Abstract
Objective
To investigate the difference in bone-implant contact (BIC) and the rate of infratemporal fossa intrusion among different apex sites for quad zygomatic implants (ZIs) design in edentulous patients with severe alveolar bone resorption.
Methods
Patients with maxillary edentulism were evaluated. Alveolar bone resorption was assessed using the Cawood and Howell classification. Participants with Class IV or Class V/VI bone resorption were selected. The zygomatic bone was devided into upper, middle and lower thirds, with four potential implant apex locations identified in each third. Virtual planning for quad ZIs, along with measurements of BIC were performed. Additionally, the occurrence of ZIs intrusion into the infratemporal fossa was examined, and the distance between ZI and orbital cavity was measured.
Results
A total of 28 CBCT scans of edentulous patients, encompassing 56 zygomas, were analyzed. Thirty-nine single lateral posterior edentulous jaws were classified into Class IV subgroup, while 17 into Class V/IV subgroup. Among all patients and patients in subgroups, the anterior and posterior ZI exhibited the highest BIC at points A3 and B2, respectively. The average zygomatic BIC at A3 apex point was 18.3 ± 3.9 mm, and that at the B2 apex point was 16.3 ± 5.3 mm. Quad ZIs risk intrusion into the infratemporal fossa when positioned at B2, B3, and at all apex points of the lower zygoma segment. Three anterior ZIs at A3 point show less than 1 mm distance to orbital cavity. Overall, A3 and B1 apex points showed high BIC and low infratemporal intrusion rate for quad ZIs, irrespective of patient’s alveolar bone resorption status.
Conclusions
The optional apex point for anterior and posterior quad ZIs is A3 and B1, respectively, regardless of the patients’s alveolar bone resorption level. Alveolar bone resorption does not affect the BIC for quad ZIs. Anterior ZI positioned at A3 point may present high risk for orbital penetration and may not be reccomended in a Quad ZI approach.
Trial registration
The clinical research is registered under the number ChiCTR2100044472.
Keywords: Edentulous, Quad zygomatic implants, Bone-implant contact, Infratemporal fossa, Optional apex point
Background
Edentulism is often a critical yet challenging case in prosthodontics. Numerous clinical studies have confirmed that implant-supported prostheses can provide substantially improved oral function rehabilitation [1, 2]. For patients with severe alveolar bone resorption, zygomatic implants (ZIs) offer a reliable and effective solution for oral rehabilitation. Studies indicate that in such patients, the success rate of zygomatic implants ranges from 94.2–100% [3–7].
The concept of zygomatic implants was introduced by Branemark in 1990 [8, 9]. Subsequently, numerous enhancements and innovations in ZI techniques have been developed [10–18]. For patients with severe maxillary alveolar bone loss, a single ZI on each side may not provide adequate stability for full-arch implant restoration and could increase potential risks. The currently recommended approach is to place two ZIs on each side, i.e., quad zygomatic implants. This can offer ample support for full-arch prosthesis in edentulous patients [19, 20].
Quad ZIs occupy a significant portion of the zygomatic bone and require precise placement. It is crucial to evaluate the zygoma’s structure and determine the suitable apex point for ZI insertion before proceeding with quad zygomatic approach. The success and durability of ZIs hinge on the extent of bone-implant contact (BIC) within the zygoma. Moreover, the implant should not harm adjacent maxillofacial structures, thereby preventing intra- and post-operative complications. The zygoma’s inner aspect is close to the infratemporal fossa, home to vital neurovascular elements like the pterygoid plexus, maxillary artery and its offshoots, and the maxillary and mandibular nerve branches. Injury to these structures can result in severe complications, including deep hematomas, sensory and motor impairments, and potentially fatal outcomes. Therefore, careful placement of quad ZIs is imperative to avoid encroaching on the infratemporal fossa and avert serious postoperative complications. Moreover, orbital cavity penetration has been reported as a intra-operative complication with the incidence of 5.9% [21]. As a typical and the most serious ZI therapy complication, orbital penetration by ZI could lead to severe pain in the region of the orbit, persistent anesthesia, physiological abduction and elevation of the involved eye [22], extraocular muscle injury, diplopia [23], eye movement limitation [24], etc. Intranasinus technique may increase the risk of orbit invasion due to lack of vision and control of the drills during implant bed preparation [25].
The alveolar ridge is categorized into six stages of resorption severity according to the Cawood and Howell classification [26]. For patients exhibiting varying degrees of alveolar bone loss, the location for quad zygomatic implants may vary. Currently, few research has been conducted to compare the choices of implant sites among patients with different levels of alveolar bone resorption.
Two studies assessed the zygomatic BIC of quad ZIs using Cone Beam Computed Tomography (CBCT) images [19, 27]. Hung et al. evaluated the zygomatic BIC at various implant sites and its association with the infratemporal fossa, proposing the most suitable implant location in the zygoma [19]. This research focused on an Asian demographic. Conversely, Bertos et al. conducted their research on a European cohort, examining the influence of alveolar bone resorption on the BIC of quad ZIs, the volume of implant-engaged zygoma bone, and its correlation with the maxillary sinus. Nevertheless, there is still a lacking of research on how alveolar bone resorption affects the BIC and its relationship with the infratemporal fossa at individual ZI sites.
This study aims to investigate the difference in BIC, the infratemporal fossa intrusion, and the relationship between ZIs and orbit among differenct apex sites for quad ZIs placement in edentulous patients with varying degrees of alveolar bone loss.
Methods
Patient selection
This study received approval from the Institutional Review Board of the University (Ethical Approval No: PKUSSIRB-202162013). The clinical research is registered under the number ChiCTR2100044472 (18/03/2021).
Edentulous patients in need of implant treatment who underwent CBCT scans at the University dental school clinic between October 2019 and August 2021, and who met the inclusion/exclusion criteria, were included in the study. All participants read and signed informed consents.
Inclusion criteria: (1) Patient age over 18 years old; (2) Maxillary edentulism for a minimum of 3 months; (3) Require implant restoration, and undergo a CBCT examination; (4) Have read and signed the informed consent form; (5) Alveolar bone resorption classified as either Class IV or Class V/VI according to the Cawood & Howell classification.
Exclusion criteria : (1) Anatomical abnormalities in the maxilla or zygoma; (2) Severe facial asymmetry; (3) Alveolar bone resorption classified from level I to III according to the Cawood & Howell classification; (4) Edentulism due to maxillofacial trauma or tumor resection surgery.
Classification of alveolar bone resorption level
The edentulous patients’ alveolar bone resorption was categorized using the Cawood & Howell classification as per Bertos et al. [13]. A knife-edge ridge form of the residual ridge, insufficient in width and exceeding 5 mm in height, was classified as Class IV alveolar bone resorption. Conversely, a flat residual ridge, insufficient in width and less than 5 mm in height, was classified as Class V/VI alveolar bone resorption. The level of alveolar bone resorption was assessed individually on each side, utilizing both two-dimensional and three-dimensional CBCT reconstructed images.
Virtual implant planning
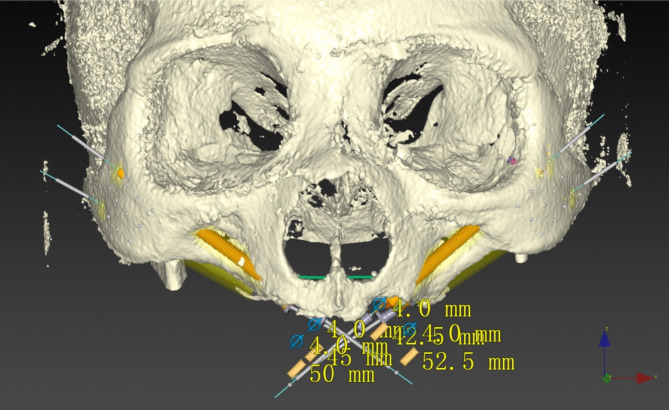
CBCT data was exported in the Digital Imaging and Communications in Medicine (DICOM) format and imported into the planning software (Nobel Clinician 2.10.1.3, Nobel Biocare). For each side of the maxilla and zygoma, two zygomatic implants (Branemark System Zygoma Tiunite RP) were virtually planned in accordance with protocols from previously published articles [19, 27], namely one anterior zygomatic implant and one posterior implant, totaling four implants per case (Fig. 1).
Fig. 1.
Quad zygomatic implants designed in edentulous maxilla
Implant site selection
Entery point on the alveolar ridge
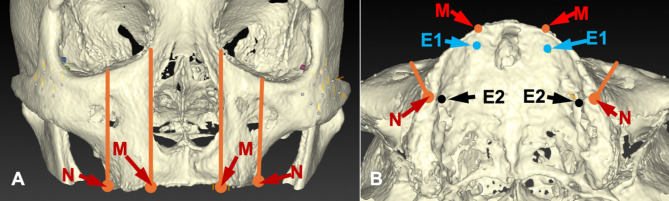
Points E1 and E2 are designated on the alveolar ridge (Fig. 2). Point E1 is located 5 mm palatally from where the lowest point of the maxillary alveolar ridge intersects with a perpendicular line extending from the lateral margin of the nasal incisure [28]. When viewing the maxilla from above, point E2 is situated 5 mm palatally from where The lowermost point of the alveolar crest was identified by taking a line at a tangent to the lateral margin of the infraorbital foramen. The degree of alveolar bone resorption is assessed individually at points E1 and E2 [19, 27, 28].
Fig. 2.
The determination of Point E1 and E2. (A) The lowest point (Point M) of the maxillary alveolar ridge intersects with a perpendicular line extending from the lateral margin of the nasal incisure. The lowermost point (Point N) of the alveolar crest was identified by taking a line at a tangent to the lateral margin of the infraorbital foramen; (B) Point E1 is located 5 mm palatally from Point M, and point E2 is situated 5 mm palatally from Point N
Apex point in the zygoma
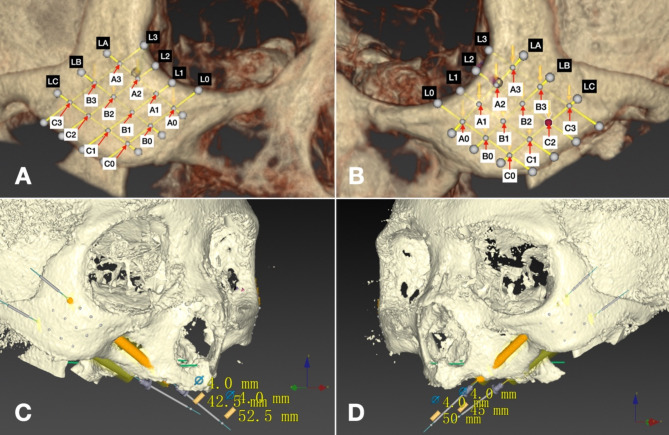
Draw a horizontal line, IM, at the lower orbital margin and a vertical line, LM, parallel to the median plane, intersecting the lateral orbital margin. At their intersection lies point C. Construct an angular bisector between IM and LM to locate point O at their intersection with the orbital margin. Connect points C and O with line L1 (Fig. 3). Shift L1 medially by 5 mm to create a parallel line L0; shift L1 laterally by 5 mm and 10 mm to form parallel lines L2 and L3, respectively. These lines extend from the orbital margin to the zygoma’s lower edge. The apex of the quad ZIs is positioned in the zygomatic bone between L0 and L3. Segment L0 and L3 into four equal parts to identify quarter points A0, B0, C0, and A3, B3, C3, from superior to inferior. Draw lines LA, LB, and LC by connecting A0 to A3, B0 to B3, and C0 to C3. The intersection points of LA, LB, LC with L1, L2 are labeled A1, B1, C1 and A2, B2, C2, respectively. The areas that the lines LA, LB, LC pass through is namely the upper, middle and lower section of the zygomatic. The 12 points thus identified represent the center of the 12 zygomatic segments [19]. The ZI apex will be positioned at these 12 points as indicated in Fig. 4.
Fig. 3.
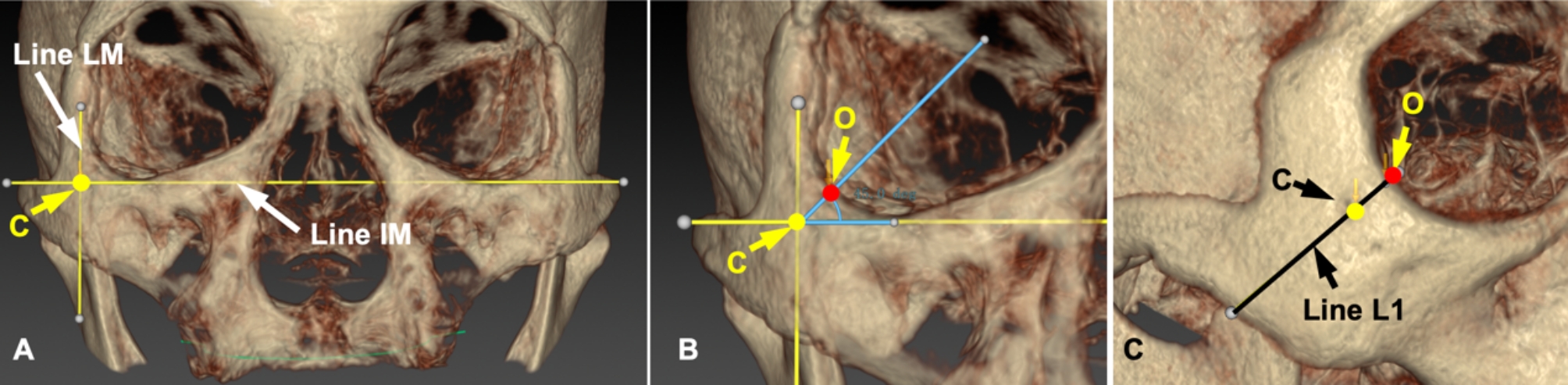
The positioning of line L1. (A) Draw a horizontal line, IM, at the lower orbital margin and a vertical line, LM, parallel to the median plane, intersecting the lateral orbital margin. At their intersection lies point C; (B) Construct an angular bisector between IM and LM to locate point O at their intersection with the orbital margin; (C) Connect points C and O with line L1
Fig. 4.
Segmentation of the zygoma and virtual placement of quad zygomatic implants with the apex targeting predetermined points. A and B, Segmentation of the left and right zygomas; C and D, Virtual quad ZIs design on the left and right zygomas with predetermined apex points
According to the previous studies of Hung and colleagues [19], the apex of the anterior ZI is positioned at the upper section (points A series), with its entry at point E1. The apex of the posterior ZI is positioned at the middle and lower sections (points B and C series), with its entry at point E2.
Measurements and data collection
The patient’s CBCT was imported into the planning software (NobelClinician 2.10.1.3, Nobel Biocare, Zurich) for virtual planning of the quad ZI site. Implant simulations (Branemark System Zygoma Tiunite RP) were virtually designed. Measurements of the quad ZIs at 12 apex locations were taken, with the following detailed metrics:
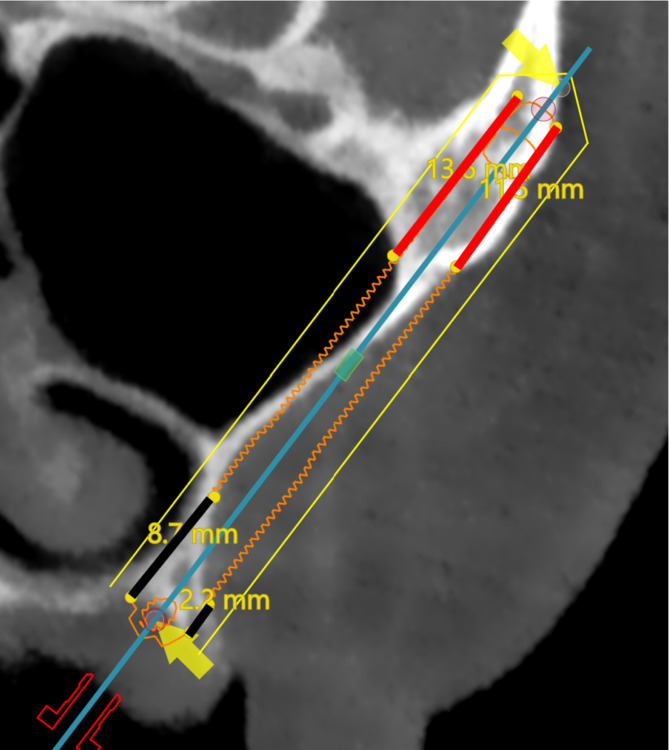
Measurements of Bone-Implant contact (BIC)
This is a linear measurement protocol. The BIC was the average value of zygomatic BIC length on the facial and the temporal sides in the facial -temporal cross section (Fig. 5) [19]. The zygomatic bone-implant contact (zBIC) and alveolar bone-implant contact (aBIC) were assessed. The average contact length between the ZI and the zygomatic or alveolar bone on both the facial and temporal sides was calculated as zBIC or aBIC, respectively. The total bone-implant contact (tBIC) represents the combined measurement of zBIC and aBIC.
Fig. 5.
The linear measurement of zygomatic bone-to-implant contact (zBIC, red lines) and the alveolar bone-to-implant (aBIC, black lines) length on the facial and the temporal sides
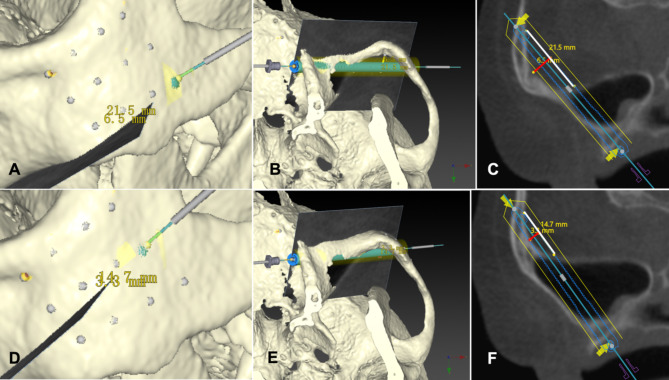
Evaluation of ZI Intrusion
The occurrence of ZI intrusion into the infratemporal fossa was examined, along with the depth and length of such intrusions (Fig. 6).
Fig. 6.
ZI intrusion into the infratemporal fossa. A & B, ZI intrusion into the infratemporal fossa when the apex point of the posterior ZI set at C3 point; C, The depth (red line) and length (white line) of ZI intrusion; D & E, ZI intrusion into the infratemporal fossa when the apex point of the posterior ZI set at B3 point; F, The depth (red line) and length (white line) of ZI intrusion
Meausrement of the distance between the orbit and the anterior implant
The closest distance between the implant and patient’s orbit cavity was measured for anterior ZI at each apex point.
Determination of Optional Zygomatic Implant position
The possible location for ZI placement within the zygoma was identified by analyzing the implant’s BIC and the frequency of infratemporal fossa intrusion and orbital penetration. This process was then applied to determine the implant sites for patients with alveolar bone resorption Class IV and V/VI. The findings from these two subgroups were compared to the overall participant data to identify any differences.
Statistical analysis
All analyses were performed with SPSS (SPSS Statistics 27.0, IBM) as follows:
A one way ANOVA was used to compare the zygomatic BIC (zBIC) and alveolar BIC (aBIC) among ZIs at various apex locations to determine the most suitable insertion points. Subsequently, BIC was assessed within each subgroup based on the degree of alveolar bone resorption, followed by a Chi-square test to compare BIC across subgroups and to ascertain the possible apex design for zygomatic implants.
A Chi-square test was employed to evaluate the frequency of ZI penetration into the infratemporal fossa among subgroups and the entire cohort. Additionally, the extent and magnitude of ZI intrusion were compared using the same statistical method.
When P is less than 0.05, it is considered that there is a significant difference.
Results
Demographics
Maxillary edentulous patients who visited the University dental school clinic from March 2021 to October 2022 for implant-supported prosthesis treatment and underwent CBCT were evaluated. A total of 48 patients were collected. The edentulous arches were classified using the Cawood and Howell classification. Of these patients, eleven were excluded because their alveolar bone classification was categorized as level III. Nine patients were excluded due to inadequate CBCT images that precluded the virtual design of zygomatic implants. Ultimately, 28 participants were included in the study, comprising 12 males and 16 females, with an average age of 63.8 ± 12.6 years. The 28 edentulous maxillae were divided into 56 hemi-maxillae, with 39 of the 56 edentulous posterior residual ridges classified as Class IV and the remaining 17 as Class V/VI. In total, 112 implants were virtually planned.
BIC of zygomatic implants
BIC of the anterior zygomatic implant
The apex points of the anterior ZIs were at A0, A1, A2, and A3. The total BIC (tBIC) and the zygomatic BIC (zBIC) of implants decreased significantly from A3 to A0 (P < 0.01, Table 1) while the alveolar BIC (aBIC) showed no significant change (P = 0.769). The average zBIC at A3, A2, A1, and A0 was 18.3 ± 3.9 mm, 13.4 ± 3.7 mm, 7.4 ± 2.8 mm, and 4.2 ± 1.7 mm respectively.
Table 1.
Total BIC, zygomatic BIC and alveolar BIC in the anterior zygomatic implants (mm)
| Entire cohort (n = 56) | Class IV Subgroup (n = 39) | Class V/VI Subgroup (n = 17) | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Mean ± SD | Min | Max | Mean ± SD | Min | Max | Mean ± SD | Min | Max | ||
| Zygomatic BIC | A0 | 4.2 ± 1.7 | 0.9 | 9.4 | 4.2 ± 1.8 | 0.9 | 9.4 | 4.1 ± 1.5 | 0.9 | 6.4 |
| A1 A1 | 7.4 ± 2.8 | 2.5 | 16.0 | 7.3 ± 2.5 | 2.5 | 14.6 | 7.5 ± 3.5 | 3.3 | 16.0 | |
| A2 | 13.4 ± 3.7 | 2.9 | 22.1 | 13.4 ± 3.2 | 2.9 | 22.1 | 13.3 ± 4.9 | 6.5 | 21.0 | |
| A3 | 18.3 ± 3.9 | 8.0 | 27.5 | 18.1 ± 3.8 | 8.0 | 24.3 | 18.7 ± 4.2 | 12.2 | 27.5 | |
| P value | P = 0.000 | P = 0.000 | P = 0.000 | |||||||
|
Alveolar BIC |
A0 | 7.6 ± 2.9 | 1.9 | 13.3 | 7.6 ± 2.8 | 2.4 | 12.9 | 7.6 ± 3.3 | 1.9 | 13.3 |
| A1 | 7.6 ± 2.9 | 2.3 | 14.8 | 7.6 ± 2.8 | 3.0 | 13.8 | 7.8 ± 3.3 | 2.3 | 14.8 | |
| A2 | 7.9 ± 3.0 | 2.3 | 15.3 | 7.8 ± 2.7 | 3.6 | 13.0 | 8.2 ± 3.6 | 2.3 | 15.3 | |
| A3 | 8.1 ± 3.2 | 2.3 | 16.2 | 8.0 ± 2.8 | 2.7 | 13.4 | 8.2 ± 4.1 | 2.3 | 16.2 | |
| P value | P = 0.769 | P = 0.849 | P = 0.939 | |||||||
| Total BIC | A0 | 11.7 ± 3.4 | 5.2 | 18.9 | 11.8 ± 3.2 | 5.4 | 18.9 | 11.7 ± 3.9 | 5.2 | 18.8 |
| A1 | 15.0 ± 4.2 | 7.0 | 23.8 | 14.9 ± 3.9 | 7.5 | 22.6 | 15.3 ± 4.9 | 7.0 | 23.8 | |
| A2 | 21.3 ± 5.6 | 8.1 | 36.2 | 21.1 ± 4.5 | 8.1 | 31.2 | 21.6 ± 7.6 | 8.8 | 36.2 | |
| A3 | 26.4 ± 5.9 | 12.75 | 41.8 | 26.2 ± 5.4 | 12.8 | 36.7 | 26.9 ± 7.0 | 14.5 | 41.8 | |
| P value | P = 0.000 | P = 0.000 | P = 0.000 | |||||||
In the Class IV subgroup, tBIC and zBIC decreased from A3 to A0, with a significant difference observed among ZIs at all apex points (P < 0.01), However, no significant difference was found in aBIC among implants at any apex points (P = 0.849).
In the Class V/VI subgroups, tBIC and zBIC also decreased from A3 to A0. A significant difference in zBIC was noted among implants at all apex points (P < 0.01), while no significant difference was observed in tBIC between implants at A3 and A2 (P = 0.217), or between those at A1 and A0 (P = 0.132). The tBIC of implants at A3 and A2 was significantly higher than that of implants at A1 and A0 (P < 0.05). No significant difference in aBIC was found among implants at any apex points (P = 0.939).
For implants at the four apex points of the upper zygoma, no significant difference in tBIC, zBIC, or aBIC was detected between the two subgroups (P > 0.05).
BIC of the posterior zygomatic implant
The apex points of the posterior implants comprised eight locations: B0, B1, B2, and B3 at the middle zygoma, and C0, C1, C2, and C3 at the lower zygoma. Within the B series, the highest zBIC and tBIC were recorded at the B2 point (16.3 ± 5.3 mm; 22.1 ± 7.5 mm), while the C series showed the highest values at the C1 point (13.8 ± 5.0 mm; 19.5 ± 5.5 mm) as indicated in Table 2. The B2 point demonstrated the highest zBIC and tBIC among all eight apex sites, with a significant difference from the other points. No significant difference in zBIC and tBIC were observed among the B1, B3, C1, and C2 points (zBIC at B3: 13.4 ± 4.8 mm, at B1: 13.5 ± 5.5 mm, at C1: 13.8 ± 5.0 mm, at C2: 12.3 ± 5.8 mm), though these were significantly higher than those at the B0, C0, and C3 points (zBIC at B0: 8.9 ± 4.9 mm, at C0: 10.9 ± 4.1 mm, at C3: 8.5 ± 4.5 mm). Across all apex points, aBIC did not show significant variation (P > 0.05) (Table 2).
Table 2.
Total BIC, zygomatic BIC and alveolar BIC in the posterior zygomatic implants (mm)
| Entire cohort (n = 56) | Class IV Subgroup (n = 39) | Class V/VI Subgroup (n = 17) | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Mean ± SD | Min | Max | Mean ± SD | Min | Max | Mean ± SD | Min | Max | ||
| Zygomatic BIC | B0 | 8.9 ± 4.9 | 1.3 | 21.4 | 8.7 ± 4.6 | 1.3 | 21.4 | 9.2 ± 5.7 | 2.3 | 20.5 |
| B1 | 13.5 ± 5.5 | 2.0 | 27.0 | 12.8 ± 5.3 | 2.0 | 27.0 | 15.2 ± 5.6 | 7.7 | 24.0 | |
| B2 | 16.3 ± 5.3 | 6.4 | 27.1 | 16.2 ± 5.3 | 6.4 | 25.3 | 16.5 ± 5.6 | 8.9 | 27.1 | |
| B3 | 13.4 ± 4.8 | 3.5 | 25.4 | 13.6 ± 4.9 | 3.5 | 25.4 | 13.1 ± 4.7 | 7.3 | 22.5 | |
| C0 | 10.9 ± 4.1 | 0.8 | 24.3 | 11.0 ± 3.9 | 0.8 | 24.3 | 10.5 ± 4.5 | 3.9 | 18.2 | |
| C1 | 13.8 ± 5.0 | 4.0 | 25.9 | 14.2 ± 5.3 | 4.0 | 25.9 | 12.8 ± 4.1 | 5.6 | 20.3 | |
| C2 | 12.3 ± 5.8 | 2.2 | 22.9 | 12.6 ± 6.3 | 2.2 | 22.9 | 11.6 ± 4.4 | 4.7 | 21.2 | |
| C3 | 8.5 ± 4.5 | 1.8 | 22.0 | 8.9 ± 5.2 | 1.8 | 22.0 | 7.5 ± 2.3 | 4.3 | 13.6 | |
| P value | P = 0.000 | P = 0.000 | P = 0.000 | |||||||
| Alveolar BIC | B0 | 5.6 ± 3.4 | 1.0 | 16.3 | 5.5 ± 3.1 | 1.0 | 14.0 | 6.0 ± 4.2 | 1.3 | 16.4 |
| B1 | 5.6 ± 3.4 | 1.0 | 14.7 | 5.4 ± 3.2 | 1.0 | 14.7 | 6.1 ± 3.9 | 1.3 | 14.7 | |
| B2 | 5.8 ± 3.6 | 1.1 | 16.0 | 5.8 ± 3.6 | 1.1 | 16.0 | 6.0 ± 3.8 | 1.4 | 14.6 | |
| B3 | 5.9 ± 3.8 | 1.2 | 18.9 | 5.8 ± 3.9 | 1.2 | 19.0 | 5.9 ± 3.7 | 1.6 | 14.6 | |
| C0 | 5.6 ± 3.4 | 1.1 | 15.4 | 6.0 ± 3.7 | 1.3 | 15.4 | 4.7 ± 2.4 | 1.1 | 9.3 | |
| C1 | 5.7 ± 3.4 | 0.9 | 14.7 | 6.0 ± 3.7 | 0.9 | 14.7 | 5.0 ± 2.4 | 1.3 | 10.0 | |
| C2 | 5.8 ± 3.5 | 1.3 | 15.1 | 6.1 ± 3.8 | 1.3 | 15.1 | 5.0 ± 2.8 | 1.4 | 9.65 | |
| C3 | 6.0 ± 3.7 | 1.1 | 14.5 | 6.3 ± 3.9 | 1.1 | 14.5 | 5.2 ± 3.0 | 1.7 | 10.8 | |
| P value | P = 0.999 | P = 0.961 | P = 0.849 | |||||||
| Total BIC | B0 | 14.5 ± 6.5 | 4.6 | 33.5 | 14.2 ± 5.5 | 4.6 | 27.8 | 15.2 ± 8.5 | 5.0 | 33.5 |
| B1 | 19.2 ± 7.0 | 6.2 | 38.6 | 18.2 ± 6.4 | 6.2 | 33.8 | 21.3 ± 7.9 | 12.9 | 38.6 | |
| B2 | 22.1 ± 7.5 | 10.5 | 38.8 | 22.0 ± 7.7 | 10.5 | 38.4 | 22.4 ± 7.2 | 13.3 | 38.8 | |
| B3 | 19.3 ± 6.8 | 8.7 | 38.8 | 19.4 ± 7.2 | 8.7 | 38.8 | 19.0 ± 6.0 | 9.8 | 35.1 | |
| C0 | 16.4 ± 5.4 | 4.4 | 29.2 | 17.0 ± 5.5 | 4.4 | 29.1 | 15.2 ± 5.3 | 8.0 | 24.3 | |
| C1 | 19.5 ± 5.5 | 7.8 | 31.2 | 20.2 ± 5.9 | 7.8 | 31.2 | 17.8 ± 4.1 | 9.8 | 23.7 | |
| C2 | 18.0 ± 5.9 | 6.6 | 34.7 | 18.7 ± 6.4 | 7.0 | 34.7 | 16.6 ± 4.4 | 6.6 | 23.2 | |
| C3 | 14.5 ± 5.5 | 6.1 | 33.3 | 15.2 ± 6.1 | 6.1 | 33.3 | 12.8 ± 3.3 | 6.8 | 18.1 | |
| P value | P = 0.000 | P = 0.000 | P = 0.000 | |||||||
In the Class IV and Class V/VI subgroups, the highest BIC was noted at the B2 point in the middle zygoma and at the C1 point in the lower zygoma. For Class IV subgroup, zBIC and tBIC at the B2 point were significantly higher compared to other apex points. Between the C1 and B1 apex points, no significant difference in zBIC and tBIC was detected. In the Class V/VI subgroup, zBIC and tBIC did not significantly differ between the B2 and B1 points, but a significant difference was found between the B2 point and other points, excluding B1 (Table 2).
No significant difference was found in aBIC and tBIC of implants at the same apex points between Class IV and V/VI subgroups.
Relationship between zygomatic implants and the Infratemporal Fossa (Table 3)
Table 3.
Intrusion rate and depth and length of quad zygomatic implant intruded into infratemporal fossa
| Apex point site | Entire cohort(n = 56) | Class IV Subgroup(n = 39) | Class V/VI Subgroup(n = 17) | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Number of ZI intrusion (%) |
average intrusion depth | average intruded length | Number of ZI (%) |
average intrusion depth | average intruded length | Number of ZI intrusion (%) |
average intrusion depth | average intruded length | ||
| Anterior ZI | A0 | 0 (0) | 0 | 0 | 0 (0) | 0 | 0 | 0 (0) | 0 | 0 |
| A1 | 0 (0) | 0 | 0 | 0 (0) | 0 | 0 | 0 (0) | 0 | 0 | |
| A2 | 0 (0) | 0 | 0 | 0 (0) | 0 | 0 | 0 (0) | 0 | 0 | |
| A3 | 1 (1.8) | 1.2 | 11.4 | 1 (2.6) | 1.2 | 11.4 | 0 (0) | 0 | 0 | |
| Posterior ZI | B0 | 0 (0) | 0 | 0 | 0 (0) | 0 | 0 | 0 (0) | 0 | 0 |
| B1 | 1 (1.8) | 2.4 | 7.2 | 0 (0) | 0 | 0 | 1 (5.9) | 2.4 | 7.2 | |
| B2 | 24 (42.9) | 2.2 ± 1.0 | 12.5 ± 3.2 | 14 (35.9) | 2.4 ± 1.0 | 13.0 ± 3.6 | 10 (58.8) | 2.0 ± 1.0 | 11.9 ± 2.5 | |
| B3 | 52 (92.9) | 3.9 ± 1.6 | 18.2 ± 4.7 | 35 (89.7) | 3.9 ± 1.7 | 18.0 ± 4.8 | 17 (100) | 3.9 ± 1.3 | 18.6 ± 4.6 | |
| C0 | 10 (17.9) | 2.5 ± 1.1 | 14.0 ± 5.8 | 6 (15.4) | 2.3 ± 0.9 | 13.8 ± 5.0 | 4 (23.5) | 2.9 ± 1.4 | 14.2 ± 7.6 | |
| C1 | 33 (58.9) | 3.3 ± 1.6 | 15.5 ± 5.0 | 22 (56.4) | 3.0 ± 1.5 | 15.1 ± 5.3 | 11 (64.7) | 3.8 ± 1.8 | 16.4 ± 4.5 | |
| C2 | 52 (92.9) | 5.2 ± 2.3 | 19.3 ± 5.8 | 36 (92.3) | 4.9 ± 2.3 | 19.1 ± 6.1 | 16 (94.1) | 5.5 ± 2.3 | 19.8 ± 5.2 | |
| C3 | 56 (100) | 7.8 ± 2.6 | 25.4 ± 5.3 | 39 (100) | 7.5 ± 2.8 | 25.3 ± 5.7 | 17 (100) | 8.3 ± 2.2 | 25.5 ± 4.5 | |
Anterior zygomatic implants and infratemporal fossa
For the anterior zygomatic implants, only one of the 56 implants (1.8%) at the A3 point intruded into the infratemporal fossa. The depth of the intrusion was 1.2 mm. No other anterior implants showed entry into the fossa. There was no significant difference in the rate of ZI intrusion among the four apex points (A series points) (P = 0.390).
The single implant that intruded into the infratemporal fossa was from the subgroup of class IV, although there was no significant difference in the rate of anterior ZI intrusion between the two subgroups.
Posterior zygomatic implants and infratemporal fossa
For the B series apex points (mid-zygoma), no implant intrusion into the infratemporal fossa was observed at B0. However, intrusion rates at B1, B2, and B3 were 1.8%, 42.9%, and 92.9%, respectively, with the average depth and length of intrusion into the infratemporal fossa increasing progressively. The average intrusion depth was 2.4 mm, 2.2 ± 1.0 mm, and 3.9 ± 1.6 mm at B1, B2, and B3 respectively. Significant differences in intrusion rates were noted between B3 and B0, and B2 and B0, but not between B1 and B0.
For the C series apex points (lower zygoma), varying rates of ZI intrusion into the infratemporal fossa were recorded across the four sites. From C0 to C3, the intrusion rate, depth and length of ZI exposure in the infratemporal fossa increased (Table 3). At the C3 apex point, all implants intruded into the infratemporal fossa, with an average intrusion depth of 7.8 ± 2.6 mm. Significant differences in intrusion rates were present among all C series sites.
In Class IV subgroup, no ZI intrusion into infratemporal fossa occurred at B0 and B1 site, while 35.9% of the ZI at B2 site and 89.7% of the ZI at B3 site showed intrusion, with intrusion depth of 2.4 ± 1.0 mm (B2) and 3.9 ± 1.7 mm (B3). For the C series apex points, 15.4% of ZI at C0, 56.4% of ZI at C1 site, and over 90% of ZI at C2 and C3 sites entered the infratemporal fossa (Table 3), with intrusion depths increasing from C0 to C3.
Within the Class V/VI subgroup, there was no ZI intrusion into the infratemporal fossa at the B0 site, and only one ZI at the B1 site (5.9%) penetrated the infratemporal fossa with an intrusion depth of 2.4 mm. In contrast, 58.8% of ZIs at the B2 site and all ZIs at the B3 site (100%) intruded into the infratemporal fossa (Table 3). Regarding the C series sites, 23.5% of ZIs at the C0 site, 64.7% of ZIs at the C1 site, and over 90% of ZIs at both the C2 and C3 sites entered the infratemporal fossa (Table 3). Although the exact values for ZI intrusion rate, as well as the average depth and length of intrusion, were higher in the Class V/VI subgroup compared to Class IVsubgroup, there was no statistically significant difference in the rate, depth, or length of ZI intrusion at any of the middle and lower zygoma apex sites between the two subgroups (P > 0.05).
The risk of orbital cavity penetration
No orbital cavity penetration was detected in all the cases at all apex points. The distance between the anterior ZI and the orbital cavity was shown in Table 4. The average distance between the anterior ZI and the orbit was 2.5 ± 1.0 mm, 3.2 ± 1.0 mm, 3.8 ± 1.0 mm, and 4.3 ± 0.9 mm at A3, A2, A1, and A0 apex points respectively. There was significant difference in ZI-orbital distance among the four apex groups (P < 0.001). No significant difference in ZI-orbital distance was found between the Class IV and Class V/VI subgroups at all the A series points. Three anterior ZI at A3 point showed less than 1 mm distance from the orbital cavity.
Table 4.
The closest distance between the anterior zygomatic implant and the orbital cavity at different apex points (mm)
| Apex point site | Entire cohort(n = 56) | Class IV Subgroup(n = 39) | Class V/VI Subgroup(n = 17) |
|---|---|---|---|
| A0 | 4.3 ± 0.9 | 4.4 ± 0.8 | 4.1 ± 1.1 |
| A1 | 3.8 ± 1.0 | 3.8 ± 1.1 | 3.8 ± 0.8 |
| A2 | 3.2 ± 1.0 | 3.2 ± 1.1 | 3.0 ± 0.8 |
| A3 | 2.5 ± 1.0 | 2.6 ± 1.2 | 2.3 ± 0.8 |
Discussion
Choice of apex site for quad zygomatic implants
The anterior ZI of quad zygomatic implant exhibited the highest zygomatic BIC when the A3 apex point at the upper zygoma was selected. The posterior ZI demonstrated the highest zygomatic BIC at the B2 apex point in the middle zygoma and the C1 apex point in the lower zygoma. These findings align with the clinical study by Wu and colleagues [19]。.
The zygomatic BIC of anterior ZI increased progressively as the apex point of ZI moved from A0 to A3, due to the elongating distance the ZI traversed through the zygoma. For the posterior ZI, the zygomatic BIC rose from B0 to B2, then diminished from B2 to B3, and similarly increased from C0 to C1 before decreasing from C1 to C3. This pattern is attributed to the portion of the ZI that is exposed in the infratemporal fossa. The more distal the apex point, the greater the percentage of ZI exposure in the infratemporal fossa. Among all middle and lower zygoma apex points, the highest average zBIC and tBIC can be achieved when ZI ended at the B2 point, The B1, B3, C1, and C2 apex points can also provide relatively high BIC for the ZI.
Infratemporal fossa serves as the passage way of many important neurovascular structure, including the maxillary artery and its branches, the pterygoid venous piexus, mandibular nerve, and more. Given the zygomatic bone’s curvature and the invariably straight path of the ZI, there’s a significant risk of implants entering the infratemporal fossa when selecting distal apex points. Rossi et al. have recommended adjusting the ZI insertion angle to prevent its encroachment into the infratemporal fossa and to protect the vital neurovascular structures [28].
For the anterior quad ZI, the selection of the A3 apex point resulted in only one instance of infratemporal fossa intrusion out of 56 ZIs. Statistical analysis indicated no significant difference in the rate of infratemporal fossa intrusion across all A series apex points, implying that A3 remains a secure and preferred choice.
For the posterior quad ZI, despite the highest zBIC and tBIC at the B2 point, the rate of infratemporal fossa intrusion was 42.9%, with an average intrusion depth of 2.2 ± 1.0 mm, potentially harming the contents in infratemporal fossa. All apex points in the lower zygoma (C series) demonstrated a risk of ZI intrusion into the infratemporal fossa, particularly at C2 and C3. However, at the B1 site, only one of the 56 posterior quad ZIs intruded into the infratemporal fossa, mirroring the anterior ZI at the A3 apex point. Therefore, placing ZI at the B1 site is considered safe for achieving high BIC while avoiding damage to the content in infratemporal fossa.
In summary, maximizing the zygomatic bone volume for optimal BIC, while ensuring patient safety, A3 and B1 emerged as the superior apex points for anterior and posterior quad ZI, respectively. The optimal sites for the apex points of quad ZIs were identified as the upper posterior and the anterior middle portions of the zygoma.
Risk of ZI intrusion into the infratemporal fossa and difference between the two subgroups
In this study the edentulous maxilla residual ridges were classified in to Class IV and Class V/VI according to the Cawood and Howell classification [26]. Simillar to the entire cohort, the highest zygomatic and total BIC for the anterior ZI in both subgroups was achieved at the A3 apex point, with no significant difference in the rate of intrusion into the infratemporal fossa between the Class IV and Class V/VI subgroups at the A3 point.
For the posterior ZI, the highest zBIC and tBIC were achieved when the ZI was placed at the B2 apex point. The second highest zBIC and tBIC point in the Class IV subgroup were observed at the C1, B3, and B1 points. In the Class V/VI subgroup, the B1 point was also a favorable choice for the apex since there was no significant difference in zBIC and tBIC between the B1 and B2 points. Considering the risk of intrusion into the infratemporal fossa, it was found that the rate of posterior ZI penetration into the infratemporal fossa was high in ZIs at B2, B3, and all C series points. Consequently, the B1 and B0 points were safer choices. Taking into account both BIC and infratemporal fossa risk factors, the optimal apex point for the posterior ZI was B1.
One case of anterior ZI intrusion into the infratemporal fossa at the A3 apex point in the Class IV subgroup was noted, along with a posterior ZI intrusion at the B1 apex point in the Class V/VI subgroup. The zygomas in these cases exhibited greater curvature and were thinner than those in other cases, resulting in a shallower infratemporal fossa and an increased likelihood of ZI penetration into infratemporal fossa. No significant differences were found between Class IV and Class V/VI subgroups at any apex point sites, indicating that the risk of ZI intrusion is influenced by zygomatic anatomy rather than the classification of residual ridge resorption. Preoperative analysis of the zygomatic anatomy is crucial, particularly for patients with prominent zygomatic bones. Should ZI intrusion be detected, the anterior ZI apex point could be moved forward to the A2 point, and the posterior ZI apex point could be adjusted toward the B0 point.
For the same apex point, no significant differences were observed in BIC or the rate, length, and depth of ZI intrusion into infratemporal fossa between Class IV and Class V/IV subgroups. These findings suggest that the classification of the edentulous residual ridge has minimal impact on the primary stability and safety of quad ZI, which can be safely applied in patients with severe maxillary residual ridge resorption.
It should be noted that the infratemporal intrusion in this Chinese population may be different from those of the western demographic groups since the facial features of asian population are characterized by a relatively flatter facial profile and more prominent zygomatic bones.
Risk of orbital cavity penetration
Orbital cavity penetration is a severe complication with the incidence of 5.9%[21] in ZI placement. Care must be taken to avoid the bony orbit during ZI placement. In this study, three anterior ZI at A3 apex point showed less than 1 mm distance from the orbital cavity. Even with the computer assisted implant surgery (CAIS), the deviation of ZI placement remains above 2 mm for static and dynamic CAIS [29]. The orbital penetration risk should be taken into account when A3 point was selected as the apex point for anterior ZI. The zygomatic anatomy-guided approach (ZAGA) concept that focus on interindividual anatomic differences can be considered to avoid this complication [17].
Possible risk of interference between the anterior and posterior ZIs
There are potential risk of interference between the anterior and posterior ZIs when this zygoma segementation protocol was used. When B series points were taken as the apex points for the posterior ZI, there are chances that the anterior ZI pass by in a distance of less than 1.6 mm at some point. There is a risk for the two ZIs coming into contact considering the deviations in ZI placement. Causions should be taken when the B series points were taken as the apex point for the posterior ZI.
This study has some limitations. First, the study design and outcome are based solely on CBCT anatomical analysis and virtual implant planning, and the BIC measurement was base on linear instead of area measurement, and these may be different from actual clinical practice. Second, the classification of the edentulous residual ridge was based on ridge height measurements and clinical examination, suggesting that a more precise classification system is needed for future research. Third, the choice of apex points for the anterior ZI was set at the A series point, in actual clinical practice, points B series can also be selected as apical points for anterior ZIs. Risk of orbital injury need to be considered when placing ZIs at A series points, especially A3 apex point. More refined zygomatic bone segmentation is needed to avoid orbital risk. These needs further investigation in future studies.
Conclusions
For the placement of quad zygomatic implants, the optional apex location for the anterior ZI is A3, while for the posterior ZI, it is B1. These apex points ensure favorable BIC and a reduced risk of infratemporal fossa invasion. Anterior ZI positioned at A3 point may present high risk for orbital penetration and may not be reccomended in a Quad ZI approach.
The degree of residual alveolar bone resorption does not affect the BIC of quad zygomatic implants.
Abbreviations
- ZI
Zygomatic Implant
- BIC
Bone-Implant Contact
- CBCT
Cone Beam Computed Tomography
- DICOM
Digital Imaging and Communications in Medicine
- zBIC
zygomatic Bone-Implant Contact
- aBIC
alveolar Bone-Implant Contact
- tBIC
total Bone-Implant Contact
Author contributions
JW: Conceptualization, Methodology, Investigation, Data curation, Formal analysis, Writing – original draft. BC: Conceptualization, Methodology, Formal analysis, Resources, Supervision, Funding acquisition, Writing – review & editing. YZ: Investigation, Data curation. SP: Methodology, Resources, Supervision, Funding acquisition, Writing – review & editing. XX: Conceptualization, Methodology, Formal analysis, Resources, Supervision, Funding acquisition, Writing – review & editing.
Funding
This research was supported by the Beijing Municipal Science & Technology Commission (Grant number: Z201100005520055), and by Peking University School of Stomatology Innovation Experiment Program for University Students (Grant number: 2020-DC-01), and and by Beijing Natural Science Foundation (No. 7222228), and by Clinical Research Foundation of Peking University School and Hospital of Stomatology (Grant number: PKUSS-2023CRF501, PKUSS-2023CRF205).
Data availability
The data used to support the findings of this study will be available from the corresponding author upon request.
Declarations
Consent for publication
Consent for publication of identifiable details, images was obtained from all individual participants.
Competing interests
The authors declare no competing interests.
Ethics approval
This study was conducted in accordance with the principles of the Declaration of Helsinki, as revised in 2013. This study received approval from the Institutional Review Board of the University (Ethical Approval No: PKUSSIRB-202162013). The clinical research is registered under the number ChiCTR2100044472.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Jiayi Wang, Bo Chen, Yuexin Zhao contributed equally to this work.
References
- 1.Pan S, Dagenais M, Thomason JM, et al. Does mandibular edentulous bone height affect prosthetic treatment success? J Dent. 2010;38(11):899–907. 10.1016/j.jdent.2010.08.002. [DOI] [PubMed] [Google Scholar]
- 2.Heydecke G, Boudrias P, Awad MA, et al. Within-subject comparisons of maxillary fixed and removable implant prostheses: patient satisfaction and choice of prosthesis. Clin Oral Implants Res. 2003;14(1):125–30. 10.1034/j.1600-0501.2003.140117.x. [DOI] [PubMed] [Google Scholar]
- 3.Esposito M, Worthington HV. Interventions for replacing missing teeth: dental implants in zygomatic bone for the rehabilitation of the severely deficient edentulous maxilla. Cochrane Database Syst Rev. 2013;9CD004151. 10.1002/14651858.CD004151.pub3. [DOI] [PMC free article] [PubMed]
- 4.Goiato MC, Pellizzer EP, Moreno A, et al. Implants in the zygomatic bone for maxillary prosthetic rehabilitation: a systematic review. Int J Oral Maxillofac Surg. 2014;43(6):748–57. 10.1016/j.ijom.2014.01.004. [DOI] [PubMed] [Google Scholar]
- 5.Malo P, Nobre Mde A, Lopes A, et al. Five-year outcome of a retrospective cohort study on the rehabilitation of completely edentulous atrophic maxillae with immediately loaded zygomatic implants placed extra-maxillary. Eur J Oral Implantol. 2014;7(3):267–81. [PubMed] [Google Scholar]
- 6.Wang F, Monje A, Lin GH, et al. Reliability of four zygomatic implant-supported prostheses for the rehabilitation of the atrophic maxilla: a systematic review. Int J Oral Maxillofac Implants. 2015;30(2):293–8. 10.11607/jomi.3691. [DOI] [PubMed] [Google Scholar]
- 7.Kammerer PW, Fan S, Aparicio C, et al. Evaluation of surgical techniques in survival rate and complications of zygomatic implants for the rehabilitation of the atrophic edentulous maxilla: a systematic review. Int J Implant Dent. 2023;9(1):11. 10.1186/s40729-023-00478-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Branemark P. Surgery and fixture installation: zygomaticus fixture clinical procedures., First edition. edn. Goteborg, Sweden: Nobel Biocare AB, 1998.
- 9.Branemark PI, Grondahl K, Ohrnell LO, et al. Zygoma fixture in the management of advanced atrophy of the maxilla: technique and long-term results. Scand J Plast Reconstr Surg Hand Surg. 2004;38(2):70–85. 10.1080/02844310310023918. [DOI] [PubMed] [Google Scholar]
- 10.Chrcanovic BR, Pedrosa AR, Neto Custodio AL. Zygomatic implants: a critical review of the surgical techniques. Oral Maxillofac Surg. 2013;17(1):1–9. 10.1007/s10006-012-0316-y. [DOI] [PubMed] [Google Scholar]
- 11.Malo P, Nobre Mde A, Lopes I. A new approach to rehabilitate the severely atrophic maxilla using extramaxillary anchored implants in immediate function: a pilot study. J Prosthet Dent. 2008;100(5):354–66. 10.1016/S0022-3913(08)60237-1. [DOI] [PubMed] [Google Scholar]
- 12.Stella JP, Warner MR. Sinus slot technique for simplification and improved orientation of zygomaticus dental implants: a technical note. Int J Oral Maxillofac Implants. 2000;15(6):889–93. [PubMed] [Google Scholar]
- 13.Xu X, Zhao S, Liu H et al. An Anatomical Study of Maxillary-Zygomatic Complex Using Three-Dimensional Computerized Tomography-Based Zygomatic Implantation. Biomed Res Int, 2017, 2017: 8027307. 10.1155/2017/8027307 [DOI] [PMC free article] [PubMed]
- 14.Bedrossian E, Rangert B, Stumpel L, et al. Immediate function with the zygomatic implant: a graftless solution for the patient with mild to advanced atrophy of the maxilla. Int J Oral Maxillofac Implants. 2006;21(6):937–42. [PubMed] [Google Scholar]
- 15.Chow J, Hui E, Lee PK, et al. Zygomatic implants–protocol for immediate occlusal loading: a preliminary report. J Oral Maxillofac Surg. 2006;64(5):804–11. 10.1016/j.joms.2006.01.021. [DOI] [PubMed] [Google Scholar]
- 16.Al-Nawas B, Wegener J, Bender C, et al. Critical soft tissue parameters of the zygomatic implant. J Clin Periodontol. 2004;31(7):497–500. 10.1111/j.1600-051X.2004.00505.x. [DOI] [PubMed] [Google Scholar]
- 17.Aparicio C, Polido WD, Zarrinkelk HM. The Zygoma anatomy-guided Approach for Placement of Zygomatic implants. Atlas Oral Maxillofac Surg Clin North Am. 2021;29(2):203–31. 10.1016/j.cxom.2021.05.004. [DOI] [PubMed] [Google Scholar]
- 18.Aparicio C, Ouazzani W, Aparicio A, et al. Extrasinus zygomatic implants: three year experience from a new surgical approach for patients with pronounced buccal concavities in the edentulous maxilla. Clin Implant Dent Relat Res. 2010;12(1):55–61. 10.1111/j.1708-8208.2008.00130.x. [DOI] [PubMed] [Google Scholar]
- 19.Hung KF, Ai QY, Fan SC, et al. Measurement of the zygomatic region for the optimal placement of quad zygomatic implants. Clin Implant Dent Relat Res. 2017;19(5):841–8. 10.1111/cid.12524. [DOI] [PubMed] [Google Scholar]
- 20.Davo R, David L. Quad Zygoma: technique and realities. Oral Maxillofac Surg Clin North Am. 2019;31(2):285–97. 10.1016/j.coms.2018.12.006. [DOI] [PubMed] [Google Scholar]
- 21.Tavelli C, Tedesco A. Survival and complication rate of zygomatic implants: a systematic review. J Oral Implantol. 2022. 10.1563/aaid-joi-D-22-00008. [DOI] [PubMed] [Google Scholar]
- 22.Krauthammer M, Shuster A, Mezad-Koursh D, et al. Extraocular muscle damage from dental implant penetration to the orbit. Am J Ophthalmol Case Rep. 2017;5:94–6. 10.1016/j.ajoc.2016.11.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Tran AQ, Reyes-Capo DP, Patel NA, et al. Zygomatic dental implant induced orbital fracture and inferior oblique trauma. Orbit. 2019;38(3):236–9. 10.1080/01676830.2018.1444063. [DOI] [PubMed] [Google Scholar]
- 24.Takamaru N, Nagai H, Ohe G, et al. Measurement of the zygomatic bone and pilot hole technique for safer insertion of zygomaticus implants. Int J Oral Maxillofac Surg. 2016;45(1):104–9. 10.1016/j.ijom.2015.07.015. [DOI] [PubMed] [Google Scholar]
- 25.Mavriqi L, Lorusso F, Conte R, et al. Zygomatic implant penetration to the central portion of orbit: a case report. BMC Ophthalmol. 2021;21(1):121. 10.1186/s12886-021-01846-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Cawood JI, Howell RA. A classification of the edentulous jaws. Int J Oral Maxillofac Surg. 1988;17(4):232–6. 10.1016/s0901-5027(88)80047-x. [DOI] [PubMed] [Google Scholar]
- 27.Bertos Quilez J, Guijarro-Martinez R, Aboul-Hosn Centenero S, et al. Virtual quad zygoma implant placement using cone beam computed tomography: sufficiency of malar bone volume, intraosseous implant length, and relationship to the sinus according to the degree of alveolar bone atrophy. Int J Oral Maxillofac Surg 2018;47(2):252–61. 10.1016/j.ijom.2017.07.004. [DOI] [PubMed] [Google Scholar]
- 28.Rossi M, Duarte LR, Mendonca R, et al. Anatomical bases for the insertion of zygomatic implants. Clin Implant Dent Relat Res. 2008;10(4):271–5. 10.1111/j.1708-8208.2008.00091.x. [DOI] [PubMed] [Google Scholar]
- 29.Wang W, Yu X, Wang F, et al. Clinical efficacy of computer-assisted zygomatic implant surgery: a systematic scoping review. J Prosthet Dent. 2023. 10.1016/j.prosdent.2023.10.032. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data used to support the findings of this study will be available from the corresponding author upon request.