Abstract
Background:
This study aimed to devise the method for the evaluation of the thumb pronation angle and calculate its reference value.
Methods:
The study was conducted from October 2021 to March 2022, and 600 hands of 300 healthy volunteers were included in this study. The participants were divided into 6 age groups with 50 participants each. In study 1, 12 participants from group 1 were randomly selected, which included 6 male and 6 female participants. We measured the thumb pronation angle using FASTRAK system and the nail tip angle of thumb-ring finger opposition (T-R angle) and also evaluated the relation between them. In study 2, we measured the T-R angle of 600 hands of 300 healthy volunteers. The T-R angle mean (SD) and 95% confidence interval (CI) of each age group were calculated as reference values.
Results:
The thumb pronation angle was correlated with the T-R angle. The T-R angle mean (SD) and 95% CI of the 6 groups were as follows: group 1, 142.5° (12.4) and 117.7 to 167.3; group 2, 139.9° (10.1) and 119.7 to 160.1; group 3, 142.3° (9.7) and 122.9 to 160.5; group 4, 140.2° (12.6) and 115.0 to 165.4; group 5, 138.3° (11.9) and 114.5 to 162.1; and group 6, 135.4° (13.0) and 109.4 to 161.4. The 95% CI tended to decrease with an increasing age.
Conclusions:
The T-R angle was a suitable evaluation method for the thumb pronation angle, and it should be evaluated by age groups.
Keywords: Kapandji score, thumb pronation, thumb opposition, nail tip angle, evaluation, research and health outcomes
Introduction
Thumb opposition is an important hand function.1,2 Thumb opposition is impaired in severe cases of carpal tunnel syndrome (CTS) and carpometacarpal joint osteoarthritis (CMJ OA) and is sometimes treated surgically.3 -7 The Kapandji score is the most common method of evaluating thumb-opposing motion, diagnosis, and treatment outcomes. 8 However, thumb opposition is a combination of 3 motions: abduction, pronation, and flexion.9 -11 The Kapandji score is not suitable for the evaluation of thumb opposition, which allows for obtaining high scores by thumb flexion alone.12,13 Specifically, thumb pronation is an important motion for thumb opposition; unlike abduction and flexion, it is difficult to quantify.
Previous studies have used computed tomography,14 -16 a sensor-engineered glove, 17 and gyroscopes 18 for evaluation. However, these methods are not easily available in the clinical setting because they are invasive, costly, and time-consuming and require special equipment. Recently, noninvasive, inexpensive, wearable sensors have been developed 18 and are expected to become widely used, but they are not yet commonly used. Bunnell reported that when the thumb pronates, the plane of the thumbnail rotates 90° from a position at a right angle to the palm to a position parallel with it. 1 Therefore, we hypothesized that we could evaluate the pronation motion of the thumb by measuring the nail tip angle of thumb-ring finger opposition (T-R angle). Furthermore, we thought that calculating the reference values of the T-R angle for each age group would improve the accuracy of the evaluation method. This study aimed to prove that the T-R angle is a useful evaluation method of the thumb pronation angle during thumb opposition and provide reference values for each age group.
Methods
This cross-sectional study was approved by the local ethics committee. Informed consent was obtained from all individual participants included in the study. Two substudies were conducted in this study.
Participants
Between October 2021 and March 2022, 600 hands of 300 healthy volunteers were included in this study. The participants were divided into 6 age groups with 50 participants each: group 1, 20 to 39 years old; group 2, 40 to 49 years old; group 3, 50 to 59 years old; group 4, 60 to 69 years old; group 5, 70 to 79 years old; and group 6, ≥80 years old). Each group had an equal number of male and female volunteers. The exclusion criteria were as follows: pain, deformity, paralysis, sensory disturbance, contracture, a history of hand and finger trauma, and inability to follow the indicated motions.
In study 1, we evaluated the relation between the thumb pronation angle and the T-R angle. From group 1, 12 participants were randomly selected, which included 6 male and 6 female participants. The selection was based on the small effect of age-related change. The sample size was determined based on reports of previous pilot studies, as there have been no similar studies in the past. 19
In study 2, we calculate the reference value of the T-R angle for each age group. A total of 600 hands of 300 healthy volunteers were included in the study. The larger the sample size, the better the calculation of normal regions. However, 300 was set as the number of people for whom recruitment was feasible within the time frame.
Study Assessments
In study 1, we measured the thumb pronation angle and the T-R angle. The thumb pronation angle was measured using FASTRAK system (Polhemus Inc, Colchester, Vermont). It is a 3-dimensional motion-tracking system for spatial analysis. This system can measure and record the position and orientation of the sensors, with the sampling ratio set at 120 Hz in a constant magnetic field. To determine the location and angular orientation of each sensor relative to the source, the source emits an electromagnetic field that is detected by sensors with a root mean square accuracy of 0.76 mm for the x, y, or z positions and 0.15 for the receiver orientation within 300 mm. A sensor was attached to the thumbnail surface to mark the long axis of the thumb. The forearm and palm were banded at 90° of forearm supination to a wooden jig. The starting point was set at the height where the ulnar edge of the thumb coincided with the palmar surface. To measure the variability (maximum to minimum) of the T-R angles, participants were asked to perform 30 oppositions in which the thumb and ring fingertip of the phalanges touched at random. The middle, ring, and little fingers were flexed together to avoid the effect of rotation of the ring finger. Measurements were taken at the point at which the thumb and ring tip of phalanges touched (Figure 1). The thumb pronation angle was measured using FASTRAK, and at the same time, a photograph was taken with the ring fingernail plane as the front plane. The T-R angle is the angle between the long axis of the nail surface of the thumb and the long axis of the nail surface of the ring finger, and it was measured twice by 1 examiner using ImageJ (Figure 2). The average value was calculated. Another examiner measured the angle twice and evaluated the reliability of the measurements.
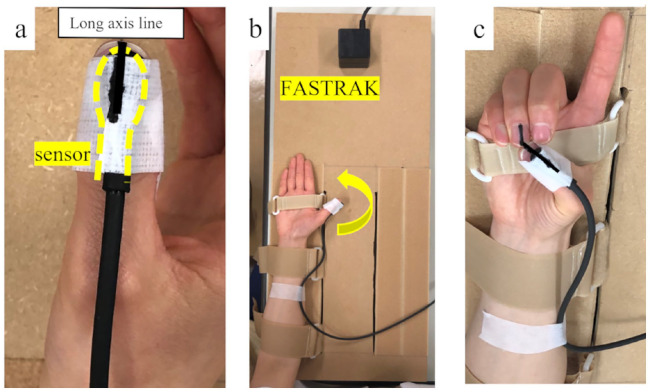
Figure 1.
Measurement of the thumb pronation angle and the nail tip angle of thumb-ring finger opposition.
Note. (a) A sensor was attached to the thumbnail surface to mark the long axis of the thumb. (b) The forearm and palm were banded at 90° of forearm supination to a wooden jig. The starting point was set at the height where the ulnar edge of the thumb coincided with the palmar surface. (c) Perform 30 thumb-ring finger oppositions at random.
Figure 2.
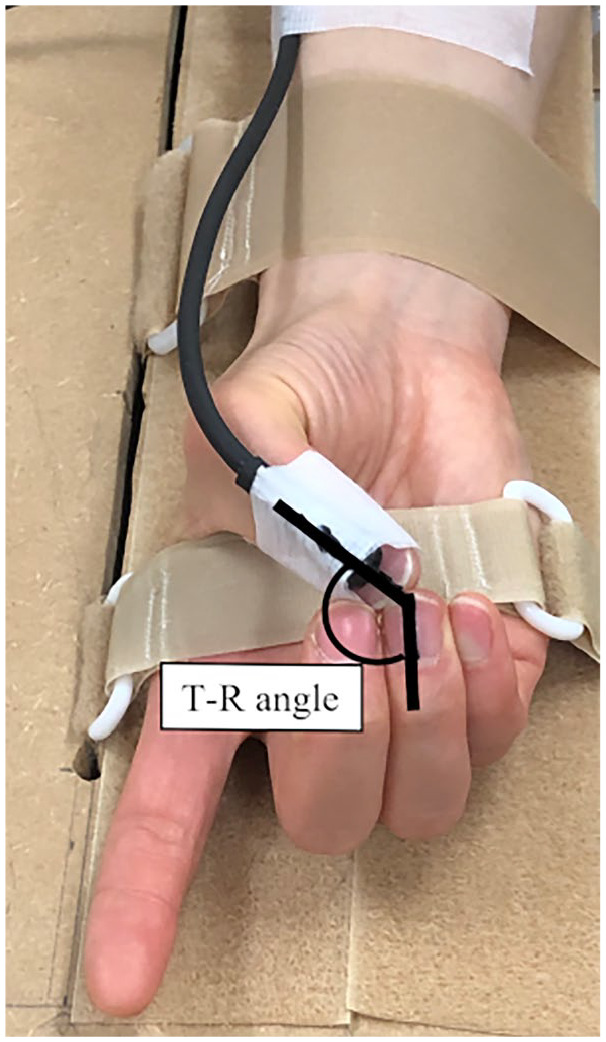
Measurement of the T-R angle.
Note. A photograph was taken with the ring fingernail plane as the front plane. T-R angle is the angle between the long axis of the nail surface of the thumb and ring finger; it was measured using ImageJ. T-R angle = nail tip angle of thumb-ring finger opposition.
In study 2, we measured the T-R angle for each age group. The T-R angles of 600 hands of 300 healthy volunteers were measured. The examiner demonstrated and explained the procedure, and the participants were asked to perform 1 maximum thumb-ring finger opposition without using a jig. As in the previous experiment, the middle, ring, and little fingers were flexed together to avoid the influence of the ring finger rotation movement. Measurements were taken at the position where the thumb and ring finger apexes touched. The measurement methods and reliability were the same as in study 1. In addition, the angle of the palmar abduction of the thumb and flexion angles of the metacarpophalangeal joints (MPJ), interphalangeal joints (IPJ) of the thumb, and MPJ, proximal interphalangeal joints (PIPJ), and distal interphalangeal joints (DIPJ) of the ring finger were measured using a goniometer when performing thumb-ring finger opposition.
Statistical Analyses
In study 1, Spearman correlation coefficient was used to evaluate the correlation between the thumb pronation angle and the T-R angle.
In study 2, the T-R angle of the 600 hands of 300 volunteers was presented as mean (standard deviation [SD]) and 95% confidence intervals (CIs) by each age group. In addition, the trend between the T-R angle and age was examined by the linear trend test. Similarly, the angle of the palmar abduction of the thumb and flexion angles of the MPJ, IPJ of the thumb, and MPJ, PIPJ, and DIPJ of the ring finger were presented as mean (SD). The Spearman correlation coefficient was used to evaluate the correlation between the T-R angle and the angle of each joint of the thumb and ring finger. In each study, the inter-rater reliability of T-R angle measurements was evaluated using the intraclass correlation coefficient (ICC). An ICC value of 1 was considered perfect, greater than 0.80 was considered very good, greater than 0.60 was considered good, and greater than 0.40 was considered moderate reliability. 20 A 2-sided test result of P < .05 was considered statistically significant. All results were analyzed using SAS version 9.4 for Windows (SAS Institute, Cary, North Carolina).
Results
Study 1: Relation Between the Thumb Pronation Angle and the T-R Angle
The participants were 6 male and 6 female patients, with a mean (SD) age of 28.4 (4.6) years. The thumb pronation angle was moderately positively correlated with the T-R angle (ρ = 0.65, P < .01) (Figure 3). The ICCs for the intraclass and interclass reliability of the T-R angle were 0.93 (95% CI, 0.91-0.94) and 0.91 (95% CI, 0.89-0.93), respectively.
Figure 3.
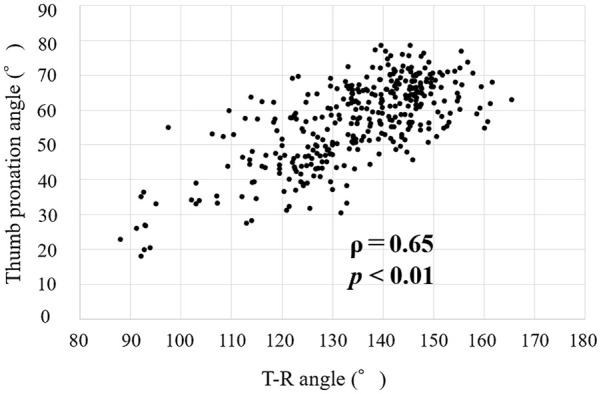
Relationship between the thumb pronation angle and T-R angle.
Note. T-R angle = nail tip angle of thumb-ring finger opposition.
Study 2: Reference Value of the T-R Angle for Each Age Group
This study included 600 hands of 300 healthy volunteers (150 men and 150 women) with a mean (SD) age of 58.7 (18.6) years. The T-R angle mean (SD) and 95% CI of the 6 groups are shown in Table 1. A negative linear trend with age was found (test for linear trend, P < .001) (Figure 4). In the correlation analysis between the T-R angle and angle of each joint of the thumb and ring finger, only the flexion angle of the thumb MPJ showed a weak negative correlation (ρ = −0.23, P < .001) (Table 2). The ICCs for the intraclass and interclass reliability of the T-R angle were 0.98 (95% CI, 0.97-0.98) and 0.98 (95% CI, 0.97-0.98), respectively.
Table 1.
T-R Angle Grouped According to Age.
| Group | Age | T-R angle (°) | ||
|---|---|---|---|---|
| Range | Mean (SD) | Mean (SD) | 95% CI | |
| 1 | 20-39 | 29.9 (5.6) | 142.5 (12.4) | 117.7-167.3 |
| 2 | 40-49 | 44.2 (2.8) | 139.9 (10.1) | 119.7-160.1 |
| 3 | 50-59 | 54.5 (2.5) | 142.3 (9.7) | 122.9-160.5 |
| 4 | 60-69 | 64.5 (3.2) | 140.2 (12.6) | 115.0-165.4 |
| 5 | 70-79 | 74.3 (2.6) | 138.3 (11.9) | 114.5-162.1 |
| 6 | ≥80 | 84.6 (3.1) | 135.4 (13.0) | 109.4-161.4 |
| Total | 58.7 (18.6) | 139.8 (11.9) | 116.0-163.6 | |
Note. T-R angle = nail tip angle of thumb-ring finger opposition; CI = confidence interval.
Figure 4.
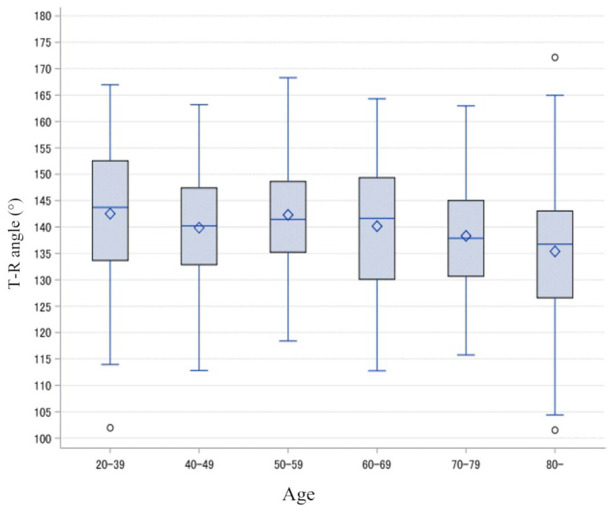
Box plots of the T-R angle for each age group.
Note. T-R angle = nail tip angle of thumb-ring finger opposition.
Table 2.
Correlation Between the T-R Angle and Angle of Each Joint of the Thumb and Ring Finger (n = 600).
| Angle (°), mean (SD) | ρ | P value | |
|---|---|---|---|
| T-R angle | 139.8 (11.9) | ||
| Thumb – Palmar abduction | 44 (6.4) | 0.08 | .061 |
| Thumb – MPJ flexion | 29 (10.4) | −0.23 | <.001** |
| Thumb – IPJ flexion | 50 (17.2) | −0.12 | .005* |
| Ring finger – MPJ flexion | 39 (9.4) | −0.07 | .104 |
| Ring finger – PIPJ flexion | 69 (10.8) | −0.11 | .007* |
| Ring finger – DIPJ flexion | 54 (11.6) | −0.01 | .84 |
Note. Data are Spearman correlation coefficients (ρ). T-R angle = nail tip angle of thumb-ring finger opposition; MPJ = metacarpophalangeal joints; IPJ = interphalangeal joints; PIPJ = proximal interphalangeal joints; DIPJ = distal interphalangeal joints.
P < .01. **P < .001.
Discussion
Currently, the most commonly used evaluation method of thumb opposition in clinical practice is the Kapandji score3,7,21; however, high scores can be obtained even in patients with severe CTS who have atrophy of the thenar muscle. Thus, the Kapandji score is not suitable for the evaluation of thumb pronation.18,22
In study 1, we examined whether the T-R angle is suitable for the evaluation of the thumb pronation angle to establish a method that can easily evaluate it in clinical practice. According to a previous report that observed changes in the position of the nail surface relative to the palm during thumb pronation, 1 the FASTRAK sensor was attached to the thumbnail surface to measure the thumb pronation angle. FASTRAK is a 3-dimensional motion-tracking system for spatial analysis and has been used to measure the thumb pronation angle in the past. 23
In this study, the maximum value of the thumb rotation angle was almost 80°, which was not largely different from past reports, that is, when the thumb pronates, the plane of the thumbnail rotates 90° from a position at a right angle to the palm to a position parallel with it. 1 The angle of pronation was slightly lower because this study assumed the position of the thumb and ring phalanx to be touched; thus, the measurement may have been taken before the thumb was fully rotated.
Cheema evaluated the pronation angle of the first metacarpal during opposition of the thumb, index, middle, ring, and little fingers and reported that the angle of pronation increased from the index finger to the small finger. 14 Given this, the maximum angle of pronation of an individual can be assessed by measuring the angle of opposition to the little finger; however, there was concern that the range of motion of the CMJ of the little finger would greatly affect the angle of opposition to the nail surface. Therefore, we proposed the T-R angle as an evaluation method, in which the ring finger was flexed together with the middle and little fingers to measure as large pronation angle as possible to avoid the influence of the CMJ rotation motion of the ring finger.
In addition, the long axis line of the ring nail was used as the axis for the measurement by taking a photograph of the frontal aspect of the ring nail, and changes in the nail surface of the thumb could be evaluated consistently. The ICC for intraclass and interclass reliability of this measurement method was greater than 0.80 (very good). There was a moderate positive correlation between the T-R angle and the thumb pronation angle, indicating that the measurement of the T-R angle is suitable for the evaluation of the thumb pronation angle.
In study 2, the 95% CI of the T-R angles for each age group was calculated as reference values. Although the participants were healthy volunteers with no hand complaints, all groups had a large range of reference values for the T-R angle, approximately 40° to 50°. This was thought to be influenced by individual differences in joint conformity and joint laxity.24,25
The T-R angle trended to decrease with an increasing age. Signori evaluated thumb opposition motion using a sensor-engineered glove and found that the performance decreased with age. 17 Normal age-related muscle loss (sarcopenia) 26 and joint degeneration 24 were also reported, which we attributed to this. Thus, the T-R angle should be evaluated according to age.
In addition, a weak negative correlation was observed only for the flexion of the MPJ of the thumb in correlation with the range of motion of each finger joint, but the correlation coefficient was low, indicating no influence. This result proves that this evaluation method can evaluate thumb pronation motion alone without being affected by other motions. Furthermore, this result is a more effective evaluation method of thumb pronation motion compared with the Kapandji score, in which a high score is obtained only for thumb flexion.
This evaluation method can evaluate the thumb pronation angle easily in a clinical environment because it requires only T-R angle measurement, without the invasiveness, cost, labor, and special equipment, which have been problems in the past.
This study had some limitations. First, the race and region of the study participants are limited, and reference values by race should be examined. Second, the study has a relatively small number of participants: the greater the number of participants, the more accurate the reference value; thus, it is necessary to further increase the number of participants. Finally, the study participants did not undergo radiograph imaging or nerve conduction study. Therefore, some patients with potential thumb CMJ OA or CTS were among the enrolled participants. However, because they were judged to be healthy based on medical consultation and examination findings, we believe that the number of such patients is small, and none of the participants had severe conditions. Because the incidence of various diseases increases with age, it is necessary to consider age-related changes in the reference values for each age group, and the method of selecting participants was considered appropriate.
Conclusions
Our study demonstrates that the T-R angle can be used to evaluate the thumb pronation motion, and it should be evaluated by age groups.
Acknowledgments
The authors would like to thank Y. Ozawa for performing data analysis and interpretation. They would also like to thank Enago (www.enago.jp) for the English language review.
Footnotes
Ethical Approval: This study was approved by our institutional review board.
Statement of Human and Animal Rights: All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (Chiba University Graduate School of Medicine Ethics Review Committee M10024, Japan) and with the Helsinki Declaration of 1975, as revised in 2008.
Statement of Informed Consent: Informed consent was obtained from all patients for being included in the study.
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iDs: Shinji Taniguchi  https://orcid.org/0000-0001-8754-7225
https://orcid.org/0000-0001-8754-7225
Koichi Nakagawa  https://orcid.org/0000-0001-7859-4310
https://orcid.org/0000-0001-7859-4310
References
- 1. Bunnell S. Opposition of the thumb. J Bone Joint Surg. 1938;20:269-284. [Google Scholar]
- 2. Swanson AB, Hagert CG, Swanson GD. Evaluation of impairment of hand function. J Hand Surg Am. 1983;8:709-722. [DOI] [PubMed] [Google Scholar]
- 3. Claire MD, Bernard A, Chung YS, et al. Thumb function and electromyography result after modified Camitz tendon transfer. J Hand Surg Asian Pac. 2017;22:275-280. [DOI] [PubMed] [Google Scholar]
- 4. Waitayawinyu T, Numnate W, Boonyasirikool C, et al. Outcomes of endoscopic carpal tunnel release with ring finger flexor digitorum superficialis opponensplasty in severe carpal tunnel syndrome. J Hand Surg Am. 2019;44(12):1095.e1-1095.e7. [DOI] [PubMed] [Google Scholar]
- 5. Hirakawa A, Komura S, Nohara M, et al. Opponensplasty by the palmaris longus tendon to the rerouted extensor pollicis brevis transfer with endoscopic carpal tunnel release in severe carpal tunnel syndrome. J Hand Surg Am. 2021;46(11):1033.e1-1033.e7. [DOI] [PubMed] [Google Scholar]
- 6. Liverneaux PA, Ichihara S, Hendriks S, et al. Fractures and dislocation of the base of the thumb metacarpal. J Hand Surg Eur Vol. 2015;40(1):42-50. [DOI] [PubMed] [Google Scholar]
- 7. Zhang X, Wang T, Wan S. Minimally invasive thumb carpometacarpal joint arthrodesis with headless screws and arthroscopic assistance. J Hand Surg Am. 2015;40(1):152-158. [DOI] [PubMed] [Google Scholar]
- 8. Kapandji A. Clinical test of apposition and counter-apposition of the thumb. Ann Chir Main. 1986;5(1):67-73. [DOI] [PubMed] [Google Scholar]
- 9. Cooney WP, III, Lucca MJ, Chao EY, et al. The kinesiology of the thumb trapeziometacarpal joint. J Bone Joint Surg Am. 1981;63(9):1371-1381. [PubMed] [Google Scholar]
- 10. Kuroiwa T, Nimura A, Takahashi Y, et al. Device development for detecting thumb opposition impairment using carbon nanotube-based strain sensors. Sensors. 2020;20:3998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Posner MA, Kapila D. Restoration of opposition. Hand Clin. 2012;28:27-44. [DOI] [PubMed] [Google Scholar]
- 12. Kuroiwa T, Nimura A, Suzuki S, et al. Measurement of thumb pronation and palmar abduction angles with a small motion sensor: a comparison with Kapandji scores. J Hand Surg Eur Vol. 2019;44(7):728-733. [DOI] [PubMed] [Google Scholar]
- 13. Tonkin M. Thumb opposition: its definition and my approach to its measurement. J Hand Surg Eur Vol. 2020;45(3):315-317. [DOI] [PubMed] [Google Scholar]
- 14. Cheema TA, Cheema NI, Tayyab R, et al. Measurement of rotation of the first metacarpal during opposition using computed tomography. J Hand Surg Am. 2006;31(1):76-79. [DOI] [PubMed] [Google Scholar]
- 15. Kimura T, Takai H, Azuma T, et al. Motion analysis of the trapeziometacarpal joint using three-dimensional computed tomography. J Hand Surg Asian Pac Vol. 2016;21(1):78-84. [DOI] [PubMed] [Google Scholar]
- 16. Kawanishi Y, Oka K, Tanaka H, et al. In vivo 3-dimensional kinematics of thumb carpometacarpal joint during thumb opposition. J Hand Surg Am. 2018;43(2):182.e1-182.e7. [DOI] [PubMed] [Google Scholar]
- 17. Signori A, Sormani MP, Schiavetti I, et al. Quantitative assessment of finger motor performance: normative data. PLoS ONE. 2017;12(10):e0186524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Kuroiwa T, Fujita K, Nimura A, et al. A new method of measuring the thumb pronation and palmar abduction angles during opposition movement using a three-axis gyroscope. J Orthop Surg Res. 2018;13:288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Julious SA. Sample size of 12 per group rule of thumb for a pilot study. Pharmaceut Statist. 2005;4:287-291. [Google Scholar]
- 20. Walter SD, Eliasziw M, Donner A. Sample size and optimal designs for reliability studies. Stat Med. 1998;17:101-110. [DOI] [PubMed] [Google Scholar]
- 21. Barakat MJ, Field J, Taylor J. The range of movement of the thumb. Hand (NY). 2013;8:179-182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Dilokhuttakarn T, Naito K, Kinoshita M, et al. Evaluation of thenar muscles by MRI in carpal tunnel syndrome. Exp Ther Med. 2017;14(3):2025-2030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Iwase M, Matsuura Y, Kuniyoshi K, et al. Biomechanical evaluation of opponensplasty for low median palsy: a cadaver study. J Hand Surg Glob Online. 2021;3(2):74-80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Halilaj E, Moore DC, Patel TK, et al. Thumb carpometacarpal joint congruence during functional tasks, thumb range-of-motion activities. Annu Int Conf IEEE Eng Med Biol Soc. 2014;2014:4354-4357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Glickel SZ, Gupta S. Ligament reconstruction. Hand Clin. 2006;22:143-151. [DOI] [PubMed] [Google Scholar]
- 26. Voermans NC, Schelhaas HJ, Munneke M, et al. Dissociated small hand muscle atrophy in aging: the “senile hand” is a split hand. Eur J Neurol. 2006;13(12):1381-1384. [DOI] [PubMed] [Google Scholar]