticism | 32.86 | 7.14 | 0.76 | − 0.43 | − 0.03 | − 0.37** | − 0.52** | ||||
| 5. Extraversion | 21.37 | 8.34 | 0.81 | 0.24 | − 0.02 | 0.51** | |||||
| 6. QLI | 4.46 | 1.59 | 0.87 | 0.39 | − 0.14 | ||||||
|
Study 2 (University students sample, n = 433) |
1. MI | 8.56 | 6.98 | 0.88 | 0.46 | − 0.74 | 0.58** | 0.53** | 0.48** | − 0.24** | − 0.39** |
| 2. ODSIS | 3.21 | 4.32 | 0.94 | 1.38 | 1.11 | 0.57** | 0.56** | − 0.32** | − 0.40** | ||
| 3. OASIS | 4.33 | 4.37 | 0.91 | 1.04 | 0.50 | 0.62** | − 0.26** | − 0.39** | |||
| 4. Neuroticism | 21.39 | 9.36 | 0.88 | 0.19 | − 0.61 | − 0.39** | − 0.36** | ||||
| 5. Extraversion | 29.62 | 8.21 | 0.88 | − 0.23 | − 0.38 | 0.27** | |||||
| 6. EQ-VAS | 78.5 | 15.7 | -1.21 | 1.74 | |||||||
Note: MI: Maladjustment Inventory; ODSIS: Overall Depression Severity and Impairment Scale; OASIS: Overall Anxiety Severity and Impairment Scale; Neuroticism: NEO-Five-Factor Personality Inventory Neuroticism; Extraversion: NEO-Five-Factor Personality Inventory Extraversion; QLI: Quality of Life Index; EQ-VAS: visual analog scale of the EuroQol-5D questionnaire; **p < .001
Table 3.
Means, standard deviations and factor loadings of the vital areas of the MI, and evidence of validity based on the relationship with other variables
| Vital areas of the MI | Study 1 | Study 2 | Mann-Whitney U-test | Z | Rank-biserial corr coef | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Clinical sample (n = 495) |
University students’ sample (n = 433) |
||||||||||
| M | SD | EFA Factor loadings |
CFA Factor loadings | M | SD | EFA Factor loadings |
CFA Factor loadings | ||||
| Item 1 (Work or studies) | 3.26 | 1.55 | 0.55 | 0.63 | 1.36 | 1.43 | 0.73 | 0.74 | 41905.50 | -16.29** | − 0.54** |
| Item 2 (Social life) | 3.07 | 1.41 | 0.76 | 0.81 | 1.53 | 1.47 | 0.84 | 0.84 | 49334.50 | -14.46** | − 0.48** |
| Item 3 (Hobbies) | 3.33 | 1.37 | 0.72 | 0.81 | 1.73 | 1.56 | 0.83 | 0.75 | 48628.00 | -14.59** | − 0.49** |
| Item 4 (Relationship) | 2.67 | 1.68 | 0.54 | 0.59 | 0.99 | 1.50 | 0.48 | 0.49 | 50395.50 | -14.42** | − 0.47** |
| Item 5 (Family life) | 2.66 | 1.42 | 0.62 | 0.66 | 1.33 | 1.47 | 0.66 | 0.76 | 55489.00 | -12.93** | − 0.43** |
| Item 6 (Global maladjustment) | 3.57 | 1.16 | 0.87 | 0.86 | 1.61 | 1.38 | 0.94 | 0.93 | 32142.50 | -18.73** | − 0.62** |
Note: MI: Maladjustment Inventory; **p < .001
Evidence of validity based on internal structure: EFA and CFA
Exploratory factorial analysis (EFA)
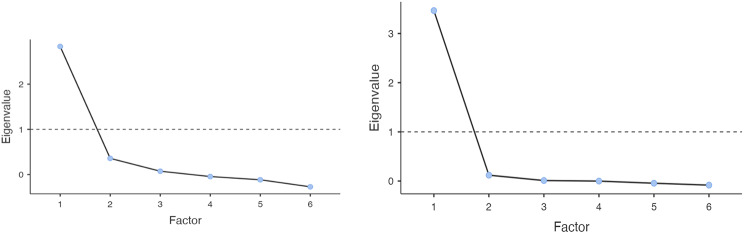
Two exploratory factor analyses were conducted with subsample 1 of the clinical sample (n = 247 participants) and of the student sample (n = 217). In clinical subsample 1, a good sampling adequacy (KMO = 0.81) was obtained, and Bartlett’s test of sphericity was 592.32 (p < .001), allowing the implementation of the exploratory factor analysis. An essentially one-dimensional solution was observed in the scree plot (Fig. 1). This solution explained 47.2% of the variance. Table 3 shows the factor loadings, which ranged from 0.54 (item 4) to 0.87 (item 6). For student subsample 1, the KMO test was 0.87. In addition, Bartlett’s test of sphericity was 730.46 (p < .001). As with the clinical subsample, the scree plot yielded a unifactorial solution (Fig. 1), which explained 57.8% of the variance. As can be seen in Table 3, factor loadings ranged from 0.48 (item 4) to 0.94 (item 6).
Fig. 1.
Scree plot of the Exploratory Factor Analysis (EFA) in the clinical and student subsample. Note: The first figure represents the results of the Exploratory Factor Analysis (EFA) in the clinical subsample, while the second figure represents the results of the EFA in the student subsample
Confirmatory factorial analysis (CFA)
Two confirmatory factor analyses were conducted with subsample 2 of the clinical sample (n = 248) and of the student sample (n = 217). In clinical subsample 2, one factor solution showed a good fit model (χ2 = 7.84, p = .551; CFI = 1.00; TLI = 1.00; RMSEA = 0.00 [90% CI = 0.00, 0.07]; SRMR = 0.04). In Table 3, factor loadings ranged from 0.59 (item 4) to 0.86 (item 6). For student subsample 2, unifactorial solution also showed good fit model (χ2 = 4.54, p = .872; CFI = 1.00; TLI = 1.00; RMSEA = 0.00 [90% CI = 0.00, 0.04]; SRMR = 0.03). In Table 3, factor loadings ranged from 0.49 (item 4) to 0.93 (item 6).
Estimation of reliability
The reliability coefficient of the MI scores showed an adequate internal consistency in the clinical sample, with a Cronbach’s alpha coefficient of 0.84 [95% CI = 0.82, 0.86] and Omega coefficient of 0.84 [95% CI = 0.82, 0.86], while in the students’ sample, the results showed a Cronbach’s alpha coefficient of 0.88 [95% CI = 0.86, 0.90] and Omega coefficient of 0.88 [95% CI = 0.87, 0.90].
Evidence of validity based on the relationship with other variables
Measurement invariance of MI showed a low model fit for Scalar Invariance, as can be seen in Appendix 1, when comparing the clinical and student subsamples, so comparisons between groups could not be carried out due to the lack of invariance following the model fit and comparison criterion. Regarding the remaining variables, statistically significant differences were found between the two samples in all variables: ODSIS (Z = -18.06, p < .001, Cohen’s d = -1.43), OASIS (Z = -18.69, p < .001, Cohen’s d = -1.55), neuroticism (Z = -17.48, p < .001, Cohen’s d = -1.39) and extraversion (Z = -13.72, p < .001, Cohen’s d = 1.00), with ODSIS, OASIS and neuroticism scores being higher for the clinical sample (vs. students), as well as lower in extroversion. As for the measurement invariance as a function of gender, as can be seen in Appendix 2, the results showed adequate model fit based on the comparison criterion, including structural invariance for both the clinical and student samples. In addition, no sex differences were found in either study for any of the MI items, nor in the total scale (p > .05).
Regarding the relationship of the MI with other variables in Study 1 (clinical sample), and as can be seen in Table 2, the Spearman’s correlation coefficient showed a positive relationships with ODSIS (rs =0.60, p < .001), OASIS (rs = 0.56, p < .001) and neuroticism (rs = 0.44, p < .001), and negative relationships with extraversion (rs = − 0.40, p < .001) and QLI (rs = − 0.62, p < .001). Similar results were found in Study 2 (university students’ sample), with the scores on the MI correlating in a statistically significant positive way with the scores on the ODSIS (rs =. 58, p < .001), OASIS (rs = 0.53, p < .001) and neuroticism (rs = 0.48, p < .001) and negatively with extraversion (rs = − 0.24, p < .001) and EQ-VAS (rs = − 0.39, p < .001).
Percentiles and T-scores for both studies
Finally, Table 4 shows the percentiles and T-scores for each of the items of the inventory, both in the clinical (Study 1) and university students’ sample (Study 2).
Table 4.
T-scores and percentiles for the Maladjustment Inventory (MI)
| Total raw score of the MI | T-scores | Percentile rank | |
|---|---|---|---|
|
Study 1 (Clinical Sample) |
14 | 45 | 25 |
| 16 | 47 | 30 | |
| 20 | 51 | 50 | |
| 21 | 53 | 60 | |
| 24 | 56 | 75 | |
| 26 | 59 | 90 | |
| 29 | 62 | 99 | |
| Study 2 (University students’ sample) | 3 | 42 | 30 |
| 8 | 49 | 50 | |
| 10 | 52 | 60 | |
| 15 | 58 | 75 | |
| 19 | 64 | 90 | |
| 26 | 74 | 99 |
Discussion
The aim of this study was to analyze the psychometric properties of MI in two samples, clinical and university students. In general, the results showed adequate psychometric properties that support the use of the MI in both samples. More specifically, if the scores obtained in these studies are compared with the MI development study [15], interesting differences are obtained. The mean scores for the clinical sample are similar, while the scores for the university student population have increased considerably. One reason may be that in the original study the sociodemographic properties of the non-clinical participants were not specified. The university period is considered highly stressful, due to the need to adapt to new routines and changes in lifestyle, an aspect that could justify the high interference scores [31]. In addition, the 20 years that have elapsed since the creation of the scale may have an influence on the scores; for example, different studies have shown that changes in social security policies [32] or negative socioeconomic changes [33] can negatively influence the mental health of the population. Another fundamental aspect that can influence the increase in MI scores is the Covid-19 pandemic. From different studies carried out, it is evident that the pandemic has had a severe and lasting impact on people’s mental health, reducing their well-being levels [34], and adopting significant changes in their lifestyle [35]. There are studies that claim that this impact has been even greater among young people [36, 37], just the age range of our university students. The original article did not explore internal structure, so the results cannot be compared.
The factor analysis showed a unifactorial solution with adequate adjustment in both samples, which refers to a latent trait of interference or functional impairment, as the measure was conceived. Regarding reliability estimation, the coefficients obtained in our study were higher than those obtained in the original article, probably because the sample size was larger, an aspect that is especially relevant when the number of items is reduced [38]. Although the instruments used in this study were different from those used in the original study, both showed evidence of validity based on the relationship with other variables [15]. In the original study, MI scores correlated significantly and positively with scales that assess severity for each of the diagnoses [15], and in the present study, the MI scores also correlated positively and significantly with the OASIS and ODSIS scores. In addition, MI scores correlated as expected with temperament traits, positively with neuroticism, and negatively with extraversion and quality of life, correlations that were also observed in other studies [14]. Regarding the differences between group scores, the results of the measurement invariance showed that MI did not behave in a similar way in both populations and were, therefore, not comparable in our study. Nevertheless, as expected, the highest scores were obtained in the clinical sample in those variables related to symptomatology or clinical interference (MI, OASIS, ODSIS, and neuroticism), while the student subsample obtained higher scores in the variables of extraversion and quality of life. In addition, differences were also observed in each of the MI items between groups. Finally, no differences were found in MI when comparing by sex. These results contrast with other studies, where women were the ones who presented greater interference [39]. In addition, the percentile and T-score data provided facilitates the clinical utility of the scale.
This research is not without limitations. One of them is based on the fact that the university students’ sample is not equivalent in their sociodemographic characteristics to the clinical sample, which could be influencing the differences observed in other variables, especially in the MI. Future studies should replicate these results with a larger number of participants, with equivalent characteristics, and from other contexts. Also, the different modes of administration of the measures in this study (face-to-face for the clinical sample and online for the sample of university students) could influence the differences observed, therefore, it is necessary to take this aspect into account in future studies. Similarly, the assessment of the presence of a diagnosis of a psychological disorder was carried out using a closed question, which could be improved in future studies by means of questionnaires or clinical diagnostic interviews. In addition, in both samples, the percentage of women is much higher than that of men. This is representative of the university student population. Specifically, the percentage of women studying university degrees related to health sciences is higher (they are the ones who have participated the most in the subsample of students) [40] and also captures the reality of the gender distribution among the clinical population [41]. Finally, future studies should include the complete administration of instruments such as the NEO-FFI to analyze personality traits in depth, or the inclusion of the first part of the EuroQol, related to the dimensions of mobility, self-care, usual activities, pain/discomfort and anxiety/depression, as recommended by the authors [23], in order to have more comprehensive results on quality of life in the student sample.
Conclusions
In sum, the present research provides updated data on a quantitative measure of impairment in the individual’s functioning, MI. This allows this variable to be evaluated not just through clinical judgement, and to take it into account when establishing a diagnosis and planning an intervention. Having normative data allows MI to be introduced into professional practice and clinical research, not reducing mental health to the absence of illness, as indicated in the main mental health diagnostic and statistical manuals [2].
As it is a brief scale and does not require specialization on the part of the professionals who apply it, it is especially indicated to be used within the National Public Health System, with its long waiting lists, long intervals between sessions and limited consultation time in each session [42]. Thus, the MI could be used in primary care to decide if patients meet the criteria of clinical significance and require an extensive assessment and intervention.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Acknowledgements
We would like to thank all the people taking part, from non-clinical participants from universities to clinical participants from mental health units. It is also necessary to recognize the participation of the different centers and professionals that made this study possible.
Abbreviations
- MI
Maladjustment Inventory
- DSM
Diagnostic and Statistical Manual for Mental Disorders
- GAF
Global Assessment of Functioning
- WHODAS
Disability Assessment Schedule
- UP
Unified Protocol for Transdiagnostic Treatment of Emotional Disorders
- OASIS
Overall Anxiety Severity and Impairment Scale
- ODSIS
Overall Depression Severity and Impairment Scale
- ADIS-L
Semi-structured Interview Schedule for Anxiety Disorders Lifetime version
- QLI
Quality of life
- EQ-VAS
Visual Analog Scale of the EuroQol-5D questionnaire
- ED
Emotional Disorder
- M
Mean
- SD
Standard Deviation
- KMO
Kaiser-Meyer-Olkin index
- EFA
Exploratory factorial analysis
- CFA
Confirmatory Factor Analysis
- DWLS
Diagonally Weighted Least Squares
- CFI
Comparative Fit Index
- TLI
Tucker-Lewis Index
- RMSEA
Root Mean Square Error Approximation
- SRMR
Standardized Root Mean Square Residual
- CI
Confidence Interval
Author contributions
All authors contributed to the study conception and design. Conceptualization was performed by J.Os.; Data curation, by A.Q.O. and Ó.P. B; Formal analysis, by J.Or.; Investigation, by J.Os., A.Q.O., J.Or., Ó.P.B., E.E.; Methodology, by J.Or. and Ó.P.B.; Project administration, by J.Os., A.Q.O. and Ó.P.B.; Supervision, by J.Os. and E.E.; Validation, by J.Os., A.Q.O. and Ó.P.B.; Visualization, by J.Os., A.Q.O. and Ó.P.B.; Writing - original draft, by A.Q.O. and Ó.P.B.; Writing - review and editing, by J.Os., A.Q.O., J.Or., Ó.P.B., E.E.
Funding
This work was supported by the PI20/00697 project integrated in Plan Estatal de I + D + I 2017–2020 and co-funded by the “ISCIII-Sub-dirección General de Evaluación y Fomento de la investigación del Fondo Europeo de Desarrollo Regional (FEDER). Otra manera de hacer Europa”. Co-funded by Gobierno de Aragón (Department of Science, University and Society knowledge) [Grant Number Research team S31_23R].
Data availability
The datasets analyzed during this study are not publicly available due to confidentiality but can be obtained from the corresponding author upon reasonable request.
Declarations
Ethical approval
This study was conducted according to the guidelines of the Declaration of Helsinki and approved by the Ethics Committee of all collaborating centers (Ethics and Research Committee of Aragon: No. CP.-C.I. PI20/053; H. Comarcal de Vinaròs: Ref. 08/2019-05/2021; USM La Milagrosa: Ref. PI_2019/92; H. U. Río Hortega: Ref. 21-PI044; CSM Ansoain: PI_2022/85 DIC; CSM Donostia-Egia: Cod: PI2021101; CSM Tarazona: Cod: 2022.202; H.U. Santa María CEIC-2479; CSM Font Sant Lluís: Cod. CEIM: 67.22; H.G.U. de Alicante: 2022 − 0256, and H.U. Reina Sofía: Ref. Comité: 5429). Informed consent to participate was obtained from all participants included in this study.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.World Health Organization. Promoting mental health: concepts, emerging evidence, practice (Summary Report). World Health Organization; 2004.
- 2.American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition, text revision. Washington, DC: American Psychiatric Association; 2022. [Google Scholar]
- 3.Forero CG, Olariu E, Álvarez P, Castro-Rodriguez J-I, Blasco MJ, Vilagut G, et al. Change in functioning outcomes as a predictor of the course of depression: a 12-month longitudinal study. Qual Life Res. 2018;27:2045–56. [DOI] [PubMed] [Google Scholar]
- 4.American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 4th ed. Washington: Author; 1994. [Google Scholar]
- 5.Endicott J, Spitzer RL, Fleiss JL, Cohen J. The Global Assessment Scale: a procedure for measuring overall severity of psychiatric disturbance. Arch Gen Psychiatry. 1976;33:766–71. [DOI] [PubMed] [Google Scholar]
- 6.van der Linden D, Dunkel CS, Prinzie P, Yamanaka-Altenstein M, von Wyl A, Hengartner MP. Overlap between general factors of psychopathology and personality: they share associations with daily life functioning and communication style. Curr Psychol. 2021. 10.1007/s12144-021-02354-7. [Google Scholar]
- 7.Goldman HH, Skodol AE, Lave TR. Revising axis V for DSM-IV: a review of measures of social functioning. Am J Psychiatry. 1992;9:149. [DOI] [PubMed] [Google Scholar]
- 8.Üstün TB, Kostanjsek N, Chatterji S, Rehm J. Measuring health and disability: Manual for WHO disability assessment schedule WHODAS 2.0. World Health Organization; 2010. [DOI] [PMC free article] [PubMed]
- 9.Gold LH. DSM-5 and the assessment of functioning: the World Health Organization Disability Assessment schedule 2.0 (WHODAS 2.0). J Am Acad Psychiatry Law. 2014;42:173–81. [PubMed] [Google Scholar]
- 10.Barlow DH, Farchione TJ, Sauer-Zavala S, Murray-Latin H, Ellard KK, Bullis JR et al. Unified Protocol for Transdiagnostic Treatment of Emotional Disorders: Therapist Guide (2.a ed.). Oxford University Press; 2018.
- 11.Norman SB, Cissel SH, Means-Christensen AJ, Stein MB. Development and validation of an overall anxiety severity and impairment scale. Depress Anxiety. 2006;23:245–9. [DOI] [PubMed] [Google Scholar]
- 12.Bentley KH, Gallagher MW, Carl JR, Barlow DH. Development and validation of the overall Depression Severity and Impairment Scale. Psychol Assess. 2014;26:815–30. [DOI] [PubMed] [Google Scholar]
- 13.Eustis EH, Gallagher MW, Tirpak JW, Nauphal M, Farchione TJ, Barlow DH. The unified protocol compared with diagnosis-specific protocols for anxiety disorders: 12-month follow-up from a randomized clinical trial. Gen Hosp Psychiatry. 2020;67:58–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Osma J, Quilez-Orden A, Suso-Ribera C, Peris-Baquero O, Norman SB, Bentley KH et al. Psychometric properties and validation of the Spanish versions of the overall anxiety and depression severity and impairment scales. J Affect Disord. 2019;252. [DOI] [PubMed]
- 15.Echeburúa E, Corral P, Fernández-Montalvo J. Maladjustment Inventory (MI): Psychometric properties in clinical contexts. Análisis Y Modificación De Conducta. 2000;26:325–40. [Google Scholar]
- 16.Brown TA, Di Nardo PA, Barlow DH. Anxiety disorder interview schedule for DSM-IV (ADIS-IV). Adult and lifetime version. Clinical manual. San Antonio: The Psychological Corporation; 1994. [Google Scholar]
- 17.Botella C, Ballester R. Trastorno De pánico, evaluación y tratamiento. Barcelona: Martínez Roca; 1997. [Google Scholar]
- 18.Brown TA, Di Nardo PA, Lehman CL, Campbell LA. Reliability of DSM-IV anxiety and mood disorders: implications for the classification of emotional disorders. J Abnorm Psychol. 2001;110:49–58. [DOI] [PubMed] [Google Scholar]
- 19.Gregoire J. ITC guidelines for translating and adapting tests. Int J Test. 2018;18:101–34. [Google Scholar]
- 20.Costa PT, McCrae RR. Revised NEO personality inventory (NEO-PI-R) and NEO five-factor inventory (NEO-FFI). Madrid: TEA Ediciones; 1999. [Google Scholar]
- 21.Mezzich JE, Ruipérez MA, Pérez C, Yoon G, Liu J, Mahmud S. The Spanish Version of the quiality of Life Index. J Nerv Ment Dis. 2000;188:301–5. [DOI] [PubMed] [Google Scholar]
- 22.Badia X, Roset M, Montserrat S, Herdman M, Segura A. The Spanish version of EuroQol: a description and its applications. European quality of Life scale. Med Clin (Barc). 1999;112:79–85. [PubMed] [Google Scholar]
- 23.Brooks R. EuroQol: the current state of play. Health Policy (New York). 1996;37:53–72. [DOI] [PubMed] [Google Scholar]
- 24.Osma J, Suso-Ribera C, García-Palacios A, Crespo-Delgado E, Robert-Flor C, Sánchez-Guerrero A, et al. Efficacy of the unified protocol for the treatment of emotional disorders in the Spanish public mental health system using a group format: Study protocol for a multicenter, randomized, non-inferiority controlled trial. Health Qual Life Outcomes. 2018;16(1):46. [DOI] [PMC free article] [PubMed]
- 25.Bullis JR, Boettcher H, Sauer-Zavala S, Farchione TJ, Barlow DH. What is an emotional disorder? A transdiagnostic mechanistic definition with implications for assessment, treatment, and prevention. Clinical Psychology: Science and Practice. 2019;26.
- 26.Hu L, Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: conventional criteria versus new alternatives. Struct Equ Model. 1999;6:1–55. [Google Scholar]
- 27.Putnick DL, Bornstein MH. Measurement invariance conventions and reporting: the state of the art and future directions for psychological research. Dev Rev. 2016;41:71–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.De Beurs E, Oudejans S, Terluin B. A common measurement scale for Self-Report instruments in Mental Health Care: T scores with a normal distribution. Eur J Psychol Assess. 2022;1015–a5759000740.
- 29.IBM Corp. IBM SPSS Statistics for Windows, Version 22.0. 2013.
- 30.Team J. JASP (Version 0.9)[Computer software]. 2018.
- 31.Cooke R, Bewick BM, Barkham M, Bradley M, Audin K. Measuring, monitoring and managing the psychological well-being of first year university students. Br J Guid Counc. 2006;34:505–17. [Google Scholar]
- 32.Simpson J, Albani V, Bell Z, Bambra C, Brown H. Effects of social security policy reforms on mental health and inequalities: a systematic review of observational studies in high-income countries. Soc Sci Med. 2021;272:113717. [DOI] [PubMed] [Google Scholar]
- 33.Barbaglia MG, Have M, ten, Dorsselaer S, Alonso J, de Graaf R. Negative socioeconomic changes and mental disorders: a longitudinal study. J Epidemiol Community Health (1978). 2015;69:55–62. [DOI] [PubMed]
- 34.Ayuso-Mateos JL, Mediavilla R, Rodriguez KR, Bravo MF. Informing the response to COVID-19 in Spain: priorities for mental health research. Revista De Psiquiatría Y Salud Mental -. J Psychiatry Mental Health. 2021;14:79–82. [DOI] [PMC free article] [PubMed]
- 35.Balanzá-Martínez V, Kapczinski F, de Azevedo Cardoso T, Atienza-Carbonell B, Rosa AR, Mota JC, et al. The assessment of lifestyle changes during the COVID-19 pandemic using a multidimensional scale. Revista De Psiquiatría Y Salud Mental -. J Psychiatry Mental Health. 2021;14:16–26. [DOI] [PMC free article] [PubMed]
- 36.Luthar SS, Ebbert AM, Kumar NL. The Well-Being Index (WBI) for schools: a brief measure of adolescents’ mental health. Psychol Assess. 2020;32:903–14. [DOI] [PubMed] [Google Scholar]
- 37.Preetz R, Filser A, Brömmelhaus A, Baalmann T, Feldhaus M. Longitudinal Changes in Life Satisfaction and Mental Health in emerging Adulthood during the COVID-19 pandemic. Risk and protective factors. Emerg Adulthood. 2021;9:602–17. [Google Scholar]
- 38.Rouquette A, Falissard B. Sample size requirements for the internal validation of psychiatric scales. Int J Methods Psychiatr Res. 2011;20:235–49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Londoño-Pérez C, Cita-Álvarez A, Niño-León L, Molano-Cáceres F, Reyes-Ruíz C, Vega-Morales A, et al. Sufrimiento psicológico en hombres y mujeres con síntomas de depresión. Terapia psicológica. 2020;38:189–202. [Google Scholar]
- 40.INE [Instituto Nacional de Estadística]. Graduados Según Nivel Educativo. Pruebas De Acceso A La Universidad. Estudiantes Matriculados en Educación Universitaria. Madrid: Instituto Nacional de Estadística; 2020. [Google Scholar]
- 41.World Health Organization. Depression and other Common Mental disorders: global health estimates. Geneva: Author; 2017. [Google Scholar]
- 42.Osma J, Peris-Baquero O, Suso-Ribera C, Farchione TJ, Barlow DH. Effectiveness of the Unified Protocol for transdiagnostic treatment of emotional disorders in group format in Spain: results from a randomized controlled trial with 6-months follow-up. Psychother Res. 2022;32:329–42. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The datasets analyzed during this study are not publicly available due to confidentiality but can be obtained from the corresponding author upon reasonable request.