Abstract
Background
Lower respiratory infections (LRIs) remain a leading cause of mortality among children, yet previous studies have primarily focused on children under 5 years of age as a whole, with limited research on more specific age groups. This study aimed to analyze the trends in mortality associated with lower respiratory infections (LRIs) among children under 14 years of age from 1990 to 2019, with particular attention to regional and age-specific disparities.
Methods
We collected annual lower respiratory infection (LRI) deaths and mortality rates for six age groups of children under 14 years from 1990 to 2019 using data from GBD 2019. Estimated annual percentage changes (EAPCs) were calculated by fitting a linear regression model to quantify temporal trends. Additionally, EAPCs for 12 risk factors by Socio-Demographic Index(SDI) and age group were calculated to assess their impact on changes in LRI mortality.
Results
Globally, LRI-related deaths among children under 14 years decreased by 68.81 %, from 2,290,115 (95 % UI 2,001,328 to 2,687,160) in 1990 to 714,315 (95 % UI 588,975 to 875,975) in 2019. The most substantial reduction was observed in East Asia, with an EAPC of −9.68 (95 % CI -9.98 to −9.38). The highest mortality occurred in the 28–364 days age group, with significant risk factors including child wasting (26.81 %), household air pollution from solid fuels (16.14 %), and low birth weight (10.15 %). In the low and lower-middle SDI regions, there was an upward trend in mortality due to ambient particulate pollution among children aged 10–14 years.
Conclusion
Despite a significant global decline in LRI mortality among children under 14 years from 1990 to 2019, regional disparities persist. Addressing these inequalities and considering the developmental stages of children are crucial for further reducing child mortality rates.
Keywords: Lower respiratory infections, Mortality, Child health, Trend
1. Introduction
Lower respiratory infections (LRIs), defined as clinician-diagnosed pneumonia or bronchiolitis in the Global Burden of Diseases (GBD) Study, are a leading cause of death worldwide, particularly among children under 5 years of age [[1], [2], [3]].
Several factors have been identified as potential correlates of LRIs among children, including the child's age, sex, type of toilet facility, and type of cooking fuel [[4], [5], [6]]. General preventive practices and early detection of risk factors are crucial for significantly reducing LRI mortality in children. review showed that general preventive practices addressing these risk factors are strongly associated with reduced odds of ALRI death in children [7]. However, there are notable variations in these factors across different income levels [4], indicating that policies and strategies based on risk factors identified in resource-rich countries may not be an effective means of preventing lower respiratory infections in resource-limited settings [8].
We searched PubMed, Embase and Web of Science for studies published after 2010, focusing on LRIs in pediatric populations and found that studies on LRIs in pediatric populations have primarily focused on children aged five and below [3,[9], [10], [11], [12]]. These studies typically examine this age group as a whole, exploring the epidemiological trends and influencing factors of LRIs.
This research extended its scope to include children up to the age of 14, aiming for a more comprehensive understanding of the mortality risks associated with LRI across various stages of childhood development. By delving into these variations, we aimed to provide valuable insights that could inform the development of targeted and effective strategies for the prevention and management of LRI. It is thus crucial to study trends and variations in LRI risk factors across different SDI regions to identify context-specific determinants and lay the groundwork for targeted public health interventions tailored to each region's unique needs.
2. Materials and methods
2.1. Data source
The Global Burden of Disease Study (GBD) 2019 provides a comprehensive and comparative assessment of the burden of 369 diseases and injuries and 87 risk factors in 204 countries and territories from 1990 to 2019. The detailed approaches used for the GBD 2019 estimation process for the death and mortality of LRIs have been described in previous studies [13,14].
Annual LRI death numbers and mortality (per 100,000) from 1990 to 2019, by region, country and age group, were obtained from the Global Health Data Exchange (GHDx) query tool (http://ghdx.healthdata.org/gbd-results-tool, accessed November 2023). Data from 204 countries and territories were available. These countries and territories were then categorized into 5 regions in terms of the sociodemographic index (SDI), namely, high SDI, high-middle SDI, middle SDI, low-middle SDI, and low SDI, and 21 regions in terms of geography. In this study, we focused on children under the age of 14, further divided into six age groups: early newborn stage (0–6 days), late newborn stage (7–27 days), infancy (28–364 days), preschool children (1–4 years), school-age children (5–9 years) and early adolescence (10–14 years).
2.2. Statistical analysis
We presented annual LRIs deaths and mortality with 95 % uncertainty intervals (UIs) from 1990 to 2019 in 21 GBD regions and 5 SDI regions. Then, we calculated the overall changes and estimated annual percentage changes (EAPCs) in mortality to assess the temporal trends in LRI mortality among children under 14. Overall changes were defined as The EAPC was calculated by fitting the linear regression line: y = α + βx + ε, where y represents ln(rate) and x refers to the calendar year. The EAPC was calculated as . Additionally, we displayed the trends in the number of deaths for various age groups globally and in 5 SDI regions from 1990 to 2019, along with the EAPCs. Moreover, LRI mortality attributable to the 12 risk factors, and their EAPCs are presented across regions. All the statistical analyses were conducted with R version 4.3.2.
3. Results
Globally, the number of deaths among children under 14 years due to LRIs decreased from 2,290,115 (95 % UI 2,001,328 to 2,687,160) in 1990 to 714,315 (95 % UI 588,975 to 875,975) in 2019, representing a decrease of 68.81 %. The mortality declined from 130.57 per 100,000 (95 % UI 114.1 to 153.2) in 1990 to 36.45 per 100,000 (95 % UI 30.05 to 44.7) in 2019, with an overall EAPC of −4.17 (95 % UI -4.27 to −4.07) (Table 1).
Table 1.
The death number, rate and temporal trends of lower respiratory infections among children under 14 years in 1990 and 2019.
| Location | Death number (95 % UI) |
Death Rate (95 % UI) |
Overall change (%) | EAPC (95 % CI) | ||
|---|---|---|---|---|---|---|
| 1990 | 2019 | 1990 | 2019 | |||
| Global | 2290115 (2001328–2687160) | 714315 (588975–875975) | 130.57 (114.1–153.2) | 36.45 (30.05–44.7) | −68.81 | −4.17 (−4.27∼-4.07) |
| High SDI | 6279 (5858–6787) | 1494 (1336–1654) | 3.64 (3.39–3.93) | 0.92 (0.82–1.01) | −76.21 | −7.25 (−7.38∼-7.12) |
| High-middle SDI | 149113 (129967–173002) | 13581 (11522–15970) | 49.12 (42.82–56.99) | 5.54 (4.7–6.51) | −90.89 | −3.03 (−3.28∼-2.78) |
| Middle SDI | 611329 (543773–698584) | 93602 (77740–112995) | 105.16 (93.54–120.16) | 16.91 (14.04–20.41) | −84.69 | −5.8 (−5.98∼-5.63) |
| Low-middle SDI | 844782 (736265–990103) | 215255 (179440–259624) | 186.32 (162.39–218.37) | 41.11 (34.27–49.59) | −74.52 | −4.23 (−4.39∼-4.07) |
| Low SDI | 677499 (553865–844582) | 389824 (309207–484819) | 279.94 (228.85–348.98) | 82.44 (65.39–102.53) | −42.46 | −4.98 (−5.12∼-4.84) |
| Central Asia | 49649 (45032–54933) | 13203 (10723–16483) | 198.95 (180.44–220.12) | 49.08 (39.86–61.28) | −73.41 | −4.48 (−4.67∼-4.3) |
| Central Europe | 8237 (7696–8956) | 754 (618–903) | 28.45 (26.59–30.94) | 4.27 (3.51–5.12) | −90.85 | −6.19 (−6.29∼-6.09) |
| Eastern Europe | 9015 (8567–9748) | 1554 (1284–1848) | 17.52 (16.65–18.95) | 4.19 (3.46–4.99) | −82.77 | −4.23 (−4.65∼-3.8) |
| Australasia | 109 (99–121) | 39 (32–48) | 2.37 (2.16–2.63) | 0.72 (0.58–0.88) | −63.78 | −3.4 (−3.7∼-3.09) |
| High-income Asia Pacific | 1391 (1268–1538) | 208 (187–230) | 3.95 (3.6–4.37) | 0.89 (0.8–0.98) | −85.06 | −4.42 (−4.66∼-4.17) |
| High-income North America | 1662 (1566–1766) | 686 (627–746) | 2.71 (2.55–2.88) | 1.04 (0.95–1.13) | −58.7 | −4.72 (−4.95∼-4.48) |
| Southern Latin America | 2459 (2277–2660) | 619 (482–774) | 16.47 (15.25–17.82) | 4.15 (3.23–5.19) | −74.85 | −4.45 (−4.62∼-4.28) |
| Western Europe | 1572 (1497–1713) | 363 (312–416) | 2.21 (2.11–2.41) | 0.53 (0.45–0.6) | −76.9 | −4.45 (−4.7∼-4.21) |
| Andean Latin America | 22926 (19966–26397) | 3748 (2813–4876) | 152.39 (132.71–175.46) | 20.72 (15.55–26.95) | −83.65 | −6.51 (−6.59∼-6.44) |
| Caribbean | 9453 (7828–11398) | 4013 (3018–5193) | 82.82 (68.59–99.87) | 34.35 (25.83–44.45) | −57.55 | −2.49 (−2.73∼-2.24) |
| Central Latin America | 36729 (32745–40269) | 8336 (6119–11065) | 57.3 (51.09–62.83) | 12.75 (9.36–16.92) | −77.3 | −4.91 (−5.1∼-4.72) |
| Tropical Latin America | 37511 (32449–45247) | 5589 (4497–6852) | 69.54 (60.15–83.88) | 11.24 (9.05–13.78) | −85.1 | −5.86 (−5.99∼-5.73) |
| North Africa and Middle East | 161876 (133238–212206) | 34134 (27615–41288) | 112.63 (92.71–147.65) | 19.41 (15.7–23.48) | −78.91 | −5.78 (−5.89∼-5.67) |
| South Asia | 740174 (633311–847142) | 204998 (167789–250185) | 168.61 (144.27–192.98) | 39.67 (32.47–48.41) | −72.3 | −4.72 (−4.91∼-4.53) |
| East Asia | 408909 (349744–475448) | 16462 (13614–19556) | 122.08 (104.42–141.95) | 7.07 (5.85–8.4) | −95.97 | −9.68 (−9.98∼-9.38) |
| Oceania | 4348 (3471–5296) | 5386 (3883–7203) | 165.48 (132.08–201.54) | 111.51 (80.4–149.13) | 23.86 | −1.01 (−1.22∼-0.79) |
| Southeast Asia | 196001 (157857–257191) | 36071 (30049–43201) | 113.8 (91.65–149.33) | 21.37 (17.8–25.6) | −81.6 | −5.59 (−5.72∼-5.46) |
| Location | Death number (95 % UI) |
Death Rate (95 % UI) |
Overall change (%) | EAPC (95 % CI) | ||
|---|---|---|---|---|---|---|
| 1990 | 2019 | 1990 | 2019 | |||
| Central Sub-Saharan Africa | 64710 (47576–85356) | 25736 (18758–34997) | 250.49 (184.17–330.41) | 45.11 (32.88–61.34) | −60.23 | −5.56 (−6.09∼-5.03) |
| Eastern Sub-Saharan Africa | 242633 (194510–302840) | 103394 (80927–131661) | 268.5 (215.24–335.12) | 58.57 (45.84–74.58) | −57.39 | −5.15 (−5.31∼-5) |
| Southern Sub-Saharan Africa | 20358 (16866–24227) | 10591 (8163–13582) | 99.91 (82.78–118.9) | 44.85 (34.57–57.52) | −47.97 | −1.9 (−2.32∼-1.48) |
| Western Sub-Saharan Africa | 270395 (212003–349975) | 238432 (185132–298701) | 307.91 (241.41–398.53) | 120.22 (93.35–150.61) | −11.82 | −3.34 (−3.6∼-3.08) |
3.1. Distribution by region
Among the 21 GBD regions, western sub-Saharan Africa exhibited the highest number of deaths (238,432, 95 % UI 185,132 to 298,701) and death rate (120.22, 95 % UI 93.35 to 150.61) among children under 14 due to LRIs in 2019. Oceania was the only region that experienced an increase, with a 23.86 % rise in deaths in 2019 (5,386, 95 % UI 3883 to 7203) compared to 1990 (4,348, 95 % UI 3471 to 5296). The most notable decrease in deaths occurred in East Asia, with a remarkable decline of 95.97 %, from 408,909 (95 % UI 349,744 to 475,448) in 1990 to 16,462 (95 % UI 13,614 to 19,556) in 2019. A decreasing trend in mortality was observed across all 21 regions, with East Asia showing the most substantial decrease (EAPC = −9.68, 95 % CI -9.98 to −9.38, Table 1).Among the SDI regions, the low SDI region exhibited both the highest number of deaths (389,824, 95 % CI 309,207 to 484,819) and the highest mortality rate (82.44, 95 % CI 65.39 to 102.53) in 2019. Mortality decreased in all SDI regions, with the most significant decrease observed in the high-middle SDI region (EAPC = −7.25, 95 % CI -7.38 to −7.12, Table 1).
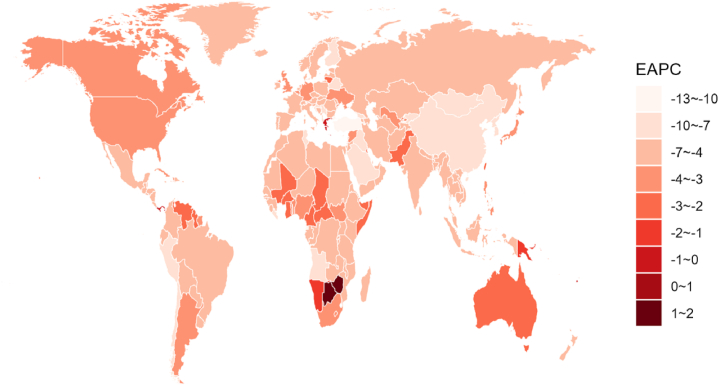
3.2. Distribution by nation
In 2019, deaths in India, Nigeria and Pakistan accounted for 56.7 % of total deaths worldwide across 204 countries and territories. From 1990 to 2019, Turkey (97.32 %), Georgia (96.63 %) and China (96.04 %) experienced the most significant reductions in deaths caused by LRIs (Supplementary Table S1). Over the 30-year period, the mortality among children under 14 in 198 countries has shown an overall declining trend. Notably, Turkey exhibited the most significant decrease (EAPC = −12.44, 95 % CI -13.32 to −11.56), followed by Equatorial Guinea (−10.5, 95 % CI -10.82 to −10.18) and China (−9.75, 95 % CI -10.06 to −9.44). Among the six countries or territories showing an upward trend, Zimbabwe demonstrated the most pronounced increase, with an EAPC of 1.13 (95 % CI 0.52 to 1.74) (Fig. 1).
Fig. 1.
The EAPCs in LRI mortality in children under 14 years of age among 204 countries and territories from 1990 to 2019.
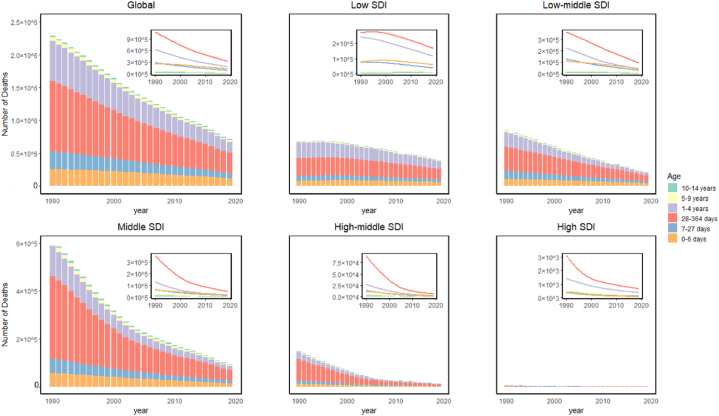
3.3. Distribution by age group
Globally, in 2019, the 28–364 days age group accounted for the greatest percentage of deaths, comprising 43 % of the total, followed by the 1–4 years age group (23.99 %). In the low-middle SDI region, the 28–364 days age group made the greatest contribution to deaths, followed by the 0–6 days group (Fig. 2, Supplementary Table S2). Across all SDI regions, a declining trend was evident in mortality rates across all age groups. This trend was most evident in low-middle SDI regions, where infants aged 28–364 days contributed the most fatalities, followed by 0–6 days neonates.
Fig. 2.
Death numbers due to LRI in different age groups globally and across SDI regions from 1990 to 2019.
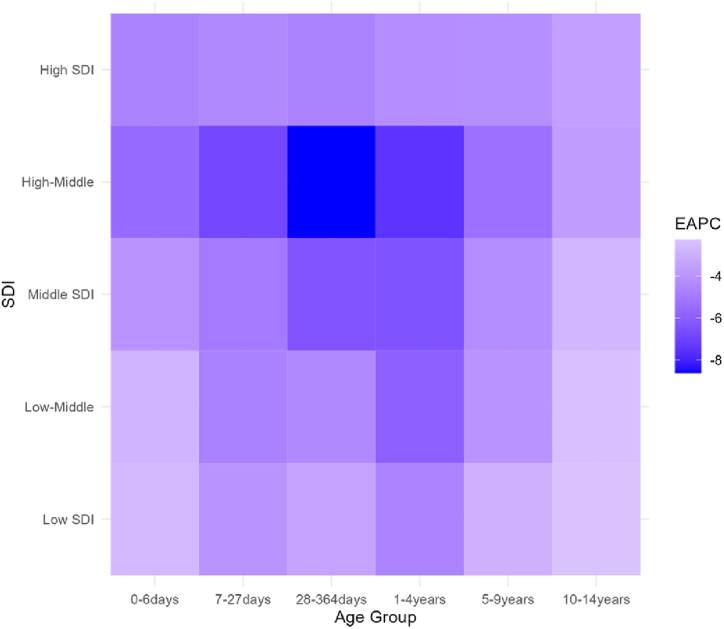
In low SDI regions, neonatal mortality (0–6 days) showed a slight increase from 1990 to 2000, followed by a gradual decline after 2000. On the other hand, infant mortality (28–364 days) has consistently decreased since 1990, with a noticeable acceleration in the decline starting in 2003. In contrast, middle, high-middle, and high SDI regions exhibit a uniform downward trend in mortality across all age groups, with the most significant reductions observed among infants aged 28–364 days. Notably, middle and high-middle SDI regions experienced significant mortality declines from 1990 to 2005, while high SDI regions achieved substantial reductions even earlier, by 2001 (Fig. 2). Notably, in the low SDI and low-middle SDI regions, the most substantial fluctuations were observed in the 7–27 days age group. Conversely, in the middle SDI, high-middle SDI, and high SDI regions, the most noticeable variations were observed among children aged 28–364 days (Fig. 3).
Fig. 3.
EAPC of LRI mortality for different age groups in various SDI regions from 1990 to 2019.
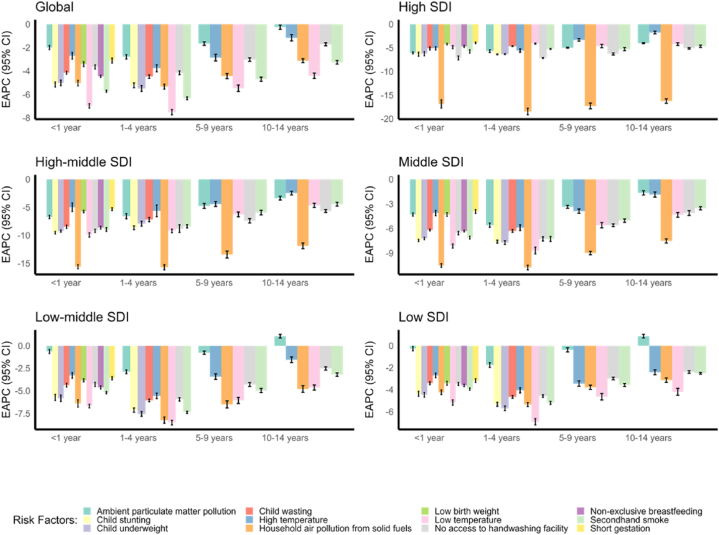
3.4. Risk factors
In 2019, child wasting (26.81 %), household air pollution from solid fuels (16.14 %), and low birth weight (10.15 %) were identified as the top three leading risk factors contributing to LRI deaths among children under 14 years old globally. Over the past 30 years, the mortality due to household air pollution from solid fuels has significantly declined, with the fastest reductions occurring in high SDI regions and high-middle SDI and middle SDI regions. In low SDI and low-middle SDI regions, there has been an upward trend in mortality attributed to ambient particulate matter pollution among children aged 10 to 14 (Fig. 4).
Fig. 4.
Global and SDI-specific EAPC in LRI mortality attributable to the 12 risk factors by age group from 1990 to 2019.
4. Discussion
This study comprehensively described the temporal trend and global geographical variations of the mortality as well as the attributable risk factors of lower respiratory infections, focusing on children under 14. Despite a significant decrease in LRI deaths during this period, it remains a major public health concern, especially in low SDI and low-middle SDI regions. Infants under 1 year old continued to be the most vulnerable group to LRI. Despite the rapid decline in mortality attributed to low temperature and low birth weight, child wasting, household air pollution from solid fuels, and low birth weight persisted as the most significant global risk factors. Additionally, trends in mortality rates associated with various risk factors exhibited distinct patterns across different SDI regions.
Our study suggested that the low SDI region and low-middle SDI region, particularly South Asia, Eastern Sub-Saharan Africa and Western Sub-Saharan Africa, bore the most substantial burden of LRIs among children under 14 years of age. This burden might be associated with low socioeconomic status, insufficient vaccine coverage, inadequate antimicrobial treatment, and severe environmental pollution [15]. In 2019, the number of deaths in Oceania increased by 23.86 % compared to 1990, which was mainly driven by a rise in Papua New Guinea, one of the least developed regions in the area. The rest of Oceania, however, continued to experience a downward trend. Notably, over the past 30 years, Turkey, Georgia, and China have achieved significant success in controlling deaths from LRIs in children under 14 years of age. This success might be attributed to rapid economic development, effective vaccination programs and reductions in household air pollution in these regions [16,17].In terms of age groups, infants under 1 year of age, particularly those aged 28–364 days, remain the most vulnerable population to LRIs [18]. Despite initiatives like the Integrated Management of Childhood Illnesses (IMCI) and the Global Alliance for Vaccines and Immunization (GAVI) [19], only a small proportion of low-income countries and lower-middle-income countries have adopted national maternal or child influenza immunization policies and, where present, most have achieved only low or unknown levels of vaccine uptake [20,21]. Future efforts should focus on strengthening policy implementation, ensuring vaccine supply, and optimizing vaccine distribution to increase coverage rates.
The rising trend in LRI mortality among the 0–6 days age group before 2000 in low SDI regions may be attributed to underdeveloped economies and a lack of maternal and child healthcare. After the Millennium Development Goals (MDGs) [22] were launched in 2000, increased focus on infant health and the widespread implementation of nutritional programs became key factors contributing to the gradual decline in mortality rates. In contrast, high SDI regions, due to their more advanced economic development, relatively abundant medical resources, and well-established healthcare systems, were able to see significant impacts more quickly during the implementation of the MDGs, leading to an earlier turning point in the downward mortality trend compared to other regions.
Based on our research findings, household air pollution from solid fuels was the leading risk factor for LRI deaths among children under 14 years of age globally, consistent with results across all age groups [19]. Studies have indicated that children in low SDI and low-middle SDI regions who relied on solid biomass for cooking, lighting and heating, were more susceptible to LRIs caused by household air pollution [23,24]. As depicted in Fig. 4, there was a significant decline in LRI mortality attributed to household air pollution from solid fuels in high SDI, high-middle SDI, and middle SDI regions from 1990 to 2019. This decline might be associated with the implementation of more effective environmental policies and improvements in air quality within these regions. Concurrently, the Global Alliance for Clean Cookstoves is leading efforts to promote the adoption of clean cookstoves and environmentally friendly fuels. Additionally, it is recommended to implement interim strategies such as educating mothers to reduce their children's exposure to burning solid fuels, shortening cooking duration, or encouraging other household members to care for infants while the mother is cooking [24]. Among children aged 10–14 years in these regions, there has been an upward trend in mortality due to ambient particulate matter pollution, which suggested that these areas may face additional sources of environmental pollution, such as industrial emissions and traffic pollution, leading to an increased concentration of particulate matter in the air and consequently increasing the risk of respiratory infections. To address this concerning trend, it is crucial to enhance monitoring and preventive measures and implement more practical and effective strategies to mitigate the adverse effects of household air pollution on children's health.
There are several limitations in our study. First of all, the accuracy of our estimates is constrained by the availability of data in the GBD study [25]. The GBD study, while extensive, faces challenges in data collection from resource-limited areas, potentially affecting accuracy. To address this, the GBD project used advanced statistical models like Cause of Death Ensemble modeling (CODEm) to estimate missing data [26]. Despite the robust validation, some bias may still exist. To mitigate this, the GBD project provided uncertainty intervals to aid in data interpretation. For our study, we used indicators such as change percentage and EAPC to further minimize these uncertainties and improve trend analysis. Secondly, as an ecological study, our research could be influenced by unaccounted confounding factors such as economic conditions and cultural backgrounds. Although we attempted to mitigate these effects by stratifying our analysis by different SDI regions, some bias may still remain in the results. Thirdly, our study data are limited to the year 2019, and further investigations are required to explore the situation after the COVID-19 pandemic [27].
The findings of this study offer several important avenues for future research. As the GBD database continues to be updated, incorporating more recent data will be crucial for providing a comprehensive understanding of trends and impacts, especially in the aftermath of the COVID-19 pandemic. Additionally, further research should focus on specific pathogens responsible for LRIs, examining changes in their prevalence, trends, and influencing factors. Such investigations will enhance our understanding of these pathogens' evolving impact and support the development of more targeted and effective preventive and treatment strategies.
In conclusion, LRI mortality among children remains a serious concern, especially in low resource settings and among infants under one year old. Continued efforts to improve child nutrition, strengthen public health initiatives, and address environmental pollution are essential. Additionally, future research should explore post-pandemic trends and focus on specific pathogens to enhance prevention and treatment strategies.
CRediT authorship contribution statement
Xufei Xing: Writing – original draft, Data curation. Siqi Tang: Formal analysis. Weiye Wang: Data curation. Haiyan Xiong: Conceptualization. Tiejun Zhang: Writing – review & editing. Weibing Wang: Writing – review & editing. Yihan Lu: Methodology. Tao Zhang: Writing – review & editing, Conceptualization. Chen Suo: Writing – review & editing.
Ethical approval statement
This study is an ecological analysis using public data freely shared by the Global Burden of Disease (GBD) database and does not involve personal information. Therefore, ethical approval is exempted.
Data availability
The data used in this study are publicly available and were obtained from the Global Burden of Disease (GBD) study 2019, which can be accessed through the Global Health Data Exchange (GHDx)(http://ghdx.healthdata.org/gbd-results-tool).
Funding source
We acknowledge financial supports from the Shanghai Municipal Science and Technology Major Project (grant numbers: ZD2021CY001, 2023SHZDZX02), and the National Key Research and Development Program of China (grant number: 2023YFC2508001).
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgement
We appreciate the works by the Global Burden of Disease study 2019 collaborators.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.heliyon.2024.e39502.
Appendix A. Supplementary data
The following is/are the supplementary data to this article.
References
- 1.Age-sex differences in the global burden of lower respiratory infections and risk factors, 1990-2019: results from the Global Burden of Disease Study 2019. Lancet Infect. Dis. 2022;22(11):1626–1647. doi: 10.1016/S1473-3099(22)00510-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Paulson KR, Kamath AM, Alam T, Bienhoff K, Abady GG, Abbas J, et al. Global, regional, and national progress towards Sustainable Development Goal 3.2 for neonatal and child health: all-cause and cause-specific mortality findings from the Global Burden of Disease Study 2019. The Lancet. 2021;398:870–905. doi: 10.1016/S0140-6736(21)01207-1. Sep 4, (10303) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Wang X., Li Y., O'Brien K.L., Madhi S.A., Widdowson M.A., Byass P., et al. Global burden of respiratory infections associated with seasonal influenza in children under 5 years in 2018: a systematic review and modelling study. Lancet Glob Health. 2020;8(4):e497–e510. doi: 10.1016/S2214-109X(19)30545-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Seidu A.A., Dickson K.S., Ahinkorah B.O., Amu H., Darteh E.K.M., Kumi-Kyereme A. Prevalence and determinants of Acute Lower Respiratory Infections among children under-five years in sub-Saharan Africa: evidence from demographic and health surveys. SSM Popul Health. 2019;8 doi: 10.1016/j.ssmph.2019.100443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Akinyemi J.O., Morakinyo O.M. Household environment and symptoms of childhood acute respiratory tract infections in Nigeria, 2003-2013: a decade of progress and stagnation. BMC Infect. Dis. 2018;18(1):296. doi: 10.1186/s12879-018-3207-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Al-Sharbatti S.S., AlJumaa L.I. Infant feeding patterns and risk of acute respiratory infections in Baghdad/Iraq. Italian Journal of Public Health. 2012;9(3) [Google Scholar]
- 7.Sonego M., Pellegrin M.C., Becker G., Lazzerini M. Risk factors for mortality from acute lower respiratory infections (ALRI) in children under five years of age in low and middle-income countries: a systematic review and meta-analysis of observational studies. PLoS One. 2015;10(1) doi: 10.1371/journal.pone.0116380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Sarfo J.O., Amoadu M., Gyan T.B., Osman A.G., Kordorwu P.Y., Adams A.K., et al. Acute lower respiratory infections among children under five in Sub-Saharan Africa: a scoping review of prevalence and risk factors. BMC Pediatr. 2023;23(1):225. doi: 10.1186/s12887-023-04033-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Shi X., Wu M., Jia X., Bao J., Wang Y., Yang C., et al. Trends of incidence, mortality, and risk factors for lower respiratory infections among children under 5 Years in China from 2000 to 2019. Int. J. Environ. Res. Publ. Health. 2023;20(4) doi: 10.3390/ijerph20043547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Quantifying risks and interventions that have affected the burden of lower respiratory infections among children younger than 5 years: an analysis for the Global Burden of Disease Study 2017. Lancet Infect. Dis. 2020;20(1):60–79. doi: 10.1016/S1473-3099(19)30410-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Collaborators GBDLRI Quantifying risks and interventions that have affected the burden of lower respiratory infections among children younger than 5 years: an analysis for the Global Burden of Disease Study 2017. Lancet Infect. Dis. 2020;20(1):60–79. doi: 10.1016/S1473-3099(19)30410-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Li Y., Wang X., Blau D.M., Caballero M.T., Feikin D.R., Gill C.J., et al. Global, regional, and national disease burden estimates of acute lower respiratory infections due to respiratory syncytial virus in children younger than 5 years in 2019: a systematic analysis. Lancet. 2022;399(10340):2047–2064. doi: 10.1016/S0140-6736(22)00478-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Global burden of 87 risk factors in 204 countries and territories, 1990-2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet. 2020;396(10258):1223–1249. doi: 10.1016/S0140-6736(20)30752-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Global burden of 369 diseases and injuries in 204 countries and territories, 1990-2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet. 2020;396(10258):1204–1222. doi: 10.1016/S0140-6736(20)30925-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Izadnegahdar R., Cohen A.L., Klugman K.P., Qazi S.A. Childhood pneumonia in developing countries. Lancet Respir. Med. 2013;1(7):574–584. doi: 10.1016/S2213-2600(13)70075-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Guo Y., Bai J., Na H. The history of China's maternal and child health care development. Semin. Fetal Neonatal Med. 2015;20(5):309–314. doi: 10.1016/j.siny.2015.07.006. [DOI] [PubMed] [Google Scholar]
- 17.Guan X., Silk B.J., Li W., Fleischauer A.T., Xing X., Jiang X., et al. Pneumonia incidence and mortality in Mainland China: systematic review of Chinese and English literature, 1985-2008. PLoS One. 2010;5(7) doi: 10.1371/journal.pone.0011721. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Xiang S., Chen Z., Dai Z., Wang F. Global burden of lower respiratory infections attributable to secondhand smoke among children under 5 years of age, 2010-2019: a systematic analysis of the global burden of disease study 2019. BMC Publ. Health. 2023;23(1):1920. doi: 10.1186/s12889-023-16848-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kang L., Jing W., Liu J., Liu M. Trends of global and regional aetiologies, risk factors and mortality of lower respiratory infections from 1990 to 2019: an analysis for the Global Burden of Disease Study 2019. Respirology. 2023;28(2):166–175. doi: 10.1111/resp.14389. [DOI] [PubMed] [Google Scholar]
- 20.Palache A., Abelin A., Hollingsworth R., Cracknell W., Jacobs C., Tsai T., et al. Survey of distribution of seasonal influenza vaccine doses in 201 countries (2004-2015): the 2003 World Health Assembly resolution on seasonal influenza vaccination coverage and the 2009 influenza pandemic have had very little impact on improving influenza control and pandemic preparedness. Vaccine. 2017;35(36):4681–4686. doi: 10.1016/j.vaccine.2017.07.053. [DOI] [PubMed] [Google Scholar]
- 21.Hirve S., Lambach P., Paget J., Vandemaele K., Fitzner J., Zhang W. Seasonal influenza vaccine policy, use and effectiveness in the tropics and subtropics - a systematic literature review. Influenza Other Respir Viruses. 2016;10(4):254–267. doi: 10.1111/irv.12374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Steele V., Patterson K., Berrang-Ford L., King N., Kulkarni M., Lwasa S., et al. Antenatal care research in East Africa during the Millennium development Goals initiative: a scoping review. Matern. Child Health J. 2022;26(3):469–480. doi: 10.1007/s10995-021-03355-5. [DOI] [PubMed] [Google Scholar]
- 23.Al-Janabi Z., Woolley K.E., Thomas G.N., Bartington S.E. A cross-sectional analysis of the association between domestic cooking energy source type and respiratory infections among children aged under five years: evidence from demographic and household surveys in 37 low-middle income countries. Int. J. Environ. Res. Publ. Health. 2021;18(16) doi: 10.3390/ijerph18168516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Arlington L., Patel A.B., Simmons E., Kurhe K., Prakash A., Rao S.R., Hibberd P.L. Duration of solid fuel cookstove use is associated with increased risk of acute lower respiratory infection among children under six months in rural central India. PLoS One. 2019;14(10) doi: 10.1371/journal.pone.0224374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.McAllister D.A., Liu L., Shi T., Chu Y., Reed C., Burrows J., et al. Global, regional, and national estimates of pneumonia morbidity and mortality in children younger than 5 years between 2000 and 2015: a systematic analysis. Lancet Glob Health. 2019;7(1):e47–e57. doi: 10.1016/S2214-109X(18)30408-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Murray C.J.L. The global burden of disease study at 30 years. Nat Med. 2022;28(10):2019–2026. doi: 10.1038/s41591-022-01990-1. [DOI] [PubMed] [Google Scholar]
- 27.Feng J.N., Zhao H.Y., Zhan S.Y. Global burden of influenza lower respiratory tract infections in older people from 1990 to 2019. Aging Clin. Exp. Res. 2023;35(11):2739–2749. doi: 10.1007/s40520-023-02553-1. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data used in this study are publicly available and were obtained from the Global Burden of Disease (GBD) study 2019, which can be accessed through the Global Health Data Exchange (GHDx)(http://ghdx.healthdata.org/gbd-results-tool).