Abstract
Background
African Americans have a higher prevalence of cardiovascular risk factors, leading to higher cardiovascular disease mortality than White adults. Our culturally tailored mobile health (mHealth) lifestyle intervention (FAITH! App) has previously demonstrated efficacy in promoting ideal cardiovascular health in African Americans.
Methods
We conducted a secondary analysis from a cluster randomized controlled trial among African-Americans from 16 churches in Minnesota that compared the FAITH! App to a delayed intervention control group. A subgroup of participants with ≥ 1 diagnosis of overweight/obesity, hyperlipidemia, hypertension, or diabetes was examined. The primary outcome was a change in LS7 score—a measure of cardiovascular health ranging from poor to ideal (range 0–14 points)—at 6-months post-intervention.
Results
The analysis included 49 participants (intervention group: n = 20; mean age 58.8 years, 75% female; control group: n = 29, mean age 52.5 years, 76% female) with no significant baseline differences in cardiovascular risk factors. Compared to the control group, the intervention group showed a greater increase in LS7 score across all cardiovascular risk factors at 6-months post-intervention, with statistically significant differences among those with overweight/obesity (intervention effect 1.77, p < 0.0001) and 2+ or 3+ cardiovascular risk factors (1.00, p = 0.03; 1.09, p = 0.04). The intervention group demonstrated a higher increase in the percentage of participants with intermediate or ideal LS7 scores than the control group, although these differences were not statistically significant.
Conclusions
Our culturally tailored mHealth lifestyle intervention was associated with significant increases in LS7 scores among African Americans with preexisting cardiovascular risk factors, suggesting its efficacy in improving cardiovascular health among this population.
Keywords: Cardiovascular health, digital health, mobile health, African Americans, cardiovascular risk factors
Introduction
African-American (AA) adults have the highest prevalence of cardiovascular disease (CVD), with approximately six out of 10 AA adults having some form of CVD. 1 CVD is inclusive of heart and circulatory disease conditions, such as coronary heart disease, stroke, heart failure, hypertension, and peripheral artery disease. 1 There are multifactorial etiologies of CVD including genetic, socioeconomic, behavioral, and environmental risk factors.2,3 The largest genetic study on CVD to date 3 found that many genetic variations linked to increased CVD risk are consistent across all major racial and ethnic groups, underscoring the significant influence of nongenetic factors, such as the social determinants of health (SDOH), in driving disparities in CVD outcomes among racially minoritized populations.2,4 The disproportionate burden of CVD among AAs is driven by high rates of cardiovascular risk factors, such as hypertension, obesity, and diabetes mellitus. 5 These disparities are exacerbated by negative psychosocial factors and SDOH, 2 rooted in racism and structural barriers. The complex interplay of these factors presents barriers to the achievement of ideal cardiovascular health (CVH) among AAs.6,7
In efforts to reduce the CVD burden among Americans, the American Heart Association (AHA) developed the Life's Simple 7 (LS7) as a metric for CVH. 8 This measurement defines CVH according to seven modifiable health behaviors and biometrics including smoking, diet, physical activity, body mass index (BMI), blood pressure, cholesterol, and blood glucose. Substantial evidence has found that improvement in LS7 scores is associated with favorable CVD outcomes for a number of conditions including hypertension, coronary artery disease, heart failure, and atrial fibrillation.9–12 Therefore, interventions capable of increasing LS7 scores, especially among individuals with multiple cardiovascular risk factors, may be pivotal in reducing CVD morbidity and mortality.
Traditional cardiovascular risk factors increase CVD risk independently; thus, individuals with multiple risk factors experience poorer health outcomes (e.g. CVD-related and all-cause mortality) compared to those with only a single risk factor.13–16 Previous studies have reported a higher prevalence of multiple cardiovascular risk factors among AA adults compared to White adults.4,17,18 To address the high prevalence of multiple risk factors among AAs, innovative culturally appropriate interventions targeting multiple risk factors are paramount. Lu et al. developed a predictive model estimating at least a 25% reduction in Black-white CVD disparity through risk-based interventions targeting risk factors, encompassing blood pressure and lipid-lowering medications, smoking cessation, and lifestyle modifications. 19 Digital tools, such as mobile apps, are highly scalable and adaptable, rendering them ideal for tackling more than one risk factor at a time. More importantly, smartphone penetration among AAs is high and the use of mobile devices to access health information is increasing.20–22 However, there is a paucity of culturally tailored mobile health (mHealth) interventions to address cardiovascular risk factors among AAs. In addition, the limited studied interventions focus on a single risk factor. In a single-arm pretest-posttest study, Joseph et al. 23 reported that a 4-month smartphone app-based intervention increased moderate-to-vigorous physical activity in AA women aged 50–65 years. Similarly, another study among adult AA women from resource-limited neighborhoods in the Washington, D.C. metropolitan area found that a digital health app using place-tailored messaging was associated with increased PA, although these findings were not statistically significant. 24 To address this gap, we employed a community-based participatory research approach to co-design the FAITH! App, an mHealth lifestyle intervention targeting multiple cardiovascular risk factors, with input from the AA community in Rochester and Minneapolis-St Paul (MSP) metropolitan areas in Minnesota.25–27 The app was rigorously tested within a 10-week randomized controlled trial (RCT) among AA adults (FAITH! Trial) comparing an immediate intervention group to a delayed intervention control group. Our preliminary findings suggested that the FAITH! App was an efficacious mHealth tool to promote ideal CVH among AAs. 28
This study aimed to assess the efficacy of the FAITH! App in improving CVH by conducting a secondary analysis of a subset of participants with preexisting cardiovascular risk factors. We hypothesized that the intervention group with preexisting cardiovascular risk factors would have a greater increase in LS7 scores than the control group with the same risk factors following the use of the FAITH! App.
Methods
Participant screening and eligibility
The parent study was conducted within predominantly AA congregations in the Rochester and MSP areas, Minnesota. AA churches were selected for their longstanding, pivotal role in health promotion within AA and marginalized communities. 29 Additionally, a nationally representative study found that 81% of AAs attend church, making AA churches ideal for participant recruitment. 30 Moreover, our longstanding academic-community partnership through community-based participatory research (CBPR) with the AA faith community underscores the intentional recruitment of participants from AA churches. We prioritized this community due to its disproportionately high burden of CVD risk. 1 It is important to highlight the collaborative co-design of the FAITH! App with the AA faith community contributed to the culturally relevant, faith-based nature of key intervention features (e.g. biblical tenets within education modules). The study recruitment and design have been detailed elsewhere.25,28 Briefly, participant recruitment for the FAITH! Trial occurred between December 2019 and October 2020. Participants meeting the following criteria were eligible to participate in the study: self-identification as AA, age 18 years or older, ownership of a smartphone (iOS or Android), have basic Internet skills, have access to the Internet at least weekly, have an active email address, consume fewer than five servings of fruits/vegetables daily, engage in < 30 minutes of daily physical activity, and capable of participating in moderate-intensity physical activity. Eligible participants provided electronic informed consent and received a $50 gift card at baseline and 6-months post-intervention health assessments, along with a Fitbit™ (Fitbit Inc./Google, San Francisco, CA) wearable as incentives. This study obtained approval from the Mayo Clinic Institutional Review Board (REC number: 18-006846).
Randomization and intervention
Participants in the parent study were randomized to the intervention and delayed intervention control group via clusters of churches in Rochester and MSP. 31 The intervention spanned 10 weeks and comprised culturally relevant modules focused on CVH, self-monitoring of diet and physical activity, and a group sharing board. At baseline, participants selected a lifestyle path, either focusing on dietary or physical activity behaviors. This choice determined the primary content of decision rule-based messages, encompassing CVH (LS7) information, cues to action, reminders, as well as motivational and encouraging messages for promoting healthy behavior change. Throughout the intervention, participants engaged with one educational module per week, featuring interactive self-assessments. Participants manually recorded their daily fruit and vegetable servings using the tracking feature within the FAITH! App. Physical activity data were automatically synchronized into the app from Fitbit™ wearable devices provided by the study team. Furthermore, participants were encouraged to post in a moderated sharing board in the app which received weekly updates featuring content from reputable sources such as the AHA and Mayo Clinic.
Study measurements
Demographics, lifestyle behaviors, and medical history were collected via electronic surveys conducted at baseline and 6-months post-intervention. To collect clinical, laboratory, and anthropometric data, in-person health assessments were conducted at baseline (October to November 2020) and 6-months post-intervention at community health centers by a mobile clinical research unit team of trained nursing personnel. Participant CVH was assessed using the AHA LS7 score. As per the AHA quantification algorithm, 8 each of the seven components of the LS7 score was assigned a score of 0, 1, or 2 points (equivalent to poor, intermediate, and ideal CVH, respectively) to obtain a composite score ranging from 0 to 14 points. Composite LS7 scores were categorized into poor (0–4), intermediate (5–9), and ideal (10–14).
Outcomes
The primary outcome in the current analysis was a change in mean LS7 score from baseline to 6-months post-intervention. The secondary outcome was a change in the percentage of participants with intermediate or ideal LS7 scores from baseline to 6-months post-intervention. The percentage of participants achieving intermediate or ideal LS7 scores was assessed to detect improvements across LS7 categories (from poor to intermediate and intermediate to ideal), with the intermediate/ideal categories aggregated due to the limited sample size.
Statistical methods
A total of 85 individuals participated in the RCT of which 41 were randomly assigned to the intervention and 44 to the control group. The secondary analysis included a subset of these participants (n = 49) with ≥ 1 diagnosis of overweight/obesity, hyperlipidemia, hypertension, or diabetes at baseline. Categorical variables (e.g. sex) were summarized as percentages while continuous variables (e.g. LS7 scores) were summarized with means and standard deviations (SD). Categorical variables were compared using the chi-square test. Normally distributed continuous variables were compared using two-sample t-tests, whereas non-normally distributed continuous or ordinal variables were assessed using Wilcoxon rank-sum tests. The within-group and between-group differences from baseline to 6-months post-intervention for the LS7 score were assessed using linear regression models incorporating generalized estimating equations (GEEs) to account for within-church correlation. 28 The intervention effect was defined as the difference in average change from baseline to 6 months between the intervention and control groups. To assess the secondary outcome (change in percentage of participants with intermediate or ideal LS7 scores 6-months post-intervention), the difference in LS7 category from baseline to 6-months post-intervention were assessed using McNemar's tests (within-group) and logistic regression models (between-group). All analyses were performed using SAS version 9.4 (SAS Institute Inc, Cary, NC). P values < 0.05 were considered statistically significant.
Results
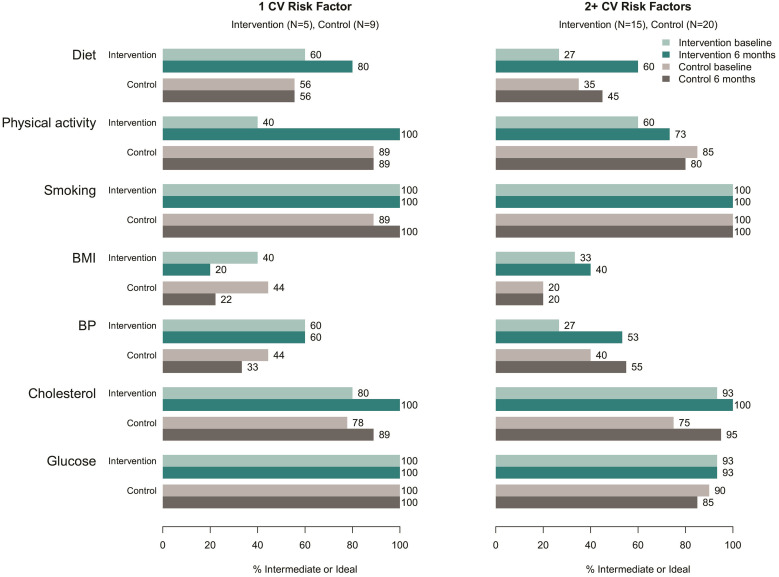
The sample for the current analysis included 49 participants (75.5% female) enrolled in either the intervention group (n = 20; mean age [SD]: 58.8 [9.5] years) or control group (n = 29, mean age [SD]: 52.5 [10.7] years). The intervention group was slightly older (p = 0.04) (Table 1). At baseline, no significant difference was observed in the prevalence of cardiovascular risk factors between the two groups. Overall, there were improved LS7 scores at the 6-month post-intervention timepoint within the intervention group compared to the control group across all cardiovascular risk factors. However, the difference in the change of LS7 scores was only statistically significant among participants with overweight/obesity (intervention effect 1.77, p < 0.001). Importantly, among participants with multiple cardiovascular risk factors, the intervention yielded a significant effect among those with three or more risk factors as well as for those with two or more risk factors (1.09, p = 0.04; 1.00, p = 0.03). Furthermore, compared to the control group, the increase in the percentage of participants achieving intermediate or ideal LS7 scores in the intervention group was higher within each participant subgroup of cardiovascular risk factors (overweight/obesity [+31.2% vs. −4.4%], hyperlipidemia [+36.3% vs. +6.7%], hypertension [+21.4% vs. 0%], diabetes [+22.3% vs. 0%], and those with least two [+26.7% vs. −5.0%] and three cardiovascular risk factors [+36.3% vs. 0%]). Nonetheless, there was insufficient statistical power to detect these differences as significant. The percentage of participants in the intervention group achieving an intermediate or ideal diet LS7 score increased significantly from baseline to 6 months (26.7% vs. 60.0%, p = 0.03). There were no additional statistically significant differences noted for any other LS7 component either within group or between groups (Figure 1, Supplemental Table 1).
Table 1.
Change in life's simple 7 (LS7) scores by cardiovascular risk factors, baseline to 6-months post-intervention.
| Intervention (N = 20) |
Control (N = 29) |
Intervention effect a | p-value | |
|---|---|---|---|---|
| Mean (SD) | Effect estimate (95% CI) | |||
| Demographic characteristics | ||||
| Age, years | 58.8 (9.5) | 52.5 (10.7) | 0.04 | |
| Sex, n (%) | 0.95 | |||
| Male | 5 (25.0) | 7 (24.1) | ||
| Female | 15 (75.0) | 22 (75.9) | ||
| Cardiovascular (CV) risk factors | ||||
| Overweight/obesity | ||||
| n (%) | 16 (80.0) | 23 (79.3) | 0.95 | |
| LS7 score at baseline | 5.94 (1.81) | 6.83 (1.85) | ||
| LS7 score at 6 months | 8.19 (2.04) | 7.30 (2.03) | ||
| ΔLS7 score | +2.25 (1.69) | +0.48 (1.83) | 1.77 (1.16, 2.38) | <0.001 |
| Within-group p-value | 0.06 | 0.71 | ||
| Δ% intermediate/ideal LS72 | +31.2 | −4.4 | ||
| Hyperlipidemia | ||||
| n (%) | 11 (55.0) | 15 (51.7) | 0.82 | |
| LS7 score at baseline | 5.36 (1.69) | 6.40 (1.88) | ||
| LS7 score at 6 months | 7.27 (1.85) | 7.60 (1.99) | ||
| ΔLS7 score | +1.91 (1.81) | +1.20 (1.70) | 0.71 (−0.44, 1.86) | 0.23 |
| Within-group p-value | 0.10 | 0.71 | ||
| Δ% intermediate/ideal LS7 b | +36.3 | +6.7 | ||
| Hypertension | ||||
| n (%) | 14 (70.0) | 21 (72.4) | 0.85 | |
| LS7 score at baseline | 5.93 (1.90) | 6.71 (1.90) | ||
| LS7 score at 6 months | 7.71 (1.94) | 7.71 (2.19) | ||
| ΔLS7 score | +1.79 (1.81) | +1.00 (1.52) | 0.79 (−0.03, 1.61) | 0.06 |
| Within-group p-value | 0.26 | 1.0 | ||
| Δ% intermediate/ideal LS7 b | +21.4 | 0.0 | ||
| Diabetes | ||||
| n (%) | 9 (45.0) | 6 (20.7) | 0.07 | |
| LS7 score at baseline | 5.33 (1.66) | 5.67 (2.66) | ||
| LS7 score at 6 months | 7.11 (1.76) | 6.50 (2.95) | ||
| ΔLS7 score | +1.78 (2.22) | +0.83 (1.60) | 0.94 (−0.62, 2.51) | 0.24 |
| Within-group p-value | 0.41 | 1.0 | ||
| Δ% intermediate/ideal LS7 b | +22.3 | 0.0 | ||
| Total CV risk factors, n (%) | ||||
| One preexisting risk factor | 5 (25.0) | 9 (31.0) | 0.41 | |
| Two preexisting risk factors | 4 (20.0) | 9 (31.0) | ||
| Three preexisting risk factors | 7 (35.0) | 6 (20.7) | ||
| Four preexisting risk factors | 4 (20.0) | 5 (17.2) | ||
| 2+ CV risk factors c | ||||
| LS7 score at baseline | 5.80 (1.78) | 6.60 (1.76) | ||
| LS7 score at 6 months | 7.60 (1.84) | 7.40 (2.11) | ||
| ΔLS7 score | +1.80 (1.82) | +0.80 (1.74) | 1.00 (0.09, 1.91) | 0.03 |
| Within-group p-value | 0.16 | 0.71 | ||
| Δ% intermediate/ideal LS7 b | +26.7 | −5.0 | ||
| 3+ CV risk factors d | ||||
| LS7 score at baseline | 5.36 (1.69) | 6.18 (2.04) | ||
| LS7 score at 6 months | 7.36 (1.91) | 7.09 (2.47) | ||
| ΔLS7 score | +2.00 (1.79) | +0.91 (1.76) | 1.09 (0.04, 2.14) | 0.04 |
| Within-group p-value | 0.10 | 1.0 | ||
| Δ% intermediate/ideal LS7 b | +36.3 | 0.0 | ||
Difference in mean change between intervention and control groups.
Difference in the percentage of participants with intermediate or ideal LS7 from baseline to 6 months. There were no significant within-group or between-group differences in % intermediate/ideal.
Participants with at least two of the four preexisting cardiovascular risk factors (N = 15 [intervention]; N = 20 [control]).
Participants with at least three of the four preexisting cardiovascular risk factors (N = 11 [intervention]; N = 11[control]).
Figure 1.
Comparison in a change in individual life's simple 7 (LS7) scores between participants with 1 and ≥ 2 cardiovascular risk factors, baseline to 6-months post-intervention.
Discussion
In this study of predominantly AA women with preexisting cardiovascular risk factors, a culturally tailored mHealth intervention promoting CVH resulted in significant improvements in composite LS7 scores at 6-months post-intervention, particularly among those with overweight/obesity or ≥ 2 cardiovascular risk factors. More importantly, the improvement in CVH was maintained among participants with ≥ 3 preexisting risk factors. Also, participants in the intervention group across participant subgroups (i.e. overweight/obesity, hypertension, hyperlipidemia, diabetes, and ≥ 2 or 3 cardiovascular risk factors) had greater attainment of intermediate/ideal CVH status than the control group. However, within the subgroups of participants categorized by the prevalence of cardiovascular risk factors, no differences in the percentage of participants achieving intermediate/ideal composite or component LS7 scores were observed between the intervention and control groups. These findings suggest that the FAITH! App intervention is efficacious in improving CVH in both AAs with and without 28 preexisting cardiovascular risk factors and may be more beneficial to those with multiple risk factors.
There is a varied distribution of cardiovascular risk factors among AA adults, with some individuals exhibiting a diverse or higher number of risk factors than others.17,32 Consequently, within this population, digital health interventions aimed at improving CVH may produce different effects among individuals, based on the prevalent individual cardiovascular risk factors and the overall magnitude of combined CVD risk. Therefore, not stratifying the impact of these innovative interventions by CVD risk profile may obscure their potential benefits or ineffectiveness in individuals with certain CVD risks. This could lead to missed opportunities to tailor cardiovascular interventions for those who may stand to gain the most. Moreover, AA adults have a disproportionately higher prevalence of cardiovascular risk factors compared to the general US population. 18 Failing to ascertain whether these innovative interventions have a positive or negative impact on this demographic could exacerbate existing disparities in CVD outcomes. These findings underscore the necessity for cardiovascular interventions that are not only culturally sensitive but also tailored to individual CVD risk profiles, with the aim of addressing inequities in CVH and CVD outcomes.16,33,34
Our study indicates varying degrees of CVH improvement based on specific risk factors. The substantial improvement in LS7 scores observed in participants with overweight/obesity may be attributed to a number of factors. First, the FAITH! App targeted behavioral modifications related to diet and physical activity, both of which are closely linked to body weight.35,36 This suggests that psychosocial factors motivating participants with overweight/obesity to improve CVH may have prompted behavioral shifts leading to improved LS7 scores in this subgroup. Additionally, the features of the FAITH! App may unintentionally be more effective in improving CVH among individuals with overweight/obesity compared to those with other risk factors. Our previous study found that the FAITH! App improved diet and physical activity significantly. 28 Analysis assessing differential changes in individual LS7 component scores could offer further insights into the intervention effect.
Digital health interventions are likely to become ubiquitous in cardiovascular care as healthcare systems adopt telemedicine in clinical care.37,38 This study underscores the importance of tailoring digital health solutions to individual patient needs and their cardiovascular risk profiles to enhance the quality of care.34,39,40 Our study suggests that digital health interventions targeting multiple cardiovascular risk factors could result in greater improvements in CVH among individuals with higher CVD risk profiles. However, it is crucial to strike a balance in designing these interventions, avoiding an excessive feature load that could lead to user fatigue and hinder long-term app engagement and retention. Additionally, the inclusion of numerous features may increase app development costs, potentially limiting intervention implementation and dissemination during the commercialization stage.41–43 Constrained dissemination of such interventions may contribute to a decreased adoption of health technologies, thereby exacerbating the prevailing digital divide among marginalized individuals.38,44 Therefore, future studies should assess the impact of providing digital access and literacy support to patients on the efficacy of digital interventions. Our forthcoming clinical trial will evaluate this hypothesis through the use of FAITH! App and digital health advocates among a larger group of AAs.
Moreover, these findings have significant implications for the AA community. The high prevalence of cardiovascular risk factors in AA communities results from a complex interplay of socioeconomic, psychosocial, and structural barriers. 2 Therefore, tailored mHealth interventions that address multiple cardiovascular risk factors simultaneously can potentially improve CVH and CVD outcomes effectively, and, ultimately, reduce the existing disparities. Additionally, the historical mistrust of healthcare systems within AA communities can hinder the impact of innovative digital health interventions in clinical settings. Co-designing culturally tailored interventions with racially minoritized communities, such as AAs, can enhance engagement by fostering trust and relevance; thus, potentially increasing their effectiveness.45,46 These interventions can be scaled by integrating them into existing community health programs led by community-based organizations that have established longstanding trust within AA communities.
Strengths and limitations
One strength of our study is that it is one of the first to assess the efficacy of an mHealth intervention in improving CVH among AA adults with multiple cardiovascular risk factors. Another strength lies in its study design; the culturally tailored mHealth intervention was community-informed via a rigorous formative evaluation of the FAITH! App ensuring that the intervention met community needs. Moreover, the selection of participants for this study involved a random assignment of churches to both the intervention and control groups. The major limitation is that our study was a secondary analysis of existing data and included a small subset of participants. As such, findings are considered preliminary, and future prospective studies are needed with larger sample sizes. The sample predominantly comprised AA women, which may limit the generalizability of our findings to AA men. An overrepresentation of women in the study sample was expected due to recruitment from the AA church community, where participation rates among AA men are typically lower. 30 Moreover, the study sample was drawn from AA churches; thus, there is potential for bias due to the exclusion of participants from other religious affiliations. However, the potential bias in the findings is likely to be minimized by the fact that the majority of AAs in AA communities attend AA churches. 30 Furthermore, the prevalence of cardiovascular risk factors among the study participants is similar to that of the general AA population in Minnesota, indicating that this study sample is representative of the AA community in the state. 47 While our study assessed the change in individual LS7 scores, statistically significant differences were solely observed in the diet component of CVH. We hypothesize that a limited sample size may have contributed to the inability to demonstrate improvement in other CVH components; thus, larger studies focusing on stratified CVH enhancements by components are warranted. Additionally, our analysis is limited to a 6-month post-intervention period, restricting the assessment of long-term efficacy for the FAITH! App in improving CVH. Lastly, this study did not examine psychosocial factors (e.g., diet and physical activity self-efficacy), which could potentially mediate the intervention effect on CVH improvement. Further studies examining potential psychosocial mechanisms linking digital interventions and enhanced CVH are warranted.
Conclusions
Our culturally tailored mHealth lifestyle intervention was associated with noteworthy increases in LS7 scores among AAs with preexisting cardiovascular risk factors, suggesting its efficacy in improving CVH among this population. These findings provide insights for informing the development of innovative culturally tailored digital technological tools aimed at enhancing patient health and the overall healthcare experience in community-based and clinical settings.
Supplemental Material
Supplemental material, sj-docx-1-dhj-10.1177_20552076241295305 for Efficacy of a culturally tailored mobile health lifestyle intervention on cardiovascular health among African Americans with preexisting risk factors: The FAITH! Trial by Mathias Lalika, Sarah Jenkins, Sharonne N Hayes, Clarence Jones, Lora E Burke, Lisa A Cooper, Christi A Patten and LaPrincess C Brewer in DIGITAL HEALTH
Acknowledgements
The authors extend their gratitude to study participants, partnering churches, and FAITH! Study team members for their contributions. Special thanks to the Mayo Clinic Clinical Research and Trials Unit, Mayo Clinic Dan Abraham Healthy Living Center, and Mayo Clinic Square Sports Medicine for their support in planning and study implementation. Appreciation goes to Jeff Gansen for video production, Nic Breutzman for graphic design, and the FAITH! Community Steering Committee for their guidance. Preliminary findings of this study were presented as an abstract at the 2023 American Heart Association (AHA) EPI|Lifestyle Scientific Sessions in Boston, Massachusetts, and the 2023 AHA Scientific Sessions in Chicago, Illinois (Best of AHA Specialty Conferences recognition).
Appendix
- AA
African-American
- AHA
American Heart Association
- BMI
body mass index
- CBPR
community-based participatory research
- CVD
cardiovascular disease
- CVH
cardiovascular health
- FAITH!
Fostering African-American Improvement in Total Health!
- GEE
generalized estimating equations
- LS7
Life's Simple 7
- mHealth
mobile health
- MSP
Minneapolis-St Paul
- PA
physical activity
- RCT
randomized controlled trial
- SD
standard deviation
- SDOH
social determinants of health
Footnotes
Contributorship: LCB, LEB, LAC, SNH, CJ, ML, and CAP were involved in the study conception and design. LCB, LEB, LAC, SNH, SJ, CJ, ML, and CAP were involved in data analysis, data interpretation, and drafting of the manuscript.
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Ethical approval: The Mayo Clinic Institutional Review Board approved this study (REC number: 18-006846).
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This work was supported by the Mayo Clinic Center for Health Equity and Community Engagement in Research, Centers for Disease Control and Prevention Foundation, National Center for Advancing Translational Sciences, National Institutes of Health/National Institute on Minority Health and Health Disparities, American Heart Association Amos Medical Faculty Development Program (grant numbers UL1 TR000135, CDC-DP18-1817, KL2 TR002379, 1 R21 MD013490-01, and 19AMFDP35040005).
Guarantor: LCB.
ORCID iDs: Sharonne N Hayes https://orcid.org/0000-0003-3129-362X
LaPrincess C Brewer https://orcid.org/0000-0002-6468-9324
Supplemental material: Supplemental material for this article is available online.
References
- 1.Martin SS, Aday AW, Almarzooq ZI, et al. 2024 heart disease and stroke statistics: a report of US and global data from the American Heart Association. Circulation 2024; 149: e347–e913. [DOI] [PubMed] [Google Scholar]
- 2.Powell-Wiley TM, Baumer Y, Baah FO, et al. Social determinants of cardiovascular disease. Circ Res 2022; 130: 782–799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Tcheandjieu C, Zhu X, Hilliard AT, et al. Large-scale genome-wide association study of coronary artery disease in genetically diverse populations. Nat Med 2022; 28: 1679–1692. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.He J, Zhu Z, Bundy JD, et al. Trends in cardiovascular risk factors in US adults by race and ethnicity and socioeconomic status, 1999–2018. Jama 2021; 326: 1286–1298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lloyd-Jones DM, Ning H, Labarthe D, et al. Status of cardiovascular health in US adults and children using the American Heart Association's new “Life's Essential 8” metrics: prevalence estimates from the National Health and Nutrition Examination Survey (NHANES), 2013 through 2018. Circulation 2022; 146: 822–835. [DOI] [PubMed] [Google Scholar]
- 6.Lloyd-Jones DM, Allen NB, Anderson CAM, et al. Life's essential 8: updating and enhancing the American Heart Association's Construct of Cardiovascular Health: a presidential advisory from the American Heart Association. Circulation 2022; 146: e18–e43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Shah NS, Huang X, Petito LC, et al. Social and psychosocial determinants of racial and ethnic differences in cardiovascular health in the United States population. Circulation 2023; 147: 190–200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lloyd-Jones DM, Hong Y, Labarthe D, et al. Defining and setting national goals for cardiovascular health promotion and disease reduction: the American Heart Association's strategic impact goal through 2020 and beyond. Circulation 2010; 121: 586–613. [DOI] [PubMed] [Google Scholar]
- 9.Hasbani NR, Ligthart S, Brown MR, et al. American Heart Association's Life's Simple 7: lifestyle recommendations, polygenic risk, and lifetime risk of coronary heart disease. Circulation 2022; 145: 808–818. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Plante TB, Koh I, Judd SE, et al. Life's simple 7 and incident hypertension: the REGARDS study. J Am Heart Assoc 2020; 9: e016482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ogunmoroti O, Michos ED, Aronis KN, et al. Life's simple 7 and the risk of atrial fibrillation: the multi-ethnic study of atherosclerosis. Atherosclerosis 2018; 275: 174–181. [DOI] [PubMed] [Google Scholar]
- 12.Spahillari A, Talegawkar S, Correa A, et al. Ideal cardiovascular health, cardiovascular remodeling, and heart failure in Blacks: the Jackson heart study. Circ Heart Fail 2017; 10(2): e003682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Yamada-Harada M, Fujihara K, Osawa T, et al. Relationship between number of multiple risk factors and coronary artery disease risk with and without diabetes mellitus. J Clin Endocrinol Metab 2019; 104: 5084–5090. [DOI] [PubMed] [Google Scholar]
- 14.Popa LE, Petresc B, Cătană C, et al. Association between cardiovascular risk factors and coronary artery disease assessed using CAD-RADS classification: a cross-sectional study in Romanian population. BMJ Open 2020; 10: e031799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Di Angelantonio E, Kaptoge S, Wormser D, et al. Association of cardiometabolic multimorbidity with mortality. Jama 2015; 314: 52–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ndumele CE, Rangaswami J, Chow SL, et al. Cardiovascular-kidney-metabolic health: a presidential advisory from the American Heart Association. Circulation 2023; 148: 1606–1635. [DOI] [PubMed] [Google Scholar]
- 17.Baruth M, Wilcox S, Egan BM, et al. Cardiovascular disease risk factor clustering among African American adults. Ethn Dis 2011; 21: 129–134. [PMC free article] [PubMed] [Google Scholar]
- 18.Lopez-Neyman SM, Davis K, Zohoori N, et al. Racial disparities and prevalence of cardiovascular disease risk factors, cardiometabolic risk factors, and cardiovascular health metrics among US adults: NHANES 2011–2018. Sci Rep 2022; 12: 19475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lu Y, Ezzati M, Rimm EB, et al. Sick populations and sick subpopulations: reducing disparities in cardiovascular disease between blacks and whites in the United States. Circulation 2016; 134: 472–485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Burke LE, Ma J, Azar KM, et al. Current science on consumer use of mobile health for cardiovascular disease prevention: a scientific statement from the American Heart Association. Circulation 2015; 132: 1157–1213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Pew Research Center. Home broadband adoption, computer ownership vary by race, ethnicity in the U.S., https://www.pewresearch.org/short-reads/2021/07/16/home-broadband-adoption-computer-ownership-vary-by-race-ethnicity-in-the-u-s/ (2021, accessed January 23, 2024).
- 22.Mahmood A, Kedia S, Wyant DK, et al. Use of mobile health applications for health-promoting behavior among individuals with chronic medical conditions. Digit Health 2019; 5: 2055207619882181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Joseph RP, Ainsworth BE, Hollingshead K, et al. Results of a culturally tailored smartphone-delivered physical activity intervention among midlife African American women: feasibility trial. JMIR Mhealth Uhealth 2021; 9: e27383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Vijayakumar NP, Neally SJ, Potharaju KA, et al. Customizing place-tailored messaging using a multilevel approach: pilot study of the step it up physical activity mobile app tailored to neighborhood environment. Circ Cardiovasc Qual Outcomes 2022; 15: e009328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Brewer LC, Jenkins S, Hayes SN, et al. Community-based, cluster-randomized pilot trial of a cardiovascular mHealth intervention: rationale, design, and baseline findings of the FAITH! Trial. Am Heart J 2022; 247: 1–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Brewer LC, Kumbamu A, Smith C, et al. A cardiovascular health and wellness mobile health intervention among church-going African Americans: formative evaluation of the FAITH! App. JMIR Form Res 2020; 4: e21450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Brewer LC, Cyriac J, Kumbamu A, et al. Sign of the times: community engagement to refine a cardiovascular mHealth intervention through a virtual focus group series during the COVID-19 pandemic. Digit Health 2022; 8: 20552076221110537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Brewer LC, Jenkins S, Hayes SN, et al. Community-based, cluster-randomized pilot trial of a cardiovascular mobile health intervention: preliminary findings of the FAITH! Trial. Circulation 2022; 146: 175–190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Brewer LC, Williams DR. We've come this far by faith: the role of the Black church in public health. Am J Public Health 2019; 109: 385–386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Taylor RJ, Chatters LM, Brown RK. African American religious participation. Rev Relig Res 2014; 56: 513–538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Tadese K, Jenkins S, Aycock D, et al. Factors facilitating academic-community research partnerships with African American churches: recruitment process for a community-based, cluster randomized controlled trial during the COVID-19 pandemic. Health Promot Pract 2024; 25: 8–12. [DOI] [PubMed] [Google Scholar]
- 32.Turkson-Ocran RN, Nmezi NA, Botchway MO, et al. Comparison of cardiovascular disease risk factors among African immigrants and African Americans: an analysis of the 2010 to 2016 national health interview surveys. J Am Heart Assoc 2020; 9: e013220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Brewer LC, Fortuna KL, Jones C, et al. Back to the future: achieving health equity through health informatics and digital health. JMIR Mhealth Uhealth 2020; 8: e14512 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Breathett K, Manning KD. Catalyzing restructure of a broken health care system. Circ Cardiovasc Qual Outcomes 2024; 17: e010009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Nour M, Lutze SA, Grech A, et al. The relationship between vegetable intake and weight outcomes: a systematic review of cohort studies. Nutrients 2018; 10. doi: 10.3390/nu10111626 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Cleven L, Krell-Roesch J, Nigg CR, et al. The association between physical activity with incident obesity, coronary heart disease, diabetes and hypertension in adults: a systematic review of longitudinal studies published after 2012. BMC Public Health 2020; 20: 726. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Takahashi EA, Schwamm LH, Adeoye OM, et al. An overview of telehealth in the management of cardiovascular disease: a scientific statement from the American Heart Association. Circulation 2022; 146: e558–e568. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Adedinsewo D, Eberly L, Sokumbi O, et al. Health disparities, clinical trials, and the digital divide. Mayo Clin Proc 2023; 98: 1875–1887. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Madanian S, Nakarada-Kordic I, Reay S, et al. Patients’ perspectives on digital health tools. PEC Innov 2023; 2: 100171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Lu Y, Liu Y, Dhingra LS, et al. National trends in racial and ethnic disparities in use of recommended therapies in adults with atherosclerotic cardiovascular disease, 1999–2020. JAMA Netw Open 2023; 6: e2345964. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Willems R, Annemans L, Siopis G, et al. Cost effectiveness review of text messaging, smartphone application, and website interventions targeting T2DM or hypertension. NPJ Digit Med 2023; 6: 150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Siegler AJ, Knox J, Bauermeister JA, et al. Mobile app development in health research: pitfalls and solutions. Mhealth 2021; 7: 32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Krebs P, Duncan DT. Health app use among US Mobile phone owners: a national survey. JMIR Mhealth Uhealth 2015; 3: e101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Thomas VE, Metlock FE, Hines AL, et al. Community-based interventions to address disparities in cardiometabolic diseases among minoritized racial and ethnic groups. Curr Atheroscler Rep 2023; 25: 467–477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Joo JY, Liu MF. Effectiveness of culturally tailored interventions for chronic illnesses among ethnic minorities. West J Nurs Res 2020; 43: 73–84. [DOI] [PubMed] [Google Scholar]
- 46.Joo JY, Liu MF. Culturally tailored interventions for ethnic minorities: a scoping review. Nurs Open 2021; 8: 2078–2090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Minnesota Department of Health. Cardiovascular Health and Diabetes Prevalence in Minnesota, https://health.state.mn.us/diseases/chronic/cdprevdata.html (2024, accessed July 11, 2024).
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-docx-1-dhj-10.1177_20552076241295305 for Efficacy of a culturally tailored mobile health lifestyle intervention on cardiovascular health among African Americans with preexisting risk factors: The FAITH! Trial by Mathias Lalika, Sarah Jenkins, Sharonne N Hayes, Clarence Jones, Lora E Burke, Lisa A Cooper, Christi A Patten and LaPrincess C Brewer in DIGITAL HEALTH