Abstract
Background
Gastrointestinal cancer is a significant cause of cancer incidence and mortality. Nevertheless, the epidemiology of the burden among adolescents and young adults (AYAs, aged 15–39 years) remains limited in the Asia-Pacific region, despite the region’s significant population. This study aims to explore the gastrointestinal cancer burden among AYAs in the Asia-Pacific region for the year 2019, while also analysing trends from 1990 to 2019 and projecting future trends up to 2044.
Methods
Annual case numbers, age-standardized rates of incidence, death, and disability-adjusted life-years (DALYs) and their estimated annual percentage changes (EAPCs) for gastrointestinal cancers were derived from the Global Burden of Disease, Injuries, and Risk Factors Study 2019. Trends over the next 25 years have also been predicted.
Results
In 2019, there were 117,714 incident cases, 61,578 deaths and 3,483,053 DALYs due to gastrointestinal cancers in the Asia-Pacific region, accounting for 68.5%, 67.6% and 72.4%, respectively, of global gastrointestinal cancers in this population. The highest agestandardized rates occurred in countries with a middle Socio-demographic Index. From 1990 to 2019, there was a decline in the age-standardized rates of incidence, death and DALY attributed to gastrointestinal cancers, with EAPC of −1.10, −2.48 and −2.44, respectively. These rates are expected to stabilize over 25 years, with notable variations in individual gastrointestinal cancers.
Conclusions
Gastrointestinal cancers among AYAs in the Asia-Pacific region have posed a significant burden over the past 30 years and are expected to persist in the coming years.
Keywords: Gastrointestinal cancers, adolescent and young adults, Asia-Pacific region, global burden of disease, disability-adjusted life years, prediction
Introduction
Individuals aged 15–39 years were defined as adolescents and young adults (AYAs) [1,2]. The incidence of cancer among AYAs is a significant concern because it can have far-reaching social consequences, primarily stemming from the potential for prolonged organ dysfunction, diminished fertility and premature mortality [3]. The distinctive cancer biology of AYAs results in a relatively poor treatment response compared to younger and older groups [4]. Unfortunately, this population is usually grouped with adult patients in clinical studies and the assessment of epidemiological patterns is inadequate [1].
Gastrointestinal (GI) cancers are one of the most common cancers worldwide, accounting for 26% of the global cancer incidence and 35% of cancer-related mortality respectively [5]. Oesophageal, gastric and liver cancer are common in Asia. Colorectal and pancreatic cancers are more frequent in Europe and Northern America, with colorectal cancer incidence rates rising rapidly in Asian countries [5,6]. Significant increases in the incidence of all five types of GI cancers have been observed shifting towards the younger generation [7,8].
As reported in studies of AYA cancers [9,10], GI cancers are among the top-ranked cancers, leading to a heavy global burden. The incidence and death cases in some Asian regions are very close to those in high-income North American regions [11]. However, research pertaining to AYA gastrointestinal cancers has primarily focused on developed European and American countries [7,8], with minimal coverage in the Asia-Pacific region, despite the latter representing over half of the global population. The epidemiology of GI cancers is changing in Asia [12,13]. However, estimates of the AYA gastrointestinal cancer burden specific to Asia-Pacific regions are outdated and inadequately assessed [14,15], implying the need for an updated and comprehensive analysis of the AYA cancer burden in Asia-Pacific regions.
The Global Burden of Diseases, Injuries, and Risk Factors Study (GBD) 2019 systematically estimated the burden of 369 diseases and injuries, allowing for further analysis of AYA cancers [16]. To our knowledge, the gastrointestinal cancer burden of AYAs in the Asia-Pacific region has not yet been estimated using GBD data. In this study, using data from the GBD 2019, we aimed to describe the burden of AYAs in the Asia-Pacific region in 2019, highlight the trends from 1990 to 2019, explore the association with the Socio-demographic Index (SDI), investigate the burden in different age groups and predict the trend over the next 25 years. Our findings provide valuable information for GI cancer control strategies and resource allocation in AYAs in the Asia-Pacific region.
Methods
Data source
The detailed presentation of the original data sources and general methodology of the GBD 2019 study has been described in previous studies [16–19]. The original data sources, study protocol and statistical codes used in the current study were obtained from http://ghdx.healthdata.org/gbd-2019/data-input-sources and http://ghdx.healthdata.org/gbd-2019/code/. We extracted yearly crude estimates of various measures of GI cancer burden between 1990 and 2019 from the GBD database using the Global Health Data Exchange query tool (http://ghdx.healt hdata.org/gbd-results-tool). The variables obtained from the database included incident cases, deaths and disability-adjusted life-years (DALYs) among individuals aged 15–39 years in the Asia-Pacific region from 1990 to 2019.
Statistical analysis
ASRs (per 100 000 population) were calculated by summing the products of the age-specific rates (ai) and the number of persons (wi) in the same age subgroup, and then dividing the sum of standard population weights [19,20]. The formula used is as follows:
The estimated annual percentage change (EAPC) was computed to describe the temporal trend in various ASRs within a specified time interval, which was calculated using a regression model. The formula is as follows: y = α + βx+ɛ, where y = ln (ASR), x = calendar year and ε is an error term. In this formula, β determines positive or negative ASR trends. The EAPC was calculated as follows: EAPC = 100 × [exp (β) −1], and the 95% confidence interval (CI) for each quantity was obtained from the linear model [21,22]. When the EAPC value and the lower boundary of the CI are greater than zero, the ASR exhibits an upward trend. Conversely, when the EAPC value and upper boundary of the CI are less than zero, the ASR exhibits a downward trend. Otherwise, the ASR was regarded as stable over time.
The package nordpred in the R program was developed by the Norwegian Cancer Registry and has been shown to perform well in predicting the incidence and mortality trends of cancers [23,24]. The nordpred was applied based on power5 age-period-cohort models to project the future trend of incidence and mortality of GI cancers between 2020 and 2044, taking into account both the change in rates and the population structure. The basic age-period-cohort model is g (λij) = μ + αi + βj + γk, (default link function is λij ^ 0.2, where μ represents the intercept, and αi, βj and γk represent the effect of age, period and cohort, respectively) [25]. In our study, GI cancer incidence and mortality were predicted over a 5-year period (2020–2024, 2025–2029, 2030–2034, 2035–2039 and 2040–2044). The estimated population and standard population structure were collected from the GBD 2019 Population Estimates (https://ghdx.healthdata.org/record/ihme-data/gbd-2019-population-estimates-1950-2019).
All statistical analyses were performed using R statistical software version 4.1.0 (Bell Laboratories, New Jersey in America). Statistical p was set than 0.05. The ggplot2 package in the R program was used to visualize the results.
Results
Burden of GI cancers
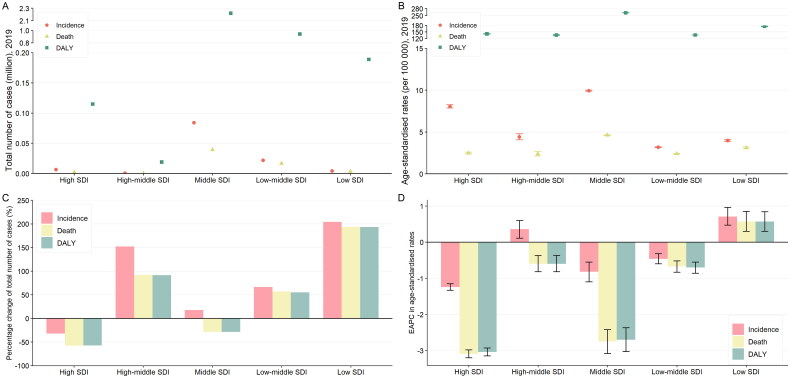
In 2019, there were 117,714 incident cases, 61,578 deaths and 3,483,053 DALYs of GI cancers among AYAs in the Asia-Pacific region, accounting for 68.5%, 67.6% and 72.4% of global GI cancers, respectively, in this population (Table 1 and Supplementary Tables S1–S3). The majority of the incidences, deaths and DALY burdens were concentrated in the middle and low-middle SDI quintiles (Figure 1A). Overall, the middle SDI settings had the highest age-standardized incidence rate (9.94), death rate (4.62) and DALY rate (261.97) (Figure 1B). Colorectal cancer was the greatest contributor to the incidence of GI cancers (41.78%), whereas stomach cancer was the greatest contributor to the death burden (30.61%) and DALY burden (30.60%) (Figures S1–S3).
Table 1.
Age-standardized incidence, death and DALY rates for GI cancers in adolescents and young adults in the Asia-Pacific region in 1990 and 2019 and their temporal trends from 1990 to 2019.
| Characteristics | Age-standardized incidence rate per 100,000 population |
Age-standardized death rate per 100,000 population |
Age-standardized DALY rate per 100,000 population |
||||||
|---|---|---|---|---|---|---|---|---|---|
| 1990 No. (95% CI) | 2019 No. (95% CI) | EAPC No. (95% CI) | 1990 No. (95% CI) | 2019 No. (95% CI) | EAPC No. (95% CI) | 1990 No. (95% CI) | 2019 No. (95% CI) | EAPC No. (95% CI) | |
| Asia-Pacific region | 8.02 (7.97 to 8.07) | 6.77 (6.73 to 6.81) | −1.10 (–1.30 to −0.91) | 6.03 (5.99 to 6.07) | 3.54 (3.51 to 3.57) | −2.48 (–2.74 to −2.22) | 338.20 (337.87 to 338.53) | 200.47 (200.26 to 200.68) | −2.44 (–2.70 to −2.18) |
| Sex | |||||||||
| Male | 9.61 (9.53 to 9.69) | 8.70 (8.64 to 8.76) | −0.80 (–0.96 to −0.63) | 7.34 (7.27 to 7.40) | 4.47 (4.43 to 4.52) | −2.33 (–2.55 to −2.11) | 409.42 (408.91 to 409.93) | 252.08 (251.75 to 252.41) | −2.29 (–2.51 to −2.07) |
| Female | 6.35 (6.28 to 6.41) | 4.77 (4.73 to 4.82) | −1.57 (–1.86 to −1.28) | 4.65 (4.60 to 4.71) | 2.57 (2.54 to 2.61) | −2.69 (–3.03 to −2.35) | 263.15 (262.73 to 263.57) | 147.20 (146.95 to 147.46) | −2.66 (–3.01 to −2.31) |
| SDI quintile | |||||||||
| High | 11.27 (11.05 to 11.50) | 8.06 (7.86 to 8.26) | −1.24 (–1.33 to −1.15) | 5.58 (5.42 to 5.74) | 2.47 (2.37 to 2.59) | −3.09 (–3.20 to −2.98) | 315.03 (313.83 to 316.22) | 141.16 (140.33 to 141.99) | −3.04 (–3.15 to −2.93) |
| High-middle | 3.50 (3.08 to 3.97) | 4.41 (4.07 to 4.78) | 0.36 (0.11 to 0.60) | 2.51 (2.15 to 2.92) | 2.39 (2.14 to 2.66) | −0.60 (–0.82 to −0.37) | 141.95 (139.16 to 144.78) | 135.66 (133.73 to 137.60) | −0.60 (–0.82 to −0.37) |
| Middle | 10.49 (10.42 to 10.57) | 9.94 (9.87 to 10.00) | −0.82 (–1.10 to −0.55) | 8.15 (8.08 to 8.22) | 4.62 (4.58 to 4.67) | −2.75 (–3.08 to −2.42) | 455.42 (454.91 to 455.93) | 261.97 (261.62 to 262.31) | −2.70 (–3.03 to −2.37) |
| Low-middle | 3.45 (3.39 to 3.51) | 3.19 (3.15 to 3.23) | −0.46 (–0.60 to −0.32) | 2.78 (2.72 to 2.83) | 2.40 (2.36 to 2.43) | −0.67 (–0.83 to −0.52) | 158.27 (157.87 to 158.67) | 136.06 (135.79 to 136.34) | −0.70 (–0.86 to −0.55) |
| Low | 3.14 (2.98 to 3.31) | 3.99 (3.87 to 4.11) | 0.71 (0.47 to 0.96) | 2.55 (2.40 to 2.70) | 3.11 (3.01 to 3.22) | 0.57 (0.30 to 0.85) | 143.36 (142.24 to 144.49) | 175.50 (174.70 to 176.30) | 0.57 (0.30 to 0.84) |
| Countries and territories | |||||||||
| Afghanistan | 9.63 (8.47 to 10.91) | 7.67 (7.16 to 8.20) | −0.77 (–0.90 to −0.63) | 8.01 (6.94 to 9.20) | 6.30 (5.84 to 6.79) | −0.82 (–0.97 to −0.68) | 451.89 (443.71 to 460.19) | 354.58 (351.06 to 358.11) | −0.83 (–0.97 to −0.68) |
| American Samoa | 6.38 (0.24 to 34.47) | 7.56 (0.43 to 36.48) | 0.70 (0.58 to 0.83) | 4.61 (0.06 to 31.58) | 5.14 (0.09 to 32.55) | 0.48 (0.35 to 0.61) | 263.48 (193.81 to 351.02) | 294.21 (220.10 to 386.20) | 0.49 (0.36 to 0.62) |
| Australia | 4.47 (3.99 to 5.00) | 5.88 (5.39 to 6.40) | 1.13 (0.96 to 1.30) | 1.78 (1.49 to 2.12) | 1.69 (1.44 to 1.99) | −0.04 (–0.19 to 0.10) | 101.94 (99.60 to 104.33) | 97.71 (95.70 to 99.76) | −0.02 (–0.16 to 0.12) |
| Bangladesh | 3.06 (2.88 to 3.24) | 2.08 (1.97 to 2.19) | −1.60 (–1.79 to −1.41) | 2.49 (2.33 to 2.65) | 1.56 (1.46 to 1.66) | −1.84 (–2.01 to −1.67) | 143.32 (142.10 to 144.55) | 89.89 (89.17 to 90.62) | −1.85 (–2.03 to −1.67) |
| Bhutan | 2.58 (0.86 to 6.07) | 2.31 (1.00 to 4.59) | −0.61 (–0.70 to −0.52) | 2.12 (0.60 to 5.44) | 1.70 (0.62 to 3.78) | −0.99 (–1.08 to −0.90) | 118.91 (104.36 to 135.01) | 96.05 (86.02 to 106.96) | −0.98 (–1.07 to −0.89) |
| Brunei Darussalam | 9.97 (5.18 to 17.48) | 8.26 (4.90 to 13.29) | −0.70 (–1.02 to −0.37) | 6.42 (2.74 to 12.89) | 4.29 (2.00 to 8.30) | −1.41 (–1.73 to −1.10) | 365.55 (332.45 to 401.13) | 243.03 (222.78 to 264.79) | −1.44 (–1.75 to −1.12) |
| Cambodia | 6.55 (5.72 to 7.48) | 5.53 (4.99 to 6.11) | −0.73 (–0.78 to −0.68) | 5.16 (4.42 to 6.00) | 3.91 (3.46 to 4.41) | −1.09 (–1.16 to −1.03) | 299.60 (293.81 to 305.49) | 227.83 (224.31 to 231.40) | −1.09 (–1.15 to −1.02) |
| China | 12.44 (12.34 to 12.54) | 12.53 (12.44 to 12.62) | −0.65 (–0.97 to −0.33) | 9.67 (9.58 to 9.76) | 5.47 (5.41 to 5.53) | −2.85 (–3.21 to −2.48) | 540.38 (539.74 to 541.02) | 309.58 (309.11 to 310.04) | −2.80 (–3.17 to −2.43) |
| Cook Islands | 5.66 (0.00 to 70.91) | 5.50 (0.00 to 77.40) | 0.12 (–0.18 to 0.43) | 3.98 (0.00 to 67.95) | 3.31 (0.00 to 73.19) | −0.33 (–0.63 to −0.02) | 226.13 (128.51 to 371.95) | 187.58 (92.64 to 339.01) | −0.35 (–0.65 to −0.06) |
| Democratic People’s Republic of Korea | 11.67 (10.91 to 12.46) | 8.73 (8.17 to 9.31) | −1.15 (–1.28 to −1.01) | 8.53 (7.88 to 9.22) | 6.06 (5.60 to 6.55) | −1.33 (–1.41 to −1.24) | 479.45 (474.52 to 484.42) | 342.77 (339.25 to 346.32) | −1.30 (–1.39 to −1.22) |
| Fiji | 3.98 (2.05 to 7.03) | 4.26 (2.41 to 7.00) | 0.50 (0.06 to 0.93) | 3.01 (1.37 to 5.79) | 3.05 (1.53 to 5.46) | 0.34 (–0.10 to 0.78) | 172.39 (157.83 to 187.97) | 174.97 (161.63 to 189.12) | 0.35 (–0.10 to 0.80) |
| Guam | 4.52 (0.86 to 14.01) | 7.79 (2.33 to 19.15) | 1.71 (1.48 to 1.94) | 2.70 (0.24 to 11.20) | 4.64 (0.83 to 14.55) | 1.84 (1.64 to 2.05) | 156.41 (126.80 to 191.04) | 264.04 (223.68 to 309.66) | 1.77 (1.58 to 1.96) |
| India | 3.16 (3.10 to 3.22) | 3.12 (3.08 to 3.17) | −0.20 (–0.38 to −0.02) | 2.56 (2.50 to 2.62) | 2.37 (2.33 to 2.41) | −0.41 (–0.60 to −0.22) | 145.91 (145.48 to 146.33) | 134.07 (133.77 to 134.37) | −0.45 (–0.64 to −0.25) |
| Indonesia | 3.53 (3.39 to 3.67) | 3.62 (3.51 to 3.74) | −0.02 (–0.16 to 0.12) | 2.70 (2.58 to 2.83) | 2.37 (2.28 to 2.46) | −0.56 (–0.72 to −0.40) | 154.35 (153.43 to 155.27) | 136.10 (135.41 to 136.80) | −0.54 (–0.70 to −0.38) |
| Iran (Islamic Republic of) | 4.25 (3.96 to 4.55) | 4.42 (4.21 to 4.63) | 0.10 (–0.17 to 0.37) | 3.13 (2.88 to 3.40) | 2.47 (2.32 to 2.63) | −0.75 (–1.01 to −0.49) | 178.74 (176.83 to 180.67) | 141.95 (140.78 to 143.12) | −0.73 (–0.99 to −0.47) |
| Japan | 11.45 (11.14 to 11.76) | 7.09 (6.83 to 7.37) | −1.58 (–1.71 to −1.45) | 4.56 (4.37 to 4.76) | 1.96 (1.82 to 2.10) | −2.98 (–3.10 to −2.87) | 256.56 (255.11 to 258.03) | 112.41 (111.33 to 113.49) | −2.90 (–3.02 to −2.79) |
| Kiribati | 10.98 (2.25 to 33.27) | 11.17 (3.73 to 25.93) | −0.07 (–0.20 to 0.06) | 8.77 (1.35 to 30.04) | 9.07 (2.57 to 23.00) | 0.03 (–0.11 to 0.16) | 498.85 (418.42 to 590.82) | 514.81 (451.65 to 584.48) | 0.02 (–0.12 to 0.15) |
| Lao People’s Democratic Republic | 5.96 (4.72 to 7.44) | 4.51 (3.78 to 5.34) | −1.12 (–1.21 to −1.04) | 4.78 (3.67 to 6.13) | 3.31 (2.69 to 4.04) | −1.41 (–1.49 to −1.34) | 270.30 (261.52 to 279.31) | 188.71 (183.82 to 193.70) | −1.38 (–1.46 to −1.31) |
| Malaysia | 3.47 (3.05 to 3.94) | 4.40 (4.06 to 4.77) | 0.38 (0.14 to 0.63) | 2.49 (2.13 to 2.90) | 2.39 (2.14 to 2.66) | −0.58 (–0.81 to −0.35) | 140.83 (138.04 to 143.66) | 135.24 (133.31 to 137.19) | −0.58 (–0.81 to −0.35) |
| Maldives | 3.06 (0.31 to 12.61) | 2.16 (0.82 to 5.47) | −1.24 (–1.66 to −0.81) | 2.37 (0.14 to 11.56) | 1.18 (0.29 to 4.20) | −2.51 (–2.89 to −2.13) | 132.63 (104.90 to 165.88) | 66.53 (57.56 to 76.99) | −2.48 (–2.85 to −2.09) |
| Marshall Islands | 7.29 (0.25 to 40.24) | 8.50 (1.04 to 30.95) | 0.40 (0.25 to 0.55) | 5.76 (0.09 to 37.73) | 6.60 (0.52 to 27.91) | 0.34 (0.16 to 0.52) | 331.11 (245.70 to 437.62) | 374.15 (300.33 to 460.81) | 0.31 (0.15 to 0.48) |
| Micronesia (Federated States of) | 8.58 (1.76 to 25.72) | 8.65 (1.95 to 24.78) | −0.10 (–0.17 to −0.02) | 6.88 (1.07 to 23.21) | 6.45 (1.02 to 21.51) | −0.35 (–0.44 to −0.26) | 388.66 (325.95 to 460.23) | 368.06 (309.41 to 434.87) | −0.31 (–0.39 to −0.23) |
| Mongolia | 9.54 (7.35 to 12.20) | 10.02 (8.48 to 11.79) | −0.43 (–0.70 to −0.17) | 8.00 (6.00 to 10.49) | 8.07 (6.70 to 9.68) | −0.60 (–0.89 to −0.31) | 442.41 (426.69 to 458.59) | 446.37 (435.75 to 457.21) | −0.61 (–0.90 to −0.32) |
| Myanmar | 5.03 (4.68 to 5.41) | 4.20 (3.93 to 4.48) | −0.87 (–1.02 to −0.73) | 4.00 (3.69 to 4.34) | 2.91 (2.69 to 3.14) | −1.33 (–1.49 to −1.17) | 227.63 (225.24 to 230.05) | 167.27 (165.56 to 168.99) | −1.30 (–1.47 to −1.14) |
| Nauru | 10.39 (0.00 to 123.58) | 10.74 (0.01 to 113.53) | −0.02 (–0.10 to 0.06) | 7.66 (0.00 to 118.56) | 7.40 (0.00 to 107.44) | −0.17 (–0.32 to −0.03) | 434.36 (250.41 to 703.47) | 421.03 (248.89 to 669.19) | −0.16 (–0.31 to −0.02) |
| Nepal | 2.79 (2.39 to 3.23) | 2.29 (2.02 to 2.58) | −0.63 (–0.90 to −0.36) | 2.27 (1.92 to 2.68) | 1.76 (1.53 to 2.02) | −0.83 (–1.08 to −0.58) | 128.30 (125.53 to 131.10) | 99.62 (97.82 to 101.46) | −0.82 (–1.07 to −0.57) |
| New Zealand | 5.48 (4.32 to 6.86) | 6.21 (4.99 to 7.64) | 0.42 (0.29 to 0.54) | 2.44 (1.69 to 3.42) | 2.05 (1.38 to 2.94) | −0.63 (–0.74 to −0.51) | 139.51 (133.37 to 145.86) | 118.26 (112.72 to 124.00) | −0.60 (–0.71 to −0.49) |
| Niue | 6.81 (0.00 to 531.55) | 6.51 (0.00 to 744.84) | −0.43 (–0.55 to −0.31) | 4.85 (0.00 to 527.64) | 3.83 (0.00 to 739.60) | −1.14 (–1.28 to −1.01) | 275.74 (34.30 to 998.22) | 220.11 (9.56 to 1124.66) | −1.10 (–1.24 to −0.97) |
| Northern Mariana Islands | 8.32 (1.04 to 33.11) | 7.72 (0.09 to 56.86) | −0.59 (–0.72 to −0.46) | 5.22 (0.26 to 28.38) | 4.26 (0.00 to 51.14) | −0.82 (–0.94 to −0.69) | 296.49 (232.28 to 374.66) | 243.70 (157.63 to 362.86) | −0.79 (–0.92 to −0.67) |
| Pakistan | 2.63 (2.45 to 2.81) | 3.68 (3.55 to 3.82) | 1.06 (0.81 to 1.32) | 2.12 (1.97 to 2.29) | 2.84 (2.72 to 2.96) | 0.89 (0.61 to 1.17) | 119.01 (117.84 to 120.19) | 159.69 (158.81 to 160.58) | 0.90 (0.62 to 1.17) |
| Palau | 7.38 (0.01 to 72.91) | 8.66 (0.02 to 83.80) | 0.69 (0.59 to 0.78) | 5.24 (0.00 to 69.01) | 5.62 (0.00 to 78.59) | 0.43 (0.30 to 0.55) | 297.06 (180.93 to 461.21) | 317.84 (197.20 to 490.53) | 0.41 (0.29 to 0.52) |
| Papua New Guinea | 3.96 (2.99 to 5.14) | 4.09 (3.48 to 4.78) | 0.16 (0.07 to 0.24) | 3.09 (2.24 to 4.16) | 3.13 (2.60 to 3.75) | 0.12 (0.03 to 0.22) | 175.95 (169.14 to 182.96) | 179.20 (174.99 to 183.49) | 0.13 (0.04 to 0.23) |
| Philippines | 6.75 (6.42 to 7.10) | 5.86 (5.63 to 6.09) | −0.64 (–0.88 to −0.39) | 5.08 (4.79 to 5.38) | 3.96 (3.78 to 4.15) | −1.10 (–1.34 to −0.85) | 287.31 (285.09 to 289.54) | 225.25 (223.84 to 226.66) | −1.06 (–1.30 to −0.82) |
| Republic of Korea | 13.83 (13.32 to 14.35) | 9.29 (8.87 to 9.73) | −1.76 (–1.99 to −1.53) | 9.07 (8.66 to 9.50) | 3.02 (2.78 to 3.27) | −4.25 (–4.44 to −4.05) | 512.44 (509.33 to 515.57) | 171.14 (169.32 to 172.97) | −4.23 (–4.42 to −4.04) |
| Samoa | 3.69 (0.39 to 14.71) | 3.86 (0.71 to 12.12) | 0.02 (–0.08 to 0.12) | 2.83 (0.17 to 13.39) | 2.76 (0.31 to 10.44) | −0.20 (–0.28 to −0.12) | 158.18 (125.16 to 197.58) | 154.19 (126.54 to 186.23) | −0.19 (–0.27 to −0.10) |
| Singapore | 6.10 (4.93 to 7.49) | 3.68 (2.96 to 4.58) | −2.10 (–2.26 to −1.94) | 3.11 (2.29 to 4.15) | 1.12 (0.75 to 1.69) | −3.99 (–4.18 to −3.80) | 174.79 (168.25 to 181.54) | 65.12 (61.96 to 68.44) | −3.85 (–4.05 to −3.66) |
| Solomon Islands | 10.81 (5.37 to 19.68) | 11.66 (7.74 to 16.88) | 0.37 (0.30 to 0.44) | 8.64 (3.86 to 16.93) | 8.89 (5.52 to 13.60) | 0.24 (0.15 to 0.33) | 490.70 (448.38 to 536.11) | 507.12 (479.03 to 536.46) | 0.25 (0.17 to 0.34) |
| Sri Lanka | 2.54 (2.18 to 2.94) | 2.45 (2.13 to 2.82) | −0.64 (–1.03 to −0.26) | 1.85 (1.54 to 2.20) | 1.35 (1.11 to 1.62) | −1.58 (–1.92 to −1.24) | 105.16 (102.79 to 107.58) | 76.73 (74.86 to 78.64) | −1.59 (–1.94 to −1.24) |
| Taiwan (Province of China) | 10.10 (9.47 to 10.77) | 12.76 (12.04 to 13.52) | 0.75 (0.51 to 0.98) | 6.03 (5.54 to 6.54) | 4.52 (4.10 to 4.98) | −1.21 (–1.39 to −1.03) | 340.88 (337.17 to 344.62) | 255.61 (252.36 to 258.90) | −1.22 (–1.40 to −1.04) |
| Thailand | 7.12 (6.78 to 7.46) | 8.42 (8.07 to 8.77) | −0.70 (–1.28 to −0.11) | 5.51 (5.22 to 5.82) | 5.24 (4.97 to 5.52) | −1.37 (–1.95 to −0.79) | 308.54 (306.32 to 310.78) | 293.03 (290.99 to 295.09) | −1.40 (–2.00 to −0.81) |
| Timor-Leste | 3.62 (1.76 to 6.69) | 3.38 (1.85 to 5.75) | −0.25 (–0.74 to 0.25) | 2.94 (1.29 to 5.81) | 2.43 (1.16 to 4.55) | −0.70 (–1.17 to −0.21) | 165.96 (151.31 to 181.70) | 138.82 (127.74 to 150.65) | −0.66 (–1.15 to −0.17) |
| Tokelau | 5.62 (0.00 to 831.31) | 5.87 (0.00 to 898.39) | 0.17 (0.14 to 0.21) | 4.38 (0.00 to 829.03) | 4.02 (0.00 to 894.79) | −0.28 (–0.32 to −0.24) | 248.22 (13.07 to 1246.97) | 229.17 (6.44 to 1300.59) | −0.26 (–0.30 to −0.22) |
| Tonga | 6.22 (0.58 to 26.07) | 6.91 (1.07 to 23.13) | 0.29 (0.12 to 0.47) | 5.02 (0.29 to 24.24) | 5.34 (0.55 to 20.70) | 0.14 (–0.04 to 0.33) | 281.84 (222.64 to 352.67) | 301.77 (246.48 to 365.96) | 0.17 (–0.01 to 0.36) |
| Tuvalu | 7.21 (0.00 to 122.81) | 7.32 (0.00 to 103.64) | 0.18 (0.12 to 0.23) | 5.69 (0.00 to 119.90) | 5.41 (0.00 to 100.12) | −0.01 (–0.07 to 0.04) | 322.73 (163.09 to 574.14) | 307.00 (166.18 to 521.58) | −0.01 (–0.07 to 0.05) |
| Vanuatu | 5.70 (1.15 to 17.26) | 6.88 (2.86 to 14.08) | 0.31 (0.16 to 0.47) | 4.60 (0.70 to 15.64) | 5.44 (1.95 to 12.15) | 0.25 (0.10 to 0.40) | 260.28 (218.09 to 308.49) | 308.33 (276.05 to 343.45) | 0.26 (0.10 to 0.41) |
| Viet Nam | 3.17 (2.95 to 3.41) | 3.87 (3.69 to 4.06) | 1.00 (0.74 to 1.26) | 2.44 (2.25 to 2.65) | 2.18 (2.04 to 2.32) | −0.12 (–0.33 to 0.09) | 136.40 (134.94 to 137.88) | 122.85 (121.81 to 123.91) | −0.09 (–0.30 to 0.13) |
Abbreviations: CI, confidence interval; DALY, disability-adjusted life-year; EAPC, estimated annual percentage change; GI cancers, gastrointestinal cancers; SDI, sociodemographic index.
Figure 1.
Total cancer incidence, death and DALY absolute counts (A) and age-standardized rates (B) in 2019, and percentage changes of cases (C) and EAPC in age-standardized rates (D) from 1990 to 2019 by SDI quintiles due to GI cancers for both sexes in adolescents and young adults in the Asia-Pacific region.
Error bars represent 95% confidence interval (CI). DALY, disability-adjusted life-year; EAPC, estimated annual percentage change; GI cancers, gastrointestinal cancers; SDI, sociodemographic index.
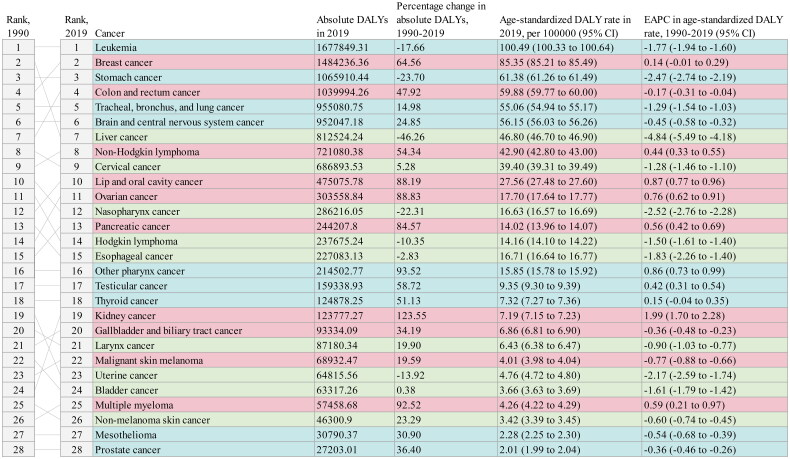
Between 1990 and 2019, the absolute number of incident cases increased by 22.65%. In contrast, the number of deaths and DALYs decreased by −14.08% and −13.95% (Table S1). Distinct alterations in each SDI quantile are shown in Figures 1C and 1D. As for specific disorders of GI cancers from 1990 to 2019, colorectal cancer moved from the seventh cause of all cancers DALYs to the fourth place, with a 47.92% increase in absolute DALYs (Figure 2). However, liver cancer dropped from second to seventh.
Figure 2.
Cancer group rankings by DALYs in 2019 and percentage change from 1990 to 2019 for both sexes in adolescents and young adults in the Asia-Pacific region.
Cancers were ordered by rank in 2019, with lines connecting their ranks in 1990. Colours refer to the directional change in cancer rank from 1990 to 2019: Red signifies an increase in rank, blue signifies no change in rank and green signifies a decrease in rank. CI = confidence interval; DALY = disability-adjusted life-year; EAPC = estimated annual percentage change.
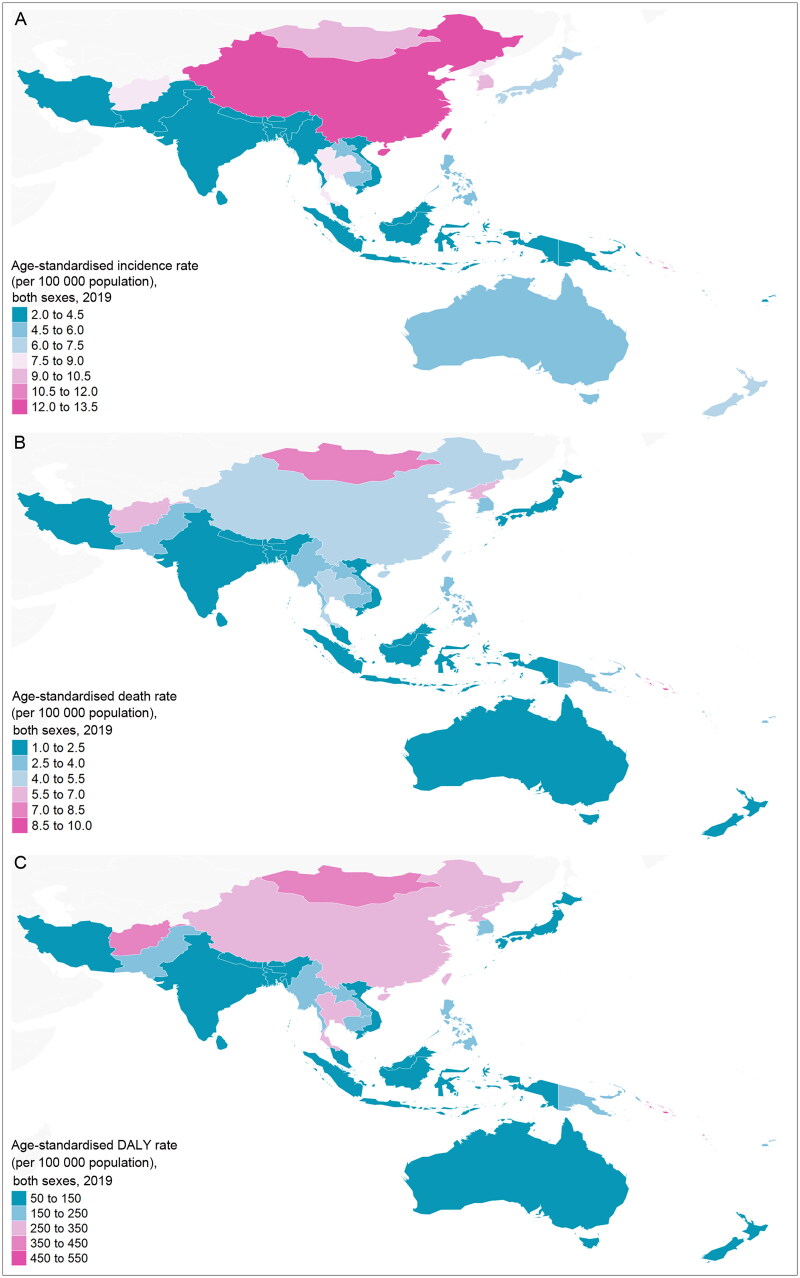
The burden of GI cancers in 2019 and the corresponding EAPCs from 1990 to 2019 exhibited significant heterogeneity across nations at both national and territorial scales. In 2019, China had the highest number of incident cases, deaths and DALYs. The highest age-standardized incidence rate was observed in Taiwan (Province of China) (12.76 per 100,000 population) and the highest age-standardized death rate and DALY rate were observed in Kiribati (9.07 and 514.81, respectively) (Figure 3). Moreover, the age-standardized incidence rate decreased over 30 years in almost half of the countries, and the age-standardized death and DALY rates decreased in almost 70% of the countries (Figures S4–S6). Guam exhibited the highest EAPCs (EAPC = 1.71, 1.84 and 1.77) for the age-standardized incidence, death and DALY rate, respectively. Conversely, Singapore had the lowest EAPC (–2.10) for the age-standardized incidence rate. The Republic of Korea demonstrated the lowest EAPCs (EAPC = −4.25 and −4.23) for age-standardized death and DALY rates, respectively.
Figure 3.
The age-standardised rates of incidence (A), death (B) and DALY (C) due to GI cancers for both sexes in adolescents and young adults in the Asia-Pacific region.
Note: The results for some geographical regions were severely limited by the paucity of data (not just variability in study design but lack of studies) and should be treated with caution. DALY = disability-adjusted life-year; GI cancers = gastrointestinal cancers.
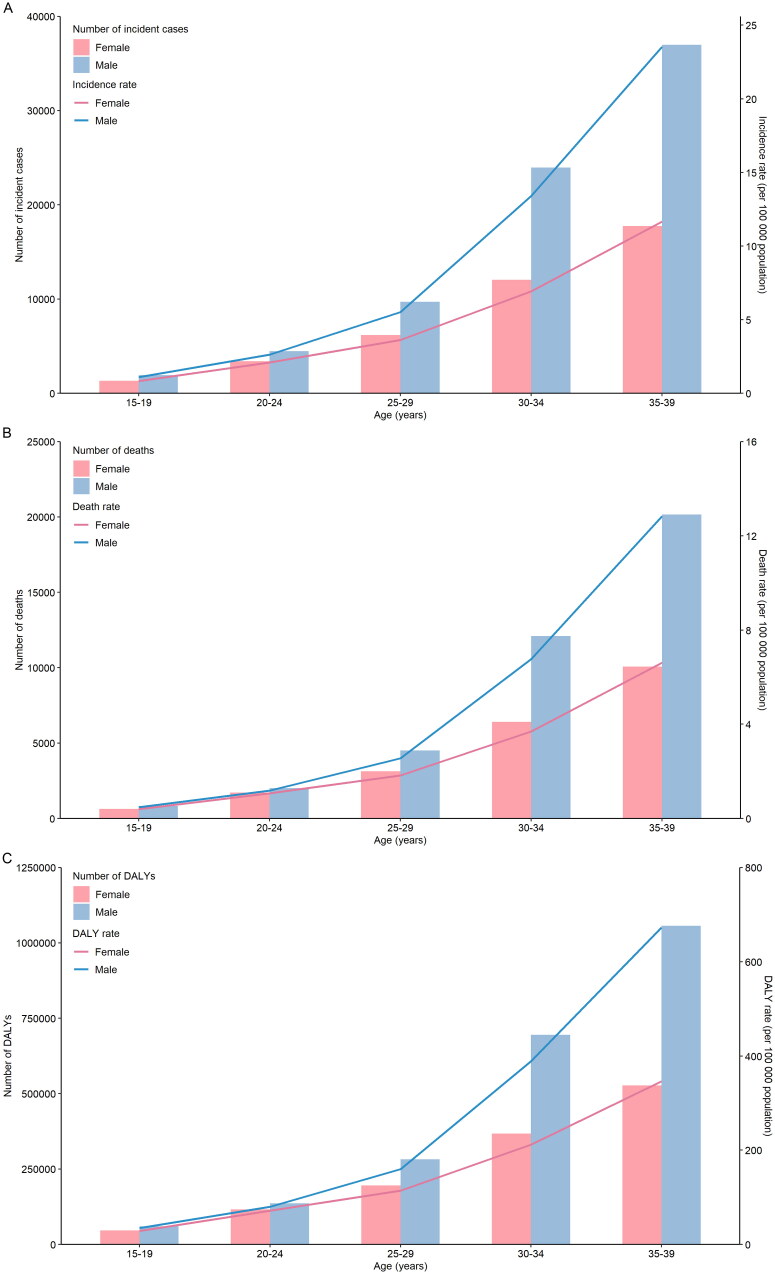
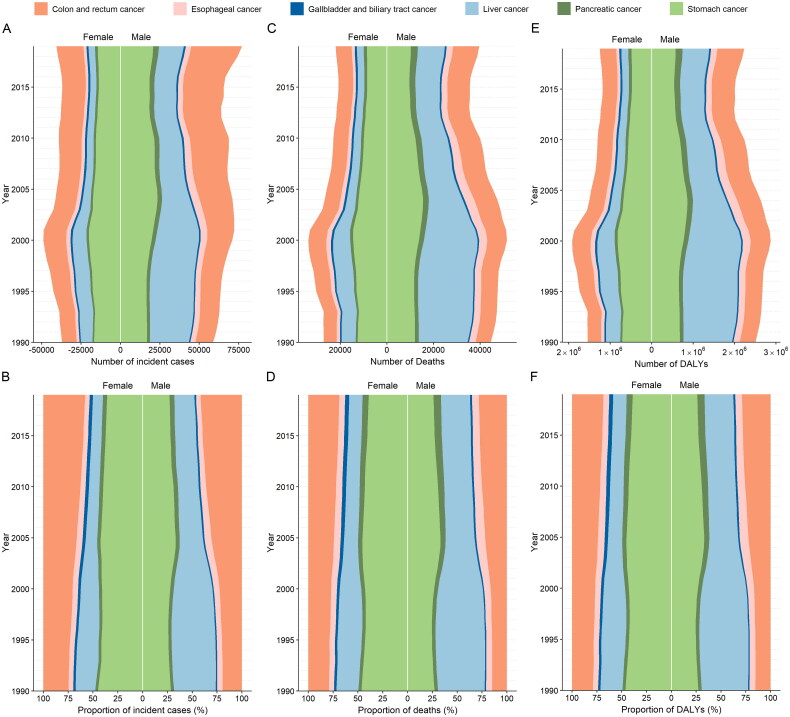
Incidence, mortality and DALYs progressively increased with age (Figures 4A–4C). In the period spanning from 1990 to 2019, the number of AYAs diagnosed with colorectal cancer, oesophageal cancer, liver cancer and pancreatic cancer were consistently higher in males than females (Figures 5A–5C). Conversely, the number attributed to gallbladder and biliary tract cancers was higher in females. There was a significant increase in the proportions of incident cases, deaths and DALYs associated with colorectal cancer, whereas the proportions decreased notably for liver cancer (Figures 5D–5F).
Figure 4.
Age patterns by sex of the absolute number and age-specific rates of incidence (A), death (B), and DALY (C) due to GI cancers in adolescents and young adults in the Asia-Pacific region in 2019.
DALY = disability-adjusted life-year; GI cancers = gastrointestinal cancers.
Figure 5.
Total trends in absolute and proportional burden of incident cases, deaths, and DALYs by GI cancers type and sex among adolescents and young adults in the Asia-Pacific region from 1990 to 2019. (A) Trends in the number of incident cases of GI cancers by types. (B) Trends in composition of total incident cases of GI cancers. (C) Trends in the number of deaths of GI cancers by types. (D) Trends in composition of total deaths of GI cancers. (E) Trends in the number of DALYs of GI cancers by types. (F) Trends in composition of total DALYs of GI cancers.
DALY = disability-adjusted life-year; GI cancers = gastrointestinal cancers.
Burden of oesophageal cancer
The incidence of oesophageal cancer increased by 7.28% from 5,074 in 1990 to 5,444 in 2019 (Table S4). However, the number of deaths and DALYs decreased by −2.91% and −2.83% 1990 to 2019. The age-standardized rates of incidence, death and DALY decreased during this period (EAPC = −1.28, −1.84 and −1.83, respectively) (Table S5).
In 2019, China had the largest number of incident cases, deaths and DALYs (Figures S7–S9). From 1990 to 2019, 60% of countries or territories in the Asia-Pacific region experienced a decrease in age-standardized rates of incidence, death and DALY, with Maldives had the largest decrease in incidence rate (EAPC = −4.42) and the Republic of Korea had the largest decrease in death rate (EAPC = −6.14) and DALY rate (EAPC = −5.85) (Figures S10–S12).
Burden of stomach cancer
In 2019, there were 35,297 incident cases of stomach cancer in AYAs in the Asia-Pacific region, an increase of 5.06% since 1990. Moreover, the number of deaths and DALYs number decreased by −23.75% and −23.70% (Table S6). Between 1990 and 2019, the age-standardized rates of incidence, death and DALY of stomach cancer decreased (EAPC = −1.28, −2.49 and −2.47, respectively) (Table S7).
At national and territorial levels, China had the highest number of incident cases (20,855), deaths (8,462) and DALYs (475,977). In 2019, the highest age-standardized incidence, death and DALY rates of stomach cancer were observed in the Solomon Islands (Figures S13–S15). Between 1990 and 2019, age-standardized rates of incidence, death and DALY were found to decrease in 80% of countries or territories, with the largest decrease in the age-standardized incidence rate in the Maldives (EAPC = −4.93) and the largest decrease in age-standardized death rate and DALY rate in the Republic of Korea (EAPC = −6.30) (Figures S16–S18).
Burden of colorectal cancer
In 2019, colorectal cancer remained the most commonly diagnosed GI cancer in AYAs in the Asia-Pacific region, representing 49,182 incident cases, an increase of 137.28% from 1990 (Table S8). The deaths and DALYs due to colorectal cancer also increased by 48.55% and 47.92%, respectively, from 1990 to 2019. Although the age-standardized rates of death and DALY for colorectal cancer decreased during the study period (EAPC = −0.18 and −0.17), the age-standardized rate of incidence increased (EAPC = 1.62) (Table S9).
Geographically, China had the largest number of incident cases, deaths and DALYs in the AYAs in 2019. The highest age-standardized incidence rate was observed in Taiwan (Province of China), and the highest age-standardized death rate and DALY rate were observed in Nauru (Figures S19–S21). Between 1990 and 2019, approximately 50% of the countries and territories demonstrated increased mortality and DALY rates (Figures S23–S24). Moreover, more than 80% of countries and territories have shown an increased incidence rate over the past 30 years, and the highest age-standardized incidence rate was noted in Vietnam (EAPC = 3.60) (Figure S22).
Burden of liver cancer
There were 19,844 incident cases, 14,494 deaths and 812,524 DALYs of liver cancer in AYAs in the Asia-Pacific region in 2019, which decreased respectively by −38.00%, −46.26% and −46.26% from 1990, respectively (Table S10). Moreover, the age-standardized rates of incidence, death and DALY also decreased from 1990 to 2019 (EAPC = −4.35, −4.87 and −4.84, respectively) (Table S11).
China had the highest number of incident cases, deaths and DALYs in the AYAs in 2019. Mongolia had the highest age-standardized incidence, death and DALY rates of liver cancer in 2019 (Figures S25–S27). From 1990 to 2019, age-standardized rates of incidence, death and DALY of liver cancer decreased in approximately half of the countries or territories in the Asia-Pacific region in AYAs, with the greatest decrease in China (EAPC = −4.49, −5.12 and −5.11, respectively) (Figures S28–S30).
Burden of pancreatic cancer
In the Asia-Pacific region, pancreatic cancer accounted for 5,366 new cases, 4,414 deaths and 244,207 DALYs in AYAs in 2019, which increased by 89.03%, 86.96% and 84.57%, respectively, from 1990 (Table S12). The age-standardized rates of these three measures also increased after 1990 (Table S13).
In 2019, China and Palau had the largest number of cases and age-standardized rates of incidence, death and DALY for pancreatic cancer (Figures S31–S33). Between 1990 and 2019, most Asia-Pacific regions demonstrated increased age-standardized rates of incidence, death and DALY (Figures S34–S36). Decreased age-standardized incidence rates were noted in the Republic of Korea, Singapore and Japan (EAPC = −2.05, −1.24 and −0.64, respectively), and decreased age-standardized death and DALY rates were observed in the Republic of Korea, Singapore, Thailand and Japan.
Burden of gallbladder and biliary tract cancer
In AYAs in the Asia-Pacific region in 2019, the number of incident cases, deaths and DALYs attributable to gallbladder and biliary tract cancer increased by 48.95%, 34.92% and 34.19%, respectively, from 1990 to 2019 (Table S14). However, the age-standardized rates of death and DALY decreased over the past 30 years, and the age-standardized rate of incidence remained stable (Table S15).
In 2019, the highest number of incident cases, deaths and DALYs of AYAs for gallbladder and biliary tract cancer were found in India, the highest age-standardized incidence rate was noted in Thailand, and the highest age-standardized death rate and DALY rate were found in Pakistan (Figures S37–S39). From 1990 to 2019, more than 70% of countries or territories in the Asia-Pacific region had a decreased age-standardized death rate and DALY rate (Figures S41–S42). While 46% of countries or territories showed decreased age-standardized incidence rates and 22% of countries or territories showed increased age-standardized incidence rates, Sri Lanka had the greatest decrease, and Viet Nam had the largest increase (Figure S40). The highest increase in the age-standardized death and DALY rates during this period was observed in India.
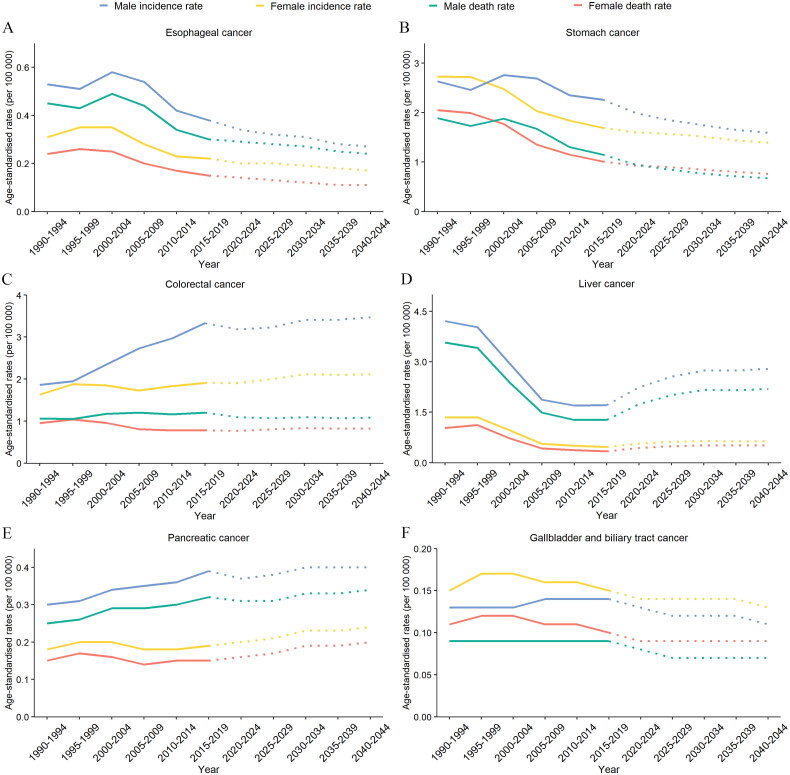
Predictions of incidence and mortality of GI cancers from 2020 to 2044
We projected the incidence and mortality rates of gastrointestinal cancers among the AYAs in the Asia-Pacific region from 2020 to 2044. When adjusted for age, the rates of GI cancers were expected to exhibit a stable trend in the overall population (Figure S43). However, when specifically considering oesophageal and stomach cancers, both the incidence and mortality rates are anticipated to decline, with a more significant decline observed in males (Figures 6A–6B). In contrast, the incidence rates of colorectal cancer are projected to increase slightly, while the mortality rates are expected to remain relatively stable (Figure 6C). In contrast, liver cancer is predicted to experience a noticeable increase in both incidence and mortality rates among males, with a slight increase projected for females (Figure 6D). For pancreatic cancer, the incidence and mortality rates are projected to increase among females but stabilize among males (Figure 6E). Lastly, gallbladder and biliary tract cancers are expected to show a decrease in mortality rates over the next 25 years, while the incidence rates are anticipated to decline initially but stabilize after 2025–2029 in both sexes (Figure 6F).
Figure 6.
Observed trends from 1990 to 2019 (solid line) and predictions from 2020 to 2044 (dashed line) in age-standardized rates of incidence and deaths due to GI cancers in adolescents and young adults in the Asia-Pacific region. (A) Oesophageal cancer. (B) Stomach cancer. (C) Colorectal cancer. (D) Liver cancer. (E) Pancreatic cancer. (F) Gallbladder and biliary tract cancer.
GI cancers = gastrointestinal cancers.
Discussion
This study presents the first comprehensive and most current assessment of GI cancer burden among AYAs in the Asia-Pacific region over the last three decades as well as predicted trends through the year 2044. In 2019, the Asia-Pacific region accounted for a significant proportion of incident cases, deaths and DALYs attributable to GI cancers among the AYAs, amounting to 68.5%, 67.6% and 72.4% of global GI cancers, respectively. The age-standardized incidence rate in the same year was found to be 6.77 per 100 000 population, indicating a nearly twofold higher incidence compared to the mortality rate, which suggests improved prognosis relative to the 1990 data. Collectively, this study offers valuable insights into the impact of such malignancies and highlights the critical need for targeted interventions designed to improve the outcomes of AYAs in the region.
Alvarez et al. reported that GI cancer contributes to 21.4% of the DALYs of cancer in AYAs globally [9]. Our investigation identified significant disparities in disease burden among the different sociodemographic index (SDI) levels. The low SDI regions showed the largest increase, which might partly result from an improved cancer registration system. Notably, we estimated that a considerable proportion of new cases (71.5%), deaths (63.9%) and DALYs (63.7%) occurred in regions classified as having middle SDI (including 60.9%, 51.1% and 50.9% in China, respectively). This result is consistent with the findings of Wen et al. [10]. Our study also showed that the incidence-to-mortality ratio shifted towards unity as one moved from high to low SDI regions, reflecting the poor prognosis in low SDI regions.
The DALYs of oesophageal cancer and gastric cancer were decreasing in most Asia-Pacific regions, which are consistent with the established epidemiological data [26,27]. They were the highest in the middle SDI regions, which also experienced the most substantial decrease in DALYs. One plausible explanation is early endoscopic screening, better food reservation, better living conditions and an enhanced reporting system [26]. For oesophageal cancer, increasing rates were observed in high SDI regions, which were historically classified as low-risk regions in our study and published data [28]. This pattern is likely due to the rising obesity rate with declining chronic Helicobacter pylori (H. pylori) infection, which has been inversely related to reflux esophagitis [24]. Notably, the mortality rates for oesophageal cancer closely followed the incidence rates, indicating a poor prognosis. Furthermore, the mortality-to-incidence ratio for gastric cancer increased as the SDI level decreased, implying a more severe prognosis in countries with a lower SDI.
Colorectal cancer is one of the major contributors to the AYA GI cancer burden, accounting for 29.8% of DALYs and 41.8% of DALYs in 2019. The age-standardized incidence rates increased in all five SDI regions, which are compatible with published epidemiological data from Western countries, showing shifts to younger generations [7,29]. The greatest increase in age-standardized incidence rates was observed in the middle SDI regions, which are primarily attributed to shifts in dietary patterns towards changed dietary habits, decreased physical activity and sedentary behaviour [30]. Although death rates have stabilized or decreased in regions with high SDI, the incidence rates remain higher than the death rates. This phenomenon may be attributed to the implementation of large-scale population-based endoscopic screening and improved treatment strategy [31]. Nonetheless, the number of colorectal cancer cases among AYAs is expected to continue rising in the years ahead, highlighting the urgent need for effective cancer control strategies.
Among gastrointestinal cancers, liver cancer showed the most significant decreasing trend. In China, the incidence rate has decreased by 50.6%. This can be largely attributed to HBV vaccination and the control of aflatoxin infection [32–34]. In contrast, it was forecast that there would be an increase in the incidence trends within the next two decades, which can be partly explained by increasing obesity, alcohol abuse and metabolic disorders [35,36]. Owing to the unfavourable prognosis of liver cancer, the pattern of death rates closely followed the incidence rates. Early detection, vaccination and lifestyle changes are potential strategies [37].
An increasing trend of pancreatic cancer in the AYAs was observed in all four regions, except for the high SDI region. Li et al. showed a negative correlation between SDI and pancreatic cancer in patients with AYAs [38]. The decrease in mortality in regions with high SDI might be the result of strict tobacco control [39]. However, upward trends in pancreatic cancer incidence can be attributed to a high body mass index (BMI) and high fasting plasma glucose levels [40].
This study has several limitations. Specifically, incomplete cancer registry systems in low SDI settings may lead to an underestimation of the disease burden in these regions, warranting caution when interpreting the results. Nevertheless, our findings provide valuable insights into regions with limited data and contribute to the overall evaluation of the global burden of GI cancers in AYAs. Furthermore, we acknowledge that the calculation of year lived with disabilities (YLDs) and DALYs may be underestimated due to the current methodology accounting for only the first 10 years after cancer diagnosis. Finally, the potential impact of the COVID-19 pandemic on the burden of GI cancers in AYAs was not included in our analysis but should be considered in future studies when such data become available.
Given the burden of GI cancer among AYAs in the Asia-Pacific region predominantly concentrated in middle SDI countries, integration of GI cancer control policies could be prioritized among AYAs in these regions. Emphasizing primary prevention as the primary strategy to alleviate this burden, it is important to identify the specific risk factors contributing to the elevated burden in middle SDI countries. This is particularly crucial for colorectal and liver cancers, the major contributors to GI cancers, with their burden anticipated to increase in the near future; hence, investigating the driving factors behind this increasing trend is necessary in future research. Furthermore, noteworthy variations in mortality-to-incidence rates across different countries within the same SDI regions underscore potential disparities in the quality of medical care, suggesting further exploration in future research. Additionally, the difference in survival rates between AYAs and other age groups suggests unique tumour biology in AYAs. Future studies could perform tumour-specific analyses utilizing histological data from the Surveillance, Epidemiology, and End Results (SEER) database.
In conclusion, this study identified a substantial burden of AYA GI cancer in the Asia-Pacific region. This burden was primarily concentrated in the middle SDI regions, with a rapid upward trend noted in the low SDI settings. Furthermore, future trends for the upcoming 25 years have been projected, revealing noteworthy variations in the trends of individual GI cancers. These findings underscore the urgent need to focus on addressing the burden of GI cancers among this historically neglected population, and could be helpful for researchers, policymakers and global health institutions to justify resource allocation in the future.
Supplementary Material
Acknowledgements
We would like to thank all the members of the Institute for Health Metrics and Evaluation (IHME) and the Bill & Melinda Gates Foundation, which supported the related GBD 2019 studies.
Glossary
Abbreviations
- GI
Cancers, gastrointestinal cancers
- AYAs
Adolescents and young adults
- GBD
Global Burden of Disease, Injuries, and Risk Factors Study
- ASR
Age-standardized rate
- CI
Confidence interval
- DALY
Disability-adjusted life-year
- EAPC
Estimated annual percentage change
- SDI
Sociodemographic index
- UI
Uncertainty interval
- YLD
Years lived with disability.
Funding Statement
This work was supported by the National Natural Science Foundation of China (Grant No. 82000527) and Natural Science Foundation of Hunan Province (Grant Nos. 2022JJ30909 and 2023JJ40908). The funders had no role in the study design, data collection, data analysis, interpretation or writing of this manuscript.
Authors contributions
Rui Wang and Decai Zhang contributed to study concept and design. Shaojun Liu contributed to acquisition of data. Decai Zhang, Minxue Shen and Rui Wang contributed to data analysis and interpretation. Rui Wang, Zhaoqi Li, Zihao Li and Decai Zhang helped in drafting the manuscript. All authors contributed to critical revision of the manuscript. All authors had full access to all data in the study and had final responsibility for the decision to submit for publication.
Ethics approval and consent to participate
The institutional review board of the Third Xiangya Hospital of Central South University in Hunan Province, China, determined that the study did not require approval because it used publicly available data.
Disclosure statement
The authors declare no conflict of interest.
Data availability statement
The data that support the findings of this study are available from the corresponding author, R.W., upon reasonable request.
References
- 1.Smith AW, Seibel NL, Lewis DR, et al. . Next steps for adolescent and young adult oncology workshop: an update on progress and recommendations for the future. Cancer. 2016;122(7):988–999. doi: 10.1002/cncr.29870. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ferrari A, Stark D, Peccatori FA, et al. . Adolescents and young adults (AYA) with cancer: a position paper from the AYA Working Group of the European Society for Medical Oncology (ESMO) and the European Society for Paediatric Oncology (SIOPE). ESMO Open. 2021;6(2):100096. doi: 10.1016/j.esmoop.2021.100096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Jim HSL, Jennewein SL, Quinn GP, et al. . Cognition in adolescent and young adults diagnosed with cancer: an understudied problem. J Clin Oncol. 2018;36(27):2752–2754. doi: 10.1200/JCO.2018.78.0627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bleyer A, Barr R, Hayes-Lattin B, et al. . The distinctive biology of cancer in adolescents and young adults. Nat Rev Cancer. 2008;8(4):288–298. doi: 10.1038/nrc2349. [DOI] [PubMed] [Google Scholar]
- 5.Arnold M, Abnet CC, Neale RE, et al. . Global burden of 5 major types of gastrointestinal cancer. Gastroenterology. 2020;159(1):335–349 e15. doi: 10.1053/j.gastro.2020.02.068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lu L, Mullins CS, Schafmayer C, et al. . A global assessment of recent trends in gastrointestinal cancer and lifestyle-associated risk factors. Cancer Commun (Lond). 2021;41(11):1137–1151. doi: 10.1002/cac2.12220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Vuik FE, Nieuwenburg SA, Bardou M, et al. . Increasing incidence of colorectal cancer in young adults in Europe over the last 25 years. Gut. 2019;68(10):1820–1826. doi: 10.1136/gutjnl-2018-317592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Sung H, Siegel RL, Rosenberg PS, et al. . Emerging cancer trends among young adults in the USA: analysis of a population-based cancer registry. Lancet Public Health. 2019;4(3):e137–e147. doi: 10.1016/S2468-2667(18)30267-6. [DOI] [PubMed] [Google Scholar]
- 9.Alvarez EM, Force LM, Xu R, et al. . The global burden of adolescent and young adult cancer in 2019: a systematic analysis for the Global Burden of Disease Study 2019. The Lancet Oncology. 2022;23(1):27–52. doi: 10.1016/S1470-2045(21)00581-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wen YF, Chen MX, Yin G, et al. . The global, regional, and national burden of cancer among adolescents and young adults in 204 countries and territories, 1990-2019: a population-based study. J Hematol Oncol. 2021;14(1):89. doi: 10.1186/s13045-021-01093-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.You L, Lv Z, Li C, et al. . Worldwide cancer statistics of adolescents and young adults in 2019: a systematic analysis of the Global Burden of Disease Study 2019. ESMO Open. 2021;6(5):100255. doi: 10.1016/j.esmoop.2021.100255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Wei WQ, Chen ZF, He YT, et al. . Long-term follow-up of a community assignment, one-time endoscopic screening study of esophageal cancer in China. J Clin Oncol. 2015;33(17):1951–1957. doi: 10.1200/JCO.2014.58.0423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lauby-Secretan B, Vilahur N, Bianchini F, et al. . The IARC perspective on colorectal cancer screening. N Engl J Med. 2018;378(18):1734–1740. doi: 10.1056/NEJMsr1714643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Song M, Kang D, Yang JJ, et al. . Age and sex interactions in gastric cancer incidence and mortality trends in Korea. Gastric Cancer. 2015;18(3):580–589. doi: 10.1007/s10120-014-0411-x. [DOI] [PubMed] [Google Scholar]
- 15.Wu CY, Lin JT.. The changing epidemiology of Asian digestive cancers: from etiologies and incidences to preventive strategies. Best Pract Res Clin Gastroenterol. 2015;29(6):843–853. doi: 10.1016/j.bpg.2015.09.016. [DOI] [PubMed] [Google Scholar]
- 16.Vos T, Lim SS, Abbafati C, et al. . Global burden of 369 diseases and injuries in 204 countries and territories, 1990-2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet. 2020;396(10258):1204–1222. doi: 10.1016/S0140-6736(20)30925-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lozano R, Fullman N, Mumford JE, et al. . Measuring universal health coverage based on an index of effective coverage of health services in 204 countries and territories, 1990-2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet. 2020;396(10258):1250–1284. doi: 10.1016/S0140-6736(20)30750-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Murray CJL, Aravkin AY, Zheng P, et al. . Global burden of 87 risk factors in 204 countries and territories, 1990-2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet. 2020;396(10258):1223–1249. doi: 10.1016/S0140-6736(20)30752-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Wang H, Abbas KM, Abbasifard M, et al. . Global age-sex-specific fertility, mortality, healthy life expectancy (HALE), and population estimates in 204 countries and territories, 1950-2019: a comprehensive demographic analysis for the Global Burden of Disease Study 2019. Lancet. 2020;396(10258):1160–1203. doi: 10.1016/S0140-6736(20)30977-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Boyle P, Parkin DM.. Cancer registration: principles and methods. Statistical methods for registries. IARC Sci Publ. 1991;(95):126–158. [PubMed] [Google Scholar]
- 21.Zi H, He SH, Leng XY, et al. . Global, regional, and national burden of kidney, bladder, and prostate cancers and their attributable risk factors, 1990-2019. Mil Med Res. 2021;8(1):60. doi: 10.1186/s40779-021-00354-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Deng Y, Zhao P, Zhou L, et al. . Epidemiological trends of tracheal, bronchus, and lung cancer at the global, regional, and national levels: a population-based study. J Hematol Oncol. 2020;13(1):98. doi: 10.1186/s13045-020-00915-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Valery PC, Laversanne M, Clark PJ, et al. . Projections of primary liver cancer to 2030 in 30 countries worldwide. Hepatology. 2018;67(2):600–611. doi: 10.1002/hep.29498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Arnold M, Laversanne M, Brown LM, et al. . Predicting the future burden of esophageal cancer by histological subtype: International Trends in Incidence up to 2030. Am J Gastroenterol. 2017;112(8):1247–1255. doi: 10.1038/ajg.2017.155. [DOI] [PubMed] [Google Scholar]
- 25.Møller B, Fekjaer H, Hakulinen T, et al. . Prediction of cancer incidence in the Nordic countries: empirical comparison of different approaches. Stat Med. 2003;22(17):2751–2766. doi: 10.1002/sim.1481. [DOI] [PubMed] [Google Scholar]
- 26.Zhang Z, Wang J, Song N, et al. . The global, regional, and national burden of stomach cancer among adolescents and young adults in 204 countries and territories, 1990–2019: a population-based study. Front Public Health. 2023;11:1079248. doi: 10.3389/fpubh.2023.1079248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Uhlenhopp DJ, Then EO, Sunkara T, et al. . Epidemiology of esophageal cancer: update in global trends, etiology and risk factors. Clin J Gastroenterol. 2020;13(6):1010–1021. doi: 10.1007/s12328-020-01237-x. [DOI] [PubMed] [Google Scholar]
- 28.Sheikh M, Roshandel G, McCormack V, et al. . Current Status and Future Prospects for Esophageal Cancer. Cancers (Basel). 2023;15(3):765. doi: 10.3390/cancers15030765. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Stoffel EM, Murphy CC.. Epidemiology and mechanisms of the increasing incidence of colon and rectal cancers in young adults. Gastroenterology. 2020;158(2):341–353. doi: 10.1053/j.gastro.2019.07.055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Nguyen LH, Liu PH, Zheng X, et al. . Sedentary behaviors, TV viewing time, and risk of young-onset colorectal cancer. JNCI Cancer Spectr. 2018;2(4):pky073. doi: 10.1093/jncics/pky073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Schreuders EH, Ruco A, Rabeneck L, et al. . Colorectal cancer screening: a global overview of existing programmes. Gut. 2015;64(10):1637–1649. doi: 10.1136/gutjnl-2014-309086. [DOI] [PubMed] [Google Scholar]
- 32.Luo Z, Li L, Ruan B.. Impact of the implementation of a vaccination strategy on hepatitis B virus infections in China over a 20-year period. Int J Infect Dis. 2012;16(2):e82-8–e88. doi: 10.1016/j.ijid.2011.10.009. [DOI] [PubMed] [Google Scholar]
- 33.Sun Z, Chen T, Thorgeirsson SS, et al. . Dramatic reduction of liver cancer incidence in young adults: 28 year follow-up of etiological interventions in an endemic area of China. Carcinogenesis. 2013;34(8):1800–1805. doi: 10.1093/carcin/bgt007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Chen W, Zheng R, Baade PD, et al. . Cancer statistics in China, 2015. CA Cancer J Clin. 2016;66(2):115–132. doi: 10.3322/caac.21338. [DOI] [PubMed] [Google Scholar]
- 35.Zhang CH, Cheng Y, Zhang S, et al. . Changing epidemiology of hepatocellular carcinoma in Asia. Liver Int. 2022;42(9):2029–2041. doi: 10.1111/liv.15251. [DOI] [PubMed] [Google Scholar]
- 36.Liu Y, Liu L.. Changes in the epidemiology of hepatocellular carcinoma in Asia. Cancers (Basel). 2022;14(18):4473. doi: 10.3390/cancers14184473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.McGlynn KA, Petrick JL, El-Serag HB.. Epidemiology of hepatocellular carcinoma. Hepatology. 2021;73 Suppl 1(Suppl 1):4–13. doi: 10.1002/hep.31288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Li J. Digestive cancer incidence and mortality among young adults worldwide in 2020: a population-based study. World J Gastrointest Oncol. 2022;14(1):278–294. doi: 10.4251/wjgo.v14.i1.278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Lucas AL, Malvezzi M, Carioli G, et al. . Global trends in pancreatic cancer mortality from 1980 through 2013 and predictions for 2017. Clin Gastroenterol Hepatol. 2016;14(10):1452–1462 e4. doi: 10.1016/j.cgh.2016.05.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Yu JR, Yang XR, He W, et al. Burden of pancreatic cancer along with attributable risk factors in Europe between 1990 and 2019 , and projections until 2039. Int J Cancer. 2021;149(5):993–1001. doi: 10.1002/ijc.33617. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data that support the findings of this study are available from the corresponding author, R.W., upon reasonable request.