Abstract
Myasthenia gravis is an acquired neuromuscular disorder characterized by weakness of the extra-ocular muscles, which progresses to generalized weakness of the voluntary muscles and fatigability. The presented case is of a 70-year-old male patient who presented with complaints of drooping of bilateral eyelids and breathlessness and was diagnosed to have myasthenia gravis and thymic mass. It is uncommon for an elderly patient to present with thymic mass and myasthenia gravis concurrently.
Keywords: Thymic mass, Elderly, Myasthenia gravis, Radiology
Introduction
Myasthenia gravis (MG) is an acquired neuromuscular disorder of the neuromuscular junction characterized by weakness of voluntary muscles and fatigability. This condition initially involves the extra-ocular muscles and progresses to generalized myasthenia gravis in the majority of the population. Thymic neoplasm is commonly associated with para-neoplastic syndrome [1]. It is a very rare presentation of thymic mass with myasthenia gravis to be seen in the elderly patient. Myasthenia gravis is a neuromuscular disorder that involves neuromuscular junction. It is most associated with thymic mass. Early detection of the thymic mass and early management of the disease are seen to reduce the severity of the symptoms. Treatment includes both medical and surgical, the latter being the treatment of choice [2].
Case report
A 70-year-old male came to the outpatient department with complaints of drooping of the bilateral eyelids with double vision and watering. Six months ago, the patient had a sudden onset of watering of both eyes, which was gradually progressive and aggravated on rubbing of eyelids and decreased on washing the eyes with cold water. The patient started having complaints of blurring of vision with double vision in the right eye. After 8 days, the patient developed drooping of the right eyelid, which was sudden in onset and rapidly progressive, such that the patient had complete drooping within ten days.
For one and half months, he was then able to see with his left eye only, after which he developed blurring of vision in the left eye, which was sudden in onset and gradually progressive. One week later, he noticed drooping of the left eyelid, followed by periorbital edema. After a week patient then developed complete drooping of the left eyelid. The patient also complained of breathlessness when walking a few steps. There is no history of hypertension, diabetes, tuberculosis, or any other known systemic illness.
On examination, there was complete ptosis, diplopia, and restricted movements of the bilateral eye. SLURP test revealed bulbar muscle fatigability. Ice was applied to the eyelids, and within 5 minutes, there was a difference of approximately 3 mm in the eyelids, which suggested a strongly positive Ice pack test. Generalized examination revealed areflexia.
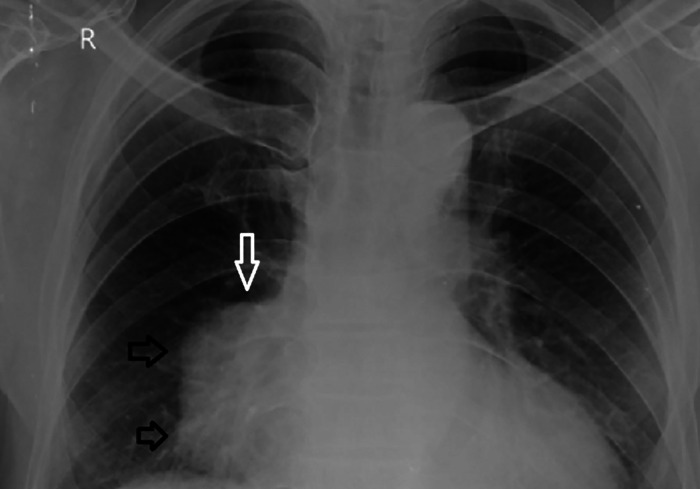
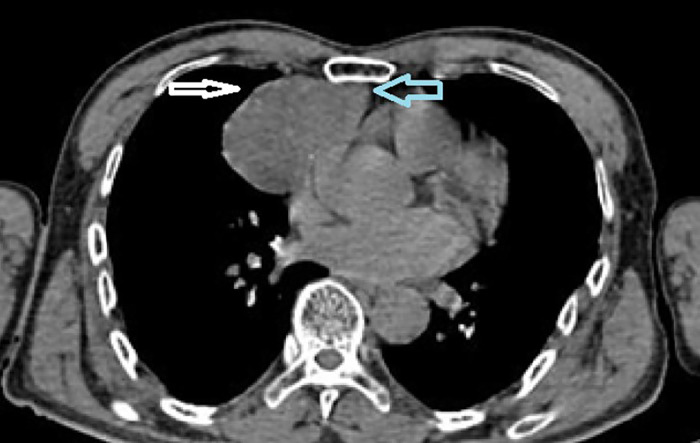
The patient underwent a chest x-ray for breathlessness, which revealed a well-defined, lobulated radio-opaque lesion in the right hemithorax adjacent to the right mediastinum, as shown in image 1. HRCT thorax revealed a well-defined round to oval, soft tissue density lesion in the anterior mediastinum, predominantly on the right side in the region of the thymus and partially obliterating the retrosternal space, suggesting it to be a thymic mass, which includes differentials of thymoma, and thymic adenoma as shown in image 2. The lesion was compressing the lateral border of the right atrium with maintained fat planes with the aorta, right atrium, and right ventricle (Figs. 1,2).
Fig. 1.
X-ray frontal view of thorax showing a well-defined, lobulated radio-opaque lesion in the right hemithorax adjacent to the right mediastinum (arrows).
Fig. 2.
Computed tomography of thorax soft tissue window axial section showing a well-defined round to oval, soft tissue density lesion in the anterior mediastinum, predominantly on the right side in the region of the thymus and partially obliterating the retrosternal space, suggesting it to be a thymic mass (arrows).
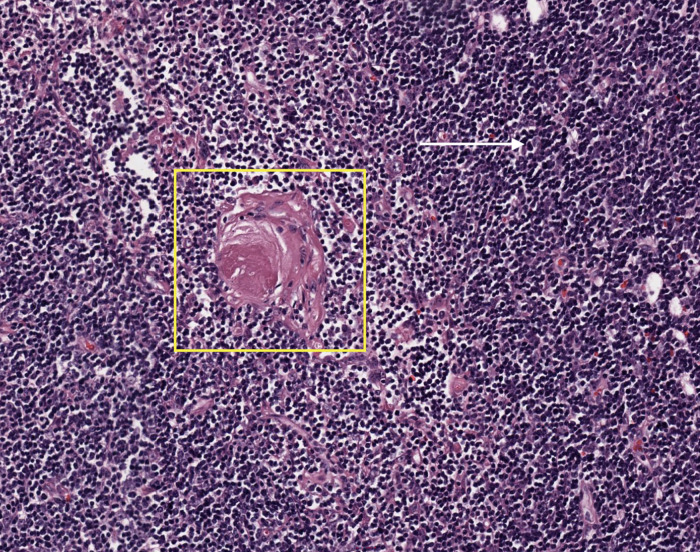
The patient underwent surgical resection of the lesion and was shifted to the surgery intensive care unit postoperation. The lesion was confirmed to be a thymoma on histopathology (Fig. 3). The patient was vitally and neurologically stable and was discharged with advice to review after 2 weeks or if symptoms persist.
Fig. 3.
Histopathological image H&E 40x showing dispersed epithelial cells without clusters in a dense background of immature T cells mimicking thymic cortex (white arrow) with areas of medullary differentiation, nodular pale areas and Hassall's corpuscles (yellow box) suggesting thymoma.
Discussion
In early childhood, the thymus is at its relatively largest size, but it is usually most significant at 11-15 years of age. With advancing age, the cellular element of the thymus starts to decrease, and fatty infiltration starts to replace the normal glandular tissue. This process is called involution of the thymus, which is completed by the age of 60 years, and the size of the thymus gland is reduced. After involution, the thymus gland is replaced by fat cells, but a few thymic remnants can still be noticed [1].
Thymic hyperplasia can mean 2 different things: 1, there is an increase in the number of the cells leading to gross enlargement of the thymus gland; second, there is the presence of lymphoid germinal centers, which is majorly found in patients with myasthenia gravis. The second type does not necessarily mean that there is an increase in the size of the thymus gland, nor does it have any association with fatty infiltration [2].
The Thymus gland can be enlarged due to thyrotoxicosis. Many causes, such as stress, adreno-corticosteroids, sex hormones, chemotherapy, and ionizing radiation, cause a reduction in the size of the thymus gland. Once these factors are removed, there is a rebound increase in the size of the thymus gland [3,4].
For the imaging of the thymus gland and its abnormalities in children, CT offers minimal to no advantage over plain radiographs unless there is the presence of abnormal signs and symptoms that require clarification. From the age of 21-45, it is very difficult to interpret the thymic abnormality when the islands of the normal thymic cells are surrounded by fatty infiltration. These islands may be rounded or ovoid, which may be due to either partial involution or thymoma. However, in older populations, CT provides an advantage over plain radiography and oblique radiography [5].
Thymic cysts can be occasionally found in patients with myasthenia gravis. It is very difficult to interpret thymic cysts on CT because the density of the cysts may or may not differ from the normal parenchyma. Histopathologically, cystic changes are associated with thymoma in about 40% of the population. These cysts can be small or can be large enough to appear as a thymoma [6].
Thymic mass with myasthenia gravis involves both medical and surgical management. Medical management involves the use of Steroids, anticholinesterase agents, and immunosuppressive drugs like Gamma Globulin, Azathioprine, and Plasmapheresis. Surgical management is the treatment of choice and involves thymectomy, which plays a tremendous role in the reduction of the symptoms of myasthenia gravis [7].
Patient consent
An informed verbal and written consent was obtained from the patient.
Footnotes
Competing Interests: The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
References
- 1.Oblakulovich KS, Muradovich YM, Ashrafovna AF, Azamovich NA, Kizi TDA. The Thymus Gland (Thymus) aspects in children (review of literature) Cent Asian J Med Nat Sci. 2022;3(2):9–16. [Google Scholar]
- 2.Manuja N, Kumar S, Acharya S, Daiya V, Sood A, Manuja N, et al. Simultaneous myasthenic crisis with thyrotoxic crisis in an adult male: an autoimmune overlap. Cureus. 2023;15 doi: 10.7759/cureus.44366. [DOI] [PMC free article] [PubMed] [Google Scholar]; Accessed August 3, 2024. Available from: https://www.cureus.com/articles/178752-simultaneous-myasthenic-crisis-with-thyrotoxic-crisis-in-an-adult-male-an-autoimmune-overlap#!/.
- 3.Wilson L, Davis H. The role of thymoma and thymic hyperplasia as prognostic risk factors for secondary generalisation in adults with ocular myasthenia gravis: a systematic narrative review. Br Irish Orthop J. 2023;19(1) doi: 10.22599/bioj.315. https://bioj-online.com/articles/10.22599/bioj.315 Accessed August 3, 2024. Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Toshniwal S, Wanjari A, Acharya S, Kumar S, Sontakke T, Toshniwal SS, et al. Myasthenia gravis mimicking status asthmaticus: the hidden crisis. Cureus. 2024;16 doi: 10.7759/cureus.53044. https://www.cureus.com/articles/223409-myasthenia-gravis-mimicking-status-asthmaticus-the-hidden-crisis#!/ Accessed August 3, 2024. Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.EBSCOhost | 146154593 | Correlation between the atypical presentation of myasthenia gravis and radio-pathological classification of the thymus – a retrospective cohort study. Accessed August 3, 2024. Available from: https://web.p.ebscohost.com/abstract?site=ehost&scope=site&jrnl=18236138&AN=146154593&h=1rom6TMn5e6fupSu/2bc49ARP/2fEuS9VAIvProv/2fdny/2bjk5JhWvL9Phw7K3FuEThLoXA39UiOpHA/2fN5wha9Xke4yA/3d/3d&crl=c&resultLocal=ErrCrlNoResults&resultNs=Ehost&crlhashurl=login.aspx/3fdirect/3dtrue/26profile/3dehost/26scope/3dsite/26authtype/3dcrawler/26jrnl/3d18236138/26AN/3d146154593.
- 6.Ackman JB, Chintanapakdee W, Mendoza DP, Price MC, Lanuti M, Shepard JAO. Longitudinal CT and MRI characteristics of unilocular thymic cysts. Radiology. 2021;301(2):443–454. doi: 10.1148/radiol.2021203593. [DOI] [PubMed] [Google Scholar]
- 7.Gibson EA, Culp WTN. Small Animal Soft Tissue Surgery. John Wiley & Sons, Ltd; 2023. Surgical treatment of thymic disease; pp. 997–1006. [DOI] [Google Scholar]