Abstract
Acute kidney injury (AKI) is a significant health challenge associated with adverse patient outcomes and substantial economic burdens. Many authors have sought to prevent and predict AKI. Here, we comprehensively review recent advances in the use of artificial intelligence (AI) to predict AKI, and the associated challenges. Although AI may detect AKI early and predict prognosis, integration of AI-based systems into clinical practice remains challenging. It is difficult to identify AKI patients using retrospective data; information preprocessing and the limitations of existing models pose problems. It is essential to embrace standardized labeling criteria and to form international multi-institutional collaborations that foster high-quality data collection. Additionally, existing constraints on the deployment of evolving AI technologies in real-world healthcare settings and enhancement of the reliabilities of AI outputs are crucial. Such efforts will improve the clinical applicability, performance, and reliability of AKI Clinical Support Systems, ultimately enhancing patient prognoses.
Keywords: Artificial intelligence, Acute kidney injury, Machine learning, Clinical decision support systems
INTRODUCTION
Acute kidney injury (AKI) poses significant health and socioeconomic issues, including extended hospital stays, high medical costs, and elevated mortality rates [1,2]. The current AKI definition using the serum creatinine level and urine output has evolved through various clinical trials [3–6]. The NGAL, KIM-1, and L-FABP levels may aid early detection and treatment [7–11]. However, the assays are costly and the utilities of these early marker levels unclear. Also, the levels do not aid the establishment of treatment plans after diagnosis; their clinical utilities are thus limited. Sequential tests are often not scheduled when AKI is not anticipated; the diagnostic contributions of these early markers are thus limited [11–13].
Recently, artificial intelligence (AI) has been used to tackle these limitations [14]. Several studies have used AI to detect AKI early, or to evaluate AKI progression and prognosis [15–18]. However, integration of AI-based AKI systems into clinical practice remains challenging. This review describes the current AI research trends in the AKI context, the challenges posed by model development, and the future integration of AI into AKI research and clinical applications.
THE CURRENT STATE OF AI IN TERMS OF AKI RESEARCH
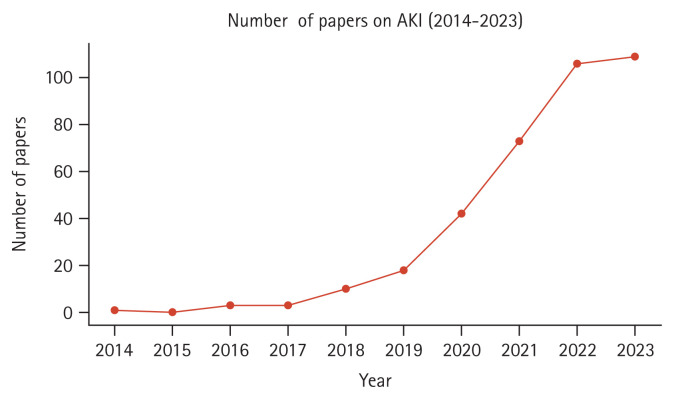
We searched the Web of Science from 2014 to 2023 using the search terms “AKI” OR “Acute Kidney Injury” (Topic) and “Deep Learning” OR “Machine Learning” (Topic). The numbers of relevant publications exhibited a rapid increase in recent years (Fig. 1). The medical data are those of individual institutions and are often not shared because they are personal [19]. Consequently, we initially focused on information in large public databases including the electronic intensive care unit (eICU) and the medical information mart for intensive care (MIMIC) [20–22]. Recent efforts have sought to refine predictions by the target group (patients in general wards or those undergoing specific surgeries); additional datasets have been built [23–26]. Most authors focused on early AKI diagnosis but some attempted to predict prognosis [27–30]. The results were good; the areas under the receiver operating characteristic curves (AUROCs) ranged from 0.7 to 0.9 [31–33]. However, it is unclear whether such models are applicable in real clinical settings. We describe the trends in AI-related AKI research and the challenges in chapter 2.
Figure 1.
The annual numbers of acute kidney injury (AKI) artificial intelligence-related publications.
Labeling issues
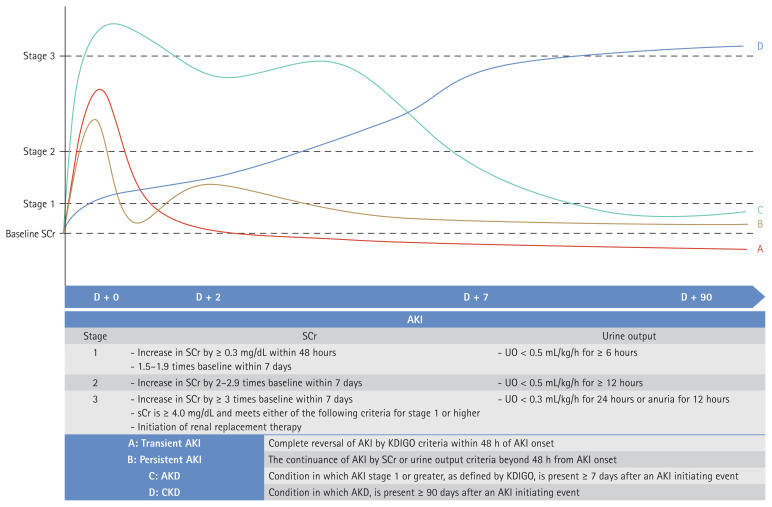
Most researchers use the Kidney Disease: Improving Global Outcomes (KDIGO) criteria when diagnosing AKI; these practical guidelines are based on serum creatinine levels and urine output [34]. Consensus statements have been developed to define recovery of kidney function. Acute kidney disease is defined as AKI of stage 1 persisting for more than 7 days but less than 90 days, and chronic kidney disease is diagnosed when kidney function does not recover after 90 days [35,36]. Figure 2 presents a summary of the various AKI diagnostic criteria. Although these are relatively clear, there is no consensus on how to determine whether AKI persists or if kidney function has recovered. Moreover, there are ongoing concerns regarding the use of serum creatinine levels and the estimated glomerular filtration rate (eGFR); it has been suggested that the GFR reserve (the stimulated GFR minus the basal GFR) might be more appropriate, but practical constraints arise when seeking to overcome the limitations of labeling [37–39].
Figure 2.
AKI definitions. AKI, acute kidney injury; SCr, serum creatinine; UO, urine output; AKD, acute kidney disease; CKD, chronic kidney disease; KDIGO, Kidney Disease: Improving Global Outcomes.
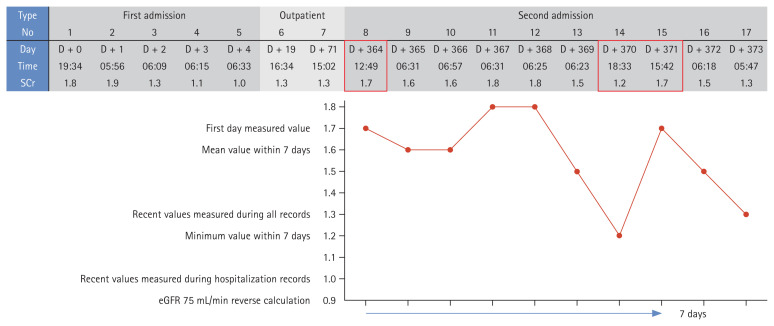
Most machine learning models are developed and evaluated using retrospective data [40–42]. As such data do not track serum creatinine levels as systematically as do prospective studies, the data are incomplete. This limits our ability to specify the exact timing of AKI occurrence and to define recovery [43,44]. Furthermore, an operational definition based on serum creatinine levels and urine output renders patient identification rather ambiguous, raising various issues. When direct patient interaction is limited, the data are inadequate, and the various criteria are inconsistently used; model reliability is low. Thus, AI model development is challenging. Researchers have often used the most recent serum creatinine value before admission or specific surgery as the baseline level. If data are limited, the serum creatinine level on day 1 is used to predict AKI occurrence from day 2 onwards. When a model is to be applied in real-time, the baseline serum creatinine level is dynamically defined based on measurements taken within a specific time (e.g., 48 hours, 168 hours) or a measurement at a specific point, time is ignored (e.g., The most recent measurement before surgery, within the first 24 hours of admission). If multiple serum creatinine measurements are available, the minimum, average, or most recent value is used [45–48]. Figure 3 shows the serum creatinine records of an actual patient. Depending on the baseline serum creatinine criterion and the research design, the patient may or may not have AKI. Accurate labeling is essential when training models. Although most research is based on the KDIGO criteria, the application of the criteria varies across studies, and this is associated with differences in the AKI status of the same patient; incorrect labeling distorts reality [49–51].
Figure 3.
SCr levels and acute kidney injury diagnoses of real patients. SCr, serum creatinine; eGFR, estimated glomerular filtration rate.
The Institutional Review Boards (IRBs) of Soonchunhyang University Cheonan Hospital approved our study protocol (approval numbers: 2019-10-023). The need for informed patient consent was waived by the IRBs as this was a retrospective review of anonymized clinical data.
Other criteria have been used when baseline serum creatinine data are not available. Sometimes, patients lacking such data are excluded. Alternatively, serum creatinine values measured over more than 7 days, or representative values obtained during the hospital stay, or back-calculations based on eGFRs are employed [52–55]. Urine output is rarely recorded in general wards, and only sometimes in intensive care units (ICUs); patients with AKI are thus not ‘labeled’ [56–59]. Of all evaluated AKI cases, only 11% met only the urine output criterion [60]. Moreover, even if the KDIGO criteria are met, it is sometimes difficult to diagnose AKI. Errors in serum creatinine measurements, variations among the measurements, or temporary changes in the levels render it challenging to define the baseline serum creatinine level; the information is fragmented. However, to the best of our knowledge, such situations have not been considered.
Data preprocessing issues
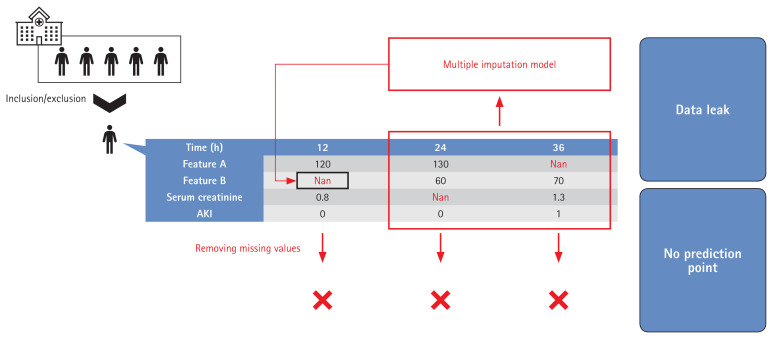
It is essential that the population used for model development is similar to the population to which the model will be applied [61]. Data preprocessing, including the handling of missing and outlier information, is both essential and time-consuming [62,63]. Model development involves definition of the target group, anonymization, handling of outlier and missing data, labeling, and feature selection. The target group characteristics are significantly affected by preprocessing; it is important to describe how the model was developed. The methods used to locate and handle missing data, and the results, must be clearly presented. Such methods include deletion of features or subjects, use of the most recently measured value or a representative value, multiple imputation, model-specific methods, or combinations thereof [64–67]. The method must be practicable, reproducible, and not cause overfitting. For example, if a representative value during the hospital stay is used, how is that value chosen? It may be difficult to find an appropriate value, or the model may be overfitted by the training dataset [68,69]. Some previous studies did not appreciate the importance of missing data handling or did not clearly define the method used. Many works did not even clearly describe the proportions of missing data before and after handling [27,31,70,71]. Care is essential when a model is to be applied in real-time. Depending on the method used to handle missing data, some patients may lack predictive points, leading to overestimations of patient numbers. If multiple imputation is employed, future information that should not be used at earlier points may be employed when handling missing data [72–74]. Figure 4 shows an example of how such situations can lead to overfitting and exaggerated patient numbers, attributable to data leakage during handling of time-series data.
Figure 4.
Overfitting and exaggeration of patient numbers caused by data leakage during processing of time-series data. AKI, acute kidney injury.
Model evaluation issues
Machine learning models discover hidden patterns in training data but can become overfitted by the data [75,76]. Patient populations vary among hospitals, and the data characteristics vary by the equipment used and/or the prescribing practices of physicians [77,78]. Moreover, factors such as the frequencies of infectious diseases (example: COVID-19) change over time, and the continuous development of new drugs and surgical methods change the nature of the data over the years [79,80]. However, many studies employed only single cohorts and, to the best of our knowledge, very few models considered temporal changes [35,81,82].
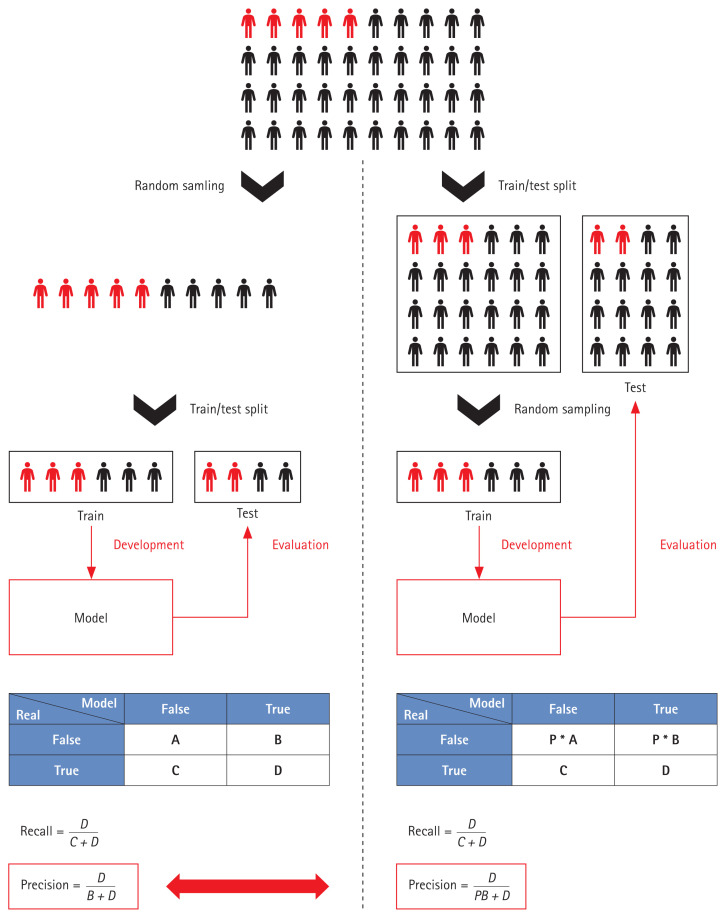
Most model outputs are performance metrics. Performance is measured in various ways, including Accuracy, Precision, Recall, the F1 value, the AUROC, the area under the precision-recall curve, among others, but the limitations mentioned above complicate the evaluation of models based solely on these metrics. The data used for performance evaluation, and the labeling methods and preprocessing methods, differ; it is meaningless to seek to compare model performance. Moreover, when handling a data imbalance during AKI model training, sampling not only of the training data but also the entire dataset can distort the performance metrics. For example, if data imbalance is severe, Recall and Precision are important evaluation metrics. In such cases, as shown in Figure 5, the Precision varies by the sampling method. Table 1 summarizes the key points made above. Full model or code details were also considered important, but very few studies publish them [18,56,60,83,84]; these elements have been excluded from the Table. More references can be found in Supplementary Table 1.
Figure 5.
Variations in performance evaluation by the sampling method employed. Red, diseased populations; Black, non-diseased populations.
Table 1.
Previous studies using artificial intelligence to predict acute kidney injury
| Ref | Year | Task | Baseline Cr | Methods for handling missing data | Model | AUROC | Presentation of missing data proportion | Using of public datasets | Real-time prediction | External validation |
|---|---|---|---|---|---|---|---|---|---|---|
| AKI definition | ||||||||||
| [15] | 2018 | AKI within 48 hours and RRT within 72 hours | The first value measured at the time of admission KDIGO without UO |
After replacing with the most recent values within 12 hours, the remaining were replaced with median and mode | GBM | 0.93 | O | X | O | X |
| [46] | 2019 | Maximum SCr and AKI within 3 days in ICU | Measured value before ICU admission or minimum value on the first day of admission KDIGO with UO |
After excluding features more than 20%, MICE was used | MLP | 0.80 | O | O | X | X |
| [40] | 2018 | AKI within 72 hours in general ward and ICU | Minimum value within 7 days or median within 365 days KDIGO with UO |
Replaced with the most recent values | XGB | 0.87 | X | O | X | X |
| [83] | 2019 | AKI within 48 hours | Median of previous values or estimated value KDIGO with UO |
Missing indicator was used | RNN | 0.92 | X | X | X | X |
| [16] | 2020 | AKI within 48 hours in emergency room, general ward, and ICU | The first value measured at the time of admission KDIGO without UO |
After replacing with the most recent values within 12 hours, the remaining were replaced with median and mode | GBM | 0.86 | X | X | O | O |
| [18] | 2020 | AKI within 48 hours | Last measured value before admission or first measured value after admission KDIGO without UO |
Replaced with the most recent values | GBM | 0.93 | X | O | O | O |
| [33] | 2020 | AKI occurrence in cardiac surgery patients (duration unspecified) | Not clearly stated KDIGO with UO |
Not clearly stated | BN | 0.85 | x | x | △ | O |
| [60] | 2020 | AKI within 7 days after cardiac thoracic surgery | Most recent value within 5 days before surgery KDIGO with UO |
After replacing with the most recent values, the remaining were filled with the same value defined by doctor | RNN | 0.89 | X | X | O | X |
| [31] | 2021 | AKI within 12 hours in ICU | Minimum reported value during hospitalization AKIN with UO |
SCr with the most recent value within 4 hours and urine output with the average within 9 hours | CNN | 0.89 | O | O | O | X |
| [32] | 2021 | AKI within 7 days in hospitalized patients and prediction SCr values over 3 days | The minimum value within 180 days before admission or the first value measured on the day of admission KDIGO without UO |
Replaced with the most recent value | RNN | 0.88 | X | X | O | O |
| [47] | 2021 | AKI within 3 days in ICU | Minimum value within 7 days before ICU admission KDIGO without UO |
Replaced with the most recent values | CNN | 0.84 | X | O | O | X |
| [48] | 2021 | AKI within 48 hours in ICU | Most recent value before admission or 20th percentile of a population with similar characteristics KDIGO with UO |
After replacing with the most recent values, the remaining were filled with the median | CNN | 0.86 | X | O | X | X |
| [51] | 2021 | AKI within 7 days after liver cancer resection surgery | Measured value before surgery KDIGO without UO |
Not clearly stated | RF | 0.92 | X | X | X | X |
| [50] | 2021 | AKI in patients who received organ donation in ICU | Not clearly stated KDIGO with UO |
Not clearly stated | RF | 0.85 | X | X | X | X |
| [17] | 2021 | Survival of AKI patients in ICU without RRT | Not clearly stated | KNN imputer was used | LSTM | 0.73 | X | O | X | X |
| [24] | 2022 | AKI in septic patients in ICU | Estimated value KDIGO with UO |
After excluding features with more than 20% missing values, multiple imputation was used | XGB | 0.82 | X | O | X | X |
| [52] | 2022 | AKI in acute cerebrovascular disease patients in ICU | Minimum value after ICU admission KDIGO without UO |
Filled with 0 | XGB | 0.88 | X | O | X | O |
| [84] | 2022 | AKI after partial nephrectomy | Measured value before surgery RIFLE and AKIN without UO |
Not clearly stated | RF | 0.75 | X | X | X | X |
| [58] | 2023 | AKI recovery at discharge in stage 3 AKI patients admitted to the ICU | Most recent value within 3 months before admission or estimated value KDIGO without UO |
After excluding features with more than 10%, the remaining were filled with mean and mode | LASSO | 0.71 | X | X | X | X |
| [27] | 2022 | Recovery of AKI at discharge in all patients with AKI | Most recent value within 7 days before admission or average within 90 days before admission KDIGO without UO |
median considering AKI stage or KNN imputer was used | XGB | 0.81 | X | X | X | X |
| [26] | 2022 | Occurrence of AKI after immune checkpoint inhibitor administration in cancer patients | Most recent value within 3 months before the first ICPi KDIGO without UO |
After excluding features with more than 20% missing values, MissForest was used | SVM | 0.82 | X | O | O | O |
| [56] | 2023 | AKI after brain surgery in ICU | Minimum value within 6 months before admission or estimated value KDIGO without UO |
After excluding features with more than 20% missing values, multiple imputation was used | Ensemble | 0.85 | X | X | X | X |
| [28] | 2023 | Death, RRT, or reduction of eGFR by more than 50% in patients with AKI within 3 days in ICU | Measured value on the day closest to admission within 365 days before admission or estimated value KDIGO without UO |
Replaced with mean value | RF | 0.78 | O | X | X | O |
Cr, creatinine; AKI, acute kidney injury; AUROC, area under the receiver operating characteristic curve; RRT, renal replacement therapy; KDIGO, Kidney Disease: Improving Global Outcomes; UO, urine output; GBM, gradient boosting machine; SCr, serum creatinine; ICU, intensive care unit; MICE, multiple imputation by chained equations; MLP, multilayer perceptron; XGB, extreme gradient boosting; RNN, recurrent neural network; BN, bayesian network; CNN, convolutional neural network; RF, random forest; KNN, K-nearest neighbors; LSTM, long short-term memory; RIFLE, risk, injury, failure, loss of kidney function, and end-stage kidney disease; AKIN, acute kidney injury network; LASSO, least absolute shrinkage and selection operator; SVM, support vector machine; ICPi, immune checkpoint inhibitor; eGFR, estimated glomerular filtration rate. “Estimated value” refers to the estimation of parameters, such as eGFR, using methods like modification of diet in renal disease when baseline is unavailable. “△” signifies insufficient information for assessment. “Ensemble” refers to the combination of individual models through methods like voting, each developed separately.
FUTURE DIRECTIONS FOR AKI AI RESEARCH
Consensus labeling standards and evaluation data
Clinical guidelines for AKI diagnosis aside, it is clear that consensus AKI labeling standards are needed for machine learning models that use retrospective data. A scientific approach and verification of clinical effectiveness are essential when the numbers of serum creatinine measurements over time vary. The use of different standards renders it difficult to compare and evaluate models. Consistent, rational labeling guidelines are essential. Ideally, a multinational, multi-institutional dataset, labeled using agreed standards, would be employed for performance evaluation of all models. Large medical databases such as eICU and MIMIC have accelerated the development of medical AI [85–88].
Multicenter studies and use of the latest technologies
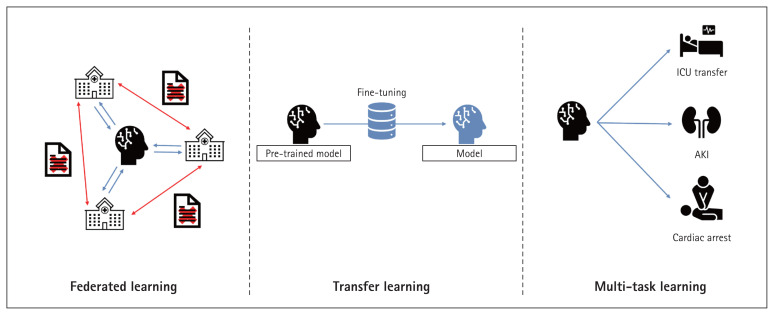
High-quality data are essential. Sparse data do not well-train models and may introduce bias toward specific groups or cause data overfitting [89,90]. When developing medical AI, consideration of patients with diverse characteristics, treated in various institutions, enhances model training [91]. However, medical data are difficult to obtain and use because of legal issues and the need for quality assurance [78,92]. Thus, federated and transfer learning are being actively researched. During federated learning, models or weights (but not data) are shared among institutions for model training. Transfer learning takes a pre-trained model and develops a new model based on that model. Both methods largely lack data security issues and effectively train models even when the data are limited [93–96]. This ensures that the cohorts used for model development are diverse. Meta-learning can overcome problems associated with among-cohort differences during model development [97], and quantifies such differences and their impacts [18,98].
Currently, most research is focused on early AKI prediction. Only a few studies have used machine learning to predict AKI prognosis [99]. This may require rather long observation periods and/or extensive serum creatinine records. No consensus recovery criteria are available; it is difficult to predict AKI prognosis. Efforts to overcome these limitations include increasing the data volume via transfer and/or federated learning, and the use of multitask learning models [100]. It is important to monitor advances in machine learning continuously and apply them in the AKI research field. Figure 6 shows the latest AI technologies.
Figure 6.
The latest artificial intelligence approaches. ICU, intensive care unit; AKI, acute kidney injury.
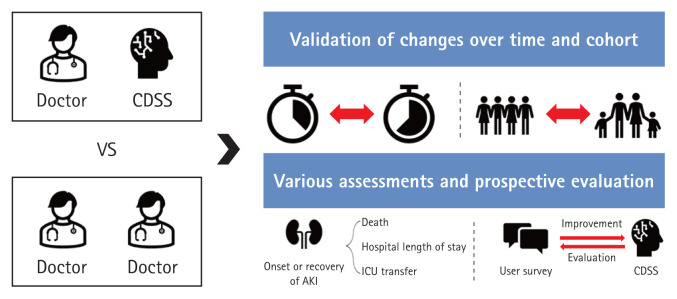
Model evaluation methods employing real users
Medical AI is meaningful only when it helps physicians and patients. Both time-based performance and external validations should be considered. All models should be thoroughly reviewed in terms of real-world effectiveness when predicting primary outcomes such as AKI occurrence or recovery, death, the hospital stay, and a need for ICU transfer. Comparing models to physicians who seek to solve the same tasks could be a useful alternative; this is frequently employed in the medical imaging AI field [101,102]. Rank et al. [60] found that AKI models outperformed physicians in terms of predicting AKI onset. However, tabular data are less informative than the information used by physicians [60]. Therefore, rather than comparing models with physicians, comparisons of physicians who do and do not use models might be better. Research on AI-based clinical decision support systems is ongoing.
Henry et al. [61] developed an AI model predicting sepsis onset, invited clinicians to use it, and conducted semi-structured interviews with 20 clinicians 6 months later. Prospective model evaluation after model introduction may be effective. Models should be continuously improved via user feedback and the results of prospective evaluations. The use of many features renders applications difficult; too much data are required [89,103]. However, if too few features are employed, a physician might have few options even if the model is accurate. Previous studies employed 15 to 1,000 features [18,104]. Useful features should be continuously sought based on model performance and user feedback. Figure 7 shows advanced model evaluation methods.
Figure 7.
Several advanced models used for patient evaluation. CDSS, clinical decision support system; AKI, acute kidney injury; ICU, intensive care unit.
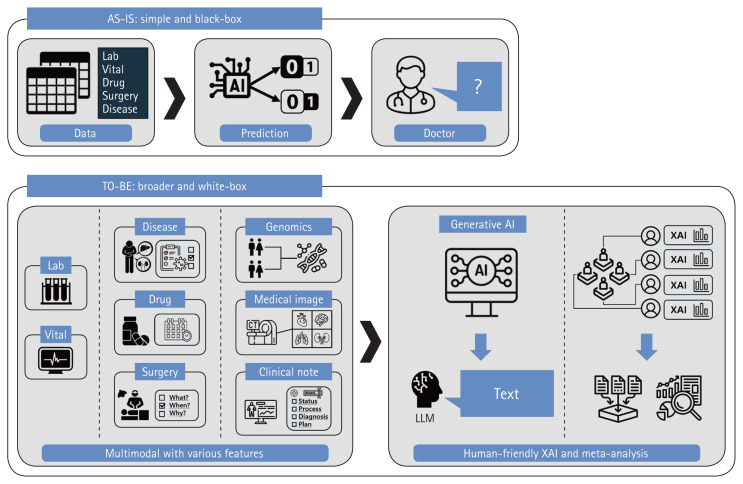
Explainable AI and causal inferences
Even if model performance is excellent, AI complexity (the ‘black box problem’) is a major obstacle to clinical applications [105]. The inner workings of a model are opaque; it is impossible to trace decision-making. In a ‘white box’ model, all operations are completely transparent, thus all steps from inputs to outputs. Many studies have sought to make black boxes white [106]. The advances range from an emphasis on simple feature importance to Local Interpretable Model-agnostic Explanations, SHapley Additive exPlanations, Partial Dependence Plots, Individual Conditional Expectation Plots, and combinations thereof [107]. However, these methods do not show how features cause certain decisions to be made. Proof of causality, as opposed to proof of mere correlations or trends, is extremely challenging. It is crucial to derive correlations between various patient features and AKI [108,109]. Meta-analyses are aimed at strong associations between certain features and AKI occurrence or recovery, enhancing confidence in models that use such features [110]. AI researchers currently seek to create an Artificial General Intelligence that thinks like humans. A new AI should consider various modalities, not only fragmented information [111]. Although model interpretation may be difficult, multimodal technologies that combine tabular data with images or natural language, and generative AI technologies, could serve as alternatives to black boxes and prove difficult causalities [112]. Explanations of models using intuitive and human-friendly methods would greatly benefit users.
Simple laboratory parameters or vital signs can aid diagnoses and, thus, appropriate interventions by physicians [113]. For example, if AKI patients are identified early, physicians can adjust drug prescriptions or surgical schedules accordingly. This alleviates the burden on medical personnel who manage AKI and mitigates the differences between regions with good and limited medical infrastructures. Physicians must thoroughly review features that could enable more proactive interventions, such as diseases apparent on admission; the indications for the planned treatments/surgeries; and the medication types, quantities, and dosing schedules [114,115]. Consideration of such features during model development and interpretation would not only facilitate early diagnosis and intervention but also the development of an AI that truly supports clinical decision-making, thus beyond simple early detection (Fig. 8).
Figure 8.
How to develop a reliable and clinically meaningful model. AI, artificial intelligence.
CONCLUSION
AI will greatly advance the practice of medicine. Many medical AI studies are in progress. In the AKI context, many works have reported high-level AI performance, confirming the potential of machine learning in terms of early AKI diagnosis and prediction of prognosis. However, medical AI is patient-intrusive; care is required. Many obstacles remain. It is time to move out of the computer laboratory into the clinic.
Footnotes
CRedit authorship contributiones
Inyong Jeong: resources, investigation, data curation, writing - original draft; Nam-Jun Cho: resources, investigation, data curation, writing - original draft; Se-Jin Ahn: data curation, visualization; Hwamin Lee: conceptualization, methodology, investigation, data curation, writing - review & editing, funding acquisition; Hyo-Wook Gil: conceptualization, methodology, resources, investigation, data curation, writing - original draft, writing - review & editing, funding acquisition
Conflicts of interest
The authors disclose no conflicts.
Funding
This study was supported by the Soonchunhyang University Research Fund.
Supplementary Information
REFERENCES
- 1.Abebe A, Kumela K, Belay M, Kebede B, Wobie Y. Mortality and predictors of acute kidney injury in adults: a hospital-based prospective observational study. Sci Rep. 2021;11:15672. doi: 10.1038/s41598-021-94946-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Rewa O, Bagshaw SM. Acute kidney injury-epidemiology, outcomes and economics. Nat Rev Nephrol. 2014;10:193–207. doi: 10.1038/nrneph.2013.282. [DOI] [PubMed] [Google Scholar]
- 3.Jung HY, Lee JH, Park YJ, et al. Duration of anuria predicts recovery of renal function after acute kidney injury requiring continuous renal replacement therapy. Korean J Intern Med. 2016;31:930–937. doi: 10.3904/kjim.2014.290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kellum JA, Sileanu FE, Murugan R, Lucko N, Shaw AD, Clermont G. Classifying AKI by urine output versus serum creatinine level. J Am Soc Nephrol. 2015;26:2231–2238. doi: 10.1681/ASN.2014070724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Allen JC, Gardner DS, Skinner H, Harvey D, Sharman A, Devonald MAJ. Definition of hourly urine output influences reported incidence and staging of acute kidney injury. BMC Nephrol. 2020;21:19. doi: 10.1186/s12882-019-1678-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kang C, Han SH, Park JS, Choi DE. Risk factors for post-contrast acute kidney injury in patients sequentially administered iodine- and gadolinium-based contrast media on the same visit to the emergency department: a retrospective study. Kidney Res Clin Pract. 2023;42:358–369. doi: 10.23876/j.krcp.22.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lee K, Jang HR. Role of T cells in ischemic acute kidney injury and repair. Korean J Intern Med. 2022;37:534–550. doi: 10.3904/kjim.2021.526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Patschan D, Erfurt S, Oess S, et al. Biomarker-based prediction of survival and recovery of kidney function in acute kidney injury. Kidney Blood Press Res. 2023;48:124–134. doi: 10.1159/000528633. [DOI] [PubMed] [Google Scholar]
- 9.Jung HH. Albuminuria, estimated glomerular filtration rate, and traditional predictors for composite cardiovascular and kidney outcome: a population-based cohort study in Korea. Kidney Res Clin Pract. 2022;41:567–579. doi: 10.23876/j.krcp.22.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kim Y, Kang E, Chae DW, et al. Insufficient early renal recovery and progression to subsequent chronic kidney disease in living kidney donors. Korean J Intern Med. 2022;37:1021–1030. doi: 10.3904/kjim.2021.308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Wen Y, Parikh CR. Current concepts and advances in biomarkers of acute kidney injury. Crit Rev Clin Lab Sci. 2021;58:354–368. doi: 10.1080/10408363.2021.1879000. [DOI] [PubMed] [Google Scholar]
- 12.Kellum JA, Bihorac A. Artificial intelligence to predict AKI: is it a breakthrough? Nat Rev Nephrol. 2019;15:663–664. doi: 10.1038/s41581-019-0203-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Yoo JJ, Park MY, Kim SG. Acute kidney injury in patients with acute-on-chronic liver failure: clinical significance and management. Kidney Res Clin Pract. 2023;42:286–297. doi: 10.23876/j.krcp.22.264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Gheisari M, Ebrahimzadeh F, Rahimi M, et al. Deep learning: applications, architectures, models, tools, and frameworks: a comprehensive survey. CAAI Trans Intell Technol. 2023;8:581–606. [Google Scholar]
- 15.Koyner JL, Carey KA, Edelson DP, Churpek MM. The development of a machine learning inpatient acute kidney injury prediction model. Crit Care Med. 2018;46:1070–1077. doi: 10.1097/CCM.0000000000003123. [DOI] [PubMed] [Google Scholar]
- 16.Churpek MM, Carey KA, Edelson DP, et al. Internal and external validation of a machine learning risk score for acute kidney injury. JAMA Netw Open. 2020;3:e2012892. doi: 10.1001/jamanetworkopen.2020.12892. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Pattharanitima P, Vaid A, Jaladanki SK, et al. Comparison of approaches for prediction of renal replacement therapy-free survival in patients with acute kidney injury. Blood Purif. 2021;50:621–627. doi: 10.1159/000513700. [DOI] [PubMed] [Google Scholar]
- 18.Song X, Yu ASL, Kellum JA, et al. Cross-site transportability of an explainable artificial intelligence model for acute kidney injury prediction. Nat Commun. 2020;11:5668. doi: 10.1038/s41467-020-19551-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Wirth FN, Meurers T, Johns M, Prasser F. Privacy-preserving data sharing infrastructures for medical research: systematization and comparison. BMC Med Inform Decis Mak. 2021;21:242. doi: 10.1186/s12911-021-01602-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Johnson AE, Pollard TJ, Shen L, et al. MIMIC-III, a freely accessible critical care database. Sci Data. 2016;3:160035. doi: 10.1038/sdata.2016.35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Johnson A, Bulgarelli L, Pollard T, Horng S, Celi LA, Mark R. MIMIC-IV [Internet] PhysioNet. 2021. [cited 2023 Dec 22]. Available from: https://physionet.org/content/mimiciv/1.0/
- 22.Pollard TJ, Johnson AEW, Raffa JD, Celi LA, Mark RG, Badawi O. The eICU Collaborative Research Database, a freely available multi-center database for critical care research. Sci Data. 2018;5:180178. doi: 10.1038/sdata.2018.178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Wei S, Zhang Y, Dong H, et al. Machine learning-based prediction model of acute kidney injury in patients with acute respiratory distress syndrome. BMC Pulm Med. 2023;23:370. doi: 10.1186/s12890-023-02663-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Yue S, Li S, Huang X, et al. Machine learning for the prediction of acute kidney injury in patients with sepsis. J Transl Med. 2022;20:215. doi: 10.1186/s12967-022-03364-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ko S, Jo C, Chang CB, et al. A web-based machine-learning algorithm predicting postoperative acute kidney injury after total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc. 2022;30:545–554. doi: 10.1007/s00167-020-06258-0. [DOI] [PubMed] [Google Scholar]
- 26.Yu X, Wu R, Ji Y, Huang M, Feng Z. Identifying patients at risk of acute kidney injury among patients receiving immune checkpoint inhibitors: a machine learning approach. Diagnostics (Basel) 2022;12:3157. doi: 10.3390/diagnostics12123157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Liu CL, Tain YL, Lin YC, Hsu CN. Prediction and Clinically important factors of acute kidney injury non-recovery. Front Med (Lausanne) 2022;8:789874. doi: 10.3389/fmed.2021.789874. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Neyra JA, Ortiz-Soriano V, Liu LJ, et al. Prediction of mortality and major adverse kidney events in critically ill patients with acute kidney injury. Am J Kidney Dis. 2023;81:36–47. doi: 10.1053/j.ajkd.2022.06.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Jiang X, Hu Y, Guo S, Du C, Cheng X. Prediction of persistent acute kidney injury in postoperative intensive care unit patients using integrated machine learning: a retrospective cohort study. Sci Rep. 2022;12:17134. doi: 10.1038/s41598-022-21428-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Li X, Wu R, Zhao W, et al. Machine learning algorithm to predict mortality in critically ill patients with sepsis-associated acute kidney injury. Sci Rep. 2023;13:5223. doi: 10.1038/s41598-023-32160-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Alfieri F, Ancona A, Tripepi G, et al. A deep-learning model to continuously predict severe acute kidney injury based on urine output changes in critically ill patients. J Nephrol. 2021;34:1875–1886. doi: 10.1007/s40620-021-01046-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Kim K, Yang H, Yi J, et al. Real-time clinical decision support based on recurrent neural networks for in-hospital acute kidney injury: external validation and model interpretation. J Med Internet Res. 2021;23:e24120. doi: 10.2196/24120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Li Y, Xu J, Wang Y, et al. A novel machine learning algorithm, Bayesian networks model, to predict the high-risk patients with cardiac surgery-associated acute kidney injury. Clin Cardiol. 2020;43:752–761. doi: 10.1002/clc.23377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Khwaja A. KDIGO clinical practice guidelines for acute kidney injury. Nephron Clin Pract. 2012;120:c179–c184. doi: 10.1159/000339789. [DOI] [PubMed] [Google Scholar]
- 35.Chawla LS, Bellomo R, Bihorac A, et al. Acute kidney disease and renal recovery: consensus report of the Acute Disease Quality Initiative (ADQI) 16 Workgroup. Nat Rev Nephrol. 2017;13:241–257. doi: 10.1038/nrneph.2017.2. [DOI] [PubMed] [Google Scholar]
- 36.Kung CW, Chou YH. Acute kidney disease: an overview of the epidemiology, pathophysiology, and management. Kidney Res Clin Pract. 2023;42:686–699. doi: 10.23876/j.krcp.23.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Lameire NH, Levin A, Kellum JA, et al. Harmonizing acute and chronic kidney disease definition and classification: report of a Kidney Disease: Improving Global Outcomes (KDIGO) Consensus Conference. Kidney Int. 2021;100:516–526. doi: 10.1016/j.kint.2021.06.028. [DOI] [PubMed] [Google Scholar]
- 38.Kim H. The new race-free equations for estimating glomerular filtration rate: should they be adopted for Asians? Kidney Res Clin Pract. 2023;42:670–671. doi: 10.23876/j.krcp.23.111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Lee YJ, Park YS, Park SJ, Jhang WK. Estimating baseline creatinine values to define acute kidney injury in critically ill pediatric patients. Kidney Res Clin Pract. 2022;41:322–331. doi: 10.23876/j.krcp.21.120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Mohamadlou H, Lynn-Palevsky A, Barton C, et al. Prediction of acute kidney injury with a machine learning algorithm using electronic health record data. Can J Kidney Health Dis. 2018;5:2054358118776326. doi: 10.1177/2054358118776326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Zhou Y, Feng J, Mei S, et al. Machine learning models for predicting acute kidney injury in patients with sepsis-associated acute respiratory distress syndrome. Shock. 2023;59:352–359. doi: 10.1097/SHK.0000000000002065. [DOI] [PubMed] [Google Scholar]
- 42.Jiang J, Liu X, Cheng Z, Liu Q, Xing W. Interpretable machine learning models for early prediction of acute kidney injury after cardiac surgery. BMC Nephrol. 2023;24:326. doi: 10.1186/s12882-023-03324-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Zhang H, Wang AY, Wu S, et al. Artificial intelligence for the prediction of acute kidney injury during the perioperative period: systematic review and Meta-analysis of diagnostic test accuracy. BMC Nephrol. 2022;23:405. doi: 10.1186/s12882-022-03025-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Kamel Rahimi A, Ghadimi M, van der Vegt AH, et al. Machine learning clinical prediction models for acute kidney injury: the impact of baseline creatinine on prediction efficacy. BMC Med Inform Decis Mak. 2023;23:207. doi: 10.1186/s12911-023-02306-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Li Y, Yao L, Mao C, Srivastava A, Jiang X, Luo Y. Early prediction of acute kidney injury in critical care setting using clinical notes. Proceedings (IEEE Int Conf Bioinformatics Biomed) 2018;2018:683–686. doi: 10.1109/bibm.2018.8621574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Zimmerman LP, Reyfman PA, Smith ADR, et al. Early prediction of acute kidney injury following ICU admission using a multivariate panel of physiological measurements. BMC Med Inform Decis Mak. 2019;19(Suppl 1):16. doi: 10.1186/s12911-019-0733-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Sato N, Uchino E, Kojima R, Hiragi S, Yanagita M, Okuno Y. Prediction and visualization of acute kidney injury in intensive care unit using one-dimensional convolutional neural networks based on routinely collected data. Comput Methods Programs Biomed. 2021;206:106129. doi: 10.1016/j.cmpb.2021.106129. [DOI] [PubMed] [Google Scholar]
- 48.Le S, Allen A, Calvert J, et al. Convolutional Neural network model for intensive care unit acute kidney injury prediction. Kidney Int Rep. 2021;6:1289–1298. doi: 10.1016/j.ekir.2021.02.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Zheng L, Lin Y, Fang K, Wu J, Zheng M. Derivation and validation of a risk score to predict acute kidney injury in critically ill cirrhotic patients. Hepatol Res. 2023;53:701–712. doi: 10.1111/hepr.13907. [DOI] [PubMed] [Google Scholar]
- 50.He ZL, Zhou JB, Liu ZK, et al. Application of machine learning models for predicting acute kidney injury following donation after cardiac death liver transplantation. Hepatobiliary Pancreat Dis Int. 2021;20:222–231. doi: 10.1016/j.hbpd.2021.02.001. [DOI] [PubMed] [Google Scholar]
- 51.Dong JF, Xue Q, Chen T, et al. Machine learning approach to predict acute kidney injury after liver surgery. World J Clin Cases. 2021;9:11255–11264. doi: 10.12998/wjcc.v9.i36.11255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Zhang X, Chen S, Lai K, Chen Z, Wan J, Xu Y. Machine learning for the prediction of acute kidney injury in critical care patients with acute cerebrovascular disease. Ren Fail. 2022;44:43–53. doi: 10.1080/0886022X.2022.2036619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Rice ML, Barreto EF, Rule AD, et al. Development and validation of a model to predict acute kidney injury following high-dose methotrexate in patients with lymphoma. Pharmacotherapy. 2024;44:4–12. doi: 10.1002/phar.2889. [DOI] [PubMed] [Google Scholar]
- 54.Ma Z, Liu W, Deng F, et al. An early warning model to predict acute kidney injury in sepsis patients with prior hypertension. Heliyon. 2024;10:e24227. doi: 10.1016/j.heliyon.2024.e24227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Zulu C, Mwaba C, Wa Somwe S. The renal angina index accurately predicts low risk of developing severe acute kidney injury among children admitted to a low-resource pediatric intensive care unit. Ren Fail. 2023;45:2252095. doi: 10.1080/0886022X.2023.2252095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Wu M, Jiang X, Du K, Xu Y, Zhang W. Ensemble machine learning algorithm for predicting acute kidney injury in patients admitted to the neurointensive care unit following brain surgery. Sci Rep. 2023;13:6705. doi: 10.1038/s41598-023-33930-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Chen Q, Zhang Y, Zhang M, Li Z, Liu J. Application of machine learning algorithms to predict acute kidney injury in elderly orthopedic postoperative patients. Clin Interv Aging. 2022;17:317–330. doi: 10.2147/CIA.S349978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Huang CY, Güiza F, De Vlieger G, et al. Development and validation of clinical prediction models for acute kidney injury recovery at hospital discharge in critically ill adults. J Clin Monit Comput. 2023;37:113–125. doi: 10.1007/s10877-022-00865-7. [DOI] [PubMed] [Google Scholar]
- 59.Sun S, Annadi RR, Chaudhri I, et al. Short- and long-term recovery after moderate/severe AKI in patients with and without COVID-19. Kidney360. 2021;3:242–257. doi: 10.34067/KID.0005342021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Rank N, Pfahringer B, Kempfert J, et al. Deep-learning-based real-time prediction of acute kidney injury outperforms human predictive performance. NPJ Digit Med. 2020;3:139. doi: 10.1038/s41746-020-00346-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Henry KE, Kornfield R, Sridharan A, et al. Human-machine teaming is key to AI adoption: clinicians’ experiences with a deployed machine learning system. NPJ Digit Med. 2022;5:97. doi: 10.1038/s41746-022-00597-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Vinisha FA, Sujihelen L. Study on missing values and outlier detection in concurrence with data quality enhancement for efficient data processing. Proceedings of the 2022, 4th International Conference on Smart Systems and Inventive Technology (ICSSIT); 2022 Jan 20–22; Tirunelveli: IEEE; 2022. pp. 1600–1607. [Google Scholar]
- 63.Hoogland J, van Barreveld M, Debray TPA, et al. Handling missing predictor values when validating and applying a prediction model to new patients. Stat Med. 2020;39:3591–3607. doi: 10.1002/sim.8682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Shawwa K, Ghosh E, Lanius S, Schwager E, Eshelman L, Kashani KB. Predicting acute kidney injury in critically ill patients using comorbid conditions utilizing machine learning. Clin Kidney J. 2020;14:1428–1435. doi: 10.1093/ckj/sfaa145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Yang J, Peng H, Luo Y, Zhu T, Xie L. Explainable ensemble machine learning model for prediction of 28–day mortality risk in patients with sepsis-associated acute kidney injury. Front Med (Lausanne) 2023;10:1165129. doi: 10.3389/fmed.2023.1165129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Peng C, Yang F, Li L, et al. A machine learning approach for the prediction of severe acute kidney injury following traumatic brain injury. Neurocrit Care. 2023;38:335–344. doi: 10.1007/s12028-022-01606-z. [DOI] [PubMed] [Google Scholar]
- 67.Luo XQ, Yan P, Zhang NY, et al. Machine learning for early discrimination between transient and persistent acute kidney injury in critically ill patients with sepsis. Sci Rep. 2021;11:20269. doi: 10.1038/s41598-021-99840-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Perez-Lebel A, Varoquaux G, Le Morvan M, Josse J, Poline JB. Benchmarking missing-values approaches for predictive models on health databases. Gigascience. 2022;11:giac013. doi: 10.1093/gigascience/giac013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Liu Y, Qin S, Yepes AJ, Shao W, Zhang Z, Salim FD. Integrated convolutional and recurrent neural networks for health risk prediction using patient journey data with many missing values. Proceedings of the 2022 IEEE International Conference on Bioinformatics and Biomedicine (BIBM); 2022 Dec 6–8; Las Vegas (NV): IEEE; pp. 1658–1663. [Google Scholar]
- 70.Zhao X, Lu Y, Li S, et al. Predicting renal function recovery and short-term reversibility among acute kidney injury patients in the ICU: comparison of machine learning methods and conventional regression. Ren Fail. 2022;44:1326–1337. doi: 10.1080/0886022X.2022.2107542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Yang Y, Xiao W, Liu X, Zhang Y, Jin X, Li X. Machine learning-assisted ensemble analysis for the prediction of acute pancreatitis with acute kidney injury. Int J Gen Med. 2022;15:5061–5072. doi: 10.2147/IJGM.S361330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Che Z, Purushotham S, Cho K, Sontag D, Liu Y. Recurrent neural networks for multivariate time series with missing values. Sci Rep. 2018;8:6085. doi: 10.1038/s41598-018-24271-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Nijman SWJ, Hoogland J, Groenhof TKJ, et al. Real-time imputation of missing predictor values in clinical practice. Eur Heart J Digit Health. 2020;2:154–164. doi: 10.1093/ehjdh/ztaa016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Nijman SWJ, Groenhof TKJ, Hoogland J, et al. Real-time imputation of missing predictor values improved the application of prediction models in daily practice. J Clin Epidemiol. 2021;134:22–34. doi: 10.1016/j.jclinepi.2021.01.003. [DOI] [PubMed] [Google Scholar]
- 75.Montesinos López OA, Montesinos López A, Crossa J. Overfitting, model tuning, and evaluation of prediction performance. In: Montesinos López OA, Montesinos López A, Crossa J, editors. Multivariate statistical machine learning methods for genomic prediction. Cham: Springer; 2022. pp. 109–139. [PubMed] [Google Scholar]
- 76.Ying X. An overview of overfitting and its solutions. J Phys Conf Ser. 2019;1168:022022. [Google Scholar]
- 77.Minvielle E, Fourcade A, Ricketts T, Waelli M. Current developments in delivering customized care: a scoping review. BMC Health Serv Res. 2021;21:575. doi: 10.1186/s12913-021-06576-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Varoquaux G, Cheplygina V. Machine learning for medical imaging: methodological failures and recommendations for the future. NPJ Digit Med. 2022;5:48. doi: 10.1038/s41746-022-00592-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Nadim MK, Forni LG, Mehta RL, et al. COVID-19-associated acute kidney injury: consensus report of the 25th Acute Disease Quality Initiative (ADQI) Workgroup. Nat Rev Nephrol. 2020;16:747–764. doi: 10.1038/s41581-020-00356-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Bravata DM, Myers LJ, Perkins AJ, et al. Heterogeneity in COVID-19 patient volume, characteristics and outcomes across US Department of Veterans Affairs facilities: an observational cohort study. BMJ Open. 2021;11:e044646. doi: 10.1136/bmjopen-2020-044646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Gao X, Ninan J, Bohman JK, et al. Extracorporeal membrane oxygenation and acute kidney injury: a single-center retrospective cohort. Sci Rep. 2023;13:15112. doi: 10.1038/s41598-023-42325-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Zamirpour S, Hubbard AE, Feng J, Butte AJ, Pirracchio R, Bishara A. Development of a machine learning model of postoperative acute kidney injury using non-invasive time-sensitive intraoperative predictors. Bioengineering (Basel) 2023;10:932. doi: 10.3390/bioengineering10080932. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Tomašev N, Glorot X, Rae JW, et al. A clinically applicable approach to continuous prediction of future acute kidney injury. Nature. 2019;572:116–119. doi: 10.1038/s41586-019-1390-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Lazebnik T, Bahouth Z, Bunimovich-Mendrazitsky S, Halachmi S. Predicting acute kidney injury following open partial nephrectomy treatment using SAT-pruned explainable machine learning model. BMC Med Inform Decis Mak. 2022;22:133. doi: 10.1186/s12911-022-01877-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Tschandl P, Rosendahl C, Kittler H. The HAM10000 dataset, a large collection of multi-source dermatoscopic images of common pigmented skin lesions. Sci Data. 2018;5:180161. doi: 10.1038/sdata.2018.161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Wagner P, Strodthoff N, Bousseljot RD, et al. PTB-XL, a large publicly available electrocardiography dataset. Sci Data. 2020;7:154. doi: 10.1038/s41597-020-0495-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Yang J, Shi R, Wei D, et al. MedMNIST v2 - a large-scale lightweight benchmark for 2D and 3D biomedical image classification. Sci Data. 2023;10:41. doi: 10.1038/s41597-022-01721-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Johnson AEW, Pollard TJ, Berkowitz SJ, et al. MIMIC-CXR, a de-identified publicly available database of chest radiographs with free-text reports. Sci Data. 2019;6:317. doi: 10.1038/s41597-019-0322-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Jain A, Patel H, Nagalapatti L, et al. Overview and importance of data quality for machine learning tasks. Proceedings of the 26th ACM SIGKDD International Conference on Knowledge Discovery & Data Mining; 2020 Jul 6–10; New York (NY): Association for Computing Machinery; pp. 3561–3562. [Google Scholar]
- 90.Alzubaidi L, Bai J, Al-Sabaawi A, et al. A survey on deep learning tools dealing with data scarcity: definitions, challenges, solutions, tips, and applications. J Big Data. 2023;10:46. [Google Scholar]
- 91.Lee SW, Lee HC, Suh J, et al. Multi-center validation of machine learning model for preoperative prediction of postoperative mortality. NPJ Digit Med. 2022;5:91. doi: 10.1038/s41746-022-00625-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Rieke N, Hancox J, Li W, et al. The future of digital health with federated learning. NPJ Digit Med. 2020;3:119. doi: 10.1038/s41746-020-00323-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Li L, Fan Y, Tse M, Lin KY. A review of applications in federated learning. Comput Ind Eng. 2020;149:106854. [Google Scholar]
- 94.Xu J, Glicksberg BS, Su C, Walker P, Bian J, Wang F. Federated learning for healthcare informatics. J Healthc Inform Res. 2021;5:1–19. doi: 10.1007/s41666-020-00082-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Jeong I, Kim Y, Cho NJ, Gil HW, Lee H. A novel method for medical predictive models in small data using out-of-distribution data and transfer learning. Mathematics. 2024;12:237. [Google Scholar]
- 96.Alzubaidi L, Al-Amidie M, Al-Asadi A, et al. Novel transfer learning approach for medical imaging with limited labeled data. Cancers (Basel) 2021;13:1590. doi: 10.3390/cancers13071590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Golriz Khatami S, Salimi Y, Hofmann-Apitius M, et al. Comparison and aggregation of event sequences across ten cohorts to describe the consensus biomarker evolution in Alzheimer’s disease. Alzheimers Res Ther. 2022;14:55. doi: 10.1186/s13195-022-01001-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Zhao S, Sinha A, He Y, Perreault A, Song J, Ermon S. Comparing distributions by measuring differences that affect decision making. Proceedings of the International Conference on Learning Representations 2022; 2022 Apr 25–29; ICLR; 2022. [Google Scholar]
- 99.Pickkers P, Darmon M, Hoste E, et al. Acute kidney injury in the critically ill: an updated review on pathophysiology and management. Intensive Care Med. 2021;47:835–850. doi: 10.1007/s00134-021-06454-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Zhang Y, Yang Q. A survey on multi-task learning. IEEE Trans Knowl Data Eng. 2022;34:5586–5609. doi: 10.1109/tkde.2020.3045924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Deperlioglu O, Kose U, Gupta D, Khanna A, Giampaolo F, Fortino G. Explainable framework for Glaucoma diagnosis by image processing and convolutional neural network synergy: analysis with doctor evaluation. Future Gener Comput Syst. 2022;129:152–169. [Google Scholar]
- 102.Song W, Li S, Liu J, Qin H, Zhang B, Zhang S, Hao A. Multitask cascade convolution neural networks for automatic thyroid nodule detection and recognition. IEEE J Biomed Health Inform. 2019;23:1215–1224. doi: 10.1109/JBHI.2018.2852718. [DOI] [PubMed] [Google Scholar]
- 103.Xu P, Ji X, Li M, Lu W. Small data machine learning in materials science. npj Comput Mater. 2023;9:42. [Google Scholar]
- 104.Hu Y, Liu K, Ho K, et al. A simpler machine learning model for acute kidney injury risk stratification in hospitalized patients. J Clin Med. 2022;11:5688. doi: 10.3390/jcm11195688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Chan B. Black-box assisted medical decisions: AI power vs. ethical physician care. Med Health Care Philos. 2023;26:285–292. doi: 10.1007/s11019-023-10153-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Rai A. Explainable AI: from black box to glass box. J Acad Mark Sci. 2020;48:137–141. [Google Scholar]
- 107.Arrieta AB, Díaz-Rodríguez N, Del Ser J, et al. Explainable Artificial Intelligence (XAI): concepts, taxonomies, opportunities and challenges toward responsible AI. Inf Fusion. 2020;58:82–115. [Google Scholar]
- 108.Roy S. Salimi Causal inference in data analysis with applications to fairness and explanations. In: Bertossi L, Xiao G, editors. Reasoning web causality, explanations and declarative knowledge. Cham: Springer; 2023. pp. 105–131. [Google Scholar]
- 109.Nogueira AR, Pugnana A, Ruggieri S, Pedreschi D, Gama J. Methods and tools for causal discovery and causal inference. Wiley Interdiscip Rev Data Min Knowl Discov. 2022;12:e1449. [Google Scholar]
- 110.Shooshtari MM, Salehi M, Khalili H, Asadollahi E, Jamali-Moghadamsiahkali S. Investigating risk factors of AKI in patients with sepsis hospitalized in the intensive care unit. Jundishapur J Chronic Dis Care. 2023;12:e130952. [Google Scholar]
- 111.Bogdanovic Z. Artificial intelligence in federal information processing systems. Am J Comput Sci Inform Technol. 2021;9:99. [Google Scholar]
- 112.Hu J, Zhang Q, Yin H. Augmenting greybox fuzzing with generative AI. arXiv:2306.06782 [Preprint] 2023 doi: 10.48550/arXiv.2306.06782. [cited 2023 Dec 22]. Available from: [DOI] [Google Scholar]
- 113.Bora M, Staboliou E, Alexakou Z, et al. #5020 heterogeneity of hospital aquired acute kidney injury and the importance of early versus late nephrology assessment: a retrospective study of one center. Nephrol Dial Transplant. 2023;38(Supplement 1):gfad063c_5020. [Google Scholar]
- 114.Miller DD. The medical AI insurgency: what physicians must know about data to practice with intelligent machines. npj Digit Med. 2019;2:62. doi: 10.1038/s41746-019-0138-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Juma S, Goldszmidt M. What physicians reason about during admission case review. Adv Health Sci Educ Theory Pract. 2017;22:691–711. doi: 10.1007/s10459-016-9701-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.