Abstract
Study Design
Retrospective Cohort Study.
Objectives
Length of Stay (LOS) and resource utilization are of primary importance for hospital administration. This study aimed to understand the incremental effect of having a specific complication on LOS among ASD patients.
Methods
A retrospective examination of prospective multicenter data utilized patients without a complication prior to discharge to develop a patient-adjusted and surgery-adjusted predictive model of LOS among ASD patients. The model was later applied to patients with at least 1 complication prior to discharge to investigate incremental effect of each identified complication on LOS vs the expected LOS.
Results
571/1494 (38.2%) patients experienced at least 1 complication before discharge with a median LOS of 7 [IQR 5 to 9]. Univariate analysis demonstrated that LOS was significantly affected by patients’ demographics (age, CCI, sex, disability, deformity) and surgical strategy (invasiveness, fusion length, posterior MIS fusion, direct decompression, osteotomy severity, IBF use, EBL, ASA, ICU stay, day between stages, Date of Sx). Using patients with at least 1 complication prior discharge and compared to the patient-and-surgery adjusted prediction, having a minor complication increased the expected LOS by 0.9 day(s), a major complication by 3.9 days, and a major complication with reoperation by 6.3 days.
Conclusion
Complications following surgery for ASD correction have different, but predictable impact on LOS. Some complications requiring minimal intervention are associated with significant and substantial increases in LOS, while complications with significant impact on patient quality of life may have no influence on LOS.
Keywords: adult spinal deformity, length of stay, adverse event, in-hospital outcomes, complications
Introduction
Adult spinal deformity (ASD) is a burdensome condition for patients, but corrective surgery has been shown to enhance quality of life significantly. 1 ASD treatment requires significant resource utilization from the care centers that manage this disease. For those undergoing corrective surgery, the total hospital costs per patient were shown to be upwards of $120,000, with readmissions alone costing an additional $70,000. 2 Complications are a common sequala after treating ASD,3-5 however, in-hospital complications that directly influence length of stay and cost metrics are not commonly specified in the literature and are often included in overall complication incidence rates.
Understanding the drivers of extended lengths of stay for surgically treated ASD patients is paramount for reducing the strain on both patients and the hospitals that treat them. The average hospital length of stay (LOS) in ASD is 8 days as demonstrated by both retrospective and prospective studies6-9 with comorbidities, pain, mobility issues, and higher surgical invasiveness leading to longer stays. 10 Surgical complications such as infection contribute to high costs and medical complications alone have been reported in over 25% of patients treated for ASD. 5 Classification systems for complications are inconsistent, and predictive models for ASD care are only valid for the parameters they are given. Previous studies have used models to classify complication types as surgical (with subcategories) or medical 10 and have applied predictive algorithms to estimate LOS using several known risk factors.11-14 Overall, the literature has not provided a specific time-dependent prediction model for individual complications. Rather, it has demonstrated that certain adverse events are associated with an overall increased length of stay. 15 Studies that have incorporated pre-operative metrics, data from radiographic imaging, and established scoring systems demonstrated that algorithms can predict length of stay in adult spinal deformity surgery with moderate accuracy.6,14 However, there is a need to not only determine the source of the complication (surgical vs medical), but to incorporate and delineate more drivers of LOS that extend beyond demographic characteristics and how exactly these complications alter expected stays.
The study aims to use multicenter data to predict the length of stay for patients being surgically treated for ASD and to apply that model to the percentage of patients that experience complications.
Methods
Patient Population
This study utilized a retrospective review of prospective multicenter data from 23 sites across North America (ClinicalTrials.gov ID NCT00738439). Institutional review board approval was granted at each participating site and the patients were prospectively consented for involvement in the study. The database was screened for the inclusion criteria of patients over the age of 18 that underwent surgery for Adult Spinal Deformity defined as at least one of the following prior to surgery: a Cobb angle of >20°, a sagittal vertical axis of >5 cm, a pelvic tilt of >20°, or a thoracic kyphosis of >60°.
Data Collection
Demographic data collected from the database included patient age, sex, body mass index (BMI), and Charlson Comorbidity Index (CCI) values. Pre-operative data included radiographic information organized according to the SRS-Schwab Classification, health-related quality of life (HRQOL) statistics based on the Oswestry Disability Index (ODI), and the Scoliosis Research Society’s SRS-22r Patient Questionnaire. Surgical information specific to the procedure performed was collected, noting the presence of direct decompression, osteotomy, inter-body fusion, percutaneous posterior fusion, and/or number of levels treated. Additional surgical information included ASA grades, any ICU stay, extended ICU stay of over 48 hours, and total in-hospital length of stay (LOS). Any in-hospital complications were gathered and stratified by severity (minor and major) based on perceived impact on patient, with an identification of the incidence of reoperation for each complication. 16
Statistical Analysis
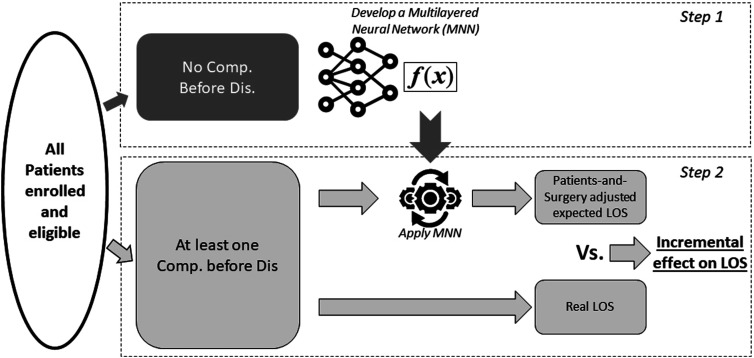
A descriptive cohort analysis was conducted based on the pre-operative and surgical data described above. A univariate analysis was conducted between LOS and the pre-operative and surgical data, utilizing correlations, Student T-tests, ANOVA, Mann-Whitney U Test, or the Kruskal-Walis Test when appropriate. Analysis was divided into 2 steps (Figure 1). First, all significant predictors of LOS from the univariate analysis were included in a multilayered Neural Network Model that was developed using 70% of patients without complications prior to discharge and tested for external accuracy using the remaining 30% to generate a patient-and-surgery adjusted expected LOS. Very briefly, a multilayered neural network model is a type of artificial intelligence system. It consists of layers of interconnected nodes (neurons), where each layer processes input data and passes it to the next layer, gradually refining the data to make accurate predictions or decisions. This structure allows the model to learn complex patterns and relationships in the data. Second, using the patients in the cohort that experienced at least 1 complication before discharge, the observed LOS for each complication the difference between the expected patient-and-surgery adjusted LOS vs the observed LOS was reported as an incremental difference. Within each category of complication type, the values were sorted based on the magnitude of the incremental difference. Only complications with at least 4 occurrences were reported.
Figure 1.
Graphical representation of the two phases of this analysis. Step 1: create a Patient-and-Surgery adjusted expected length of stay prediction using patient without a complication before discharge. Step 2: apply this prediction to patient experiencing at least one complication to evaluate the incremental effect of complication on LOS.
Results
Cohort Description
A total of 1494 patients were included in this analysis, with a median age of 64, a mean BMI of 28.1 ± 6.0, and a median CCI of 2.763 patients (51.4%) reported an history of previous spine surgery. The assessment of preoperative HRQOL demonstrated some severe disability (ODI: 45 ± 17), and preoperative measurements indicated severe sagittal and/or coronal deformity defined by the SRS-Schwab classification system as the most common indication for surgery (Table 1).
Table 1.
Pre-operative Information (Demographic, HRQOL and Radiographic) for the Entire Cohort. Value Reported as Either Mean ± StD, Median (25th to 75th Percentile) or N (Percentage) as Appropriate.
| Demographic | |||
| Age | 64 (55 to 70) | Sex (F) | 1079 (72.2%) |
| BMI | 28.1 ± 6.0 | Prior spine Sx | 763 (51.1%) |
| CCI | 2 (0 to 3) | Frailty index | 0.34 (0.23 to 0.46) |
| HRQOL | |||
| ODI | 45 ± 17 | SRS Acti. | 2.81 ± 0.86 |
| ODI>20 | 1342 (89.8%) | SRS pain | 2.34 ± 0.83 |
| ODI>40 | 901 (60.3%) | SRS Appea. | 2.41 ± 0.76 |
| MCS | 45 ± 14 | SRS Mental | 3.42 ± 0.90 |
| PCS | 31 ± 9 | SRS total | 2.75 ± 0.64 |
| SRS-Schwab classification | |||
| Type | N: 654 (43.8%) L: 449 (30.1%) D: 331 (22.2%) | ||
| SVA | 0: 566 (37.9%) +: 434 (29.0%) ++: 477 (31.9%) | ||
| PI-LL | 0: 521 (34.9%) +: 318 (21.3%) ++: 651 (43.6%) | ||
| PT | 0: 489 (32.7%) +:570 (38.2%) ++:431 (28.8%) | ||
In terms of surgical data collected, 728 patients (48.7%) had ASA classified as Grade II and 637 patients (42.6%) as Grade III. The majority of patients (98%) underwent some form of posterior fusion surgery, 70% received some osteotomy, 67% had some interbody fusion (26% ALIF, 30% PLIF or TLIF, 19% some LLIF), and 56% had a direct decompression. A smaller portion of patients had some staged procedure (21%) with the median number of days between stages being 2 (IQR 1 to 4), 13% underwent posterior fusion using specifically minimally invasive procedures, and 18% were treated with a 3-column osteotomy. There was a median of 9 spinal levels treated (IQR 8 to 13) for the cohort, with 12.7% having 1 to 4 levels, 60.1% having 5 to 12 levels, and 27.0% having 13 or more levels treated. For all procedures, the median time in the operating room was 405 minutes (IQR 307 to 527), and the median estimated blood loss was 1200 cc (600 to 2100).
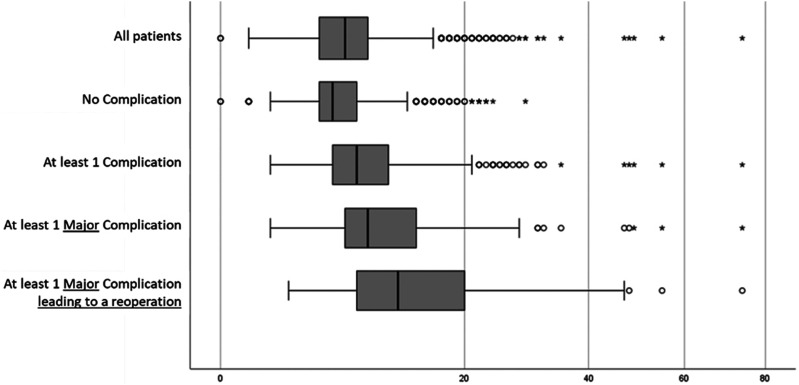
The in-hospital course for patients was represented by ICU stay information and LOS values for no complications, any complication, and any complication requiring a return to the operating room. 956 (64%) patients had some ICU stay, but only 167 of those individuals stayed over 48 hours. The median length of stay for the cohort as a whole was 7 days (IQR 5 to 9), with vast variability from 0 to 74 days. 571 (38.2%) patients experienced at least 1 complication before discharge, with a median LOS of 8 days (IQR 6 to 11), while only 69 (4.6%) patients needed a return to the operating room before discharge, with a median LOS of 12 days (IQR 7.5 to 20). 923 patients that did not have a complication prior to discharge had a median LOS of 6 days (IQR 5 to 8). A comparison of LOS between patients with and without complications yielded a significant association between the presence of at least 1 complication before discharge and an increase in LOS (P < .001) (Figure 2).
Figure 2.
Boxplot of the Length of stay (LOS) for all patients as well as stratified by presence of at least 1 complication before discharge, at least 1 major complication before discharge, and at least 1 major complication before discharge treated with a reoperation. X-axis is displayed using a root square scale for clarity.
Prediction of LOS Outside of Complications
The baseline predictive model for LOS was generated using the 923 patients without reported complications before discharge. The univariate analysis demonstrated that LOS increased with increasing age (P = .001), higher CCI scores (P < .001), and female sex (P = .001). There was no significant association between LOS and previous spine surgery (P = .238) or BMI (P = .896). In terms of HRQOL, LOS was significantly increased with all metrics for disability and pain, which was further stratified by ODI value, with patient presenting with an ODI score of less than 40 had a median LOS of 6 days (IQR 4 to 7) and patient with an ODI score above 40 had to a median LOS of 6 days (IQR 5 to 9) (P < .001). Applying the SRS-Schwab classification system to pre-operative risk factors showed an increased LOS as sagittal deformity severity increased (P < .001) and in the presence of either Lumbar or double major curve (all P < .001). The impact of surgical procedure type and staging on LOS in the uncomplicated sample population is presented in Table 2. LOS was increased in staged surgeries, among patients with higher ASA grades, increased length of fusion, use of direct decompression, more severe osteotomies, and in cases treated with any interbody fusion. Higher values for estimated blood loss (r = 0.363, P < .001), any ICU stay (median 5 vs 7 days, P < .001) or an extended ICU stay (median: 6 vs 7.5 days, P < .001) were all associated with increased LOS. Additionally, patients with more recent surgeries experienced a shorter LOS (r = −0.107, P = .001).
Table 2.
Comparison of Length of Stay (LOS) Between Type of Procedure Among Patient Without Complication Before Discharge.
| N | Mean | StD | 25th | 50th | 75th | P | ||
|---|---|---|---|---|---|---|---|---|
| Staged surgery? | Same day | 729 | 5.8 | 2.6 | 4 | 6 | 7 | P < 0.001* |
| Stage | 194 | 10.1 | 4.2 | 7 | 9 | 12 | ||
| ASA grade | I or II | 524 | 6.5 | 3.3 | 5 | 6 | 8 | P = 0.028* |
| III or IV | 376 | 7.0 | 3.6 | 5 | 6 | 9 | ||
| MIS posterior fusion? | No | 759 | 7.0 | 3.4 | 5 | 6 | 8 | P < 0.001* |
| Yes | 164 | 5.6 | 3.4 | 3 | 5 | 7 | ||
| Fusion length | 1 to 4 lvl | 160 | 4.4 | 2.4 | 3 | 4 | 5.75 | P < 0.001” |
| 5 to 12 lvl | 558 | 7.0 | 3.2 | 5 | 6 | 8 | ||
| 13 and more lvl | 201 | 8.1 | 3.8 | 6 | 7 | 9 | ||
| Direct decompression? | No | 420 | 6.3 | 3.3 | 4 | 6 | 7.75 | P < 0.001* |
| Yes | 499 | 7.1 | 3.6 | 5 | 6 | 8 | ||
| Osteotomy performed? | No | 324 | 6.0 | 3.2 | 4 | 6 | 7 | P < 0.001” |
| SPO | 480 | 7.0 | 3.5 | 5 | 6 | 8 | ||
| 3CO | 119 | 7.7 | 3.6 | 5 | 7 | 9 | ||
| IBF placed? | No | 312 | 6.3 | 2.7 | 5 | 6 | 7 | P = 0.010* |
| Yes | 607 | 7.0 | 3.7 | 5 | 6 | 9 | ||
| ALIF | 234 | 8.3 | 4.1 | 5 | 7.5 | 10 | - | |
| P/TLIF | 247 | 6.3 | 2.5 | 5 | 6 | 7 | - | |
| LLIF | 208 | 7.0 | 4.3 | 4 | 6 | 9 | - |
*Mann-Whitney U test, “Kruskal-Wallis test.
The multilayered neural network demonstrated an acceptable level of accuracy of prediction when tested on the remaining 30% of the sample. The relative error on testing the sample was 0.6 days, and an XLM model was generated for further deployment on external databases.
Incremental Effect of Complication on LOS
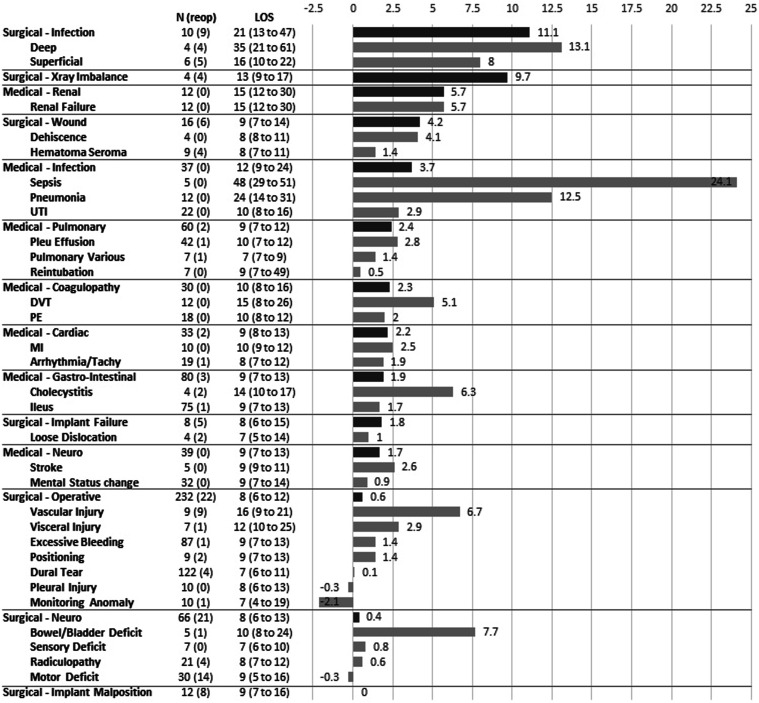
The incremental effect of complications on LOS was calculated as compared to the group of patients that did not have a reported complication prior to discharge. The median LOS for patient with at least 1 complication prior to discharge was 8 days (IQR 6 to 11), representing no increase in LOS (IQR -1 to 3 days) as compared to a patient-and-surgery adjusted predicted LOS. When considering complication severity, those with major complications needing a reoperation had a median LOS of 12 days (IQR 7.5 to 20) with an incremental increase of 4 days (IQR -1 to 11 days). Patients with a major complication that did not require a second operation had a median LOS of 9 days (IQR 7 to 14) with an incremental increase of 2 days (IQR 0 to 4 days). Surgical complications were associated with a LOS of 8 days (IQR 6 to 12) and an incremental increase of 1 day (IQR -1 to 4). Medical complications had a median LOS of 9 days (IQR 7 to 13) with an incremental increase of 2 days (IQR 0 to 4). Median and interquartile values of LOS, as well as median incremental increases in LOS, are reported for each type and sub-type of complication in Figure 3. Of particular note, the median incremental increase in LOS varied from +11.1 days for surgical site infection, +9.7 days for x-ray imbalance, +3.7 days for medical infection, +1.7 days for medical neurologic complications, down to +0.6 days for operative complications, and +0 days for implant malposition.
Figure 3.
Incidence, rate of reoperation (reop), median length of stay (LOS) and interquartile range (25th and 75th quartile) reported by type and sub-type of complications. Bargraph represent the median Incremental effect of complication on LOS by classes of complications as calculated by a multilayered neural network model. For clarity, only complications with at least an incidence of 4 were reported in this table.
Discussion
This study investigated specific inpatient complications in ASD surgery as related to length of stay and evaluated the accuracy of a patient-and-surgery adjusted predictive model. More than 1 third (38.2%) of patients experienced at least 1 complication before discharge, and LOS was increased for those patients as compared to those without complications prior to discharge. Overall, sepsis was found to have the largest increase in LOS and the largest difference from the from the predicted non-complication LOS. The overall median LOS was 7 days, which was 1 day shorter than previously published literature.6-9 However, patients without complications had a LOS of 6 days, while those with 1 complication stayed for a median of 8 days. Patients needing reoperation stayed twice as long as their uncomplicated counterparts. Moreover, a minor complication added an extra 0.9 day(s), a major complication added 3.9 days, and a major complication with reoperation added 6.3 days. Identifying complications or risks for complications at the time of operation can be difficult, and delineating those complications as due to spine surgery or incidental medical problems provides insight into how hospitals can better manage these patients, specifically regarding costs and resource utilization associated with care.
LOS prediction without complication revealed an association between older age, female sex, higher CCI scores, greater disability, pain, and invasive procedures with longer stays. These results are similar to what is found in the literature. In a study by Elsamadicy et al, female sex was found to be an independent predictor of increased LOS and was associated with an increased incidence of UTI and hematoma, 17 both of which can contributed to longer stays. A study of ASD patients in Denmark revealed that 81% of cases with extended LOS were due to medical complications, and both older age and CCI score above 3 increased the chance of longer stays. 9 Among the cohort of patients in this investigation, there was an average of 9 spinal levels treated, with a median OR time of 405 minutes and a total blood loss of 1200cc. Previous work has shown that shorter OR times, defined as less than 359 minutes, are associated with fewer minor complications and similar patient outcomes to those with long OR times. In a paper by Arzeno et al, ASD patients undergoing staged anterior/posterior approaches had an overall longer LOS, but this was not different when a risk adjustment was made, 18 and another study found that more invasive procedures resulted in a higher likelihood of extended LOS. 19 This demonstrates that OR time or staged procedures alone can be expected to affect the LOS, even without complications, likely as a proxy for more invasive techniques or more complex deformity. This may serve as a concrete metric by which practices or hospital systems may evaluate efficiency against quality of care to both reduce resource utilization and maximize positive patient outcomes. With regards to the clinical practicality and utility of the multilayered neural network model as a tool for resource utilization, there is an opportunity for this model to incorporate a broader group encompassing more clinically relevant situations. For example, instead of using patients without complications, the model could be developed for patients with varying stays (example: less than 3 days, 4 to 7 days, more than 7 days).
The application of the multilayered neural network model to the population of patients with at least 1 complication reported prior to discharge revealed that medical complications had a slightly longer LOS than surgical complications (8 vs 9 days). Sepsis and deep surgical site infection were among the strongest drivers of extended LOS as compared to the predicted stay without complications. A systematic review by Akintürk et al found that the infection rate for adult spinal deformity surgery across 33 studies was on average 3.6%, 3 which is greater than the infection rate of 0.6% among all patients in this study, with 4 patients experiencing a deep infection and 6 with a superficial infection. Infection is a modifiable risk factor for increased length of stay that practices or hospital systems should consider evaluating if there is a high incidence given its strong effect on LOS. The total incidence of pre-discharge complications in this study was 38.2%, with an 15.7% incidence of major complications. A previous retrospective review of 1040 ASD patients yielded a major complication rate of 9.3%, 20 a difference which may be attributed to classification systems, identification of complications themselves, and the retrospective nature of the studies. Pleural injury, monitoring anomaly, and motor deficits were associated with a negative incremental difference between the predicted and actual LOS, but when rounded to the nearest whole number, pleural injury and motor deficits were aligned with the prediction. These specific complications, as well as dural tear, are addressed intraoperatively and thus may have little impact on LOS after the operation is complete.
Determining which complications should be singled out by the health systems in which they occur is largely subjective and differs across patient populations. As with any surgical procedure, there are inherent risks and complications that are unavoidable, thus leading to longer stays. There is, however, an opportunity to identify the minor complications that were associated with large increases in LOS as compared to major complications that did not influence how long patients remained in the hospital. For example, urinary tract infection led to an additional 3 days in the hospital, while major cardiovascular events such as myocardial infarction and stroke led to a similar stay. Major complications may be given more attention and thus do not lead to an unexpectedly long LOS, as is the case for monitoring anomaly, 21 while other complications like wound infection can quickly lead to reoperation if preoperative risk factors are not adequately considered.18,22,23 Ensuring that practices or hospital systems are up to date on practice guidelines as well as implementing prophylactic measures for common minor complications as appropriate are actionable steps toward reducing length of stay for ASD patients. This study found wide variability in incremental change within each larger category of complication. For example, medical complications such as sepsis led to a 24.1 day increase in LOS whereas UTI added 2.9 days, and operative complications such as vascular injury led to a 6.7-day incremental increase in LOS while monitoring anomaly had a 2.1-day incremental decrease from expected. It is therefore beneficial to have a granular view of complications as presented in this study rather than relying on larger groupings or classifications.
The multicenter setting and large cohort were significant strengths of this investigation, allowing for a more in-depth analysis of complication types because of higher incidence rates. Rather than simply classifying complications as mild vs severe or medical vs surgical, a wider array was presented. However, the retrospective nature of the chart review has inherent limitations considering the possibility of misreporting or underreporting of certain complications in the database, as well as a difficulty contextualizing the manner in which the complications arose and were treated. Additionally, complications may have manifested in the outpatient setting and are therefore not captured by the results. Although the multi-center approach allowed for a large cohort, the inherent slight variances in care between hospitals represents a possible limitation of the study design. The decision to develop the multilayered neural network with only 70% of the uncomplicated patients could be altered in the future, with a larger proportion of the sample being included in development. This, however, diminishes the strength of the validation step. There was also a degree of balancing the underfitting and overfitting for generalization purposes, while trying to maintain the accuracy of data prediction.
This predictive model has the opportunity to be validated further and published on a website for public use given the potential benefit of a patient-and-surgery adjusted tool for predicting resource allocation and extended LOS. In the future, it may be beneficial for researchers to view complications from a resource utilization perspective, with special consideration for complications with high clinical importance in terms of severity vs practical importance in terms of metrics such as LOS. LOS should not be used alone as a measure of complication severity because it is often multifactorial and can be unrelated to the indicated treatment, but long-term quality of life statistics for the patient should be included in the evaluation with consideration for social factors that may influence patient care. Anticipation would be advantageous for care centers. For example, early treatment of minor complications that greatly increase LOS or understanding the expected LOS for major complications intrinsic to the surgical treatment of ASD offer key insights into management decisions. Additional studies may incorporate complication-specific costs to the health system and the patient as measurements of severity.
Conclusion
Complications following surgery for ASD correction can have varying, yet predictable, effects on length of stay in the hospital. Some complications, which necessitate minimal intervention and are often classified as minor due to their minimal effect on patient health, can still lead to a significant and substantial increase in LOS. Conversely, other complications that significantly impair patient quality of life may not affect LOS at all. Classification systems and categorization of complications should consider these 2 aspects to accurately assess the relevance of their proposed schemes.
Footnotes
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: The International Spine Study Group (ISSG) is funded through research grants from DePuy Synthes (current), Nuvasive (current), K2M (current), Innovasis (past), Biomet (past), and individual donations. Funding sources did not play a role in investigation.
IRB Approval: This study was conducted according to strict institutional review board standards at each institution and abided by ethical guidelines for human subject research. Details can be find on ClinicalTrials.gov under ID NCT00738439.
ORCID iDs
Renaud Lafage https://orcid.org/0000-0002-4820-1835
Connor Sheehan https://orcid.org/0009-0004-3304-4824
Justin S. Smith https://orcid.org/0000-0003-0467-5534
Alan Daniels https://orcid.org/0000-0001-9597-4139
Bassel Diebo https://orcid.org/0000-0002-7835-2263
Munish Gupta https://orcid.org/0000-0002-4711-4377
Han Jo Kim https://orcid.org/0000-0002-7482-6994
Virginie Lafage https://orcid.org/0000-0002-0119-7111
References
- 1.Riley MS, Bridwell KH, Lenke LG, Dalton J, Kelly MP. Health-related quality of life outcomes in complex adult spinal deformity surgery. J Neurosurg Spine. 2018;28(2):194-200. doi: 10.3171/2017.6.SPINE17357. [DOI] [PubMed] [Google Scholar]
- 2.McCarthy IM, Hostin RA, Ames CP, et al. Total hospital costs of surgical treatment for adult spinal deformity: an extended follow-up study. Spine J. 2014;14(10):2326-2333. doi: 10.1016/j.spinee.2014.01.032. [DOI] [PubMed] [Google Scholar]
- 3.Akintürk N, Zileli M, Yaman O. Complications of adult spinal deformity surgery: a literature review. J Craniovertebr Junction Spine. 2022;13(1):17-26. doi: 10.4103/jcvjs.jcvjs_159_21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bortz C, Pierce KE, Brown A, et al. Frequency and implications of concurrent complications following adult spinal deformity corrective surgery. Spine. 2021;46(21):E1155-E1160. doi: 10.1097/BRS.0000000000004064. [DOI] [PubMed] [Google Scholar]
- 5.Lovecchio F, Jordan Y, Punyala A, et al. Timing of inpatient medical complications after adult spinal deformity surgery: early ambulation matters. Spine J. 2023;23(2):219-226. doi: 10.1016/j.spinee.2022.09.001. [DOI] [PubMed] [Google Scholar]
- 6.Safaee MM, Scheer JK, Ailon T, et al. Predictive modeling of length of hospital stay following adult spinal deformity correction: analysis of 653 patients with an accuracy of 75% within 2 days. World Neurosurg. 2018;115:e422-e427. doi: 10.1016/j.wneu.2018.04.064. [DOI] [PubMed] [Google Scholar]
- 7.Wick JB, Blandino A, Smith JS, et al. The ISSG-AO complication intervention score, but not major/minor designation, is correlated with length of stay following adult spinal deformity surgery. Global Spine J. 2023. doi: 10.1177/21925682231202782. Published online. [DOI] [PubMed] [Google Scholar]
- 8.Sciubba D, Jain A, Kebaish KM, et al. Development of a preoperative adult spinal deformity comorbidity score that correlates with common quality and value metrics: length of stay, major complications, and patient-reported outcomes. Global Spine J. 2021;11(2):146-153. doi: 10.1177/2192568219894951. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Pitter FT, Lindberg-Larsen M, Pedersen AB, Dahl B, Gehrchen M. Readmissions, length of stay, and mortality after primary surgery for adult spinal deformity: a 10-year Danish nationwide cohort study. Spine. 2019;44(2):E107-E116. doi: 10.1097/BRS.0000000000002782. [DOI] [PubMed] [Google Scholar]
- 10.Soroceanu A, Burton DC, Oren JH, et al. Medical complications after adult spinal deformity surgery incidence, risk factors, and clinical impact. Spine. 2016;41(22):1718-1723. doi: 10.1097/BRS.0000000000001636. [DOI] [PubMed] [Google Scholar]
- 11.Arora A, Demb J, Cummins DD, Callahan M, Clark AJ, Theologis AA. Predictive models to assess risk of extended length of stay in adults with spinal deformity and lumbar degenerative pathology: development and internal validation. Spine J. 2023;23(3):457-466. doi: 10.1016/j.spinee.2022.10.009. [DOI] [PubMed] [Google Scholar]
- 12.Arora A, Lituiev D, Jain D, et al. Predictive models for length of stay and discharge disposition in elective spine surgery: development, validation, and comparison to the ACS NSQIP risk calculator. Spine. 2023;48(1):E1-E13. doi: 10.1097/BRS.0000000000004490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Passias PG, Poorman GW, Vasquez-Montes D, et al. Predictive analytics for determining extended operative time in corrective adult spinal deformity surgery. Int J Spine Surg. 2022;16(2):291-299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Zhang AS, Veeramani A, Quinn MS, Alsoof D, Kuris EO, Daniels AH. Machine learning prediction of length of stay in adult spinal deformity patients undergoing posterior spine fusion surgery. J Clin Med. 2021;10(18):4074. doi: 10.3390/jcm10184074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Klineberg EO, Passias PG, Jalai CM, et al. Predicting extended length of hospital stay in an adult spinal deformity surgical population. Spine. 2016;41(13):E798-E805. doi: 10.1097/BRS.0000000000001391. [DOI] [PubMed] [Google Scholar]
- 16.Lafage R, Fong AM, Klineberg E, et al. Complication rate evolution across a 10-year enrollment period of a prospective multicenter database. J Neurosurg Spine. 2022;36(6):1012. doi: 10.3171/2021.10.SPINE21795. [DOI] [PubMed] [Google Scholar]
- 17.Elsamadicy AA, Freedman IG, Koo AB, et al. Influence of gender on discharge disposition after spinal fusion for adult spine deformity correction. Clin Neurol Neurosurg. 2020;194:105875. doi: 10.1016/j.clineuro.2020.105875. [DOI] [PubMed] [Google Scholar]
- 18.Arzeno AH, Koltsov J, Alamin TF, Cheng I, Wood KB, Hu SS. Short-term outcomes of staged versus same-day surgery for adult spinal deformity correction. Spine Deform. 2019;7(5):796-803. doi: 10.1016/j.jspd.2018.12.008. [DOI] [PubMed] [Google Scholar]
- 19.Arora A, Wague A, Srinivas R, et al. Risk factors for extended length of stay and non-home discharge in adults treated with multi-level fusion for lumbar degenerative pathology and deformity. Spine Deform. 2023;11(3):685-697. doi: 10.1007/s43390-022-00620-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Dinizo M, Dolgalev I, Passias PG, Errico TJ, Raman T. Complications after adult spinal deformity surgeries: all are not created equal. Int J Spine Surg. 2021;15(1):137-143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Yoshida G, Ushirozako H, Kobayashi S, et al. Intraoperative neuromonitoring during adult spinal deformity surgery: alert-positive cases for various surgical procedures. Spine Deform. 2019;7(1):132-140. doi: 10.1016/j.jspd.2018.05.015. [DOI] [PubMed] [Google Scholar]
- 22.Chan L, Li Y, Hai Y, Liu Y, Zhang Y. Risk factors of unintended return to the operating room in adult spinal deformity. J Orthop Surg Res. 2021;16(1):240. doi: 10.1186/s13018-021-02385-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Li XJ, Lenke LG, Jin L, et al. Surgeon-specific risk stratification model for early complications after complex adult spinal deformity surgery. Spine Deform. 2020;8(1):97-104. doi: 10.1007/s43390-020-00047-y. [DOI] [PubMed] [Google Scholar]