Abstract
Public health policy interventions are associated with many important public health achievements. To provide public health practitioners and decision makers with practical approaches for examining and employing evidence-based public health (EBPH) policy interventions, we describe the characteristics and benefits that distinguish EBPH policy interventions from programmatic interventions. These characteristics include focusing on health at a population level, focusing on upstream drivers of health, and involving less individual action than programmatic interventions. The benefits of EBPH policy interventions include more sustained effects on health than many programs and an enhanced ability to address health inequities. Early childhood education and universal preschool provide a case example that illustrates the distinction between EBPH policy and programmatic interventions. This review serves as the foundation for 3 concepts that support the effective use of public health policy interventions: applying core component thinking to understand the population health effects of EBPH policy interventions; understanding the influence of existing policies, policy supports, and the context in which a particular policy is implemented on the effectiveness of that policy; and employing a systems thinking approach to identify leverage points where policy implementation can have a meaningful effect.
Keywords: public health policy interventions, evidence-based public health policy, public health impact, population health, social determinants of health
Public health scholars observe that public health policies account for many of the most important public health successes of the past several decades.1-3 While these dramatic improvements in population health involved changes in behavior, they would not have been possible without collective action and investment at the community, state, and national levels—changes brought about by public health policies. Examples of public health policies and their positive effect on population health abound. 4 Mortality associated with vehicle miles traveled has decreased by more than 90% since 1925, with declines rapidly following the adoption of laws and policies setting standards for motor vehicle, highway, and traffic safety in the 1960s and 1970s. 5 More recently, an estimated 53 000 deaths were avoided due to tobacco control policies implemented between 1970 and 2005.6,7 It is perhaps not surprising, then, that the revised 10 Essential Public Health Services, a framework for public health activities updated as part of the Futures Initiative, features the development, adoption, implementation, and use of policies, laws, and legal and regulatory actions to protect and improve public health. 8
Despite the central role of policy in public health, much of the discussion about health-related policies focuses on “downstream” individual behavior change or health care. 9 Moreover, the center of attention in evaluation remains focused on programmatic interventions, not broad-scale policy interventions. As such, we turn the spotlight on evidence-based public health (EBPH) policy interventions, which are distinct from public health programmatic interventions, other types of health interventions, and other types of public policy. An EBPH approach to policy fosters community engagement in decision-making as well as reliance on the best available evidence of various types.10,11 This practice can confer many benefits, “including access to more and higher-quality information on what works, a higher likelihood of successful programs and policies being implemented, greater workforce productivity, and more efficient use of public and private resources.” 10 In this review, we describe the distinct features of EBPH policies and how they compare with public health programmatic interventions. The review also provides a foundation for future work that offers public health practitioners and decision makers, as well as researchers, practical approaches for examining and employing EBPH policies as effective public health interventions.
What Distinguishes EBPH Policy Interventions From Other Health Interventions?
In general terms, an intervention is an attempt to alter the behavior of an individual, an organization, a system, or a course of events in a way that improves performance or outcomes in some way.12,13 While “public health” has abundant and varied definitions, the National Academy of Medicine succinctly defines public health as “what society does collectively to assure the conditions for people to be healthy.” 14 EBPH is an approach to decision-making, defined “as the process of integrating science-based interventions with community preferences to improve the health of populations.” 15 As such, we consider policy interventions that aim to improve health or well-being at the population level, incorporate community engagement, and are guided by the best available evidence to be EBPH policy interventions.10,16,17
It is important to ensure that public health policies are based, wherever possible, on evidence that has been developed with scientific rigor (eg, collected in a systematic and methodological way).10,14 To that end, the evidence base for EBPH policies encompasses various types of evidence, such as evidence of the public health issue (eg, extent, causation) and effect of the policy intervention, as well as evidence related to the translation, implementation, and adoption (eg, context) of the public health policy intervention.10,11,17-19 Implementing policies without the benefit of evidence—evaluative, theoretical, or practice based—can lead to detrimental unintended consequences, unrealistic policy goals, or implementation challenges—or no effect. 20 The evidence base for a policy is intended to complement, not replace, the broader range of considerations (eg, legislative priorities, input from community members and other interested parties, implementation feasibility) that are usually taken into account when designing policy. For example, in developing EBPH policy, the Centers for Disease Control and Prevention (CDC) explicitly identifies partner engagement (both listening and education) along all steps of the policy process, from problem identification, policy analysis, and strategy/policy development to policy enactment and policy implementation. 21
Programs lacking evidentiary bases can have similar shortcomings. What, then, distinguishes EBPH policy interventions from EBPH programmatic interventions in practice? We present 3 distinguishing characteristics and 2 benefits associated with employing public health policy interventions to address public health challenges.
This activity was reviewed by CDC and was conducted consistent with applicable federal law and CDC policy (see eg, 45 CFR part 46; 21 CFR part 56; 42 USC §241[d]; 5 USC §552a; 44 USC §3501 et seq). Human participant protection was not required because this work did not involve human participants.
Discussion
Key Characteristics of EBPH Policy Interventions
Focus on health at a population level
Perhaps most notably, EBPH policy interventions are more likely to focus on the health of a population than on the health of an individual. The scope or size of “population” varies by context. For a national public health agency, “population” may connote the entire (or at least large sections of) the population of the nation. For a county health department, by contrast, “population” may connote a large share of individuals in the county.
However, the term “population” can include the presence of multiple groups, each with discernible characteristics. 22 Many authors, furthermore, emphasize that public health policy interventions often seek to affect not only geographic or “at-risk populations” but also to “shift the curve” among broader “populations of interest.” 23 At-risk populations include those with identified risk factors for a particular condition or health outcome, such as diagnosed hypertension, depression, or substance use disorder. Populations of interest, by contrast, are populations that are “essentially healthy, but whose health status could be enhanced or protected.” 22 Policy interventions may affect parts of a population in different ways. For example, public health policy interventions can be used to change community design to create physical activity–friendly routes, thereby encouraging large numbers of individuals to be more active. Moreover, the ways in which individuals interact with one another can amplify the effects of such policy interventions; this interaction can be seen in physical activity interventions, which often account for peer effects that encourage intervention uptake. 24 Therefore, policy interventions can have secondary effects that arise from friends, neighbors, peers, and social networks encouraging one another to change their behavior. 25 A growing body of evidence suggests the influence of shared cultures and mindsets on health. 26 Similarly, Auerbach notes that policy interventions can affect future populations, underscoring the multigenerational potential of such total population or community-wide policy interventions. 27
Focus on upstream drivers
EBPH policy interventions are more likely than programmatic interventions to focus on “upstream” factors such as social determinants of health (SDOH). CDC defines SDOH as “conditions in the places where people live, learn, work, and play that affect a wide range of health risks and outcomes.” 28 These factors are characterized as “upstream” because they are the root causes of the community’s subsequent or “downstream” health outcomes.29,30
Interventions used to address health conditions or risk factors can occur at multiple levels. For example, Brownson et al 9 distinguished between “midstream” interventions (ie, intraorganizational initiatives such as worksite-based wellness programs) and “downstream” interventions (ie, “individual-level behavioral approaches for prevention or disease management”) from “upstream” interventions (eg, population-level approaches to improve water quality and access in schools). Similarly, Castrucci and Auerbach 30 described upstream interventions as those that seek to improve community conditions, midstream interventions as those that address an individual’s social needs (eg, food insecurity, housing needs, transportation to medical appointments), and downstream interventions as those that seek to deliver clinical care to individuals. Upstream interventions include “policy approaches that can affect large populations through regulation, increased access, or economic incentives,” such as tobacco taxes.9,30
EBPH policy interventions have greater capacity than programmatic interventions to address upstream factors. 30 This greater capacity does not negate, however, the need for or the effect of individual-level interventions 27 or the extent to which public health policy interventions can encompass individual-level interventions delivered at scale (eg, maternal and infant home visiting programs at scale) 31 through community-level (or population-level) action. When policies are enacted that make programmatic-level interventions accessible across a geographic area or available to everyone in a population of focus (along with other enabling factors such as sustained funding), a program that previously benefited only a few now benefits many at the population level because of the policy action and in essence becomes an EBPH policy. Indeed, Brownson et al 9 observed that “a difference between individual-level health care and population-level approaches for improving health is that public health interventions often occur at multiple levels.” For example, Keller et al 22 pointed to the example of an approach to prenatal domestic abuse that includes broad, population-level screening for abuse during all prenatal assessments (upstream, population level), a media campaign with tailored outreach in specific communities (mid-stream, community level), and follow-up home visits after domestic disputes that involved calls to police (downstream, individual level). Similarly, Auerbach 27 maintained that public health policies are potentially most effective when implemented in coordination with downstream program interventions in clinical and community settings.
Involve less individual action and more action by governments and civil society
The capacity of EBPH policy interventions to address upstream, population-level factors also has implications for which entity acts to achieve the intervention’s intended goal; policies that address SDOH and other upstream drivers involve less individual action and more action by governments and civil society. This sentiment is reflected in various public health strategies. The vision for Public Health 3.0, offered by DeSalvo et al, 32 prioritizes “environmental, policy, and systems-level actions that directly affect the social determinants of health.” Perhaps the clearest articulation of this principle is represented by the Health Impact Pyramid. 33 In it, 5 intervention types are arranged in tiers, from those with the greatest potential population effect (and requiring the least individual effort) at the base of the pyramid to those with the least potential population effect (and requiring the most individual effort) at the peak of the pyramid (Figure 1). 33 The bottom tier includes interventions to modify SDOH, such as income level and education. The interventions that fit into the tier second from the bottom involve changing the context so that health promotion becomes the “default” (eg, water fluoridation, reduction of sodium in packaged food, elimination of lead paint and asbestos exposures).33-35 The tier third from the bottom includes long-lasting individual-level protective clinical interventions that, once delivered, involve little or no ongoing individual effort (eg, male circumcision). The interventions in the top 2 tiers involve, respectively, ongoing access to individual clinical care (eg, prescription of medications for hypertension) and counseling and education to advance behavior change by individuals (eg, smoking cessation counseling). 33
Figure 1.
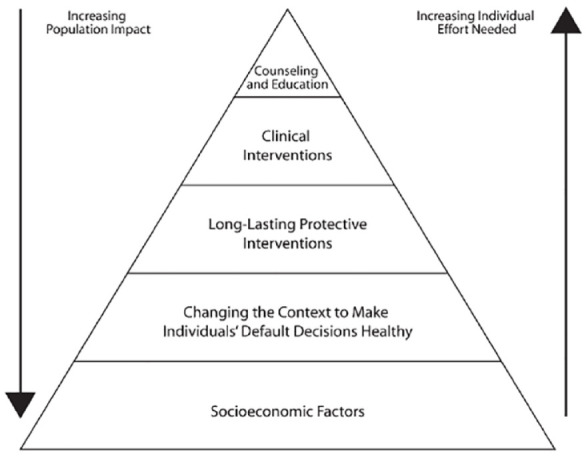
The Health Impact Pyramid. Reproduced from Frieden, 33 with permission.
The pyramid also demonstrates how complementary interventions at different levels can create synergies to address a common health issue from different angles; a comprehensive approach is often the most effective. 33 For example, it can be difficult for individuals to have good nutrition in environments that are considered food deserts (ie, neighborhoods with limited food purchase options). Tier 5 public health policies, such as large-scale supplemental income and nutrition support programs, including the Special Supplemental Nutrition Program for Women, Infants and Children (WIC),36,37 the Supplemental Nutrition Assistance Program (SNAP), 38 Community Provision Eligibility,39,40 and the National School Lunch Program and School Breakfast Program,41,42 have been shown to provide low-income families with increased food security and economic stability as well as support long-term health and cognitive, behavioral, and physical development among participants. These programs provide for increased nutritious food options, reduce food insecurity, and reduce the economic burden of food purchases on families, thereby addressing key SDOH related to economic stability and food security.43-45
Furthermore, improved access to healthy food has been shown to reduce the risk of several chronic diseases. 45 Strategies at other levels of the pyramid, such as filling school vending machines with healthy snacks (tier 4: changing the context to make the healthy choice the easy choice), screening for obesity (tier 2: clinical interventions), and recommending nutritional counseling (tier 1: counseling and education), can supplement public health policies and augment their effect. 46 EBPH policy interventions that affect populations often involve cross-sector partnerships that leverage the collective efforts and unique capabilities of government, philanthropic, and community-based organizations. 47
History provides many illustrations of the broader effect of interventions at or close to the base of the pyramid compared with interventions at the top of the pyramid. For example, major progress in motor vehicle safety has been achieved by an assortment of regulatory policies and requirements, including the high visibility enforcement of seat belt, child restraint, and motorcycle helmet laws and improved standards for motor vehicle safety. Several studies found that states with strong seat belt laws (eg, laws that allow violators to be stopped and cited independently of other traffic behavior) have increased seat belt use and reduced occupant fatalities.48,49 These gains are particularly important given the limited degree of seat belt use and public skepticism about seat belt laws during the 1970s and 1980s. 50 As Schmid et al summarized, “It is unreasonable to expect large proportions of the population to make individual behavior changes that are discouraged by the environment and existing social norms.” 1
Benefits of Using EBPH Policy Interventions
The characteristics of EBPH policies described previously bring with them 2 advantages over individual programmatic interventions.
More sustained effects
By virtue of tackling upstream drivers, EBPH policy interventions in various domains often produce more sustained effects than interventions that rely heavily on individual actions.51,52 For example, downstream nutrition education programs tailored toward low-income individuals seek to change dietary habits, but they often do so without addressing any of the upstream factors that can foster healthy eating (eg, providing healthy food options locally). By contrast, cash transfer programs such as SNAP can address upstream factors by lifting food-insecure households into more stable economic circumstances.38,43,53 An improved economic situation, in turn, facilitates opportunities for healthier food purchasing and food preparation in the home, freeing income for health, utility, and transportation expenditures, which may also improve health and broader social and economic benefits during the life course.38,43,53,54
Better able to address health equity concerns
Finally, the broad reach of EBPH policy interventions is important in promoting health equity—“the state in which everyone has a fair and just opportunity to attain their highest level of health.” 55 The more expansive reach of policy interventions, compared with many programmatic interventions, is particularly advantageous when the goal of a public health approach is to deliver additional resources to people at greatest need 56 or where individual decisions are broadly guided by an applicable change in the community context (eg, development and community investment decisions influence access to healthy food retail and food shopping behaviors). 57 Critically, poorly designed or inequitable policy interventions that fail to authentically engage communities, account for distinct contexts, or anticipate unintended consequences can undermine equity by facilitating inequitable treatment and benefits across entire populations.57,58
Case Example: Early Childhood Education and Universal Preschool
Early childhood education interventions yield a wide array of cognitive, emotional, and academic benefits and improvements in education-associated health outcomes for the child as well as increased maternal employment and family income and savings.59,60 Consider 2 strategies to leverage this effect. An individual programmatic intervention might consist of a learning curriculum implemented by appropriately trained staff within an organization located in a community that serves families experiencing poverty. Such an approach may yield developmental benefits for children enrolled in the program that uses the learning curriculum. It may also identify promising practices that could guide future efforts. But the program’s direct benefits are limited to children taught from the learning curriculum, and the program itself may be limited in scope or time-bound even within that particular organization.
How might a related public health policy intervention differ in its effect when state-level policy actions are taken? Oklahoma’s universal high-quality preschool policy provides a useful illustration. 61 First and most obvious, the policy action of making an individual high-quality preschool program universally available has broad population reach; it is available for all 4-year-old children, regardless of family income, and reaches more than 70% of 4-year-old children living in the state. Second, the policy affects upstream drivers of health by improving community conditions at scale (ie, available to all children aged 4 y). 59 Third, the policy intervention involves little individual action in that parents do not need to search or pay for a preschool with the program. 61 As a result, the policy is well-positioned to sustain effects given that it is widely implemented across the state and funded through a combination of state and federal appropriations. 61 In 2019, Oklahoma ranked third among all states for serving 4-year-old children and met 9 of 10 of the National Institute for Early Education Research’s quality standards benchmarks. 61 In addition, the preschool curriculum is aligned with the state’s broader kindergarten–12th-grade curriculum, thereby fostering educational continuity. Finally, without any income requirements, the policy facilitates equitable access to early childhood education, particularly for low-income families unable to access private options. 62
Public Health Implications and the Direction of Future Work
This topical review described how EBPH policy interventions meaningfully differ from EBPH programmatic interventions. The former generally focus on health at a population level, address upstream drivers of health outcomes, and involve less individual action. These distinctions, in turn, enable EBPH policies to achieve sustained effects across time and settings and reduce inequities. Such characteristics help explain the role of public health policy interventions in facilitating many important public health achievements.
Given the potential effect of public health policies, we will be exploring other aspects of and approaches to using EBPH policy interventions and will describe these interventions in future work that will extend and translate existing concepts and frameworks for use in public health policy. This work will cover 3 concepts (Figure 2).
Figure 2.
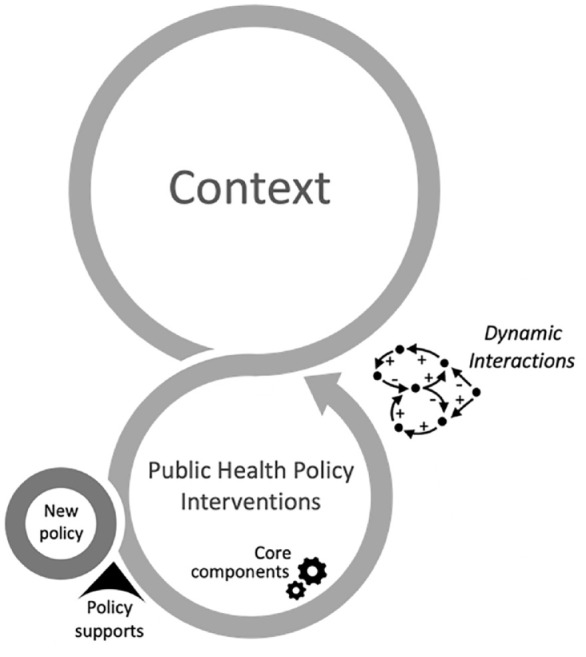
Key concepts and operation of evidence-based public health policy interventions.
EBPH Policies Affect Populations Through Their Core Components
We will draw on the growing literature on core components to describe how public health policy interventions affect populations, often through action at multiple levels. We will also discuss implications of this approach for developing and evaluating evidence related to EBPH policy interventions. 63
The Effectiveness of a Particular Policy Is Influenced by Existing Policies, Policy Supports, and the Broader Context in Which It Is Implemented
The authors will introduce the concept of “policy milieu” to describe the dynamic interaction of factors—context, existing policies, and policy supports—that together help shape a policy’s implementation and effectiveness. We will posit how policy makers can use policy supports to tailor policies to specific milieus while retaining the essential core components of a particular policy.
Complex Systems, Dynamic Interactions, and Leverage Points Facilitate a Policy’s Effect
We will explore the utility of systems thinking to identify “leverage points” within systems in which adoption and implementation of policy interventions can have a meaningful effect. This discussion will be rooted in an increasing recognition that problems arise from interactions among interested parties and in complex systems, and, therefore, considering system dynamics when deciding where in those systems to intervene (ie, “leverage points”) creates interventions that have a meaningful effect on public health outcomes.
Application of these concepts, both individually and collectively, can serve as tools to enhance public health practitioners’ and decision makers’ policy fluency and capacity to use EBPH policy interventions.
Acknowledgments
The authors thank Sangita M. Baxi, MAS, Pardee RAND Graduate School, RAND Corporation, for her contribution to the research related to this article.
Footnotes
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The authors disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This study was supported by a contract (Concepts in Public Health Policy Analysis; contract numbers GS10F0275P and 75D30121P10093) between RAND Corporation and the Centers for Disease Control and Prevention (CDC) of the US Department of Health and Human Services (HHS).
Disclaimer: The findings and conclusions in this article are those of the authors and do not represent the official position or policy of, or implied endorsement by, CDC, HHS, or the US government.
ORCID iDs: Megan A. Kelly, JD, MPH  https://orcid.org/0000-0001-9498-3789
https://orcid.org/0000-0001-9498-3789
Richard W. Puddy, PhD, MPH  https://orcid.org/0000-0002-9770-2134
https://orcid.org/0000-0002-9770-2134
Sameer M. Siddiqi, PhD  https://orcid.org/0000-0001-8094-5677
https://orcid.org/0000-0001-8094-5677
References
- 1. Schmid TL, Pratt M, Howze E. Policy as intervention: environmental and policy approaches to the prevention of cardiovascular disease. Am J Public Health. 1995;85(9):1207-1211. doi: 10.2105/ajph.85.9.1207 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Deaton A. The Great Escape: Health, Wealth, and the Origins of Inequality. Princeton University Press; 2013. doi: 10.2307/j.ctt3fgxbm [DOI] [Google Scholar]
- 3. Pollack Porter KM, Rutkow L, McGinty EE. The importance of policy change for addressing public health problems. Public Health Rep. 2018;133(1 suppl):9S-14S. doi: 10.1177/0033354918788880 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Moulton AD, Mercer SL, Popovic T, et al. The scientific basis for law as a public health tool. Am J Public Health. 2009;99(1):17-24. doi: 10.2105/AJPH.2007.130278 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Centers for Disease Control and Prevention. Motor-vehicle safety: a 20th century public health achievement. MMWR Morb Mortal Wkly Rep. 1999;48(18):369-374. [PubMed] [Google Scholar]
- 6. Bowser D, Canning D, Okunogbe A. The impact of tobacco taxes on mortality in the USA, 1970-2005. Tob Control. 2016;25(1):52-59. doi: 10.1136/tobaccocontrol-2014-051666 [DOI] [PubMed] [Google Scholar]
- 7. Centers for Disease Control and Prevention. Ten great public health achievements—worldwide, 2001-2010. MMWR Morb Mortal Wkly Rep. 2011;60(24):814-818. [PubMed] [Google Scholar]
- 8. Public Health Accreditation Board. The 10 Essential Public Health Services. National Center for Innovations; September 2020. Accessed November 18, 2022. https://phaboard.org/center-for-innovation/public-health-frameworks/the-10-essential-public-health-services [Google Scholar]
- 9. Brownson RC, Seiler R, Eyler AA. Measuring the impact of public health policy. Prev Chronic Dis. 2010;7(4):A77. [PMC free article] [PubMed] [Google Scholar]
- 10. Brownson RC, Fielding JE, Maylahn CM. Evidence-based public health: a fundamental concept for public health practice. Annu Rev Public Health. 2009;30:175-201. doi: 10.1146/annurev.publhealth.031308.100134 [DOI] [PubMed] [Google Scholar]
- 11. Jacobs JA, Jones E, Gabella BA, Spring B, Brownson RC. Tools for implementing an evidence-based approach in public health practice. Prev Chronic Dis. 2012;9:110324. doi: 10.5888/pcd9.110324 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Kindig DA. Understanding population health terminology. Milbank Q. 2007;85(1):139-161. doi: 10.1111/j.1468-0009.2007.00479.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Barbero C, Gilchrist S, Schooley MW, Chriqui JF, Luke DA, Eyler AA. Appraising the evidence for public health policy components using the quality and impact of component evidence assessment. Glob Heart. 2015;10(1):3-11. doi: 10.1016/j.gheart.2014.12.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Institute of Medicine Committee for the Study of the Future of Public Health. The Future of Public Health. National Academies Press; 1988. [Google Scholar]
- 15. Kohatsu N, Robinson J, Torner J. Evidence-based public health: an evolving concept. Am J Prev Med. 2004;27(5):417-421. doi: 10.1016/j.amepre.2004.07.019 [DOI] [PubMed] [Google Scholar]
- 16. Briss PA, Zaza S, Pappaioanou M, et al. Developing an evidence-based Guide to Community Preventive Services—methods. The Task Force on Community Preventive Services. Am J Prev Med. 2000;18(1 suppl):S35-S43. doi: 10.1016/S0749-3797(99)00119-1 [DOI] [PubMed] [Google Scholar]
- 17. Spencer LM, Schooley MW, Anderson LA, et al. Seeking best practices: a conceptual framework for planning and improving evidence-based practices. Prev Chronic Dis. 2013;10:E207. doi: 10.5888/pcd10.130186 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Puddy RW, Wilkins N. Understanding Evidence Part 1: Best Available Research Evidence. A Guide to the Continuum of Evidence of Effectiveness. National Center for Injury Prevention and Control, Centers for Disease Control and Prevention, US Department of Health and Human Services; 2011. Accessed March 21, 2024. https://www.cdc.gov/violenceprevention/pdf/understanding_evidence-a.pdf [Google Scholar]
- 19. Khoury MJ, Gwinn M, Yoon PW, Dowling N, Moore CA, Bradley L. The continuum of translation research in genomic medicine: how can we accelerate the appropriate integration of human genome discoveries into health care and disease prevention? Genet Med. 2007;9(10):665-674. doi: 10.1097/GIM.0b013e31815699d0 [DOI] [PubMed] [Google Scholar]
- 20. Oliver K, Lorenc T, Tinkler J, Bonnell C. Understanding the unintended consequences of public health policies: the views of policymakers and evaluators. BMC Public Health. 2019;19(1):1057-1066. doi: 10.1186/s12889-019-7389-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Centers for Disease Control and Prevention, Office of Policy, Performance, and Evaluation. The CDC policy process. Last reviewed January 2, 2019. Accessed December 11, 2023. https://www.cdc.gov/policy/polaris/policyprocess/index.html
- 22. Keller LO, Strohschein S, Lia-Hoagberg B, Schaffer MA. Population-based public health interventions: practice-based and evidence-supported. Part I. Public Health Nurs. 2004;21(5):453-468. doi: 10.1111/j.1525-1446.1998.tb00341.x [DOI] [PubMed] [Google Scholar]
- 23. Rose G. Sick individuals and sick populations. Int J Epidemiol. 2001;30(3):427-434. doi: 10.1093/ije/30.3.427 [DOI] [PubMed] [Google Scholar]
- 24. De La Haye K, Robins G, Mohr P, Wilson C. How physical activity shapes, and is shaped by, adolescent friendships. Soc Sci Med. 2011;73(5):719-728. doi: 10.1016/j.socscimed.2011.06.023 [DOI] [PubMed] [Google Scholar]
- 25. Frank RH. Under the Influence: Putting Peer Pressure to Work. Princeton University Press; 2020. [Google Scholar]
- 26. Chandra A, Miller CE, Acosta JD, Weilant S, Trujillo M, Plough A. Drivers of health as a shared value: mindset, expectations, sense of community, and civic engagement. Health Aff (Millwood). 2016;35(11):1959-1963. doi: 10.1377/hlthaff.2016.0603 [DOI] [PubMed] [Google Scholar]
- 27. Auerbach J. The 3 buckets of prevention. J Public Health Manag Pract. 2016;22(3):215-218. doi: 10.1097/PHH.0000000000000381 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Centers for Disease Control and Prevention. Social determinants of health at CDC. Last reviewed December 8, 2022. Accessed June 5, 2023. https://www.cdc.gov/about/sdoh/index.html
- 29. McKinlay JB. A case for refocusing upstream: the political economy of illness. IAPHS Occasional Classics. November 18, 2019. Accessed March 21, 2024. https://iaphs.org/wp-content/uploads/2019/11/IAPHS-McKinlay-Article.pdf
- 30. Castrucci BC, Auerbach J. Meeting individual social needs falls short of addressing social determinants of health. Health Affairs Forefront. January 16, 2019. Accessed March 21, 2024. doi: 10.1377/forefront.20190115.234942 [DOI] [Google Scholar]
- 31. US Department of Health and Human Services. Home visiting. May 19, 2022. Accessed November 23, 2022. https://www.acf.hhs.gov/occ/home-visiting
- 32. DeSalvo KB, O’Carroll PW, Koo D, Auerbach JM, Monroe JA. Public health 3.0: time for an upgrade. Am J Public Health. 2016;106(4):621-622. doi: 10.2105/AJPH.2016.303063 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Frieden TR. A framework for public health action: the health impact pyramid. Am J Public Health. 2010;100(4):590-595. doi: 10.2105/AJPH.2009.185652 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Marmot M. Social determinants of health inequalities. Lancet. 2005;365(9464):1099-1104. doi: 10.1016/S0140-6736(05)71146-6 [DOI] [PubMed] [Google Scholar]
- 35. Braveman P, Egerter S, Williams DR. The social determinants of health: coming of age. Annu Rev Public Health. 2011;32:381-398. doi: 10.1146/annurev-publhealth-031210-101218 [DOI] [PubMed] [Google Scholar]
- 36. Venkataramani M, Ogunwole SM, Caulfield LE, et al. Maternal, infant, and child health outcomes associated with the Special Supplemental Nutrition Program for Women, Infants, and Children. Ann Intern Med. 2022;175(10):1411-1422. doi: 10.7326/M22-0604 [DOI] [PubMed] [Google Scholar]
- 37. Jackson MI. Early childhood WIC participation, cognitive development and academic achievement. Soc Sci Med. 2015;126:145-153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Bronchetti ET, Christensen G, Hoynes HW. Local food prices, SNAP purchasing power, and child health. J Health Econ. 2019;68:102231. doi: 10.1016/j.jhealeco.2019.102231 [DOI] [PubMed] [Google Scholar]
- 39. Billings KC, Carter JA. Serving free school meals through the Community Eligibility Provision (CEP): background and participation (R46371). Congressional Research Service. May 20, 2020. Accessed December 20, 2023. https://crsreports.congress.gov/product/details?prodcode=R46371 [Google Scholar]
- 40. Hecht AA, Pollack Porter KM, Turner L. Impact of the Community Eligibility Provision of the Healthy, Hunger-Free Kids Act on student nutrition, behavior, and academic outcomes: 2011-2019. Am J Public Health. 2020;110(9):1405-1410. doi: 10.2105/AJPH.2020.305743 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Kenney EL, Barrett JL, Bleich SN, Ward ZJ, Cradock AL, Gortmaker SL. Impact of the Healthy, Hunger-Free Kids Act on obesity trends. Health Aff (Millwood). 2020;39(7):1122-1129. doi: 10.1377/hlthaff.2020.00133 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Community Preventive Services Task Force. Task Force Findings and Rationale Statement—Social Determinants of Health: Healthy School Meals for All. Community Preventive Services Task Force, US Department of Health and Human Services; July 2022. Updated August 31, 2022. Accessed March 21, 2024. https://www.thecommunityguide.org/media/pdf/sdoh-healthy-school-meals-for-all-508.pdf [Google Scholar]
- 43. National Academies of Sciences, Engineering, and Medicine. Vibrant and Healthy Kids: Aligning Science, Practice, and Policy to Advance Health Equity. National Academies Press; 2019. [PubMed] [Google Scholar]
- 44. US Department of Health and Human Services. Healthy people 2030. Food insecurity. 2023. Accessed January 5, 2024. https://health.gov/healthypeople/priority-areas/social-determinants-health/literature-summaries/food-insecurity [Google Scholar]
- 45. US Department of Health and Human Services. Healthy People 2030. Access to foods that support healthy dietary patterns. 2023. Accessed November 23, 2022. https://health.gov/healthypeople/priority-areas/social-determinants-health/literature-summaries/access-foods-support-healthy-dietary-patterns#cit19 [Google Scholar]
- 46. Centers for Disease Control and Prevention. Overweight & obesity. What can be done. 2012. Updated September 15, 2022. Accessed November 23, 2022. https://www.cdc.gov/obesity/php/about/obesity-strategies-what-can-be-done.html
- 47. Koo D, O’Carroll PW, Harris A, DeSalvo KB. An environmental scan of recent initiatives incorporating social determinants in public health. Prev Chronic Dis. 2016;13:E86. doi: 10.5888/pcd13.160248 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Foss R, Martell C, Goodwin A, O’Brien N. Measuring Changes in Teenage Driver Crash Characteristics During the Early Months of Driving. AAA Foundation for Traffic Safety; September 2011. Accessed November 23, 2022. https://aaafoundation.org/measuring-changes-teenage-driver-crash-characteristics-early-months-driving [Google Scholar]
- 49. Beck LF, West B. Vital signs: nonfatal, motor vehicle–occupant injuries (2009) and seat belt use (2008) among adults—United States. MMWR Morb Mortal Wkly Rep. 2011;59(51):1681-1686. [PubMed] [Google Scholar]
- 50. Mashaw JL, Harfst DL. The Struggle for Auto Safety. Harvard University Press; 1990. [Google Scholar]
- 51. Levy DT, Tam J, Kuo C, Fong GT, Chaloupka F. The impact of implementing tobacco control policies: the 2017 tobacco control policy scorecard. J Public Health Manag Pract. 2018;24(5):448-457. doi: 10.1097/PHH.0000000000000780 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Pitt AL, Humphreys K, Brandeau ML. Modeling health benefits and harms of public policy responses to the US opioid epidemic. Am J Public Health. 2018;108(10):1394-1400. doi: 10.2105/AJPH.2018.304590 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Bailey MJ, Hoynes HW, Rossin-Slater M, Walker R. Is the Social Safety Net a Long-term Investment? Large-scale Evidence From the Food Stamps Program. National Bureau of Economic Research working paper 26942. April 2020. Accessed March 21, 2024. doi: 10.3386/w26942. https://www.nber.org/system/files/working_papers/w26942/w26942.pdf [DOI] [PMC free article] [PubMed]
- 54. Lorenc T, Petticrew M, Welch V, Tugwell P. What types of interventions generate inequalities? Evidence from systematic reviews. J Epidemiol Community Health. 2013;67(2):190-193. doi: 10.1136/jech-2012-201257 [DOI] [PubMed] [Google Scholar]
- 55. Centers for Disease Control and Prevention. Health equity. What is health equity? October 11, 2022. Accessed November 17, 2022. https://www.cdc.gov/healthequity/index.html [Google Scholar]
- 56. Hart KD, Kunitz SJ, Sell RR, Mukamel DB. Metropolitan governance, residential segregation, and mortality among African Americans. Am J Public Health. 1998;88(3):434-438. doi: 10.2105/ajph.88.3.434 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Brown AF, Ma GX, Miranda J, et al. Structural interventions to reduce and eliminate health disparities. Am J Public Health. 2019;109(suppl 1):S72-S78. doi: 10.2105/AJPH.2018.304844 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Rothstein R. The Color of Law: A Forgotten History of How Our Government Segregated America. Liveright; 2017. [Google Scholar]
- 59. Centers for Disease Control and Prevention. Early childhood education: interventions addressing the social determinants of health. August 5, 2016. Updated January 11, 2023. Accessed June 5, 2023. https://www.cdc.gov/policy/hi5/earlychildhoodeducation/index.html
- 60. Cascio EU, Schanzenbach DW. The impacts of expanding access to high-quality preschool education. National Bureau of Economic Research working paper 19735. December 2013. Accessed March 21, 2024. https://www.nber.org/papers/w19735
- 61. Friedman-Krauss AH, Barnett WS, Garver KA, Hodges KS, Weisenfeld GG, Gardiner BA. The State of Preschool 2019: State Preschool Yearbook. National Institute for Early Education Research; 2020. [Google Scholar]
- 62. Martin A, Johnson AD, Castle S. Reframing high-quality public preschool as a vehicle for narrowing child health disparities based on family income. Acad Pediatr. 2021;21(3):408-413. doi: 10.1016/j.acap.2020.07.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Puddy RW, Kelly MA, Nelson C, et al. Advancing evidence-based public health policy: how core component thinking can illuminate the multilevel nature of public health policy. Public Health Rep. Published online May 23, 2024. doi: 10.1177/00333549241247708 [DOI] [PMC free article] [PubMed] [Google Scholar]


