Abstract
Background
Every patient in residential healthcare has a bed. Falling out of bed is associated with preventable patient harm. Various interventions to prevent injury are available. Bed rails are the most common intervention designed to prevent patients falling out of bed; however, their effectiveness is uncertain and bed rail entrapment can also result in injuries.
Objectives
To assess the effectiveness of interventions designed to prevent patient injuries and falls from their beds.
Search methods
We searched the Cochrane Injuries Group Specialised Register, Cochrane Central Register of Controlled Trials 2010, Issue 2 (The Cochrane Library), MEDLINE (Ovid), EMBASE (Ovid), CINAHL (EBSCO), ISOI Web of Science and Web‐based trials registers (all to December 2010) as well as reference lists.
Selection criteria
Randomised controlled trials of interventions designed to prevent patient injuries from their beds which were conducted in hospitals, nursing care facilities or rehabilitation units were eligible for inclusion.
Data collection and analysis
Two review authors independently assessed the risk of bias and extracted data from the included studies. Authors contacted investigators to obtain missing information.
Main results
Two studies met the inclusion criteria, involving a total of 22,106 participants. One study tested low height beds and the other tested bed exit alarms. Both studies used standard care for their control group and both studies were conducted in hospitals. No study investigating bed rails met the inclusion criteria. Due to the clinical heterogeneity of the interventions in the included studies pooling of data and meta‐analysis was inappropriate, and so the results of the studies are described.
A single cluster randomised trial of low height beds in 18 hospital wards, including 22,036 participants, found no significant reduction in the frequency of patient injuries due to their beds (there were no injuries in either group), patient falls in the bedroom (rate ratio 0.69, 95% CI 0.35 to 1.34), all falls (rate ratio 1.26, 95% CI 0.83 to 1.90) or patient injuries due to all falls (rate ratio 1.35, 95% CI 0.68 to 2.68).
One randomised controlled trial of bed exit alarms in one hospital geriatric ward, involving 70 participants, found no significant reduction in the frequency of patient injuries due to their beds (there were no injuries in either group), patient falls out of bed (rate ratio 0.25, 95% CI 0.03 to 2.24), all falls (rate ratio 0.42, 95% CI 0.15 to 1.18) or patient injuries due to all falls (no injuries in either group).
Authors' conclusions
The effectiveness of interventions designed to prevent patient injuries from their beds (including bed rails, low height beds and bed exit alarms) remains uncertain. The available evidence shows no significant increase or decrease in the rate of injuries with the use of low height beds and bed exit alarms. Limitations of the two included studies include lack of blinding and insufficient power. No randomised controlled trials of bed rails were identified. Future reports should fully describe the standard care received by the control group.
Keywords: Humans, Beds, Accidental Falls, Accidental Falls/prevention & control, Equipment Design, Equipment Safety, Randomized Controlled Trials as Topic, Safety Management, Safety Management/methods, Wounds and Injuries, Wounds and Injuries/prevention & control
Plain language summary
Interventions designed to prevent healthcare bed‐related injuries in patients
Patients in hospitals, nursing care facilities and rehabilitation units sometimes fall out of bed. Associated injuries include skin lacerations, bone fractures, joint dislocations and brain haemorrhage, and these injuries may result in permanent disability and death. Bed rails are the most common intervention designed to prevent patients falling out of bed. However, reports of fatal bed rail entrapment have caused uncertainty regarding their use. Determining which interventions effectively and safely prevent patient injuries from their beds would be beneficial and allow healthcare staff an evidence‐based practice.
Two randomised studies are included in this review. Both studies targeted patients most likely to fall. One trial was of low height beds (22,036 patients) and the other investigated bed exit alarms (70 patients). The results of each study showed there is no significant increase or decrease in the rate of injuries or falls from bed. Although one study was large, fewer than half of the patients received a low height bed and so this group of patients may have been too small to detect a statistically significant benefit or harm in the analysis.
No randomised controlled trials of bed rails were found. The researchers suggest that future reports should fully describe what standard care was received by the control group.
Background
The bed is essential and ubiquitous in healthcare, but it can be the source of preventable patient harm. Falling out of bed is the most common cause of bed‐related injury. The most common intervention designed to prevent patients falling out of bed are bed rails. However, the effectiveness of bed rails is uncertain and patients have died through bed rail entrapment.
In the United States, Medicare no longer pays for the treatment of falls from bed or bed rail entrapment and passes this cost to the healthcare organisation. Therefore, there are both medical and financial incentives for addressing this challenge (Rosenthal 2007). This review aims to evaluate interventions designed to prevent patient injuries from their beds.
Description of the condition
In healthcare, a fall may be defined as an unintended impact with the ground, which may or may not result in physical or psychological harm (Campbell 1981). The incidence of falls among elderly patients in hospitals is between 4‐14 per 1000 bed days (Healey 2008) and between 1.6‐10 per 1000 bed days in long‐term care institutions such as nursing homes and rehabilitation units (Rubenstein 2006). Between 20‐25% of all falls in healthcare are from the bed (NPSA 2007a).
Injury is defined as physical harm and can be categorised into serious injury or minor injury. Serious injury includes skin lacerations that require suturing, bone fractures, joint dislocations and intra‐cranial haemorrhage. Minor injury includes physical harm that does not result in suturing, fractures, dislocations or intra‐cranial haemorrhage. One third of falls are associated with injury in hospital or nursing home care, with head injury rates of 214 per 1000 person years in women and 433 per 1000 person years in men (Nurmi 2002). The incidence of fractures is up to 70 per 1000 person years in nursing homes and 9 out of 10 fractures are the result of a fall (Ytterstad 1999).
Other consequences of falls include anxiety and depression, a fear of falling, increased length of hospital stay and increased healthcare costs (Murphy 1982; Vetter 1989; Bates 1995). Falls are the most commonly reported patient safety incident. The consequences for the healthcare organisation include complaints, litigation and the costs of compensation (Oliver 2008).
Risk factors for falls include older age, physical weakness, imbalance, gait disturbance, poor vision, limited mobility, cognitive impairment, impaired functional status and postural hypotension (Rubenstein 2006). Risk factors for bed rail entrapment include older age and cognitive impairment (Todd 1997).
Description of the intervention
Bed rails are also known as cot sides, side rails and safety rails. The term 'bed rails' in this review refers to rails on the sides of adult patients' beds and not to the use of rails on trolleys or children's cots. Bed rails are used for 8‐64% of hospital patients and 9‐71% of nursing home patients internationally (Healey 2008). Bed rails are used for 8‐25% of hospital in‐patients at night (O'Keeffe 1996; Healey 2009). Interventions for the prevention of patient injuries from their beds other than bed rails are rarely implemented and sparsely represented in the literature. They include low height beds (Haines 2010), bed exit alarms (Capezuti 2009) and bed‐side floor mats (Hoffman 2003; Bowers 2008).
How the intervention might work
Patients can fall out of bed by slipping, sliding or rolling (NPSA 2007b). Bed rails prevent this by providing a physical and visual barrier. Low height beds reduce the kinetic energy of the fall and the chance of injury. Bed‐side floor mats soften the impact with the ground. Bed exit alarms detect movements which indicate that the patient is about to get out of bed, and may be at risk of falling, or has already fallen from the bed. By immediately alerting healthcare professionals to provide the patient with assistance, bed exit alarms might reduce both the frequency of falling out of bed and the consequences of injured patients remaining unattended.
Why it is important to do this review
Bed rails cause fatal injuries through entrapment (Miles 1996; Miles 1998; Jehan 1999; Osculati 2000; Miles 2002; O'Connor 2003). A review of incident reports spanning a period of 21 years (1985‐2006) revealed that 691 incidents of bed rail entrapment were reported to the Food & Drug Administration in the United States. Of these incidents, 413 resulted in death and 120 resulted in injuries (FDA 2006). Of 74 bed rail‐associated deaths identified over a 4‐year period (1993‐1996) in the United States; 70% were caused by entrapment between the mattress and a bed rail which left the face pressed against the mattress, 18% were caused by entrapment and compression of the neck within the bed rails, and 12% were caused by entrapment between the bed rails after sliding partially off the bed and having the neck flexed or the chest compressed (Parker 1997).
If the bed rail barrier is insufficient to prevent a patient from exiting their bed, the patient must then reach the ground from the top of the bed rail, which is higher than the mattress and may result in more severe injuries. However, retrospective and before‐and‐after studies of removing bed rails (or reducing their use) have either found no significant difference or an increased rate of injuries and falls (Brown 1997; Hanger 1999; van Leeuwen 2001; Capezuti 2002; Hoffman 2003; Krauss 2005; NPSA 2007a). A recent systematic review regarding bed rails included non‐randomised before‐and‐after studies, cohort studies, case‐control studies, retrospective surveys and case reports. This concluded that bed rails were not associated with an increased frequency of injuries or falls and tentatively suggested that safely designed and appropriately implemented bed rails may be beneficial (Healey 2008).
Despite this evidence, an accurate measure of harm caused by bed rails is unknown, because voluntary incident reporting systems and non‐randomised controlled studies are open to bias. Currently, the literature remains divided as to the effectiveness of bed rails. Some authors advocate reducing the use of bed rails (Capezuti 2007), but "requests for bed rails being ignored" is the second most commonly cited reason to pursue litigation in the event of an injurious fall (Oliver 2008).
The aim of this review is to systematically identify and evaluate evidence from randomised controlled trials and cluster randomised controlled trials of interventions designed to prevent injuries to patients from their beds. This will allow the quality of the currently available evidence to be demonstrated, healthcare staff an evidence‐based practice, best practice standards to be set and key areas for future research to be identified.
Objectives
To assess the effectiveness of interventions designed to prevent patient injuries from their beds.
Methods
Criteria for considering studies for this review
Types of studies
All randomised controlled trials and cluster randomised controlled trials investigating interventions designed to prevent patient injuries from their beds.
Types of participants
Adult patients in residential healthcare were included. Adults were defined as people aged 18 years or older. The definition of residential healthcare includes hospital in‐patients, nursing home patients and patients in rehabilitation units.
This review does not include patients in Accident & Emergency departments on trolleys, patients receiving day case surgery, patients at General Practitioner facilities, patients at out‐patient clinics and patients receiving nursing care at home.
Types of interventions
Eligible interventions included:
bed rails;
low height beds;
bed exit alarms;
bed‐side floor mats;
educational programmes and protocols to prevent falls;
other interventions designed to prevent patient injuries from their beds.
Interventions such as physical restraint devices applied to the patient's body or chemical restraint (e.g. sedation) were excluded.
Types of outcome measures
Primary outcome measures formed part of the inclusion criteria.
Primary outcomes
Frequency of patient injuries from their beds.
Frequency of patient falls out of bed.
Secondary outcomes
Frequency of patient injuries due to falls out of bed.
Frequency of patient injuries due to the intervention (e.g. bed rail entrapment).
Frequency of all falls in the study populations.
Frequency of patient injuries due to all falls in the study populations.
Frequency of all patient injuries in the study populations.
Search methods for identification of studies
Our search for studies was not restricted by date, language or publication type.
Electronic searches
We searched the following electronic databases:
Cochrane Injuries Group Specialised Register (searched 15th December 2010);
Cochrane Central Register of Controlled Trials 2010, Issue 2 (The Cochrane Library);
MEDLINE (Ovid) 1950 to 21st December 2010;
EMBASE (Ovid) 1947 to 20th December 2010;
CINAHL (EBSCO) 1982 to 21st December 2010;
ISI Web of Science: Science Citation Index Expanded (SCI‐EXPANDED) (1970 to December 2010);
ISI Web of Science: Conference Proceedings Citation Index‐Science (CPCI‐S) (1990 to December 2010);
The full search strategies are presented in Appendix 1.
Searching other resources
We searched the reference lists of all relevant trial reports and reviews in order to find further eligible studies. We searched the Internet using Google www.google.com (on 22nd December 2010) with selected terms from the MEDLINE search strategy and used the same selected terms to search the Online trials database www.clinicaltrials.gov (on 22nd December 2010).
We contacted bed manufacturers and searched their Web sites for any further unpublished or grey literature. The list of bed manufacturers we contacted can be found in Appendix 2.
Data collection and analysis
We collated the results of the searches into a single list of titles, abstracts and keywords of citations.
Selection of studies
Two review authors (OA and PB) independently screened the titles, abstracts and keywords of all citations found in the searches and decided if they were potentially relevant. Two review authors (OA and PB) obtained the full text of all potentially relevant articles and independently assessed whether each study met the pre‐determined inclusion criteria (Anderson 2011).
We requested further information from the authors of all included, excluded and ongoing studies. Ten study authors and two bed manufacturers replied. One author (Haines 2010) provided additional unpublished data (rate ratios and standard errors).
One author (OA) is a content area expert and one (PB) is a methodology expert. All authors knew the details of the papers being reviewed. The third review author (GH), who is a second methodology expert, would have independently arbitrated disagreements regarding study inclusion had there been any.
Data extraction and management
Two review authors (OA and PB) extracted data from selected studies independently using a data collection form. The third review author (GH) would have independently resolved disagreements had they occurred. We extracted data regarding "the total number of events in each group, and the total amount of person‐time at risk in each group" to allow count data to be analysed as rates according to the Cochrane Handbook section 7.7.5.4 (Higgins 2008). We extracted the total number of participants as part of the description of the study although this is not required for an analysis of rate data. We also extracted data on the following:
study design;
participant characteristics;
intervention characteristics;
outcome measures;
statistical analyses.
Assessment of risk of bias in included studies
Two review authors (OA and PB) independently assessed included studies for risk of bias using the recommended tool in the Cochrane Handbook section 8.5 (Higgins 2008). The assessed criteria included: sequence generation, allocation concealment, blinding of participants, personnel and outcome assessors, incomplete outcome data, selective outcome reporting and other potential threats to validity. The third review author (GH) would have independently resolved disagreements had they occurred. The review authors' judgements and the reasons for these decisions are recorded in risk of bias tables and in Figure 1 and Figure 2.
1.
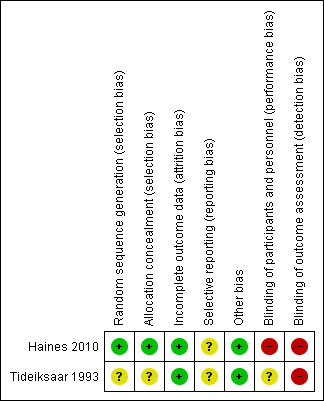
Risk of bias summary: review authors' judgements about each risk of bias item for each included study.
2.
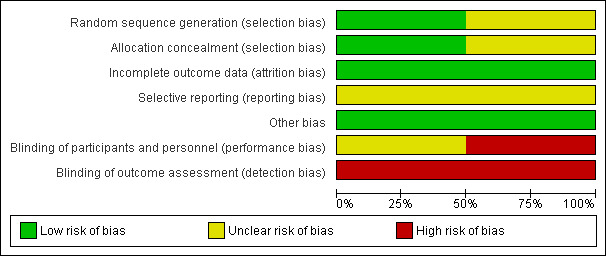
Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included studies. Please note there are only two studies included in this review.
Measures of treatment effect
We calculated the rate ratio and standard error of outcome data according to the Cochrane Handbook section 9.4.8 and 16.3 (Higgins 2008). For the Tideiksaar 1993 study, data from the study report were used. Haines 2010 provided us with original study data and we calculated the rate ratio and standard error ourselves.
Unit of analysis issues
We converted data into rate ratios. We assessed data from cluster randomised trials according to the Cochrane Handbook section 16.3 (Higgins 2008). We sought statistical advice to determine if the effect estimates and standard errors reported formed correct analyses that took account of the cluster design. As the analysis was correct, the data were analysed using the generic inverse variance method. (If the reported analysis had not taken account of the cluster design, we would have conducted approximate analyses by calculating effective sample sizes if the required data were available, including: number of clusters randomised to each group; or the average (mean) size of each cluster, number or proportion of individuals with events, or means and standard deviations and an estimate of the intra cluster correlation coefficient. If neither of these methods had been possible, we would have analysed data from cluster randomised trials at the level of allocation using a summary measurement from each cluster.)
Dealing with missing data
We requested additional and missing data from the original authors of all included and excluded studies. We conducted an intention to treat analysis and there were no participants missing due to drop‐out. We received replies from the authors of seven out of fifteen studies that reported the rate of all falls, but did not report the rate of patient injuries from their beds or falls out of bed. However none of them provided the rate of patient injuries from their beds or falls out of bed, because this data was not collected.
Assessment of heterogeneity
We assessed clinical heterogeneity by determining whether the intervention and control groups between the studies had the same participants, interventions and outcomes. We did not perform a meta‐analysis or assess statistical heterogeneity, because the two included studies had different interventions.
Assessment of reporting biases
We did not assess reporting bias through the symmetry of funnel plots, because there were too few studies to include.
Data synthesis
We did not pool data for meta‐analysis, because clinical heterogeneity between the two included studies made this inappropriate.
Subgroup analysis and investigation of heterogeneity
We intended to investigate subgroups, as described in the protocol for this review (Anderson 2011), but insufficient data were available and no subgroup analysis was performed.
Sensitivity analysis
We did not perform a sensitivity analysis, because of the risk of bias in both included studies.
Results
Description of studies
See: Characteristics of included studies; Characteristics of excluded studies; and Characteristics of ongoing studies.
Results of the search
Our searches found: 117 records from the Cochrane Injuries Group Specialised Register, 205 records from the Cochrane Central Register of Controlled Trials, 199 records from MEDLINE, 266 records from EMBASE, 93 records from CINAHL, 240 records from Web of Science and 0 from Current Controlled Trials. Collating the results of these searches yielded a total of 698 unique records. Three additional, potentially relevant papers were identified from searches of Google, the Web sites of healthcare bed manufacturers or bibliography searches of relevant papers and progressed to full text review (Figure 3).
3.
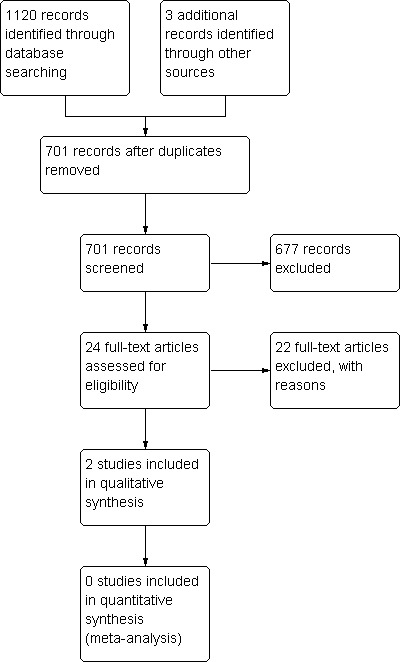
Study retrieval and selection process
Included studies
Twenty‐four studies were considered for this review of which two studies with a combined total of 22,106 participants met the criteria for inclusion. One of the included studies used a cluster randomised design (Haines 2010) and the other used an individually randomised design (Tideiksaar 1993). All 22,106 participants were hospital in‐patients. One study was set in 18 general hospital wards the other was set in one geriatric hospital ward. The studies were conducted in Australia and in the USA. The cluster randomised study contributed 22,036 participants and did not report their demographics. The other study contributed 70 participants, 14% of these were male and the mean age was 84 (range 67‐97) years. In both studies, the intervention was delivered to hospital patients that were at a high‐risk of falling based on the results of a falls risk assessment.
Both included studies randomised a single intervention and compared this with a control group that received standard care. The use of bed rails was not mentioned in either study as being included in standard care. Participants in both studies were followed up until they were discharged from the hospital wards. Both included studies reported the frequency of patient injuries from their beds, all falls and patient injuries due to all falls. The cluster randomised study reported the frequency of patient falls in the bedroom and the individually randomised study reported the frequency of patient falls out of bed. The intervention in the cluster randomised trial was low height beds. The low height beds had a height range of 28.5‐64cm above the ground. The height range of normal beds was not reported. Experimental wards received one low height bed for every 12 normal beds. The intervention in the individually randomised study was the use of bed exit alarms. Due to the clinical heterogeneity of the interventions, pooling of data and meta‐analysis was inappropriate.
Excluded studies
Twenty‐two studies were excluded. Four studies were not randomised trials. One study examining bed exit alarms was excluded, because the primary outcome measure was reduction in the use of physical restraints and not patient injuries from their beds or falls out of bed (Kwok 2006). In fifteen studies, the objective was the prevention of all falls and not patient injuries from their beds or falls out of bed, which were not reported. Another two studies were neither randomised trials nor designed with the primary objective of preventing patient injuries from their beds or falls out of bed.
Risk of bias in included studies
Both included studies gathered data on the primary outcome measure from incident reports completed by healthcare staff who were not blinded to the allocation of the intervention (Figure 1; Figure 2).
Generation of the randomisation sequence (selection bias)
In one study, the randomisation sequence was generated by a coin toss (Haines 2010). The generation of the randomisation sequence was not described in the other study (Tideiksaar 1993).
Allocation
Haines 2010 allocated clusters based on the randomly generated sequence. The allocation of individual participants was not described in sufficient detail in the other study (Tideiksaar 1993).
Blinding
Neither study blinded the participants, healthcare staff or outcome assessors.
Incomplete outcome data
Both studies accounted for 100% of their data. In the cluster randomised study, one ward ceased using the intervention half way through the intended time period (3 instead of 6 months). This intervention ward was paired with a control ward. Data from both wards were included in the intention to treat analysis for the period of time that the intervention was not in use (Haines 2010).
Selective reporting
No study protocol was available for either study and so selective outcome reporting could not be assessed. The cluster randomised study reported the frequency of patient falls in the bedroom. This was made up of patients who were witnessed to have fallen out of bed or found fallen at the bedside or in the bedroom. The frequency of falls out of bed was not reported, because an unknown number of patients were found fallen at the bedside or in the bedroom.
Other potential sources of bias
No other potential sources of bias were identified in the included studies. The cluster randomised study demonstrated insufficient information to determine recruitment bias, but did demonstrate that there was no baseline imbalance or loss of clusters and a correct analysis for clustering was used (Haines 2010).
Effects of interventions
Due to the clinical heterogeneity of the interventions in the included studies, pooling of data and meta‐analysis was inappropriate.
Frequency of patient injuries from their beds.
In both studies there were no patient injuries from their beds. As there were no injuries, an effect is not estimable (Appendix 3).
Frequency of patient falls out of bed.
Tideiksaar 1993 found no significant reduction in the rate of patient falls out of bed (rate ratio 0.25, 95% CI 0.03 to 2.24; 1 trial, 70 participants).
Haines 2010 found no significant reduction in the rate of falls in the bedroom, which included falls out of bed (rate ratio 0.69, 95% CI 0.35 to 1.34; 1 trial, 22,036 participants).
| Study ID | Effect measure | Treatment effect | 95% CI | N (intervention) | N (control) | Standard error |
| Haines 2010 | Rate ratio (calculated by review authors) | 0.69 | 0.35 to 1.34 | 12 183 | 9 853 | 0.35 |
| Tideiksaar 1993 | Rate ratio (calculated by review authors) | 0.25 | 0.03 to 2.24 | 35 | 35 | 1.12 |
Frequency of patient injuries due to falls out of bed.
The frequency with which patients were injured from falls from their beds was not reported in Haines 2010 and no injuries were reported in Tideiksaar 1993. Therefore the outcome was not estimable.
Frequency of patient injuries due to the intervention (e.g. bed rail entrapment).
In both studies there were no patient injuries due to the intervention; therefore an effect is not estimable.
Frequency of all falls in the study populations.
Neither study found a significant reduction in the rate of all falls in the intervention group.
| Study ID | Effect measure | Treatment effect | 95% CI | N (intervention) | N (control) | Standard error |
| Haines 2010 | Rate ratio (calculated by review authors) | 1.26 | 0.83 to 1.90 | 12 183 | 9 853 | 0.21 |
| Tideiksaar 1993 | Rate ratio (calculated by review authors) | 0.42 | 0.15 to 1.18 | 35 | 35 | 0.53 |
Frequency of patient injuries due to all falls in the study populations.
Haines 2010 found no reduction in the rate of patient injuries due to all falls in the intervention group. In the Tideiksaar 1993 study there were no injuries in the intervention or the control group.
| Study ID | Effect measure | Treatment effect | 95% CI | N (intervention) | N (control) | Standard error |
| Haines 2010 | Rate ratio (calculated by review authors) | 1.35 | 0.68 to 2.68 | 12 183 | 9 853 | 0.34 |
| Tideiksaar 1993 | Rate ratio (calculated by review authors) | Not estimable | Not estimable | 35 | 35 | Not estimable |
Frequency of all patient injuries in the study populations.
The frequency of all patient injuries was not reported in either study.
Discussion
Summary of main results
We systematically reviewed the effectiveness of interventions designed to prevent injuries to patients from their beds. We included 2 studies that randomised 22,106 participants. Data on the rate of patient injuries from their beds, falls from bed and all falls were extracted.
Pooled results
Due to the clinical heterogeneity of the interventions, pooling of data and meta‐analysis was inappropriate.
Low height beds
One trial in hospitals investigated low height beds (Haines 2010). This study did not demonstrate that low height beds significantly reduced the rate of patient injuries from their beds, falls in the bedroom, all falls or injuries due to all falls. The study was powered to detect a >50% reduction in the rate of falls. It was suggested by the authors that this study may be underpowered to detect a clinically significant benefit. The conditions of the comparator group, such as the minimum height of standard beds, were not described. The trends favoured low height beds for bedroom falls, but favoured the control for all falls and injuries due to all falls.
Bed exit alarms
One trial in hospitals investigated bed exit alarms (Tideiksaar 1993). This study did not demonstrate that bed exit alarms significantly reduced the rate of patient injuries from their beds, falls from bed, all falls or injuries due to all falls. It was suggested by the authors that this study may be underpowered to detect a clinically significant benefit. The conditions of the comparator group were not controlled.
Overall completeness and applicability of evidence
The objective of this review was to assess the effectiveness of interventions designed to prevent patient injuries from their beds. We have established that the evidence currently available does not demonstrate that interventions designed to prevent patient injuries from their beds are effective. Included studies investigated low height beds and bed exit alarms. No randomised controlled trials of bed rails or bed‐side floor mats were identified. Therefore, all relevant types of intervention have not been adequately investigated.
The outcome measures used in the two included studies focused on falls, including falls from bed and falls with injuries. They did not focus on injuries that were not due to falls, which is important to assess, especially if the intervention may cause harm to the patient in any way other than through falls. Both trials reported that there were no adverse consequences due to the interventions.
Neither of the included studies incorporated an economic analysis to determine if the interventions provided value for money.
Quality of the evidence
Two studies incorporating 22,106 participants were included. Neither study blinded the participants or the healthcare staff to the allocation of the intervention. Healthcare staff reported injuries and falls and so these outcomes may have been subject to reporting bias. Also, both studies may have been underpowered. Overall the quality of evidence is insufficient to conclude that interventions designed to prevent patient injuries from their beds have no significant benefit.
Potential biases in the review process
After we reviewed titles and abstracts, only a single foreign language study progressed to full text review. This was excluded, because the primary objective of the intervention was prevention of falls and not falls from bed. No foreign language restrictions were imposed on the search strategy and multiple databases were searched.
Agreements and disagreements with other studies or reviews
We identified no previous reviews incorporating the two included studies or interventions such as bed exit alarms, low height beds and bed‐side floor mats.
Bed rails are commonly implemented to prevent healthcare bed‐related injuries in patients and have been reviewed (Healey 2008). A review of bed rails incorporating non‐randomised studies, that were excluded from this review, concluded "that serious direct injury from bedrails is usually related to use of outmoded designs and incorrect assembly rather than being inherent" (Healey 2008). The review incorporated non‐randomised studies, none of which met 100% of the quality criteria, and the size of the included studies was small thereby limiting power. The findings of this review do "not support the prevailing orthodoxy that bedrails increase the likelihood of falls and injury, or that bedrails result in an inherent risk of fatal entrapment" (Healey 2008).
Authors' conclusions
Implications for practice.
There is insufficient evidence from randomised controlled trials to conclude that interventions designed to prevent patient injuries from their beds are effective, including: low height beds, bed exit alarms, bed‐side floor mats and bed rails. Instead, this review demonstrates that there is a lack of high‐quality evidence for or against the use of these interventions. Until the results of more randomised controlled trials are available, healthcare staff will rely on clinical judgement and less robust forms of evidence on which to base their decisions. Readers are advised that pragmatic guidance regarding bed rail design to prevent entrapment is available (FDA 2006; MHRA 2006).
Implications for research.
Future trials of interventions designed to reduce patient injuries from their beds should report the outcome 'patient injuries from their beds' in addition to 'falls out of bed,' 'patient injuries due to falls out of bed,' 'patient injuries due to the intervention,' 'all falls,' 'patient injuries due to all falls,' and 'all patient injuries' to allow direct comparisons between studies. Reports of future trials should clearly describe how the researchers performed sequence generation, allocation concealment, blinding, controlled conditions of comparator groups and objective measures of outcomes to address the potentially significant effects of bias. Future trials should report the risk factors for falls in participants and investigate sub‐groups of high‐risk fallers that may benefit from targeted interventions tailored to their needs.
This review included two studies that investigated the effectiveness of low height beds and bed exit alarms for the prevention of patient injuries from their beds. Neither of these studies found a significant effect of the intervention. Both of these studies were potentially underpowered and open to bias. This review demonstrates that more randomised trials of interventions designed to prevent patient injuries from their beds are required to allow healthcare staff an evidence‐based practice and best practice standards to be set.
What's new
| Date | Event | Description |
|---|---|---|
| 9 February 2012 | Amended | The plain language title was changed. |
History
Protocol first published: Issue 1, 2011 Review first published: Issue 11, 2011
| Date | Event | Description |
|---|---|---|
| 14 November 2011 | New citation required but conclusions have not changed | Author contact details amended. |
Acknowledgements
The authors wish to thank Karen Blackhall for help with the searches, Emma Sydenham for general advice, Terence Haines for providing unpublished raw data and explaining the original analysis and Mary‐Jane Anderson for help with statistics.
This study forms part of a program of research from the Designing Out Medical Errors project. <www.domeproject.org.uk> The DOME project is funded by a grant from the Engineering and Physical Sciences Research Council.
The Department of Surgery and Cancer is affiliated with the Clinical Safety Research Unit and the Centre for Patient Safety and Service Quality at Imperial College Healthcare NHS Trust which is funded by the National Institute of Health Research.
Appendices
Appendix 1. Search strategies
Cochrane Injuries Group Specialised Register (searched 15 Dec 2010) Bed* or bedside* or bed‐side* or bedrail* or bed‐rail* or siderail* or side‐rail* or cotside* or cot‐side* or floormat* or floor‐mat* or exit‐alarm* or exit‐sensor* or (bed* and (high or low* or height))
Cochrane Central Register of Controlled Trials (The Cochrane Library 2008, Issue 2) #1. BEDS single term (MeSH) #2. (bed* or bedside*) #3. ((side* next rail*) or (safety next rail*) or (security next rail*)) #4. (bedrail* or siderail* or cotside*) #5. (floormat* or (floor near mat*)) #6. (exit* next (alarm* or sensor*)) #7. (ultra‐low or (low next height)) #8. (#1 or #2 or #3 or #4 or #5 or #6 or #7) #9. ACCIDENTS single term (MeSH) #10. ACCIDENTAL FALLS single term (MeSH) #11. ACCIDENT PREVENTION explode tree 1 (MeSH) #12. WOUNDS AND INJURIES explode tree 1 (MeSH) #13. (fall* or faller* or fell or injur* or accident*) #14. #9 or #10 or #11 or #12 or #13 #15. HOSPITALS explode tree 1 (MeSH) #16. RESIDENTIAL FACILITIES explode tree 1 (MeSH) #17. HOSPITALIZATION single tem (MeSH) #18. INSTITUTIONALIZATION single tem (MeSH) #19. LONG‐TERM CARE single tem (MeSH) #20. ((care or nursing or residential or aged) near (institution* or facilit* or home*)) #21. ((care) near (long next term)) #22. hospital* #23. (#15 or #16 or #17 or #18 or #19 or #20 or #21 or #22) #24. (#8 and #14 and #23)
MEDLINE (Ovid) 1950 to 21st December 2010 1. Beds/ 2. (bed$1 or bedside$1 or bed?side$1).tw. 3. ((side$1 or safety or security) adj3 rail$1).tw. 4. (bedrail$1 or bed?rail$1 or siderail$1 or side?rail$1 or cotside$1 or cot?side$1).tw. 5. (floormat* or floor?mat$1 or ((floor) adj3 mat$1)).tw. 6. (exit$ adj3 (alarm$1 or sensor$1)).tw. 7. (ultra‐low or ((low$) adj3 height)).tw. 8. (bed?height or bed?exit$ or bed?alarm$1 or bed?sensor$1 or bed?mat$1).tw. 9. or/1‐8 10. Accidents/ 11. Accidental Falls/ 12. exp Accident Prevention/ 13. exp "Wounds and Injuries"/ 14. (fall$1 or faller$1 or fell or injur$ or accident$).tw. 15. or/10‐14 16. exp Hospitals/ 17. exp Residential Facilities/ 18. Hospitalization/ 19. Institutionalization/ 20. Long‐Term Care/ 21. ((care or nursing or residential or aged) adj3 (institution$1 or facilit$ or home$1)).tw. 22. ((long?term or longterm) adj3 care).tw. 23. hospital$1.tw. 24. or/16‐23 25. and/9, 15, 24 26. Randomized Controlled Trials/ 27. Random Allocation/ 28. Double Blind Method/ 29. Single Blind Method/ 30. Cross‐Over Studies/ 31. randomi?ed.tw. 32. randomized controlled trial.pt. 33. controlled clinical trial.pt. 34. cluster randomi?ed trial.pt. 35. placebo.tw. 36. clinical trials as topic.sh. 37. random$.tw. 38. or/26‐37 39. (animals not (humans and animals)).sh. 40. 38 not 39 41. 25 and 40
EMBASE (Ovid) 1947 to 20th December 2010
1. exp Bed/ 2. (bed$1 or bedside$1 or bed?side$1).tw. 3. ((side$1 or safety or security) adj3 rail$1).tw. 4. (bedrail$1 or bed?rail$1 or siderail$1 or side?rail$1 or cotside$1 or cot?side$1).tw. 5. (floormat* or floor?mat$1 or ((floor) adj3 mat$1)).tw. 6. (exit$ adj3 (alarm$1 or sensor$1)).tw. 7. (ultra‐low or ((low$) adj3 height)).tw. 8. (bed?height or bed?exit$ or bed?alarm$1 or bed?sensor$1 or bed?mat$1).tw. 9. or/1‐8 10. Falling/ 11. Accident/ 12. exp Injury/ 13. Accident Prevention/ 14. (fall$1 or faller$1 or fell or injur$ or accident$).tw. 15. or/10‐14 16. exp Hospital/ 17. Residential Home/ 18. Nursing Home/ 19. Home for the Aged/ 20. exp Long Term Care/ 21. Hospitalization/ 22. Institutionalization/ 23. ((care or nursing or residential or aged) adj3 (institution$1 or facilit$ or home$1)).tw. 24. ((long?term or longterm) adj3 care).tw. 25. hospital$1.tw. 26. or/16‐25 27. and/9, 15, 26 28. Randomized Controlled Trial/ 29. Double Blind Procedure/ 30. Single Blind Procedure/ 31. Crossover Procedure/ 32. Controlled Study/ 33. Controlled Clinical Trial/ 34. randomi?ed.tw. 35. randomized controlled trial.pt. 36. controlled clinical trial.pt. 37. cluster randomi?ed trial.pt. 38. placebo.tw. 39. clinical trials as topic.sh. 40. or/28‐39 41. (animals not (humans and animals)).sh. 42. 40 not 41 43. 27 and 42
CINAHL 1982 to 21st December 2010
1. exp Beds And Mattresses/ 2. (bed$1 or bedside$1 or bed?side$1).tw. 3. ((side$1 or safety or security) adj3 rail$1).tw. 4. (bedrail$1 or bed?rail$1 or siderail$1 or side?rail$1 or cotside$1 or cot?side$1).tw. 5. (floormat* or floor?mat$1 or ((floor) adj3 mat$1)).tw. 6. (exit$ adj3 (alarm$1 or sensor$1)).tw. 7. (ultra‐low or ((low$) adj3 height)).tw. 8. (bed?height or bed?exit$ or bed?alarm$1 or bed?sensor$1 or bed?mat$1).tw. 9. or/1‐8 10. Accidents/ 11. Accidental Falls/ 12. exp "Wounds and Injuries"/ 13. Fall Prevention/ 14. (fall$1 or faller$1 or fell or injur$ or accident$).tw. 15. or/10‐14 16. exp Hospitals/ 17. exp Residential Facilities/ 18. Hospitalization/ 19. Institutionalization/ 20. Nursing Home Patients/ 21. Long Term Care/ 22. ((care or nursing or residential or aged) adj3 (institution$1 or facilit$ or home$1)).tw. 23. ((long?term or longterm) adj3 care).tw. 24. hospital$1.tw. 25. or/16‐24 26. and/9, 15, 25 27. exp Clinical Trials/ 28. exp Evaluation Research/ 29. Comparative Studies/ 30. Crossover Design/ 31. randomi?ed.tw. 32. randomized controlled trial.pt. 33. controlled clinical trial.pt. 34. cluster randomi?ed trial.pt. 35. placebo.tw. 36. clinical trials as topic.sh. 37. trial.ti. 38. or/27‐37 39. (animals not (humans and animals)).sh. 40. 38 not 39 41. 26 and 40
ISI Web of Science: Science Citation Index Expanded (SCI‐EXPANDED) (1970 to December 2010) ISI Web of Science: Conference Proceedings Citation Index‐Science (CPCI‐S) (1990 to December 2010);
#1.TS=(bed or beds or bedside or bedsides or bed‐side or bed‐sides) #2.TS=(bedrail or bedrails or bed‐rail or bed‐rails or siderail or siderails or side‐rail or side‐rails or safety‐rail or security‐rail or ((side or sides or safety or security) SAME (rail or rails))) #3.TS=(cotside or cotsides or cot‐side or cot‐sides or (cot SAME (side or sides))) #4.TS=(floormat or floormats or floor‐mat or floor‐mats or (floor SAME (mat or mats))) #5.TS=((bed‐exit or exit) SAME (alarm or alarms or sensor or sensors or bed‐sensor or bed‐sensors)) #6. or/1‐6 #7.TS=(fall or falls or faller or fallers or fell or injur* or accident*) #8. 6 and 7 #9.TS=((care or nursing or residential or aged) SAME (institution* or facilit* or home*)) #11.TS=((longterm or long‐term or (long adj1 term)) adj1 care) #12.TS=hospital* #13. or/9‐12 #14. 8 and 13 #15.TS=((crossover) or (cross‐over) or (cross SAME over)) #16. TS=((single or double or triple) SAME (blind)) #17. TS=(random*) #18. TS=((cluster‐trial) or (cluster SAME trial) #19. TS=(placebo*) #20. or/15‐19 #21. 14 and 20
Current Controlled Trials [www.controlled‐trials.com/] (searched on 2010 December 22)
ICRCTN Register (International) copy of ISRCTN Register
Action Medical Research (UK) ‐ subset from ISRCTN Register
Medical Research Council (UK) ‐ subset from ISRCTN Register
NIH ClinicalTrials.gov Register (International) ‐ subset of randomised trial records
NIHR Health Technology Assessment Programme (HTA) (UK) ‐ subset from ISRCTN Register
The Wellcome Trust (UK) ‐ subset from ISRCTN Register
UK trials (UK) ‐ subset from ISRCTN Register, UK trials only
Appendix 2. Details of contacted bed manufacturers
| Company name | Website address | E‐mail address |
| Hill‐Rom UK | http://www.hill‐rom.co.uk | uk.marketing@hill‐rom.com |
| Sigma‐care | http://www.sigmabed.com/ | sigmabed@ms64.hinet.net |
| Narang Medical | http://www.narang.com/ | NET@narang.com |
| Invacare | http://www.invacare.co.uk/index‐home.php | uk@invacare.com |
| Park House Healthcare | http://www.parkhouse‐hc.com/ | info@parkhouse‐hc.com |
| Scan Mobility | http://www.scanmobility.co.uk/ | sales@scanmobility.co.uk |
| Talley Group | http://www.talleygroup.com/ | sales@talleygroup.com |
| Days Healthcare | http://www.dayshealthcare.co.uk/ | info@dayshealthcare.co.uk |
| Linet | http://linet.uk.com/ | info@linet.uk.com |
| Volker | http://www.nursingbeds.co.uk/index.php | info@volker.co.uk |
| Harvest Healthcare | http://www.harvesthealthcare.biz/ | sales@harvesthealthcare.biz |
| Liscare | http://www.lisclare.com/ | info@lisclare.com |
| Sidhil | http://www.sidhil.com/ | sales@sidhil.com |
| Pavillion Medical | http://www.pavillionmedical.com/ | info@pavillionmedical.com |
| Huntleigh Healthcare | http://www.arjo.com/ukh/default.asp | http://www.arjo.com/ukh/Contact.asp?PageNumber=2029 |
| Nightingale Care Beds | http://www.nightingalebeds.co.uk/ | info@nightingalebeds.co.uk |
| Pegasus Healthcare | http://www.pegasushealthcare.com/index.html | http://www.pegasushealthcare.com/Contact_Us.html |
| Westmeria | http://www.westmeria.co.uk/ | enquiry@westmeria.com |
| Prism Medical | http://www.prismmedical.co.uk/ | info@prismmedical.co.uk |
| Tr Equipment Limited | http://www.trequipment.se/ | info@trequipment.se |
| Astor‐Bannerman (Medical) Limited | http://www.astorbannerman.co.uk/ | sales@astorbannerman.co.uk |
| Newstyle | http://www.newstylehealthcareservices.co.uk/ | http://www.newstylehealthcareservices.co.uk/index.php?id=contact |
| Well Run Technology Co., Ltd. | http://www.wellrun.com.tw/ | http://www.wellrun.com.tw/contactus.php |
| Renqiu Medical Equipment Factory | http://www.kangerle.com | medical@kangerle.com |
| Hospex‐Health Co., Ltd. | http://www.hospex‐health.com/ | info@hospex‐health.com |
| Zhangjiagang Aegean Technology Co., Ltd. | http://www.aegeantech.com | sales@aegeantech.com |
| Zhangjiagang City Yongxin Medical‐Use Facilities Making Co., Ltd. | http://www.yongxinsb.cn/ | sales@yongxinsb.cn |
| Hebei Baiyang Bed Manufactory | http://www.baiyangcy.com | baiyang@baiyangcy.com |
| Jinan Zhong Ya Sincerity Import & Export Co., Ltd. | http://www.jnzyxc.com | jnzyxc98@jjnjachem.cn |
| Ticare Medical Instruments Co., Ltd. | http://www.ticare.net/ch/index.asp | enquiry@ticare.net |
| Shanghai Carable Medical Instrument Co., Ltd. | http://www.care‐able.com/index.html | careable@126.com |
| Guangdong Heshan Litai Medical Healthcare Equipment Ltd. | http://www.hslitai.com | litai@hslitai.com |
| Ningbo Hecai Medical Equipment Co.,Ltd. | http://www.nbhecai.com/en/index.aspx | trade@nbhecai.com |
| Guangdong Kaiyang Medical Technology Co., Ltd. | http://en.nhkaiyang.com/newEbiz1/EbizPortalFG/portal/html/index.html | ky@nhkaiyang.com |
| Chang Gung Medical Supplies & Equipment Corp. | http://www.cgmc.com.tw/ | cgmc@cgmc.com.tw |
| Ningbo Kangmailong Medical Apparatus Co., Ltd. | http://www.chinakml.com/ | kml88@chinakml.com |
| Zhongshan Aolike Medical Equipment Technology Co., Ltd. | http://www.aolike.net/home.html | sales@aolike.net |
| YOHO Wheelchair Factory | http://www.yohowheelchair.com/ | yohowheelchair@hotmail.com |
| Zhangjiagang Medycon Machinery Co., Ltd. | http://www.medycon.net/En/About.htm | sales@medycon.com |
| Kangshen Medical Equipment Factory | http://www.gdkangshen.com/enindex.asp | info@gdkangshen.com |
| Poly Medical and Health Product Factory | http://www.poly‐medical.com/ | gztianhe@pub.guangzhou.gd.cn |
| Shanghai Power Flower Medical Equipment Co.,Ltd. | http://www.shrhyl.com/english/Html/main.asp | shrhyl@163.com |
| Tianjin Xuhua Medical Equipment Factory | http://www.xuhuamedical.com/ | david@xuhuamedical.com |
| Worldcare International Enterprise Limited | http://www.hkworldcare.com/index.asp | hkworldcare@163.com |
| Ginnian Medical Equipment Co., Ltd. | http://www.ginnian.com/main/home/main.php | ginnian@yeah.net |
| Shenzhen OTTO Technology Co., Ltd. | http://www.otto‐med.com/index.asp | otto_cathy@vip.163.com |
| Galaxy Medical Equipments & Instruments Co., Ltd. | http://www.gmeok.com/en/products.htm | info@gmeok.com |
| Hangzhou Dunli Medical Instruments Co., Ltd. | http://www.dunlimedical.com/en/ | dunlimedical@dunli.com |
| Medtrue Enterprise Co., Ltd. | http://www.medtrue.com/medtrue/check.html | info@medtrue.com |
| Jiangsu Defeng Medical Equipment Co., Ltd. | http://www.defeng‐medic.com/eng/ | chris@defeng‐medic.com |
| Foshan Suncare Medical Products Co., Ltd. | http://www.suncare‐medical.com/ | sales@suncare‐medical.com |
| Zhangjiagang CentraLand Imp & Exp Co., Ltd. | centralandhardware@gmail.com | |
| Suzhou Uniontech Imp. & Exp. Co., Ltd. | http://www.szutmedical.com/index.htm | sales@szutmedical.com |
| Shanghai JWFU Industry Co., Ltd. | http://en.jwfu.com | sales@jwfu.cn |
| Shanghai Keling International Trading Co., Ltd. | http://www.shkeling.com/en/ | sale@shkeling.com |
| TRIUP International Corp. | http://www.triup.com/ | triup@triup.com |
| Nanjing Foinoe Co., Ltd. | http://www.foinoe.com/ | info@foinoe.com |
| Meditech India | http://www.meditech‐india.com/enquiry.html | info@meditech‐india.com |
Appendix 3. Outcomes that were not estimable
| Study ID | Intervention | Outcomes that were not estimable |
| Haines 2010 | Low height beds vs standard care | Frequency of patient injuries from their beds Frequency of patient injuries due to falls out of bed Frequency of patient injuries due to the intervention Frequency of all patient injuries in the study populations |
| Tideiksaar 1993 | Bed exit alarms vs standard care |
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Haines 2010.
| Methods | Cluster randomised trial. 18 wards matched into pairs on the basis of their pre‐intervention fall rates. Randomised with a coin toss. No blinding. 1 ward ceased using the intervention after 3 of the intended 6 months. Data were included from the one ward that ceased using the intervention and that of its matched pair ward for the same time period in the intention to treat analysis. |
|
| Participants | Setting: 18 publicly funded hospital wards in Queensland, Australia with no previous access to the intervention. N: admissions (occupied bed days) 22,036 (131,805) Inclusion criteria: all admissions. Exclusion criteria: nil. |
|
| Interventions | One "low‐low" (28.5‐64cm height) bed for every 12 regular beds per ward. Control group received standard care. |
|
| Outcomes | Falls were recorded by staff as incident reports.
|
|
| Notes | No significant difference in outcomes demonstrated. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Coin tossing. |
| Allocation concealment (selection bias) | Low risk | Central allocation. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Missing outcome data balanced in intervention and control group and unlikely to be introducing bias. |
| Selective reporting (reporting bias) | Unclear risk | The study protocol was not available. |
| Other bias | Low risk | The study appears to be free of other sources of bias. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Staff were not blinded to ward allocation; participants were not blinded to the intervention. |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Staff who recorded falls were not blinded to the ward allocation status. |
Tideiksaar 1993.
| Methods | Randomised controlled trial. Method of randomisation not reported. No blinding. No losses to follow up reported. Intention‐to‐treat analysis. |
|
| Participants | Setting: one geriatric ward in the USA. N=70 Sample: 14% male. Age: mean (range) 84 (67‐97) years. Inclusion criteria: poor bed mobility (according to one or more abnormal factors on an observational 9 point performance‐orientated environmental mobility screen). Exclusion criteria: nil. |
|
| Interventions | Bed‐alarm system that produces an audible alert when the patient is about to exit or exits their bed. Control group received standard care. |
|
| Outcomes | 1. Frequency of patient falls out of bed; 2. Frequency of all falls; 3. Frequency of patient injuries due to all falls; 4. Alarm response times; 5. Number of true alarms. | |
| Notes | No significant difference in outcomes demonstrated. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Insufficient information about the sequence generation process was available to permit judgement. |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information about the sequence generation process was available to permit judgement. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No incomplete outcome data. |
| Selective reporting (reporting bias) | Unclear risk | The study protocol was not available. |
| Other bias | Low risk | The study appears to be free of other sources of bias. |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Not stated. |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Outcomes were recorded by the study nurses who were not blind to intervention group. |
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Bowling 1992 | The primary objective of the intervention (hospital or nursing home care) was prevention of falls and not bed‐related injuries, which were not reported. |
| Broe 2007 | The primary objective of the intervention (vitamin D) was prevention of falls and not bed‐related injuries, which were not reported. |
| Burleigh 2007 | The primary objective of the intervention (vitamin D) was prevention of falls and not bed‐related injuries, which were not reported. |
| Capezuti 2002 | The intervention (physical restraint reduction) was not randomly assigned. |
| Cumming 2008 | The primary objective of the multifactorial intervention was prevention of falls and not bed‐related injuries, which were not reported. |
| Dykes 2010 | The primary objective of the intervention (fall prevention tool kit risk assessment) was prevention of falls and not bed‐related injuries, which were not reported. |
| Fonda 2006 | The multi strategy intervention was not randomly assigned and the primary objective of the intervention was prevention of falls and not bed‐related injuries, which were not reported. |
| Kelly 2002 | The intervention (bed‐exit alarm) was not randomly assigned. |
| Koczy 2005 | The primary objective of the intervention was prevention of falls and not bed‐related injuries, which were not reported. |
| Kwok 2006 | The primary outcome of the intervention (bed‐exit alarm) was reduction of physical restraint use. |
| Latham 2003 | The primary objective of the intervention (exercise & vitamin D) was prevention of falls and not bed‐related injuries, which were not reported. |
| Law 2006 | The primary objective of the intervention (vitamin D) was prevention of falls and not bed‐related injuries, which were not reported. |
| Lightbody 2002 | The primary objective of the multifactorial intervention was prevention of falls and not bed‐related injuries, which were not reported. |
| Morgan 2004 | The primary objective of the intervention (exercise) was prevention of falls and not bed‐related injuries, which were not reported. |
| O'Halloran 2004 | The primary objective of the intervention (hip protectors) was prevention of falls and not bed‐related injuries, which were not reported. |
| Ray 1997 | The primary objective of the intervention (consultation service) was prevention of falls and not bed‐related injuries, which were not reported. |
| Ray 2005 | The primary objective of the intervention (staff education) was prevention of falls and not bed‐related injuries, which were not reported. |
| Reuben 1995 | The primary objective of the intervention (comprehensive geriatric assessment) was prevention of falls and not bed‐related injuries, which were not reported. |
| Schwendimann 2006 | The intervention (multi‐component) was not randomly assigned. |
| Spetz 2007 | The intervention (bed‐exit alarm) was not randomly assigned. |
| Vassallo 2004 | The primary objective of the intervention (multi‐disciplinary team) was prevention of falls and not bed‐related injuries, which were not reported. |
| Young 2005 | The intervention (multi‐disciplinary team) was not randomly assigned and the primary objective of the intervention was prevention of falls and not bed‐related injuries, which were not reported. |
Characteristics of ongoing studies [ordered by study ID]
Vass 2009.
| Trial name or title | REFINE (Reducing Falls in In‐patient Elderly). |
| Methods | Randomised controlled trial. Randomisation performed with a computer independently. Blinded data analysis only. Intention to treat analysis. |
| Participants | Setting: five geriatric wards in the UK. |
| Interventions | Bed and chair exit alarms. Control group receives standard care. |
| Outcomes |
|
| Starting date | August 2008 |
| Contact information | catherine.vass@nottingham.ac.uk (Corresponding author) |
| Notes |
Differences between protocol and review
The secondary outcomes: Frequency of all falls in the study population, Frequency of injuries due to all falls in the study population and Frequency of all patient injuries in the study population were added at the review stage. These additional outcomes provide useful information, because some interventions may decrease the rate of bed‐related falls and injuries, but increase the rate of all falls and injuries, e.g. because low‐height beds are easier for the patient to exit, the patient may be more likely to sustain injuries away from the bedside. The outcome: Frequency of falls in the bedroom, was included, because the outcome, Frequency of patient falls out of bed was open to bias in the cluster randomised study (Haines 2010).
Contributions of authors
Oliver Anderson is the first author and first conceived the idea for this review; all authors contributed to the protocol.
Oliver Anderson conducted the searches with the aid of Karen Blackhall. Piers Boshier contacted bed manufacturers. Oliver Anderson and Piers Boshier screened titles and abstracts and reviewed full text papers and extracted data. Oliver Anderson and Professor George Hanna contacted study authors. Professor George Hanna provided arbitration, however none was required. Oliver Anderson wrote the manuscript and Piers Boshier and Professor George Hanna reviewed the manuscript.
Sources of support
Internal sources
No sources of support supplied
External sources
Engineering and Physical Sciences Research Council, UK.
National Institute of Health Research, UK.
Declarations of interest
None known.
Edited (no change to conclusions)
References
References to studies included in this review
Haines 2010 {published and unpublished data}
- Haines TP, Bell RAR, Varghese PN. Pragmatic, Cluster Randomized Trial of a Policy to Introduce Low‐Low Beds to Hospital Wards for the Prevention of Falls and Fall Injuries. Journal of the American Geriatrics Society 2010;58(3):435‐41. [PUBMED: 20398112] [DOI] [PubMed] [Google Scholar]
Tideiksaar 1993 {published data only (unpublished sought but not used)}
- Tideiksaar R, Feiner CF, Maby J. Falls prevention: the efficacy of a bed alarm system in an acute care setting. The Mount Sinai journal of medicine, New York 1993;60(6):522‐7. [PUBMED: 8121429] [PubMed] [Google Scholar]
References to studies excluded from this review
Bowling 1992 {published data only (unpublished sought but not used)}
- Bowling A, Formby J, Grant K. Accidents in elderly care: a randomised controlled trial (part 3). Nursing Standard 1992;6(31):25‐7. [DOI] [PubMed] [Google Scholar]
Broe 2007 {published data only (unpublished sought but not used)}
- Broe KE, Chen TC, Weinberg J, Bischoff‐Ferrari HA, Holick MF, Kiel DP. A higher dose of vitamin d reduces the risk of falls in nursing home residents: a randomized, multiple‐dose study. Journal of the American Geriatrics Society 2007;55(2):234‐9. [DOI] [PubMed] [Google Scholar]
Burleigh 2007 {published data only (unpublished sought but not used)}
- Burleigh E, McColl J, Potter J. Does vitamin D stop inpatients falling? A randomised controlled trial. Age & Ageing 2007;36(5):507‐13. [DOI] [PubMed] [Google Scholar]
Capezuti 2002 {published data only (unpublished sought but not used)}
- Capezuit E, Maislin G, Strumpf N, Evans LK. Side rail use and bed‐related fall outcomes among nursing home residents. Journal of the American Geriatrics Society 2002;50(1):90‐6. [DOI] [PubMed] [Google Scholar]
Cumming 2008 {published data only (unpublished sought but not used)}
- Cumming RG, Sherrington C, Lord SR, Simpson JM, Vogler C, Cameron ID, et al. Prevention of Older People's Injury Falls Prevention in Hospitals Research Group. Cluster randomised trial of a targeted multifactorial intervention to prevent falls among older people in hospital. British Medical Journal 758‐60;336(7647):758‐60. [DOI] [PMC free article] [PubMed] [Google Scholar]
Dykes 2010 {published data only (unpublished sought but not used)}
- Dykes PC, Carroll DL, Hurley DL, Lipsitz S, Benoit A, Chang F, et al. Fall prevention in acute care hospitals: a randomized trial. Journal of the American Medical Association 2010;304(17):1912‐8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Fonda 2006 {published data only (unpublished sought but not used)}
- Fonda D, Cook J, Sandler V, Bailey M. Sustained reduction in serious fall‐related injuries in older people in hospital. Medical Journal of Australia 2006;184(8):379‐82. [DOI] [PubMed] [Google Scholar]
Kelly 2002 {published data only (unpublished sought but not used)}
- Kelly KE, Phillips CL, Cain KC, Polissar NL, Kelly PB. Evaluation of a nonintrusive monitor to reduce falls in nursing home patients. Journal of the American Medical Directors Association 2002;3(6):377‐82. [PUBMED: 12807607] [DOI] [PubMed] [Google Scholar]
Koczy 2005 {published data only (unpublished sought but not used)}
- Koczy P, Klie T, Kron M, Bredthauer D, Rissmann U, Branitzki S, et al. Effectiveness of a multifactorial intervention to reduce physical restraints in nursing home residents with dementia [Effektivität einer multifaktoriellen Intervention zur Reduktion von körpernaher Fixierung bei demenzerkrankten Heimbewohnern]. Zeitschrift fur Gerontologie und Geriatrie 2005;38(1):33‐9. [DOI] [PubMed] [Google Scholar]
Kwok 2006 {published data only (unpublished sought but not used)}
- Kwok T, Mok F, Chien WT, Tam E. Does access to bed‐chair pressure sensors reduce physical restraint use in the rehabilitative care setting?. Journal of Clinical Nursing 2006;15(5):581‐7. [PUBMED: 16629967] [DOI] [PubMed] [Google Scholar]
Latham 2003 {published data only (unpublished sought but not used)}
- Latham NK, Anderson CS, Lee A, Bennett DA, Moseley A, Cameron ID. A randomized, controlled trial of quadriceps resistance exercise and vitamin D in frail older people: the Frailty Interventions Trial in Elderly Subjects (FITNESS). Journal of the American Geriatrics Society 2003;51(3):291‐9. [DOI] [PubMed] [Google Scholar]
Law 2006 {published data only (unpublished sought but not used)}
- Law M, Withers H, Morris J, Anderson F. Vitamin D supplementation and the prevention of fractures and falls: results of a randomised trial in elderly people in residential accommodation. Age and ageing 2006;35(5):482‐6. [DOI] [PubMed] [Google Scholar]
Lightbody 2002 {published data only (unpublished sought but not used)}
- Lightbody E, Watkins C, Leathley M, Sharma A, Lye M. Evaluation of a nurse‐led falls prevention programme versus usual care: a randomized controlled trial. Age and ageing 2002;31(3):203‐10. [DOI] [PubMed] [Google Scholar]
Morgan 2004 {published data only (unpublished sought but not used)}
- Morgan RO, Vimig BA, Duque M, Abdel‐Moty E, Devito CA. Low‐intensity exercise and reduction of the risk for falls among at‐risk elders. Journals of Gerontology Series A‐Biological Sciences & Medical Sciences 2004;59(10):1062‐7. [DOI] [PubMed] [Google Scholar]
O'Halloran 2004 {published data only (unpublished sought but not used)}
- O'Halloran PD, Cran GW, Beringer TRO, Kernohan G, O'Neill C, Orr J, et al. A cluster randomised controlled trial to evaluate a policy of making hip protectors available to residents of nursing homes. Age and ageing 2004;33(6):582‐8. [DOI] [PubMed] [Google Scholar]
Ray 1997 {published data only (unpublished sought but not used)}
- Ray WA, Taylor JA, Meador KG, Thapa PB, Brown AK, Kajihara HK, et al. A randomized trial of a consultation service to reduce falls in nursing homes. Journal of the American Medical Association 1997;278(7):57‐62. [PubMed] [Google Scholar]
Ray 2005 {published data only (unpublished sought but not used)}
- Ray WA, Taylor JA, Brown AK, Gideon P, Hall K, Arbogast P, et al. Prevention of fall‐related injuries in long‐term care: a randomized controlled trial of staff education. Archives of internal medicine 2005;165(19):2293‐8. [DOI] [PubMed] [Google Scholar]
Reuben 1995 {published data only (unpublished sought but not used)}
- Reuben DB, Borok GM, Wolde‐Tsadik G, Ershoff DH, Fishman LK, Ambrosini VL, et al. A randomized trial of comprehensive geriatric assessment in the care of hospitalized patients. New England Journal of Medicine 1995;332(20):1345‐50. [DOI] [PubMed] [Google Scholar]
Schwendimann 2006 {published data only (unpublished sought but not used)}
- Schwendimann R, Milisen K, Buhler H, Geest S. Fall prevention in a Swiss acute care hospital setting: Reducing multiple falls. Journal of gerontological nursing 2006;32(3):13‐22. [DOI] [PubMed] [Google Scholar]
Spetz 2007 {published data only (unpublished sought but not used)}
- Spetz J, Jacobs J, Hatler C. Cost effectiveness of a medical vigilance system to reduce patient falls. Nursing economics 2007;25(6):333‐8, 352. [PubMed] [Google Scholar]
Vassallo 2004 {published data only (unpublished sought but not used)}
- Vassallo M, Vignaraja R, Sharma JC, Hallam H, Binns K, Briggs R, et al. The Effect of Changing Practice on Fall Prevention in a Rehabilitative Hospital: The Hospital Injury Prevention Study. Journal of the American Geriatrics Society 2004;52(3):335‐9. [DOI] [PubMed] [Google Scholar]
Young 2005 {published data only (unpublished sought but not used)}
- Young JB, Robinson M, Chell S, Sanderson D, Chaplin S, Burns E, et al. A whole system study of intermediate care services for older people. Age and ageing 2005;34(6):577‐83. [DOI] [PubMed] [Google Scholar]
References to ongoing studies
Vass 2009 {published data only (unpublished sought but not used)}
- Vass CD, Sahota O, Drummond A, Kendrick D, Gladman J, Sach T, et al. REFINE (Reducing Falls in In‐patient Elderly) ‐ A randomised controlled trial. Trials 2009;10(83):1745. [DOI] [PMC free article] [PubMed] [Google Scholar]
Additional references
Anderson 2011
- Anderson O, Boshier P, Hanna G. Interventions to prevent healthcare bed‐related injuries in patients. Cochrane Database of Systematic Reviews 2011, Issue 1. [DOI: 10.1002/14651858.CD008931] [DOI] [PubMed] [Google Scholar]
Bates 1995
- Bates DW, Pruess K, Souney P, Platt R. Serious falls in hospitalized patients: correlates and resource utilization. American Journal of Medicine 1995;99(2):137‐43. [DOI] [PubMed] [Google Scholar]
Bowers 2008
- Bowers B, Lloyd J, Lee W, Powell‐Cope G, Baptiste A. Biomechanical evaluation of injury severity associated with patient falls from bed. Rehabilitation Nursing 2008;33(6):253‐9. [DOI] [PubMed] [Google Scholar]
Brown 1997
- Brown EL. A study of a side rail reduction program in a long‐term care facility: implications for a professional nursing staff. University of Columbia 1997.
Campbell 1981
- Campbell AJ, Reinken J, Allan BC, Martinez GS. Falls in old age: a study of frequency and related clinical factors. Age Ageing 1981;10:264‐70. [DOI] [PubMed] [Google Scholar]
Capezuti 2007
- Capezuti E, Wagner LM, Brush BL, Boltz M, Renz S, Talerico KA. Consequences of an intervention to reduce restrictive side rail use in nursing homes. Journal of the American Geriatrics Society 2007;55(3):334‐41. [DOI] [PubMed] [Google Scholar]
Capezuti 2009
- Capezuti E, Brush BL, Lane S, Rabinowitz HU, Secic M. Bed‐exit alarm effectiveness. Archives of Gerontological Geriatrics 2009;49(1):27‐31. [DOI] [PMC free article] [PubMed] [Google Scholar]
FDA 2006
- United States Food, Drug Administration. Guidance on Hospital Bed Design to Reduce Patient Entrapment. Available from: www.fda.gov/bbs/topics/NEWS/2006/NEW01331.html 2006.
Hanger 1999
- Hanger HC, Ball MC, Wood LA. An analysis of falls in the hospital: can we do without bedrails?. Journal of the American Geriatrics Society 1999;47(5):529‐31. [DOI] [PubMed] [Google Scholar]
Healey 2008
- Healey F, Oliver D, Milne A, Connelly JB. The effect of bedrails on falls and injury: a systematic review of clinical studies. Age and Ageing 2008;37:368‐78. [DOI] [PubMed] [Google Scholar]
Healey 2009
- Healey FM, Cronberg A, Oliver D. Bedrail use in English and Welsh hospitals. Journal of the American Geriatrics Society 2009;57(10):1887‐91. [DOI] [PubMed] [Google Scholar]
Higgins 2008
- Higgins JPT, Green S (editors). Cochrane Handbook for Systematic Reviews of Interventions. The Cochrane Collaboration. Available from www.cochrane‐handbook.org issue Version 5.1.0 [updated March 2011].
Hoffman 2003
- Hoffman SB, Powell‐Cope G, MacClellan L, Bero K. BedSAFE. A bed safety project for frail older adults. Journal of Gerontological Nursing 2003;29(11):34‐42. [DOI] [PubMed] [Google Scholar]
Jehan 1999
- Jehan W. Restraint or protection? The use of bedside rails. Nursing Management (Harrow) 1999;6(2):9‐13. [PubMed] [Google Scholar]
Krauss 2005
- Krauss MJ, Evanoff B, Hitcho E, Ngugi KE, Dunagan WC, Fischer I, et al. A case‐control study of patient, medication, and care‐related risk factors for inpatient falls. Journal of General Internal Medicine 2005;20(2):116‐22. [DOI] [PMC free article] [PubMed] [Google Scholar]
MHRA 2006
- United Kingdom Medicines & Healthcare Regulatory Authority. Device Bulletin: Safe Use of Bed Rails. Available from: http://www.mhra.gov.uk/Publications/Safetyguidance/DeviceBulletins/CON2025348 2006.
Miles 1996
- Miles S. A case of death by physical restraint: new lessons from a photograph. Journal of the American Geriatrics Society 1996;44(3):291‐2. [DOI] [PubMed] [Google Scholar]
Miles 1998
- Miles S, Parker K. Pictures of fatal bedrail entrapment. American Family Physician 1998;58(8):1755, 59‐60. [PubMed] [Google Scholar]
Miles 2002
- Miles SH. Deaths between bedrails and air pressure mattresses. Journal of the American Geriatrics Society 2002;50(6):1124‐4. [DOI] [PubMed] [Google Scholar]
Murphy 1982
- Murphy J, Isaacs B. The post‐fall syndrome. A study of 36 elderly patients. Gerontology 1982;28(4):265‐70. [DOI] [PubMed] [Google Scholar]
NPSA 2007a
- NPSA. Slips, trips and falls in hospital. Available from: www.npsa.nhs.uk 2007.
NPSA 2007b
- NPSA. Safe and effective use of bedrails in hospitals: Resource set 2007. Available from: www.npsa.nhs.uk. 2007.
Nurmi 2002
- Nurmi I, Luthje P. Incidence and costs of falls and fall injuries among elderly in institutional care. Scandinavian Journal of Primary Health Care 2002;20(2):118‐22. [PubMed] [Google Scholar]
O'Connor 2003
- O'Connor B, Moore A, Watts M. Hess' sign produced by bedrail injury. Irish Medical Journal 2003;96(10):313. [PubMed] [Google Scholar]
O'Keeffe 1996
- O'Keeffe S, Jack CI, Lye M. Use of restraints and bedrails in a British hospital. Journal of the American Geriatrics Society 1996;44(9):1086‐8. [DOI] [PubMed] [Google Scholar]
Oliver 2008
- Oliver D, Killick S, Even T, Willmott M. Do falls and falls‐injuries in hospital indicate negligent care ‐ and how big is the risk? A retrospective analysis of the NHS Litigation Authority Database of clinical negligence claims, resulting from falls in hospitals in England 1995 to 2006. Quality and Safety in Health Care 2008;17(6):431‐6. [DOI] [PubMed] [Google Scholar]
Osculati 2000
- Osculati A, Fassina G. Two cases of accidental asphyxia by neck compression between bed bars. American Journal of Forensic Medical Pathology 2000;21(3):217‐9. [DOI] [PubMed] [Google Scholar]
Parker 1997
- Parker K, Miles SH. Deaths caused by bedrails. Journal of American Geriatrics 1997;45(7):797‐802. [DOI] [PubMed] [Google Scholar]
Rosenthal 2007
- Rosenthal MB. Nonpayment for performance? Medicare's new reimbursement rule. New England Journal of Medicine 2007;357(16):1573‐5. [DOI] [PubMed] [Google Scholar]
Rubenstein 2006
- Rubenstein LZ. Falls in older people: epidemiology, risk factors and strategies for prevention. Age and Ageing 2006;35(Supplement 2):ii37‐41. [DOI] [PubMed] [Google Scholar]
Todd 1997
- Todd JF, Ruhl CE, Gross TP. Injury and death associated with hospital bed side‐rails: Reports to the U.S. Food and Drug Administration from 1985‐1995. American Journal of Public Health 1997;87:1675‐7. [DOI] [PMC free article] [PubMed] [Google Scholar]
van Leeuwen 2001
- Leeuwen M, Bennett L, West S, Wiles V, Grasso J. Patient falls from bed and the role of bedrails in the acute care setting. Australian Journal of Advanced Nursing 2001;19(2):8‐13. [PubMed] [Google Scholar]
Vetter 1989
- Vetter N, Ford D. Anxiety and depression scores in elderly fallers. International Journal of Geriatric Psychiatry 1989;4:168‐73. [Google Scholar]
Ytterstad 1999
- Ytterstad B. The Harstad injury prevention study: the characteristics and distribution of fractures amongst elders ‐ an eight year study. International Journal of Circumpolar Health 1999;58(2):84‐95. [PubMed] [Google Scholar]


