Abstract
Background and Purpose
The acute vertebrobasilar occlusion associated with the poor prognosis, particularly tandem occlusion. However, few data on the efficacy of the endovascular therapy was indicated in this occlusion. We investigated whether the additional rescue extracranial vertebral stenting improved clinical outcome by modified Rankin scale (mRS) score within 3 months after the procedure.
Methods
This was a retrospective analysis of patients with acute posterior tandem occlusion who were treated with rescue extracranial vertebral stenting between December 2020 and January 2024 at our hospital. Clinical, neuroimaging, procedural, and complication data were collected. Primary outcomes included the rate of good outcomes (mRS ≤ 2) at 3-month follow-up.
Results
Nine patients who underwent rescue extracranial vertebral stenting in posterior circulation tandem occlusions were enrolled in the study. All patients were achieved the successful recanalization (mTICI ≥ 2b). Of Dotter technique in the “distal-to-proximal” approach, Diagnostic-Dotter made up 66.7%. Five patients (55.6%) with good outcome (mRS ≤ 2) at 3 months, and 1 patient (11.1%) underwent suboccipital decompressive craniectomy due to the malignant cerebellar infarction.
Conclusion
Our study suggests that despite the small series with posterior tandem occlusions, the rescue extracranial vertebral stenting could be an important alternative treatment followed by mechanical thrombectomy.
Keywords: Thrombectomy, ischemia, vertebrobasilar insufficiency, balloon-expandable stents, extracranial arteries
Introduction
Acute vertebrobasilar artery occlusion is one of the cerebrovascular diseases with high disability and mortality rates. Although mechanical thrombectomy has recently been demonstrated an effective treatment for large vessel occlusions of posterior circulation,1–4 the treatment strategies depending on the specific pathophysiology. 5 Tandem occlusion in posterior circulation is less frequent than in anterior one, comprises severe stenosis or occlusion of the extracranial vertebral artery ipsilateral to its intracranial and basilar occlusion. 5 The recent studies showed the benefit of the “distal-to-proximal” approach, there were many techniques to achieved the successful recanalization. Besides, the use of Dotter techniques allowed 8F guiding catheter to cross over the extracranial lesions easily in order to restore the intracranial occlusions under the most favorable conditions.6,7 However, the Diagnostic-Dotter, like the Dilator-Dotter, has not been mentioned in previous studies. Therefore, the aim of our study was to assess the improvement of outcomes at 3 months posttreatment in patients receiving rescue extracranial vertebral stenting.
Methods
The data that support the findings of this study are available from the corresponding author on reasonable request.
Subjects
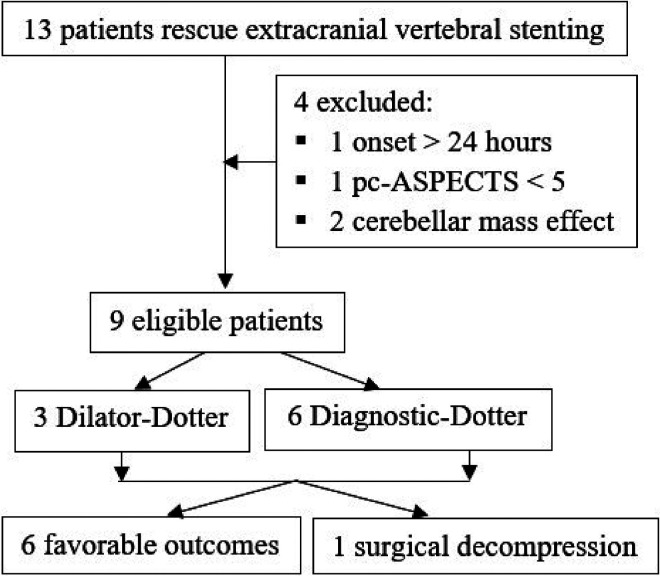
We retrospectively evaluated a prospective database for 9 consecutive patients diagnosed acute tandem occlusions of posterior circulation by DSA who were treated with rescue extracranial vertebral stenting at our hospital between December 2020 and January 2024. Inclusion criteria were: (1) age > 18 years old; (2) the admission of National Institutes of Health Stroke Scale (NIHSS) > 5; (3) onset to treatment time < 24 h; (4) posterior circulation Acute Stroke Prognosis Early CT Score (pc-ASPECTS) ≥ 5. The exclusion criteria were: (1) premorbid mRS > 2; (2) cerebellar mass effect on neuroimaging (Figure 1).
Figure 1.
Flow-chart of patient inclusion in the study.
Procedures
The general anesthesia was used before intervention. An 8F sheath was accessed into the femoral artery. In tandem occlusion, the “distal-to-proximal” approach was defined that the mechanical thrombectomy was firstly performed in the intracranial occlusion followed by recanalization of the extracranial occlusion by stenting. After identifying the dominant vertebral artery, a coaxial system with an 8F guiding catheter and 5F diagnostic catheter was generally attempted first to crossed through the occluded segment with a 0.035-inch guide wire (the so-called “Diagnostic-Dotter” technique). If this access through the extracranial occlusion was impossible, the Dilator-Dotter was applied by a straight 6F 90-cm Neuron MAX 088 guiding catheter (Penumbra, Alameda, CA) with the inner dilator and a 0.035-inch guide wire to pass over the extracranial occlusion segment. Mechanical thrombectomy was performed to recanalize the intracranial segments and the successful recanalization was identified by the modified Treatment In Cerebral Infarction (mTICI ≥ 2b). After that, the 8F guiding catheter was pulled in the ipsilateral subclavian artery and a loading dose of dual antiplatelet therapy (300 mg clopidogrel and 162 mg aspirin) was used via nasogastric tube. 8 The placement of balloon-expandable stent was in the extracranial lesion. 9 After the procedure, a head CT scan or MRI was performed to determine complications: malignant cerebellar edema and intracranial hemorrhage. If the results of neuroimaging were negative, dual antiplatelet therapy (75 mg clopidogrel and 100 mg aspirin) was taken orally daily. Informed consent was obtained from all patient representatives after detailed explanation about the procedures. Our study has followed the STROBE guidelines.
Outcomes
At 3 months, the primary endpoint was the good clinical outcome assessed by applying the mRS (mRS ≤ 2). The favorable outcome comprised of good and moderate outcome (mRS 3). These scores were evaluated through telephone interviews (Figure 1).
Statistical analyses
All statistical analyses were carried out using Stata statistical software, version 17 (StataCorp LLC, Texas, USA). Statistical significance for intergroup differences was assessed with Fisher exact test for categorical variables. All tests were two sided with p < 0.05 considered to be statistically significant.
Results
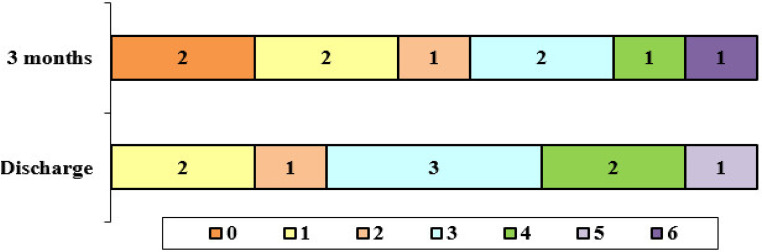
From December 2020 to January 2024, 9 eligible cases (8 men and 1 woman, mean age 65.8 ± 15.3 years) with acute posterior tandem occlusions were treated by rescue stent extracranial vertebral stenting and mechanical thrombectomy at our hospital. Median NIHSS score at admission was 15.6 ± 4.9 (range 10 to 22). Overall, the median time from symptom onset to hospital arrival was 4.8 ± 1.3 h and the median door-to-groin puncture time was 167.6 ± 138.6 min. Although smoking was identified in 88.9% of patients, only 33.3% of patients had poor outcome (Table 2). In 9 cases, 7 occlusive lesions were visible after the angiography. As shown in Table 1, 8 patients were treated with aspiration alone in intracranial occlusion and 1 case involved the embolic protection devices (EPDs) after mechanical thrombectomy. All of patients were achieved successful recanalization (mTICI ≥ 2b). Sample case was shown in Figure 2. Diagnostic-Dotter technique was used in 6 of 9 (66.7%) cases and Dilator-Dotter technique was in 3 of 9 (33.3%) cases. Besides, no significant difference between the Dotter techniques were found in poor outcome at 3 months (p = 0.5, Table 2). Follow-up MRI obtained after procedure showed 1 malignant cerebellar edema case, who was immediately performed by surgical decompression. Average length of stay in Intensive Care Unit (ICU) was 5 ± 3.8 days (range, 2–14 days), whereas mean length of stay in hospital was 11.8 ± 6.4 (range, 7–28 days). At 3 months follow-up, 5 patients (55.6%) had a good outcome (mRS ≤ 2), 1 (11.1%) had a moderate outcome (mRS 3), and 3 (33.3%) had a poor outcome (mRS ≥ 4) (Figure 3). Mortality was 11.1% (Table 1).
Table 2.
Association of main characteristics with clinical outcomes at 3-month.
| Baseline characteristics | Favorable Outcome (n = 6) | Poor Outcome (n = 3) | p |
|---|---|---|---|
| Age ≥ 70 years, n (%) | 2 (22.2%) | 1 (11.1%) | 1 |
| Male sex, n (%) | 5 (55.6%) | 3 (33.3%) | 1 |
| Smoking, n (%) | 5 (55.6%) | 3 (33.3%) | 1 |
| Onset time < 6 h, n (%) | 4 (44.4%) | 2 (22.2%) | 1 |
| NIHSS ≥ 16, n (%) | 2 (22.2%) | 2 (22.2%) | 0.5 |
| Left side, n (%) | 5 (55.6%) | 1 (11.1%) | 0.2 |
| pc-ASPECTS ≥ 8, n (%) | 3 (33.3%) | 0 | 0.5 |
| Procedural time > 60 min, n (%) | 3 (33.3%) | 3 (33.3%) | 0.5 |
| Dilator-Dotter technique, n (%) | 3 (33.3%) | 0 | 0.5 |
| Sedation after procedure, n (%) | 1 (11.1%) | 2 (22.2%) | 0.2 |
| Length of stay in ICU < 6 days, n (%) | 5 (55.6%) | 2 (22.2%) | 1 |
| Length of hospital stay < 14 days, n (%) | 5 (55.6%) | 2 (22.2%) | 1 |
Table 1.
Baseline characteristics of patients with rescue extracranial vertebral stenting.
| Patient characteristics | Rescue stenting (N = 9) |
|---|---|
| Age in year, mean (SD) | 65.8 (15.3) |
| Male sex, n (%) | 8 (88.9) |
| Smoking, n (%) | 8 (88.9) |
| Admission NIHSS, mean (SD) | 15.6 (4.9) |
| Onset-to-door time in hours, mean (SD) | 4.8 (1.3) |
| Door-to-groin puncture time in minutes, mean (SD) | 167.6 (138.6) |
| pc-ASPECTS, mean (SD) | 6.9 (0.9) |
| Occlusive lesion, n (%) | 7 (77.8) |
| Procedural time in minute, mean (SD) | 88.9 (47.1) |
| Procedural time > 60 min, n (%) | 6 (66.7) |
| Aspiration only, n (%) | 8 (88.9) |
| EPD, n (%) | 1 (11.1) |
| Diagnostic-Dotter technique, n (%) | 6 (66.7) |
| Sedation after procedure, n (%) | 3 (33.3) |
| Malignant cerebellar edema, n (%) | 1 (11.1) |
| Surgical decompression, n (%) | 1 (11.1) |
| Length of stay in ICU in days, mean (SD) | 5 (3.8) |
| Length of hospital stay in days, mean (SD) | 11.8 (6.4) |
| Stroke rehabilitation, n (%) | 5 (55.6) |
| Good outcome, n (%) | 5 (55.6) |
| Mortality, n (%) | 1 (11.1) |
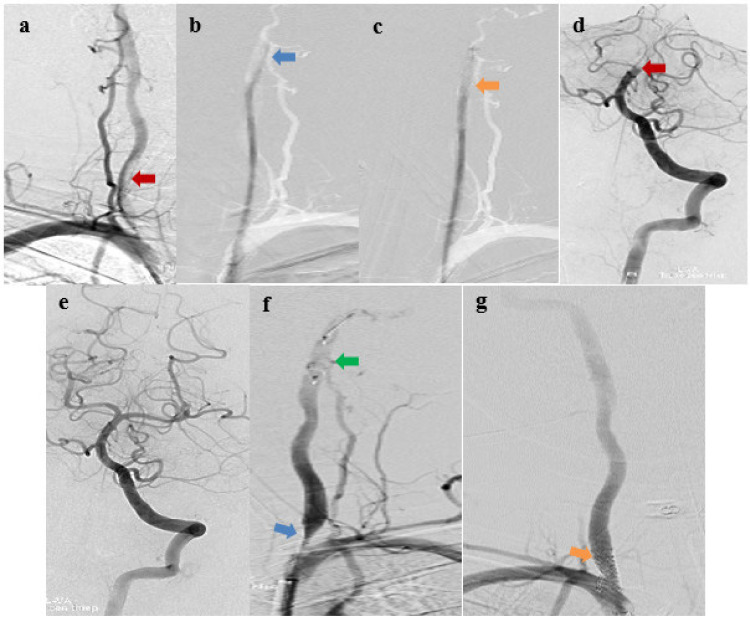
Figure 2.
Sample case: a) Extracranial vertebral artery occlusion (red arrow); b) the 5F diagnostic catheter selected through occlusion (blue arrow); c) the coaxial system with an 8F guiding catheter and 5F diagnostic catheter attempted to crossed through the occluded segment (orange arrow); d) Occlusion of top basilar artery (red arrow); e) Intracranial restoration after aspiration; f) Severe stenosis extracranial vertebral artery (blue arrow) and embolic protection devices (EPDs) (green arrow); g) Placement of balloon-expandable stent (Dynamic Renal 5/15; Biotronik AG, Bülach, Switzerland) (orange arrow). The mRS 1 was after 3-month.
Figure 3.
Distributions of the 3-month mRS in rescue extracranial vertebral stenting patients.
Discussion
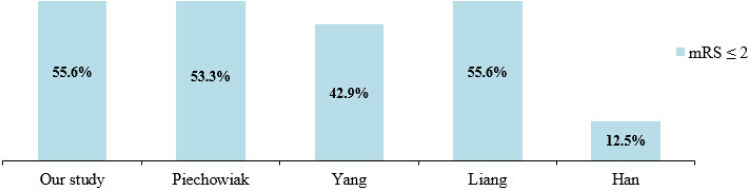
Tandem vertebrobasilar occlusions are the complex lesions of posterior circulation stroke, which made longer procedural time and more risky than the isolated lesions with embolic occlusions. Most studies have documented recanalization of the vertebrobasilar arterial system in tandem occlusions in the posterior circulation through the distal-to-proximal approach technique5–7,10–12 and a few have applied the proximal-to-distal approach.5,13 The proximal-to-distal approach allowed balloon pre-dilation alone or balloon-expandable stent first at extracranial occlusion followed by restoring the intracranial occlusion with mechanical thrombectomy; and the distal-to-proximal approach had the reverse order of steps of the proximal-to-distal one. For the proximal-to-distal approach, advancing the 8F guiding catheter to the V2 segment of vertebral artery through placement of stent before is a substantial challenge and partial angioplasty in stent could allow to advance the guiding catheter to the V2 segment. The careful consideration should be given to choose appropriate technique. However, for the proximal-to-distal approach, there are the following disadvantages: (1) when extracranial stent is placed at the origin of the vertebral artery, the 8F guiding catheter can be only in the subclavian artery, which may affect the process of inserting the devices to recanalize the intracranial occlusions; (2) early restoration of blood flow of vertebral artery may increase the risk of migration of residual thrombus to distal segments; (3) influence on the stability of the stent during mechanical thrombectomy in intracranial segments. That is the reason why our study, Han, 7 Xing, 10 and Liang 14 all prioritize the distal-to-proximal approach. In order to advance the guiding catheter through the extracranial lesions, Xing 10 and Liang 14 chose the temporary angioplasty, whereas Han et al. 7 only chose the Dilator-Dotter technique which used the coaxial of a straight 6F 90-cm Neuron MAX 088 guiding catheter (Penumbra, Alameda, CA) with the inner dilator. Dilator-Dotter technique supported the coaxial system be stronger to go through extracranial occlusion after the determination the true lumen with 4F MPA catheter (Cordis, Miami Lakes). 7 In our study, the Diagnostic-Dotter technique (6 cases) was performed more than the Dilator-Dotter one because the 5F diagnostic catheter had clearer radiopaque part and softer than the dilator. These reasons showed the 8F guiding catheter passed through the occlusion effectively and safely. None of procedural complications (vessel perforation, dissection, thromboembolism, …) recorded. This result was similar to the study of Cohen, 5 Han, 7 Yang, 13 and Liang, 14 whereas Piechowiak et al. 11 recorded 2 cases (13.3%) of vertebral artery dissection due to excessive advance of the 8F guiding catheter through the extracranial lesion, but no specific treatment was required. In our study, the rate of good outcomes after 3 months was 55.6% (Table 1), was similar to the study of Liang 14 and more than the previous studies7,11,13 (Figure 4) and no significant difference was recorded. Although 1 case with malignant cerebellar infarction was performed by decompressive craniotomy, the clinical outcome improved mRS 3 after 3 months and aspirin 81 mg was taken orally daily.
Figure 4.
Comparison of good outcomes (mRS ≤ 2) at 3 months between relevant studies.
Although our study had several limitations with a relatively small sample size and retrospective data at a single center, it provided essential data to suggest the approaches in tandem vertebrobasilar occlusions.
Conclusions
In summary, this study showed high recanalization and favorable clinical outcome rate can be improved with rescue extracranial vertebral stenting for the acute posterior tandem occlusion. Further randomized trials are needed to confirm these results.
Acknowledgments
We would like to acknowledge our colleagues at Can Tho S.I.S General Hospital and Can Tho University of Medicine and Pharmacy for their wonderful collaboration. We would like to thank our supervisors: Assoc.Prof.PhD.MD. Dinh Nguyen Hoang, Assoc.Prof.PhD.MD. Nam Nguyen Hoai, and PhD.MD. Luan Tran Minh Bao at the Department of Cardiovascular Surgery - University of Medicine and Pharmacy at Ho Chi Minh City, whose expertise were invaluable in formulating the methodology.
Footnotes
Author contributions: TLM, CTC, and GNL handled the conceptualization of the study. TLM, CTC, and TNT did the data curation of the study. TLM, CTC, and HNDN conducted the formal analysis of the study. TLM, CTC, and GNL did the investigation on the study. CTC, NNH, DNH, LTMB, and TLM handled the methodology of the study. CTC handled the project administration of the study. TLM, CTC, GNL, HNDN, and LDH handled the resources of the study. TLM and TNT took care of the software of the study. TLM, CTC, GNL, TNT, and LDH supervised the study. TLM, CTC, GNL, and HNDN validated the study. TLM, CTC, and GNL took care of the visualization of the study. TLM, CTC, NNH, DNH, GNL, and LTMB contributed to the writing - original draft of the study. TLM, CTC, NNH, DNH, GNL, and LTMB contributed to the writing - review and editing.
Data availability statement: The data that support the findings of this study are available from the corresponding author upon reasonable request.
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The authors received no financial support for the research, authorship, and/or publication of this article.
Ethics approval: Our study is registered in the ClinicalTrials.gov with ID NCT06365294. The study involving human participants was reviewed and approved by the Ethics Council in biomedical research in Can Tho S.I.S General Hospital (11723/QD-S.I.S) and Ethical Board of the University of Medicine and Pharmacy at Ho Chi Minh City (number 1087/HDDD-DHYD on November 02nd, 2023).
Informed consent: Informed consent was obtained from all patient representatives after detailed explanation about the procedures.
ORCID iD: Thang Le Minh https://orcid.org/0000-0002-3245-6286
References
- 1.Liu X, Dai Q, Ye R, et al. Endovascular treatment versus standard medical treatment for vertebrobasilar artery occlusion (BEST): an open-label, randomised controlled trial. Lancet Neurol 2020; 19: 115–122. pmid: https://pubmed.ncbi.nlm.nih.gov/31831388. [DOI] [PubMed] [Google Scholar]
- 2.Langezaal LCM, van der Hoeven E, Mont'Alverne FJA, et al. “Endovascular therapy for stroke due to basilar-artery occlusion”. N Engl J Med 2021; 384: 1910–1920. pmid: https://pubmed.ncbi.nlm.nih.gov/34010530. [DOI] [PubMed] [Google Scholar]
- 3.Jovin TG, Li C, Wu L, et al. Trial of thrombectomy 6 to 24 hours after stroke due to basilar-artery occlusion. N Engl J Med 2022; 387: 1373–1384. pmid: https://pubmed.ncbi.nlm.nih.gov/36239645. [DOI] [PubMed] [Google Scholar]
- 4.Tao C, Li R, Zhu Y, et al. Endovascular treatment for acute basilar artery occlusion: a multicenter randomized controlled trial (ATTENTION). Int J Stroke 2022; 17: 815–819. pmid: https://pubmed.ncbi.nlm.nih.gov/35102797. [DOI] [PubMed] [Google Scholar]
- 5.Cohen JE, Leker RR, Gomori JM, et al. Emergent revascularization of acute tandem vertebrobasilar occlusions: endovascular approaches and technical considerations-confirming the role of vertebral artery ostium stenosis as a cause of vertebrobasilar stroke. J Clin Neurosci 2016; 34: 70–76. pmid: https://pubmed.ncbi.nlm.nih.gov/27522497. [DOI] [PubMed] [Google Scholar]
- 6.Cox M, Layton K, Hise J. Dilator-Dotter technique for acute ischemic stroke: further applications in the vertebral arteries. AJNR Am J Neuroradiol 2022; 43: E7–E8. pmid: https://pubmed.ncbi.nlm.nih.gov/35210275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Han N, Ma L, Zhao L, et al. The dilator-dotter technique can successfully treat tandem lesions of posterior circulation. Medicine (Baltimore) 2024; 103: e37044. pmid: https://pubmed.ncbi.nlm.nih.gov/38277540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Yahia MI, Marnat G, Finitsis S, et al. Acute carotid stenting plus aspirin during thrombectomy of tandem occlusions: a matched case-control study. Interv Neuroradiol 2023: 159101992311753. pmid: https://pubmed.ncbi.nlm.nih.gov/37229632. [DOI] [PubMed] [Google Scholar]
- 9.Lim J, Baig AA, Aguirre AO, et al. Use of drug-eluting, balloon-expandable resolute onyx coronary stent as a novel treatment strategy for vertebral artery ostial stenosis: case series. Interv Neuroradiol 2022: 159101992211381. pmid: https://pubmed.ncbi.nlm.nih.gov/36357368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Xing P-f, Zhang Y-w, Li Z-f, et al. The “distal-to-proximal” strategy for the treatment of posterior circulation tandem occlusions: a single-centre experience. Neuroradiology 2020; 62: 867–876. pmid: https://pubmed.ncbi.nlm.nih.gov/32242265. [DOI] [PubMed] [Google Scholar]
- 11.Piechowiak EI, Kaesmacher J, Zibold F, et al. Endovascular treatment of tandem occlusions in vertebrobasilar stroke: technical aspects and outcome compared with isolated basilar artery occlusion. J Neurointerv Surg 2020; 12: 25–29. pmid: https://pubmed.ncbi.nlm.nih.gov/31113810. [DOI] [PubMed] [Google Scholar]
- 12.Klail T, Piechowiak EI, Krug N, et al. Endovascular revascularization of vertebrobasilar tandem occlusions in comparison to isolated basilar artery occlusions: a multi-center experience. Interv Neuroradiol 2024: 15910199241240045. pmid: https://pubmed.ncbi.nlm.nih.gov/38576395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Yang H, Ma N, Zhang S, et al. Endovascular revascularisation of acute tandem vertebrobasilar artery occlusion: seven case series with literature reviews. Stroke Vasc Neurol 2018; 3: 17–21. pmid: https://pubmed.ncbi.nlm.nih.gov/29600003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Liang K, Wang B, Zhao L, et al. Management of posterior circulation tandem occlusions in acute ischemic stroke: recanalize the dominant vertebral artery with priority. Interv Neuroradiol 2023; 29: 570–576. pmid: https://pubmed.ncbi.nlm.nih.gov/35876354. [DOI] [PMC free article] [PubMed] [Google Scholar]