Abstract
Context:
Anterior cruciate ligament (ACL) tears are a common orthopaedic injury, and the incidence of ACL reconstruction (ACLR) continues to increase. Current clinical practice guidelines (CPGs) recognize the role of psychological factors in rehabilitation, but patient-reported outcome measures (PROs) and psychological readiness are rarely incorporated into rehabilitation.
Objective:
The purpose of this review was to highlight the importance of psychological health after ACL injury, understand the current metrics used to monitor psychological recovery, and outline how psychological recovery can be better incorporated in current CPGs.
Data Sources:
A systematic review was conducted using the Preferred Reporting Items for Systematic reviews and Meta-Analyses guidelines (PRISMA); 63 studies were identified with a PubMed search using the term “ACL Injuries/psychology”.
Study Selection:
Exclusion criteria included lack of consideration of psychological effects or studies validating PROs after ACLR. Studies were reviewed by multiple reviewers, and a total of 38 studies were included after applying exclusion criteria.
Study Design:
Systematic review.
Level of Evidence:
Level 3b.
Data Extraction:
Two independent reviewers analyzed the included articles to extract sample size, psychological readiness scale or other measures used, and key results.
Results:
Psychological outcomes, especially kinesiophobia and fear of reinjury, are seen commonly after ACLR. Psychological factors were shown to impede return to sport (RTS), alter measurable knee biomechanics, and potentially increase the risk for re-rupture. Targeted interventions such as kinesiotaping, knee bracing, and imagery training can help improve psychological and functional testing after ACLR.
Conclusion:
ACLR is often complicated by psychological factors. Psychological readiness is a crucial yet often unincorporated part of rehabilitation. Patients with higher levels of kinesiophobia and lower psychological readiness to RTS specifically should be identified to allow for administration of interventions, such as imagery training, knee bracing, or kinesiotaping, that can mitigate the negative effects of psychological outcomes and improve recovery.
Keywords: ACL, athletic training, knee, ligaments, physical therapy/rehabilitation, psychological aspects of sport
Anterior cruciate ligament (ACL) tears are a common orthopaedic injury with an incidence of isolated ACL tears of 68.6 per 100,000 person-years. In female patients, the highest incidence for ACL tears is between 14 and 18 years old, compared with 19 to 25 years old for male patients. 38 The rate of ACL tears after athletic activities is significantly higher in high school female athletes compared with that in male athletes. 15 The incidence of ACL reconstruction (ACLR) continues to increase, from 61.4 per 100,000 person-years in 2002 to 74.6 per 100,000 person-years in 2014.15,18 This increase may be due to increasing activity level among patients and a desire to return to activity after ACL injury, or potentially due to changes in treatment patterns.30,38
Current clinical practice guidelines (CPGs) for return to play and rehabilitation after ACLR were summarized in a 2020 review article. 2 Early full weightbearing and immediate knee mobilization within the first week can increase joint range of motion, reduce knee pain, and prevent soft tissue adverse events. Incorporation of isometric, closed, and open kinetic chain strength exercises should also be implemented in rehabilitation. While progression through rehabilitation is made on an individual basis, most therapists use at least 1 method of objective measurement. 16 Objective data most often include a combination of knee strength via dynamometry or repetition maximum (rep-max) testing and functional testing via Y-balance testing, hop testing, lateral stepdown testing, and functional movement screening, to name a few. 16 For final return to sport (RTS), CPGs recommend graft biological healing, clinical assessment, functional assessment, and psychological assessment milestones to determine whether the patient should progress in their rehabilitation. 2
As outlined above, most of the metrics used to aid in progression of rehabilitation focus on external measures of strength and functional testing. While patient-reported outcome measures (PROs) and psychological assessment are noted to be important based on CPGs, this has not translated to practice. 19 Based on a recent report surveying physical therapists, less than half reported using PROs, and even less implemented some form of psychological readiness. 16 When looking at the ACLR patient population themselves, only around 50% of patients had some form of PRO data available. 36 When PROs were available, the Lower Extremity Functional Scale was the most common PRO reported. 16 Specifically regarding psychological recovery, <10% of physical therapists reported incorporating PROs related to fear or athletic confidence into the rehabilitation process. 16
ACL injuries are associated with numerous psychological after-effects that may influence return to play, but psychological readiness is not currently a point of emphasis in ACLR recovery and rehabilitation. Early studies into psychological recovery indicate its importance in the rehabilitation process and final return to play.5,6,7,20 Hesitancy, lack of confidence, fear of reinjury, and lack of a support system have all been cited to negatively influence functional outcomes.6,46 On the other hand, reduced pain catastrophizing, higher knee self-efficacy, and strong support systems during rehabilitation were seen to help instill a positive outlook on injury and increased the odds of meeting rehabilitation criteria.6,8 Psychological readiness is not currently a central component of ACLR rehabilitation, but it is known to significantly influence patient outcomes after ACL injury. The goals of this review were to highlight the importance of psychological health after ACL injury, understand the current metrics used to monitor psychological recovery after injury, and outline how psychological recovery can be better incorporated in current CPGs.
Methods
A systematic review was conducted using the Preferred Reporting Items for Systematic reviews and Meta-Analyses guidelines (PRISMA). A literature review was performed in December 2022 using PubMed, OVID, and EMBASE. All literature pertaining to the evaluation of psychological readiness in ACL injuries was identified. Identifying the target literature involved a MeSH term search of PubMed using the search term “ACL Injuries/psychology”.
Inclusion criteria included articles in the English language or with English language translation, mention of ACL injuries and evaluation, and mention of psychological aspects of ACL injuries. Exclusion criteria included lack of consideration of psychological effects or studies validating PROs after ACLR.
The MeSH search resulted in 63 citations for initial identification. With the above inclusion and exclusion criteria, after screening the titles and abstracts, 38 studies were eligible for analysis and the full-length texts were obtained (Figure 1).
Figure 1.
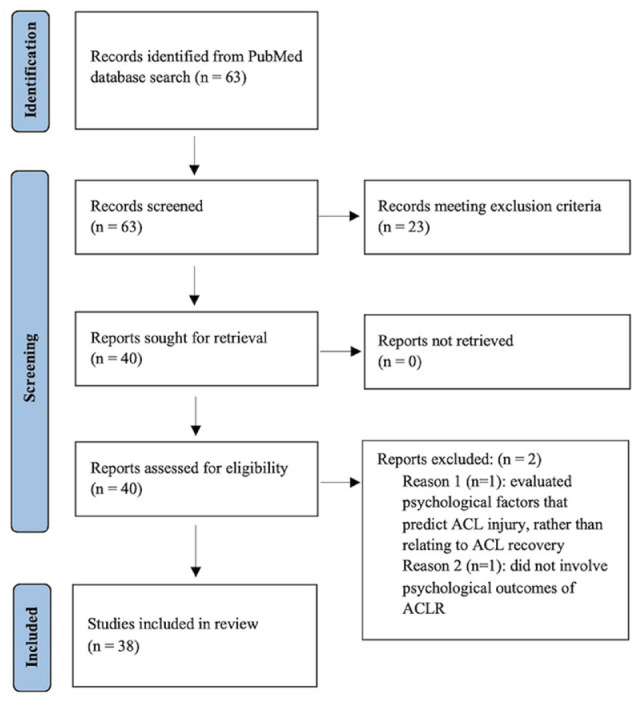
PRISMA flowchart of study. ACL, anterior cruciate ligament; ACLR, ACL reconstruction; PRISMA, Preferred Reporting Items for Systematic reviews and Meta-Analyses.
Analysis of each article included recording data of (1) sample size, (2) timing of screening/intervention, (3) psychological readiness scale or other measure used, (4) statistical measures, (5) study objective, and (6) main results.
Results
The 38 included studies in this review analyzed a variety of topics related to psychological factors after ACLR. Of these 38 studies, 5 identified and described psychological outcomes after ACLR, and 13 identified associations between psychological or other PROs and outcomes after ACLR, including RTS; 9 studies explored the role of psychological factors on knee biomechanics; 3 studies evaluated the role of psychological factors in ACL re-rupture; 5 studies analyzed a potential role of sex in different psychological outcomes after ACLR; 1 study proposed a link between psychological dysfunction and abnormal motor function after ACLR; and 4 studies looked at the impact on various interventions on psychological factors after ACLR.
Patient and Study Characteristics
The sample sizes of patients varied widely, ranging from 9 to 635 patients post-ACLR.39,48 There was also a wide range of screening tools used (Table 1). The most used tools were the Tampa Kinesiophobia Scale (TSK), ACL Return to Sport after Injury (ACL-RSI), Tegner Activity Scale, International Knee Documentation Committee (IKDC), and Knee Injury and Osteoarthritis Outcome Score (KOOS); 14 studies used the TSK,3,8,10,11,17,21,23,24,26,29,33,44,45,47 13 studies used the ACL-RSI,13,22,23,25 -27,31,34,35,41,43,48,50 11 studies used the Tegner Activity Scale,3,11,13,23,24,23,29,34,41,45,49 10 studies used the IKDC,8,10,29,32,41,42,45,47 -49 and 10 studies used the KOOS.3,10,11,21,24,29,35,39,44,47 Other PROs included the ACL-Quality of Life (ACL-QoL),13,41 Knee Activity Self-Efficacy (KASE),8,26 Self-Efficacy for Rehabilitation (SER), 8 Knee Self-Efficacy Scale (K-SES),3,10,13,34,35 Photograph Series of Sports Activities for ACLR (PHOSA-ACLR), 21 Lysholm Scale,9,24 Fear-Avoidance Belief Questionnaire (FABQ), 4 Pain Catastrophizing Scale (PCS),8,10,3,44 Marx Activity Scale,33,49 Global Rating Scale (GRS), 17 International Physical Activity Questionnaire, 24 Single Assessment Numeric Evaluation (SANE), 13 General Self-Efficacy Scale (GSE), 13 Athlete Fear Avoidance Questionnaire, 11 Lower Extremity Functional Scale (LEFS), 47 Athletic Coping Skills Inventory 28 (ACSI-28), 12 Godin Leisure-Time Exercise questionnaire, 29 and Subjective Patient Outcome for Return to Sports (SPORTS). 10
Table 1.
Patient-reported outcome measures
| Name of PRO | What It Measures | Interpretation of Score |
|---|---|---|
| ACL-RSI | Psychological readiness for sport participation | Higher score = increased psychological readiness (cut-off of 70 for return to sport) |
| ACL-QoL | Knee-related QoL | Higher score = better quality of life |
| TSK | Kinesiophobia, or pain-related fear of movement/reinjury | Higher score = greater kinesiophobia |
| KASE | Self-efficacy, or confidence, for performing activities involving the knee | Higher score = greater self-efficacy |
| SER | Confidence or self-efficacy in performing tasks encountered in rehabilitation after knee or hip surgery | Higher score = greater rehabilitation self-efficacy |
| K-SES | How certain the patient is about certain activities despite pain or discomfort | Higher score = increased self-efficacy |
| PHOSA-ACLR | Fear of harm | Higher score = more fear of harm |
| KOOS | Self-reported functioning | Higher score = better function |
| Lysholm scale | Knee function after knee ligament injury | Higher score = better function |
| FABQ | Fear-avoidance beliefs | Higher score = more fear-avoidance beliefs |
| PCS | Patient’s frequency in engaging in pain catastrophizing behaviors | Higher score = increased pain catastrophizing |
| IKDC-SKF | Knee-specific evaluation of symptoms, function, and sport activity | Higher score = fewer limitations |
| Tegner activity scale | Level of activity before injury and postinjury | Higher score = higher level of activity |
| Marx activity scale | Level of activity in patients with knee disorders who participate in sports | Higher score = higher level of activity |
| GRS | Self-reported knee function | Higher score = better function |
| International Physical Activity Questionnaire | Last 7 days of physical activity | Open-ended questions on physical activity |
| SANE | Function as pertaining to area of injury in comparison with preinjury baseline | Higher score = better function |
| GSE | Optimistic self-beliefs to cope with variety of difficult demands | Higher score = increased self-efficacy |
| Athlete Fear Avoidance Questionnaire | Sport-injury-related fear avoidance in athletes | Higher score = higher fear avoidance |
| LEFS | Lower extremity function | Higher score = better function |
| ACSI-28 | Athlete’s psychological coping skills | Higher score = better coping skills |
| Godin Leisure-Time Exercise questionnaire | How many times per week the patient engages in strenuous, moderate, or mild/light exercise | Higher score = higher level of activity |
| SPORTS | Athlete’s ability to return to their sport | Higher score = more complete return |
ACL, anterior cruciate ligament; ACL-QoL, ACL-Quality of Life; ACLR, ACL reconstruction; ACL-RSI, ACL Return to Sport after Injury; ASCI-28, ; Athletic Coping Skills Inventory FABQ, Fear-Avoidance Belief Questionnaire; GRS, Global Rating Scale; GSE, General Self-Efficacy Scale; IKDC-SKF, International Knee Documentation Committee Subjective Knee Form; KASE, Knee Activity Self-Efficacy; KOOS, Knee Injury and Osteoarthritis Outcome Score; K-SES, Knee Self-Efficacy Scale; LEFS, Lower Extremity Functional Scale; PCS, Pain Catastrophizing Scale; PHOSA-ACLR, Photograph Series of Sports Activities for ACLR; PRO, patient-reported outcome measure; QoL, qualify of life; SANE, Single Assessment Numeric Evaluation; SER, Self-Efficacy for Rehabilitation Outcome; SPORTS, Subjective Patient Outcome for Return to Sports; TSK, Tampa Kinesiophobia Scale.
Psychological Outcomes After ACLR
Five studies described the psychological outcomes of ACL injury and ACLR, primarily fear of reinjury and loss of identity. Neural processing and muscle coordination after negative emotional stimuli were evaluated in patients after ACLR compared with healthy controls. Fear- and injury-related pictures resulted in lower valence (more sadness), higher arousal values, and increased fear compared with neutral pictures, and this effect was greater in patients after ACLR. Sport knee injury-related pictures induced greater heartrate deceleration and parietal power in the ACLR group than the fear-related pictures. During acoustic startle conditions, fearful pictures increased joint stiffness in the ACLR group at mid- and long-range compared with neutral pictures. 1 Furthermore, patients with ACL injuries have described their injury as a disruptive “journey” that profoundly influenced their lives. Patients reported a loss of identity and how life at the present had changed from their previous experience. These factors were influenced by support systems and experiences with their care team. The injury overall was found to cause a dramatic change to their lives, which was also reflected in a lower knee-related quality of life reports. 3
Impacts of Psychological Factors on ACLR Outcomes and RTS
A total of 13 studies evaluated the impact of psychological factors on outcomes after ACLR, including RTS. A review paper identified factors affecting patient expectations and satisfaction after ACLR. One article found that 65% of respondents described their knowledge of ACL injury and surgical management as “little” or “none.” Expectations of surgery included return to normal or nearly normal condition and no increased osteoarthritis risk. Another study found strong correlations between patient-derived subjective knee rating scores and patient satisfaction in ACLR patients. Many studies have found that higher patient expectations preoperatively have been associated with more dissatisfaction postoperatively. 9 Higher expectations for surgical outcomes were also associated with lower self-reported knee function. 10
Many studies reported the impacts of psychological factors on ACLR outcomes. Poorer coping skills as measured by the ACSI-28 were found to be correlated with delayed recovery time. 12 It was also found that higher levels of fear of movement or reinjury, lower self-efficacy, and higher pain catastrophizing were correlated with lower odds of RTS, lower self-reported knee function, lower knee-related quality of life, and greater knee pain.10,44 From completion of patient interviews, it was found that those who felt hesitant or lacked confidence in their knees described limiting their involvement in sports or activity. Many patients also reported hyperawareness of both knee function and their ability to perform competitively after injury. 5 More pain catastrophizing was also associated with increased pain intensity. 8
Multiple studies found an impact on psychological factors in RTS or progression in rehabilitation. Not returning to sport (NRTS) was associated with lower self-reported knee function, less satisfaction with activity level, and lower motivation during rehabilitation to RTS, but similar function on a variety of physical performance measures.42,49 Those who returned to a greater extent estimated preoperatively that it was possible to return to their earlier activity level compared with those who had not returned. 42 The highest reported reason for NRTS was fear of reinjury, followed by lack of confidence. 32 Persons with elevated levels of self-reported kinesiophobia were 17% less likely to RTS. 3 It was also found that patients reported more psychosocial barriers than physical barriers to RTS, including feeling that sport-based activities were now associated with injury, a persistent sense of uncertainty regarding full recovery, and a sense that comparison with others with ACLR by parents or coaches hindered their ability to progress. 11 Patients ready for advanced rehabilitation also had higher self-reported knee function and lower fear of reinjury compared with patients not ready for advanced rehabilitation. 8
Impacts of Psychological Factors on Knee Biomechanics
Nine studies specifically analyzed the effect of psychological variables on biomechanical data for the affected limb. Patients with higher fear of reinjury had higher biceps femoris electromyographic (EMG) amplitude and higher anterior-posterior co-contraction index during landing than patients with lower fear of reinjury and controls. These patients also had more trunk, hip, and knee flexion compared with controls. 24 Separately, a negative relationship was seen between fear of reinjury and knee, hip, and trunk flexion, with a positive relationship related to hip adduction and gluteus maximus preparatory activity. 45 Activity level overall was reduced 2 to 5 years after ACL injury compared with preinjury, but in general there was symmetric functional performance with mean limb symmetry index (LSI) >90% on all performance tests and at best weak correlations between performance tests and PROs. 41 Age and LSI of quadriceps strength at 3 months were significant predictors of ACL-RSI scores at 9 months in multiple regression analysis. 43 With regards to knee kinematics, ACL-RSI was seen to correlate with 2 kinematic variables: knee flexion angle at initial contact (IC) and peak knee flexion (PKF). Lower ACL-RSI scores were associated with greater limb asymmetry. At IC, the low ACL-RSI group displayed less knee flexion in the surgical limb versus nonsurgical limb, while middle and high groups did not display interlimb differences. For PKF, the low, middle, and high groups all displayed less PKF in the surgical limb compared with the nonsurgical limb. 50 Corroborating these findings of knee asymmetry, a separate study noted that patients who did not recover symmetrical muscle function at the 12-month follow-up reported inferior knee-related self-efficacy and quality of life than patients who recovered symmetrical muscle function at almost all follow-ups. The proportion of patients who stated they achieved their rehabilitation goal at 12 months was 17% for the entire cohort, 24% for patients who recovered muscle function, and 5% for patients who did not recover muscle function. 35 Results have also reported on functional testing, where kinesiophobia was associated with lesser hamstring strength, hop performance, and patient-reported function, as well as an overall worse recovery from ACLR. 29
Impacts of Psychological Factors on ACL Re-Rupture
Three studies analyzed the impact of psychological factors on re-rupture of the ACL after primary reconstruction. While there was no difference in psychological readiness seen at the preoperative time point, patients who sustained a second injury trended toward lower psychological readiness at 12 months compared with noninjured patients. Younger patients (<20 years) with second ACL injury had significantly lower psychological readiness to RTS than young noninjured patients, but no difference was found in older patients. 25 Conversely, ACL re-rupture patients were found to have greater psychological readiness (greater confidence in performance, lesser negative emotions, and lesser risk appraisal) to RTS at 8 months and 12 months, and greater knee-related self-efficacy at 8 months and 12 months compared with matched groups. ACL re-rupture patients also had a greater level of present knee-strenuous sport measured with the Tegner Activity Scale after their primary ACLR compared with controls at 12 months. Lastly, patients who later had a second ACL injury had a greater TSK-11 score at the time of RTS than those who did not suffer a second ACL injury. Patients with a TSK-11 score of ≥19 at the time of RTS were 13 times more likely to suffer a second ACL tear within 24 months after RTS. 33
Role of Sex in Psychological Outcomes After ACLR
Five studies found a potential role of sex in psychological outcomes after ACLR. One study found that female sex was a significant contributor for NRTS. 48 It was also found that male patients had significantly lower fear of harm, as measured by PHOSA-ACLR score, than female patients, and that female sex was related to fear of reinjury after ACLR.13,21 Two studies identified sex differences in factors related to psychological readiness. Male patients reported a stronger sense of internal locus of control using positive internal reinforcement, whereas female patients described balancing internal and external control and valuing external support systems. Male participants described mood changes influenced by physical and social limitations, referring to the inability to take part in social activities. Female participants closely monitored their emotions throughout recovery and were more influenced by rehabilitation fluctuations (changed day to day). Short-term, men were more apt to focus on physical limitations (ie, smaller muscles), whereas women tended to focus on limitations in physical fitness and wanting to stay in shape. Both groups expressed fear related to movement and activity, but male participants emphasized sport-specific movements like cutting, landing, or those caused by other athletes, while female participants had more fear with activities of daily living and general forms of activity. Female participants encountered a more noticeable daily disruption in their athletic identity after injury, but found positive experiences with engaging with the team, while male participants had negative experiences with continued team involvement.23,40
Effects of Interventions on Psychological Factors After ACLR
Four studies identified how certain interventions altered psychological impairment after ACLR. In an advanced training program, KASE score was higher in the training versus no training group, but the ACL-RSI, TSK-11, and fear intensity scores were not significantly different between groups. The RTS criteria passing rate was not significantly different between groups at baseline or follow-up; however, the training group showed better progression toward meeting RTS criteria at follow-up, including a higher proportion meeting the hop test criterion. 26 The use of knee braces and kinesiotaping were found to be effective in improving balance and hop distance compared with no intervention but only use of knee braces was found to increase quadricep and hamstring torque. Knee braces were found to also improve self-reported knee function. 17 Another advanced group training program was found to improve mean ACL-RSI and single-leg hop test scores and led to more patients meeting ACL-RSI and single-hop test threshold scores for RTS. 27 Imagery training was also shown to be effective in reducing fear and was posed as a potential method to assist in reduction in anxiety, pain, and tension, ultimately reducing psychological distress in the patient. 37
Study characteristics are summarized in Appendix Tables A1 and A2, available in the online version of this article.
Discussion
This review has highlighted the crucial role that psychological factors play in ACL injuries and recovery (Figure 2). Psychological recovery is an important aspect of the entire rehabilitation process and begins preoperatively. Managing expectations of surgery and recovery are crucial, and surgeons need to provide an honest outlook of what patients can expect on an individual basis. Patients do not often realize that surgery is only the beginning of the recovery period. It has been shown that many ACLR patients do not have a strong knowledge base of ACL injuries or the surgical management, and that patients often expect return to normal or nearly normal conditions. Higher preoperative expectations have been shown to be associated with more dissatisfaction after operation, highlighting the importance of patient counseling in recovery.9,10 It should be emphasized that surgery addresses the injury, but that physical therapy and commitment after surgery will truly determine success.
Figure 2.

Effects of poor psychological function on ACLR recovery. ACLR, anterior cruciate ligament reconstruction.
After surgical repair, there are a variety of psychological outcomes that present after ACL injury and surgery. One important complication of ACL injuries is kinesiophobia, involving lack of confidence in the injured knee, hyperawareness of mobility restrictions, and fear of reinjury. Kinesiophobia was commonly seen in this review, demonstrating its high incidence after ACLR. Psychological factors in turn influence RTS and functional outcomes. Satisfaction with activity level, motivation during rehabilitation to RTS, belief that it is possible to return to the same level of activity, and self-reported knee function were all vital factors in RTS that differed between those who did and did not return.42,49 Most importantly, kinesiophobia was a major driver in NRTS. Multiple studies found that persons with elevated kinesiophobia were less likely to RTS.3,8,10,11,22,32 Specifically, those with higher self-reported kinesiophobia were 17% less likely to RTS. 3 Importantly, however, physical performance measures did not differ between those who did and did not RTS. This indicates that patients who are functionally ready to RTS are being held back by psychological barriers that are not addressed in rehabilitation. 49 Lower levels of kinesiophobia were also associated with improvement of symptom resolution, higher activity, higher self-reported knee function, and higher knee-related quality of life.4,10,33,44 Poorer coping skills were also associated with delayed recovery time. 12 Kinesiophobia, poor coping skills, satisfaction, and motivation may therefore predict who is at risk for delayed progression through rehabilitation and failed RTS. These patients may necessitate further intervention and support.
Psychological recovery also has an impact on measurable knee biomechanics. Patients with higher TSK scores had higher biceps femoris EMG amplitude and higher anterior-posterior co-contraction index during landing, greater hip adduction and gluteus maximus preparatory activity,24,45 as well as lower levels of activity, lower limb symmetry, and lower quadriceps strength symmetry. 33 Higher kinesiophobia was also found to be associated with lower hamstring strength, hop performance, greater hamstring fatigue, and less regional function. 29 Effects of trunk, hip, and knee flexion were varied, with 1 study showing more flexion with more fear of reinjury, and another study showing less flexion.24,45 These studies demonstrate the risk associated with higher fear of reinjury, including altered limb biomechanics that could predispose to future injury.
Targeted interventions have been shown to improve psychological barriers in ACLR rehabilitation. Use of kinesiotaping and knee braces were found to improve self-reported knee function and performance on functional testing in patients after ACLR, potentially indicating their use in reducing kinesiophobia and giving patients more confidence and improved strength and performance. 17 Imagery training was also shown to be useful in reducing fear of reinjury, providing another potential intervention for patients with significant kinesiophobia. 29 These interventions can therefore bolster both psychological and functional testing parameters in those who need it.
There are certain patient populations for which psychological outcomes may require greater attention. Psychological factors were shown to play a vital role in potential re-rupture after ACLR, indicating the importance of psychological measures in second-time ACL injuries. Patients with a TSK-11 score of ≥19 at the time of RTS were found to be 13 times more likely to suffer a second ACL tear. 33 Younger patients with lower psychological readiness by ACL-RSI were also found to be at higher risk for ACL re-rupture. 25 However, these data are not conclusive, as too much confidence may also be a risk for second injury, as 1 study found that greater psychological readiness to RTS and knee-related self-efficacy may be associated with re-rupture within 2 years of ACLR. 34 This indicates the profound need for psychological screening of patients after ACLR to maximize prevention of a second injury. Sex was found to have a potential role in recovery as well, as female participants were noted to have a higher fear of reinjury in several studies.48,13,2. However, other studies did not note a difference, indicating that future research is needed to determine whether sex-specific interventions are warranted. 23
Based on this review, the authors suggest several guidelines for incorporating psychological monitoring during ACLR rehabilitation. First, this process starts preoperatively. It is imperative to ensure that patients understand honest surgical and rehabilitation outcomes. A realistic and clear set of expectations could help improve satisfaction and outcomes after surgery. Fear of movement or reinjury, pain catastrophizing, and impaired psychological readiness have been shown to be associated with a range of negative outcomes after ACLR, indicating that the ACL-RSI and/or TSK-11 screening tools should be incorporated regularly into PROs. If patients with impaired psychological readiness and/or kinesiophobia are identified, measures can be taken to help improve their psychological profile and mitigate negative outcomes. Intervening quickly with bracing, kinesiotaping, and/or imagery training may be indicated to help mitigate negative effects. Patients should also be encouraged to increase mobility outside of rehabilitation as much as possible. Doing so could allow the patient to build confidence without a physical therapist and experience their knee on their own. This could increase confidence, reduce fear of reinjury, and reduce pain catastrophizing by helping patients learn that their knee is safe. In patients that are consistently scoring poorly on psychological PROs, special attention should be paid to knee kinematics and biomechanics in recovery. Pathologic asymmetry was found to occur to a higher degree in these patients, which may predispose them to future injury. Finally, tracking and managing psychological recovery is even more crucial in cases of re-rupture, as psychological outcomes have been correlated with reinjury risk.
Gagnier et al 14 conducted a review of the existing currently available patient-reported outcome questionnaires for patients with ACL injury. They found that the ACL-RSI was a reliable and valid tool for assessment of patients after ACLR and was the highest quality instrument overall. This indicates that the ACL-RSI may be an effective first step in adding psychological PROs consistently to the rehabilitation process after ACLR. Patient-reported outcome questionnaires are easy and quick to administer and can have a profound impact on the patient’s recovery process. 28
As demonstrated by this review, most patients who undergo ACLR are impacted on some psychological level. Especially with return to play, psychological readiness plays an extremely important, yet unincorporated, part of rehabilitation. Barriers to RTS are often psychological rather than physical, demonstrating that including psychological monitoring as part of the ACL rehabilitation process is crucial to effective recovery. Identifying patients with higher levels of kinesiophobia and lower psychological readiness to RTS can allow for interventions, such as imagery training, knee bracing, or kinesiotaping, that can mitigate the multiple negative effects that can come from poor psychological outcomes. Nearly every patient can benefit from tracking psychological readiness. In those with poor psychological recovery, this also serves as another site of intervention that has been shown to help both RTS and recovery of normal daily function and identity.
Supplemental Material
Supplemental material, sj-docx-1-sph-10.1177_19417381241256930 for Impact of Psychological Factors on Rehabilitation After Anterior Cruciate Ligament Reconstruction: A Systematic Review by Victoria J. Nedder, Akash G. Raju, Andrew J. Moyal, Jacob G. Calcei and James E. Voos in Sports Health
Supplemental material, sj-docx-2-sph-10.1177_19417381241256930 for Impact of Psychological Factors on Rehabilitation After Anterior Cruciate Ligament Reconstruction: A Systematic Review by Victoria J. Nedder, Akash G. Raju, Andrew J. Moyal, Jacob G. Calcei and James E. Voos in Sports Health
Acknowledgments
The authors would like to thank the medical students, Victoria Nedder and Akash Raju, for putting together this literature review on behalf of the School of Medicine and University Hospitals.
Footnotes
The authors report no potential conflicts of interest in the development and publication of this article.
ORCID iD: Victoria J. Nedder  https://orcid.org/0000-0002-9044-5315
https://orcid.org/0000-0002-9044-5315
References
- 1. An YW, Lobacz AD, Baumeister J, et al. Negative emotion and joint-stiffness regulation strategies after anterior cruciate ligament injury. J Athl Train. 2019;54(12):1269-1279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Andrade R, Pereira R, van Cingel R, Staal JB, Espregueira-Mendes J. How should clinicians rehabilitate patients after ACL reconstruction? A systematic review of clinical practice guidelines (CPGs) with a focus on quality appraisal (AGREE II). Br J Sports Med. 2020;54(9):512-519. [DOI] [PubMed] [Google Scholar]
- 3. Baez SE, Hoch MC, Hoch JM. Psychological factors are associated with return to pre-injury levels of sport and physical activity after ACL reconstruction. Knee Surg Sports Traumatol Arthrosc. 2020;28(2):495-501. [DOI] [PubMed] [Google Scholar]
- 4. Barchek AR, Dlugonski D, Baez SE, Hoch MC, Hoch J. The relationship between injury-related fear and physical activity in people with a history of anterior cruciate ligament reconstruction. Phys Ther Sport. 2021;50:201-205. [DOI] [PubMed] [Google Scholar]
- 5. Burland JP, Lepley AS, Cormier M, DiStefano LJ, Arciero R, Lepley LK. Learned helplessness after anterior cruciate ligament reconstruction: an altered neurocognitive state? Sports Med. 2019;49(5):647-657. [DOI] [PubMed] [Google Scholar]
- 6. Burland JP, Toonstra J, Werner JL, Mattacola CG, Howell DM, Howard JS. Decision to return to sport after anterior cruciate ligament reconstruction, Part I: a qualitative investigation of psychosocial factors. J Athl Train. 2018;53(5):452-463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Burland JP, Toonstra JL, Howard JS. Psychosocial barriers after anterior cruciate ligament reconstruction: a clinical review of factors influencing postoperative success. Sports Health. 2019;11(6):528-534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Chmielewski TL, George SZ. Fear avoidance and self-efficacy at 4 weeks after ACL reconstruction are associated with early impairment resolution and readiness for advanced rehabilitation. Knee Surg Sports Traumatol Arthrosc. 2019;27(2):397-404. [DOI] [PubMed] [Google Scholar]
- 9. Cole BJ, Cotter EJ, Wang KC, Davey A. Patient understanding, expectations, outcomes, and satisfaction regarding anterior cruciate ligament injuries and surgical management. Arthroscopy. 2017;33(5):1092-1096. [DOI] [PubMed] [Google Scholar]
- 10. Coronado RA, Bley JA, Huston LJ, et al. Composite psychosocial risk based on the fear avoidance model in patients undergoing anterior cruciate ligament reconstruction: cluster-based analysis. Phys Ther Sport. 2021;50:217-225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. DiSanti J, Lisee C, Erickson K, Bell D, Shingles M, Kuenze C. Perceptions of rehabilitation and return to sport among high school athletes with anterior cruciate ligament reconstruction: a qualitative research study. J Orthop Sports Phys Ther. 2018;48(12):951-959. [DOI] [PubMed] [Google Scholar]
- 12. Ellis HB, Sabatino M, Nwelue E, Wagner KJ, III, Force E, Wilson P. The use of psychological patient reported outcome measures to identify adolescent athletes at risk for prolonged recovery following an ACL reconstruction. J Pediatr Orthop. 2020;40(9):e844-e852. [DOI] [PubMed] [Google Scholar]
- 13. Filbay S, Kvist J. Fear of reinjury following surgical and nonsurgical management of anterior cruciate ligament injury: an exploratory analysis of the NACOX multicenter longitudinal cohort study. Phys Ther. 2022;102(2):pzab273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Gagnier JJ, Shen Y, Huang H. Psychometric properties of patient-reported outcome measures for use in patients with anterior cruciate ligament injuries: a systematic review. JBJS Rev. 2018;6(4):e5. [DOI] [PubMed] [Google Scholar]
- 15. Gornitzky AL, Lott A, Yellin JL, Fabricant PD, Lawrence JT, Ganley TJ. Sport-specific yearly risk and incidence of anterior cruciate ligament tears in high school athletes: a systematic review and meta-analysis. Am J Sports Med. 2016;44(10):2716-2723. [DOI] [PubMed] [Google Scholar]
- 16. Greenberg EM, Greenberg ET, Albaugh J, Storey E, Ganley TJ. Rehabilitation practice patterns following anterior cruciate ligament reconstruction: a survey of physical therapists. J Orthop Sports Phys Ther. 2018;48(10):801-811. [DOI] [PubMed] [Google Scholar]
- 17. Harput G, Ulusoy B, Ozer H, Baltaci G, Richards J. External supports improve knee performance in anterior cruciate ligament reconstructed individuals with higher kinesiophobia levels. Knee. 2016;23(5):807-812. [DOI] [PubMed] [Google Scholar]
- 18. Herzog MM, Marshall SW, Lund JL, Pate V, Mack CD, Spang JT. Trends in incidence of ACL reconstruction and concomitant procedures among commercially insured individuals in the United States, 2002-2014. Sports Health. 2018;10(6):523-531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Kaye JA, Spence D, Alexanders J. Using a biopsychosocial approach within ACL rehabilitation: an exploration of student physiotherapists’ perceptions and experiences. Physiother Theory Pract. 2022;38(11):1718-1730. [DOI] [PubMed] [Google Scholar]
- 20. Kosaka M, Nakase J, Numata H, et al. Psychological traits regarding competitiveness are related to the incidence of anterior cruciate ligament injury in high school female athletes. Knee. 2016;23(4):681-685. [DOI] [PubMed] [Google Scholar]
- 21. Lankveld WV, Pat-El RJ, Melick NV, Cingel RV, Staal JB. Is fear of harm (FoH) in sports-related activities a latent trait? The item response model applied to the Photographic Series of Sports Activities for Anterior Cruciate Ligament Rupture (PHOSA-ACLR). Int J Environ Res Public Health. 2020;17(18):6764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Liew BXW, Feller JA, Webster KE. Understanding the psychological mechanisms of return to sports readiness after anterior cruciate ligament reconstruction. PLoS One. 2022;17(3):e0266029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Lisee CM, DiSanti JS, Chan M, et al. Gender differences in psychological responses to recovery after anterior cruciate ligament reconstruction before return to sport. J Athl Train. 2020;55(10):1098-1105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Markström JL, Grinberg A, Häger CK. Fear of reinjury following anterior cruciate ligament reconstruction is manifested in muscle activation patterns of single-leg side-hop landings. Phys Ther. 2022;102(2):pzab218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. McPherson AL, Feller JA, Hewett TE, Webster KE. Psychological readiness to return to sport is associated with second anterior cruciate ligament injuries. Am J Sports Med. 2019;47(4):857-862. [DOI] [PubMed] [Google Scholar]
- 26. Meierbachtol A, Obermeier M, Yungtum W, et al. Advanced training enhances readiness to return to sport after anterior cruciate ligament reconstruction. J Orthop Res. 2022;40(1):191-199. [DOI] [PubMed] [Google Scholar]
- 27. Meierbachtol A, Yungtum W, Paur E, Bottoms J, Chmielewski TL. Psychological and functional readiness for sport following advanced group training in patients with anterior cruciate ligament reconstruction. J Orthop Sports Phys Ther. 2018;48(11):864-872. [DOI] [PubMed] [Google Scholar]
- 28. Nagao M, Doi T, Saita Y, et al. A novel patient-reported outcome measure for anterior cruciate ligament injury: evaluating the reliability, validity, and responsiveness of Japanese anterior cruciate ligament questionnaire 25. Knee Surg Sports Traumatol Arthrosc. 2016;24(9):2973-2982. [DOI] [PubMed] [Google Scholar]
- 29. Norte GE, Solaas H, Saliba SA, Goetschius J, Slater LV, Hart JM. The relationships between kinesiophobia and clinical outcomes after ACL reconstruction differ by self-reported physical activity engagement. Phys Ther Sport. 2019;40:1-9. [DOI] [PubMed] [Google Scholar]
- 30. Nyland J, Gamble C, Franklin T, Caborn DNM. Permanent knee sensorimotor system changes following ACL injury and surgery. Knee Surg Sports Traumatol Arthrosc. 2017;25(5):1461-1474. [DOI] [PubMed] [Google Scholar]
- 31. Ohji S, Aizawa J, Hirohata K, et al. The psychological readiness to return to sports of patients with anterior cruciate ligament reconstruction preoperatively and 6 months postoperatively. Phys Ther Sport. 2021;50:114-120. [DOI] [PubMed] [Google Scholar]
- 32. Patel NK, Sabharwal S, Hadley C, Blanchard E, Church S. Factors affecting return to sport following hamstrings anterior cruciate ligament reconstruction in non-elite athletes. Eur J Orthop Surg Traumatol. 2019;29(8):1771-1779. [DOI] [PubMed] [Google Scholar]
- 33. Paterno MV, Flynn K, Thomas S, Schmitt LC. Self-reported fear predicts functional performance and second ACL injury after ACL reconstruction and return to sport: a pilot study. Sports Health. 2018;10(3):228-233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Piussi R, Beischer S, Thomeé R, et al. Greater psychological readiness to return to sport, as well as greater present and future knee-related self-efficacy, can increase the risk for an anterior cruciate ligament re-rupture: a matched cohort study. Arthroscopy. 2022;38(4):1267-1276.e1. [DOI] [PubMed] [Google Scholar]
- 35. Piussi R, Beischer S, Thomeé R, Hamrin Senorski E. Superior knee self-efficacy and quality of life throughout the first year in patients who recover symmetrical muscle function after ACL reconstruction. Knee Surg Sports Traumatol Arthrosc. 2020;28(2):555-567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Randsborg PH, Cepeda N, Adamec D, Rodeo SA, Ranawat A, Pearle AD. Patient-reported outcome, return to sport, and revision rates 7-9 years after anterior cruciate ligament reconstruction: results from a cohort of 2042 patients. Am J Sports Med. 2022;50(2):423-432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Rodriguez RM, Marroquin A, Cosby N. Reducing fear of reinjury and pain perception in athletes with first-time anterior cruciate ligament reconstructions by implementing imagery training. J Sport Rehabil. 2019;28(4):385-389. [DOI] [PubMed] [Google Scholar]
- 38. Sanders TL, Maradit Kremers H, Bryan AJ, et al. Incidence of anterior cruciate ligament tears and reconstruction: a 21-year population-based study. Am J Sports Med. 2016;44(6):1502-1507. [DOI] [PubMed] [Google Scholar]
- 39. Scott SM, Perry MA, Sole G. “Not always a straight path”: patients’ perspectives following anterior cruciate ligament rupture and reconstruction. Disabil Rehabil. 2018;40(19):2311-2317. [DOI] [PubMed] [Google Scholar]
- 40. Sims M, Mulcahey MK. Sex-specific differences in psychological response to injury and return to sport following ACL reconstruction. JBJS Rev. 2018;6(7):e9. [DOI] [PubMed] [Google Scholar]
- 41. Sonesson S, Kvist J, Ardern C, Österberg A, Silbernagel KG. Psychological factors are important to return to pre-injury sport activity after anterior cruciate ligament reconstruction: expect and motivate to satisfy. Knee Surg Sports Traumatol Arthrosc. 2017;25(5):1375-1384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Sonesson S, Österberg A, Gauffin H, Ardern CL, Kvist J, Hägglund M. Low correlation between functional performance and patient reported outcome measures in individuals with non-surgically treated ACL injury. Phys Ther Sport. 2021;47:185-192. [DOI] [PubMed] [Google Scholar]
- 43. Suzuki M, Ishida T, Matsumoto H, et al. Psychological readiness at 9 months after anterior cruciate ligament reconstruction - which factors affect? Phys Ther Sport. 2022;58:74-79. [DOI] [PubMed] [Google Scholar]
- 44. Tichonova A, Rimdeikienė I, Petruševičienė D, Lendraitienė E. The relationship between pain catastrophizing, kinesiophobia and subjective knee function during rehabilitation following anterior cruciate ligament reconstruction and meniscectomy: a pilot study. Medicina (Kaunas). 2016;52(4):229-237. [DOI] [PubMed] [Google Scholar]
- 45. Trigsted SM, Cook DB, Pickett KA, Cadmus-Bertram L, Dunn WR, Bell DR. Greater fear of reinjury is related to stiffened jump-landing biomechanics and muscle activation in women after ACL reconstruction. Knee Surg Sports Traumatol Arthrosc. 2018;26(12):3682-3689. [DOI] [PubMed] [Google Scholar]
- 46. van Lankveld W, van Melick N, Habets B, Roelofsen E, Staal JB, van Cingel R. Measuring individual hierarchy of anxiety invoking sports related activities: development and validation of the Photographic Series of Sports Activities for Anterior Cruciate Ligament Reconstruction (PHOSA-ACLR). BMC Musculoskelet Disord. 2017;18(1):287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Van Wyngaarden JJ, Jacobs C, Thompson K, et al. Quadriceps strength and kinesiophobia predict long-term function after ACL reconstruction: a cross-sectional pilot study. Sports Health. 2021;13(3):251-257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Webster KE, Nagelli CV, Hewett TE, Feller JA. Factors associated with psychological readiness to return to sport after anterior cruciate ligament reconstruction surgery. Am J Sports Med. 2018;46(7):1545-1550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Werner JL, Burland JP, Mattacola CG, Toonstra J, English RA, Howard JS. Decision to return to sport participation after anterior cruciate ligament reconstruction, Part II: self-reported and functional performance outcomes. J Athl Train. 2018;53(5):464-474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Zarzycki R, Failla M, Capin JJ, Snyder-Mackler L. Psychological readiness to return to sport is associated with knee kinematic asymmetry during gait following anterior cruciate ligament reconstruction. J Orthop Sports Phys Ther. 2018;48(12):968-973. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-docx-1-sph-10.1177_19417381241256930 for Impact of Psychological Factors on Rehabilitation After Anterior Cruciate Ligament Reconstruction: A Systematic Review by Victoria J. Nedder, Akash G. Raju, Andrew J. Moyal, Jacob G. Calcei and James E. Voos in Sports Health
Supplemental material, sj-docx-2-sph-10.1177_19417381241256930 for Impact of Psychological Factors on Rehabilitation After Anterior Cruciate Ligament Reconstruction: A Systematic Review by Victoria J. Nedder, Akash G. Raju, Andrew J. Moyal, Jacob G. Calcei and James E. Voos in Sports Health


