Abstract
Background:
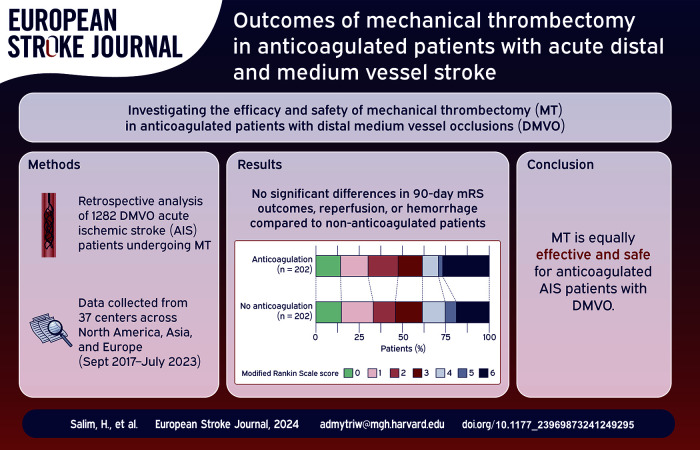
Stroke remains a major health concern globally, with oral anticoagulants widely prescribed for stroke prevention. The efficacy and safety of mechanical thrombectomy (MT) in anticoagulated patients with distal medium vessel occlusions (DMVO) are not well understood.
Methods:
This retrospective analysis involved 1282 acute ischemic stroke (AIS) patients who underwent MT in 37 centers across North America, Asia, and Europe from September 2017 to July 2023. Data on demographics, clinical presentation, treatment specifics, and outcomes were collected. The primary outcomes were functional outcomes at 90 days post-MT, measured by modified Rankin Scale (mRS) scores. Secondary outcomes included reperfusion rates, mortality, and hemorrhagic complications.
Results:
Of the patients, 223 (34%) were on anticoagulation therapy. Anticoagulated patients were older (median age 78 vs 74 years; p < 0.001) and had a higher prevalence of atrial fibrillation (77% vs 26%; p < 0.001). Their baseline National Institutes of Health Stroke Scale (NIHSS) scores were also higher (median 12 vs 9; p = 0.002). Before propensity score matching (PSM), anticoagulated patients had similar rates of favorable 90-day outcomes (mRS 0–1: 30% vs 37%, p = 0.1; mRS 0–2: 47% vs 50%, p = 0.41) but higher mortality (26% vs 17%, p = 0.008). After PSM, there were no significant differences in outcomes between the two groups.
Conclusion:
Anticoagulated patients undergoing MT for AIS due to DMVO did not show significant differences in 90-day mRS outcomes, reperfusion, or hemorrhage compared to non-anticoagulated patients after adjustment for covariates.
Keywords: Stroke, thrombectomy, anticoagulation
Graphical abstract.
Introduction
Despite a global decline in age-standardized stroke mortality rates over the past two decades due to advancements in diagnosis and treatment, the worldwide impact of stroke remains substantial.1,2 Oral anticoagulants are commonly prescribed to prevent stroke in individuals with atrial fibrillation and those with artificial heart valves.3–7 In cases of acute stroke, intravenous thrombolysis within the first 4.5 h of symptom onset is indicated, unless contraindications exist8,9 such as treatment with vitamin K antagonists (VKAs) and an international normalized ratio (INR) greater than 1.7 or Direct Oral Anticoagulants (DOACs).8,9
Clinical data supporting Mechanical Thrombectomy (MT) for distal medium vessel occlusions (DMVOs) is progressively emerging, though it remains relatively sparse.10,11 Several ongoing trials and studies are aiming to evaluate the benefit of MT in DMVO.12–18
Data regarding the efficacy and safety of MT in patients who were taking anticoagulation before stroke onset are scarce. 19 While studies have reported the feasibility of MT in anticoagulated patients with large vessel occlusion stroke,20–26 none has evaluated this in DMVO.
In this study, we aim to evaluate the efficacy and safety of MT in anticoagulated patients with DMVO.
Methods
Setting
Characteristics and outcomes of patients with acute ischemic stroke (AIS) due to DMVO treated with MT without IVtPA were collected at 37 academic centers in North America, Asia, and Europe. In this study, participating centers conducted a retrospective analysis on a consecutive series of patients admitted for acute ischemic stroke. These patients underwent MT for occlusions in medium-proximal vessels or primary medium-distal vessels, as defined by Saver et al. 10 This study adheres to Strengthening the Reporting of Observational studies in Epidemiology (STROBE) guidelines. 27
The data collection period spanned from September 2017 to July 2023. The local board-certified neurointerventionalists reviewed all cases before sending their data to the Multicenter Analysis of primary Distal medium vessel occlusions: effect of Mechanical Thrombectomy (MAD-MT) consortium. They determined the angiographic treatment success before the data was sent to the consortium, which was self-reported by each center. All treatment decisions were made at the discretion of the treating clinicians.
Study population and inclusion criteria
We focused on patients with acute ischemic stroke due to distal medium vessel occlusion (DMVO) of the MCA. Inclusion criteria were: (1) acute ischemic stroke patients with DMVO in the M2, M3, and M4 segments of the middle cerebral artery. 10 (2) undergoing MT without IV-tPA; (3) availability of 90-day modified Rankin Scale (mRS) data post-MT.
Data collection
Baseline characteristics and risk factors were recorded for patients. These included sex (male or female), age, hypertension, hypercholesterolemia, diabetes mellitus, and smoking status. Atrial fibrillation was identified based on patient history and diagnostic findings at presentation, encompassing both individuals with previously diagnosed atrial fibrillation and those identified at the presentation. Pre-morbid modified Rankin Scale (mRS) score and occluded vessel/segment, stratified into subgroups based on their occlusion location during the initial angiography, differentiating between medium proximal (M2) and medium distal vessels (M3, M4), were similarly recorded. The onset of stroke was trichotomized into witnessed, unknown, or wake-up stroke. National Institutes of Health Stroke Scale (NIHSS) was recorded at the presentation. Baseline Alberta Stroke Program Early CT Score (ASPECTS) was collected per each institution’s protocol.
Procedural details of interest included antiplatelet and anticoagulation medication status, with patients deemed anticoagulated if they were on home VKAs or DOACs upon presentation. Other procedural details includes mothership versus drip-and-ship, time from onset to puncture and recanalization, vital sign readings (blood pressure, temperature, heart rate), glycemic readings, anesthesia type (general, sedation, or local), access site (femoral or radial), heparin administration, and imaging after MT (computed tomography [CT], magnetic resonance [MR], or none).
Outcomes
The primary outcomes of interest were excellent and good functional outcomes defined as an mRS score of 0–1 and 0–2 measured at 90 days, respectively. Secondary outcomes of interest included first-pass effect (FPE), modified thrombolysis in cerebral infarction (mTICI) scores, number of thrombectomy passes, and mRS scores at 90 days. mRS and mTICI scores were adjudicated as per each institution’s protocol. Safety outcomes included Intracerebral hemorrhage (ICH), which was defined per “The Heidelberg Bleeding Classification.” 28
Procedural and technical details
Treatment consisted of MT alone. MT access site (femoral artery or radial artery), number of passes, and MT device selection and type (aspiration or stent-retriever) were left at the individual operator’s discretion.
Statistical analysis
The statistical analysis was performed using R studio, version 4.2.2. Categorical variables were summarized as frequencies and percentages and compared using the χ^2 test. Continuous variables were presented as medians and interquartile ranges (IQRs) and compared by Mann-Whitney U test.
Propensity score matching (PSM) was used to control for potential confounders. We estimated the propensity scores using logistic regression, the optimal matching algorithm was used to match the cohort according to the estimated propensity, with 1:1 matching ratio. Selection of variables for PSM was informed by literature reviews, particularly focusing on factors likely to influence outcomes or complications. These predictors included age, sex, time to treatment, baseline NIHSS score, baseline mRS score, and history of antiplatelet medication use. We also considered comorbid conditions like diabetes mellitus, hypertension, hypercholesterolemia, and occlusion location (medium vs distal).
To assess the effectiveness of the balance of covariates after PSM, we utilized the standardized mean difference, considering a threshold of <0.1 as indicative of effective balance. Results were considered statistically significant if they had a p value of 0.05 or less.
Missing data
We addressed the issue of missing data in our analysis by making the assumption that it was either completely missing at random or randomly missing (Supplemental Figure 1). We opted to retain cases with missing values to minimize bias and loss of statistical power that case exclusion could have introduced.
To handle missing data, we employed multiple imputation using chained equations. Fifty imputed datasets were produced using this method; each dataset was generated via five iterations of the imputation procedure. Our methodology for imputation was tailored to each variable: we employed predictive mean matching for continuous variables, logistic regression for binary variables, and polynomial regression for categorical variables. Significantly, imputations were performed exclusively on matched data. No imputation was performed on cases with missing data on outcomes of interest (90 days mRS, reperfusion rates, mortality, and hemorrhagic complications).
Logistic regression analysis
After performing the imputation, we applied a logistic regression model to investigate the relationship between the use of anticoagulants at baseline and the observed outcomes. We further modified our multivariable models to incorporate a variety of relevant variables. The adjustments encompassed treatment-level variables, such as the time to treatment, as well as patient-level variables, including sex and age, the location of the occlusion, and comorbidities.
Results
Patient characteristics
A total of 653 patients were included in this study examining the efficacy and safety of MT in anticoagulated versus not anticoagulated stroke patients. Among them, 223 (34%) were on anticoagulation therapy before intervention, while 430 (66%) were not. Anticoagulated patients were older, with a median age of 78 years compared to 74 years in the non-anticoagulated group (p < 0.001). The proportion of male patients was slightly higher in the anticoagulated group compared to the non-anticoagulated group (52% vs 47%, p = 0.18) (Table 1).
Table 1.
Baseline characteristics of patients before PSM.
| Variable a | No anticoagulation, N = 430 (66%) | Anticoagulation, N = 223 (34%) | p-value b |
|---|---|---|---|
| Male, n (%) | 202 (47) | 117 (52) | 0.18 |
| Age, median (IQR) | 74 (64, 82) | 78 (69, 84) | <0.001 |
| Hypercholesterolemia, n (%) | 145 (37) | 110 (50) | <0.001 |
| Hypertension, n (%) | 276 (64) | 167 (75) | 0.006 |
| Diabetes, n (%) | 118 (28) | 51 (23) | 0.2 |
| Atrial fibrillation, n (%) | 111 (26) | 172 (77) | <0.001 |
| Current smokers, n (%) | 58 (14) | 26 (12) | 0.5 |
| Previous use of antiplatelet drugs, n (%) | 156 (36) | 45 (21) | <0.001 |
| Baseline mRS (0–1), n (%) | 328 (78) | 154 (70) | 0.022 |
| Baseline mRS (0–2), n (%) | 365 (87) | 189 (86) | 0.68 |
| Site of initial occlusion | 0.47 | ||
| Medium (M2) | 366 (85) | 185 (83) | |
| Distal (M3, M4) | 64 (15) | 38 (17) | |
| ASPECTS, Median (IQR) | 9.00 (7.00, 10.00) | 9.00 (8.00, 10.00) | 0.15 |
| Baseline NIHSS, Median (IQR) | 9 (5, 16) | 12 (7, 18) | 0.002 |
| First line technique, n (%) | 0.024 | ||
| Aspiration | 105 (25) | 35 (16) | |
| Both | 252 (60) | 152 (69) | |
| Stentretriever | 65 (15) | 32 (15) | |
| Mothership versus drip and ship, n (%) | 0.78 | ||
| Drip and ship | 172 (41) | 93 (42) | |
| Mothership | 250 (59) | 129 (58) | |
| Onset to arterial puncture (min), Median (IQR) | 356 (210, 661) | 263 (186, 411) | <0.001 |
| Onset to recanalization (min), Median (IQR) | 403 (260, 696) | 324 (230, 473) | <0.001 |
| Anesthesia, n (%) | 0.84 | ||
| CS/LA | 285 (68) | 151 (69) | |
| GA | 133 (32) | 68 (31) | |
| Puncture site, n (%) | 0.26 | ||
| Femoral | 294 (97) | 138 (95) | |
| Radial | 8 (2.6) | 7 (4.8) | |
| Imaging after MT, n (%) | 0.14 | ||
| CT | 265 (64) | 146 (69) | |
| Both | 70 (17) | 22 (10) | |
| MRI | 76 (18) | 44 (21) | |
| No imaging | 3 (0.7) | 1 (0.5) | |
mRS: modified Rankin scale; NIHSS: National Institutes of Health Stroke Scale; ASPECTS: Alberta Stroke Program Early CT Score; CS/LA: conscious sedation/local anesthesia; GA: general anesthesia.
Pearson’s chi-squared test; Wilcoxon rank sum test; Fisher’s exact test.
The prevalence of hypercholesterolemia was significantly higher in the anticoagulated group (50% vs 37%, p < 0.001). Hypertension was also more common in the anticoagulated group (75% vs 64%, p = 0.006). Atrial fibrillation was more prevalent in the anticoagulated group (77% vs 26%, p < 0.001). However, the rates of diabetes and current smoking were similar between the two groups (p = 0.2 and p = 0.5, respectively).
Baseline functional status, as estimated by the mRS, showed fewer anticoagulated patients had a baseline of mRS 0–1 (70% vs 78%, p = 0.022) but the groups had similar proportions for mRS 0–2 (86% vs 87%, p = 0.68). The baseline NIHSS score was higher in the anticoagulated group (median 12 vs 9, p = 0.002). The onset to arterial puncture and onset to recanalization times were significantly shorter in the anticoagulated group (p < 0.001 for both).
Outcomes
The proportion of patients achieving mTICI 2c-3 reperfusion was identical in the anticoagulated group compared to the non-anticoagulated group (57% vs 57%, p > 0.99). TICI 2b-3 reperfusion rates were also similar between the groups (86% in anticoagulated vs 85% in non-anticoagulated, p = 0.85) (Table 2).
Table 2.
Outcomes of patients before PSM.
| Variable a | No anticoagulation, N = 430 (66%) | Anticoagulation, N = 223 (34%) | p-value b |
|---|---|---|---|
| TICI 2c-3, n (%) | 233 (57) | 121 (57) | >0.99 |
| TICI 2b-3, n (%) | 350 (85) | 183 (86) | 0.85 |
| FPE, n (%) | 131 (34) | 73 (35) | 0.94 |
| 90-day mRS 0–1, n (%) | 159 (37) | 68 (30) | 0.1 |
| 90-day mRS 0–2, n (%) | 217 (50) | 105 (47) | 0.41 |
| 90-day mortality, n (%) | 74 (17) | 58 (26) | 0.008 |
| Intracranial hemorrhage (any type), n (%) | 155 (36) | 77 (35) | 0.7 |
| Intracranial hemorrhage (by type), n (%) | |||
| HI1 | 70 (16) | 27 (12) | 0.16 |
| HI2 | 12 (2.8) | 5 (2.3) | 0.68 |
| PH1 | 15 (3.5) | 8 (3.6) | 0.94 |
| PH2 | 12 (2.8) | 6 (2.7) | 0.94 |
| SAH | 41 (9.6) | 28 (13) | 0.23 |
| Embolization in new territories, n (%) | 16 (3.8) | 9 (4.1) | 0.86 |
| Perforation, n (%) | 15 (3.6) | 8 (3.7) | 0.96 |
TICI: thrombolysis in cerebral infarction; FPE: first-pass effect; HI1: hemorrhagic infarction type 1; HI2: hemorrhagic infarction type 2; PH1: parenchymal hemorrhage type 1; PH2: parenchymal hemorrhage type 2; SAH: subarachnoid hemorrhage.
Pearson’s chi-squared test; Wilcoxon rank sum test; Fisher’s exact test.
The proportion of patients achieving an excellent 90-day outcome (mRS 0–1) was not significantly different between the anticoagulated group and the non-anticoagulated group (30% vs 37%, p = 0.1). Similarly, the proportion of patients with a good 90-day outcome (mRS 0–2) was comparable between the groups (47% vs 50%, p = 0.41). However, the 90-day mortality rate was higher in the anticoagulated group (26% vs 17%, p = 0.008).
Propensity score matching and regression analysis
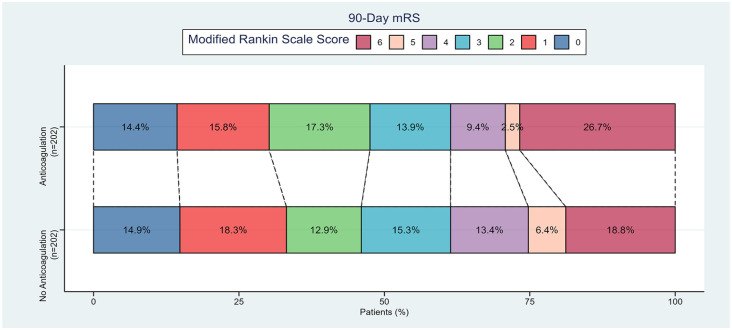
PSM resulted in 202 matched pairs (Table 3). After adjusting for covariates, anticoagulated patients did not show significant differences in outcomes such as 90-day mRS scores (Figure 1), recanalization, or hemorrhage when compared to non-anticoagulated patients. The results of both adjusted and unadjusted multivariable regression analyses are summarized in Table 4, showing no significant differences in the adjusted outcomes between the two groups. The sensitivity analysis using pre-imputation data showed similar trends. (Supplemental Table 1).
Table 3.
Baseline characteristics of patients after PSM.
| Variable a | No anticoagulation, N = 202 (50%) b | Anticoagulation, N = 202 (50%) b | p-value c |
|---|---|---|---|
| Male | 108 (53%) | 100 (50%) | 0.43 |
| Age | 76 (67, 84) | 77 (69, 84) | 0.44 |
| Hypercholesterolemia | 78 (42%) | 89 (45%) | 0.55 |
| Hypertension | 140 (69%) | 146 (72%) | 0.51 |
| Diabetes | 51 (25%) | 51 (25%) | >0.99 |
| Atrial fibrillation | 57 (28%) | 154 (76%) | <0.0001 |
| Current smokers | 24 (12%) | 23 (11%) | 0.88 |
| Previous use of antiplatelet drugs | 45 (22%) | 45 (23%) | 0.87 |
| Baseline mRS (0–1) | 152 (76%) | 146 (73%) | 0.49 |
| Baseline mRS (0–2) | 178 (89%) | 173 (87%) | 0.45 |
| Site of initial occlusion | 0.68 | ||
| Medium (M2) | 171 (85%) | 168 (83%) | |
| Distal (M3, M4) | 31 (15%) | 34 (17%) | |
| ASPECTS | 9.00 (7.00, 10.00) | 9.00 (8.00, 10.00) | 0.50 |
| Baseline NIHSS | 12 (5, 18) | 11 (7, 18) | 0.44 |
| First line technique | 0.38 | ||
| Aspiration | 42 (21%) | 32 (16%) | |
| Both | 124 (63%) | 136 (69%) | |
| Stentretriever | 31 (16%) | 30 (15%) | |
| Mothership versus drip and ship | 0.63 | ||
| Drip and ship | 82 (41%) | 88 (44%) | |
| Mothership | 116 (59%) | 113 (56%) | |
| Onset to arterial puncture (min) | 273 (180, 479) | 265 (189, 415) | 0.58 |
| Onset to recanalization (min) | 355 (234, 530) | 328 (240, 476) | 0.30 |
| Anesthesia | 0.88 | ||
| CS/LA | 136 (69%) | 136 (69%) | |
| GA | 60 (31%) | 62 (31%) | |
| Puncture site | 0.17 | ||
| Femoral | 132 (99%) | 127 (95%) | |
| Radial | 2 (1.5%) | 6 (4.5%) | |
| Imaging after MT | 0.28 | ||
| CT | 124 (65%) | 130 (68%) | |
| Both | 31 (16%) | 21 (11%) | |
| MRI | 35 (18%) | 41 (21%) | |
| No imaging | 1 (0.5%) | 0 (0%) | |
mRS: modified Rankin scale; NIHSS: National Institutes of Health Stroke Scale; ASPECTS: Alberta stroke program early CT score; CS/LA: conscious sedation/local anesthesia; GA: general anesthesia.
n (%); Median (IQR).
Pearson’s chi-squared test; Wilcoxon rank sum test; Fisher’s exact test.
Figure 1.
Bar charts display the percentage distribution of 90-day modified Rankin Scale (mRS) scores for stroke patients.
Table 4.
Adjusted and unadjusted logistic regression after propensity score matching.
| Outcome a | No anticoagulation | Anticoagulation | Unadjusted | Adjusted * | ||
|---|---|---|---|---|---|---|
| N = 202 (50%) c | N = 202 (50%) c | OR (95% CI) b | p-value | OR (95% CI) b | p-value | |
| TICI 2b-3 | 161 (83%) | 167 (85%) | 1.14 (0.66–1.99) | 0.63 | 1.20 (0.69–2.08) | 0.52 |
| TICI 2c-3 | 109 (56%) | 111 (57%) | 1.01 (0.67–1.50) | 0.98 | 1.02 (0.68–1.53) | 0.93 |
| FPE | 57 (32%) | 66 (34%) | 1.10 (0.71–1.70) | 0.66 | 1.14 (0.73–1.80) | 0.56 |
| 90-day mRS 0–1 | 67 (33%) | 61 (30%) | 0.87 (0.57–1.33) | 0.52 | 1.05 (0.61–1.81) | 0.86 |
| 90-day mRS 0–2 | 93 (46%) | 96 (48%) | 1.06 (0.72–1.57) | 0.76 | 1.24 (0.79–1.96) | 0.35 |
| 90-day mortality | 38 (19%) | 54 (27%) | 1.57 (0.99–2.53) | 0.059 | 1.56 (0.95–2.59) | 0.082 |
| ICH (Any type) | 80 (40%) | 69 (34%) | 0.79 (0.53–1.19) | 0.26 | 0.77 (0.51–1.17) | 0.22 |
| ICH (By type) | ||||||
| HI1 | 34 (17%) | 25 (13%) | 0.70 (0.40–1.22) | 0.21 | 0.74 (0.42–1.29) | 0.28 |
| HI2 | 7 (3·5%) | 4 (2·0%) | 0.57 (0.15–1.90) | 0.37 | 0.56 (0.16–1.99) | 0.37 |
| PH1 | 8 (4·0%) | 7 (3·5%) | 0.88 (0.30–2.48) | 0.8 | 0.85 (0.30–2.41) | 0.76 |
| PH2 | 6 (3·0%) | 5 (2·5%) | 0.83 (0.24–2.81) | 0.77 | 0.89 (0.26–3.05) | 0.85 |
| SAH | 23 (12%) | 25 (13%) | 1.11 (0.60–2.03) | 0.74 | 1.06 (0.57–1.98) | 0.84 |
| Embolization in new territories | 9 (4·6%) | 8 (4·0%) | 0.87 (0.32–2.34) | 0.79 | 0.90 (0.34–2.39) | 0.83 |
| Perforation | 8 (4·1%) | 7 (3·5%) | 0.86 (0.30–2.45) | 0.78 | 0.83 (0.29–2.38) | 0.72 |
ICH: intracranial hemorrhage; TICI: thrombolysis in cerebral infarction; FPE: first-pass effect; HI1: hemorrhagic infarction type 1; HI2: hemorrhagic infarction type 2; PH1: parenchymal hemorrhage type 1; PH2: parenchymal hemorrhage type 2; SAH: subarachnoid hemorrhage.
OR: odds ratio; CI: confidence interval.
n (%); Median (IQR).
All estimates were adjusted for Sex, Age, High blood pressure, High cholesterol, Diabetes, Smoking, mRS before stroke, Baseline NIHSS, ASPECTS, Occlusion Site and onset to puncture time.
Discussion
This study compared the safety and efficacy of MT in anticoagulated versus non-anticoagulated distal and medium middle cerebral artery acute ischemic stroke patients. Patients who were on anticoagulation therapy exhibited higher mortality rates, and less mRS 0–1 and 0–2 scores. After propensity score matching, anticoagulated patients had similar outcomes compared to those with no anticoagulation.
In our study, we found that recanalization rates were similar, regardless of whether anticoagulation therapy had been administered. This is in contrast to some studies which reported better TICI scores in anticoagulated patients suggesting that clots with cardioembolic origin may be more easily removed compared to atherothrombotic clots or that anticoagulation could facilitate persistent recanalization.23,24
Safety is a serious concern in anticoagulated patients receiving endovascular therapy and hemorrhagic transformation is one of the most feared outcomes. Our results showed that the rates of intracranial hemorrhagic outcomes of any type as well as perforation were similar between anticoagulated and non-anticoagulated patients. These findings align with several published studies which suggest the safety of mechanical thrombectomy in both group of patients, even in those with high International Normalized Ratio (INR).22,23,29,30 Notably, while the observed rate of perforation within our cohorts may appear elevated, it is consistent with existing literature suggesting an increased risk of vessel perforation during MT in the context of DMVO.31,32
After 90 days of follow-up, 40% of patients, regardless of their anticoagulation status, achieved mRS score ⩽ 2. After adjusting for possible confounders, functional outcomes measured by mRS 0–1 and 0–2 were similar in both anticoagulated and non-anticoagulated patients. However, several studies revealed a less favorable outcomes in anticoagulated patients.23,29,33 While some studies have suggested a higher mortality rates in anticoagulated patients after mechanical thrombectomy, others have reported improved survival rates in this population.23,29 Our study showed that anticoagulated patients had no difference in mortality rate at 3 months compared to those who were not anticoagulated.
Our study has multiple strengths, including large-scale, multinational, multicenter, and real-world data, thereby improving generalizability. However, our study is not without limitations. Firstly, the retrospective nature of the analysis introduces the possibility of selection bias, potentially influencing the generalizability of the findings. Secondly, the scope of the study is limited to a 90-day post-intervention follow-up period, which restricts our insight into the long-term repercussions of MT complications on patients’ functional recovery and overall quality of life.
Additionally, our research does not distinguish among the specific anticoagulation therapies—VKAs versus DOACs—within the patient cohort. This omission restrain a nuanced understanding of the differential effects these therapies may have on outcomes post-MT. The study also omits an examination of the optimal timing for resuming anticoagulation therapy following MT, an aspect that could significantly affect three-month functional outcomes.
The effectiveness of anticoagulation therapy in the studied cohort remains unassessed due to the lack of initial INR levels, as well as other potential moderating factors like drug interactions and adherence to medication regimens. Furthermore, the absence of detailed patient histories regarding prior strokes—particularly given that patients receiving anticoagulation as secondary prevention exhibit a higher risk of recurrent stroke and a more adverse vascular profile than those receiving it for primary prevention—posed a limitation. Although the dataset did not permit a direct accounting for this variable, we attempted to compensate its potential impact by the balanced pre-morbid mRS scores observed between the anticoagulated and non-anticoagulated groups.
Conclusion
In conclusion, this comprehensive retrospective study provides valuable insights into the efficacy and safety of MT in anticoagulated patients with acute ischemic stroke. The analysis revealed no significant differences in 90-day mRS, recanalization rates, or hemorrhage incidences between anticoagulated and non-anticoagulated patients after adjusting for various covariates. Further research is warranted to enhance our understanding and management of acute ischemic stroke in anticoagulated patients, especially in the context of evolving endovascular therapies.
Supplemental Material
Supplemental material, sj-docx-1-eso-10.1177_23969873241249295 for Outcomes of mechanical thrombectomy in anticoagulated patients with acute distal and medium vessel stroke by Hamza Salim, Basel Musmar, Nimer Adeeb, Vivek Yedavalli, Dhairya Lakhani, Sahibjot Singh Grewal, Kareem El Naamani, Nils Henninger, Sri Hari Sundararajan, Anna Luisa Kühn, Jane Khalife, Sherief Ghozy, Luca Scarcia, Benjamin YQ Tan, Robert W Regenhardt, Jeremy J Heit, Nicole M Cancelliere, Joshua D Bernstock, Aymeric Rouchaud, Jens Fiehler, Sunil Sheth, Ajit S Puri, Christian Dyzmann, Marco Colasurdo, Xavier Barreau, Leonardo Renieri, João Pedro Filipe, Pablo Harker, Răzvan Alexandru Radu, Mohamad Abdalkader, Piers Klein, Thomas R Marotta, Julian Spears, Takahiro Ota, Ashkan Mowla, Pascal Jabbour, Arundhati Biswas, Frédéric Clarençon, James E Siegler, Thanh N Nguyen, Ricardo Varela, Amanda Baker, Muhammed Amir Essibayi, David Altschul, Nestor R Gonzalez, Markus A Möhlenbruch, Vincent Costalat, Benjamin Gory, Christian Paul Stracke, Mohammad Ali Aziz-Sultan, Constantin Hecker, Hamza Shaikh, David S Liebeskind, Alessandro Pedicelli, Andrea M Alexandre, Illario Tancredi, Tobias D Faizy, Erwah Kalsoum, Boris Lubicz, Aman B Patel, Vitor Mendes Pereira, Adrien Guenego and Adam A Dmytriw in European Stroke Journal
Supplemental material, sj-docx-2-eso-10.1177_23969873241249295 for Outcomes of mechanical thrombectomy in anticoagulated patients with acute distal and medium vessel stroke by Hamza Salim, Basel Musmar, Nimer Adeeb, Vivek Yedavalli, Dhairya Lakhani, Sahibjot Singh Grewal, Kareem El Naamani, Nils Henninger, Sri Hari Sundararajan, Anna Luisa Kühn, Jane Khalife, Sherief Ghozy, Luca Scarcia, Benjamin YQ Tan, Robert W Regenhardt, Jeremy J Heit, Nicole M Cancelliere, Joshua D Bernstock, Aymeric Rouchaud, Jens Fiehler, Sunil Sheth, Ajit S Puri, Christian Dyzmann, Marco Colasurdo, Xavier Barreau, Leonardo Renieri, João Pedro Filipe, Pablo Harker, Răzvan Alexandru Radu, Mohamad Abdalkader, Piers Klein, Thomas R Marotta, Julian Spears, Takahiro Ota, Ashkan Mowla, Pascal Jabbour, Arundhati Biswas, Frédéric Clarençon, James E Siegler, Thanh N Nguyen, Ricardo Varela, Amanda Baker, Muhammed Amir Essibayi, David Altschul, Nestor R Gonzalez, Markus A Möhlenbruch, Vincent Costalat, Benjamin Gory, Christian Paul Stracke, Mohammad Ali Aziz-Sultan, Constantin Hecker, Hamza Shaikh, David S Liebeskind, Alessandro Pedicelli, Andrea M Alexandre, Illario Tancredi, Tobias D Faizy, Erwah Kalsoum, Boris Lubicz, Aman B Patel, Vitor Mendes Pereira, Adrien Guenego and Adam A Dmytriw in European Stroke Journal
Supplemental material, sj-docx-3-eso-10.1177_23969873241249295 for Outcomes of mechanical thrombectomy in anticoagulated patients with acute distal and medium vessel stroke by Hamza Salim, Basel Musmar, Nimer Adeeb, Vivek Yedavalli, Dhairya Lakhani, Sahibjot Singh Grewal, Kareem El Naamani, Nils Henninger, Sri Hari Sundararajan, Anna Luisa Kühn, Jane Khalife, Sherief Ghozy, Luca Scarcia, Benjamin YQ Tan, Robert W Regenhardt, Jeremy J Heit, Nicole M Cancelliere, Joshua D Bernstock, Aymeric Rouchaud, Jens Fiehler, Sunil Sheth, Ajit S Puri, Christian Dyzmann, Marco Colasurdo, Xavier Barreau, Leonardo Renieri, João Pedro Filipe, Pablo Harker, Răzvan Alexandru Radu, Mohamad Abdalkader, Piers Klein, Thomas R Marotta, Julian Spears, Takahiro Ota, Ashkan Mowla, Pascal Jabbour, Arundhati Biswas, Frédéric Clarençon, James E Siegler, Thanh N Nguyen, Ricardo Varela, Amanda Baker, Muhammed Amir Essibayi, David Altschul, Nestor R Gonzalez, Markus A Möhlenbruch, Vincent Costalat, Benjamin Gory, Christian Paul Stracke, Mohammad Ali Aziz-Sultan, Constantin Hecker, Hamza Shaikh, David S Liebeskind, Alessandro Pedicelli, Andrea M Alexandre, Illario Tancredi, Tobias D Faizy, Erwah Kalsoum, Boris Lubicz, Aman B Patel, Vitor Mendes Pereira, Adrien Guenego and Adam A Dmytriw in European Stroke Journal
Supplemental material, sj-docx-4-eso-10.1177_23969873241249295 for Outcomes of mechanical thrombectomy in anticoagulated patients with acute distal and medium vessel stroke by Hamza Salim, Basel Musmar, Nimer Adeeb, Vivek Yedavalli, Dhairya Lakhani, Sahibjot Singh Grewal, Kareem El Naamani, Nils Henninger, Sri Hari Sundararajan, Anna Luisa Kühn, Jane Khalife, Sherief Ghozy, Luca Scarcia, Benjamin YQ Tan, Robert W Regenhardt, Jeremy J Heit, Nicole M Cancelliere, Joshua D Bernstock, Aymeric Rouchaud, Jens Fiehler, Sunil Sheth, Ajit S Puri, Christian Dyzmann, Marco Colasurdo, Xavier Barreau, Leonardo Renieri, João Pedro Filipe, Pablo Harker, Răzvan Alexandru Radu, Mohamad Abdalkader, Piers Klein, Thomas R Marotta, Julian Spears, Takahiro Ota, Ashkan Mowla, Pascal Jabbour, Arundhati Biswas, Frédéric Clarençon, James E Siegler, Thanh N Nguyen, Ricardo Varela, Amanda Baker, Muhammed Amir Essibayi, David Altschul, Nestor R Gonzalez, Markus A Möhlenbruch, Vincent Costalat, Benjamin Gory, Christian Paul Stracke, Mohammad Ali Aziz-Sultan, Constantin Hecker, Hamza Shaikh, David S Liebeskind, Alessandro Pedicelli, Andrea M Alexandre, Illario Tancredi, Tobias D Faizy, Erwah Kalsoum, Boris Lubicz, Aman B Patel, Vitor Mendes Pereira, Adrien Guenego and Adam A Dmytriw in European Stroke Journal
Acknowledgments
Dr. Regenhardt serves on a DSMB for a trial sponsored by Rapid Medical, serves as site PI for studies sponsored by Penumbra and Microvention, and receives stroke research grant funding from the National Institutes of Health, Society of Vascular and Interventional Neurology, and Heitman Stroke Foundation.
Dr. Guenego reports consultancy for Rapid Medical and Phenox, not directly related to the present work.
Dr. Clarençon reports conflicts of interest with Medtronic, Balt Extrusion (consultant), ClinSearch (core lab), Penumbra, Stryker (payment for reading) and Artedrone (Board) ; all not directly related to the present work
Dr. Henninger received support from W81XWH-19-PRARP-RPA form the CDMRP/DoD, NS131756 and U24NS113844 from the NINDS, and NR020231 from the NINR and received compensation from Myrobalan, Inc. and General Dynamics during the conduct of this study unrelated to this work
Dr. Liebeskind is consultant as Imaging Core Lab to Cerenovus, Genentech, Medtronic, Stryker, Rapid Medical
Dr. Yeo reports Advisory work for AstraZeneca, Substantial support from NMRC Singapore and is a medical advisor for See-mode, Cortiro and Sunbird Bio, with equity in Ceroflo. All unrelated to the present work
Dr. Griessenauer reports a proctoring agreement with Medtronic and research funding by Penumbra
Dr. Marnat reports conflicts of interest with Microvention Europe, Stryker Neurovascular, Balt (consulting), Medtronic, Johnson & Johnson and Phenox (paid lectures), all not directly related to the present work
Dr. Puri is a consultant for Medtronic Neurovascular, Stryker NeurovascularBalt, Q’Apel Medical, Cerenovus, Microvention, Imperative Care, Agile, Merit, CereVasc and Arsenal Medical, he received research grants from NIH, Microvention, Cerenovus, Medtronic Neurovascular and Stryker Neurovascular, and holds stocks in InNeuroCo, Agile, Perfuze, Galaxy and NTI
Dr. Tjoumakaris is a consultant for Medtronic and Microvention (funds paid to institution, not personally)
Dr. Jabbour is a consultant for Medtronic, Microvention and Cerus
Footnotes
The author(s) declared the following potential conflicts of interest with respect to the research, authorship, and/or publication of this article: Dr. Regenhardt serves on a DSMB for a trial sponsored by Rapid Medical, serves as site PI for studies sponsored by Penumbra and Microvention, and receives stroke research grant funding from the National Institutes of Health, Society of Vascular and Interventional Neurology, and Heitman Stroke Foundation.
Dr. Guenego reports consultancy for Rapid Medical and Phenox, not directly related to the present work.
Dr. Clarençon reports conflicts of interest with Medtronic, Balt Extrusion (consultant), ClinSearch (core lab), Penumbra, Stryker (payment for reading) and Artedrone (Board); all not directly related to the present work.
Dr. Henninger received support from W81XWH-19-PRARP-RPA form the CDMRP/DoD, NS131756 and U24NS113844 from the NINDS, and NR020231 from the NINR and received compensation from Myrobalan, Inc. and General Dynamics during the conduct of this study unrelated to this work.
Dr. Liebeskind is consultant as Imaging Core Lab to Cerenovus, Genentech, Medtronic, Stryker, Rapid Medical.
Dr. Yeo reports Advisory work for AstraZeneca, Substantial support from NMRC Singapore and is a medical advisor for See-mode, Cortiro and Sunbird Bio, with equity in Ceroflo. All unrelated to the present work.
Dr. Griessenauer reports a proctoring agreement with Medtronic and research funding by Penumbra.
Dr. Marnat reports conflicts of interest with Microvention Europe, Stryker Neurovascular, Balt (consulting), Medtronic, Johnson & Johnson and Phenox (paid lectures), all not directly related to the present work.
Dr. Puri is a consultant for Medtronic Neurovascular, Stryker NeurovascularBalt, Q’Apel Medical, Cerenovus, Microvention, Imperative Care, Agile, Merit, CereVasc and Arsenal Medical, he received research grants from NIH, Microvention, Cerenovus, Medtronic Neurovascular and Stryker Neurovascular, and holds stocks in InNeuroCo, Agile, Perfuze, Galaxy and NTI.
Dr. Tjoumakaris is a consultant for Medtronic and Microvention (funds paid to institution, not personally).
Dr. Jabbour is a consultant for Medtronic, Microvention and Cerus.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Ethical approval and Informed consent: The study received approval from the local ethical standards committee at each participating site, and informed consent from patients was waived. The data supporting this study’s findings are available from the corresponding author upon reasonable request.
Guarantor: Adam A Dmytriw
Contributorship: H.S, B.M, N.A, V.Y, D.L, S.G, K.N, N.H, S.S, A.K, J.K, S.G, L.S, B.T, R.R, J.H, N.C, J.B, A.R, J.F, S.S, A.P, C.D, M.C, X.B, L.R, J.F, P.H, R.R, M.A, P.K, T.M, J.S, T.O, A.M, P.J, A.B, F.C, J.S, T.N, R.V, A.B, M.E, D.A, N.G, M.M, V.C, B.G, C.S, M.A, C.H, H.S, D.L, A.P, A.A, I.T, T.F, E.K, B.L, A.P, V.P, A.G, A.D,. contributed to the conception and design of the work.
H. S, B.M, N.A, V.Y, D.L, S.G, K.N, N.H, S.S, A.K, J.K, S.G, L.S, B.T, R.R, J.H, N.C, J.B, A.R, J.F, S.S, A.P, C.D, M.C, X.B, L.R, J.F, P.H, R.R, M.A, P.K, T.M, J.S, T.O, A.M, P.J, A.B, F.C, J.S, T.N, R.V, A.B, M.E, D.A, N.G, M.M, V.C, B.G, C.S, M.A, C.H, H.S, D.L, A.P, A.A, I.T, T.F, E.K, B.L, A.P, V.P, A.G, A.D,. were involved in the acquisition of data, and data analysis and interpretation.
H. S, B.M, N.A, V.Y, D.L, S.G, K.N, N.H, S.S, A.K, J.K, S.G, L.S, B.T, R.R, J.H, N.C, J.B, A.R, J.F, S.S, A.P, C.D, M.C, X.B, L.R, J.F, P.H, R.R, M.A, P.K, T.M, J.S, T.O, A.M, P.J, A.B, F.C, J.S, T.N, R.V, A.B, M.E, D.A, N.G, M.M, V.C, B.G, C.S, M.A, C.H, H.S, D.L, A.P, A.A, I.T, T.F, E.K, B.L, A.P, V.P, A.G, A.D,. drafted the work and revised it critically for important intellectual content.
All authors gave final approval of the version to be published and agree to be accountable for all aspects.
ORCID iDs: Hamza Salim  https://orcid.org/0000-0002-5208-8425
https://orcid.org/0000-0002-5208-8425
Basel Musmar  https://orcid.org/0009-0000-4910-6090
https://orcid.org/0009-0000-4910-6090
Dhairya Lakhani  https://orcid.org/0000-0001-7577-1887
https://orcid.org/0000-0001-7577-1887
Luca Scarcia  https://orcid.org/0000-0002-1316-0383
https://orcid.org/0000-0002-1316-0383
Robert W. Regenhardt  https://orcid.org/0000-0003-2958-3484
https://orcid.org/0000-0003-2958-3484
Jens Fiehler  https://orcid.org/0000-0001-8533-7478
https://orcid.org/0000-0001-8533-7478
Răzvan Alexandru Radu  https://orcid.org/0000-0001-6375-8466
https://orcid.org/0000-0001-6375-8466
Piers Klein  https://orcid.org/0000-0001-7468-137X
https://orcid.org/0000-0001-7468-137X
Takahiro Ota  https://orcid.org/0000-0002-5108-6719
https://orcid.org/0000-0002-5108-6719
Pascal Jabbour  https://orcid.org/0000-0002-8965-2413
https://orcid.org/0000-0002-8965-2413
Thanh N. Nguyen  https://orcid.org/0000-0002-2810-1685
https://orcid.org/0000-0002-2810-1685
Muhammed Amir Essibayi  https://orcid.org/0000-0001-8325-2382
https://orcid.org/0000-0001-8325-2382
Nestor R. Gonzalez  https://orcid.org/0000-0002-8277-6317
https://orcid.org/0000-0002-8277-6317
Markus A. Möhlenbruch  https://orcid.org/0000-0002-5075-704X
https://orcid.org/0000-0002-5075-704X
Supplemental Material: Supplemental material for this article is available online.
References
- 1. Townsend N, Nichols M, Scarborough P, et al. Cardiovascular disease in Europe–epidemiological update 2015. Eur Heart J 2015; 36: 2696–2705. [DOI] [PubMed] [Google Scholar]
- 2. Feigin VL, Forouzanfar MH, Krishnamurthi R, et al. Global and regional burden of stroke during 1990–2010: findings from the Global Burden of Disease Study 2010. Lancet 2014; 383: 245–255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Park TH, Ko Y, Lee SJ, et al. Identifying target risk factors using population attributable risks of ischemic stroke by age and sex. Stroke 2015; 17: 302–311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Sanna T, Diener HC, Passman RS, et al.; CRYSTAL AF Investigators. Cryptogenic stroke and underlying atrial fibrillation. New Engl J Med 2014; 370: 2478–2486. [DOI] [PubMed] [Google Scholar]
- 5. Barrios V, Escobar C, Calderón A, et al. Use of antithrombotic therapy according to CHA2DS2-VASc score in patients with atrial fibrillation in primary care. Rev Española Cardiol Engl Ed 2014; 67: 150–151. [DOI] [PubMed] [Google Scholar]
- 6. Kirchhof P, Benussi S, Kotecha D, et al.; ESC Scientific Document Group. 2016 ESC guidelines for the management of atrial fibrillation developed in collaboration with EACTS. Eur Heart J 2016; 37: 2893–2962. [DOI] [PubMed] [Google Scholar]
- 7. Ruff CT, Giugliano RP, Braunwald E, et al. Comparison of the efficacy and safety of new oral anticoagulants with warfarin in patients with atrial fibrillation: a meta-analysis of randomised trials. Lancet 2014; 383: 955–962. [DOI] [PubMed] [Google Scholar]
- 8. Wahlgren N, Moreira T, Michel P, et al.; For ESO-KSU, ESO, ESMINT, ESNR and EAN. Mechanical thrombectomy in acute ischemic stroke: consensus statement by ESO-Karolinska stroke update 2014/2015, supported by ESO, ESMINT, ESNR and EAN. Int J Stroke 2016; 11: 134–147. [DOI] [PubMed] [Google Scholar]
- 9. Powers WJ, Derdeyn CP, Biller J, et al.; American Heart Association Stroke Council. 2015 American Heart Association/American Stroke Association focused update of the 2013 guidelines for the early management of patients with acute ischemic stroke regarding endovascular treatment: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke 2015; 46: 3020–3035. [DOI] [PubMed] [Google Scholar]
- 10. Saver JL, Chapot R, Agid R, et al.; Distal Thrombectomy Summit Group. Thrombectomy for distal, medium vessel occlusions: a consensus statement on present knowledge and promising directions. Stroke 2020; 51: 2872–2884. [DOI] [PubMed] [Google Scholar]
- 11. Ospel JM, Goyal M. A review of endovascular treatment for medium vessel occlusion stroke. J Neurointerv Surg 2021; 13: 623–630. [DOI] [PubMed] [Google Scholar]
- 12. ANZCTR. FRONTIER-AP: Randomized controlled trial of the clinical outcome and safety of endovascular versus standard medical therapy for stroke with medium sized vessel occlusion, https://www.anzctr.org.au/ (2021, accessed 12 December 2023).
- 13. ClinicalTrials.gov. Study details and Distal ischemic stroke treatment with adjustable low-profile stentriever, https://clinicaltrials.gov/study/NCT05152524?term=NCT05152524&rank=1 (2021, accessed 12 December, 2023).
- 14. ClinicalTrials.gov. Study details and Endovascular therapy plus best medical treatment (BMT) versus BMT alone for medium vessel occlusion stroke, https://clinicaltrials.gov/study/NCT05029414?term=NCT05029414&rank=1 (2021, accessed 12 December 2023)
- 15. ClinicalTrials.gov. Study details and Endovascular treatment to improve outcomes for medium vessel occlusions (ESCAPE-MeVO Trial), https://clinicaltrials.gov/study/NCT05151172?term=NCT05151172&rank=1 (2021, accessed 12 December 2023). [DOI] [PMC free article] [PubMed]
- 16. ClinicalTrials.gov. Study details and Evaluation of mechanical thrombectomy in acute ischemic stroke related to a distal arterial occlusion, https://clinicaltrials.gov/study/NCT05030142?term=NCT05030142&rank=1 (2021, accessed 12 December 2023) [DOI] [PubMed]
- 17. Siegler J, Shaikh H, Khalife J, et al. Aspiration versus stent-retriever as first-line endovascular therapy technique for primary medium and distal intracranial occlusions: a propensity-score matched multicenter analysis. Stroke Vasc Interv Neurol 2023; 3: e000931. [Google Scholar]
- 18. Radu RA, Costalat V, Fahed R, et al. First pass effect as an independent predictor of functional outcomes in medium vessel occlusions: an analysis of an international multicenter study. Eur Stroke J 2024; 9: 114–123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Zapata-Wainberg G, Ximénez-Carrillo A, Trillo S, et al. Mechanical thrombectomy in orally anticoagulated patients with acute ischemic stroke. J Neurointerv Surg 2018; 10: 834–838. [DOI] [PubMed] [Google Scholar]
- 20. Purrucker JC, Wolf M, Haas K, et al. Safety of endovascular thrombectomy in patients receiving non-vitamin K antagonist oral anticoagulants. Stroke 2016; 47: 1127–1130. [DOI] [PubMed] [Google Scholar]
- 21. Xian Y, Federspiel JJ, Hernandez AF, et al. Use of intravenous recombinant tissue plasminogen activator in patients with acute ischemic stroke who take non-vitamin K antagonist oral anticoagulants before stroke. Circulation 2017; 135: 1024–1035. [DOI] [PubMed] [Google Scholar]
- 22. Mundiyanapurath S, Tillmann A, Möhlenbruch MA, et al. Endovascular stroke therapy may be safe in patients with elevated international normalized ratio. J Neurointerv Surg 2017; 9: 1187–1190. [DOI] [PubMed] [Google Scholar]
- 23. Benavente L, Larrosa D, García-Cabo C, et al. Safety and efficacy of mechanical thrombectomy in acute ischemic stroke of anticoagulated patients—a prospective observational study. J Stroke Cerebrovasc Dis 2016; 25: 2093–2098. [DOI] [PubMed] [Google Scholar]
- 24. Alonso de, Leciñana M, Fuentes B, Ximénez-Carrillo Á, et al.; Madrid Stroke Network. A collaborative system for endovascular treatment of acute ischaemic stroke: the Madrid Stroke Network experience. Eur J Neurol 2016; 23: 297–303. [DOI] [PubMed] [Google Scholar]
- 25. Fuentes B, Alonso de, Leciñana M, Ximénez-Carrillo A, et al.; Madrid Stroke Network. Futile interhospital transfer for endovascular treatment in acute ischemic stroke: the Madrid Stroke Network Experience. Stroke 2015; 46: 2156–2161. [DOI] [PubMed] [Google Scholar]
- 26. Chen JH, Hong CT, Chung CC, et al. Safety and efficacy of endovascular thrombectomy in acute ischemic stroke treated with anticoagulants: a systematic review and meta-analysis. Thromb J 2022; 20: 35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Cuschieri S. The STROBE guidelines. Saudi J Anaesth 2019; 13: S31–S34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. von Kummer R, Broderick JP, Campbell BCV, et al. The Heidelberg bleeding classification. Stroke 2015; 46: 2981–2986 https://www.ahajournals.org/doi/10.1161/STROKEAHA.115.010049 (accessed 18 January 2024). [DOI] [PubMed] [Google Scholar]
- 29. Rebello LC, Haussen DC, Belagaje S, et al. Endovascular treatment for acute ischemic stroke in the setting of anticoagulation. Stroke 2015; 46: 3536–3539. [DOI] [PubMed] [Google Scholar]
- 30. Seiffge DJ, Hooff RJ, Nolte CH, et al. Recanalization therapies in acute ischemic stroke patients: impact of prior treatment with novel oral anticoagulants on bleeding complications and outcome. Circulation 2015; 132: 1261–1269. [DOI] [PubMed] [Google Scholar]
- 31. Dmytriw AA. Incidence and clinical outcomes of perforations during mechanical thrombectomy for medium vessel occlusion in acute ischemic stroke: a retrospective, multicenter, and multinational study. Eur Stroke J. Epub ahead of print 26 February 2024. DOI: 10.1177/23969873231219412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Schulze-Zachau V, Brehm A, Ntoulias N, et al. Incidence and outcome of perforations during medium vessel occlusion compared with large vessel occlusion thrombectomy. J Neurointerv Surg. Epub ahead of print 31 July 2023. DOI: 10.1136/bcr-2014-208197. https://pubmed.ncbi.Nlm.nih.gov/37524518/ (accessed 22 March 2024). [DOI] [PubMed]
- 33. Bendszus M, Thomalla G, Hacke W, et al.; THRILL investigators. Early termination of THRILL, a prospective study of mechanical thrombectomy in patients with acute ischemic stroke ineligible for I.V. Thrombolysis. Clin Neuroradiol 2016; 26: 499–500. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-docx-1-eso-10.1177_23969873241249295 for Outcomes of mechanical thrombectomy in anticoagulated patients with acute distal and medium vessel stroke by Hamza Salim, Basel Musmar, Nimer Adeeb, Vivek Yedavalli, Dhairya Lakhani, Sahibjot Singh Grewal, Kareem El Naamani, Nils Henninger, Sri Hari Sundararajan, Anna Luisa Kühn, Jane Khalife, Sherief Ghozy, Luca Scarcia, Benjamin YQ Tan, Robert W Regenhardt, Jeremy J Heit, Nicole M Cancelliere, Joshua D Bernstock, Aymeric Rouchaud, Jens Fiehler, Sunil Sheth, Ajit S Puri, Christian Dyzmann, Marco Colasurdo, Xavier Barreau, Leonardo Renieri, João Pedro Filipe, Pablo Harker, Răzvan Alexandru Radu, Mohamad Abdalkader, Piers Klein, Thomas R Marotta, Julian Spears, Takahiro Ota, Ashkan Mowla, Pascal Jabbour, Arundhati Biswas, Frédéric Clarençon, James E Siegler, Thanh N Nguyen, Ricardo Varela, Amanda Baker, Muhammed Amir Essibayi, David Altschul, Nestor R Gonzalez, Markus A Möhlenbruch, Vincent Costalat, Benjamin Gory, Christian Paul Stracke, Mohammad Ali Aziz-Sultan, Constantin Hecker, Hamza Shaikh, David S Liebeskind, Alessandro Pedicelli, Andrea M Alexandre, Illario Tancredi, Tobias D Faizy, Erwah Kalsoum, Boris Lubicz, Aman B Patel, Vitor Mendes Pereira, Adrien Guenego and Adam A Dmytriw in European Stroke Journal
Supplemental material, sj-docx-2-eso-10.1177_23969873241249295 for Outcomes of mechanical thrombectomy in anticoagulated patients with acute distal and medium vessel stroke by Hamza Salim, Basel Musmar, Nimer Adeeb, Vivek Yedavalli, Dhairya Lakhani, Sahibjot Singh Grewal, Kareem El Naamani, Nils Henninger, Sri Hari Sundararajan, Anna Luisa Kühn, Jane Khalife, Sherief Ghozy, Luca Scarcia, Benjamin YQ Tan, Robert W Regenhardt, Jeremy J Heit, Nicole M Cancelliere, Joshua D Bernstock, Aymeric Rouchaud, Jens Fiehler, Sunil Sheth, Ajit S Puri, Christian Dyzmann, Marco Colasurdo, Xavier Barreau, Leonardo Renieri, João Pedro Filipe, Pablo Harker, Răzvan Alexandru Radu, Mohamad Abdalkader, Piers Klein, Thomas R Marotta, Julian Spears, Takahiro Ota, Ashkan Mowla, Pascal Jabbour, Arundhati Biswas, Frédéric Clarençon, James E Siegler, Thanh N Nguyen, Ricardo Varela, Amanda Baker, Muhammed Amir Essibayi, David Altschul, Nestor R Gonzalez, Markus A Möhlenbruch, Vincent Costalat, Benjamin Gory, Christian Paul Stracke, Mohammad Ali Aziz-Sultan, Constantin Hecker, Hamza Shaikh, David S Liebeskind, Alessandro Pedicelli, Andrea M Alexandre, Illario Tancredi, Tobias D Faizy, Erwah Kalsoum, Boris Lubicz, Aman B Patel, Vitor Mendes Pereira, Adrien Guenego and Adam A Dmytriw in European Stroke Journal
Supplemental material, sj-docx-3-eso-10.1177_23969873241249295 for Outcomes of mechanical thrombectomy in anticoagulated patients with acute distal and medium vessel stroke by Hamza Salim, Basel Musmar, Nimer Adeeb, Vivek Yedavalli, Dhairya Lakhani, Sahibjot Singh Grewal, Kareem El Naamani, Nils Henninger, Sri Hari Sundararajan, Anna Luisa Kühn, Jane Khalife, Sherief Ghozy, Luca Scarcia, Benjamin YQ Tan, Robert W Regenhardt, Jeremy J Heit, Nicole M Cancelliere, Joshua D Bernstock, Aymeric Rouchaud, Jens Fiehler, Sunil Sheth, Ajit S Puri, Christian Dyzmann, Marco Colasurdo, Xavier Barreau, Leonardo Renieri, João Pedro Filipe, Pablo Harker, Răzvan Alexandru Radu, Mohamad Abdalkader, Piers Klein, Thomas R Marotta, Julian Spears, Takahiro Ota, Ashkan Mowla, Pascal Jabbour, Arundhati Biswas, Frédéric Clarençon, James E Siegler, Thanh N Nguyen, Ricardo Varela, Amanda Baker, Muhammed Amir Essibayi, David Altschul, Nestor R Gonzalez, Markus A Möhlenbruch, Vincent Costalat, Benjamin Gory, Christian Paul Stracke, Mohammad Ali Aziz-Sultan, Constantin Hecker, Hamza Shaikh, David S Liebeskind, Alessandro Pedicelli, Andrea M Alexandre, Illario Tancredi, Tobias D Faizy, Erwah Kalsoum, Boris Lubicz, Aman B Patel, Vitor Mendes Pereira, Adrien Guenego and Adam A Dmytriw in European Stroke Journal
Supplemental material, sj-docx-4-eso-10.1177_23969873241249295 for Outcomes of mechanical thrombectomy in anticoagulated patients with acute distal and medium vessel stroke by Hamza Salim, Basel Musmar, Nimer Adeeb, Vivek Yedavalli, Dhairya Lakhani, Sahibjot Singh Grewal, Kareem El Naamani, Nils Henninger, Sri Hari Sundararajan, Anna Luisa Kühn, Jane Khalife, Sherief Ghozy, Luca Scarcia, Benjamin YQ Tan, Robert W Regenhardt, Jeremy J Heit, Nicole M Cancelliere, Joshua D Bernstock, Aymeric Rouchaud, Jens Fiehler, Sunil Sheth, Ajit S Puri, Christian Dyzmann, Marco Colasurdo, Xavier Barreau, Leonardo Renieri, João Pedro Filipe, Pablo Harker, Răzvan Alexandru Radu, Mohamad Abdalkader, Piers Klein, Thomas R Marotta, Julian Spears, Takahiro Ota, Ashkan Mowla, Pascal Jabbour, Arundhati Biswas, Frédéric Clarençon, James E Siegler, Thanh N Nguyen, Ricardo Varela, Amanda Baker, Muhammed Amir Essibayi, David Altschul, Nestor R Gonzalez, Markus A Möhlenbruch, Vincent Costalat, Benjamin Gory, Christian Paul Stracke, Mohammad Ali Aziz-Sultan, Constantin Hecker, Hamza Shaikh, David S Liebeskind, Alessandro Pedicelli, Andrea M Alexandre, Illario Tancredi, Tobias D Faizy, Erwah Kalsoum, Boris Lubicz, Aman B Patel, Vitor Mendes Pereira, Adrien Guenego and Adam A Dmytriw in European Stroke Journal