Abstract
Objectives
Mechanical thrombectomy for medium vessel occlusion (MeVO) is a challenging field with limited results. In this study, we aimed at evaluating the efficacy and safety of a procedural strategy beginning with occluded vessel diameter measurement and matched aspiration catheter selection.
Materials and Methods
We retrospectively analyzed all sequentially treated patients by mechanical thrombectomy at two comprehensive stroke centers between May 2020 and April 2023, focusing on the occluded vessel diameter. We included patients who underwent thrombectomy for MeVO based on the matching strategy (a procedural approach involving vessel diameter assessment, matching aspiration catheter selection, and firm clot engagement with or without a stent retriever). We evaluated efficacy and safety using the modified Thrombolysis in the Cerebral Infarction Scale (mTICI) and intracranial hemorrhage (ICH) and procedure-related complications.
Results
Seventy patients fulfilled the final inclusion criteria. The median occluded vessel diameter was 1.71 mm. We achieved mTICI 2b/2c/3 in 82.9% and mTICI 2c/3 in 51.4% of the cases and did not observe any symptomatic ICH. We detected asymptomatic subarachnoid hemorrhage (SAH) in 24.3% of the cases, that is, 5.6%, 20.0%, and 45.5% in the vessel diameter groups ≥2.0, 1.5–2.0, and ≤1.5 mm, respectively. The SAH incidence was significantly higher in narrower vessel groups. The occluded vessel diameter and the contact method with clots predicted clinical outcomes.
Conclusions
Matching strategy-based thrombectomy yields acceptable efficiency and safety results. In narrower vessels, it is optimal to engage matched aspiration catheters and clots without the assistance of conventional stent retrievers.
Keywords: Medium vessel occlusion, thrombectomy, vessel diameter, matching strategy, aspiration catheter
Introduction
Recent clinical outcomes and technical advancements of mechanical thrombectomy for large vessel occlusions (LVOs) reach satisfactory levels, medium vessel occlusions (MeVOs) thus become potential new targets, yielding promising treatment results.1–3 However, MeVOs are more amenable to medical treatments such as intravenous thrombolysis. In addition, MeVO thrombectomy is associated with a higher risk of intracranial hemorrhage (ICH) due to thinner vessel walls and higher tortuosity.4,5 Achieving a clinical advantage in the case of MeVO thrombectomy is challenging compared to that for LVOs. Therefore, to maximize the benefits of MeVO thrombectomy, designing a recanalization rate-enhancing treatment strategy would be necessary while ensuring safety measures to prevent hemorrhagic complications.
Stent retriever use might result in unexpectedly high pull-out resistance, potentially leading to small perforating artery stretching or avulsion, thereby possibly contributing to hemorrhagic complications.5–9 To minimize pull-out resistance-related complications, the primary treatment strategy of aspiration catheter use would be preferable. For recanalization rate maximization with aspiration catheters, catheter selection with an outer diameter as closely matching the vessel diameter as possible is key.10,11 Furthermore, for medium-sized vessel treatment, three-dimensional rotational angiography (3D-RA) could contribute to safety by providing vessel diameter and tortuosity on the route to the thrombus. 12
Considering the abovementioned factors, we designed a thrombectomy strategy with a vessel diameter-matching aspiration catheter as the first line of treatment, referred to as the matching strategy. In this study, we aimed at demonstrating the efficacy and safety of the matching strategy for MeVOs as well as improving surgeon proficiency in the technical aspects of this strategy.
Methods
Patient selection
We conducted a retrospective analysis of the clinical and radiological databases of all patients with acute ischemic stroke sequentially treated by mechanical thrombectomy at two comprehensive stroke centers between May 2020 and April 2023. The common indication for mechanical thrombectomy is the presence of a salvageable penumbral area in the eloquent territory of the patient identified by clinical symptoms, diffusion-weighted imaging (DWI), and fluid-attenuated inversion recovery images, along with the occlusion of the vessel supplying the territory. Based on the inclusion criteria, we involved in this study patients: (1) who underwent matching strategy-based mechanical thrombectomy and (2) with a MeVO: intracranial occlusion located in the M2 and M3 segments of the middle cerebral artery, the anterior cerebral artery (ACA), or the posterior cerebral artery (PCA). The exclusion criteria comprised: (1) lesions requiring balloon angioplasty before thrombectomy and (2) lack of imaging for evaluation.
Matching strategy-based procedures
The guidelines for the matching strategy were as follows:
Prepare aspiration catheters of different sizes and keep them ready for use.
Detect treatable occlusions using diagnostic angiography followed by 3D-RA. Refer to both images to assess the tortuosity and vessel diameter of the pathway leading to occlusion.
Select an aspiration catheter with the largest outer diameter that does not exceed the vessel diameter at the occlusion point. If access up to the occlusion point is challenging, select an aspiration catheter with the largest outer diameter that does not exceed the vessel diameter at the accessible point.
Navigate the aspiration catheter to the proximal end of the clots. If the catheter cannot be navigated to the proximal end of the clot alone, a stent retriever can be used as an anchor. If the catheter cannot be safely navigated to the occlusion point and is placed at the proximal accessible point, the use of a stent retriever is also acceptable for retrieving the clots to the tip of the aspiration catheter.
Adjust the interaction angle between the aspiration catheter and clots to be linear and in a way that they firmly engage. Subsequently, start aspiration and remove the clots.
The surgeon has discretion over several choices, including the determination of anesthesia type (general or local), puncture site, guiding catheter, microcatheter, thrombectomy device, and the decision on whether to extract the stent retriever while leaving the aspiration catheter in place or to extract both devices postengagement. To prevent underestimation, the vessel diameter right before the clots should be measured in the late phase of conventional angiography.
Data collection
We collected baseline characteristics including age, sex, National Institutes of Health Stroke Scale (NIHSS) score on admission and prestroke modified Rankin scale (mRS), DWI-Alberta Stroke Program Early Computer Tomography Score (ASPECTS), stroke subtypes, use of intravenous thrombolysis, and the anatomical location of the lesion. Procedural data comprised the occluded vessel diameter, outer diameter of the aspiration catheter tip, number of attempts, use of stent retriever in conjunction, and procedural time. The catheter-to-vessel ratio was defined as the outer diameter of the largest used aspiration catheter tip divided by the occluded vessel diameter. 10
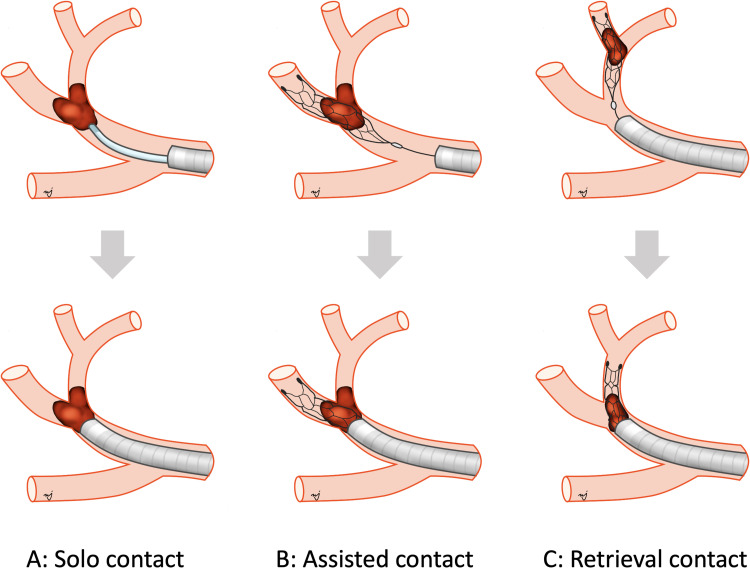
The methods for establishing contact between the aspiration catheter and the clots could be classified into three categories: solo contact (i.e., the aspiration catheter contacted the clots without using a stent retriever), assisted contact (i.e., deployment of a stent retriever on the clots, serving as an anchor to push the aspiration catheter up to contact the proximal end of the clots), and retrieval contact (i.e., a stent retriever was deployed on the clots and used to pull it toward the tip of the aspiration catheter, which was positioned in the proximal portion) (Figure 1). If assisted contact was performed even once and retrieval contact was not performed, the case was classified under the assisted contact group. If retrieval contact was used even once, the case was classified under the retrieval contact group.
Figure 1.
Three contact methods between the aspiration catheter and clot. (a) Solo contact: the clot gets in contact with the aspiration catheter alone, without a stent retriever. (b) Assisted contact: the stent retriever is deployed on the clot as an anchor, assisting the aspiration catheter in reaching the proximal end of the clot. (c) Retrieval contact: the stent retriever is deployed on the clot, pulling it toward the aspiration catheter tip in the proximal position.
We evaluated the efficacy based on the recanalization grade and functional outcome. We assessed the recanalization grade using the modified Thrombolysis in the Cerebral Infarction Scale (mTICI), where good recanalization corresponded to mTICI scale values of 2b, 2c, or 3. We assessed the functional outcome using the mRS 3 months after thrombectomy and defined a favorable outcome as mRS 0–2 or a return to the previous level (if prestroke mRS was >2). We evaluated safety for vessel perforation during device navigation, extravasation following device retrieval, and postprocedural ICH. For the latter, we performed follow-up imaging within 24 ± 8 h. We defined symptomatic ICH as that associated with an increase of ≥4 points on the NIHSS score from baseline assessment. The efficacy and safety outcomes among the occluded vessel diameter groups were compared. Moreover, the tolerability of the adjunctive use of stent retrievers was assessed.
Statistical analysis
To analyze the differences in the procedural data and outcomes between the two groups, we performed χ2 analysis. We categorized occluded vessel diameters into three groups (i.e., ≥2.0 mm, 1.5–2.0 mm, and ≤1.5 mm) for comparative analysis. We compared the incidence rate between the three groups using the Tukey–Kramer Honest Significant Difference test and analyzed the results using commercially available statistical software (JMP 8; SAS Institute, Cary, NC, USA). We considered P-values of p < 0.05 statistically significant.
Results
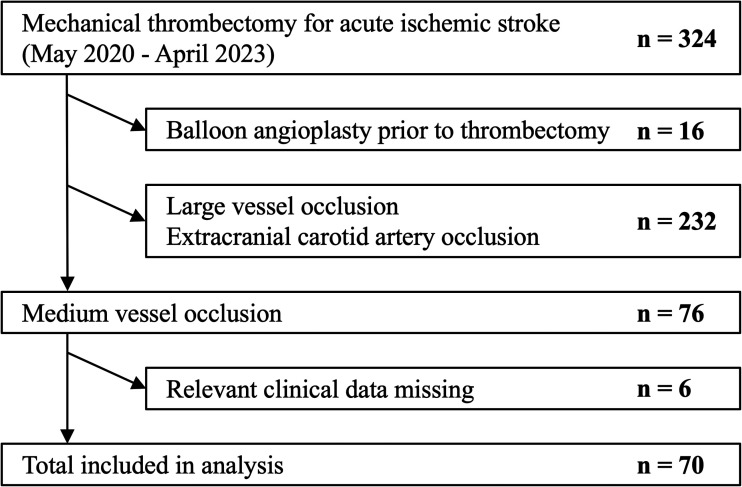
During the study period, 324 patients underwent mechanical thrombectomy for acute ischemic stroke and 70 of them fulfilled the inclusion criteria (Figure 2). Table 1 summarizes the baseline characteristics of the study. The median age, median NIHSS score, and median ASPECTS were 79 years (IQR 74–89), 15 (IQR 9–24), and 8 (IQR 7–10), respectively. Three cases (4.3%) involved multiple vessel occlusions. The initially treated occluded sites for thrombectomy were as follows: 62.9%, 21.4%, 2.9%, 4.3%, and 8.6% in proximal M2, distal M2, and M3 or distal, ACA, and PCA, respectively. The median occluded vessel diameter was 1.71 mm (IQR 1.50–1.98).
Figure 2.
Procedure diagram.
Table 1.
Patient characteristics.
| Number of patients, n | 70 |
| Age, median (IQR) | 79 (74–89) |
| Sex, male/female | 31/39 |
| Pre-NIHSS, median (IQR) | 15 (9–24) |
| Site, right/left | 33/37 |
| Occluded vessel, n (%) | |
| Proximal M2 | 44 (62.9%) |
| Distal M2 | 15 (21.4%) |
| M3 or distal | 2 (2.9%) |
| ACA | 3 (4.3%) |
| PCA | 6 (8.6%) |
| Multiple vessel occlusion, n (%) | 3 (4.3%) |
| Occluded vessel diameter, median (IQR) | 1.71 mm (1.50–1.98) |
| DWI-ASPECTS, median (IQR) | 8 (7–10) |
| Stroke subtype, n (%) | |
| Cardioembolic infarction | 53 (75.8%) |
| Atherothrombotic infarction | 4 (5.7%) |
| Others/unclassified | 13 (18.6%) |
| Use of intravenous tPA, n (%) | 19 (27.1%) |
IQR: interquartile range; NIHSS: National Institutes of Health Stroke Scale; M2: middle cerebral artery M2 portion; M3: middle cerebral artery M3 portion; ACA: anterior cerebral artery; PCA: posterior cerebral artery; ASPECTS: Alberta Stroke Program Early CT Score; tPA: tissue-type plasminogen activator; DWI: diffusion-weighted imaging.
Table 2 summarizes the procedural details as well as the safety and clinical outcomes. The median catheter-to-vessel ratio was 0.95. We used eight aspiration catheter types during the study period, combined with stent retrievers in 72.9% of the cases. We used REACT 71 (Medtronic Neurovascular, Irvine, CA, USA), SOFIA FLOW plus (MicroVention Terumo, Tustin, CA, USA), SOFIA FLOW (MicroVention Terumo, Tustin, CA, USA), 4MAX (Penumbra, Alameda, CA, USA), 3MAX (Penumbra, Alameda, CA, USA), and three other aspiration catheters in cases 11, 35, 5, 13, 3, and 3, respectively. We used Tron Fx (MicroVention Terumo, Tustin, CA, USA), Solitaire (Medtronic Neurovascular, Irvine, CA, USA), and two other retriever types in 34, 15, and 2 cases, respectively. We applied stent retrievers for assisted and retrieval contacts in 30 and 21 cases, respectively. The good recanalization rate was 82.9%, and we achieved mTICI 2c/3 and a favorable outcome in 51.4% and 54.3% of the cases, respectively. From a safety perspective, we observed no instances of vessel perforation during navigation and detected extravasation in two cases after device retrieval. In both cases, extravasation resolved spontaneously, leaving asymptomatic focal subarachnoid hemorrhage (SAH) on the CT. We observed 25 cases of asymptomatic ICH (35.7%), including SAH in 17 cases (24.3%), and no symptomatic ICH. Figures 3 and 4 illustrate representative cases of the matching strategy.
Table 2.
Procedural data as well as efficacy and safety outcomes.
| Occluded vessel diameter | All (n = 70) | ≥2.0 mm (n = 18) | 1.5–2.0 mm (n = 30) | ≤1.5 mm (n = 22) |
|---|---|---|---|---|
| Procedural data | ||||
| Number of attempts | 1.64 ± 0.96 | 1.72 ± 0.99 | 1.87 ± 1.12 | 1.27 ± 0.45 |
| Catheter-to-vessel ratio | 0.95 (0.89–1.04) | 0.84 (0.80–0.99) | 0.93 (0.90–0.99) | 1.04 (0.95–1.27) |
| Stent retriever use | 51 (72.9%) | 10 (55.5%) | 23 (76.7%) | 18 (81.8%) |
| Intravenous tPA use | 19 (27.1%) | 4 (22.2%) | 8 (26.7%) | 7 (31.9%) |
| P-to-R time, min | 49 (38–65) | 49 (40–72) | 42 (38–58) | 53 (45–65) |
| Contact method | ||||
| Solo contact | 19 (27.1%) | 8 (44.4%) | 7 (23.3%) | 4 (18.2%) |
| Assisted contact | 30 (42.9%) | 6 (33.3%) | 18 (60.0%) | 6 (27.3%) |
| Retrieval contact | 21 (30.0%) | 4 (22.2%) | 5 (16.7%) | 12 (54.5%) |
| Efficacy outcomes | ||||
| mTICI 2b/2c/3 | 58 (82.9%) | 15 (83.3%) | 27 (90.0%) | 16 (72.7%) |
| mTICI 2c/3 | 36 (51.4%) | 11 (61.1%) | 16 (53.3%) | 9 (40.9%) |
| First-pass effect | 24 (34.3%) | 6 (33.3%) | 12 (40.0%) | 6 (27.3%) |
| 3-mo favorable outcome | 38 (54.3%) | 14 (77.7%) | 12 (40.0%) | 12 (54.5%) |
| Safety outcomes | ||||
| Perforation during navigation | 0 | 0 | 0 | 0 |
| Extravasation following retrieval | 2 (2.9%) | 0 | 0 | 2 (9.1%) |
| Symptomatic ICH | 0 | 0 | 0 | 0 |
| Asymptomatic ICH | 25 (35.7%) | 2 (11.1%) | 11 (36.6%) | 12 (54.5%) |
| Subarachnoid hemorrhage | 17 (24.3%) | 1 (5.6%) | 6 (20.0%) | 10 (45.5%) |
| Intraparenchymal hemorrhage | 10 (14.3%) | 2 (11.1%) | 6 (20.0%) | 2 (9.1%) |
The catheter-to-vessel ratio was defined as the outer diameter of the largest used aspiration catheter tip divided by the occluded vessel diameter.
tPA: tissue-type plasminogen activator; P-to-R: puncture-to-recanalization; mTICI: modified Treatment in Cerebral Ischemia Scale; ICH: intracranial hemorrhage.
The number of attempts is presented as average (± SD). The catheter-to-vessel ratio and P-to-R time are presented as the median (IQR). Other data are presented as n (%).
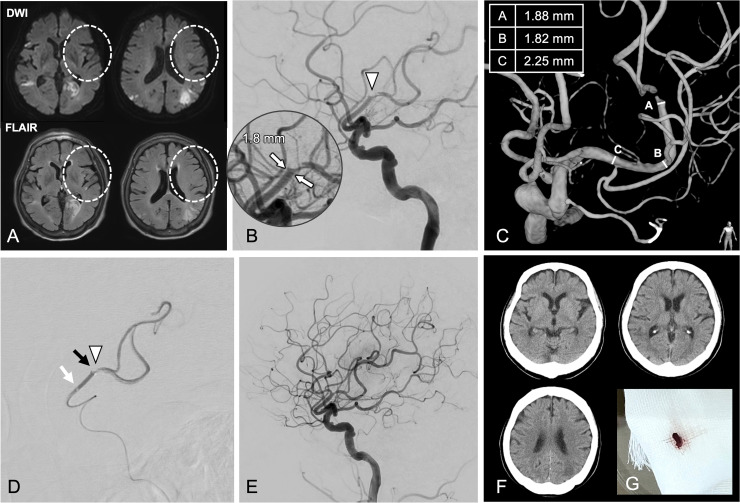
Figure 3.
A 74-year-old man was hospitalized with a minor stroke, displaying new-onset right-sided paralysis, aphasia, and a National Institutes of Health Stroke Scale score of 16. (a) The MRI did not detect any evidence of acute cerebral infarction in the occluded vessel area (circle). (b) The lateral angiogram demonstrated M2 occlusion (arrowhead). (c) The occluded vessel diameter was 1.8 mm (white arrow). The treatable tortuosity and pathway were revealed using 3D rotational angiography. (d) A 1.7-mm outer diameter aspiration catheter established contact with a clot (arrowhead) via the solo contact method. Tip of the aspiration catheter (black arrow) and that of the microcatheter (white arrow), which was pulled proximally. (e) Complete recanalization visualized by angiography. (f) Lack of hemorrhage on CT. (g) Retrieved clot.
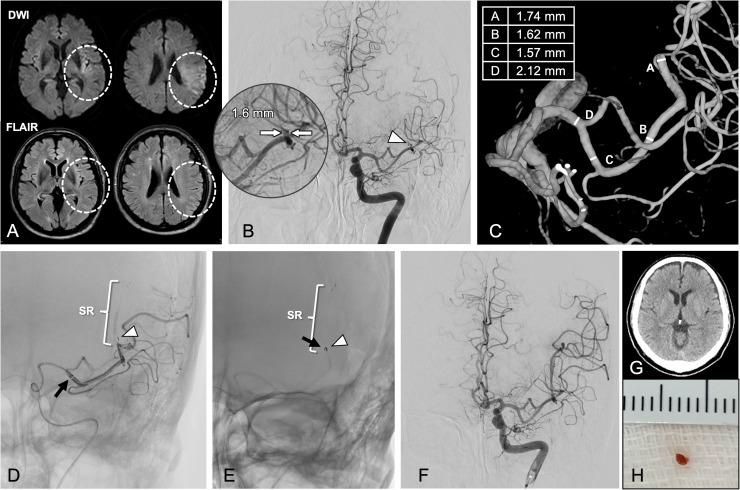
Figure 4.
A 74-year-old man was presented with mild right-sided paralysis, aphasia, and a National Institutes of Health Stroke Scale score of 9. (a) The DWI indicated a faint high signal and the FLAIR detected nothing (circle). (b) Angiography demonstrating distal M2 occlusion (arrowhead). The occluded vessel diameter was 1.6 mm (white arrow). (c) The treatable tortuosity and pathway were revealed using 3D rotational angiography. We selected 1.4-mm outer diameter aspiration catheters. (d) The stent retriever (SR) deployed on the clots (arrowhead) as an anchor and the tip of the aspiration catheter (black arrow). (e) The aspiration catheter established contact with a clot via the assisted contact method. (f) Near-complete recanalization visualized by angiography. (g) Lack of hemorrhage on the CT. (h) Retrieved clot.
The predominant methods were solo, assisted, and retrieval contact in the groups with vessel diameters of ≥2.0 mm (44.4%), 1.5–2.0 mm (60.0%), and ≤1.5 mm (54.5%), respectively. Among the asymptomatic SAH cases, 1 (5.6%), 6 (20.0%), and 10 (45.5%) cases occurred in the groups with vessel diameters of ≥2.0 mm, 1.5–2.0 mm, and ≤1.5 mm, respectively. The SAH frequency was significantly higher in the group with a narrower vessel diameter (p = 0.01). Although the number of attempts was significantly lower in 22 patients with an occluded vessel diameter of maximum 1.5 mm compared with that in patients with vessel diameters beyond 1.5 mm (1.27 ± 0.46 vs. 1.81 ± 1.08, p = 0.03), we registered a higher asymptomatic SAH percentage (14.6% vs. 45.5%, p < 0.01). The impact of vessel diameter and contact method on clinical outcome is demonstrated in Tables 3 and 4. The solo contact and assisted contact methods were used to achieve mTICI 2c/3 recanalization in >50% of cases, irrespective of occluded vessel diameter. The 17 cases in which the retrieval contact method was used for vessels smaller than 2.0 mm demonstrated significantly lower recanalization rates than the remaining 53 cases (29.4% vs. 58.5%, p = 0.04). Additionally, the retrieval contact method for the <2.0 mm diameter group and the assisted contact method for the ≤1.5 mm diameter group demonstrated significantly higher SAH frequency than the remaining 47 cases (56.5% vs. 8.5%, p < 0.001).
Table 3.
Success rate of mTICI 2c/3.
| ≥2.0 mm (n = 18) | 1.5–2.0 mm (n = 30) | ≤1.5 mm (n = 22) | |
|---|---|---|---|
| Solo contact | 5/8 (62.5%) | 5/7 (71.4%) | 2/4 (50.0%) |
| Assisted contact | 4/6 (66.7%) | 10/18 (55.5%) | 3/6 (50.0%) |
| Retrieval contact | 2/4 (50.0%) | 1/5 (20.0%) | 4/12 (33.3%) |
mTICI: modified Treatment in Cerebral Ischemia Scale.
Table 4.
Incidence of subarachnoid hemorrhage.
| ≥2.0 mm (n = 18) | 1.5–2.0 mm (n = 30) | ≤1.5 mm (n = 22) | |
|---|---|---|---|
| Solo contact | 1/8 (12.5%) | 1/7 (14.3%) | 0/4 (0%) |
| Assisted contact | 0/6 (0%) | 2/18 (11.1%) | 4/6 (66.7%) |
| Retrieval contact | 0/4 (0%) | 3/5 (60.0%) | 6/12 (50.0%) |
Discussion
In this study, we present the “matching strategy,” designed to achieve both good efficacy and safety in MeVO thrombectomy. Our strategy involves vessel diameter and tortuosity assessment as well as aspiration catheter use of adequate diameter, matching the abovementioned vessel characteristics as a first-line treatment. Rodriguez et al. evaluated 22 studies involving 971 patients undergoing mechanical thrombectomy for MeVO. Results showed that 84% of the patients achieved TICI 2b-3. Further, 64% had favorable functional outcomes at 90 days, and 6% presented with symptomatic ICH. 2 Perez et al. evaluated the clinical outcomes of thrombectomy using blind exchange with the mini-pinning technique, a combined technique incorporating the anchor technique, for MeVO. Results showed that 78.6% of the patients achieved TICI 2b-3 and that 50.9% had favorable functional outcomes at 90 days. Moreover, 1.9% of the patients presented with symptomatic ICH and 23.1% with SAH. 8 The efficacy and safety outcomes of our strategy area were comparable to those of previous studies.2,8,13–15
This strategy is unique due to the vessel diameter-based aspiration catheter selection (rather than following occluded vessel-associated anatomical nomenclature) and the use of stent retrievers as assisted devices when the aspiration catheter alone could not achieve firmly engaging positions.
A basic experiment that compared stent retriever and aspiration catheter pull-out resistance reported that the pull-out resistance during clot retrieval was greater in the stent retriever. 6 Clinical studies have also reported a higher incidence of hemorrhagic complications in the case of MeVO thrombectomy with the stent retriever compared that with the aspiration catheter, and small perforating artery stretching or avulsion during mechanical traction is a major concern.5,7–9 However, thrombectomy using aspiration catheters has a higher recanalization rate associated with a higher catheter-to-vessel ratio, calculated by the division of the nominal inner and outer diameters of the employed aspiration catheter by the vessel diameter.10,11 The outer diameter of commercially available aspiration catheters ranges between approximately 1.2 and 2.2 mm. Therefore, in the case of MeVO with smaller target vessel diameters, matching the aspiration catheter diameter to that of the vessel is easier.
Aspiration catheter use for thrombectomy might reduce pull-out resistance-induced hemorrhagic complications. However, caution should be taken as larger aspiration catheter use might increase the risk of vessel injury during navigation compared with retrieval. Advancements in device technology and anchor technique application have turned distal navigation with larger aspiration catheters less of a technical challenge 16 ; however, anatomical conditions are critical for procedural success. Therefore, the use of 3DRA to confirm tortuosity and vessel diameter up to the occlusion contributes to procedural safety. 12
Even in the case of selecting a sufficiently large aspiration catheter, clot retrieval is not possible without being able to engage it in the catheter. Notably, the surgeon must be aware that engagement is easier when the interaction angle between the aspiration catheter and the clot is closer to yielding a straight line. 17 Furthermore, if suction is initiated with a small gap between the catheter and the clot, this space might be vacuumed and could collapse. The surgeon should also be aware that pulling out the catheter under such conditions might not effectively remove the clot. The sequence of engaging and then starting suction is essential, whether applying solo, assisted, or retrieval contact.18,19
Focusing on vessel diameter and contact method
Using our strategies, the occluded vessel diameter in all cases was measured, which allowed us to conduct an analysis focusing on the vessel diameter. Our study demonstrated a higher SAH incidence after thrombectomy in the group with a smaller occluded vessel diameter. Certain studies indicated that SAH does not correlate with poor clinical outcomes, whereas others reported that asymptomatic intracerebral hemorrhage is associated with worsened clinical outcomes.20,21 As SAH could be a potential catheter manipulation-associated mechanical injury indicator, 7 we think that reducing postprocedural SAH, regardless of the symptoms, contributes to improved safety outcomes. Because the use of a stent retriever has been associated with an increased risk of SAH in thrombectomy for MeVO,22–24 it can be anticipated that SAH will be less likely to occur if thrombectomy is performed solely with an aspiration catheter in all cases. However, in 72.9% of our cases, the combined usage with stent retrievers was necessary to firmly engage the aspiration catheter with the clot. When focusing on the contact methods between the clot and tip of the aspiration catheter, the combined usage with stent retrievers can be categorized into two types: the assisted contact method and retrieval contact method. The use of a stent retriever to navigate the aspiration catheter to the proximal end of the clot is referred to as assisted contact. The role of the stent retriever in the assisted contact method is limited anchoring or correcting the interaction angle. Thus, its invasiveness can be minimal. However, if the operator recognized that the aspiration catheter could not be safely navigated to the proximal end of the clot, a stent retriever was used to pull the clot to the tip of the aspiration catheter and engage it within the catheter. This type of contact method was referred to as retrieval contact. Similar to the use of a stent retriever alone, pull-out resistance in the retrieval contact can be higher than that in the assisted contact. 6 Therefore, we focused on examining the correlation of vessel diameter and contact methods with clinical outcomes.
In the ≥2.0 mm diameter group, the success rate of mTICI 2c/3 exceeded 50%, and the incidence of SAH remained low regardless of the contact method. Even in cases of MeVO, when the occluded vessel diameter is ≥2 mm, the use of stent retrievers may not increase the risk of bleeding, similar to LVO. In the group 1.5–2.0 mm diameter group, 23 cases (76.7%) required stent retriever support for catheter–clot contact. The success rate of mTICI 2c/3 exceeded 50%, and the incidence of SAH remained low with both the solo and assisted contact methods. Conversely, the success rate of mTICI 2c/3 remained at 20%, and the incidence of SAH was high with the retrieval contact method. Avoiding retrieval contact method and using solo or assisted contact method might improve efficacy and safety outcomes in this group. In the ≤1.5 mm diameter group, 18 cases (81.8%) required stent retriever support for catheter–clot contact. The solo contact method alone achieved an mTICI 2c/3 success rate of 50% and a low incidence of SAH. In very small-vessel (≤1.5 mm) thrombectomy, the use of a stent retriever might increase hemorrhagic complications even with supportive usage.
Thrombectomy using the aspiration catheter alone had high success rates of recanalization and low incidence of SAH across all vessel diameter groups. However, in the smaller diameter vessel group, fewer cases reached the occlusion point using the solo contact method, thereby showing a practical need to rely on stent retrievers. Hence, if the vessel is narrower, there are more ledge effects and tortuosity that should be overcome, making it challenging to guide the aspiration catheter to match the vessel diameter. The development of more flexible and low-profile novel aspiration catheters, specially designed novel delivery catheter to minimize the ledge effect, such as the Tenzing series (Route 92 Medical, San Mateo, CA, USA) and SENDit Technology (Penumbra, Alameda, CA, USA), and novel anchoring devices that can control pull-out resistance may help overcome adverse anatomic conditions without stent retrievers.25–27 Further studies should be performed to examine whether advancements in these devices will improve clinical outcomes in the narrower vessel diameter group.
Based on the abovementioned results, the occluded vessel diameter could be a clinical indicator in MeVO thrombectomy. Discussing validity based on the occluded vessel diameter rather than the anatomical nomenclature might be more beneficial for MeVO outcome evaluation. The use of the retrieval contact method with conventional stent retrievers for vessels with a diameter of <2.0 mm is unlikely to result in acceptable outcomes. The anatomical assessment of whether an aspiration catheter can be navigated independent of a conventional stent retriever is essential, particularly in narrower vessels.
Limitations
This study had a retrospective observational design, and the sample size in each vessel diameter group was small. Furthermore, we analyzed the effective and safety outcomes by focusing on the diameter of the occluded vessel, but not the aspiration catheter type, meaning that different catheter types with similar diameters might produce different results. Although the discussion covered various contact methods and the SAH incidence, it did not consider the stent retriever types, meaning that the different stent retriever types could yield different results. The matching strategy is a procedural approach that involves accurate vessel diameter assessment, selecting a matching aspiration catheter, then firmly engaging the clot. This strategy allows for a high degree of flexibility to the surgeon. Therefore, the results might vary depending on the skill and experience. However, as this is a simple, theoretical foundation-based strategy, it could become universally applicable despite the future introduction of various aspiration catheter sizes and shapes into the market.
Conclusion
The matching strategy is an effective and safe approach for MeVO thrombectomy. However, in the smaller diameter vessel group, the occlusion point was reached using the solo contact method only in a few cases. Further, the dependence on the stent retriever increased, resulting in a higher incidence of SAH. To identify the validity of MeVO thrombectomy, it is essential to focus on the occluded vessel diameter and conduct an anatomical assessment of whether matched aspiration catheter can be navigated independent of a conventional stent retriever.
Acknowledgment
The authors would like to thank Enago (http://www.enago.jp) for the English language review.
Footnotes
Author contributions: Yujiro Tanaka, Conceptualization, Methodology, Data curation, Writing – Original Draft, Visualization. Daisuke Watanabe, Conceptualization, Methodology, Writing – Review & Editing, Visualization. Yusuke Kanoko, Investigation, Writing – Review & Editing. Aya Inoue, Investigation, Data curation, Writing – Review & Editing. Daichi Kato, Investigation, Writing – Review & Editing. Shota Igasaki, Investigation, Writing – Review & Editing. Akira Kikuta, Investigation, Writing – Review & Editing. Motoyori Ogasawara, Investigation, Writing – Review & Editing. Kodai Kanemaru, Investigation, Writing – Review & Editing. Hibiku Maruoka, Investigation, Writing – Review & Editing.
Data availability: Raw data were generated at Fujieda Municipal General Hospital and IMS Tokyo Katsushika General Hospital. Derived data supporting the findings of this study area available from the corresponding author on request.
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Ethics approval: This study was approved by the review boards of Fujieda Municipal General Hospital (approval number: R05-10) and IMS Tokyo Katsushika General Hospital (approval number: R05-71).
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iD: Yujiro Tanaka https://orcid.org/0000-0003-4529-0489
References
- 1.Marchal A, Bretzner M, Casolla B, et al. Endovascular thrombectomy for distal medium vessel occlusions of the middle cerebral artery: a safe and effective procedure. World Neurosurg 2022; 160: e234–e241. [DOI] [PubMed] [Google Scholar]
- 2.Rodriguez-Calienes A, Vivanco-Suarez J, Sequeiros JM, et al. Mechanical thrombectomy for the treatment of primary and secondary distal medium-vessel occlusion stroke: systematic review and meta-analysis. J Neurointerv Surg 2023; 15: e460–e467. [DOI] [PubMed] [Google Scholar]
- 3.Menon BK, Hill MD, Davalos A, et al. Efficacy of endovascular thrombectomy in patients with M2 segment middle cerebral artery occlusions: meta-analysis of data from the HERMES collaboration. J Neurointerv Surg 2019; 11: 1065–1069. [DOI] [PubMed] [Google Scholar]
- 4.Schulze-Zachau V, Brehm A, Ntoulias N, et al. Incidence and outcome of perforations during medium vessel occlusion compared with large vessel occlusion thrombectomy. J Neurointerv Surg 2023; 31: jnis-2023. [DOI] [PubMed] [Google Scholar]
- 5.Saber H, Narayanan S, Palla M, et al. Mechanical thrombectomy for acute ischemic stroke with occlusion of the M2 segment of the middle cerebral artery: a meta-analysis. J Neurointerv Surg 2018; 10: 620–624. [DOI] [PubMed] [Google Scholar]
- 6.Tanaka Y, Kanoko Y, Yokoyama T, et al. Experimental validation of pullout resistance for stent retrievers and aspiration catheters. J Neuroendovasc Ther 2022; 16: 446–451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Pilgram-Pastor SM, Piechowiak EI, Dobrocky T, et al. Stroke thrombectomy complication management. J Neurointerv Surg 2021; 13: 912–917. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Pérez-García C, Moreu M, Rosati S, et al. Mechanical thrombectomy in medium vessel occlusions: blind exchange with mini-pinning technique versus mini stent retriever alone. Stroke 2020; 51: 3224–3231. [DOI] [PubMed] [Google Scholar]
- 9.Baharvahdat H, Ooi YC, Khatibi K, et al. Increased rate of successful first passage recanalization during mechanical thrombectomy for M2 occlusion. World Neurosurg 2020; 139: e792–e799. [DOI] [PubMed] [Google Scholar]
- 10.Kyselyova AA, Fiehler J, Leischner H, et al. Vessel diameter and catheter-to-vessel ratio affect the success rate of clot aspiration. J Neurointerv Surg 2021; 13: 605–608. [DOI] [PubMed] [Google Scholar]
- 11.Nikoubashman O, Nikoubashman A, Büsen M, et al. Necessary catheter diameters for mechanical thrombectomy with ADAPT. AJNR Am J Neuroradiol 2017; 38: 2277–2281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Rosi A, Bernava G, Hofmeister J, et al. Three-dimensional rotational angiography improves mechanical thrombectomy recanalization rate for acute ischaemic stroke due to middle cerebral artery M2 segment occlusions. Interv Neuroradiol 2022; 18: 15910199221145745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Romano DG, Frauenfelder G, Caragliano A, et al. Multicentric experience with an intermediate aspiration catheter for distal M2 ischemic stroke. J Stroke Cerebrovasc Dis 2020; 29: 105389. [DOI] [PubMed] [Google Scholar]
- 14.Haussen DC, Al-Bayati AR, Eby B, et al. Blind exchange with mini-pinning technique for distal occlusion thrombectomy. J Neurointerv Surg 2020; 12: 392–395. [DOI] [PubMed] [Google Scholar]
- 15.Grossberg JA, Rebello LC, Haussen DC, et al. Beyond large vessel occlusion strokes: distal occlusion thrombectomy. Stroke 2018; 49: 1662–1668. [DOI] [PubMed] [Google Scholar]
- 16.Singh J, Wolfe SQ, Janjua RM, et al. Anchor technique: use of stent retrievers as an anchor to advance thrombectomy catheters in internal carotid artery occlusions. Interv Neuroradiol 2015; 21: 707–709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bernava G, Rosi A, Boto J, et al. Direct thromboaspiration efficacy for mechanical thrombectomy is related to the angle of interaction between the aspiration catheter and the clot. J Neurointerv Surg 2020; 12: 396–400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Guenego A, Mine B, Bonnet T, et al. Thrombectomy for distal medium vessel occlusion with a new generation of Stentretriever (Tigertriever 13). Interv Neuroradiol 2022; 28: 444–454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Johnson S, Dwivedi A, Mirza M, et al. A review of the advancements in the in vitro modelling of acute ischemic stroke and its treatment. Front Med Technol 2022; 4: 879074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Suzuki K, Matsumaru Y, Takeuchi M, et al. The impact of SAH finding on CT to the clinical outcome after mechanical thrombectomy for large vessel occlusion. J Neurol Sci 2023; 453: 120797. [DOI] [PubMed] [Google Scholar]
- 21.Jiang F, Zhao W, Wu C, et al. Asymptomatic intracerebral hemorrhage may worsen clinical outcomes in acute ischemic stroke patients undergoing thrombectomy. J Stroke Cerebrovasc Dis 2019; 28: 1752–1758. [DOI] [PubMed] [Google Scholar]
- 22.Renieri L, Valente I, Dmytriw AA, et al. Mechanical thrombectomy beyond the circle of Willis: efficacy and safety of different techniques for M2 occlusions. J Neurointerv Surg 2022; 14: 546–550. [DOI] [PubMed] [Google Scholar]
- 23.Maegerlein C, Prothmann S, Lucia KE, et al. Intraprocedural thrombus fragmentation during interventional stroke treatment: a comparison of direct thrombus aspiration and stent retriever thrombectomy. Cardiovasc Intervent Radiol 2017; 40: 987–993. [DOI] [PubMed] [Google Scholar]
- 24.Haussen DC, Eby B, Al-Bayati AR, et al. A comparative analysis of 3MAX aspiration versus 3 mm Trevo retriever for distal occlusion thrombectomy in acute stroke. J Neurointerv Surg 2020; 12: 279–282. [DOI] [PubMed] [Google Scholar]
- 25.Grieb D, Greling B, Schulz K, et al. Endovascular treatment of distal medium vessel occlusions using microcatheter aspiration thrombectomy. Interv Neuroradiol 2024; 30: 234–241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Dallas J, Nguyen VN, Sequeiros JM, et al. Distal mechanical thrombectomy using beveled tip aspiration zoom catheters: a preliminary study. Interv Neuroradiol 2024; 3: 15910199241258289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Settecase F, Kim WT, Sivapatham T, et al. Improved catheter delivery for aspiration thrombectomy using Tenzing 7 ledge reducing catheter and FreeClimb 70. Interv Neuroradiol 2023; 28: 15910199231177754. [DOI] [PubMed] [Google Scholar]