Abstract
Leiomyoma of the bladder is an unusual cause of benign smooth muscle tumor, only reported about 250 times in the literature. Imaging studies including computed tomography (CT) and magnetic resonance imaging (MRI) scans are useful in defining the extent and location of the tumor, however, immunohistology samples must be obtained to rule out similar appearing cancerous masses. In this article, we report the case of a 50-year-old male diagnosed with leiomyoma of the bladder that initially presented as dysuria and raised suspicion of a bladder transitional cell carcinoma (TCC). We focus on the utilization of radiological imaging modalities for diagnosis, management, and preoperational planning with pathological findings for an optimized diagnosis.
Keywords: Leiomyoma, Bladder, CT, MRI, Dysuria, Atypical
Introduction
Leiomyomas are benign smooth muscle neoplasms most commonly found along the lining of the uterus, stomach, small bowel, and bladder [1]. Originating from the mesenchymal layer, the pathophysiological emergence of leiomyomas remains unclear. Typically causing obstructive or irritating symptoms, leiomyomas often remain asymptomatic for a long time before presenting as pelvic pain, pressure, and/or difficulty urinating [2,3]. Initial evaluation usually includes cystoscopy followed by ultrasound, magnetic resonance imaging (MRI), and/or computed tomography (CT) imaging. These images are analyzed concurrently with urinalysis and kidney function [4]. In this article, we report on an unusual bladder leiomyoma case in a 50-year-old male. We present CT and MRI imaging, comparing the features of each to the pathological reports of the mass for accurate diagnosis.
Case presentation
A 50-year-old male with a past medical history of hyperlipidemia and Lyme disease presented to an outside healthcare provider with difficulty urinating. There was no history of gross hematuria or other irritative or obstructive symptoms. A cystoscopy was performed at an outside institution revealing an extravesical mass encroaching on the left side of the bladder creating a mass effect. Based on these findings, a CT (Figs. 1A-C) and MRI (Figs. 2A-C) scan of the lower abdomen and pelvis with and without IV contrast were obtained. The CT demonstrated an 8cm x 6.8cm well-circumscribed submucosal mass arising from the left lateral wall of the bladder. On MRI, it measured 7.4cm x 6.6cm. Given the rounded appearance and submucosal location, TCC was considered, however, a benign lesion such as a leiomyoma, albeit at an unusual location, was also a strong differential.
Fig. 1.
CT images of a bladder leiomyoma. (A) Axial noncontrast CT image of the pelvis shows a well-circumscribed soft tissue mass along the left posterior bladder wall (arrow). (B) Axial and (C) coronal delayed phase IV contrast-enhanced CT images show mild enhancement within the bladder mass with smooth contours.
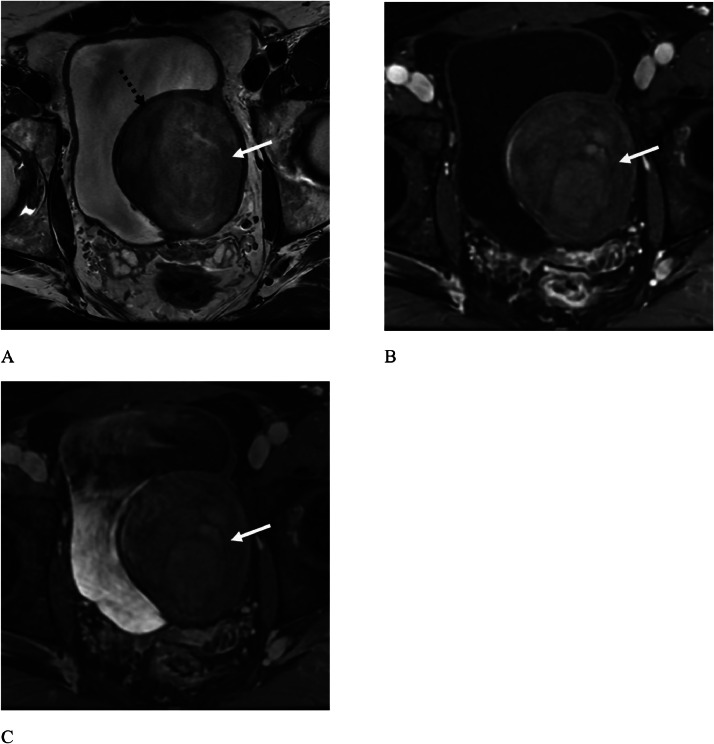
Fig. 2.
MR images of a bladder leiomyoma. (A) Axial T2-weight MR image of the pelvis shows a well-circumscribed mass with heterogeneous T2 signal (arrow). The superior tissue resolution of MR clearly shows its submucosal location, beneath the normal bladder mucosa (dotted black arrow). (B) Axial T1-weighted MR image in the venous phase and (C) delayed phase show mild internal enhancement of the bladder tumor (arrows).
The patient underwent transurethral bladder tumor (TURBT) resection to confirm the pathologic diagnosis. On cystoscopy, no intraluminal bladder tumor was present, however, the left bladder wall was visibly indented by the extraluminal mass. The left bladder wall and tumor were partially resected, confirming the pathology of bladder leiomyoma. Immunohistochemistry reported that the tumor cells were strongly and diffusely positive for desmin and negative for DOG1 and CD117 biomarkers. After a thorough tumor board review, the mass was determined to be amenable for resection and a partial cystectomy is planned.
Discussion
Here, we review this unique case of leiomyoma of the bladder, an extremely rare presentation, accounting for approximately < 0.5% of all bladder tumor cases [4,5], with only 250 cases reported worldwide [6]. Bladder leiomyomas are the most common type of benign soft tissue neoplasms of the bladder, constituting roughly 35% of all cases [7]. A systematic literature review of 90 isolated urinary bladder leiomyoma cases by Silva-Ramos et al. [8] concluded that the mean age of incidence was 45.3 years and 75.6% of patients were women. The most frequently reported symptoms were irritative (50%), followed by obstructive symptoms (24.4%), and the remainder were asymptomatic (26.7%). Predominantly, the leiomyomas presented in the endoluminal space (51.1%), followed by the intramural space (30%), and least often in the extravesical space (16.7%). The etiology of leiomyomas of the bladder largely remains unclear, however, many speculate the occurrence of the tumor is related to abnormal endocrine alterations or chromosomal abnormalities [3,9].
Despite the rarity of this type of neoplasm, its benign character supports an excellent prognosis, so treatment plans generally include complete surgical resection of the mass with the possibility of a partial cystectomy [6,9]. Certain risks are considered when resecting leiomyomas of the bladder including; decreased urine capacity, scarring of the bladder wall, urinary incontinence, and recurrence of mass. Depending on the size and location of mass, the degree of risk fluctuates [10]. In our case, due to its proximity to the left ureter, a left ureter reimplant would likely be needed following the partial cystectomy.
Radiologic imaging is critical for the detection, characterization, and staging of bladder masses. On CT, bladder leiomyomas typically present as solid masses with smooth compression of the bladder lumen. On MRI, bladder leiomyomas typically show intermediate signal on T1 weighted images, hypointense signal on T2 weighted images, and variable enhancement on post contrast images. Cystic degeneration is occasionally seen, with hyperintense signal on T2 weighted images. MRI is superior to CT in delineating the submucosal location compared to CT [11]. CT and MRI features may be helpful in differentiating bladder leiomyoma from paraganglioma, another type of submucosal bladder tumor [12]. CT and MRI also provide important information for surgical planning of bladder tumor resection, including proximity to the ureter and any evidence of systemic disease.
Conclusion
Leiomyoma of the bladder in this 50-year-old male is a rare and unique presentation of benign smooth muscle tumor, accounting for approximately < 0.5% of all bladder masses. Oftentimes suspected as a TCC of the bladder, which also presents as a well-defined appearance on radiological scans, leiomyomas of the bladder are confidently diagnosed using imaging and immunohistology. The prognosis for leiomyomas of the bladder is very optimistic, with a high likelihood of full resection surgically and minimal adverse effects on the bladder.
Patient consent
The patient reported in the manuscript signed the informed consent/authorization for participation in research, which includes the permission to use data collected in future research projects such as the presented case details and images used in this manuscript.
Footnotes
Competing Interests: The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
References
- 1.Xin J, Lai HP, Lin SK, et al. Bladder leiomyoma presenting as dyspareunia: case report and literature review. Medicine (Baltimore) 2016;95(28):e3971. doi: 10.1097/MD.0000000000003971. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Florence AM, Fatehi M. StatPearls. StatPearls Publishing; 2024. Leiomyoma.http://www.ncbi.nlm.nih.gov/books/NBK538273/ [accessed 09.24.24] [PubMed] [Google Scholar]
- 3.Mavridis C, Georgiadis G, Lagoudaki ED, et al. Bladder leiomyoma with synchronous solitary fibrous tumor of the pleura. Case Rep Urol. 2020;2020 doi: 10.1155/2020/3717506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kashkoush J, Park A. Bladder Leiomyoma presenting as urinary retention: a case report. Urol Case Rep. 2022;45 doi: 10.1016/j.eucr.2022.102253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Mendes JE, Ferreira AV, Coelho SA, Gil C. Bladder leiomyoma. Urol Ann. 2017;9(3):275–277. doi: 10.4103/UA.UA_164_16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.He L, Li S, Zheng C, Wang C. Rare symptomatic bladder leiomyoma: case report and literature review. J Int Med Res. 2018;46(4):1678–1684. doi: 10.1177/0300060517752732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Knoll LD, Segura JW, Scheithauer BW. Leiomyoma of the bladder. J Urol. 1986;136(4):906–908. doi: 10.1016/s0022-5347(17)45124-x. [DOI] [PubMed] [Google Scholar]
- 8.Silva-Ramos M, Massó P, Versos R, Soares J, Pimenta A. [Leiomyoma of the bladder. Analysis of a collection of 90 cases] Actas Urol Esp. 2003;27(8):581–586. doi: 10.1016/s0210-4806(03)72979-9. [DOI] [PubMed] [Google Scholar]
- 9.Ortiz M, Henao DE, Cardona Maya W, Ceballos MM. Leiomyoma of the urinary bladder: a case report. Int Braz J Urol. 2013;39(3):432–434. doi: 10.1590/S1677-5538.IBJU.2013.03.18. [DOI] [PubMed] [Google Scholar]
- 10.Cornella JL, Larson TR, Lee RA, Magrina JF, Kammerer-Doak D. Leiomyoma of the female urethra and bladder: report of twenty-three patients and review of the literature. Am J Obstet Gynecol. 1997;176(6):1278–1285. doi: 10.1016/s0002-9378(97)70346-6. [DOI] [PubMed] [Google Scholar]
- 11.Mouli S, Casalino DD, Nikolaidis P. Imaging features of common and uncommon bladder neoplasms. Radiol Clin North Am. 2012;50(2):301–316. doi: 10.1016/j.rcl.2012.02.001. –, vi. [DOI] [PubMed] [Google Scholar]
- 12.Hu X, Wang K, Sun M, Li C, Wang H, Guan J. Quantitative MRI in distinguishing bladder paraganglioma from bladder leiomyoma. Abdom Radiol (NY) 2023;48(3):1051–1061. doi: 10.1007/s00261-023-03812-5. [DOI] [PubMed] [Google Scholar]