Introduction
With the continuous advancement of cancer treatment drugs and equipment, the survival rates and quality of life for patients with cancer have greatly improved. Every year, innovative cancer drugs are introduced, making it possible for patients to receive the most effective cancer treatments. However, according to reported data, >19.3 million new cancer cases were diagnosed in 2020, with ∼10 million deaths related to cancer that year.1 The number of cancer deaths globally has increased by 40% in just the past decade.2 This trend continues, with the latest estimates predicting >35 million new cancer cases by 2050, a 77% increase from 20 million in 2022, with the majority occurring in low- and middle-income countries (LMICs).3 These statistics suggest that, despite advances in cancer treatment globally, the overall health outcomes for patients with cancer may not be fundamentally improved, and access to cancer care remains unequal. Significant disparities exist in cancer prevention, screening, diagnosis, treatment, and palliative care between different countries.
Most people cannot benefit from expensive, innovative cancer drugs
Advanced medical technologies and drugs, such as gene therapy and cellular therapy, are emerging every year, offering the possibility of curing advanced cancers and improving survival rates. However, a critical issue that is often overlooked is the prohibitive cost of these advanced cancer drugs, which limits access to a small segment of the population. The availability of high-quality, affordable cancer drugs remains scarce. The root cause of this strange phenomenon is the domination of commercial companies in drug research. In short, the research of innovative cancer drugs is driven primarily by capital interests rather than patient accessibility. It is undeniable that these innovative drugs represent significant advances in medical technology and have the potential to enhance the quality of life for patients with cancer, especially those who are wealthier. However, the high prices of innovative drugs make them inaccessible to the majority of people with low socioeconomic status. As a result, most patients with cancer in LMICs are unable to access or benefit from these treatments.
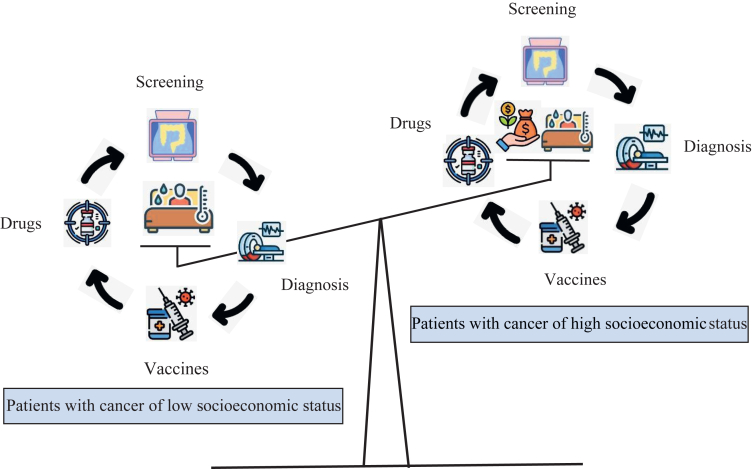
Similarly, in pursuing profits, some hospitals and pharmaceutical companies have introduced advanced examination and treatment instruments, such as Da Vinci robots and proton therapy systems. These technologies come with high price tags, making them neither accessible nor affordable for most patients with cancer. While there is continuous innovation in anticancer drugs and treatment equipment, the quality of life for many patients with cancer has not substantially improved. This ironic and troubling phenomenon warrants serious reflection. Figure 1 shows the inequality among patients with cancer of different socioeconomic status.
Figure 1.
Inequality among patients with cancer of different socioeconomic status.
Pharmaceutical companies dominate the research agenda for new cancer drugs rather than noncommercial research organisations. Driven by profit motives, these companies invest substantial funds in developing new medications, which are then marketed at high prices and protected by patents. Furthermore, the desire for market monopoly pushes pharmaceutical companies to launch new drugs as quickly as possible. These drugs are often designed with short-term endpoints, prioritising statistical significance over clinical relevance. However, as Common Sense Oncology has pointed out, the emphasis on developing new drugs for cancer has come at the expense of investments in surgery and radiotherapy, both of which have the potential to cure many more patients than cancer medicines.4 This issue is not confined to cancer drugs; other high-quality but less profitable medications are also gradually being pushed out of the market.
Inequalities in cancer prevention, screening, diagnosis, and treatment
Pharmaceutical companies in high-income countries benefit from substantial research funding, allowing them to focus primarily on drug development for white populations in developed regions. However, this approach often overlooks regional, ethnic, cultural, and environmental differences, leading to limitations in the generalisability and transferability of new drugs, especially in LMICs. For example, in sub-Saharan Africa, the lack of investment in healthcare systems has prevented the proper evaluation of population-based prostate-specific antigen testing effectiveness.5 This neglect has contributed to low survival rates and a high incidence of advanced prostate cancer among men in this region.
Patients with cancer can benefit much more from cancer prevention, screening, and early diagnosis than from advanced-stage care. However, the current excessive focus on developing new drugs has led to the neglect of crucial areas such as diagnosis and screening. For example, lung cancer, one of the most commonly diagnosed cancers worldwide, had an estimated 2.3 million new cases in 2020. It is also the leading cause of cancer death, accounting for ∼1.8 million deaths in 2020.6 Lung cancer screening primarily relies on computed tomography, a technology not covered by basic health insurance and often unavailable in undeveloped countries due to its high cost and limited medical resources. As a result, lung cancer is usually detected at an advanced stage, leaving patients with only palliative care options, such as expensive targeted drugs, to prolong life. Unfortunately, these drugs remain unaffordable for most families in developing countries. Therefore, investing in the development of high-quality, low-cost cancer detection and diagnosis technologies is more valuable than focusing solely on new targeted drugs.
The high cost of vaccines significantly hinders people’s likelihood of getting vaccinated. Cervical cancer is one of the most common gynaecological cancers, leading to >300 000 deaths in 2022, with 90% of these deaths occurring in LMICs.7,8 The 9-valent human papillomavirus (HPV) vaccine can substantially prevent cervical cancer, with large international randomised controlled trials demonstrating its safety and high effectiveness (>93% in preventing persistent HPV infections and cervical precancerous lesions in women).9 However, the 9-valent HPV vaccine is monopolised and patent-protected by international pharmaceutical companies, making it expensive and often not covered by health insurance in LMICs. As a result, the vaccine is not widely available to women in these regions. Fewer than 30% of LMICs have introduced HPV vaccination into their national immunisation schedules, compared with over 85% of high-income countries.10 In addition, in low-income countries where financial and medical resources are scarce, the majority of women lack access to genetic screening for cancer and complementary therapies, resulting in high morbidity and mortality rates from breast and ovarian cancer.
How to change the global inequality in cancer care?
International research initiatives are essential for enhancing cancer research infrastructure and capacity building in LMICs. These initiatives should prioritise research in radiotherapy and surgery, which are among the most cost-effective, efficient, and widely utilised treatments for cancer. There is an urgent need to increase funding for cancer screening and diagnostic research in LMICs, while continuously expanding screening programs for individuals at high risk of developing cancer.
Global frameworks, such as those led by the World Health Organisation and the Global Fund, should focus on reducing drug prices and improving the accessibility of medicines through financing, procurement, and distribution efforts. Supporting academic cooperative groups in conducting collaborative drug research is also vital, with careful consideration of the diverse ethnic, cultural, and environmental contexts across different countries and regions. Ensuring the involvement of LMICs in research initiatives is particularly important.
International collaboration in clinical trials is essential to ensure the safety and efficacy of new drugs. Sharing cancer data among countries can enhance the global breadth and accuracy of research, providing a more robust scientific foundation for cancer treatment. Ultimately, prioritising the interests of patients with cancer means focusing on the actual clinical utility of drugs rather than solely pursuing advanced efficacy, and avoiding the pitfalls of excessive commercialisation.
Governments must enhance macro-control efforts to maintain the market share of essential cancer drugs, accelerate the approval and availability of cancer prevention and treatment medications, and strengthen support for cancer drug research. Priority should be given to research focused on cancer drugs that patients urgently need, and there should be encouragement for the generic production of clinically necessary cancer drugs whose patents have expired or are nearing expiration. To reduce the financial burden on patients with cancer, governments should implement measures such as lowering drug prices through nationally negotiated access systems, centralised bulk purchasing, and including more cancer drugs in the medical insurance catalogue. In addition, countries can collaborate in negotiating drug purchases, leading to better price advantages through collective bargaining.
Pharmaceutical companies can support drug innovation through government and public agency funding, tax incentives, and subsidies as alternatives to the traditional patent system. Governments or international organisations can support drug research by providing direct funding and reward programs, enabling pharmaceutical companies to avoid relying on high drug prices to recoup research costs. Encouraging open and collaborative drug research practices among pharmaceutical companies can further reduce research costs. For example, pharmaceutical companies collaborating with academic institutions and nonprofit organisations, along with sharing research results, can minimise duplication and decrease overall expenses. Table 1 shows the summary of actions to change the global inequality in cancer care.
Table 1.
The summary of actions to change the global inequality in cancer care
 International organisations International organisations |
|
 Governments Governments |
|
 Pharmaceutical companies Pharmaceutical companies |
|
LMIC, low- and middle-income countries.
Conclusions
With the advancement of cancer medical technology, patients with cancer are experiencing longer survival times. Many cancers have become manageable chronic diseases, which require more cancer drugs to maintain survival.11 Access to quality cancer care is a fundamental human right.12 However, significant global inequalities persist across all aspects of cancer prevention, diagnosis, and treatment. To bridge the cancer care gap, it is essential to prioritise the interests of patients with cancer over commercial interests. Maximising patient benefits is the original goal of cancer care. Global stakeholders must take concerted action to ensure more equitable access to cancer care for all patients.
Acknowledgments
Funding
None declared.
Disclosure
The authors have declared no conflicts of interest.
References
- 1.Ferlay J., Colombet M., Soerjomataram I., et al. Cancer statistics for the year 2020: an overview. Int J Cancer. 2021;149(4):778–789. doi: 10.1002/ijc.33588. [DOI] [PubMed] [Google Scholar]
- 2.The Lancet Cancer research equity: innovations for the many, not the few. Lancet. 2024;403(10425):409. doi: 10.1016/S0140-6736(24)00196-X. [DOI] [PubMed] [Google Scholar]
- 3.WHO Cancer/WHO fact sheet. https://www.who.int/news-room/fact-sheets/detail/cancer
- 4.Booth C.M., Sengar M., Goodman A., et al. Common Sense Oncology: outcomes that matter. Lancet Oncol. 2023;24(8):833–835. doi: 10.1016/S1470-2045(23)00319-4. [DOI] [PubMed] [Google Scholar]
- 5.Seraphin T.P., Joko-Fru W.Y., Manraj S.S., et al. Prostate cancer survival in sub-Saharan Africa by age, stage at diagnosis, and human development index: a population-based registry study. Cancer Causes Control. 2021;32(9):1001–1019. doi: 10.1007/s10552-021-01453-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sung H., Ferlay J., Siegel R.L., et al. Global Cancer Statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2021;71(3):209–249. doi: 10.3322/caac.21660. [DOI] [PubMed] [Google Scholar]
- 7.Dau H., Trawin J., Nakisige C., et al. The social and economic impacts of cervical cancer on women and children in low- and middle-income countries: a systematic review. Int J Gynaecol Obstet. 2023;160(3):751–761. doi: 10.1002/ijgo.14395. [DOI] [PubMed] [Google Scholar]
- 8.Xu T., Yang X., He X., Wu J. The study on cervical cancer burden in 127 countries and its socio-economic influence factors. J Epidemiol Glob Health. 2023;13(1):154–161. doi: 10.1007/s44197-022-00081-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Joura E.A., Giuliano A.R., Iversen O.E., et al. A 9-valent HPV vaccine against infection and intraepithelial neoplasia in women. N Engl J Med. 2015;372(8):711–723. doi: 10.1056/NEJMoa1405044. [DOI] [PubMed] [Google Scholar]
- 10.Dorji T., Nopsopon T., Tamang S.T., Pongpirul K. Human papillomavirus vaccination uptake in low- and middle-income countries: a meta-analysis. EClinicalMedicine. 2021;34 doi: 10.1016/j.eclinm.2021.100836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Pituskin E., Joy A.A., Fairchild A. Advanced cancer as a chronic disease: introduction. Semin Oncol Nurs. 2021;37(4) doi: 10.1016/j.soncn.2021.151176. [DOI] [PubMed] [Google Scholar]
- 12.Prager G.W., Braga S., Bystricky B., et al. Global cancer control: responding to the growing burden, rising costs and inequalities in access. ESMO Open. 2018;3(2) doi: 10.1136/esmoopen-2017-000285. [DOI] [PMC free article] [PubMed] [Google Scholar]