Abstract
Background:
Nerve injuries from gunshot wounds (GSWs) to the upper arm can cause significant morbidity and loss of function. However, indications for surgical exploration and nerve reconstruction remain unclear as both low- and high-grade injuries can present with an abnormal neurological examination.
Methods:
Adult patients presenting with a history of isolated GSW to the upper arm between 2010 and 2019 at a single urban level 1 trauma center were screened for inclusion in this retrospective study. Patient demographics, neurological examination findings, concurrent injuries, and intraoperative findings were gathered. Bivariate analysis was performed to characterize factors associated with nerve injuries.
Results:
There were 139 adult patients with isolated brachial GSWs, and 49 patients (35%) presented with an abnormal neurological examination and significantly associated with concurrent humerus fractures (39% vs 21%, P = .026) and brachial artery injuries (31% vs 2%, P < .001). Thirty of these 49 patients were operatively explored. Fifteen patients were found to have observed nerve injuries during operative exploration including 8 patients with nerve transections. The radial nerve was the most commonly transected nerve (6), and among the 16 contused nerves, the median (8) was most common.
Conclusion:
Nerve injury from upper arm GSWs is common with directly traumatized nerves confirmed in at least 39% and nerve transection in at least 16% of patients with an abnormal neurological examination. Timely referral to a hand and/or peripheral nerve surgeon for close clinical follow-up, appropriate diagnosis, and any necessary surgical reconstruction with nerve grafts, tendon transfers, and nerve transfers is recommended.
Keywords: firearm injury, gunshot wound, upper extremity, nerve injury, upper arm, brachium, nerve transfer, tendon transfer, nerve graft
Introduction
Gunshot wounds (GSWs) are a leading cause of morbidity and mortality in the United States, which possesses one of the highest rates of firearm injury in the developed world.1,2 Nonfatal gunshot injuries often result in significant functional disability and have only continued to increase in prevalence.3,4 The extremities are involved in over 60% of nonfatal gunshot injuries, with the upper extremities comprising roughly one-third of all GSWs.4,5 Nerve injuries in upper extremity GSWs greatly contribute to compromised function and persistent disability if they are not appropriately recognized and treated. 6
Firearm injuries comprise a heterogenous spectrum of complex injuries that cause tissue damage via multiple mechanisms.7,8 Functional deficits from traumatic nerve injuries often ensue secondary to neurapraxia, axonotmesis, and/or neurotmesis. 9 Nerve injuries are typically difficult to characterize under ideal circumstances, and appropriate categorization of GSW-related nerve injuries is especially challenging in the face of other concomitant injuries.10,11 Clinically, these patients present with visible traumatic injury, pain, and an abnormal neurological examination consisting of sensory and motor deficits, and it is routinely difficult to immediately determine whether these findings represent a severe nerve injury. Electrodiagnostic (EDX) studies at the time of injury are not informative for classifying neuropraxic (Sunderland I), axonotmetic (Sunderland II/III), or neurotmetic (Sunderland IV/V) injuries. 12 Although complete nerve transections clearly require surgical intervention and are typically treated with nerve allograft or autograft, indications for nerves injuries remaining in at least partial continuity are not well defined. A wide range of treatments for these poorly defined nerve injuries have been described to include observation, rehabilitation, surgical decompression, surgical neurolysis, tendon transfer, and nerve transfer.6,13 -15
Given the dense anatomy of the upper extremity, a multidisciplinary surgical team (orthopedic, vascular, and plastic surgery) is required to appropriately diagnose and treat the full scope of these injuries. However, limited data exist on patients with nerve injuries from isolated upper arm GSWs, and information regarding injury pattern and clinical management is scarce. The purpose of this study is to characterize the presentation and management of isolated GSWs to the upper arm with an emphasis on the identification and management of nerve injury.
Methods
A retrospective cohort study at an urban level 1 trauma center was performed following approval by our Institutional Review Board. All adult patients who sustained upper extremity GSWs over a 10-year period (2010-2019) were reviewed. Patients were identified using International Classification of Diseases, Ninth Revision (ICD-9) and International Classification of Diseases, Tenth Revision (ICD-10) codes, and electronic medical records were reviewed to confirm upper extremity GSW. Patients with an isolated firearm injury to any part of the upper extremity between but not including the shoulder and the elbow joints met inclusion criteria. Patients with any firearm injury outside of the brachium, with multiple GSWs, who died in the emergency department, and patients less than 18 years of age at the time of injury were excluded. Demographic information, mechanism, injury pattern, treatment, complications, and clinical outcomes were collected.
For the purposes of determining injury to specific structures, injury to the humerus was determined by radiographic evaluation and orthopedic surgery clinical documentation. For vascular injuries to the brachial artery, injury was confirmed by computed tomographic angiogram and vascular surgery clinical documentation. The respective operative notes were reviewed to determine the type of surgical repair, if any, that these patients underwent.
Orthopedic and plastic surgery clinical notes were reviewed to determine the presence of an abnormal neurological examination distal to the site of upper arm injury as well as any putative nerve distribution corresponding to the median, ulnar, radial, or musculocutaneous nerve. Sensory deficit was defined as any distal numbness or decreased sensation corresponding to any known nerve distribution on presentation. Motor deficit was defined as any distal weakness or absence of motor function corresponding to any known nerve distribution on presentation.
Statistical analysis was conducted in R Version 4.0.2 using the tidyverse package Version 1.3.0 (R Foundation, Vienna, Austria). 16 Intergroup comparisons were conducted with unpaired t tests, 1-way analysis of variance, Fisher’s exact test, or chi-squared testing. The threshold for significance was defined at P < .05.
Results
Population Characteristics
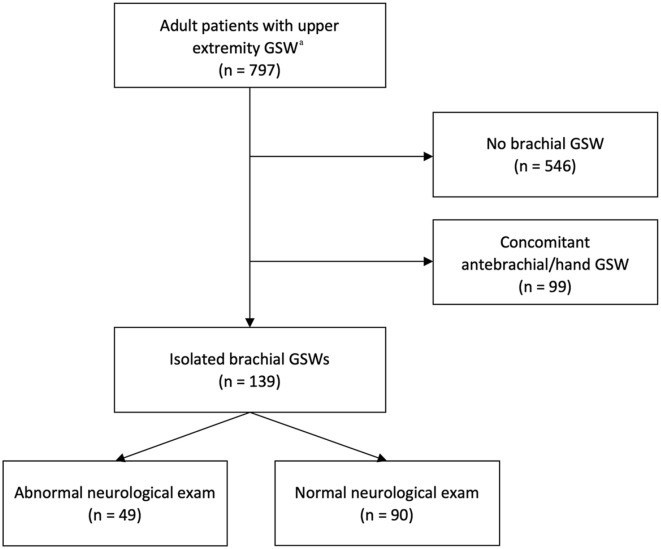
Seven hundred and ninety-seven adult patients with GSWs to the upper extremity were identified. After applying the above exclusion criteria, the study cohort consisted of 139 patients with isolated brachial GSWs (Figure 1). Demographically, most patients in this cohort were young (median age 24 years), black/African American (94%), and men (86%). Most of these patients were healthy, with 92% having no medical comorbidities. Most patients used tobacco products regularly (56%) with 39% endorsing other substance use. The left arm was affected 55% of the time (Table 1).
Figure 1.
Study design and patient cohort flowchart.
Note. GSW = gunshot wound.
aThirteen patients did not survive following GSW.
Table 1.
Patient Demographics and Baseline Clinical Characteristics.
| Patient Characteristic | No. (%) |
|---|---|
| Total | 139 |
| Age, median (SD) | 24 (9) |
| Gender | |
| Male | 120 (86) |
| Female | 19 (14) |
| Race | |
| Black | 130 (94) |
| White | 7 (5) |
| Asian | 1 (1) |
| Unknown | 1 (1) |
| Comorbidities | |
| Diabetes | 3 (2.2) |
| Immunosuppression | 2 (1.4) |
| Renal | 2 (1.4) |
| Psych | 5 (4) |
| None | 128 (92) |
| Active drug use | |
| Yes, intravenous | 4 (3) |
| Yes, not intravenous | 50 (36) |
| No | 80 (57) |
| Unknown | 6 (4) |
| Tobacco use | |
| Yes | 78 (56) |
| No | 57 (41) |
| Mechanism of injury | |
| Violence | 137 (99) |
| Self | 1 |
| Accidental | 1 |
| Arm involved | |
| Right | 62 (45) |
| Left | 77 (55) |
Concomitant Injury Distribution
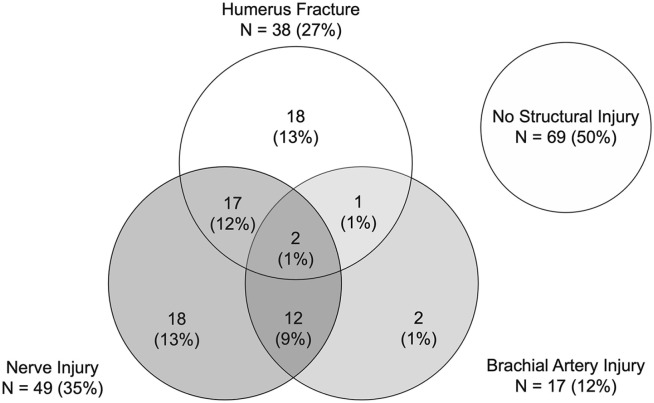
Sixty-nine patients (50%) had no humerus fracture, brachial artery injury, or an abnormal neurological examination. Of the 70 patients with structural injuries, 38 patients (27%) presented with a humerus fracture, 17 patients (12%) with a brachial artery injury, and 49 patients (35%) with an abnormal neurological examination (Figure 2). Thirty-two patients (23%) had concomitant injuries.
Figure 2.
Distribution of bone, vascular, and nerve injuries. Venn diagram demonstrates the distribution of isolated and concurrent injuries sustained in the study population of isolated brachium gunshot wounds.
Abnormal Neurological Examination
Of the 49 patients presenting with an abnormal neurological examination, 41 had a sensory deficit (84%) and 40 had a motor deficit (82%), whereas 32 had a mixed motor/sensory deficit (65%; Supplemental Table 1). Patients with an abnormal neurological examination were more likely to present with a humerus fracture (P = .026) and brachial artery injury (P < .001) at 39% and 29% compared with 19% and 3% of patients with a normal examination, respectively (Table 2). The level of humerus fracture was significantly associated with likelihood of nerve injury (P < .003). On post hoc adjusted z-score analysis, a middle-third humerus fracture was associated with a clinical nerve deficit (P = .048), whereas a proximal-third humerus fracture was significantly associated with no nerve deficit (P < .004). 17 Overall level of GSW to the brachium was significantly associated with likelihood of clinical nerve deficit (P < .002). With post hoc adjusted z-score analysis, a GSW to the upper-third brachium was significantly associated with no clinical nerve deficit (P < .001). 17
Table 2.
Associated Injury Characteristics for an Abnormal Neurological Examination Following Upper Arm Gunshot Wounds.
| Injury Characteristic | Total | Abnormal examination | Normal examination | P value |
|---|---|---|---|---|
| No. (%) | 139 | 49 (35) | 90 (65) | |
| Mechanism of injury | .293 | |||
| Violence | 137 | 49 | 88 | |
| Self | 1 | 0 | 1 | |
| Accidental | 1 | 0 | 1 | |
| Arm involved | .959 | |||
| Right | 62 | 22 | 40 | |
| Left | 77 | 27 | 50 | |
| Humerus fracture | 38 (27) | 19 (39) | 19 (21) | .026 |
| Location of humerus fracture | .003 | |||
| Proximal third | 10 | 1 | 9 | |
| Middle third | 16 | 11 | 5 | |
| Distal third | 12 | 7 | 5 | |
| Brachial artery injury | 17 (12) | 14 (29) | 3 (2) | <.001 |
| Transection | 16 | 14 | 2 | |
| Dissection | 1 | 0 | 1 | |
| Location of gunshot wound | .002 | |||
| Proximal brachium | 41 | 4 | 37 | |
| Middle brachium | 66 | 28 | 38 | |
| Distal brachium | 32 | 17 | 15 |
Note. Nerve deficits were significantly more likely to be present in the event of a humerus fracture or brachial artery injury.
Injury Treatment
Forty-one patients underwent surgical exploration and repair of damaged structures with 32 patients (78%) taken acutely within 48 hours. Of the 38 patients with humerus fractures, 19 (50%) were treated surgically, with plate and screw fixation being the most common technique. Of the 17 patients with brachial artery injuries, 16 (94%) were repaired surgically, with autograft being the most common vascular reconstruction (Table 3).
Table 3.
Operative Management of Upper Arm Gunshot Wounds.
| Injury Characteristic | No. (%) |
|---|---|
| Total | 139 |
| Operative treatment | 41 (29) |
| Acute (<48 h) | 32 (23) |
| Delayed (>48 h) | 9 (6) |
| Humerus fracture | 38 (27) |
| Plate fixation | 15 (11) |
| Intramedullary nail | 3 (2) |
| External fixation | 1 (1) |
| Nonoperative | 20 (14) |
| Brachial artery injury | 17 (12) |
| Autograft | 13 (9) |
| Allograft | 2 (1) |
| Primary repair | 1 (1) |
| Nonoperative | 1 (1) |
| Compartment syndrome | 8 (6) |
| Fasciotomy | 8 (6) |
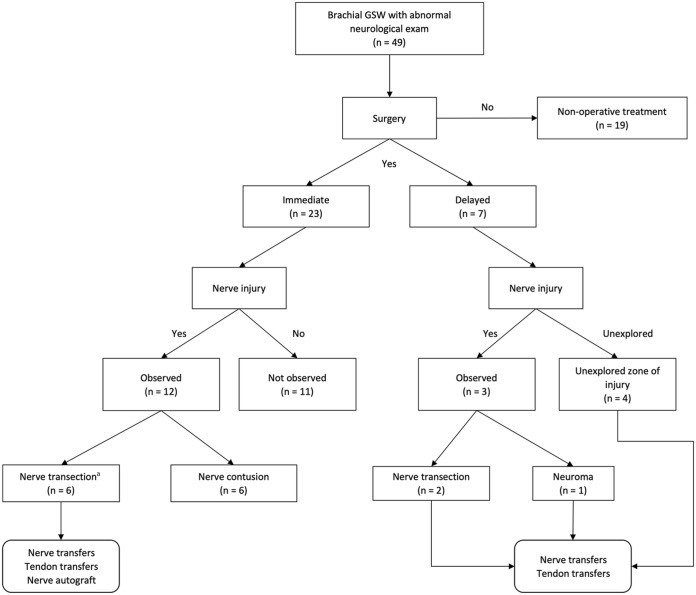
Of the 49 patients presenting with abnormal neurological examination, 30 patients (61%) underwent surgery. Twenty-three patients (47%) underwent acute operative exploration (mean 0.6 days, range 0-4 days) for humerus fracture or brachial artery injury initially. Visible nerve trauma was noted in 12 patients out of the 23 patients (52%) undergoing acute surgery, comprising 6 nerve transections (4 radial, 1 median, 1 ulnar) and 14 nerve contusions (7 median, 5 ulnar, 1 musculocutaneous, 1 radial; Table 4). No immediate nerve reconstructions were performed at the time of acute exploration, but 4 patients with severe nerve injuries went on to delayed nerve grafting, nerve transfer, and/or tendon transfers at 3 to 11 months postinjury (Figure 3).
Table 4.
Operative Findings in Patients With an Abnormal Neurological Examination.
| Operative findings (30 patients) | Acute (23 patients) | Delayed (7 patients) | ||||
|---|---|---|---|---|---|---|
| Injury Finding | Contusion | Transection | Contusion | Transection | Contusion | Transection |
| Radial | 1 | 6 | 1 | 4 | 0 | 2 |
| No deficit | 0 | 0 | 0 | 0 | — | 0 |
| Sensory deficit | 1 | 6 | 1 | 4 | — | 2 |
| Motor deficit | 0 | 6 | 0 | 4 | — | 2 |
| Musculocutaneous | 1 | 0 | 1 | 0 | 0 | 0 |
| No deficit | 0 | — | 0 | — | — | — |
| Sensory deficit | 1 | — | 1 | — | — | — |
| Motor deficit | 1 | — | 1 | — | — | — |
| Median | 8 | 1 | 7 | 1 | 1 a | 0 |
| No deficit | 0 | 0 | 0 | 0 | 0 | — |
| Sensory deficit | 7 | 1 | 6 | 1 | 1 | — |
| Motor deficit | 8 | 1 | 7 | 1 | 1 | — |
| Ulnar | 6 | 1 | 5 | 1 | 1 a | 0 |
| No deficit | 0 | 0 | 0 | 0 | 0 | — |
| Sensory deficit | 5 | 1 | 4 | 1 | 1 | — |
| Motor deficit | 6 | 1 | 5 | 1 | 1 | — |
| Total | 16 | 8 | 14 | 6 | 2 | 2 |
Neuroma-in-continuity.
Figure 3.
Diagnostic and surgical management framework of patients with an abnormal neurological examination.
Note. GSW = gunshot wound.
aIncludes concomitant nerve transection and contusion injuries.
aIncludes concomitant nerve transection and contusion injuries.Seven patients (14%) with an abnormal neurological examination underwent delayed operative treatment (mean 213 days, range 18-637 days postinjury) for persistent nerve dysfunction that failed conservative treatment. Visible nerve trauma was confirmed in 3 patients (43%) following direct exploration of the injury with 2 radial nerve transections, and 1 patient presenting with median and ulnar neuromas-in-continuity. The zone of injury was not directly explored in the other 4 patients as they only underwent functional reconstruction with distal nerve and tendon transfers (Figure 3). Lack of functional recovery is nearly certainly attributable to severe nerve, but these patients were not classified as such without visual confirmation.
Follow-up for this patient cohort was limited and precluded meaningful reporting of outcomes. Median length of follow-up for the overall cohort of 139 patients with brachium GSWs was 16 days, with many not returning for any care after being seen in the emergency room. Of the 49 patients with clinical nerve deficits, median length of follow-up was 75 days, which was deemed insufficient for the meaningful comparison of clinical nerve outcomes.
Discussion
Gunshot wound injuries to the upper arm cause significant disability and decreased quality of life for many years beyond the acute phase of injury.1,18,19 In concordance with many other studies, the data presented here find that most patients with isolated GSWs to the upper arm tend to be healthy men under 30 years of age, overwhelmingly of African American descent, and are victims of violence.4,20 For many of these patients, long-term health impact, economic disability, and long-term pain can be caused by the loss of function through permanent neurovascular damage. 21
Traumatic nerve injuries from GSWs to the upper extremity have been previously described in many studies.10,11,19,22 -25 Due to differential cross-sectional proportions of tissue types from proximal to distal along the upper extremity, studies examining general extremity injuries lack the specificity to guide clinical judgment for treating GSW to the brachium. In one of the largest studies to date, a national trauma database cohort of 6987 patients with any upper/lower extremity GSW reported a fracture rate of 22%, vascular injury rate of 6%, and nerve injury rate of 3.6%. 19 When narrowed to shoulder-fingertip upper extremity GSW, recent reports describe a fracture rate of 70% to 80%, vascular injury rate of 8% to 23%, and nerve injury rate of 15% to 30%.6,26,27 More recently, studies of GSWs limited to the forearm and hand report higher rates of fracture, vascular injury, and nerve injury.28 -31 However, many of these upper extremity studies likely overestimate these injuries as only patients with known fractures or operatively managed patients are included. This information is thus of limited applicability when considering brachial GSWs.
At the authors’ institution, isolated upper arm GSWs represent a distinct injury pattern that commonly comes to the attention of the plastic, orthopedic, and vascular surgery services. In this group, we observed a humerus fracture rate of 27%, brachial artery injury rate of 12%, and an abnormal neurological examination in 35% of patients. The rate of nerve dysfunction is less than the 45% rate reported by Elstrom et al 31 in their study of forearm GSWs suggesting that the larger cross-section of the arm compared with the forearm may reduce the likelihood of nerve deficits. In comparison, the combined arm and forearm GSW series presented by Pannell et al 6 report a 63% rate of nerve deficit although their inclusion of only operatively managed patients likely oversamples patients with an abnormal neurological examination. This study finds that concomitant humerus fractures, especially those of the middle third, were 2 times more likely and brachial artery injuries were 15 times more likely to be significantly associated with nerve dysfunction. Stated otherwise, 82% of patients with brachial artery injury and 50% of patients with humerus fracture also presented with nerve deficits. Clinicians assessing these GSW patients should then have heightened suspicion for nerve injury when presented with these injuries.
The reporting of nerve dysfunction after ballistic injury is highly variable because GSWs injure nerves in various ways—direct trauma, shock, thermal, or compression.7,8,32 For this reason, this study sorts patients who underwent operative exploration with direct visualization of nerve injuries from those who were not explored at all, as well as those surgically treated in acute compared with delayed fashion. Operative exploration in 30 of the 49 patients with clinically apparent nerve deficits found 15 patients to have visually apparent nerve trauma. The most commonly lacerated nerve was the radial nerve in 20% of all operatively explored patients, likely secondary to near the humerus and its risk of damage in the event of fracture.33,34 In contrast, a combined arm and forearm GSW series reported that the most commonly lacerated nerve was the ulnar nerve, whereas a retrospective review of 1565 patients with any surgically managed peripheral nerve trauma reported the median nerve to be the most often lacerated.6,35 These differences are likely explained by the mixing of arm and forearm GSWs in various proportions by other studies. The study here also reports the most commonly contused nerve was the median nerve found in 27% of all operatively explored patients, which again differs from prior studies that found the ulnar nerve to be most commonly contused, likely reflecting a differential risk profile between the arm and forearm.6,36
Although it is impossible to know the true incidence of nerve injury without operative exploration in every patient, we can provide an estimate based on the data presented in this study. These estimation ranges are constructed using opposite assumptions surrounding missing data to provide upper and lower bounds of a range presumed to contain the true value. Of the 23 brachial GSW patients with an abnormal neurological examination acutely explored, 12 (52%) were found to have definitive nerve injury. Combining this statistic with the remaining 7 patients who underwent delayed nerve reconstruction for persistent nerve dysfunction, and the 19 nerve deficit patients who remain uncharacterized, we can estimate that the incidence of any appreciable nerve injury among patients with an abnormal neurological examination lies between 39% and 78% (19-38 out of 49 total nerve deficit patients). A similar calculation for estimating the incidence of true nerve transection yields 16% to 63% (8-31 out of 49 total patients; Figure 3).
The expectation of neuropraxic injury and impending functional recovery after GSW has led to a bias toward passive watchful waiting in cases where early exploration was not undertaken. 37 While this may be a reasonable approach, our calculated 16% to 63% rate of nerve transection and 21% to 67% rate of confirmed nerve injury underscores that severe nerve injuries that may not improve without surgery are relatively common. This finding is in agreement with a recent study that reported no improvement in 32% to 40% of upper extremity GSW patients. 26 As such, surgically unexplored patients should not be categorically assumed to have neuropraxic injury, and impending recovery should not always be expected. Rather, close follow-up with a hand and/or peripheral nerve surgeon is strongly suggested so higher grade Sunderland III to VI injuries that would benefit from surgery can be appropriately treated.
At our institution, we now believe that efforts aimed at the early identification of severe nerve injuries represent an opportunity for improved care. At minimum, this should include intraoperative nerve examination when a vascular injury or humerus fracture is being treated acutely. More complex cases where the anatomy or injury severity is less obvious may require intraoperative assessment by a hand or peripheral nerve surgeon. Intraoperative assessment must necessarily be followed by careful documentation of the findings, especially if the examining surgeon will not ultimately be following the patient’s nerve recovery and making decisions regarding potential reconstruction. When early exploration is not otherwise indicated, close clinical follow-up is critical, and impending recovery should not be assumed. Even when identified in a late fashion, many of these patients may be treated with tendon transfers and nerve transfers for functional reconstruction (Figure 3). 38 In addition to EDX evaluation, ultrasound, and/or magnetic resonance imaging, neurography may be useful for the early identification of severe nerve injury that would benefit from nerve reconstruction or lower grade nerve injury that might benefit from distal decompression. 35 Ultrasound is also increasingly being used at 3 to 6 weeks post-GSW to help early identification of nerve transection injuries and is useful after resolution of injury-related hematoma and profound swelling.
Strengths of this study include the long data collection period and high patient volume at a large level 1 trauma center, which allowed for the focused investigation of upper arm GSWs instead of the general upper extremity. However, despite screening nearly 800 upper extremity adult GSW patients, our study remains too small for detailed analysis of subgroups based on vascular/osseous/nerve injury pattern. Given the civilian environment and incidence of interpersonal violence (99%) in the study, the type of firearm was unable to be determined from the electronic medical record; however, most GSWs were most likely caused by handguns, and so these results may be less applicable to military scenarios.20,39 Furthermore, the preoperative and postoperative assessments of nerve injury were performed retrospectively and are inherently subjective to some degree. Intraoperative assessment of nontransecting nerve injury is also somewhat subjective, and it is possible that some nerve injuries were unappreciated at the time of orthopedic or vascular exploration. Finally, comprehensive outcomes reporting in this patient cohort were limited by heterogeneity in population, injury characteristics, and treatment strategy and exacerbated by incomplete follow-up. Prior attempts from our institution to ascertain longer term follow-up in a nontraumatic population over the same time period resulted in a less than 15% response rate, and similar efforts are less likely to be beneficial in this more challenging population. 40 Prospective enrollment of patients is thus needed to conclusively determine surgical treatment algorithms.
Conclusion
Management of nerve injuries from upper arm GSWs remains without a clear algorithm for diagnosis and treatment. Surgeons should approach patients with concurrent humerus fractures, especially middle-third fractures, and brachial artery injuries with heightened suspicion for nerve injuries. Observable nerve trauma is relatively common with directly traumatized nerves in at least 39% and nerve transection in at least 16% of patients with clinical nerve deficits. Operative exploration for treatment of vascular or bony injury represents an early opportunity for nerve exploration by a hand and/or peripheral nerve surgeon, which may be helpful in triaging nerve injuries to reconstruction or expectant management. If surgical exploration is not undertaken, there is a substantial chance that nerve recovery may not be forthcoming. Timely referral to a hand and/or peripheral nerve surgeon is recommended for close observation and potential functional reconstruction with nerve grafts, tendon transfers, and nerve transfers.
Supplemental Material
Supplemental material, sj-docx-1-han-10.1177_15589447231221170 for Brachial Gunshot Wounds: Injury Patterns and Considerations for Managing the Abnormal Neurological Examination by David Chi, Damini Tandon, Adam G. Evans, Danielle J. Brown, Rachael M. Payne, Amelia C. Van Handel, Kevin G. Shim, Susan E. Mackinnon and Mitchell A. Pet in HAND
Footnotes
Supplemental material is available in the online version of the article.
Ethical Approval: This study was approved by our institutional review board.
Statement of Human and Animal Rights: All information in this study was deidentified and did not involve human or animal subjects.
Statement of Informed Consent: All information in this study was deidentified and did not involve human or animal subjects.
The author(s) declared the following potential conflicts of interest with respect to the research, authorship, and/or publication of this article: MAP has received research funding from 3M and Checkpoint and is a scientific consultant for KLISBio. DC, DT, AGE, DJB, RMP, ACVH, KGS, and SEM have no financial disclosures or conflicts of interest to report.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iDs: David Chi  https://orcid.org/0000-0003-3902-5136
https://orcid.org/0000-0003-3902-5136
Adam G. Evans  https://orcid.org/0000-0001-8535-7583
https://orcid.org/0000-0001-8535-7583
Amelia C. Van Handel  https://orcid.org/0000-0002-2591-7961
https://orcid.org/0000-0002-2591-7961
Susan E. Mackinnon  https://orcid.org/0000-0002-5561-6027
https://orcid.org/0000-0002-5561-6027
Mitchell A. Pet  https://orcid.org/0000-0002-5072-1733
https://orcid.org/0000-0002-5072-1733
References
- 1. Bauchner H, Rivara FP, Bonow RO, et al. Death by gun violence: a public health crisis. JAMA. 2017;318(18):1763-1764. [DOI] [PubMed] [Google Scholar]
- 2. Cook A, Osler T, Hosmer D, et al. Gunshot wounds resulting in hospitalization in the United States: 2004-2013. Injury. 2017;48(3):621-627. [DOI] [PubMed] [Google Scholar]
- 3. Cook PJ, Lawrence BA, Ludwig J, et al. The medical costs of gunshot injuries in the United States. JAMA. 1999;282(5):447-454. [DOI] [PubMed] [Google Scholar]
- 4. Fowler KA, Dahlberg LL, Haileyesus T, et al. Firearm injuries in the United States. Prev Med. 2015;79:5-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Dougherty PJ, Vaidya R, Silverton CD, et al. Joint and long-bone gunshot injuries. J Bone Joint Surg Am. 2009;91(4):980-997. [PubMed] [Google Scholar]
- 6. Pannell WC, Heckmann N, Alluri RK, et al. Predictors of nerve injury after gunshot wounds to the upper extremity. Hand. 2017;12(5):501-506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Omid R, Stone MA, Zalavras CG, et al. Gunshot wounds to the upper extremity. J Am Acad Orthop Surg. 2019;27(7):e301-e310. [DOI] [PubMed] [Google Scholar]
- 8. Bartlett CS, Helfet DL, Hausman MR, et al. Ballistics and gunshot wounds: effects on musculoskeletal tissues. J Am Acad Orthop Surg. 2000;8(1):21-36. [DOI] [PubMed] [Google Scholar]
- 9. Kaya Y, Sarikcioglu L. Sir Herbert Seddon (1903-1977) and his classification scheme for peripheral nerve injury. Childs Nerv Syst. 2015;31(2):177-180. [DOI] [PubMed] [Google Scholar]
- 10. Secer HI, Daneyemez M, Tehli O, et al. The clinical, electrophysiologic, and surgical characteristics of peripheral nerve injuries caused by gunshot wounds in adults: a 40-year experience. Surg Neurol. 2008;69(2):143-152; discussion 152. [DOI] [PubMed] [Google Scholar]
- 11. Persad IJ, Reddy RS, Saunders MA, et al. Gunshot injuries to the extremities: experience of a U.K. Injury. 2005;36(3):407-411. [DOI] [PubMed] [Google Scholar]
- 12. Sunderland S. A classification of peripheral nerve injuries producing loss of function. Brain. 1951;74(4):491-516. [DOI] [PubMed] [Google Scholar]
- 13. Pereira C, Boyd JB, Olsavsky A, et al. Outcomes of complex gunshot wounds to the hand and wrist: a 10-year level I urban trauma center experience. Ann Plast Surg. 2012;68(4):374-377. [DOI] [PubMed] [Google Scholar]
- 14. Chi D, Ha AY, Alotaibi F, et al. A surgical framework for the management of incomplete axillary nerve injuries. J Reconstr Microsurg. 2023;39:616-626. [DOI] [PubMed] [Google Scholar]
- 15. Peters BR, Pripotnev S, Chi D, et al. Complete foot drop with normal electrodiagnostic studies: Sunderland “zero” ischemic conduction block of the common peroneal nerve. Ann Plast Surg. 2022;88(4):425-428. [DOI] [PubMed] [Google Scholar]
- 16. R: a language and environment for statistical computing. R Foundation for Statistical Computing, 2020. https://www.R-project.org. Accessed December 13, 2023.
- 17. Beasley MT, Schumacker RE. Multiple regression approach to analyzing contingency tables: post hoc and planned comparison procedures. The Journal of Experimental Education. 1995;64(1):79-93. [Google Scholar]
- 18. Agarwal S. Trends and burden of firearm-related hospitalizations in the United States across 2001-2011. Am J Med. 2015;128(5):484-492. [DOI] [PubMed] [Google Scholar]
- 19. Berg RJ, Okoye O, Inaba K, et al. Extremity firearm trauma: the impact of injury pattern on clinical outcomes. Am Surg. 2012;78(12):1383-1387. [PubMed] [Google Scholar]
- 20. Hooper RC, Shauver MJ, Chou CH, et al. Epidemiology of upper extremity firearm injuries among major trauma hospitals in the United States. Plast Reconstr Surg. 2021;148(3):571-579. [DOI] [PubMed] [Google Scholar]
- 21. Vella MA, Warshauer A, Tortorello G, et al. Long-term functional, psychological, emotional, and social outcomes in survivors of firearm injuries. JAMA Surg. 2020;155(1):51-59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Degiannis E, Levy RD, Sofianos C, et al. Arterial gunshot injuries of the extremities: a South African experience. J Trauma. 1995;39(3):570-575. [DOI] [PubMed] [Google Scholar]
- 23. Dunn JC, Eckhoff MD, Nicholson TC, et al. Combat-Sustained Peripheral Nerve Injuries in the United States Military. J Hand Surg Am. 2021;46(2):148.e1-148.e8. [DOI] [PubMed] [Google Scholar]
- 24. Birch R, Misra P, Stewart MP, et al. Nerve injuries sustained during warfare: part II: outcomes. J Bone Joint Surg Br. 2012;94(4):529-535. [DOI] [PubMed] [Google Scholar]
- 25. Birch R, Misra P, Stewart MP, et al. Nerve injuries sustained during warfare: part I–Epidemiology. J Bone Joint Surg Br. 2012;94(4):523-528. [DOI] [PubMed] [Google Scholar]
- 26. Straszewski AJ, Schultz K, Dickherber JL, et al. Gunshot-related upper extremity nerve injuries at a level 1 trauma center. J Hand Surg Am. 2022;47(1):88e1-88. [DOI] [PubMed] [Google Scholar]
- 27. Kouyoumdjian JA. Peripheral nerve injuries: a retrospective survey of 456 cases. Muscle Nerve. 2006;34(6):785-788. [DOI] [PubMed] [Google Scholar]
- 28. Lenihan MR, Brien WW, Gellman H, et al. Fractures of the forearm resulting from low-velocity gunshot wounds. J Orthop Trauma. 1992;6(1):32-35. [PubMed] [Google Scholar]
- 29. Mehta SK, Dale WW, Dedwylder MD, et al. Rates of neurovascular injury, compartment syndrome, and early infection in operatively treated civilian ballistic forearm fractures. Injury. 2018;49(12):2244-2247. [DOI] [PubMed] [Google Scholar]
- 30. Veltre DR, Tornetta P, 3rd, Krause P, et al. Gunshot fractures of the forearm: a multicenter evaluation. J Orthop Trauma. 2021;35(10):e364-e370. [DOI] [PubMed] [Google Scholar]
- 31. Elstrom JA, Pankovich AM, Egwele R. Extra-articular low-velocity gunshot fractures of the radius and ulna. J Bone Joint Surg Am. 1978;60(3):335-341. [PubMed] [Google Scholar]
- 32. Hollerman JJ, Fackler ML, Coldwell DM, et al. Gunshot wounds: 1. Bullets, ballistics, and mechanisms of injury. AJR Am J Roentgenol. 1990;155(4):685-690. [DOI] [PubMed] [Google Scholar]
- 33. Bercik MJ, Kingsbery J, Ilyas AM. Peripheral nerve injuries following gunshot fracture of the humerus. Orthopedics. 2012;35(3):e349-352. [DOI] [PubMed] [Google Scholar]
- 34. Akhavan-Sigari R, Mielke D, Farhadi A, et al. Study of radial nerve injury caused by gunshot wounds and explosive injuries among Iraqi soldiers. Open Access Maced J Med Sci. 2018;6(9):1622-1626. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Daneyemez M, Solmaz I, Izci Y. Prognostic factors for the surgical management of peripheral nerve lesions. Tohoku J Exp Med. 2005;205(3):269-275. [DOI] [PubMed] [Google Scholar]
- 36. Oberlin C, Rantissi M. Gunshot injuries to the nerves. Chir Main. 2011;30(3):176-182. [DOI] [PubMed] [Google Scholar]
- 37. Omer GE., Jr. Results of untreated peripheral nerve injuries. Clin Orthop Relat Res. 1982;163:15-19. [PubMed] [Google Scholar]
- 38. Davidge KM, Yee A, Kahn LC, et al. Median to radial nerve transfers for restoration of wrist, finger, and thumb extension. J Hand Surg Am. 2013;38(9):1812-1827. [DOI] [PubMed] [Google Scholar]
- 39. Foote CW, Doan XL, Vanier C, et al. Suicide versus homicide firearm injury patterns on trauma systems in a study of the National Trauma Data Bank (NTDB). Sci Rep. 2022;12(1):15672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Bettlach CR, Gibson E, Daines JM, et al. The stigma of digital amputation: a survey of amputees with analysis of risk factors. J Hand Surg Eur Vol. 2022;47(5):461-468. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-docx-1-han-10.1177_15589447231221170 for Brachial Gunshot Wounds: Injury Patterns and Considerations for Managing the Abnormal Neurological Examination by David Chi, Damini Tandon, Adam G. Evans, Danielle J. Brown, Rachael M. Payne, Amelia C. Van Handel, Kevin G. Shim, Susan E. Mackinnon and Mitchell A. Pet in HAND