Abstract
Introduction
Femoral neck fractures (FNF) represent a significant challenge in orthopedic practice, demanding prompt intervention to restore function and mobility in affected individuals. Numerous surgical interventions have been developed to address these fractures, including internal fixation with devices such as the Femoral Neck System (FNS, DePuy Synthes, Inc., West Chester, PA, USA). However, the optimal fixation system remains unclear. Understanding the postoperative outcomes associated with these interventions is crucial for optimizing patient care and informing treatment decisions.
Significance
This PRISMA-compliant systematic literature review evaluates the efficacy and safety of the Femoral Neck System relative to other operative treatment options. Clinical and safety outcomes included mortality, perioperative complications, postoperative complications at 1 year, and reoperation.
Results
A total of 117 studies with 68,567 patients with FNF treated with internal fixation were identified. Of these, thirteen included FNS as a treatment arm (1078 patients). Due to heterogeneity in study designs and populations, only the eleven studies that directly compared FNS to other operative treatments, and 2 non-comparative studies that treated with FNS were included in the systematic review. Seven of the eleven included studies had high risk of bias, 2 had moderate risk of bias, and 2 had low risk of bias. FNS groups had similar or significantly lower incidences of postoperative complications, reoperations, and mortality compared to cannulated screw, cancellous screw, or dynamic or sliding hip screw groups in all studies.
Conclusion
FNS can be a safe and effective operative treatment option for FNF. Safety outcomes and reoperation rates are comparable between patients treated with FNS and patients treated with cannulated screws, cancellous screws, and dynamic or sliding hips screws. Future prospective, controlled studies are needed to confirm the safety and efficacy of FNS relative to other operative treatment options.
Keywords: femoral neck fracture, femoral neck system, hip fracture, dynamic screws
Introduction
Femoral neck fractures (FNF), the most common hip fracture, 1 are frequently treated with internal fixation, but complications frequently arise, which may require reoperation. 2 Recently, a new fixation device, Femoral Neck System (FNS, DePuy Synthes, Inc., West Chester, PA, USA) was launched for treatment of femoral neck fractures, including basilar, transcervical, and subcapital fractures, in adults and adolescents (age 12-21 years) in which the growth plates have fused or will not be crossed (Figure 1). FNS was developed to reduce complications and reoperations by increasing construct stability, reducing surgical invasiveness, and reducing the risk of lateral implant protrusion. 3 The FNS design compensated for 15 mm of femoral neck shortening without lateral protrusion by a telescoping mechanism. 3 Moreover, a single insertion handle allows for placement of the central bolt as well as the antirotation screw to reduce procedural complexity and enhance operational efficiency. 3 The bolt is currently available in units of 5 mm and a technical note has reported a modified technique for improved control of the depth of the bolt. 4
Figure 1.
Three dimensional models of the FNS device. Used with permission.
Mechanical testing of FNS with standardized foam models has indicated up to 40% increased rotational stability compared to a sliding hip screw (SHS), and a minimum of 150% more rotational stability compared to a 3 cannulated screw.5,6 A biomechanical study in a cadaveric model found that FNS had comparable stability to dynamic hip screws paired with antirotation screws or blades and superior stability compared to 3 cannulated screws for treating femoral neck fractures. 7 However, the relative safety and efficacy of FNS compared to other treatment options remain undetermined. Here, we report the results of a systematic literature review to evaluate safety and efficacy outcomes associated with FNS relative to traditional operative treatment options in femoral neck fractures resulting from any mechanism of injury.
Methods
Literature Search and Study Selection
This study adheres to PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) guidelines. 8 The PRISMA checklist associated with this systematic review can be found in Supplemental Files 1 and 2. A protocol was prepared based on the PROSPERO protocol guidelines. The review was not registered. Searches of PubMed were completed using the Application Program Interface (API) in the AutoLit platform (Nested Knowledge, nested-knowledge.com). All study metadata and abstracts from the search results were also obtained via API. Searches of Cochrane Library and Embase databases were completed through their respective web interfaces and the results were uploaded to the AutoLit platform. Searches were restricted to studies published after January 1, 2012 to capture the previous decade of comparative treatments and cover the date that FNS came on the market in 2017. Search terms included the phrases “femoral neck fracture”, “femoral neck system”, “sliding hip screw”, “cannulated screw”, and “internal fixation”. The full search strings are available in Supplemental Table 1.
Identified studies were evaluated for inclusion in the systematic review. Study inclusion criteria included those reporting adult patients with femoral neck fracture treated with FNS. All mechanisms of injury were included. Exclusion criteria were studies that did not report patients treated with FNS, studies that did not report the outcomes of interest, studies that did not separate patient outcomes by intervention, studies with less than 5 patients, studies that did not relate to femoral neck fracture, studies not reporting interventions or outcomes of interest, and studies reporting on a subpopulation that could introduce bias, including studies that focused on patients with cancer, HIV, or Parkinson’s disease. In vivo/in vitro studies, symposium/conferences, qualitative review articles, letters of correspondence, in silico study/mathematical models, guideline articles, technical notes, editorial/opinion articles, meta-analyses or systematic reviews, secondary analyses, protocols, studies not written in English, or interim analyses were also excluded. The reference lists of identified articles were also screened for potentially relevant papers. Each study was screened by a single investigator.
Data Extraction
Data was extracted by a single investigator for each study and reviewed by 2 independent investigators. Patient characteristics included age and fracture stability (Garden classification). Procedure characteristics included length of operation, intraoperative blood loss, and length of hospital stay. Methods for measuring blood loss vary widely, potentially introducing heterogeneity into the data. Intraoperative blood loss was extracted as reported in the study. Clinical and safety outcomes included mortality, perioperative complications (deep vein thrombosis [DVT] and perioperative surgical site infection), postoperative complications at 1 year (avascular necrosis [AVN] of the femoral head, non-union, internal fixture loosening, postoperative surgical site infection, hematoma, iatrogenic fracture, and femoral neck shortening), and reoperation (unspecified, implant removal, or conversion to another treatment).
Risk of Bias
Risk of bias (RoB) was assessed for comparative studies using the Newcastle-Ottawa Scale. 9 Criteria for rating a study as low, moderate, or high risk of bias were made based on the decision rules described by Sharmin et al, 10 outlined in Supplemental Table 2. The RoB was completed independently by 2 reviewers with any disagreements adjudicated by a third reviewer.
Statistical Analysis
Due to heterogeneity in data and the limited number of multi-armed studies available that distinguished between patients with acute and delayed instrumentation, inferential statistics were not performed, and data are expressed as descriptive statistics only. Statistics are reported as counts and percentages, median (interquartile range (IQR)), or mean ± standard deviation (SD).
Results
Literature Search Results
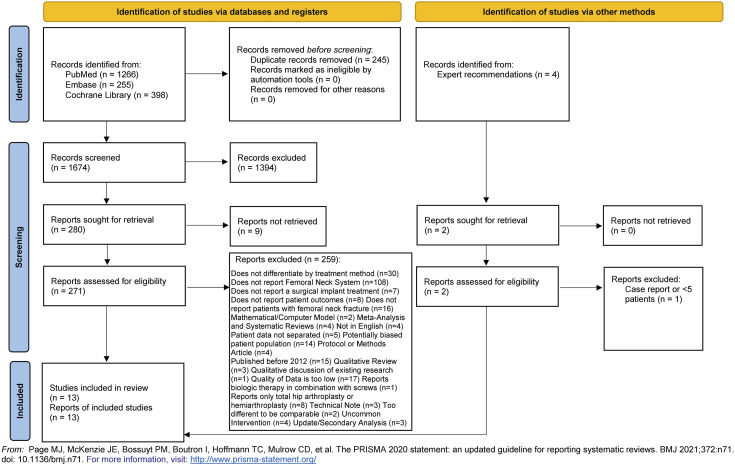
Our searches identified 1674 individual studies. Of the identified studies, 1394 were excluded based on title and abstract review (see PRISMA flowchart in Figure 2). The remaining 271 articles underwent full-text review. Four articles were identified through expert recommendation, which also underwent full-text review. Nine articles did not have full texts available, and 259 articles were excluded for other reasons, while 108 studies reported a comparable intervention but did not report patients treated with FNS (see PRISMA flowchart in Figure 2). Due to heterogeneity in study designs and populations, only the 13 studies that included patients treated with FNS were included in the systematic review.11-23 Results from all 117 studies reporting either FNS or a comparable intervention are summarized in Supplemental Tables 3-6. Of the 13 studies reporting FNS, all were retrospective cohort studies.11-23 Three studies compared dynamic or sliding hip screws or cannulated screws to FNS,16,17,20 2 studies had a single intervention of FNS with no comparator,12,18 1 study compared dynamic or sliding hip screws or cancellous screws to FNS, 21 1 study compared dynamic or sliding hip screws to FNS, 16 and 6 studies compared cannulated screws to FNS.13-15,19,22,23 Two studies were found to have low risk of bias,19,23 2 had moderate risk of bias,13,16 and 7 had high risk of bias.11,14,15,17,20-22 The 2 non-comparative studies were not included in the risk of bias (Supplemental Table 7)
Figure 2.
PRISMA study selection flowchart.
FNS vs Cannulated Screws
Study Characteristics
Seven studies compared FNS against cannulated screws.13-15,19,20,22,23 Of these, Vazquez et al 20 compared a third treatment such that head-to-head comparisons between FNS and cannulated screws were not made. Nibe et al 15 and Zhang et al 22 restricted study patients to ≥65 years old and Vazquez et al 20 reported outcomes in patients ≥75 years old. Hu et al restricted to patients under 60 years old. 14 Zhang et al 22 restricted their study to patients with AO31-B type fractures, which include Garden Type II, III, and IV, Zhou et al 23 reported only patients with Pauwels Type III fractures, and Vazquez et al 20 restricted their study to patients with Garden Type I and II fractures. Two studies did not apply fracture type or age-based selection criteria, but excluded pathological fractures.13,19
Three studies did not specify mechanism of injury.14,19,20 In He et al, the majority of fractures were caused by falls in both groups (63.6% [21/33] in patients treated with FNS and 69.4% [25/36] in patients treated with cannulated screws). 13 In Nibe et al, the majority of fractures were caused by low-energy falls in both groups (88.0% [22/25] in patients treated with FNS and 81.5% [22/27] in patients treated with cannulated screws). The remaining fractures were caused by traffic accidents (8.0% [2/25] in patients treated with FNS only), other high-energy injuries (3.7% [1/27] in patients treated with cannulated screws only) or unknown causes (4.0% [1/25] in patients treated with FNS and 14.8% [4/27] in patients treated with cannulated screws). 15 In Zhou et al, fractures were caused by traffic accidents or falls and pathological fractures were excluded. 23
Two studies had low risk of bias,19,23 1 had moderate risk of bias, 13 and 4 had high risk of bias.14,15,20,22 Common sources of risk of bias were selection bias, lack of comparability between groups, and short follow-up. A summary of risk of bias assessments can be found in Supplemental Table 7.
Patient Baseline Characteristics
Patient baseline characteristics are presented in Supplemental Table 3. Across studies, the average age ranged from 47.6 ± 10.3 13 to 85.0 ± 6.6 20 for patients with cannulated screws, and from 50.5 ± 8.5 14 to 86.1 ± 4.6 20 for patients with FNS. No studies reported statistically significant differences in age between groups. Only Nibe et al 15 and Zhou et al 23 did not present Garden classification. Except for Vazquez et al, 20 in which most injuries were Type I, most injuries were Type II or above. No study reported significant differences for Garden classification between groups. Most studies had follow-up periods >12 months, but Vazquez et al 20 had follow-ups from 1-6 months and Zhou et al 23 had follow-ups from 10-22 months. The longest follow-up period was a range of 14-24 months. 19
Procedure Characteristics
Procedure characteristics are presented in Table 1. The average length of operation ranged from 40.9 ± 5.2 23 to 76.8 ± 13.1 22 minutes for cannulated screws, and from 42.0 ± 13.0 15 to 79.8 ± 26.4 14 for FNS. Compared to cannulated screws, 2 studies reported lower mean operation time in patients treated with FNS,15,22 but 1 study reported significantly higher mean operation time (Table 1). 14 Four studies reported intraoperative blood loss, ranging from 23.7 ± 28.1 14 to 47.3 ± 9.3 mL 19 for cannulated screws and from 36.0 ± 25.0 15 to 99.7 ± 52.7 mL 23 for FNS. Two studies reported significantly higher intraoperative blood loss in patients treated with FNS compared to cannulated screws, but both studies also reported that patients treated with FNS had lower incidence of complications, indicating that the difference in blood loss may not be clinically significant.14,23 All but Hu et al 14 and Nibe et al 15 reported length of hospital stay. No studies reported significant differences in length of hospital stay between patients treated with FNS and cannulated screws. Studies that restricted study patients to ≥65 years old found that FNS had significantly lower operation time and no significant differences in intraoperative blood loss or hospital stay compared to cannulated screws.15,20,22
Table 1.
Procedure Characteristics.
| Study | Intervention | N | Length of Operation (minutes) | P value | Intraoperative Blood Loss (mL) | P value | Length of Hospital Stay (days) | P value | Reported Conclusions |
|---|---|---|---|---|---|---|---|---|---|
| He, 2021 13 | Cannulated screw | 36 | 56.1 ± 12.5 | 0.062 a | -- | -- | 4.8 ± 1.6 | 0.410 a | The interventions had no significant differences in procedural characteristics |
| FNS (DePuy synthes) | 33 | 49.9 ± 14.5 | -- | 5.1 ± 1.9 | |||||
| Hu, 2021 14 | Cannulated screw | 24 | 64.6 ± 18.6 | 0.031 a | 23.7±28.1 | <0.001 a | -- | -- | FNS had a higher length of operation and intraoperative blood loss |
| FNS (DePuy synthes) | 20 | 79.8 ± 26.4 | 69.5±50.5 | -- | |||||
| Nibe, 2021 15 | Cannulated screw | 27 | 53 ± 21 | 0.032 a | 41±40 | 0.58 a | -- | -- | FNS had a lower length of operation and intraoperative blood loss |
| FNS (DePuy synthes) | 25 | 42 ± 13 | 36±25 | -- | |||||
| Tang, 2021 19 | Cannulated screw | 45 | 42 ± 11.9 | 0.590 b | 47.3±9.3 | 0.284 b | 4.8 ± 1.4 | 0.113 b | The interventions had no significant differences in procedural characteristics |
| FNS (DePuy synthes) | 47 | 52.4 ± 11.0 | 50.6 ± 10.6 | 5.5 ± 1.3 | |||||
| Vazquez, 2021 20 | Cannulated screw | 32 | 66.9 ± 25.4 | <0.001 c | -- | -- | 12.2 ± 6.2 | 0.131 d | FNS had a lower length of operation |
| Dynamic or sliding hip screw | 16 | 70.7 ± 20.0 | -- | 12.4 ± 5.3 | |||||
| FNS (DePuy synthes) | 15 | 43.3 ± 10.1 | -- | 10.3 ± 6.0 | |||||
| Zhang, 2022 22 | Cannulated screw | 36 | 76.81 ± 13.10 | 0.000 a | -- | -- | 8.5 ± 1.95 | 0.082 a | FNS had a lower length of operation |
| FNS (DePuy synthes) | 33 | 60.00 ± 12.44 | -- | 7.57 ± 2.39 | |||||
| Zhou, 2021 23 | Cannulated screw | 51 | 40.9 ± 5.2 | 0.122 a | 30.27 ± 9.04 | <0.001 a | 5.3 ± 1.5 | 0.133 a | FNS had a higher intraoperative blood loss |
| FNS (DePuy synthes) | 30 | 42.8 ± 4.7 | 99.73 ± 52.73 | 5.1 ± 1.3 | |||||
| Niemann, 2022 16 | Dynamic or sliding hip screw | 19 | 91.68 ± 23.96 | <0.01 e | -- | -- | 7.35 ± 3.43 | 0.94 e | FNS had a lower length of operation |
| FNS (DePuy synthes) | 12 | 54 ± 26.1 | -- | 8 ± 5.27 | |||||
| Schuetze, 2022 17 | Dynamic or sliding hip screw | 108 | 54.7 ± 17.4 | <0.05 f | -- | -- | 11.3 ± 6.8 | <0.05 f | FNS had a lower length of operation and length of hospital stay |
| FNS (DePuy synthes) | 113 | 36.3 ± 11.6 | -- | 8.9 ± 4.3 | |||||
| Xu, 2022 21 | Cancellous screw | 51 | 49 (38-61) | <0.001 d | 30 (20-45) | <0.001 d | 3 (2-4) | <0.001 d | FNS had a lower length of operation, intraoperative blood loss, and length of hospital stay |
| Dynamic or sliding hip screw | 52 | 72 (55-88.75) | 50 (30-50) | 3.5 (3-6) | |||||
| FNS (DePuy synthes) | 54 | 45 (40-59) | 30 (20-50) | 2 (2-4) | |||||
| Cintean, 2021 11 | FNS (DePuy synthes) | 29 | -- | -- | -- | -- | 9.8 ± 3.8 | <0.001 e | FNS had a lower length of hospital stay |
| Hemiarthroplasty | 34 | -- | -- | 15.1 ± 5.1 | |||||
| Non-comparative studies | |||||||||
| Davidson, 2022 12 | FNS (DePuy synthes) | 102 | 44 ± 14 | -- | 51 ± 47 | -- | 5.7 ± 3.9 | -- | No comparison between interventions |
| Stassen, 2021 18 | FNS (DePuy synthes) | 34 | Mean: 33 (95% CI: 29.3-36.9) | -- | Mean: 34 (95% CI: 24.7-44.6) | -- | 4 ± 2.8 | -- | No comparison between interventions |
Data are expressed as mean ± SD or median (IQR). “--” indicates no data reported.
aIndependent-samples t test.
bAnalysis unclear (either Mann-Whitney U test or independent-samples t test).
cLinear regression.
dKruskal-Wallis test.
eMann-Whitney U test.
fStatistical methods not clearly reported.
Patient Outcomes
Patient outcomes are presented in Table 2. No significant differences between FNS and cannulated screws were reported for non-union events,13-15,19 loosening or failure of the internal fixture,13,15,19 avascular necrosis,14,19,23 deep vein thrombosis,19,23 or mortality.20,22 Hu et al 14 found that significantly more cannulated screw patients experienced femoral neck shortening than FNS patients (9/24 vs 2/20, P = 0.04), but Zhang et al 22 found no significant difference between groups (5/36 vs 2/33, P = 0.28). He et al 13 found that 8.3% (3/36) of cannulated screw patients and 3.0% (1/33) of FNS patients experienced femoral neck shortening, but did not report a statistical analysis. Nibe et al 15 found significantly more reoperations for cannulated screw patients than FNS patients (6/21 vs 0/25, P = 0.23). Three other studies reported incidence of reoperation,20,22,23 but no other study reported a statistical analysis. Studies that restricted study patients to ≥65 years old found that FNS had significantly lower incidence of reoperation compared to cannulated screws, with no other significant differences.15,20,22
Table 2.
Patient Outcomes.
| Study | Intervention | N | Non-union | Internal Fixture Loosening/Failure | Other Postoperative Complications | Reoperation | Mortality | P values | Reported Conclusions |
|---|---|---|---|---|---|---|---|---|---|
| He, 2021 13 | Cannulated screw | 36 | 5.6% (2/36) | 8.3% (3/36) | Femoral neck shortening: 8.3% (3/36) | -- | -- | -- | FNS had a lower incidence of overall complications (combining non-union, nail retreat, femoral neck shortening, and internal fixation cutout) |
| FNS (DePuy synthes) | 33 | 0.0% (0/33) | 3.0% (1/33) | Femoral neck shortening: 3.0% (1/33) | -- | -- | |||
| Hu, 2021 14 | Cannulated screw | 24 | 12.5% (3/24), P = 0.795 | -- | AVN: 12.5% (3/24), Femoral neck shortening: 4.54±2.75 mm 37.5% (9/24) |
-- | -- | AVN: P = 0.389
a
Femoral neck shortening length: P = 0.005 b Femoral neck shortening incidence: P = 0.036 a |
FNS had a lower degree of femoral neck shortening and a lower incidence femoral neck shortening, but no difference in incidence of non-union or AVN. |
| FNS (DePuy synthes) | 20 | 10.0% (2/20) | -- | AVN: 5.0% (1/20) Femoral neck shortening: 2.40±1.81 mm 10.0% (2/20) |
-- | -- | |||
| Nibe, 2021 15 | Cannulated screw | 27 | 18.5% (5/27) | 7.4% (2/27) | -- | Overall: 28.6% (6/21) Conversion to HA: 11.1% (3/27) Implant removal: 11.1% (3/27) |
-- | Non-union: P = 0.052
c
Overall reoperation: P = 0.023 c |
FNS had a significantly lower incidence of reoperation |
| FNS (DePuy synthes) | 25 | 0.0% (0/25) | -- | -- | 0.0% (0/25) | -- | |||
| Tang, 2021 19 | Cannulated screw | 45 | 8.9% (4/45) | 11.1% (5/45) | AVN: 6.7% (3/45) DVT: 0.0% (0/45) |
-- | -- | Non-union: P = 0.430
a
Internal fixture loosening/failure: P = 0.481 a AVN: P = 0.356 a |
The interventions had no significant differences in patient outcomes |
| FNS (DePuy synthes) | 47 | 4.3% (2/47) | 6.4% (3/47) | AVN: 2.1% (1/47) DVT: 0.0% (0/47) |
-- | -- | |||
| Vazquez, 2021 20 | Cannulated screw | 32 | -- | -- | 3.1% (1/32) | 9.4% (3/32) | Mortality: P = 0.585 c | The interventions had no significant differences in patient outcomes | |
| Dynamic or sliding hip screw | 16 | -- | -- | -- | 0.0% (0/16) | 12.5% (2/16) | |||
| FNS (DePuy synthes) | 15 | -- | -- | -- | 0.0% (0/15) | 0.0% (0/15) | |||
| Zhang, 2022 22 | Cannulated screw | 36 | -- | -- | Femoral neck shortening: 13.89% (5/36) | Implant removal: 13.89% (5/36) | 0.0% (0/36) | Femoral neck shortening: P = 0.282
a
Implant removal: P = 0.026 a |
FNS had a lower incidence of implant removal |
| FNS (DePuy synthes) | 33 | -- | -- | Femoral neck shortening: 6.06% (2/33) | Implant removal: 0.0% (0/33) | 0.0% (0/33) | |||
| Zhou, 2021 23 | Cannulated screw | 51 | -- | -- | AVN: 0.0% (1/51) DVT: 0.0% (0/51) |
Conversion to HA: 3.9% (2/51) | -- | -- | FNS had a lower incidence of overall complications |
| FNS (DePuy synthes) | 30 | -- | -- | AVN: 0.0% (0/30) DVT: 0.0% (0/30) |
Conversion to HA: 3.3% (1/30) | -- | |||
| Niemann, 2022 16 | Dynamic or sliding hip screw | 19 | -- | -- | AVN: 0.0% (0/19) Femoral neck shortening: 0.0% (0/19) Femoral neck shortening: 0.0% (0/12) |
-- | -- | -- | The interventions had no significant differences in patient outcomes |
| FNS (DePuy synthes) | 12 | -- | -- | AVN: 0.0% (0/12) | -- | -- | -- | ||
| Schuetze, 2022 17 | Dynamic or sliding hip screw | 108 | -- | 10.2% (11/108) | Femoral neck shortening: 4.8±2.1 mm 27.7% (30/108) Hematoma: 5.6% (6/108) Surgical site infection: 2.8% (3/108) |
Conversion to THA: 8.3% (9/108) Implant removal: 1.9% (2/108) |
0.9% (1/108) | Failure, hematoma, or infection: P = 0.479
d
Femoral neck shortening: 0.455 d Mortality: >0.05 d |
The interventions had no significant differences in patient outcomes |
| FNS (DePuy synthes) | 113 | -- | 12.4% (14/113) | Femoral neck shortening: 5.3±1.9 mm 27.4% (31/113) Hematoma: 0.9% (1/113) Surgical site infection: 0.0% (0/113) |
Conversion to THA: 11.5% (13/113) Implant removal: 0.9% (1/113) |
3.5% (4/113) | |||
| Xu, 2022 21 | Cancellous screw | 51 | -- | 3.9% (2/51) | AVN: 0.0% (0/51) DVT: 0.0% (0/51) Femoral neck shortening: 1.9 mm (0.2-3.5) |
-- | -- | Internal fixture loosening/failure: P = 1.000
c
Femoral neck shortening: P = 0.452 e |
The interventions had no significant differences in patient outcomes |
| Dynamic or sliding hip screw | 52 | -- | 3.8% (2/52) | AVN: 0.0% (0/52) DVT: 0.0% (0/52) Femoral neck shortening: 2.0 mm (0.2-4.8) |
-- | -- | |||
| FNS (DePuy synthes) | 54 | -- | 5.6% (3/54) | AVN: 0.0% (0/54) DVT: 0.0% (0/54) Femoral neck shortening: 2.2 mm (0.4-4.1) |
-- | -- | |||
| Cintean, 2021 11 | FNS (DePuy synthes) | 29 | -- | -- | AVN: 0.0% (0/21) Femoral neck shortening: 3.3±4.5 mm, 100.0% (21/21) |
Overall: 13.8% (4/29) Conversion to hemiarthroplasty: 10.3% (3/29) Removal of implant: 3.4% (1/29) |
6.9% (2/29) | Mortality: P = 0.663 c | The interventions had no significant difference in patient outcomes |
| Hemiarthroplasty | 34 | -- | -- | -- | Overall: 8.8% (3/34) Conversion to HA: 2.9% (1/34) |
8.8% (3/34) | |||
| Non-comparative studies | |||||||||
| Davidson, 2022 12 | FNS (DePuy synthes) | 102 | 1.0% (1/102) | 1.0% (1/102) | AVN: 2.9% (3/102) | Conversion to THA: 8.8% (9/102) | 0.0% (0/102) | -- | No comparison between interventions |
| Stassen, 2021 18 | FNS (DePuy synthes) | 34 | -- | 5.9% (2/34) | AVN: 11.8% (4/34) | Conversion to THA: 17.6% (6/34) Implant removal: 5.9% (2/34) |
0.0% (0/34) | -- | No comparison between interventions |
Data are expressed as mean ± SD, median (IQR), or % (n) unless otherwise indicated. “--“ indicates no data reported.
AVN = avascular necrosis; DVT = deep vein thrombosis; FNS = Femoral Neck System; HA = hip arthroplasty; THA = total hip arthroplasty.
aChi-squared test of independence.
bIndependent-samples t-test.
cFisher's exact test.
dStatistical methods not clearly reported.
eKruskal-Wallis test.
FNS vs Dynamic or Sliding Hip Screw
Study Characteristics
Four studies compared FNS with dynamic or sliding hip screws.16,17,20,21 Of these, Vazquez et al 20 and Xu et al 21 compared a third treatment such that head-to-head comparisons between FNS and cannulated screws were not made. Three studies applied age-related inclusion criteria: Vazquez et al 20 (≥75 years old), Schuetze et al 17 (≥50 years old) and Xu et al 21 (<65 years old). Vazquez et al 20 and Xu et al 21 restricted their studies to patients with Garden Type I and II fractures. Niemann et al 16 and Schuetze et al 17 excluded pathological fractures. No studies specified mechanism of injury. One study had moderate risk of bias 16 and 3 studies had high risk of bias.17,20,21 Common sources of risk of bias included selection bias, failure to account for imbalances in important patient characteristics between cohorts, short follow-up, and failure to properly adjust analyses for imbalances in follow-up periods between cohorts. A summary of risk of bias assessments can be found in Supplemental Table 7.
Patient Baseline Characteristics
Across studies, the average age ranged from 60.5 ± 17 16 to 83.4 ± 7.3 years 20 for patients with dynamic or sliding hip screw, and from 60.7 ± 15.2 21 to 86.1 ± 4.6 years 21 for FNS patients. No study found significant differences in age between groups. Likewise, no study reported significant differences in Garden classification between groups. Follow-up periods ranged from 7.4 ± 3.4 days 16 to 12-16 months. 21 No study reported significant differences for follow-up periods between groups (Supplemental Table 3).
Procedure Characteristics
The average duration of operation ranged from 54.7 ± 17.4 17 to 91.7 ± 24.0 minutes 16 for dynamic or sliding hip screw patients, and from 36.3 ± 11.6 17 to 54.0 ± 26.1 minutes 16 for FNS patients. In each study, FNS had significantly shorter operation time than dynamic or sliding hip screws.16,17,20,21 Only Xu et al 21 reported on intraoperative blood loss; dynamic or sliding hip screws operations had significantly more blood loss than FNS (median, range: 50, 30-50 vs median, range: 30, 20-50; P < 0.01). Length of hospital stay ranged from 3-6 21 to 12.4 ± 5.3 days 20 for dynamic or sliding hip screws and from 2-4 21 to 10.3 ± 6.0 days 20 for FNS. Only Schuetze et al 17 and Xu et al 21 found significant differences for length of hospital stay between groups; in both cases, FNS patient stays were significantly shorter than dynamic or sliding hip screw patient stays (Table 1).
Patient Outcomes
No study reported incidence of non-union. No significant differences between FNS and dynamic or sliding hip screws were reported for loosening or failure of the internal fixure,17,21 avascular necrosis,17,21 deep vein thrombosis, 21 femoral neck shortening,16,17,21 hematoma or surgical site infection, 17 reoperation,17,20 or mortality17,20 (Table 2).
FNS vs Other Comparators
Xu et al 21 compared FNS with cancellous screws. The study excluded patients >65 years old who had Garden Type III or IV fractures or pathological fractures and did not specify mechanisms of injury. The study had a high risk of bias, primarily due to selection bias, failure to account for imbalances in important patient characteristics between cohorts, short follow-up, and failure to properly adjust analyses for imbalances in follow-up periods between cohorts. Xu et al 21 used linear regression that included a third procedure such that head-to-head comparisons were not made, median operation time, blood loss, and length of hospital stay were lower for FNS than cancellous screws (Table 1). No differences in patient outcomes were reported between the FNS and cancellous screws (Table 2).
Cintean et al 11 compared FNS with hemiarthroplasty. The study did not apply age-based selection criteria and did not specify mechanisms of injury. The study had high risk of bias due to lack of comparability between the groups, short follow-up, and loss of patients to follow-up. There were no significant differences between groups for age, Garden classification, or follow-up period (Supplemental Table 3). Cintean et al 11 found that length of hospital stay was significantly shorter for FNS than hemiarthroplasty (Table 1), but did not find any differences in patient outcomes (Table 2).
Non-Comparative Studies
There were 2 non-comparative studies of FNS.12,18 Davidson et al 12 excluded cases with pathological fractures and Stassen et al 18 excluded patients with polytrauma. Neither study applied age-related selection criteria or specified mechanism of injury. The average age in both studies was 63 years. In both studies, more than half of the fractures were at or below Garden Type II. The mean follow-up periods were 7 12 and 6 months 18 (Supplemental Table 3). Mean length of operations were 44 12 and 33 minutes. 18 Mean intraoperative blood-loss was 51 12 and 34 mL. 18 Average length of hospital stay was 5.7 ± 3.9 12 and 4.0 ± 2.8 days 18 (Table 1). Davidson et al 12 reported 1.0% (1/102) non-union events and 1.0% (1/102) patients with loosening/failure of internal fixtures, while Stassen et al 18 did not report on non-union events and reported 5.9% (2/34) patients with loosening or failure of internal fixtures. Avascular necrosis was reported in 2.9% (3/102) 12 and 11.8% (4/34) 18 cases. Davidson et al 12 reported that 8.8% (9/102) of cases were converted to hemiarthroplasty while Stassen et al 18 reported that 17.6% (6/34) were converted with another 5.9% (2/34) implants removed. Neither study reported any deaths12,18 (Table 2).
Discussion
The results of our systematic literature review suggest that FNS can be safely and effectively used to treat FNF compared to other operative treatments. The majority of studies reported no significant difference in patient outcomes including non-union,11,15,19 change in internal fixture loosening/failure,17,19,21,22 postoperative complications,11,16,17,23 reoperation, 11 and mortality,11,17,20 with respect to the comparator device. Studies identified significantly better outcomes associated with FNS compared to cannulated screws, for reduced femoral neck shortening length and incidence, 14 reduced incidence of reoperation, 15 and lower incidence of implant removal. 22 One study, a systematic review by Zhou et al, reported that FNS were associated with a significantly lower incidence of overall complications compared to those treated with cannulated screws. 23
The relative incidences of complications and mortality found in the thirteen studies reporting FNS are also comparable or lower than the incidences reported for comparators in the 104 comparator-only studies, supporting the conclusion that FNS is comparable to similar operative treatments. The 2 non-comparative studies found similar results when using FNS. These conclusions are also in line with previous systematic reviews comparing operative treatments, which have found that dynamic and sliding hip screws and cannulated cancellous screws are largely comparable with respect to safety outcomes.24,25 Recently, another case series was published reporting outcomes in 12 patients after treatment with FNS, which found higher rates of complications compared to previously reported incidences for comparators. 26 A larger case series recently reported a high incidence of femoral neck shortening in patients treated with FNS, with no effect on fracture healing. 27 However, a recent comparative study found no difference in incidence of complications between patients treated for femoral neck fractures with FNS or cancellous screws, while patients treated with FNS had significantly better joint function, 28 and another comparative study found that FNS was more effective compared to a dynamic compression locking plate system. 29 Future comparative studies are need to confirm the relative incidence of complications in patients treated with FNS and address considerations such as long-term stability and mobility, which may have different priorities in different patient populations, depending on age and activity.
Factors other than implant choice impact revision and conversion rates and incidence of AVN, potentially explaining the low effect size between groups. The use of computed tomography scans or magnetic resonance imagery, rather than basic X-rays, may improve diagnostic accuracy by allowing physicians to visualize the fracture more clearly. Different imaging methods and protocols for when patients received imaging may have contributed to heterogeneity in reported incidence AVN between studies and among patients in individual studies. Better visualization may lead to more accurate classification of fracture displacement, informing treatment decisions.30-32 Stable internal fixation is key to prevent non-union and allow for positive functional outcomes, especially in younger patients, who have higher functional demands 33 and a high rate reoperation and conversion to total hip arthroplasty. 34 Young patients with Pauwels Type III FNF specifically have increased likelihood of loss of reduction and non-union. 35 The use of adjunctive implants is currently uncommon, but combining established implants with other stabilizing measures may provide additional stability and improve patient functional outcomes, particularly in young patients with displaced fractures.36-39
A simplified classification scheme of stable vs unstable may also improve treatment decision-making. Current guidelines suggest classifying fractures as non-displaced (Garden Type I or II) or displaced (Garden Type III or IV). 40 Both non-displaced and displaced fractures may be treated with internal fixation in younger patients,33,41 but currently only non-displaced fractures are recommended to be treated with internal fixation in older patients. 40 However, Vazquez et al suggest that using implants, including FNS, cannulated screws, or dynamic or sliding hip screws, to treat displaced fractures in older patients can lead to positive safety outcomes and low rates of reoperation. 20
Reduction quality and implant placement were not consistently reported in the studies reviewed. Achieving excellent reduction, including open reduction if necessary, and using standardized intraoperative imaging to ensure correct implant placement can both lower the need for revision or conversion and lower the incidence of AVN.42-44 Reduction quality and measures of implant placement should be assessed during treatment and reported in further studies to enable future analyses to accurately compare implants.
Limitations
The primary limitation of our review was the lack of prospective studies on patients treated with FNS, particularly the lack of RCTs. Heterogeneity in study design and patient and procedure characteristics prevented a broader meta-analysis, including studies that did not report use of FNS. This variability is likely due to heterogeneity in trauma patients, as well as differences in study designs. Many data elements were reported inconsistently, especially perioperative and postoperative complications. As mentioned above, methods for measuring blood loss varied widely, introducing heterogeneity into the data and precludes a definitive conclusion. Variations in fracture classification, patient age, follow-up time, mechanism of injury, and data collection methodologies between studies likely contributed to the heterogeneity of the results. Additionally, over half of the included studies had high risk of bias. Lack of comparability between cohorts was a common source of risk of bias, likely due to the heterogenous nature of trauma patient presentation. Finally, all but 1 study 19 in this review did not have long enough follow-up for the outcomes of interest to occur, indicating a need for longer-term studies on FNF treatment with FNS to verify these findings.
Conclusions
FNS can be a safe and effective treatment for FNF, including in older patients, with published incidences of complications similar to comparable treatment options. Further studies are necessary to prospectively compare FNS to other operative treatments.
Supplemental Material
Supplemental Material for Evaluation of Post-Operative Outcomes of Femoral Neck Fracture Interventions: A Systematic Review by Erin Sheffels, Mariam Khalil, Kristen Hutchison, Nicole J. Hardy, Ranita Tarchand, John M. Pederson, Anjani Parikh, and Michael Blauth in Geriatric Orthopaedic Surgery & Rehabilitation
Supplemental Material for Evaluation of Post-Operative Outcomes of Femoral Neck Fracture Interventions: A Systematic Review by Erin Sheffels, Mariam Khalil, Kristen Hutchison, Nicole J. Hardy, Ranita Tarchand, John M. Pederson, Anjani Parikh, and Michael Blauth in Geriatric Orthopaedic Surgery & Rehabilitation
Supplemental Material for Evaluation of Post-Operative Outcomes of Femoral Neck Fracture Interventions: A Systematic Review by Erin Sheffels, Mariam Khalil, Kristen Hutchison, Nicole J. Hardy, Ranita Tarchand, John M. Pederson, Anjani Parikh, and Michael Blauth in Geriatric Orthopaedic Surgery & Rehabilitation
Acknowledgements
The authors acknowledge Superior Medical Experts and Nested Knowledge, Inc. for research and editorial assistance. The authors acknowledge Karl Holub, Stephen Mead, Jeffrey Johnson, and Darian Lehmann-Plantenberg for their design, development, and support of the Nested Knowledge meta-analytical software.
Appendix.
List of Abbreviations
- API
Application program interface
- AVN
avascular necrosis
- CT
computed tomography
- DVT
deep vein thrombosis
- FNF
femoral neck fracture
- FNS
femoral neck system
- IQR
interquartile range
- MRI
magnetic resonance imagery
- PRISMA
Preferred reporting items for systematic reviews and meta-analyses
- PROSPERO
International prospective register of systematic reviews
- RCT
randomized controlled trial
- RoB
risk of bias
- SHS
sliding hip screw
- SD
standard deviation
Author Contributions: ES contributed to the study design and drafted and revised the manuscript. MK, KH, and RT contributed to the data acquisition. NJH contributed to the study design and the acquisition and analysis of the data. JMP contributed to the study design, data analysis, and drafting and revision of the manuscript. AP and MB contributed to the conception and design of the study and the revision of the manuscript. All authors read and approved the final manuscript.
The author(s) declared the following potential conflicts of interest with respect to the research, authorship, and/or publication of this article: ES is employed by and hold equity in Superior Medical Experts. JMP is employed by and hold equity in Superior Medical Experts and Nested Knowledge. MK and RT are employed by Nested Knowledge. KH is employed by Superior Medical Experts and Nested Knowledge. NJH is employed by and holds equity in Nested Knowledge. AP and MB are employed by Johnson & Johnson (JnJ) and own stock in the company.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This study is sponsored by Johnson & Johnson.
Supplemental Material: Supplemental material for this article is available online.
Ethical Statement
Ethical Approval
Institutional Review Board approval and patient consent is not required for this study type.
Informed Consent
Not applicable.
ORCID iDs
Erin Sheffels https://orcid.org/0000-0001-8356-6517
Nicole J. Hardy https://orcid.org/0000-0002-1597-0371
References
- 1.Davidovitch RI, Jordan CJ, Egol KA, Vrahas MS. Challenges in the treatment of femoral neck fractures in the nonelderly adult. J Trauma. 2010;68(1):236-242. [DOI] [PubMed] [Google Scholar]
- 2.Lu-Yao GL, Keller RB, Littenberg B, Wennberg JE. Outcomes after displaced fractures of the femoral neck. A meta-analysis of one hundred and six published reports. J Bone Joint Surg Am. 1994;76(1):15-25. [DOI] [PubMed] [Google Scholar]
- 3.Femoral Neck System (FNS); 2023; https://www.jnjmedtech.com/en-US/product/femoral-neck-system. (Accessed May 05 2023). [Google Scholar]
- 4.Cha Y, Song JU, Yoo JI, et al. Improved control over implant anchorage under the use of the femoral neck system for fixation of femoral neck fractures: a technical note. BMC Muscoskel Disord. 2021;22(1):621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.DePuy Synthes Report: Static Cut through Rotation Test in Bone Foam. DePuy Synthes; 2016:0000165855. [Google Scholar]
- 6.DePuy Synthes Report: Static Cut through Rotation Test in Bone Foam. DePuy Synthes; 2018:0000277853. [Google Scholar]
- 7.Stoffel K, Zderic I, Gras F, et al. Biomechanical evaluation of the femoral neck system in unstable Pauwels III femoral neck fractures: a comparison with the dynamic hip screw and cannulated screws. J Orthop Trauma. 2017;31(3):131-137. [DOI] [PubMed] [Google Scholar]
- 8.Moher D, Liberati A, Tetzlaff J, Altman DG, PRISMA Group . Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. J Clin Epidemiol. 2009;62(10):1006-1012. [DOI] [PubMed] [Google Scholar]
- 9.Stang A. Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur J Epidemiol. 2010;25(9):603-605. [DOI] [PubMed] [Google Scholar]
- 10.Sharmin S, Kypri K, Khanam M, Wadolowski M, Bruno R, Mattick RP. Parental supply of alcohol in childhood and risky drinking in adolescence: systematic review and meta-analysis. Int J Environ Res Publ Health. 2017;14(3):287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Cintean R, Pankratz C, Hofmann M, Gebhard F, Schütze K. Early results in non-displaced femoral neck fractures using the femoral neck system. Geriatr Orthop Surg Rehabil. 2021;12:21514593211050153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Davidson A, Blum S, Harats E, et al. Neck of femur fractures treated with the femoral neck system: outcomes of one hundred and two patients and literature review. Int Orthop. 2022;46(9):2105-2115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.He C, Lu Y, Wang Q, et al. Comparison of the clinical efficacy of a femoral neck system versus cannulated screws in the treatment of femoral neck fracture in young adults. BMC Muscoskel Disord. 2021;22(1):994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hu H, Cheng J, Feng M, Gao Z, Wu J, Lu S. Clinical outcome of femoral neck system versus cannulated compression screws for fixation of femoral neck fracture in younger patients. J Orthop Surg Res. 2021;16(1):370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Nibe Y, Matsumura T, Takahashi T, Kubo T, Matsumoto Y, Takeshita K. A comparison between the femoral neck system and other implants for elderly patients with femoral neck fracture: a preliminary report of a newly developed implant. J Orthop Sci. 2021;27(4):876-880. Online ahead of print. [DOI] [PubMed] [Google Scholar]
- 16.Niemann M, Braun KF, Ahmad SS, Stöckle U, Märdian S, Graef F. Comparing perioperative outcome measures of the dynamic hip screw and the femoral neck system. Medicina (Kaunas). 2022;58(3):352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Schuetze K, Burkhardt J, Pankratz C, et al. Is new always better: comparison of the femoral neck system and the dynamic hip screw in the treatment of femoral neck fractures. Arch Orthop Trauma Surg. 2023;143(6):3155-3161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Stassen RC, Jeuken RM, Boonen B, Meesters B, de Loos ER, van Vugt R. First clinical results of 1-year follow-up of the femoral neck system for internal fixation of femoral neck fractures. Arch Orthop Trauma Surg. 2022;142(12):3755-3763. [DOI] [PubMed] [Google Scholar]
- 19.Tang Y, Zhang Z, Wang L, Xiong W, Fang Q, Wang G. Femoral neck system versus inverted cannulated cancellous screw for the treatment of femoral neck fractures in adults: a preliminary comparative study. J Orthop Surg Res. 2021;16(1):504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Vazquez O, Gamulin A, Hannouche D, Belaieff W. Osteosynthesis of non-displaced femoral neck fractures in the elderly population using the femoral neck system (FNS): short-term clinical and radiological outcomes. J Orthop Surg Res. 2021;16(1):477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Xu X, Fan J, Zhou F, et al. Comparison of femoral neck system to multiple cancellous screws and dynamic hip screws in the treatment of femoral neck fractures. Injury. 2022;2:S28-S35. online ahead of print. [DOI] [PubMed] [Google Scholar]
- 22.Zhang Y-Z, Lin Y, Li C, et al. A comparative analysis of femoral neck system and three cannulated screws fixation in the treatment of femoral neck fractures: a six-month follow-up. Orthop Surg. 2022;14(4):686-693. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Zhou XQ, Li ZQ, Xu RJ, et al. Comparison of early clinical results for femoral neck system and cannulated screws in the treatment of unstable femoral neck fractures. Orthop Surg. 2021;13(6):1802-1809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Xia Y, Zhang W, Zhang Z, Wang J, Yan L. Treatment of femoral neck fractures: sliding hip screw or cannulated screws? A meta-analysis. J Orthop Surg Res. 2021;16(1):54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Lim EJ, Shon H-C, Cho J-W, Oh J-K, Kim J, Kim C-H. Dynamic hip screw versus cannulated cancellous screw in Pauwels type II or type III femoral neck fracture: a systematic review and meta-analysis. J Personalized Med. 2021;11(10):1017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Stegelmann SD, Butler JT, Mathews DJ, Ostlie HC, Boothby BC, Phillips SA. Survivability of the Femoral Neck System for the treatment of femoral neck fractures in adults. Eur J Orthop Surg Traumatol. 2023;33(6):2555-2563. [DOI] [PubMed] [Google Scholar]
- 27.Wang K, Lin D, Chen P, et al. Incidence and factors influencing neck shortening after screw fixation of femoral neck fractures with the femoral neck system. J Orthop Surg Res. 2023;18(1):317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Jiang T, Gao H, Xu B, Lv F, Liu T. The comparison of femoral neck system and cancellous screws internal fixation for femoral neck fracture. Biotechnol Genet Eng Rev. 2023;12:1-12. [DOI] [PubMed] [Google Scholar]
- 29.Wang H, Wang B, Zhao C, Song L, Zhu L. Efficacy of femoral neck system fixation vs KHS femoral neck dynamic compression locking plate system in femoral neck fracture. Alternative Ther Health Med. 2023;29(5):97-101. [PubMed] [Google Scholar]
- 30.Rogers NB, Hartline BE, Achor TS, et al. Improving the diagnosis of ipsilateral femoral neck and shaft fractures: a new imaging protocol. J Bone Joint Surg Am. 2020;102(4):309-314. [DOI] [PubMed] [Google Scholar]
- 31.Sadozai Z, Davies R, Warner J. The sensitivity of ct scans in diagnosing occult femoral neck fractures. Injury. 2016;47(12):2769-2771. [DOI] [PubMed] [Google Scholar]
- 32.Zamora T, Klaber I, Ananias J, et al. The influence of the CT scan in the evaluation and treatment of nondisplaced femoral neck fractures in the elderly. J Orthop Surg. 2019;27(2):2309499019836160. [DOI] [PubMed] [Google Scholar]
- 33.Ly TV, Swiontkowski MF. Management of femoral neck fractures in young adults. Indian J Orthop. 2008;42(1):3-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Stockton DJ, O’Hara LM, O’Hara NN, Lefaivre KA, O’Brien PJ, Slobogean GP. High rate of reoperation and conversion to total hip arthroplasty after internal fixation of young femoral neck fractures: a population-based study of 796 patients. Acta Orthop. 2019;90(1):21-25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Wang SH, Yang JJ, Shen HC, Lin LC, Lee MS, Pan RY. Using a modified Pauwels method to predict the outcome of femoral neck fracture in relatively young patients. Injury. 2015;46(10):1969-1974. [DOI] [PubMed] [Google Scholar]
- 36.Lin S, Li J, Wang R, et al. The effect of anteromedial support plate with three cannulated screws in the treatment of Pauwels type III femoral neck fracture in young adults. Eur J Trauma Emerg Surg. 2022;48(5):4011-4017. Online ahead of print. [DOI] [PubMed] [Google Scholar]
- 37.Ye Y, Chen K, Tian K, Li W, Mauffrey C, Hak DJ. Medial buttress plate augmentation of cannulated screw fixation in vertically unstable femoral neck fractures: surgical technique and preliminary results. Injury. 2017;48(10):2189-2193. [DOI] [PubMed] [Google Scholar]
- 38.Kunapuli SC, Schramski MJ, Lee AS, et al. Biomechanical analysis of augmented plate fixation for the treatment of vertical shear femoral neck fractures. J Orthop Trauma. 2015;29(3):144-150. [DOI] [PubMed] [Google Scholar]
- 39.Su Z, Liang L, Hao Y. Medial femoral plate with cannulated screw for Pauwels type III femoral neck fracture: a meta-analysis. J Back Musculoskelet Rehabil. 2021;34(2):169-177. [DOI] [PubMed] [Google Scholar]
- 40.Fischer H, Maleitzke T, Eder C, Ahmad S, Stöckle U, Braun KF. Management of proximal femur fractures in the elderly: current concepts and treatment options. Eur J Med Res. 2021;26(1):86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Upadhyay A, Jain P, Mishra P, Maini L, Gautum VK, Dhaon BK. Delayed internal fixation of fractures of the neck of the femur in young adults. A prospective, randomised study comparing closed and open reduction. J Bone Joint Surg Br. 2004;86(7):1035-1040. [DOI] [PubMed] [Google Scholar]
- 42.Wang Y, Ma JX, Yin T, et al. Correlation between reduction quality of femoral neck fracture and femoral head necrosis based on biomechanics. Orthop Surg. 2019;11(2):318-324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Zhu J, Li Y, Zhang Y, Cheng X. Clinical outcome and biomechanical analysis of dynamic hip screw combined with derotation screw in treating displaced femoral neck fractures based on different reduction qualities in young patients (≤65 years of age). BioMed Res Int. 2022;2022:9505667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Nyholm AM, Palm H, Sandholdt H, Troelsen A, Gromov K, Danish Fracture Database Collaborators . Osteosynthesis with parallel implants in the treatment of femoral neck fractures: minimal effect of implant position on risk of reoperation. J Bone Joint Surg Am. 2018;100(19):1682-1690. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental Material for Evaluation of Post-Operative Outcomes of Femoral Neck Fracture Interventions: A Systematic Review by Erin Sheffels, Mariam Khalil, Kristen Hutchison, Nicole J. Hardy, Ranita Tarchand, John M. Pederson, Anjani Parikh, and Michael Blauth in Geriatric Orthopaedic Surgery & Rehabilitation
Supplemental Material for Evaluation of Post-Operative Outcomes of Femoral Neck Fracture Interventions: A Systematic Review by Erin Sheffels, Mariam Khalil, Kristen Hutchison, Nicole J. Hardy, Ranita Tarchand, John M. Pederson, Anjani Parikh, and Michael Blauth in Geriatric Orthopaedic Surgery & Rehabilitation
Supplemental Material for Evaluation of Post-Operative Outcomes of Femoral Neck Fracture Interventions: A Systematic Review by Erin Sheffels, Mariam Khalil, Kristen Hutchison, Nicole J. Hardy, Ranita Tarchand, John M. Pederson, Anjani Parikh, and Michael Blauth in Geriatric Orthopaedic Surgery & Rehabilitation