Abstract
Background:
Mental health disorders are linked to prolonged concussion symptoms. However, the association of premorbid anxiety/depression symptoms with postconcussion return-to-play timelines and total symptom burden is unclear.
Objective:
To examine the association of self-reported premorbid anxiety/depression symptoms in collegiate student-athletes with (1) recovery times until asymptomatic, (2) return-to-play, and (3) postconcussion symptom burden.
Study Design:
Athletes in the Concussion Assessment, Research and Education Consortium completed baseline concussion assessments (Sport Concussion Assessment Tool [SCAT3] and Brief Symptom Inventory-18 [BSI-18]). Athletes were tested postinjury at <6 hours, 24 to 48 hours, time of asymptomatic and start of return-to-play protocol, unrestricted return-to-play, and 6 months after injury. Injured athletes were categorized into 4 groups based on BSI-18 scores: (1) B-ANX, elevated anxiety symptoms only; (2) B-DEP, elevated depression symptoms only; (3) B-ANX&DEP, elevated anxiety and depression symptoms; and (4) B-NEITHER, no elevated anxiety or depression symptoms. Relationship between age, sex, BSI-18 group, SCAT3 total symptom and severity scores, and time to asymptomatic status and return-to-play was assessed with Pearson’s chi-squared test and robust analysis of variance.
Level of Evidence:
Level 3.
Results:
Among 1329 athletes with 1352 concussions, no respondents had a self-reported premorbid diagnosis of anxiety/depression. There was no difference in time until asymptomatic or time until return-to-play between BSI-18 groups (P = 0.15 and P = 0.11, respectively). B-ANX, B-DEP, and B-ANX&DEP groups did not have higher total symptom or severity scores postinjury compared with the B-NEITHER group.
Conclusion:
Baseline anxiety/depression symptoms in collegiate student-athletes without a mental health diagnosis are not associated with longer recovery times until asymptomatic, longer time to return-to-play, or higher postconcussion total symptom and severity scores compared with athletes without baseline symptoms.
Clinical Relevance:
Anxiety and depression symptoms without a clear mental health diagnosis should be considered differently from other comorbidities when discussing prolonged recovery in collegiate student-athletes.
Keywords: anxiety, concussion, depression, mental health
Over the last 3 decades, sport-related concussion (SRC) has garnered increasing attention from sports medicine clinicians, researchers, media, sports organizations, and athletes due to its reported prevalence, acute effects, and potential long-term neurological consequences. 53 It is estimated that 1.6 to 3.8 million SRC occur in the United States (US) annually, and SRC is more common in contact- and collision-sport athletes at all participation levels.43,55,56
Concussions may result in a range of signs and symptoms across physical, cognitive, and emotional domains. Whereas some symptoms may present rapidly and resolve spontaneously, persistent symptoms may also occur.3,29,31,32,49,51,53 Existing mental health conditions have been linked broadly to prolonged concussion symptoms in youths and adults. 35 Collegiate student-athletes are at high risk for experiencing anxiety and depression due to new life stressors, reduced parental support, the challenges associated with competitive intercollegiate sports, and difficulty coping with injury.22,40,45,80,83 Discerning the role premorbid anxiety and/or depression symptoms may have on postconcussion symptom duration and return-to-play timeline is therefore essential to the care of this unique population.
Extensive research over the past 2 decades indicates that some collegiate athletes may take longer than the typical recovery window of 7 to 10 days to clinically return-to-play after a concussion (ie, 10-14 days in adults).3,29,31,32,49,51,53 Symptoms and severity usually improve 2 weeks postconcussion, with a majority of concussed athletes recovering within 1 month postinjury.35,36,52
Previous studies have found that the strongest and most consistent predictor of prolonged recovery after concussion was a greater severity of acute and subacute symptoms postinjury.35,54 Multiple studies have investigated preinjury characteristics associated with increased risk for prolonged recovery.9,28,35 These include female sex,3,6,41,85 adolescent age,4,8,74,85 personal or family history of migraine,58,85 and personal or family history of mental health problems.2,17,24,25,48,58,84,85 Results for nearly all studies investigating potential predictors of clinical recovery are mixed, and there are some studies that do not show a significant association between potential predictors and duration of clinical recovery. This is likely due to variable qualities of the studies, methodologies utilized (specifically, measured outcomes, sample sizes, and statistical power), sport population representativeness, and study follow-up duration.9,30,35,54,75 Recent studies continue to demonstrate conflicting results of psychiatric history on concussions. Lumba-Brown et al 47 found that concussed college student-athletes with a history of mental health problems and higher symptoms of anxiety and mood disruption at baseline were more likely to have higher postinjury reports of mood and anxiety symptoms following injury. However, a recent systematic review of SRC did not find psychiatric history as a strong factor in symptom recovery, 65 similar to findings in a smaller study where concussion did not have a significant impact on trait anxiety. 18
The objective of the current study was to examine whether self-reported premorbid anxiety and/or depression symptoms in collegiate student-athletes are associated with longer times until asymptomatic and return-to-play postconcussion. A secondary objective was to determine whether collegiate student-athletes with self-reported premorbid anxiety and/or depression symptoms have higher total symptom scores and symptom severity scores postinjury. We hypothesized that collegiate student-athletes with self-reported premorbid anxiety and/or depression-related symptoms would have longer recovery periods after SRC before returning to play and have higher symptom burden postinjury, compared with athletes without these conditions.
Methods
Overview of Study Design and NCAA-DoD CARE Consortium
The current analysis investigated prospectively collected data on 1329 collegiate student-athletes with 1352 concussions who participated in the Concussion Assessment, Research and Education (CARE). The National Collegiate Athletic Association (NCAA)-Department of Defense (DoD) sponsored the CARE Consortium to study clinical and neurobiological recovery after SRC. The NCAA-DoD CARE Consortium is the largest prospective cohort study of SRC in collegiate athletes and US military service cadets, and it has enrolled over 40,000 athletes at 30 NCAA Division I, II, and III institutions.10,50 Data collection was carried out from 2014 to 2018 by the Consortium at 33 participating sites, and participant informed consent was obtained. Data were anonymized and approved by the appropriate Institutional Review Board for use following their ethics guidelines. All participating athletes had undergone detailed preseason baseline testing including concussion assessments. 50 The current study utilized the most recent baseline before the date of their first postinjury assessment. The CARE postinjury protocol involves follow-up testing of concussed athletes at several timepoints: <6 hours, 24 to 48 hours, time of asymptomatic and start of return-to-play protocol, unrestricted return-to-play, and 6 months after injury. Demographics, clinical recovery, management, return-to-play, and repeat concussion are recorded. 10 Demographics and history were provided by athletes on a self-report questionnaire. The definition of concussion for diagnosis is based on the observed mechanism of injury and clinical criteria of the DoD: “a change in brain function after a force to the head that may be accompanied by temporary loss of consciousness but is identified in awake individuals with the use of measures of neurologic and cognitive dysfunction.” 12 Trained physicians and athletic trainers made the diagnosis of concussion, assessments of recovery, and decisions on return-to-play.
Assessments included symptom evaluation using the graded symptom checklist from the Sport Concussion Assessment Tool (SCAT3) and Brief Symptom Inventory 18 (BSI-18) – a psychological state assessment. 15 The BSI-18 has been validated as a measure of emotional state in concussed athletes and may portray psychological distress in the general population.26,42 The BSI-18 contains 3 scales: somatization, anxiety, and depression; in this analysis, we focused on the anxiety and depression scales. The BSI-18 scores range from 0 to 24 and were calculated by sum scores for anxiety and depression items.21,26 Determination of “asymptomatic” on the BSI-18 was based on gender norms per the instrument’s published manual; to have clinical significance of anxiety or depression, a cut-off ≥5 was used for male subjects, and ≥7 was used for female subjects.20,21 On the SCAT3 graded symptom checklist, “asymptomatic” was defined as a symptom score of 0. We recognize there is discussion among experts regarding whether a “0” symptom score accurately defines asymptomatic; for this study, to be consistent with other studies, we opted to use 0. 14
In the current analysis, athletes were categorized based on self-reported premorbid anxiety/depression symptoms on the BSI-18. Athletes self-reported being diagnosed with anxiety/depression in response to the following questionnaire item:
“For every condition below, have you ever been diagnosed by a Physician/MD with:
Psychiatric Disorder: [ ] Yes, [ ] No
– [ ] Unknown
– [ ] Mood Disorder (excluding depression and bipolar disorder)
– [ ] Anxiety Disorder
– [ ] PTSD
– [ ] Personality Disorder
– [ ] Alcohol Abuse
– [ ] Drug Abuse
– [ ] Personality Disorder
– [ ] Psychiatric Disorder (excluding schizophrenia)
– [ ] Other
Depression: [ ] Yes, [ ] No”
Concussed athletes were categorized into 4 groups as follows: (1) B-ANX, elevated anxiety symptoms only on the BSI-18, (2) B-DEP, elevated depression symptoms only on the BSI-18, (3) B-ANX&DEP, elevated anxiety and depression symptoms on the BSI-18, and (4) B-NEITHER, no elevation of anxiety or depression symptoms on baseline BSI-18.
Outcome Measures
Primary outcomes were time until asymptomatic and time to return-to-play. Time until asymptomatic was calculated as the number of days from injury to being determined asymptomatic and beginning the return-to-play protocol. Time to return-to-play was calculated as the number of days from injury to return to unrestricted sport-related activities. Secondary outcomes were total symptom score (ie, total number of symptoms endorsed) and symptom severity score (ie, sum of severity scores for each symptom) as measured by the SCAT3 graded symptom checklist at 24 to 48 hours and 6 months postconcussion. 13
Inclusion and Exclusion Criteria
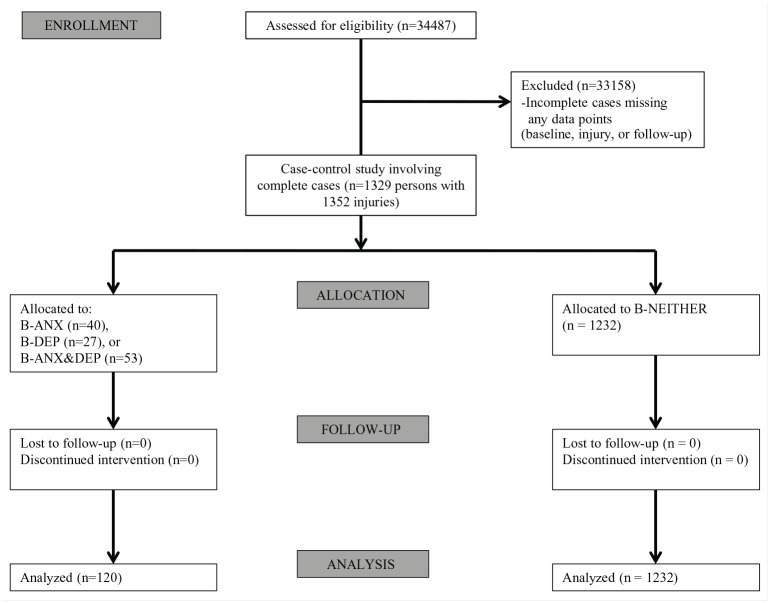
A CONSORT diagram detailing participants and eligibility criteria is presented in Figure 1. The 1352 concussive injuries included were those containing data for all 5 timepoints in chronological order: baseline, 24 hours postinjury, time until asymptomatic, time to return-to-play, and 6 months postinjury. If any timepoints were missing, then the case was excluded. Persons with multiple injuries were included if the second or third injury likewise had complete chronological data. Athletes who self-reported a diagnosis of a psychiatric disorder, unknown psychiatric disorder, mood disorder, posttraumatic stress disorder (PTSD), somatoform disorder, personality disorder, psychotic disorder, other psychiatric disorder not otherwise specified, bipolar disorder, or schizophrenia were not excluded. Athletes who self-reported prescription medication use (ie, antidepressants, anti-anxiety medication, antipsychotic medication, psychostimulant medication, or other prescription medication) also were not excluded. Our source file conforms with updated CARE guidelines to include data through 2018.
Figure 1.
Consort diagram detailing participant and case inclusion and exclusion criteria. B-ANX, elevated anxiety symptoms only on BSI-18; B-ANX&DEP, elevated anxiety and depression symptoms on BSI-18; B-DEP, elevated depression symptoms only on BSI-18; B-NEITHER, no elevation of anxiety or depression symptoms on baseline BSI-18; BSI-18, Brief Symptom Inventory 18.
Data Analysis
Primary Analysis
Groups categorized by having both, neither, or only anxiety- or depression-related symptoms on the BSI-18 were compared. Time until asymptomatic and time to return-to-play were analyzed as a function of self-reported symptoms on the BSI-18. Pearson’s chi-squared test and robust analysis of variance (ANOVA; Welch’s test) were used to compare age, sex (assigned at birth), the aforementioned groups, time to asymptomatic status, and time to return-to-play. Welch’s ANOVA is unaffected by unequal variances and thus is statistically robust compared with the traditional Fisher ANOVA.
Secondary Analysis
Welch’s test was employed to assess whether the self-reported symptoms on BSI-18 have higher symptom severity and/or higher total symptom scores at multiple follow-up assessments, compared with the control group. Symptom scores and severity at 24 to 48 hours and 6 months postinjury were the main focus. Statistical analyses were conducted in R Version 3.6.3. 68
Results
Baseline data included 47,397 rows of data (“reports”) from 34,487 athletes who were assessed for eligibility in our study. Out of 34,487 athletes, 33,158 cases were excluded for missing datapoints (baseline, injury, or follow-up datapoints). In our analysis, there were 1329 remaining athletes comprising 1352 separate injuries who had complete cases. A total of 680 athletes answered “Yes” to being diagnosed with Anxiety Disorder and 1320 with Depression; however, all of these cases were excluded due to missing datapoints. Due to our exclusion criteria, 0 out of 1329 athletes in our analysis reported a diagnosis of anxiety and/or depression at baseline (ie, athletes who answered “Yes” to a diagnosis of anxiety or depression lacked a complete dataset). Thus, our analysis specifically involves athletes without a diagnosis of anxiety/depression but who may report anxiety/depression symptoms.
Sample Characteristics
The sample included 1329 collegiate student-athletes with 1352 concussions. A total of 1329 student-athletes had a single injury, 19 had a second injury with a complete dataset, and 2 had a third injury with a complete dataset. Student-athletes were 41.16% female (n = 547) and 58.84% male (n = 782) (Table 1), with multiple races and ethnicities represented (Table 2), and participated in a variety of sports (Table 3 and Figure 2). Sample characteristics are presented in Table 1.
Table 1.
Summary of target group and injury characteristics in the current study
| Target Group Characteristics | Mean (SD) | |||
|---|---|---|---|---|
| Injuries, n Female subjects Male subjects |
B-ANX n = 27 n = 12 n = 15 |
B-DEP n = 40 n = 13 n = 27 |
B-ANX&DEP n = 53 n = 19 n = 34 |
B-NEITHER n = 1232 n = 512 n = 720 |
| Total n = 1352 Female subjects, n = 556; Total % = 41.12% Male subjects, n = 796; Total % = 58.88% |
||||
| Age, y | 19.40 (1.37) Median = 19 Age 17, n = 40 Age 18, n = 390 Age 19, n = 340 Age 20, n = 265 Age 21, n = 196 Age 22, n = 75 Age 23, n = 18 Age 24, n = 5 |
|||
| Participation in primary sport, y | 10.79 (4.00) for n = 931; Range, 1-15 “NA”, n = 398 |
|||
| Previous concussions, n | 0.72 (0.87); Range, 0-7 Median = 1 “NA”, n = 12 |
|||
| Current use of prescription medications | “No”, n = 935 “Yes”, n = 376 Birth control, n = 210 Antidepressants, n = 33 Anti-anxiety medication, n = 21 Sleep sedatives, n = 8 Psychostimulant, n = 22 |
|||
| + Reported diagnosed anxiety | 0 % | |||
| + Reported diagnosed depression | 0 % | |||
| B-ANX | 0.06 (0.24) | |||
| B-DEP | 0.07 (0.25) | |||
| Injury characteristics | ||||
| Time until asymptomatic, days | 17.38 (35.01) | |||
| Time to return-to-play, days | 27.25 (37.93) | |||
| SCAT3 total symptoms 24 hours postconcussion, n | 10.02 (6.32) | |||
| SCAT3 symptom severity 24 hours postconcussion, n | 23.51 (21.53) | |||
| SCAT3 total symptoms 6 mo postconcussion (n) | 0.70 (1.74) | |||
| SCAT3 symptom severity 6 mo postconcussion, n | 1.07 (3.48) | |||
B-ANX, elevated anxiety symptoms only on BSI-18; B-DEP, elevated depression symptoms only on BSI-18; BSI-18, Brief Symptom Inventory 18; SCAT3, Sport Concussion Assessment Tool.
Table 2.
Race and ethnicity of participants
| Hispanic | Non-Hispanic | Skipped | Unknown | NA | Total Number (%) | |
|---|---|---|---|---|---|---|
| African American | 7 | 133 | 15 | 18 | 13 | 186 (14.00) |
| Asian | 2 | 45 | 1 | 1 | 1 | 50 (3.76) |
| Hawaiian/Pacific Islander | 3 | 5 | 1 | 2 | 0 | 11 (0.83) |
| American Indian/Alaskan Native | 4 | 4 | 0 | 0 | 0 | 8 (0.60) |
| Multiple races | 10 | 107 | 6 | 5 | 1 | 129 (9.71) |
| Skipped | 14 | 1 | 1 | 0 | 0 | 16 (1.20) |
| Unknown | 9 | 0 | 0 | 5 | 0 | 14 (1.05) |
| White | 70 | 793 | 17 | 25 | 5 | 910 (68.47) |
| NA | 3 | 0 | 1 | 1 | 0 | 5 (0.38) |
NA, participants who did not supply any entry for one or the other of the 2 items.
Table 3.
Sorted proportion of reports (n = 47,397 reports from 34,487 athletes) by sport
| Sport | Sorted Proportion of Reports, % |
|---|---|
| Football | 19.82 |
| Cross country/track | 11.90 |
| Soccer | 9.85 |
| Swimming | 6.69 |
| Baseball | 6.46 |
| Rowing/crew | 6.26 |
| Basketball | 5.90 |
| Lacrosse | 4.97 |
| Softball | 3.49 |
| Volleyball | 3.46 |
| Field event | 3.26 |
| Tennis | 3.14 |
| Wrestling | 3.06 |
| Cheerleading | 2.40 |
| Gymnastics | 2.13 |
| Golf | 2.07 |
| Water polo | 1.61 |
| Ice hockey | 1.42 |
| Field hockey | 1.40 |
| Diving | 0.99 |
| Rugby | 0.77 |
| Fencing | 0.73 |
| Sprint football | 0.44 |
| Rifle | 0.34 |
| Sailing | 0.28 |
| Beach volleyball | 0.11 |
| Boxing | 0.08 |
| Track and field | 0.01 |
| Bowling | 0.01 |
Figure 2.
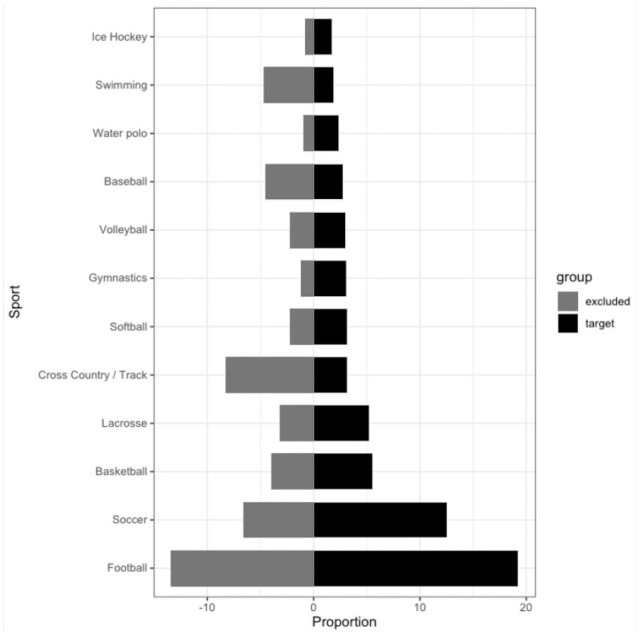
Sorted proportion of athletes in the 12 most popular sports in the target group, along with proportion of athletes in the excluded group for the same sports (n = 47,397 reports from 34,487 athletes).
Fewer than 7% of responses had numerical ratings on the BSI-18 that were at or above the validated sex-specific cut-off scores. There were no significant differences between BSI groups in terms of sex, age, years of participation, previous concussions, and current medication prescription use.
Using the full baseline CARE dataset (n = 34,487), approximately 1% (n = 341) of those who responded “Yes” to taking mental health medication (anti-anxiety or antidepressant medication) at baseline reported a corresponding mental health diagnosis (self-reported anxiety and/or depression). The odds ratio for the relationship between any mental health medication usage and any self-reported mental health diagnosis was found to be 47.4 times more likely; thus, reported anti-anxiety or antidepressant medication use is associated with premorbid mental health diagnosis of anxiety or depression (95% CI [39.9, 56.2], P < 0.01).
Time Until Asymptomatic and Time to Return-to-Play
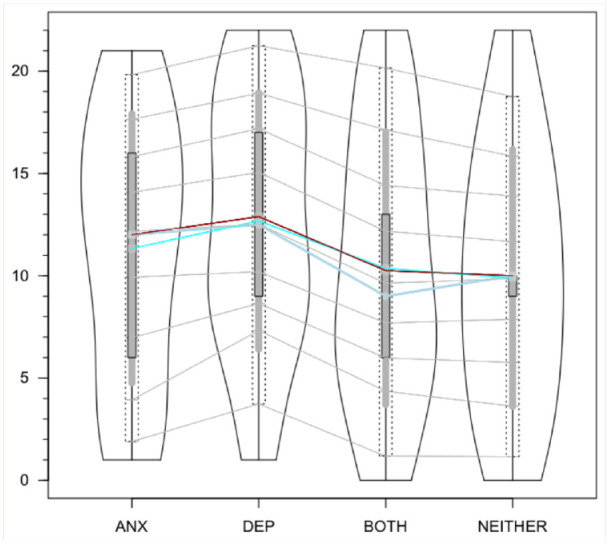
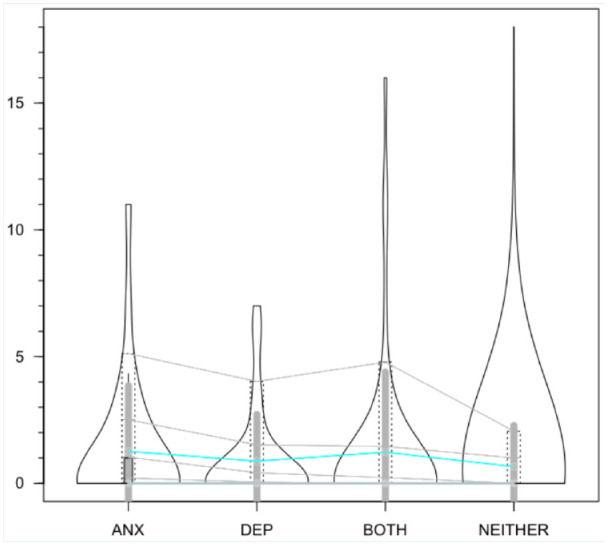
There was no evidence by Welch’s ANOVA that time until asymptomatic (F[3,40.069] = 1.888; P = 0.15) or time to return-to-play (F[3,40.385] = 2.175; P = 0.11) differs by BSI group (B-ANX, B-DEP, B-ANX&DEP, and B-NEITHER). Table 4 lists means and medians for recovery time with respect to each BSI group, and Figures 3 and 4 demonstrate violin plot representations for group distributions. The degree to which the mean diverges from the median due to marked skewness in the data distributions indicates that conventional statistical testing is likely to be inadequate.
Table 4.
Time until asymptomatic and time to return-to-play per BSI group
| B-ANX | B-DEP | B-ANX&DEP | B-NEITHER | |
|---|---|---|---|---|
| Time until asymptomatic | ||||
| Mean (SD) | 8.47 (5.86) | 11.11 (11.45) | 13.52 (20.49) | 17.95 (36.31) |
| Median | 6.38 | 8.27 | 8.19 | 8.38 |
| Time until return-to-play | ||||
| Mean (SD) | 16.34 (10.18) | 19.29 (12.75) | 25.72 (25.45) | 27.81 (39.24) |
| Median | 12.88 | 15.72 | 18.01 | 15.92 |
B-ANX, elevated anxiety symptoms only on BSI-18; B-ANX&DEP, elevated anxiety and depression symptoms on BSI-18; B-DEP, elevated depression symptoms only on BSI-18; B-NEITHER, no elevation of anxiety or depression symptoms on baseline BSI-18; BSI-18, Brief Symptom Inventory 18.
Figure 3.
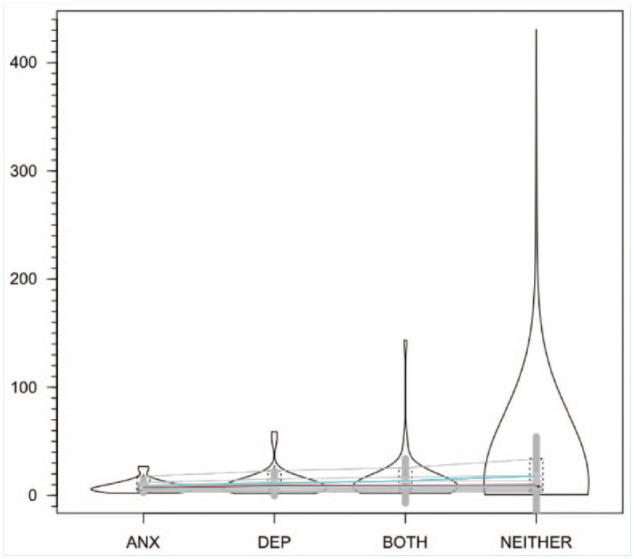
Time until asymptomatic per BSI group. Violin plots are shown with colored lines connecting the medians (dark gray), averages (blue) and Huber’s robust estimates of the distribution centers (crimson), along with deciles connected by thin gray lines. ANX, anxiety; BSI, Brief Symptom Inventory; DEP, depression.
Figure 4.
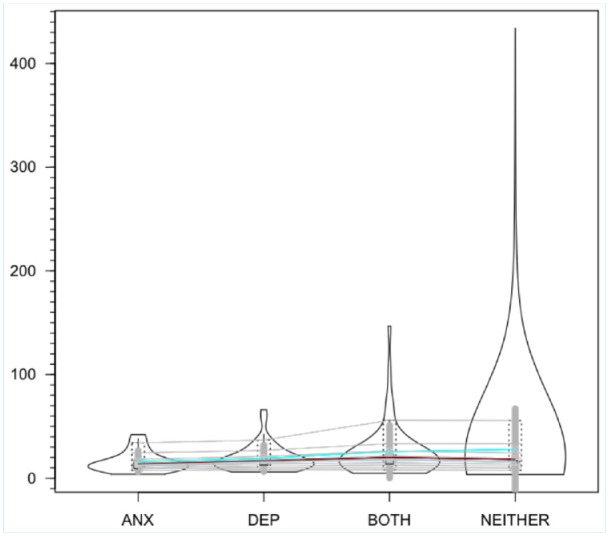
Time to return-to-play per BSI group. ANX, anxiety; BSI, Brief Symptom Inventory; DEP, depression.
Using Pearson’s chi-squared test, there were no statistically significant differences between any of the 4 BSI groups (B-ANX, B-DEP, B-ANX&DEP, B-NEITHER) in relation to sex (χ2 = 2.06;P = 0.56). Using Pearson’s chi-squared test with Yates’ continuity correction, there was no statistically significant difference in relation to sex between all +BSI groups combined (B-ANX, B-DEP, and B-ANX&DEP) compared with B-NEITHER (χ2 = 0.89; P= 0.35).
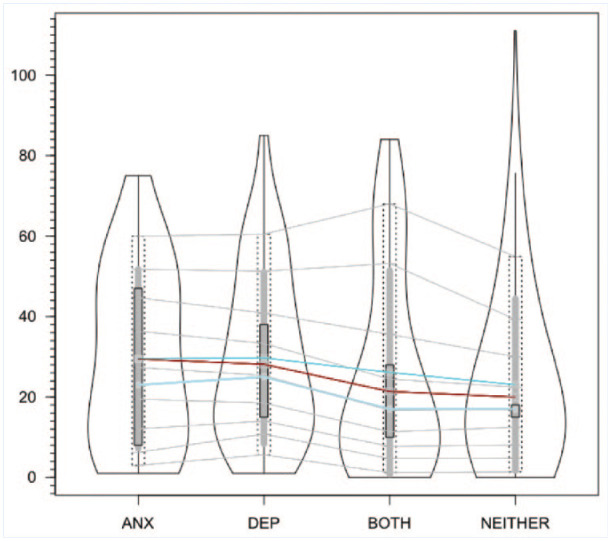
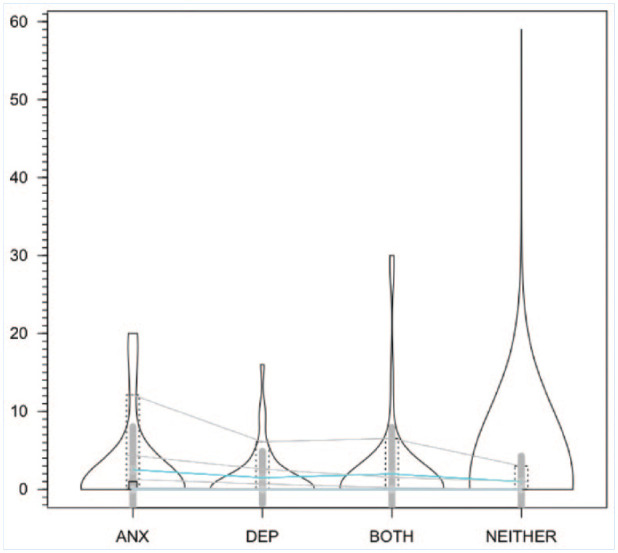
Total Symptom Score and Symptom Severity Score
The 4 BSI groups outlined above were also analyzed in relation to SCAT3 total symptom scores and symptom severity scores at 24 hours and 6 months postinjury. Analysis demonstrated that B-ANX, B-DEP, and B-ANX&DEP groups did not have higher total symptom scores or higher symptom severity scores at postassessments, when compared with B-NEITHER. SCAT3 total symptom score at 24 hours postconcussion differed between B-NEITHER and B-DEP, with a higher total symptom score reported in B-DEP, but this is not statistically significant in Welch’s ANOVA (F[3,37.88] = 2.51; P = 0.07). Findings suggest that BSI groups differ in SCAT3 total symptoms at 6 months postconcussion, but Welch’s test indicates no statistically significant difference (F[3,37.25] = 0.19; P = 0.90). Total SCAT3 symptoms per BSI group at 24 hours and 6 months postinjury are shown in Figures 5 and 6, respectively.
Figure 5.
SCAT3 total symptom score per BSI group at 24 hours postinjury. ANX, anxiety; BSI, Brief Symptom Inventory; DEP, depression; SCAT3, Sport Concussion Assessment Tool.
Figure 6.
SCAT3 total symptom score per BSI group at 6 months postinjury. ANX, anxiety; BSI, Brief Symptom Inventory; DEP, depression; SCAT3, Sport Concussion Assessment Tool.
There was no statistical difference between SCAT3 symptom severity score at 24 hours postconcussion by BSI group (F[3,37.07] = 1.98; P = 0.13). Findings suggest that the SCAT3 symptom severity score at 6 months postconcussion differs by BSI group, but Welch’s ANOVA indicates no statistically significant difference (F[3,36.68] = 0.18; P = 0.91). Table 5 demonstrates mean and median scores for all BSI groups. Symptom severity scores per BSI group at 24 hours and 6 months postinjury are depicted in Figures 7 and 8, respectively.
Table 5.
Total symptom and symptom severity scores per BSI group
| B-ANX | B-DEP | B-ANX&DEP | B-NEITHER | |
|---|---|---|---|---|
| Total symptom score at 24 hours postinjury | ||||
| Mean (SD) | 11.33 (6.58) | 12.68 (6.27) | 10.36 (6.66) | 9.89 (6.29) |
| Median | 12.16 | 12.52 | 9.63 | 9.86 |
| Total symptom score at 6 months postinjury | ||||
| Mean (SD) | 1.25 (2.60) | 0.88 (1.84) | 1.23 (3.17) | 0.66 (1.62) |
| Median | 0.02 | 0.00 | 0.00 | 0.00 |
| Mean symptom severity score at 24 hours postinjury | ||||
| Mean (SD) | 29.52 (22.19) | 29.73 (21.29) | 26.11 (25.30) | 23.06 (21.31) |
| Median | 27.35 | 25.35 | 16.66 | 16.91 |
| Mean symptom severity score at 6 months postinjury | ||||
| Mean (SD) | 2.52 (5.53) | 1.50 (3.37) | 1.98 (5.98) | 0.98 (3.27) |
| Median | 0.02 | 0.00 | 0.00 | 0.00 |
B-ANX, elevated anxiety symptoms only on BSI-18; B-ANX&DEP, elevated anxiety and depression symptoms on BSI-18; B-DEP, elevated depression symptoms only on BSI-18; B-NEITHER, no elevation of anxiety or depression symptoms on baseline BSI-18; BSI-18, Brief Symptom Inventory 18.
Figure 7.
SCAT3 symptom severity score per BSI group at 24 hours postinjury. ANX, anxiety; BSI, Brief Symptom Inventory; DEP, depression; SCAT3, Sport Concussion Assessment Tool.
Figure 8.
SCAT3 Symptom Severity Score per BSI Group at 6 months postinjury. ANX, anxiety; BSI, Brief Symptom Inventory; DEP, depression; SCAT3, Sport Concussion Assessment Tool.
Discussion
To our knowledge, no multicenter study has directly addressed the role of premorbid symptoms of anxiety and/or depression with regard to postconcussion symptom duration and return-to-play timeline, particularly in NCAA collegiate student-athletes. Findings in our study suggest that, in collegiate student-athletes without a diagnosis of anxiety or depression, baseline anxiety- or depression-related symptoms as determined on a validated symptom scale are not associated with longer recovery time until asymptomatic, longer time to return-to-play, or higher postconcussion total symptom and symptom severity scores compared with athletes without baseline anxiety/depression symptoms. These findings support the 2018 single-center study by Putukian et al 66 that demonstrated self-reported anxiety/depression symptoms were not predictive of recovery times until asymptomatic or return-to-play. The lack of demonstrated association between anxiety-/depression-related symptoms and longer recovery time is an intriguing result, as it is not congruent with what many previous studies have found regarding a premorbid diagnosis of anxiety and/or depression and prolonged concussion recovery. Notably, in our analysis, there were no athletes with a complete dataset who reported a diagnosis of anxiety and/or depression. As such, we cannot extend our conclusions to definitively say that premorbid self-reported diagnosis of anxiety/depression are unrelated to prolonged symptoms; rather, we can only conclude that, in this highly defined sample, self-reported anxiety and/or depression symptoms at baseline were not predictive of prolonged SRC symptoms.
Much of the previously published literature has demonstrated that premorbid mental health issues result in delayed recovery and higher postinjury symptom burden. Previous research has looked at many comorbidities for SRC, including history of previous concussion, learning disability, personal or family history of migraine, family psychiatric history, as well as personal history of mental health problems, all of which have been associated with prolonged concussion recovery.11,27,35,54,62,63 In particular, previous psychiatric history has been investigated in relation to concussion recovery with mixed findings.2,17,24,25,39,58,62,63,74,84,85
Differences between the current analysis and previous studies include that this analysis had zero athletes who identified a diagnosis of anxiety/depression. In various other CARE publications, there is a baseline report of diagnosis of anxiety and/or depression of approximately 4%, which is similar to our study’s baseline percentages for these diagnoses before exclusion criteria (4.2%).
It is possible that some athletes included in our study had an actual diagnosis of anxiety or depression but did not report it.5,16,33,69 Collegiate student-athletes may underreport mental health issues to avoid perceived stigma or consequences. Changing the social stigma associated with mental health issues and seeking psychological help may aid in providing greater social awareness and access to treatment for those who could benefit from it, particularly on college campuses where prevalence has been rising. 5 Interestingly, although no athletes included in the analysis endorsed a history of anxiety/depression, 7% rated themselves as anxious and/or depressed based on the BSI symptom scale cut-offs; this may be interpreted as athletes were willing to rate their anxiety/depression symptoms but not endorse a history of diagnosis. Still, underreporting of symptoms may have occurred. In a previous study, fewer student-athletes report anxiety- or depression-related symptoms compared with their nonathlete counterparts: 48% of female student-athletes and 31% of male student-athletes report experiencing anxiety symptoms compared with 56% female and 40% male nonathlete counterparts, while 28% of female student-athletes and 21% of male student-athletes “felt depressed” compared with 33% female and 27% male nonathlete counterparts within the last 12 months. 23 Involvement in sports may be protective against premorbid anxiety/depression symptoms. Aerobic exercise has been shown to reduce symptoms of anxiety and depression, in acute and chronic settings.37,44,59,70,71,78 While premorbid diagnoses of anxiety/depression in previous studies have been associated with higher symptom burden postconcussion, premorbid anxiety/depression symptoms may not affect an athlete’s time until asymptomatic or return-to-play due to the protective effects of aerobic exercise.
Although other studies have focused on broader populations (eg, children, adolescents, and slightly older adults), 39 the current study is limited to collegiate student-athletes. Student-athletes are notably different from the general population in terms of rates of anxiety and depression, general health, and quality of life. College campuses have recently seen an increase in the number of students experiencing mental health issues such as anxiety and depression. 60 Former Division I athletes report decreased levels of wellness and health-related quality of life, specifically psychologically, socially and physically, compared with former nonathletes.72,76 Although sports encourage physical activity and promote healthy lifestyle, the demands of Division I sports may result in lingering injuries that decrease future quality of life in former athletes. 72 Looking at all college students (athletes and nonathletes), 11.9% admit to a history of any anxiety disorder, and 7.0% have a history of major depression disorder. 7 The prevalence of depression in college students is 10% to 85%, with weighted mean prevalence of 30.6%. 34 Although estimates regarding anxiety/depression prevalence rates in college student-athletes remain controversial, previous studies have suggested depression prevalence rates to be 15.6% to 21%.64,83 One study found the prevalence of depressive symptoms to be as high as 23.7%, with 6% expressing moderate-to-severe depressive symptoms, consistent with the major depression prevalence rate of 6.7% in adults.34,46,82 While some studies of collegiate student-athletes show rates of depression symptoms comparable with the nonathlete college population, 82 other studies have shown that college athletes have lower levels of depression than nonathletes.1,64 Weber et al 77 found that, of 8652 collegiate student-athletes who participated in the CARE Consortium, 59 (0.7%) reported premorbid anxiety, 283 (3.3%) reported premorbid depression, and 68 (0.8%) reported both. In the current study, prevalence rates of premorbid self-reported anxiety/depression diagnoses in collegiate student-athletes are notably below general college population rates, likely due to athlete underreporting due to concerns about the self- and public stigma associated with mental health conditions.
Factors thought to be protective in curbing depression in athletes include having a social network and team support. 1 Athletes have unique risk factors for anxiety and depression compared with nonathletes, including sports injury, involuntary career termination, athletic performance expectations, and, possibly, overtraining. 81 In certain subsets of athletes, there appears to be a higher rate of depression than in nonathletes. Female athletes have reported experiencing higher levels of depression and social anxiety compared with their male counterparts.73,81,83 Track and field was associated with the highest risk of depressive symptoms by sport. 82 The incidence of suicide in collegiate student-athletes at 0.93 per 100,000 students remains below the suicide rate of all collegiate students; out of all collegiate sports, football maintains the highest suicide rate. 67
By determining an accurate prognosis for college athletes with SRC, clinicians may be able to provide more reliable information to patients and potentially intervene earlier in patients who are actually at higher risk of developing persistent postconcussive symptoms (PPCS).9,53 It is possible that persons with preinjury psychiatric history may respond to experiencing mild traumatic brain injury and PPCS with greater anxiety, thus potentially exacerbating their symptoms. 63
Study Limitations
Several limitations of the current analysis warrant recognition. First, this study was limited to college athletes and may not be applicable to other athletic populations. Second, our requirement for a complete dataset (baseline, postinjury, and all follow-up timepoints) excluded an analysis of athletes with a self-reported diagnosis of anxiety or depression. While this was not the intent of our inclusion/exclusion criteria, our findings provide unique insights regarding self-reported anxiety/depression symptoms on the BSI-18 and how this may (or may not) impact concussion prognosis and recovery. We compared the demographics of the target group with the excluded group, and these 2 groups had similar demographics by sex (M/F ratio = 1.44/1 in target group vs 1.72/1 in excluded group), age (mean age, 18.80 years [SD 1.18] in target group vs 19.21 years [SD 1.43] in excluded group), and sport (Figure 2). Since the included and excluded groups have similar demographics, the generalizability of our findings is strengthened. Third, our study utilized self-reported diagnoses of anxiety and/or depression by athletes using a yes/no questionnaire, which may differ from medical diagnoses of anxiety and/or depression by a physician and DSM-V (Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition) criteria, and this may have contributed to underreporting. In comparison with younger patient populations, where parents may report formal medical diagnoses, adolescents may be more likely to report “depression” or “anxiety” as a premorbid condition, despite never having received this clinical diagnosis. 54 In the college population, this is likely the first time athletes are answering their own medical history while lacking parental support. Furthermore, in freshmen, increased stress levels while completing the baseline BSI-18 due to recently moving from home to a new environment limits the ability to tease out true anxiety/depression from situational symptoms. Depression and anxiety are cyclic issues, worsening during stressful time periods such as fall and winter, and remitting during summer - when baseline testing is usually performed; therefore, some athletes may not have had baseline testing elevations. Fourth, we recognize that our main measure of recovery was self-reported symptom resolution by the athlete. While modern tools assist in clinical assessment, the medical professional’s clinical judgment employed in this study remains the gold standard for injury management and guiding return-to-play. Fifth, although our results indicate that symptoms of anxiety or depression may not influence recovery time in student-athletes, we did not test for cognitive misattribution of expectation, anxiety sensitivity, or kinesiophobia - possible factors related to anxiety/depression that may contribute to the development of postconcussive symptoms and prolonged recovery after concussion, and can be mistaken for anxiety/depression.11,19,38,57,61,79 Cognitive misattribution or “expectation as etiology” was coined after investigating the expectation of symptoms after a head injury, which resulted in the misattribution of common symptoms to the injury.19,62 Anxiety sensitivity is a personality trait where a person demonstrates a fearful response associated with bodily sensations due to the belief that these sensations precede dangerous outcomes, which may influence how people perceive pain postconcussion.57,61 The Tampa Scale for Kinesiophobia-11 may be utilized to capture the construct of fear of movement in workers across pain levels, ages, and sexes. 79 Sixth, sports medicine specialists care for college athletes in our study, thus impacting the ability to generalize our findings to clinical management of concussion in other settings. Finally, our analysis was a prospective study, unlike most retrospective reports that sample from clinics, and it is an example of how prospective research can add to our understanding of a given topic, considering that it does not bring with it the selection bias issues to which retrospective studies are prone.
Future Research
Further research may investigate anxiety sensitivity and kinesiophobia as possible contributors to prolonged recovery in collegiate student-athletes, and whether there is a correlation of BSI-18 findings immediately postinjury compared with those at baseline. In addition, assessing recovery timelines with less restrictive criteria (ie, including participants with a baseline history of anxiety or depression) would be beneficial.
Conclusion
Our findings suggest that baseline anxiety and/or depression symptoms in collegiate student-athletes without a mental health diagnosis are not associated with longer recovery times until asymptomatic, longer time to return-to-play, or higher postconcussion total symptom and severity scores compared with athletes without baseline symptoms. Our results highlight the importance of understanding the role of mental health, specifically symptoms associated with anxiety and depression, on concussion recovery in collegiate student-athletes. Anxiety and depression symptoms without a clear mental health diagnosis should be considered differently from other comorbidities, such as previous concussion, migraine, or other psychiatric illnesses, when discussing prolonged recovery in collegiate student-athletes. Understanding the role these underlying symptoms play in postinjury concussion recovery and symptom severity is essential for healthcare professionals managing concussions in collegiate student-athletes.
Acknowledgments
The authors would like to thank the research and medical staff at each of the participating sites. This publication was made possible, in part, with support from the Grand Alliance CARE Consortium, funded by the NCAA and the DoD. The USAMRAA (US Army Medical Research Acquisition Activity) is the awarding and administering acquisition office. This work was supported by the Office of the Assistant Secretary of Defense for Health Affairs through the Psychological Health and Traumatic Brain Injury Program under Award No. W81XWH-14-2-0151. Opinions, interpretations, conclusions, and recommendations are those of the authors and are not necessarily endorsed by the DoD (Defense Health Program funds).
Footnotes
The following authors declared potential conflicts of interest: T.W.K. has received royalties from American Psychiatric Association Publishing and honoraria from Harvard Medical School. C.C.G. has received royalties from Blackwell/Wiley, consulting fees from the National Basketball Association (NBA), National Football League (NFL), National Hockey League/National Hockey League Players Association (NHL/NHLPA), and Highmark Interactive, honoraria from Harvard and New York University (NYU), speaker hospitality from Concussion in Sport Group, the National Collegiate Athletic Association (NCAA), the National Acquired Brain Injury Society (NABIS), and Neuro Grand Rounds, and stock options from Highmark Interactive. M.M. has received royalties from Oxford University Press and consulting fees from Neurotrauma Sciences and the Green Bay Packers. C.C.G. holds stock options with Highmark Interactive, and has received funding from National Institutes of Health-National Institute of Neurological Disorders and Stroke (NIH-NINDS) and University of California Los Angeles (UCLA) unrelated to the current work, consulting fees from the NBA, NFL, NHL/NHLPA, and the Los Angeles (LA) Lakers. A.P.K. has received royalties from APA Books, funding from the University of Pittsburgh/Centers for Disease Control and Prevention (CDC), Chuck Noll Foundation for Brain Injury Research, Department of Defense (DoD), NFL, and NIH. J.T.E. has a device patent to the University of Michigan. J.M. has received funding from the CDC, NIH, DoD, National Operating Committee on Standards for Athletic Equipment (NOCSAE), NFL, and Football Research unrelated to the present study.
This publication was made possible, in part, with support from the Grand Alliance Concussion Assessment, Research, and Education (CARE) Consortium, funded, in part by the NCAA and the DoD. The United States Army Medical Research Acquisition Activity, 820 Chandler Street, Fort Detrick MD 21702-5014 is the awarding and administering acquisition office. This work was supported by the Office of the Assistant Secretary of Defense for Health Affairs, through the Combat Casualty Care Research Program, endorsed by the DOD, through the Joint Program Committee 6/Combat Casualty Care Research Program - Psychological Health and Traumatic Brain Injury Program under Award No. W81XWH1420151. Opinions, interpretations, conclusions and recommendations are those of the author and are not necessarily endorsed by the DoD.
ORCID iD: Christopher C. Giza  https://orcid.org/0000-0002-5721-2667
https://orcid.org/0000-0002-5721-2667
Contributor Information
Sabrina P. Sawlani, UCLA Division of Sports Medicine, Departments of Family Medicine and Orthopaedics, Los Angeles, California, and UCLA Steve Tisch BrainSPORT Program, Los Angeles, California.
Joshua T. Goldman, UCLA Division of Sports Medicine, Departments of Family Medicine and Orthopaedics, Los Angeles, California, and UCLA Steve Tisch BrainSPORT Program, Los Angeles, California.
Talin Babikian, UCLA Steve Tisch BrainSPORT Program, Los Angeles, California, UCLA Division of Neuropsychology, Department of Psychiatry and Biobehavioral Sciences, Los Angeles, and UCLA Division of Neurology, Department of Pediatrics, UCLA-Mattel Children’s Hospital, Los Angeles.
David L. McArthur, UCLA Steve Tisch BrainSPORT Program, Los Angeles, California, and UCLA Department of Neurosurgery, David Geffen School of Medicine at UCLA, Los Angeles.
Douglas Polster, UCLA Steve Tisch BrainSPORT Program, Los Angeles, California, UCLA Division of Neuropsychology, Department of Psychiatry and Biobehavioral Sciences, Los Angeles, and UCLA Division of Neurology, Department of Pediatrics, UCLA-Mattel Children’s Hospital, Los Angeles.
Michael McCrea, Department of Neurosurgery, Medical College of Wisconsin, Milwaukee, Wisconsin.
Thomas McAllister, Department of Psychiatry, Indiana University School of Medicine, Indianapolis, Indiana.
Christopher C. Giza, UCLA Steve Tisch BrainSPORT Program, Los Angeles, UCLA Division of Neurology, Department of Pediatrics, UCLA-Mattel Children’s Hospital, Los Angeles, and UCLA Department of Neurosurgery, David Geffen School of Medicine at UCLA, Los Angeles.
Justus D. Ortega, California Polytechnic University Humboldt.
Nicholas Port, Indiana University.
Margot Putukian, Princeton University.
Jane McDevitt, Temple University.
Joshua T. Goldman, University of California, Los Angeles.
Holly J. Benjamin, University of Chicago.
Thomas W. Kaminski, University of Delaware.
James R. Clugston, University of Florida.
Luis A. Feigenbaum, University of Miami.
James T. Eckner, University of Michigan.
Jason P. Mihalik, University of North Carolina at Chapel Hill.
Scott Anderson, University of Oklahoma.
Christina L. Master, University of Pennsylvania.
Anthony P. Kontos, University of Pittsburgh Medical Center.
Sara P.O. Chrisman, University of Washington.
Kenneth Cameron, United States Military Academy.
Stefan Duma, Virginia Tech.
Christopher M. Miles, Wake Forest University.
References
- 1. Armstrong S, Oomen-Early J. Social connectedness, self-esteem, and depression symptomatology among collegiate athletes versus nonathletes. J Am Coll Health. 2009;57(5):521-526. [DOI] [PubMed] [Google Scholar]
- 2. Asken BM, McCrea MA, Clugston JR, Snyder AR, Houck ZM, Bauer RM. “Playing through it”: delayed reporting and removal from athletic activity after concussion predicts prolonged recovery. J Athl Train. 2016;51(4):329-335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Baker JG, Leddy JJ, Darling SR, Shucard J, Makdissi M, Willer BS. Gender differences in recovery from sports-related concussion in adolescents. Clin Pediatr (Phila). 2016;55(8):771-775. [DOI] [PubMed] [Google Scholar]
- 4. Barlow KM, Crawford S, Stevenson A, Sandhu SS, Belanger F, Dewey D. Epidemiology of postconcussion syndrome in pediatric mild traumatic brain injury. Pediatrics. 2010;126(2):e374-e381. [DOI] [PubMed] [Google Scholar]
- 5. Benton SA, Robertson JM, Tseng WC, Newton FB, Benton SL. Changes in counseling center client problems across 13 years. Prof Psychol Res Pract. 2003:24(1):66-72. [Google Scholar]
- 6. Berz K, Divine J, Foss KB, Heyl R, Ford KR, Myer GD. Sex-specific differences in the severity of symptoms and recovery rate following sports-related concussion in young athletes. Phys Sportsmed. 2013;41(2):58-63. [DOI] [PubMed] [Google Scholar]
- 7. Blanco C, Okuda M, Wright C, et al. Mental health of college students and their non-college-attending peers: results from the National Epidemiologic Study on Alcohol and Related Conditions. Arch Gen Psychiatry. 2008;65(12):1429-1437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Blume HK, Vavilala MS, Jaffe KM. Headache after pediatric traumatic brain injury: a cohort study. Pediatrics. 2012;129(1):e31-e39. [DOI] [PubMed] [Google Scholar]
- 9. Booker J, Sinha S, Choudhari K, Dawson J, Singh R. Description of the predictors of persistent post-concussion symptoms and disability after mild traumatic brain injury: the SHEFBIT cohort. Br J Neurosurg. 2019;33(4):367-375. [DOI] [PubMed] [Google Scholar]
- 10. Broglio SP, McCrea M, McAllister T, et al. A national study on the effects of concussion in collegiate athletes and US military service academy members: the NCAA-DoD Concussion Assessment, Research and Education (CARE) Consortium structure and methods. Sports Med. 2017;47(7):1437-1451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Broshek DK, De Marco AP, Freeman JR. A review of post-concussion syndrome and psychological factors associated with concussion. Brain Injury. 2015;29(2):228-237. [DOI] [PubMed] [Google Scholar]
- 12. Carney N, Ghajar J, Jagoda A, et al. Concussion guidelines step 1: systematic review of prevalent indicators. Neurosurgery. 2014;75(1):S3-S15. [DOI] [PubMed] [Google Scholar]
- 13. Chin EY, Nelson LD, Barr WB, McCrory P, McCrea MA. Reliability and validity of the Sport Concussion Assessment Tool-3 (SCAT3) in high school and collegiate athletes. Am J Sports Med. 2016;44(9):2276-2285. [DOI] [PubMed] [Google Scholar]
- 14. Committee on Sports-Related Concussions in Youth; Board on Children, Youth, and Families; Institute of Medicine; National Research Council; Graham R, Rivara FP, Ford MA, et al. eds. Sports-Related Concussions in Youth: Improving the Science, Changing the Culture. Washington (DC): National Academies Press (US); 2014. Appendix C, Clinical Evaluation Tools. [PubMed] [Google Scholar]
- 15. Concussion in Sport Group. SCAT3: Sport Concussion Assessment Tool - 3rd ed. Br J Sports Med. 2013:259-262. [Google Scholar]
- 16. Corrigan P. How stigma interferes with mental health care. Am Psych. 2004;59(7):614-625. [DOI] [PubMed] [Google Scholar]
- 17. Corwin DJ, Zonfrillo MR, Master CL, et al. Characteristics of prolonged concussion recovery in a pediatric subspecialty referral population. J Pediatr. 2014;165(6):1207-1215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Covassin T, Zynda AJ, Loftin MC, Pollard-McGrandy AM, Tracey AJ, Tomczyk CP. Changes in state and trait anxiety throughout concussion recovery in high school and college-aged individuals. J Athl Train. 2023;58(9):775-780. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Damsgård E, Fors T, Anke A, Røe C. The Tampa Scale of Kinesiophobia: a Rasch analysis of its properties in subjects with low back and more widespread pain.J Rehabil Med. 2007;39(9):672-678. [DOI] [PubMed] [Google Scholar]
- 20. Derogatis L. BSI 18: Brief Symptom Inventory 18: Administration, Scoring, and Procedure Manual. Minneapolis, MN: NCS Pearson; 2001. [Google Scholar]
- 21. Derogatis L, Fitzpatrick M. The SCL-90-R, the Brief Symptom Inventory (BSI), and the BSI-18. In: Maruish ME, ed. Instruments for Adults: The Use of Psychological Testing for Treatment Planning and Outcomes Assessment. Vol. 3. 3rd ed. Mahwah, NJ: Lawrence Erlbaum Associates; 2004. [Google Scholar]
- 22. Dyson R, Renk K. Freshmen adaptation to university life: depressive symptoms, stress, and coping. J Clin Psychol. 2006;62(10):1231-1244. [DOI] [PubMed] [Google Scholar]
- 23. Egan K. Supporting mental health and well-being among student-athletes. Clin Sports Med. 2019;38(4):537-544. [DOI] [PubMed] [Google Scholar]
- 24. Eisenberg MA, Andrea J, Meehan W, Mannix R. Time interval between concussions and symptom duration. Pediatrics. 2013;132(1):8-17. [DOI] [PubMed] [Google Scholar]
- 25. Ellis MJ, Ritchie LJ, Koltek M, et al. Psychiatric outcomes after pediatric sports-related concussion. J Neurosurg Pediatr. 2015;16(6):709-718. [DOI] [PubMed] [Google Scholar]
- 26. Franke GH, Jaeger S, Glaesmer H, Barkmann C, Petrowski K, Braehler E. Psychometric analysis of the brief symptom inventory 18 (BSI-18) in a representative German sample. BMC Med Res Methodol. 2017;17(1):14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Goreth MB, Palokas M. The association of premorbid neuropsychological conditions with pediatric mild traumatic brain injury/concussion recovery time and symptom severity: a systematic review protocol. JBI Database System Rev Implement Rep. 2018;16(3):603-608. [DOI] [PubMed] [Google Scholar]
- 28. Guerriero RM, Kuemmerle K, Pepin MJ, Taylor AM, Wolff R, Meehan WP, III. The association between premorbid conditions in school-aged children with prolonged concussion recovery. J Child Neurol. 2018;33(2):168-173. [DOI] [PubMed] [Google Scholar]
- 29. Guskiewicz KM, McCrea M, Marshall SW, et al. Cumulative effects associated with recurrent concussion in collegiate football players. JAMA. 2003;290(19):2549-2555. [DOI] [PubMed] [Google Scholar]
- 30. Haase E. Impacts of Depression and Anxiety on an Adolescent’s Concussion Recovery: An Examination of Mediation and Moderation Effects. PhD thesis. Washington, DC: The George Washington University; 2014. [Google Scholar]
- 31. Hang B, Babcock L, Hornung R, Ho M, Pomerantz WJ. Can computerized neuropsychological testing in the emergency department predict recovery for young athletes with concussions? Pediatr Emerg Care. 2015;31(10):688-693. [DOI] [PubMed] [Google Scholar]
- 32. Henry LC, Elbin RJ, Collins MW, Marchetti G, Kontos AP. Examining recovery trajectories after sport-related concussion with a multimodal clinical assessment approach. Neurosurgery. 2016;78(2):232-241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Hoge CW, Castro CA, Messer SC, McGurk D, Cotting DI, Koffman RL. Combat duty in Iraq and Afghanistan, mental health problems, and barriers to care. New Engl J Med. 2004:351(1):13-22. [DOI] [PubMed] [Google Scholar]
- 34. Ibrahim AK, Kelly SJ, Adams CE, Glazebrook C. A systematic review of studies of depression prevalence in university students. J Psychiatr Res. 2013;47(3):391-400. [DOI] [PubMed] [Google Scholar]
- 35. Iverson GL, Gardner AJ, Terry DP, et al. Predictors of clinical recovery from concussion: a systematic review. Br J Sports Med. 2017;51(12):941-948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Iverson GL. Outcome from mild traumatic brain injury. Curr Opin Psychiatry. 2005;18(3):301-317. [DOI] [PubMed] [Google Scholar]
- 37. Jayakody K, Gunadasa S, Hosker C. Exercise for anxiety disorders: systematic review. Br J Sports Med. 2014;48(3):187-196. [DOI] [PubMed] [Google Scholar]
- 38. Jørgensen MB, Damsgård E, Holtermann A, Anke A, Søgaard K, Røe C. Properties of the Tampa Scale for kinesiophobia across workers with different pain experiences and cultural backgrounds: a Rasch analysis. J Appl Meas. 2015:16(2):218-227. [PubMed] [Google Scholar]
- 39. Karr JE, Iverson GL, Huang SJ, Silverberg ND, Yang C-C. Perceived change in physical, cognitive, and emotional symptoms after mild traumatic brain injury in patients with pre-injury anxiety or depression. J Neurotrauma. 2020;37(10):1183-1189. [DOI] [PubMed] [Google Scholar]
- 40. Kisch J, Leino EV, Silverman MM. Aspects of suicidal behavior, depression, and treatment in college students: results from the spring 2000 National College Health Assessment Survey. Suicide Life Threat Behav. 2005;35(1):3-13. [DOI] [PubMed] [Google Scholar]
- 41. Kostyun RO, Hafeez I. Protracted recovery from a concussion: a focus on gender and treatment interventions in an adolescent population. Sports Health. 2015;7(1):52-57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Lancaster MA, McCrea MA, Nelson LD. Psychometric properties and normative data for the Brief Symptom Inventory-18 (BSI-18) in high school and collegiate athletes. Clin Neuropsychol. 2016;30(2):338-350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Langlois JA, Rutland-Brown W, Wald MM. The epidemiology and impact of traumatic brain injury: a brief overview. J Head Trauma Rehabil. 2006;21(5):375-378. [DOI] [PubMed] [Google Scholar]
- 44. Lawlor DA, Hopker SW. The effectiveness of exercise as an intervention in the management of depression: systematic review and meta-regression analysis of randomised controlled trials. BMJ. 2001;322(7289):763-767. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Leddy M, Lambert M, Ogles B. Psychological consequences of athletic injury among high-level competitors. Res Q Exerc Sport. 1994;65(4):347-354. [DOI] [PubMed] [Google Scholar]
- 46. Lindsey BJ, Fabiano P, Stark C. The prevalence and correlates of depression among college students. Coll Student J. 2009;43(4):999-1014. [Google Scholar]
- 47. Lumba-Brown A, Teramoto M, Zhang R, et al. Multicentre evaluation of anxiety and mood among collegiate student athletes with concussion. BMJ Open Sport Exerc Med. 2023;9(1):e001446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. McCauley SR, Wilde EA, Miller ER, et al. Preinjury resilience and mood as predictors of early outcome following mild traumatic brain injury. J Neurotrauma. 2013;30(8):642-652. [DOI] [PubMed] [Google Scholar]
- 49. McCrea M, Barr WB, Guskiewicz K, et al. Standard regression-based methods for measuring recovery after sport-related concussion. J Int Neuropsy Soc. 2005;11(1):58-69. [DOI] [PubMed] [Google Scholar]
- 50. McCrea M, Broglio S, McAllister T, et al. Return to play and risk of repeat concussion in collegiate football players: comparative analysis from the NCAA Concussion Study (1999-2001) and CARE Consortium (2014-2017). Br J Sports Med. 2020;54(2):102-109. [DOI] [PubMed] [Google Scholar]
- 51. McCrea M, Guskiewicz KM, Marshall SW, et al. Acute effects and recovery time following concussion in collegiate football players. JAMA. 2003;290(19):2556-2563. [DOI] [PubMed] [Google Scholar]
- 52. McCrea M, Guskiewicz K, Randolph C, Barr WB, et al. Incidence, clinical course, and predictors of prolonged recovery time following sport-related concussion in high school and college athletes. J Int Neuropsycholog Soc. 2013;19(1):22-33. [DOI] [PubMed] [Google Scholar]
- 53. McCrory P, Meeuwisse W, Dvorak J, et al. Consensus statement on concussion in sport - the 5th international conference on concussion in sport held in Berlin, October 2016. Br J Sports Med. 2017;51(11):838-847. [DOI] [PubMed] [Google Scholar]
- 54. Meehan WP, III, Mannix R, Monuteaux MC, Stein CJ, Bachur RG. Early symptom burden predicts recovery after sport-related concussion. Neurology. 2014;83(24):2204-2210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Meeuwisse WH, Fowler PJ. Frequency and predictability of sports injuries in intercollegiate athletes. Can J Sports Sci. 1988;13(1):35-42. [PubMed] [Google Scholar]
- 56. Meeuwisse WH, Sellmer R, Hagel BE. Rates and risks of injury during intercollegiate basketball. Am J Sports Med. 2003;31(3):379-385. [DOI] [PubMed] [Google Scholar]
- 57. Mittenberg W, DiGiulio DV, Perrin S, Bass AE. Symptoms following mild head injury: expectation as aetiology. J Neurol Neurosurg Psychiatry. 1992;55(3):200-204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Morgan CD, Zuckerman SL, Lee YM, et al. Predictors of postconcussion syndrome after sports concussion in young athletes: a matched case-control study. J Neurosurg Pediatr. 2015;15(6):589-598. [DOI] [PubMed] [Google Scholar]
- 59. National Institute of Mental Health. Statistics. https://www.nimh.nih.gov/health/statistics/index.shtml. Accessed January 1, 2021.
- 60. NCAA. NCAA GOALS Study of the Student-Athlete Experience: Initial Summary of Findings. Indianapolis, IN: NCAA; ; 2016. [Google Scholar]
- 61. Peterson RA, Helibronner RL. The anxiety sensitivity index: construct validity and factor analytic structure. J Anxiety Disord. 1987;1(2):117-121. [Google Scholar]
- 62. Ponsford J, Cameron P, Fitzgerald M, Grant M, Mikocka-Walus A, Schönberger M. Predictors of postconcussive symptoms 3 months after mild traumatic brain injury. Neuropsychology. 2012;26(3):304-313. [DOI] [PubMed] [Google Scholar]
- 63. Ponsford J, Nguyen S, Downing M, et al. Factors associated with persistent post-concussion symptoms following mild traumatic brain injury in adults. J Rehabil Med. 2019;51(1):32-39. [DOI] [PubMed] [Google Scholar]
- 64. Proctor SL, Boan-Lenzo C. Prevalence of depressive symptoms in male intercollegiate student-athletes and nonathletes. J Clin Sport Psychol. 2010;4(3):204-220. [Google Scholar]
- 65. Putukian M, Purcell L, Schneider KJ, et al. Clinical recovery from concussion - return to school and sport: a systematic review and meta-analysis. Br J Sports Med. 2023;57(12):798-809. [DOI] [PubMed] [Google Scholar]
- 66. Putukian M, Riegler K, Amalfe S, Bruce J, Echemendia R. Preinjury and postinjury factors that predict sports-related concussion and clinical recovery time. Clin J Sports Med. 2021;31(1):15-22. [DOI] [PubMed] [Google Scholar]
- 67. Rao AL, Asif IM, Drezner JA, Toresdahl BG, Harmon KG. Suicide in national collegiate athletic association (NCAA) athletes: a 9-year analysis of the NCAA resolutions database. Sports Health. 2015;7(5):452-457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68. R Core Team. R: A Language and Environment for Statistical Computing. R Foundation for Statistical Computing, Vienna, Austria; 2020. [Google Scholar]
- 69. Remington N. Low validity of self-report in identifying recent mental health diagnosis among US service members completing pre-deployment health assessment (PreDHA) and deployed to Afghanistan, 2007: a retrospective cohort study. BMC Public Health. 2009;9:376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70. Saeed SA, Antonacci DJ, Bloch RM. Exercise, yoga, and meditation for depressive and anxiety disorders. Am Fam Physician. 2010;81(8):981-986. [PubMed] [Google Scholar]
- 71. Sarac N, Sarac B, Pedroza A, Borchers J. Epidemiology of mental health conditions in incoming division I collegiate athletes. Phys Sportsmed. 2018;46(2):242-248. [DOI] [PubMed] [Google Scholar]
- 72. Simon JE, Docherty CL. Current health-related quality of life is lower in former Division I collegiate athletes than in non-collegiate athletes. Am J Sport Med. 2014;42(2):423-429. [DOI] [PubMed] [Google Scholar]
- 73. Storch EA, Storch JB, Killiany EM, Roberti JW. Self-reported psychopathology in athletes: a comparison of intercollegiate student-athletes and non-athletes. J Sport Behav. 2005;28:86-98. [Google Scholar]
- 74. Tarkenton T, Hynan L, Didehbani N, Silver C, Cullum M. Does trauma influence post-concussive symptom recovery in youth? Arch Clin Neuropsychol. 2019;34(6):843. [Google Scholar]
- 75. Theadom A, Starkey N, Barker-Collo S, et al. Population-based cohort study of the impacts of mild traumatic brain injury in adults four years post-injury. PloS ONE. 2018;13(1):e0191655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76. Watson JC, Kissinger DB. Athletic participation and wellness: implications for counseling college student-athletes. J Coll Couns. 2007;10(2):153-162. [Google Scholar]
- 77. Weber ML, Dean JHL, Hoffman NL, et al. Influences of mental illness, current psychological state, and concussion history on baseline concussion assessment performance. Am J Sports Med. 2018;46(7):1742-1751. [DOI] [PubMed] [Google Scholar]
- 78. Wegner M, Helmich I, Machado S, et al. Effects of exercise on anxiety and depression disorders: review of meta-analyses and neurobiological mechanisms. CNS Neurol Disord Drug Targets. 2014;13(6):1002-1014. [DOI] [PubMed] [Google Scholar]
- 79. Whittaker R, Kemp S, House A. Illness perceptions and outcome in mild head injury: a longitudinal study. J Neurol Neurosurg Psychiatry. 2007;78(6):644-646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80. Wiese-Bjornstal DM, Smith AM, Shaffer SM, Morrey MA. An integrated model of the response to sport injury: psychological and sociological dynamics. J Appl Sport Psychol. 1998;10(1):46-69. [Google Scholar]
- 81. Wolanin A, Gross M, Hong E. Depression in athletes: prevalence and risk factors. Curr Sports Med Rep. 2015;14(1):56-60. [DOI] [PubMed] [Google Scholar]
- 82. Wolanin A, Hong E, Marks D, et al. Prevalence of clinically elevated depressive symptoms in college athletes and differences by gender and sport. Br J Sports Med. 2016;50(3):167-171. [DOI] [PubMed] [Google Scholar]
- 83. Yang J, Peek-Asa C, Corlette J, Cheng G, Foster DT, Albright J. Prevalence of and risk factors associated with symptoms of depression in competitive collegiate student athletes. Clin J Sport Med. 2007;17(6):481-487. [DOI] [PubMed] [Google Scholar]
- 84. Yang J, Peek-Asa C, Covassin T, Torner JC. Post-concussion symptoms of depression and anxiety in Division I collegiate athletes. Dev Neuropsychol. 2015;40:18-23. [DOI] [PubMed] [Google Scholar]
- 85. Zemek R, Barrowman N, Freedman SB, et al. Clinical risk score for persistent postconcussion symptoms among children with acute concussion in the ED. JAMA. 2016;315(10):1014-1025. [DOI] [PubMed] [Google Scholar]