Abstract
Study Design
Retrospective cohort study.
Objective
Professional hockey players have a high incidence of lumbar disc herniations (LDH). The purpose of this study was to determine the impact of LDH on the performance and financial earnings of National Hockey League (NHL) players.
Methods
NHL players who sustained a LDH were retrospectively reviewed utilizing an online database and a 2:1 matched control cohort. Player performance and game usage was compared at one- and three-season(s) pre- and post-injury season within the cohorts. Injured and matched players were divided into 3 groups based on the player’s adjusted index season salary.
Results
A total of 181 players were included, with 62 LDH players matched to 119 healthy controls. Return to play after LDH was 79%. The LDH cohort had fewer seasons played throughout their career compared to the matched group (12.5 ± 4.3 vs 14.2 ± 3.8; P = .031). At 1 season post-index, the LDH cohort had significantly fewer goals per 60 and points per 60 when compared to pre-index. At 3 seasons post-index, the LDH cohort exhibited a significant decline in time-on-ice per game played, goals per 60, and points per 60 compared to pre-index.
Conclusion
The majority of NHL players who sustained a LDH returned to play (79%) but had shorter careers overall and decreased performance outcomes when compared to matched cohorts at both 1 and 3 seasons post-injury.
Keywords: lumbar spine, national hockey league, return to sport
Introduction
Ice hockey is a fast-paced, high collision sport that places players at an elevated risk for spinal injuries that may be devastating to health and performance.1-4 The aggressive nature of the sport, specifically with body checks at high speeds, poses an elevated risk for hockey players compared with other athletes. 5 Despite multiple interventions to prevent spinal injuries, these injuries are not uncommon and have important implications on performance, career longevity, and financial productivity for players and teams. 6
Lumbar spine injuries comprise about 13% of all NHL player injuries, with disc herniations being the most common in comparison to only 1%–3% prevalence amongst patients in the general population.4,7 These injuries may be treated both non-operatively and operatively.4,8-10 Although lumbar disc herniation (LDH) is relatively common, few studies report player performance following return to play (RTP). 11 Studies have reported successful RTP following discectomy and spinal fusion for LDH in National Hockey League (NHL) players and other professional athletes.4,8-10,12-14 However, the effect of these injuries and interventions on NHL player performance and career longevity following RTP is still largely unknown. Additionally, there is little consensus on whether surgical vs conservative treatment is associated with better outcomes for these NHL athletes. 4 There is mixed RTP after surgical and non-surgical treatment in other professional sports.8-10,15,16 Few studies have looked specifically at NHL players and no studies have looked at performance differences following these different interventions for injury.4,8,12,17 Additionally, injuries to professional athletes can have a significant impact on financial earnings of both the player and the team. However, to our knowledge, no studies have investigated the financial impact of LDH in NHL players.18-21
With the paucity of literature assessing the performance and financial outcomes of LDH in professional hockey players, the purpose of this study was to investigate the impact of LDH on career longevity and athletic performance in NHL players. Secondarily, we sought to assess the financial impact of LDH in NHL players. We hypothesized that NHL players who sustained LDH would have decreased career longevity, performance, and financial earnings.
Methods
A retrospective review of all NHL players who sustained a LDH from 1971 to 2020 (“Injured Cohort”) was performed. Consistent with previous literature, players who missed games due to injury were identified by searching the terms “back injury” and “disc herniation” in the online database Pro Sports Transactions.3,7,22 Players identified through the database were confirmed as having a LDH using individual team injury reports. Treatment of injury (surgical vs nonsurgical) was also collected for each player based on review of the previously mentioned publicly available sources. Players were excluded from performance analysis if the injury occurred outside of NHL participation, before the player’s NHL career, during NHL preseason, or if the injured player did not RTP following injury. The entire NHL season in which the injury occurred constituted the index season. A 2:1 matched control cohort (“Matched Cohort”) was created for comparison. Players were matched by age, body mass index ±5, position played, and ±2 years of experience before the index season. Players who could not be matched were excluded from the performance and financial analysis. The same index season was used for both injured and matched cohorts to ensure player age and seasons of experience were similar between cohorts.
Player demographics, game use, and performance metrics at 1 season and 3 seasons before and after index season were collected. Financial data was collected at the index season and 1, 2, 3, and 4 seasons after index season. These time periods were selected to capture the short- and long-term impact of LDH. Financial data was collected at more frequent intervals to capture the more rapidly changing financial landscape experienced in professional sports. 23 Player demographics included age, height, weight, body mass index, position, handedness, RTP rate, seasons in career, and seasons after RTP. Comparisons between the injured and matched cohorts were performed for demographics. Game use (games played [GP], time-on-ice per game played [TOI/GP]) and performance metrics (goals per 60, assists per 60, points per 60, shooting percentage, Corsi percentage, Fenwick percentage, shooting plus save percentage [PDO]) were recorded for both injured and matched cohorts 1 season and 3 seasons before and after index season. Goals per 60, assists per 60, and points per 60 are the average number of goals, assists, and points that a player has in 60 minutes of time-on-ice. These metrics are calculated by dividing a player’s total goals, assists, and points by total time-on-ice in minutes then multiplying by 60 minutes. Corsi and Fenwick percentages are measures used to determine a player’s contribution to their team’s puck possession compared to their opponents. Corsi percentage is calculated by dividing the number of shot attempts (including shots on goal, goals, missed shots, and blocked shots) for a player’s team by the number of shot attempts for both teams while a player is on ice. Fenwick percentage is calculated in the same manner but only includes shots on goal, goals, and missed shots (excludes blocked shots) in the offensive zone. Corsi and Fenwick percentages range from zero to 100%. As values approach 100%, puck possession for a player’s team is increased compared to their opponents while the player is on ice. 24 Advanced sabermetric data (Corsi percentage, Fenwick percentage, PDO) were only available for players from 2008 to 2021. Game use and performance metrics at 1 season and 3 seasons pre- and post-index were compared between the injured and matched cohorts. Game use and performance 1 season pre-index were also compared to 1 season and 3 seasons post-index within the injured and matched cohorts. Additionally, subgroup analysis using the same technique was performed on players comparing nonoperative verses operative management.
For financial analysis, index and post-index salaries were collected for each player in the injured and matched cohorts using an internet database. 23 In the injured cohort, the annual salary earned during the index season and the annual salary in the next 4 seasons after the injury were collected. For the matched cohort, the same protocol was used with the corresponding injured player’s index season as the point of reference for index and post-index annual salaries. Salaries were multiplied by the inflation conversion factor using an online calculator to adjust for inflation and equate to 2021. 25 Injured and matched players were divided into 3 groups based on the player’s index season salary: group A, <$1,000,000; group B, $1,000,000 - $3,500,000; and group C, >$3,500,000. These were designed to split the cohorts into 3 groups that represented their respective performance level and importance to the team to analyze the effect of injury on financial outcomes. The percentage of injured and matched players remaining in the NHL and the mean salary of those players were compared at index season and 1, 2, 3, and 4 seasons post-index. Mean salary for each group was calculated by multiplying the percentage of each cohort continuing to play at each time point by their mean salary and compounding the mean salary per season. Salaries impacted by LDH were calculated by finding the differences between the mean total 4-year salary of the injured and matched cohorts.
Informed consent was not applicable and no Institutional Review Board approval was necessary due to the study information being publicly available online.
Statistical Analysis
All analyses were performed using SPSS Statistics 28.0.1.1 (IBM, Armonk, NY, USA). Descriptive statistics were calculated with categorical data reported as counts with percentages and continuous data as mean ± standard deviation. To evaluate categorical data, 2-group univariate comparisons were analyzed using χ2 for values greater than 5 and Fisher exact tests for values less than 5. Continuous variables were analyzed using independent or paired-sample t-tests for normally distributed variables and Wilcoxon rank-sum or Wilcoxon signed-rank for non-normally distributed variables.
Results
Of the 62 players who suffered a LDH, 49 players (79.0%) returned to play. There was no significant difference in age, height, weight, or body mass index between the injured and matched cohorts. Position and handedness were not significantly different between cohorts. There was a significant decrease in career seasons for players who suffered a LDH compared to the matched cohort (12.5 ± 4.3 seasons vs 14.2 ± 3.8 seasons; P = .031); however, seasons after RTP were similar between the injured cohort and their healthy matched controls (P = .385) (Table 1).
Table 1.
Demographic Characteristics of NHL Players Who Sustained a LDH Injury versus Matched Controls.
| Response | Injured (n = 62) | Matched (n = 119) | P Value |
|---|---|---|---|
| Age | 28.9 ± 4.4 | 29.3 ± 4.4 | .573 |
| Height | 72.6 ± 2.8 | 72.6 ± 1.7 | .321 |
| Weight | 200.0 ± 15.3 | 196.9 ± 16.1 | .506 |
| Body mass index | 26.6 ± 1.6 | 26.4 ± 1.4 | .370 |
| Position | .963 | ||
| C | 14 (22.6%) | 24 (20.11%) | |
| D | 20 (32.3%) | 34 (28.6%) | |
| G | 5 (8.1%) | 10 (8.4%) | |
| LW | 12 (19.3%) | 27 (22.7%) | |
| RW | 11 (17.7%) | 24 (20.2%) | |
| Handedness | .853 | ||
| Left | 21 (33.9%) | 45 (37.8%) | |
| Right | 40 (64.5%) | 71 (59.7%) | |
| Unspecified | 1 (1.6%) | 3 (2.5%) | |
| Treatment | |||
| Discectomy | 10 (16.1%) | ||
| Fusion | 7 (11.3%) | ||
| Unspecified surgery | 24 (38.7%) | ||
| No surgery | 21 (33.9%) | ||
| RTP | 49 (79.0%) | ||
| Seasons in career | 12.5 ± 4.3 | 14.2 ± 3.8 | .031 |
| Seasons after RTP | 4.3 ± 4.0 | 4.9 ± 4.8 | .385 |
Continuous variables are presented using mean ± standard deviation. Categorical variables are presented using count (percentage). Significant values are noted in bold, P ≤ .05. Age represented by years; height represented in inches; weight represented in pounds; body mass index represented by kg/m2; seasons represented in years. C, center; D, defenseman; G, goalie; kg/m2, kilograms per meter squared; LDH, lumbar disc herniation; LW, left wing; NHL, National Hockey League; RTP, return to play; RW, right wing.
Game and performance data was available for 47 injured players and 94 healthy matched controls. At 1 season post-injury, injured players demonstrated significantly decreased goals per 60 (16.0 ± 15.2 vs 11.7 ± 9.2; P = .006) and points per 60 (39.1 ± 33.7 vs 31.3 ± 23.3; P = .016) compared to their pre-injury season. At 3 seasons post-injury, injured players had decreased TOI/GP (16.3 ± 3.8 vs 15.3 ± 3.8; P = .037), goals per 60 (16.0 ± 15.2 vs 13.8 ± 11.3; P = .004), and points per 60 (39.1 ± 33.7 vs 37.2 ± 23.1; P = .009) compared to their pre-injury season. No significant differences were found in performance at 1 or 3 seasons post injury in the matched cohort (Tables 2 and 3).
Table 2.
Game Utilization and Performance 1 Season before and after LDH Injury.
| Response | Time Point | Injured (n = 47) | Matched (n = 94) |
|---|---|---|---|
| GP | Pre | 56.4 ± 21.9 | 65.3 ± 19.9 |
| Post | 54.1 ± 25.3 | 66.5 ± 18.3 | |
| P value | .347 | .752 | |
| GP/TOI | Pre | 16.3 ± 3.8 | 17.7 ± 4.5 |
| Post | 15.0 ± 4.0 | 17.3 ± 5.4 | |
| P value | .118 | .941 | |
| Goals/60 | Pre | 16.0 ± 15.2 | 14.8 ± 12.6 |
| Post | 11.7 ± 9.2 | 13.4 ± 9.9 | |
| P value | .006 | .627 | |
| Assists/60 | Pre | 23.1 ± 20.1 | 25.3 ± 16.9 |
| Post | 19.6 ± 15.7 | 24.8 ± 12.2 | |
| P value | .213 | .653 | |
| Points/60 | Pre | 39.1 ± 33.7 | 40.1 ± 27.1 |
| Post | 31.3 ± 23.3 | 38.2 ± 19.7 | |
| P value | .016 | .537 | |
| Shooting % | Pre | 11.6 ± 6.1 | 10.8 ± 7.2 |
| Post | 11.8 ± 8.8 | 10.5 ± 5.9 | |
| P value | .633 | .400 | |
| Corsi % | Pre | 51.2 ± 4.4 | 51.7 ± 4.1 |
| Post | 50.4 ± 7.1 | 51.1 ± 3.9 | |
| P value | .593 | .470 | |
| Fenwick % | Pre | 51.0 ± 4.4 | 51.5 ± 4.1 |
| Post | 50.2 ± 6.9 | 50.8 ± 3.6 | |
| P value | .602 | .338 | |
| PDO | Pre | 99.4 ± 2.2 | 100.8 ± 2.2 |
| Post | 99.3 ± 3.0 | 100.2 ± 21.9 | |
| P value | 1.000 | .561 |
Continuous variables are presented using mean ± standard deviation. Significant values are noted in bold, P ≤ .05. GP represented by games; TOI/GP represented by minutes; goals/60, assists/60, points/60 represented by counts; shooting %, Corsi %, Fenwick % represented by percentages; PDO represented by shooting plus save percentage. Assists/60, assists per 60 minutes; goals/60, goals per 60 minutes; GP, games played; LDH, lumbar disc herniation; PDO, shooting plus save percentage; points/60, points per 60 minutes; TOI/GP, time on ice per game played.
Table 3.
Game Use and Performance 1 Season before and 3 Seasons after LDH Injury.
| Response | Time Point | Injured (n = 47) | Matched (n = 94) |
|---|---|---|---|
| GP | Pre | 56.4 ± 21.9 | 65.3 ± 19.9 |
| Post | 59.3 ± 21.9 | 68.4 ± 16.3 | |
| P value | .904 | .770 | |
| GP/TOI | Pre | 16.3 ± 3.8 | 17.7 ± 4.5 |
| Post | 15.3 ± 3.8 | 18.7 ± 4.5 | |
| P value | .037 | .519 | |
| Goals/60 | Pre | 16.0 ± 15.2 | 14.8 ± 12.6 |
| Post | 13.8 ± 11.3 | 14.3 ± 11.4 | |
| P value | .004 | .614 | |
| Assists/60 | Pre | 23.1 ± 20.1 | 25.3 ± 16.9 |
| Post | 23.4 ± 13.3 | 26.2 ± 14.9 | |
| P value | .057 | .496 | |
| Points/60 | Pre | 39.1 ± 33.7 | 40.1 ± 27.1 |
| Post | 37.2 ± 23.1 | 40.5 ± 24.1 | |
| P value | .009 | .448 | |
| Shooting % | Pre | 11.6 ± 6.1 | 10.8 ± 7.2 |
| Post | 10.4 ± 5.4 | 10.0 ± 5.7 | |
| P value | .135 | .735 | |
| Corsi % | Pre | 51.2 ± 4.4 | 51.7 ± 4.1 |
| Post | 48.7 ± 4.8 | 52.1 ± 3.8 | |
| P value | .087 | .740 | |
| Fenwick % | Pre | 51.0 ± 4.4 | 51.5 ± 4.1 |
| Post | 48.0 ± 5.4 | 52.0 ± 3.9 | |
| P value | .082 | .918 | |
| PDO | Pre | 99.4 ± 2.2 | 100.8 ± 2.2 |
| Post | 100.6 ± 3.7 | 100.0 ± 2.1 | |
| P value | .394 | .398 |
Continuous variables are presented using mean ± standard deviation. Significant values are noted in bold, P ≤ .05. GP represented by games; TOI/GP represented by minutes; goals/60, assists/60, points/60 represented by counts; shooting %, Corsi %, Fenwick % represented by percentages; PDO represented by shooting plus save percentage. Assists/60, assists per 60 minutes; goals/60, goals per 60 minutes; GP, games played; LDH, lumbar disc herniation; PDO, shooting plus save percentage; points/60, points per 60 minutes; TOI/GP, time on ice per game played.
At 1 season post-injury, there was a decrease in GP (54.1 ± 25.3 vs 66.5 ± 18.3; P = .011) between injured players and healthy matched controls. At 3 season post-index, there was a significant decrease in GP (59.3 ± 21.9 vs 68.4 ± 16.3; P = .050), TOI/GP (15.3 ± 3.8 vs 18.7 ± 4.5; P = .027), Corsi percentage (48.7 ± 4.8 vs 52.1 ± 3.8; P = .041), and Fenwick percentage (48.0 ± 5.4 vs 52.0 ± 3.9; P = .048) between injured players and healthy matched controls (Table 4).
Table 4.
Game Use and Performance 1 Season before and 1 Season after LDH by Treatment Type.
| Response | Operative | Nonoperative | |||
|---|---|---|---|---|---|
| Time point | Injured (n = 29) | Matched (n = 58) | Injured (n = 18) | Matched (n = 36) | |
| GP | Pre | 61.4 ± 16.6 | 66.9 ± 18.9 | 49.3 ± 26.6 | 62.7 ± 21.6 |
| Post | 56.5 ± 25.0 | 67.5 ± 18.3 | 50.7 ± 26.2 | 64.8 ± 18.5 | |
| P value | .133 | .564 | .905 | .887 | |
| GP/TOI | Pre | 16.6 ± 3.6 | 19.1 ± 4.4 | 15.8±4.4 | 15.1±3.5 |
| Post | 14.8±3.5 | 17.4±5.8 | 15.3±5.0 | 16.9±4.2 | |
| P value | .054 | .229 | 1.000 | .122 | |
| Goals/60 | Pre | 18.0±17.7 | 15.5±14.0 | 13.1±10.5 | 13.6±10.0 |
| Post | 12.0 ± 10.2 | 13.2 ± 10.0 | 11.3 ± 7.8 | 13.7 ± 9.9 | |
| P value | .038 | .808 | .078 | .540 | |
| Assists/60 | Pre | 25.3 ± 23.9 | 24.5 ± 16.8 | 20.0 ± 13.0 | 26.8 ± 17.3 |
| Post | 18.5 ± 18.0 | 23.2 ± 11.6 | 21.0 ± 12.3 | 27.6 ± 12.8 | |
| P value | .081 | .851 | .837 | .712 | |
| Points/60 | Pre | 43.3 ± 40.9 | 39.9 ± 28.8 | 33.0 ± 18.9 | 40.4 ± 24.5 |
| Post | 30.5 ± 27.2 | 36.4 ± 19.6 | 32.3 ± 17.3 | 41.3 ± 20.0 | |
| P value | .024 | .913 | .379 | .608 | |
| Shooting % | Pre | 12.4 ± 6.1 | 11.5 ± 8.0 | 10.5 ± 6.1 | 9.8 ± 5.6 |
| Post | 10.8 ± 5.9 | 10.7 ± 6.1 | 13.3 ± 11.8 | 10.3 ± 5.5 | |
| P value | .566 | .417 | .424 | .799 | |
| Corsi % | Pre | 51.4 ± 3.8 | 51.5 ± 4.5 | 50.8 ± 5.9 | 52.1 ± 3.2 |
| Post | 50.8 ± 5.9 | 50.1 ± 3.8 | 49.7 ± 10.1 | 54.6 ± 1.5 | |
| P value | .762 | .309 | .607 | .199 | |
| Fenwick % | Pre | 51.1 ± 4.1 | 51.3 ± 4.2 | 50.8 ± 5.4 | 52.2 ± 4.2 |
| Post | 50.7 ± 6.1 | 49.8 ± 3.5 | 49.2 ± 9.3 | 54.2 ± 1.4 | |
| P value | .864 | .265 | .438 | .534 | |
| PDO | Pre | 98.8 ± 2.3 | 100.8 ± 1.8 | 100.6 ± 1.5 | 100.7 ± 3.4 |
| Post | 99.0 ± 3.3 | 100.3 ± 1.7 | 99.9 ± 2.3 | 100.0 ± 2.6 | |
| P value | .814 | .248 | .688 | .787 | |
Continuous variables are presented using mean ± standard deviation. Significant values are noted in bold, P ≤ .05. GP represented by games; TOI/GP represented by minutes; goals/60, assists/60, points/60 represented by counts; shooting %, Corsi %, Fenwick % represented by percentages; PDO represented by shooting plus save percentage. Assists/60, assists per 60 minutes; goals/60, goals per 60 minutes; GP, games played; LDH, lumbar disc herniation; PDO, shooting plus save percentage; points/60, points per 60 minutes; TOI/GP, time on ice per game played.
Operative vs Nonoperative Sub-analysis
Amongst the 62 players who sustained a LDH, 41 were treated operatively and 21 were treated non-operatively. Amongst the operatively treated players, 10 (24%) players underwent discectomy, 7 players (17%) underwent spinal fusion, and 24 players (59%) underwent an unspecified surgery. Of the 41 operatively treated players, 30 players (73.2%) returned to play and of the 21 non-operatively treated players, 19 players (90.5%) returned to play. There was a significant decrease in career seasons for operatively treated players compared to the matched cohort (12.1 ± 4.2 seasons vs 13.9 ± 3.2 seasons; P = .017) and no significant difference in career seasons for nonoperatively treated players compared to the matched cohort (13.3 ± 4.4 seasons vs 14.9 ± 4.8 seasons; P = .215). Seasons after RTP were similar between the operatively (3.5 ± 3.6 seasons vs 4.4 ± 4.5 seasons; P = .254) and non-operatively (5.8 ± 4.3 seasons vs 5.9 ± 5.4 seasons; P = .959) injured cohorts and their healthy matched controls. Game and performance data was available for 29 players treated operatively and 18 players treated non-operatively and was compared to 58 and 36 healthy matched controls. At 1 season post-injury, operatively treated players exhibited a significant decrease in goals per 60 (18.0 ± 17.7 vs 12.0 ± 10.2; P = .038) and points per 60 (43.3 ± 40.9 vs 30.5 ± 27.2; P = .024) compared to their pre-injury season. Players treated non-operatively did not experience any significant decline in game use or performance. At 3 seasons post-injury, operatively managed players exhibited a significant decline in GP/TOI (16.6 ± 3.6 vs 14.4 ± 4.4; P = .049), goals per 60 (18.0 ± 17.7 vs 14.6 ± 14.4; P = .003), assists per 60 (25.3 ± 23.9 vs 23.5 ± 16.0; P = .040), points per 60 (43.3 ± 40.9 vs 38.0 ± 29.4; P = .010), and shooting percentage (12.4 ± 6.1 vs 10.1 ± 6.4; P = .014). At 3 seasons post-injury, players who were treated non-operatively experienced a significant decrease in Fenwick percentage (50.8 ± 5.4 vs 47.6 ± 1.4; P = .047) and no other significant differences in game use or performance (Table 5).
Table 5.
Game Use and Performance 1 Season before and 3 Seasons after LDH by Treatment Type.
| Response | Operative | Nonoperative | |||
|---|---|---|---|---|---|
| Time point | Injured (n = 29) | Matched (n = 58) | Injured (n = 18) | Matched (n = 36) | |
| GP | Pre | 61.4 ± 16.6 | 66.9 ± 18.9 | 49.3 ± 26.6 | 62.7 ± 21.6 |
| Post | 55.4 ± 26.9 | 64.9 ± 18.1 | 63.5 ± 14.8 | 73.7 ± 11.6 | |
| P value | .296 | .330 | .456 | .168 | |
| GP/TOI | Pre | 16.6 ± 3.6 | 19.1 ± 4.4 | 15.8 ± 4.4 | 15.1 ± 3.5 |
| Post | 14.4 ± 4.4 | 18.9 ± 4.8 | 17.1 ± 1.6 | 18.0 ± 3.8 | |
| P value | .049 | 1.000 | .465 | .032 | |
| Goals/60 | Pre | 18.0 ± 17.7 | 15.5 ± 14.0 | 13.1 ± 10.5 | 13.6 ± 10.0 |
| Post | 14.6 ± 14.4 | 13.7 ± 10.7 | 13.0 ± 7.1 | 15.2 ± 12.6 | |
| P value | .003 | .372 | .403 | .547 | |
| Assists/60 | Pre | 25.3 ± 23.9 | 24.5 ± 16.8 | 20.0 ± 13.0 | 26.8 ± 17.3 |
| Post | 23.5 ± 16.0 | 25.2 ± 14.8 | 23.3 ± 10.1 | 27.8 ± 15.3 | |
| P value | .040 | .916 | .667 | .231 | |
| Points/60 | Pre | 43.3 ± 40.9 | 39.9 ± 28.8 | 33.0 ± 18.9 | 40.4 ± 24.5 |
| Post | 38.0 ± 29.4 | 38.9 ± 23.0 | 36.3 ± 14.9 | 43.0 ± 25.8 | |
| P value | .010 | .692 | .414 | .445 | |
| Shooting % | Pre | 12.4 ± 6.1 | 11.5 ± 8.0 | 10.5 ± 6.1 | 9.8 ± 5.6 |
| Post | 10.1 ± 6.4 | 10.0 ± 5.0 | 10.7 ± 4.4 | 10.1 ± 6.7 | |
| P value | .014 | .755 | .648 | .893 | |
| Corsi % | Pre | 51.4 ± 3.8 | 51.5 ± 4.5 | 50.8 ± 5.9 | 52.1 ± 3.2 |
| Post | 48.8 ± 5.9 | 52.2 ± 3.8 | 48.4 ± 0.7 | 51.9 ± 4.1 | |
| P value | .326 | .966 | .063 | .689 | |
| Fenwick % | Pre | 51.1 ± 4.1 | 51.3 ± 4.2 | 50.8 ± 5.4 | 52.2 ± 4.2 |
| Post | 48.1 ± 6.6 | 52.1 ± 3.9 | 47.6 ± 1.4 | 51.7 ± 4.5 | |
| P value | .341 | .837 | .047 | .634 | |
| PDO | Pre | 98.8 ± 2.3 | 100.8 ± 1.8 | 100.6 ± 1.5 | 100.7 ± 3.4 |
| Post | 100.9 ± 4.4 | 100.0 ± 2.3 | 100.0 ± 1.7 | 99.9 ± 1.8 | |
| P value | .367 | .384 | .438 | .900 | |
Continuous variables are presented using mean ± standard deviation. Significant values are noted in bold, P ≤ .05. GP represented by games; TOI/GP represented by minutes; goals/60, assists/60, points/60 represented by counts; shooting %, Corsi %, Fenwick % represented by percentages; PDO represented by shooting plus save percentage. Assists/60, assists per 60 minutes; goals/60, goals per 60 minutes; GP, games played; LDH, lumbar disc herniation; PDO, shooting plus save percentage; points/60, points per 60 minutes; TOI/GP, time on ice per game played.
Financial Analysis
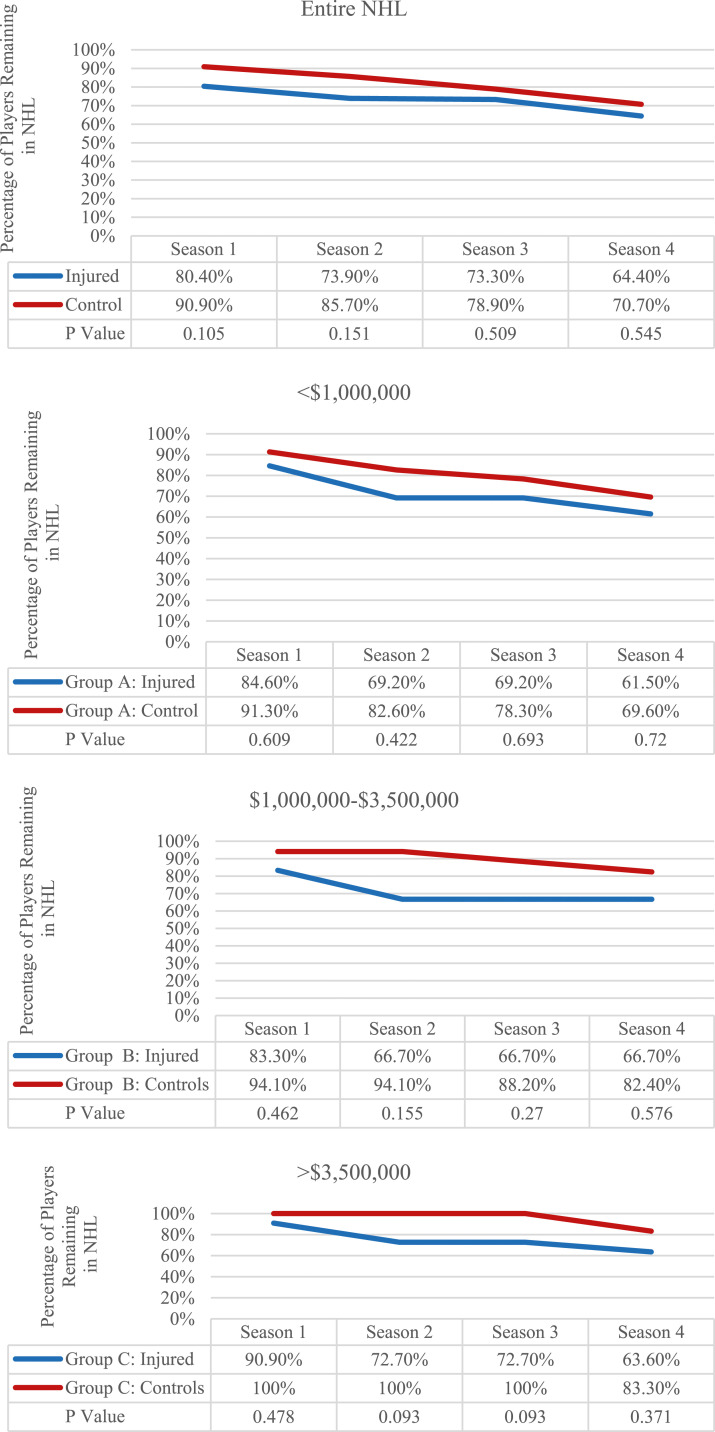
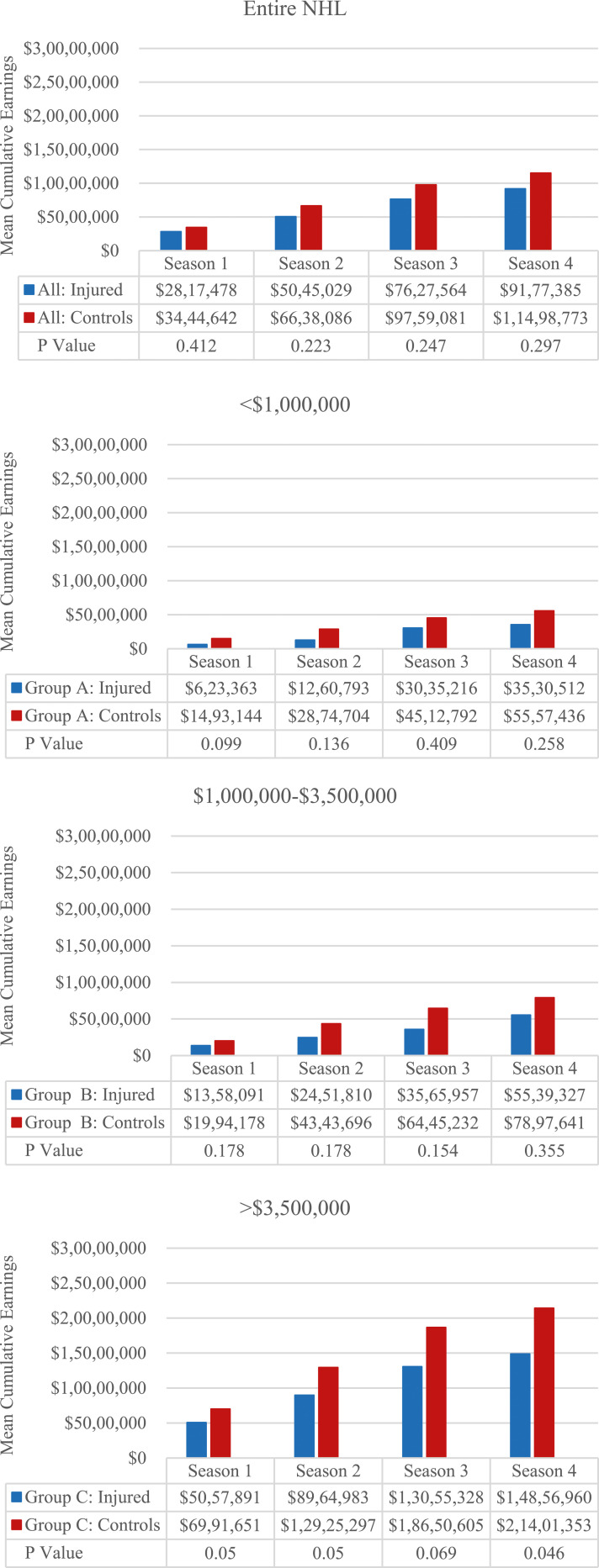
Salary data was available for 46 players with a LDH and was compared to 77 healthy matched controls. There were no significant differences in percentage of players remaining in the NHL up to 4 seasons post-index compared to healthy matched controls (Figure 1). Within salary groups A, B, and C there were no significant differences in players remaining in the NHL compared to healthy matched controls up to 4 seasons post-index. No significant differences in salary were found between injured players and healthy matched cohorts up to 4 seasons post injury season in salary groups A and B and in total salary. Within group C, however, players with LDHs had significantly lower mean cumulative earnings at 1 ($5,057,891 ± $2,125,589 vs $6,991,651 ± $2,977,127; P = .050), 2 ($8,964,983 ± $4,571,217 vs $12,925,297 ± $5,903,925; P = .050), and 4 ($14,856,960 ± $8,854,135 vs $21,401,353 ± $9,721,683; P = .046) seasons post-index compared to healthy matched controls (Figure 2).
Figure 1.
Percentage by season of (A) players who remained in the NHL after LDH injury compared with the rest of the NHL and (B–D) LDH-injured players in (B) group A (<$1,000,000), (C) group B ($1,000,000-$3,500,000), and (D) group C (>$3,500,000) who remained in the NHL compared with salary-matched controls. LDH, lumbar disc herniation; NHL, National Hockey League.
Figure 2.
Mean salary by season of (A) all LDH–injured players who remained in the NHL compared with the rest of the NHL and (B–D) LDH-injured players by initial salary: (B) <$1,000,000, (C) $1,000,000 to $3,500,000, and (D) >$3,500,000 compared with salary-matched controls. LDH, lumbar disc herniation; NHL, National Hockey League.
Discussion
The present study demonstrated that following a LDH, NHL players returned to play at a relatively high rate of 79% but played fewer career seasons overall compared to healthy matched controls. These players experienced significant reductions in game use per season and performance following injury at both 1 and 3 seasons post-injury. When stratifying players by treatment, operatively managed players had significantly decreased performance at 1 and 3 seasons post-index, while nonoperatively managed players had no performance deficits. Financially, injured players in the highest salary category had lower mean cumulative earnings at all post injury seasons that were analyzed, however no differences were found in the other salary categories or in players remaining in the NHL at all salary groups. Overall, these findings suggest that LDHs have a significant impact on NHL player career longevity as well as game use, performance, and financial outcomes.
Hockey places unique physical demands on the lumbar spine. Compared to other sports, hockey requires players to frequently rotate around their low back to pass or shoot. This repetitive motion may lead to gradual wear and tear of their lumbar discs and subsequent herniation over years of competitive play. 4 Several studies have demonstrated a high RTP rate for professional athletes suffering from LDHs.4,8,12,14,15,17,26-29 RTP rates range from 75%–100% depending on the sport. However, few studies have focused specifically on NHL players. Schroeder et al 4 reported that the RTP rate overall for NHL players suffering from a LDH was 85%. This study also found that games played per season following injury significantly decreased in players with LDH. Our study demonstrated a similar RTP of 79% after LDH with fewer games played per season after injury. While Schroeder et al had similar findings, it only included players between 1967 and 2009. In comparison, our study included more recent players over a broader time period up to 2021, giving an updated impact of LDHs on player RTP as well as analysis using more modern game performance statistics such as Corsi and Fenwick percentages. Furthermore, our study compared injured players to matched controls and found that both groups played in a similar number of seasons following RTP, but injured players had significantly shorter careers overall. We also found that there was a significant reduction in games played per season following RTP in injured players compared to matched controls. These findings together suggest that while RTP remains high, the sequela of LDH still has a negative impact on player utilization following injury which could be due to residual symptoms.
Multiple studies have examined professional athlete performance following LDHs with mixed findings.4,8,15,16,27 Hsu 10 and Savage et al 28 examined National Football League (NFL) player performance following LDH. Both studies found that player performance was not significantly different after injury compared to their pre-injury statistics. Anakwenze et al 15 examined National Basketball Association (NBA) player performance following LDH and found no significant differences between pre-injury and post-injury performance metrics for injured players. Earhart et al 16 examined performance following LDH in professional baseball players and found decreases in post-injury earned run average and walks plus hits per inning pitched for pitchers and runs and runs batted in for hitters whose lumbar injury was treated operatively. Potential reasons for these decreases in operatively treated athletes included older age in athletes treated operatively, the different contract incentives unique to professional baseball, and the unique body demands including heavy torque loads in professional baseball. Schroeder et al 4 studied performance after LDH in NHL players and reported significantly worse points per game and performance score (based on goals, assists, penalty minutes, and plus/minus) in the post-injury period. We similarly found that significantly decreased performance in both 1 and 3 seasons after injury. While these results are likely multifactorial, NHL players sustain significant torsional stress on their lumbar spines and likely have accumulated injuries to their lower backs over many years of competitive play. Their longer career length likely gives the opportunity for them to realize the degenerative changes with repeated wear and tear following LDH.20,30,31 These injuries, although treatable, are the results of continued degeneration of the low back that cannot be simply reversed by rehabilitation or surgery.4,20,31-33
Our study demonstrated that players treated surgically showed significant decreases in performance at both 1 and 3 years post-injury compared to pre-injury. However, players managed nonoperatively had similar performance following injury. Typically, LDH is initially treated non-operatively, with operative options being reserved for patients who have symptoms for greater than 8 weeks or for patients who present with severe or worsening motor deficits. 23 It is likely that operatively treated patients were those who failed initial non-operative management, and thus could be considered more “severe” cases. Schroeder et al 4 similarly found significant decreases in usage and performance following operative treatment of LDH. However, they also found decreases in the nonoperative group. Kajy et al 34 compared the RTP of multiple sports after lumbar discectomy amongst professional athletes including NHL players and demonstrated that performance peaked within 2 years after surgery for NBA, NFL, and NHL players, but steeply declined in subsequent years following the procedure. A meta-analysis by Sedrak et al, 29 comparing RTP between operative and non-operative treatment of LDH reported that there were no differences in RTP rates for players who underwent lumbar discectomy compared to those treated conservatively with average RTP of 5.19 and 4.11 months respectively. Non-operatively treated players in our study overall had returned to pre-injury usage and performance which could be attributed to more modern treatment and rehabilitation protocols.
One often overlooked aspect following injury in professional sports is the economic impact an injury creates for a player and the team. Donaldson et al 35 looked at the overall incidence of injuries in the NHL and the associated cost. They found that 50.9% of players missed at least 1 game within a season due to injury, and that the total salary cost associated with these injuries was $218 million annually. Navarro et al 19 examined the financial impact associated with concussions in the NHL and the total annual financial impact from salary reductions after 1 concussion was $57 million throughout the league and a decrease of $292,000 per year in contract value for an individual player. Secrist et al 20 examined the impact of anterior cruciate ligament injuries on salary in NFL athletes and found these players earned $2,070,521 less than salary-matched controls over a 4-year period post-injury. Our study found a significant decrease in cumulative earnings only in the highest salary group (index season salary >$3,500,00) that had LDHs. This shows LDHs had a minimal financial impact on players, which is consistent with the high RTP and acceptable post-injury performance. The lower cumulative earnings in the higher salary group could potentially be due to the higher skill and worth of these higher paid players being more affected by injury than the lower salary groups. 20 Overall, the financial impact of LDH on NHL players is similar to matched non-injured players.
There are several limitations to this study. Due to the retrospective nature, it is subject to information bias. Publicly available sources used to gather information for the study could be inaccurate as many reporters do not understand the nuances and details of spine pathology, injury classification, treatment modalities, and recovery. RTP could also have been affected by other injuries sustained alongside the LDH that were not reported in the reviewed sources. Information available was also prone to selection bias as more prominent athletes typically get more media coverage and therefore potentially more coverage of their injury compared to less well-known players. We are also unable to access official medical records or a centralized injury database and therefore were unable to completely confirm injuries, rule out concomitant injuries, and confirm specific treatments. These are important considerations when evaluating a player’s injury, such as the chronicity of the injury, presence of lower back pain with or without radiculopathy, and how this pathology was managed surgically. It is also important to consider that patients treated surgically may have more severe injuries than those treated nonoperatively. In addition, our study features a broad time spectrum of injuries covering 51 years. There have been significant changes in how these LDH are managed over time due to advances in surgical techniques and technology. Lastly, the typically reported performance markers used in this study may not accurately represent a player’s role or importance to a team. Certain players in the NHL, for example, serve as enforcers, penalty killers, or faceoff specialists rather than goal scorers. 36
Conclusion
NHL players demonstrated a moderately high RTP following LDH with reductions in game use and performance at 1 and 3 seasons after injury compared to pre-injury and matched controls.37-48 NHL players who underwent operative treatment had significant reductions in performance compared to nonoperatively treated players. Financial earnings were also reduced for the highest earning players who sustained LDHs.
Footnotes
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iD
Michael A. Gaudiani https://orcid.org/0000-0002-3366-1708
References
- 1.Ambrozaitis KV, Kontautas E, Spakauskas B, Vaitkaitis D. Nugaros smegenu pazeidimo patofiziologija [pathophysiology of acute spinal cord injury]. Medicina (Kaunas). 2006;42(3):255-261. [PubMed] [Google Scholar]
- 2.Eckert MJ, Martin MJ. Trauma: spinal cord injury. Surg Clin North Am. 2017;97(5):1031-1045. [DOI] [PubMed] [Google Scholar]
- 3.Nobunaga AI, Go BK, Karunas RB. Recent demographic and injury trends in people served by the model spinal cord injury care systems. Arch Phys Med Rehabil. 1999;80(11):1372-1382. [DOI] [PubMed] [Google Scholar]
- 4.Schroeder GD, McCarthy KJ, Micev AJ, Terry MA, Hsu WK. Performance-based outcomes after nonoperative treatment, discectomy, and/or fusion for a lumbar disc herniation in National Hockey League athletes. Am J Sports Med. 2013;41(11):2604-2608. [DOI] [PubMed] [Google Scholar]
- 5.Anderson GR, Melugin HP, Stuart MJ. Epidemiology of injuries in ice hockey. Sports Health. 2019;11(6):514-519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Morrissette C, Park PJ, Lehman RA, Popkin CA. Cervical spine injuries in the ice hockey player: current concepts in epidemiology, management and prevention. Global Spine J. 2021;11(8):1299-1306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Fjeld OR, Grøvle L, Helgeland J. et al. Complications, reoperations, readmissions, and length of hospital stay in 34 639 surgical cases of lumbar disc herniation. Bone Joint Lett J. 2019;101-B(4):470-477. [DOI] [PubMed] [Google Scholar]
- 8.Hsu WK, McCarthy KJ, Savage JW. et al. The Professional Athlete Spine Initiative: outcomes after lumbar disc herniation in 342 elite professional athletes Spine. J. 2011;11(3):180-186. [DOI] [PubMed] [Google Scholar]
- 9.Hsu WK. Outcomes following nonoperative and operative treatment for cervical disc herniations in National Football League athletes. Spine. 2011;36(10):800-805. [DOI] [PubMed] [Google Scholar]
- 10.Hsu WK. Performance-based outcomes following lumbar discectomy in professional athletes in the National Football League. Spine. 2010;35(12):1247-1251. [DOI] [PubMed] [Google Scholar]
- 11.Overley SC, McAnany SJ, Andelman S, et al. Return to play in elite athletes after lumbar microdiscectomy: a meta-analysis. Spine. 2016;41(8):713-718. doi: 10.1097/BRS.0000000000001325. [DOI] [PubMed] [Google Scholar]
- 12.Reiman MP, Sylvain J, Loudon JK, Goode A. Return to sport after open and microdiscectomy surgery versus conservative treatment for lumbar disc herniation: a systematic review with meta-analysis. Br J Sports Med. 2016;50(4):221-230. [DOI] [PubMed] [Google Scholar]
- 13.Roberts DW, Roc GJ, Hsu WK. Outcomes of cervical and lumbar disk herniations in Major League Baseball pitchers. Orthopedics. 2011;34(8):602-609. [DOI] [PubMed] [Google Scholar]
- 14.Weistroffer JK, Hsu WK. Return-to-play rates in National Football League linemen after treatment for lumbar disk herniation. Am J Sports Med. 2011;39(3):632-636. [DOI] [PubMed] [Google Scholar]
- 15.Anakwenze OA, Namdari S, Auerbach JD. et al. Athletic performance outcomes following lumbar discectomy in professional basketball players. Spine. 2010;35(7):825-828. [DOI] [PubMed] [Google Scholar]
- 16.Earhart JS, Roberts D, Roc G, Gryzlo S, Hsu W. Effects of lumbar disk herniation on the careers of professional baseball players. Orthopedics. 2012;35(1):43-49. [DOI] [PubMed] [Google Scholar]
- 17.Iwamoto J, Sato Y, Takeda T, Matsumoto H. The return to sports activity after conservative or surgical treatment in athletes with lumbar disc herniation. Am J Phys Med Rehabil. 2010;89(12):1030-1035. [DOI] [PubMed] [Google Scholar]
- 18.King DA, Hume PA, Hind K, Clark TN, Hardaker N. The incidence, cost, and burden of concussion in women's rugby league and rugby union: a systematic review and pooled analysis. Sports Med. 2022;52(8):1751-1764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Navarro SM, Pettit RW, Haeberle HS. et al. Short-term impact of concussion in the NHL: an analysis of player longevity, performance, and financial loss. J Neurotrauma. 2018;35(20):2391-2399. [DOI] [PubMed] [Google Scholar]
- 20.Secrist ES, Bhat SB, Dodson CC. The financial and professional impact of anterior cruciate ligament injuries in national football league athletes. Orthop J Sports Med. 2016;4(8):2325967116663921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Yengo-Kahn AM, Kelly PD, Liles DC. et al. The cost of a single concussion in American high school football: a retrospective cohort study. Concussion. 2020;5(4):CNC81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Pro Sports Transactions . Search Hockey Transactions. Pro Sports Transactions. https://www.prosportstransactions.com/hockey/ (2023). [Google Scholar]
- 23.Schoenfeld AJ, Weiner BK. Treatment of lumbar disc herniation: evidence-based practice. Int J Gen Med. 2010;3:209-214. doi: 10.2147/ijgm.s12270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Hockey-Statistics . Introduction to Hockey Statistics – First Chapter. Lausanne: Hockey-Statistics; 2022. https://hockey-statistics.com/2022/06/08/introduction-to-hockey-statistics-first-chapter/ [Google Scholar]
- 25.Bureau of Labor Statistic . Inflation Calculator. Washington: Bureau of Labor Statistic; 2023. https://data.bls.gov/cgi-bin/cpicalc.pl. [Google Scholar]
- 26.Minhas SV, Kester BS, Hsu WK. Outcomes after lumbar disc herniation in the national basketball association. Sports Health. 2016;8(1):43-49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Nair R, Kahlenberg CA, Hsu WK. Outcomes of lumbar discectomy in elite athletes: the need for high-level evidence. Clin Orthop Relat Res. 2015;473(6):1971-1977. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Savage JW, Hsu WK. Statistical performance in National Football League athletes after lumbar discectomy. Clin J Sport Med. 2010;20(5):350-354. [DOI] [PubMed] [Google Scholar]
- 29.Sedrak P, Shahbaz M, Gohal C, Madden K, Aleem I, Khan M. Return to play after symptomatic lumbar disc herniation in elite athletes: a systematic review and meta-analysis of operative versus nonoperative treatment. Sports Health. 2021;13(5):446-453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Schroeder GD, Vaccaro AR. Cervical spine injuries in the athlete. J Am Acad Orthop Surg. 2016;24(9):e122-e133. [DOI] [PubMed] [Google Scholar]
- 31.Tator CH, Carson JD, Edmonds VE. Spinal injuries in ice hockey. Clin Sports Med. 1998;17(1):183-194. [DOI] [PubMed] [Google Scholar]
- 32.Andrews E, Jildeh TR, Abbas MJ, Lindsay-Rivera K, Berguson J, Okoroha KR. Concussions in the national hockey league: analysis of incidence, return to play, and performance. Orthop J Sports Med. 2022;10(1):23259671211052069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Montgomery DL. Physiology of ice hockey. Sports Med. 1998;5(2):99-126. [DOI] [PubMed] [Google Scholar]
- 34.Kajy M, Higginbotham DO, Ball G, Vaidya R. Fantasy points" associated with professional athlete performance after lumbar discectomy or microdiscectomy. Spartan Med Res J. 2022;7(1):30766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Donaldson L, Li B, Cusimano MD. Economic burden of time lost due to injury in NHL hockey players. Inj Prev. 2014;20(5):347-349. [DOI] [PubMed] [Google Scholar]
- 36.Castle JP, Cotter DL, Jildeh TR, et al. Reduced career longevity but return to baseline performance after arthroscopic shoulder labral repair in national hockey league players. Arthrosc Sports Med Rehabil. 2022;4(2):e599-e605. doi: 10.1016/j.asmr.2021.11.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Berube ER, Lopez CD, Trofa DP, Popkin CA. A systematic review of the orthopedic literature involving national hockey league players. Open Access J Sports Med. 2020;11:145-160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Chatha K, Al-Mansoori A, Guo E, Whaley JD, Sabesan VJ. Impact of the 7-day disabled list rule change on economics and performance after reported concussion injuries in major league baseball. Orthop J Sports Med. 2019;7(2):2325967119825502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Daly PJ, Sim FH, Simonet WT. Ice hockey injuries. A review. Sports Med. 1990;10(2):122-131. [DOI] [PubMed] [Google Scholar]
- 40.France JC, Karsy M, Harrop JS, Dailey AT. Return to play after cervical spine injuries: a consensus of opinion. Global Spine J. 2016;6(8):792-797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Jack RA, 2nd, Sochacki KR, Hirase T, Vickery JW, Harris JD. Performance and return to sport after hip arthroscopy for femoroacetabular impingement in professional athletes differs between sports. Arthroscopy. 2019;35(5):1422-1428. [DOI] [PubMed] [Google Scholar]
- 42.Longstaffe R, Leiter J, MacDonald P. Anterior cruciate ligament injuries in the national hockey league: epidemiology and performance impact. Clin J Sport Med. 2020;30(3):224-230. [DOI] [PubMed] [Google Scholar]
- 43.McKay CD, Tufts RJ, Shaffer B, Meeuwisse WH. The epidemiology of professional ice hockey injuries: a prospective report of six NHL seasons. Br J Sports Med. 2014;48(1):57-62. [DOI] [PubMed] [Google Scholar]
- 44.Sim FH, Chao EY. Injury potential in modern ice hockey. Am J Sports Med. 1978;6(6):378-384. [DOI] [PubMed] [Google Scholar]
- 45.Sys J, Michielsen J, Bracke P, Martens M, Verstreken J. Nonoperative treatment of active spondylolysis in elite athletes with normal X-ray findings: literature review and results of conservative treatment. Eur Spine J. 2001;10(6):498-504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Szukics PF, Otlans PT, Arevalo A, Meade M, DeLuca P, Salvo JP. A scoping review of injuries in amateur and professional men’s ice hockey. Orthop J Sports Med. 2022;10(4):23259671221085968. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Vartiainen MV, Holm A, Peltonen K, Luoto TM, Iverson GL, Hokkanen L. King-Devick test normative reference values for professional male ice hockey players. Scand J Med Sci Sports. 2015;25(3):e327-e330. [DOI] [PubMed] [Google Scholar]
- 48.Engebretsen L, Steffen K, Alonso JM, et al. Sports injuries and illnesses during the winter olympic games 2010. Br J Sports Med. 2010;44(11):772-780. [DOI] [PubMed] [Google Scholar]