Abstract
Background: Initial fixed-bearing hinge designs for primary total knee arthroplasty (TKA) had high rates of aseptic loosening. There are limited data on contemporary rotating-hinge implants. Purpose: We sought to determine survivorship and functional outcomes of contemporary rotating-hinge implants used in primary TKA. Methods: Retrospective review identified 54 primary rotating-hinge TKAs implanted in 49 patients from 2014 to 2018 at a single institution. Patients identified were 76% women, the mean body mass index was 29 kg/m2, the mean age was 65 years, and the mean follow-up was 3 years. The primary diagnosis for TKA in all cases was severe instability and ligamentous compromise. Secondary diagnoses included post-traumatic osteoarthritis (11, 20%), neurologic disease (10, 19%), inflammatory arthritis (10, 19%), connective tissue disease (3, 6%), valgus deformity (16, 30%), varus deformity (2, 4%), and recurvatum (2, 4%). Preoperative, postoperative (within 6 weeks), and most recent radiographs were reviewed. In this study, we collected preoperative, 1-year, and 2-year patient-reported outcome measures (PROMs) for patients with primary rotating-hinge TKA. Patient-reported outcome measures were prospectively collected, including the Knee Injury and Osteoarthritis Outcome Survey for Joint Replacement (KOOS JR) scores and the Mental (MCS) and Physical Component Scores (PCS) of the Veterans RAND 12-Item Health Survey (VR-12). Kaplan-Meier analysis was used to determine implant survivorship. Results: Reoperation was required in 6% (3/54); indications included periprosthetic joint infection (1), peripatellar fibrosis (1), and periprosthetic femur fracture (1). At both 2 and 5 years, survivorship free from all-cause reoperation was 95% and from revision for aseptic loosening was 100%. Mean KOOS JR scores increased from 47 preoperatively to 65 at 2 years postoperatively. On radiographic review, there were no progressive radiolucent lines consistent with aseptic loosening at final follow-up. Conclusion: The findings of this single-center, multi-surgeon retrospective case series on the use of rotating-hinge implants for primary TKA suggest excellent 2-year survivorship free from reoperation and no revisions for aseptic loosening. We report modest improvement in a variety of PROMs at 1-year and 2-year follow-up. Despite improvement, clinical outcomes were poor for a primary implant. Longer-term follow-up is required to monitor the durability of primary hinges.
Keywords: primary total knee arthroplasty, hinged knee implants, implant design, radiographic outcomes, patient-reported outcome measures
Introduction
To perform primary total knee arthroplasty (TKA), functional collateral ligaments are required for proper alignment and stability [2,10]. Hinged implants are indicated in cases of severe deformity, bone loss, or non-correctable ligamentous deficiency [2]. Initial designs of hinged TKA implants permitted only knee flexion and extension. These fixed-hinge designs transmitted torsional loads to the bone-implant interface that quickly exceeded the tolerance of the implant-cement or bone-cement interfaces, leading to a high rate of failure; they were suitable only for salvage situations such as neoplasm resection [10,12]. However, later designs have sought to address this problem by enabling axial rotation [20]. These rotating-hinge knee implants are the latest iteration of hinged knee implants and better simulate normal kinematics. Although still often used in revision TKA, they are used more frequently in the primary setting [1].
Studies reporting outcomes after primary rotating-hinge TKAs used for non-oncologic indications are sparse. Owing to the relatively rare use of this implant, many studies combined primary and revision TKA [5,7,14]. Others assessed a specific brand of rotating-hinge implants including Endo-Model [3,22] (Waldemar LINK GmbH and Co), Modular Rotating Hinge System [15] (Stryker), and Legion Hinge Knee Replacement [19] (Smith & Nephew).
We sought to report our institutional experience with these contemporary implants. Our objectives were to determine reoperation rate, early survivorship, radiographic results, and patient-reported outcome measures (PROMs) of a primary, rotating-hinge TKA for non-oncologic indications.
Methods
After institutional review board approval at the Hospital for Special Surgery for this single-center, multi-surgeon retrospective case series, we performed a retrospective review of medical records for all cases of primary TKA using 4 contemporary rotating-hinge implant designs for non-oncologic indications from 2014 to 2018 (Table 1). We selected 2018 as the cutoff for the study period to allow for minimum follow-up of 5 years. Any cases of revision TKA, conversion TKA, and TKA with distal femoral replacement were excluded from the study. Relevant clinical and surgical information was recorded, including preoperative diagnosis, patient demographic data, postoperative reoperations, and follow-up data.
Table 1.
Patient demographics, characteristics, indications, and implants.
| Variable | Mean (SD) or number (%) |
|---|---|
| Age, years | 65 (SD = 12) |
| Female | 41 (76%) |
| Body mass index, kg/m2 | 29 (SD = 10) |
| American Society of Anesthesiology Risk Level | |
| 1 | 1 (2%) |
| 2 | 32 (59%) |
| 3 | 21 (40%) |
| Indication | |
| Severe ligamentous instability | 34 (63%) |
| Severe, uncorrectable valgus | 16 (29%) |
| Severe, uncorrectable varus | 2 (4%) |
| Recurvatum | 2 (4%) |
| Implants | |
| Modular Rotation Hinge Knees | 23 (43%) |
| NexGen Rotating Hinge Knees | 18 (33%) |
| Legion HK Hinge Knees | 9 (17%) |
| S-ROM Noiles Rotating Hinges | 4 (7%) |
SD standard deviation.
Preoperative, postoperative (within 6 weeks), and most recent radiographs were reviewed using the picture archiving and communication system (PACS) system (Sectran). Preoperative radiographs were reviewed to discern the presence of previous hardware, evaluate bone loss using the Anderson Orthopaedic Research Institute (AORI) system [8], and verify preoperative diagnosis. The AORI classification scores femoral and tibial bone loss based on severity [8]. Briefly, the AORI classification is as follows: type I bone loss includes minor defects of the femur or tibial with intact metaphyseal bone and no loss of component stability; type II bone loss represents metaphyseal bone loss and is subclassified into either IIA (unicondylar) and IIB (bicondylar); and type III bone loss represents significant metaphyseal bone loss compromising a major portion of the femoral condyles or tibial plateau [8].
The first postoperative radiographs were reviewed to elucidate the following implant and fixation characteristics: level of constraint (verification of hinge TKA) and implant model, type of stem fixation, lengths of femoral and tibial constructs, and presence of cones or sleeves. The last available radiographs were compared with the first postoperative radiographs to evaluate for gross implant loosening, implant failure, and osteolysis in periprosthetic bone. Radiographs were evaluated for signs of reoperation and/or revision to verify these variables on medical records. Radiographs were also inspected for radiolucent lines at the bone-cement interface, cement-implant interface, or bone-implant interface using a previously published percentage-based system to evaluate for aseptic loosening [4]. Percent involvement of the femoral implant (body, cone/sleeve, and stem) interface was based on the lateral radiograph, whereas percent involvement of the tibial implant (baseplate, cone/sleeve, and stem) interface was based on anteroposterior (AP) and lateral interfaces. All radiographs were manually reviewed by 2 orthopedic surgeons (TDB and AP) with fellowship training in complex adult reconstruction and joint replacement.
The PROMs are prospectively collected as part of our institution’s arthroplasty registry. In this study, we collected preoperative, 1-year, and 2-year PROMs for patients with primary rotating-hinge TKA. Specifically, we collected the Knee Injury and Osteoarthritis Outcome Survey for Joint Replacement (KOOS JR) scores as well as both Mental (MCS) and Physical Component Scores (PCS) of the Veterans RAND 12-Item Health Survey (VR-12). The KOOS JR is a validated short-form survey that combines pain and function into a single score out of that encompasses a patient’s knee health [17]. The scoring is on a 100-point scale, with 0 representing the complete knee disability and 100 representing the perfect knee health [17]. The VR-12 covers 7 health domains: general health perception, physical functioning, role limitations due to physical or emotional problems, bodily pain, energy levels, social functioning, and mental health [23]. For this study, mental and physical health components were assessed. These various PROMs were collected to capture multiple facets of patient health and recovery from primary TKA.
Normally distributed data were presented as means with standard deviations. Survivorship free from all-cause reoperation TKA at 2 and 5 years was determined through a Kaplan-Meier survival analysis. In the approach, patients are censored based on last clinical or radiographic follow-up [13]. Significance was set at P < .05. All tests were 2-tailed. Statistical analyses were performed using SAS 9.4.
Fifty-four primary rotating-hinge TKAs in 49 patients were included. The treating surgeon determined primary TKA with rotating-hinge knee components was appropriate in cases of significant instability and/or deformity not amenable to treatment with lower levels of constraint. Seventeen different arthroplasty surgeons contributed to this case series. The study group was 76% female with a mean age of 65 years (standard deviation [SD] = 12), mean body mass index (BMI) was 29 kg/m2 (SD = 10), and the mean follow-up was 3 years (Table 1).
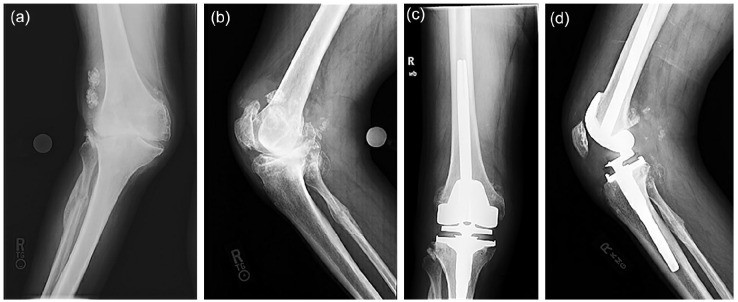
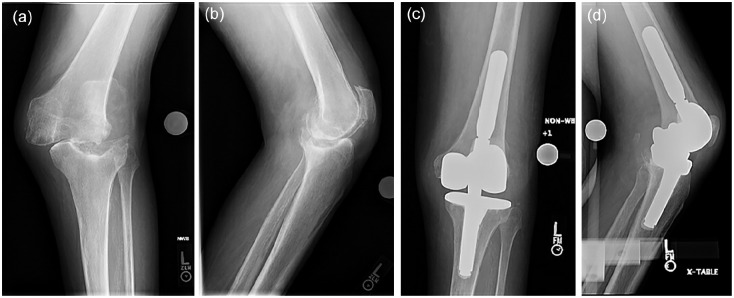
The primary indication for primary TKA using rotating-hinge knee components was instability in 34 knees (63%), valgus deformity in 16 knees (29%), varus deformity in 2 knees (4%), and recurvatum in 2 knees (4%). Instability was associated with previous trauma (11, 20%) (Fig. 1), neurologic disease (10, 19%) (Fig. 2), inflammatory arthritis (10, 19%), or connective tissue disease (3, 6%). Femoral bone loss was classified as AORI 1 in 33 (61%), AORI 2A in 18 (33%), and AORI 2B in 3 (6%). Tibial bone loss was classified as AORI 1 in 27 (50%), AORI 2A in 23 (43%), AORI 2B in 3 (6%), and AORI 3 in 1 (1%). There were 6 cases (11%) with previous hardware (5 screws, 1 plate).
Fig. 1.
A 59-year-old patient with a history of complex ligamentous injury to the right knee while playing football that was surgically addressed but eventually led to progressive right knee deformity and pain medially that made knee flexion difficult. Anteroposterior (a) and lateral (b) preoperative radiographs demonstrated severe valgus deformity, tricompartmental joint space narrowing and osteophytes, subchondral collapse, and healed proximal fibular fracture with callus formation. Intraoperatively, the medial collateral ligament was grossly attenuated, and the lateral tibial defect was filled with a bone autograft. Postoperatively, anteroposterior (c) and lateral (d) radiographs demonstrated hinged implants with neutral alignment and without complication.
Fig. 2.
A 73-year-old patient with a history of idiopathic demyelinating neuropathy presented with left knee pain and varus deformity that progressed significantly over a year. He could not bear weight on his left leg due to knee pain and instability. Anteroposterior (a) and lateral (b) preoperative radiographs demonstrate lateral femoral-tibial joint subluxation, large central tibial bone defect, and bone fragmentation of the medial femoral condyle. The patient was indicated for primary TKA with a hinge implant. Intraoperatively, the medial collateral ligament was incompetent, and the tibial defect was filled with bone autograft. Postoperative anteroposterior (c) and lateral (d) radiographs demonstrated hinge implants with excellent alignment and no complication.
The 54 rotating-hinge TKAs implanted included 23 Modular Rotating Hinge Knees (Stryker), 18 NexGen Rotating Hinge Knees (Zimmer Biomet), 9 Legion HK Hinge Knees (Smith & Nephew), and 4 S-ROM Noiles Rotating Hinges (DePuy Synthes). Mean femoral and tibial construct lengths were 146 mm (SD 47) and 121 mm (SD 37), respectively. No cones were used. Sleeves were used in 4 knees (7%) (all with DePuy S-ROM Noiles implants). On the femoral side, 28 stems were cemented (52%), and 26 were cementless (48%). On the tibial side, 35 stems were cemented (65%), and 16 were cementless (30%). Mean operative time was 141 minutes (range = 1-5 hours). Postoperative protocols were personalized based on the patient’s condition. Patients were routinely made weightbearing as tolerated without range of motion constraints. All patients received thromboprophylaxis starting on day of surgery or postoperative day 1 and minimum standard antibiotic prophylaxis.
Results
The overall reoperation rate was 6% (3/54). There were no reoperations for aseptic loosening. In 1 patient, a periprosthetic joint infection (PJI) at 2 years postsurgery was managed with debridement, antibiotics, irrigation, and implant retention (DAIR). One month later, this patient developed a patella fracture managed with a patellectomy and extensor mechanism reconstruction using hamstring autograft. A second patient was treated with arthroscopic debridement of peripatellar fibrosis 4 months post primary hinge which went on to require polyethylene insert exchange for instability 1 year later. A third patient suffered a distal periprosthetic femur fracture after a ground-level fall 8 years after primary TKA. The femoral implants were found to be loose, and the patient underwent revision TKA with a distal femoral replacement and revision rotating hinge components. All patients had stable and functional implants at the time of final follow-up. Survivorship free from all-cause reoperation was 95% (95% confidence interval [CI] = 88%-100%) at both 2 and 5 years (Fig. 3). Survivorship free from reoperation for aseptic loosening was 100% at 2 and 5 years.
Fig. 3.
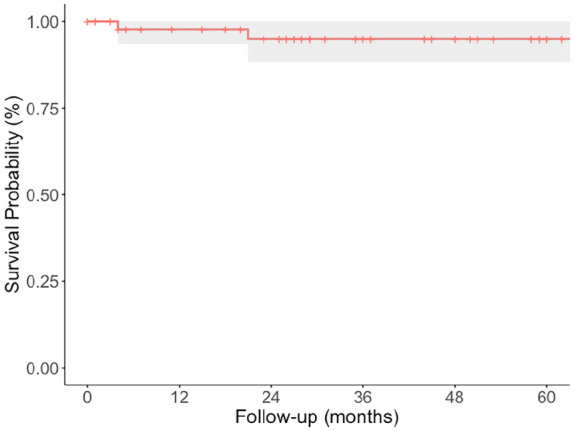
Kaplan-Meier survival plot of primary hinges with all-cause postoperative reoperation as the endpoint. The shaded section corresponds to the 95% confidence interval.
After primary TKA with a rotating-hinge knee implant, there were minimal postoperative complications. No patients developed wound complications or surgical site infection. One patient developed venous thromboembolism; that person, who had a prior history of clotting and inferior vena cava filter, developed a popliteal vein clot 2 weeks postoperatively that was treated with enoxaparin. No patients went on to require manipulation under anesthesia (MUA).
At mean radiographic follow-up of 3 years, there were no signs of gross implant loosening, implant failure, or osteolysis. With respect to radiolucent lines on the femoral side, there were incomplete non-progressive radiolucent lines in 9 patients. On the tibial side, there were incomplete non-progressive radiolucent lines in 2 patients.
There were modest increases in KOOS JR, VR-12 MCS, and VR-12 PCS scores from preoperative to 1-year and 2-year follow-up (Table 2). The proportion of PROM completion at each time point ranged from 24% to 33%. Mean KOOS JR increased from 47 (SD 14) preoperatively to 65 (SD 19) at 1 year and 64 (SD = 24) at 2 years. There were 6 cases with both preoperative and 1-year KOOS JR scores, of which 4 (67%) achieved KOOS JR minimum clinically important difference (MCID). There were 7 cases with both preoperative and 2-year KOOS JR scores, of which 4 (57%) achieved KOOS JR MCID. Mean VR-12 MCS increased from 48 (SD = 9) preoperatively to 52 (SD = 11) at 1 year and returned to 48 (SD = 17) at 2 years. Mean VR-12 PCS increased from 29 (SD = 7) preoperatively to 34 (SD = 10) at 1 year and 37 (SD = 12) at 2 years.
Table 2.
Preoperative and 1-year and 2-year postoperative patient-reported outcome measure (PROM) scores.
| PROM | Preoperative | % Completion | 1 year | % Completion | 2 years | % Completion |
|---|---|---|---|---|---|---|
| KOOS JR, mean (SD) | 47 (14) | 24 | 65 (19) | 26 | 64 (24) | 28 |
| VR-12 PCS, mean (SD) | 29 (7) | 33 | 34 (10) | 26 | 37 (12) | 24 |
| VR-12 MCS, mean (SD) | 48 (9) | 33 | 52 (11) | 26 | 48 (17) | 24 |
SD standard deviation, KOOS JR Knee Injury and Osteoarthritis Outcome Score for Joint Replacement, VR-12 Veterans RAND 12-Item Health Survey, PCS physical component score, MCS mental component score.
Discussion
We sought to analyze reoperation, early survivorship, radiographic outcomes, and PROMs in patients undergoing primary TKA with contemporary rotating-hinge implants. In this retrospective case series, we report low reoperations, excellent early survivorship free from reoperation, minimal evidence of loosening or other implant failure on radiographic review, and among the patients who completed the questionnaires, modest improvements in PROMs from preoperative to 2-year postoperative time points.
There are several limitations in this study. First, this study is subject to the pitfalls of a retrospective review including selection bias and confounding. Second, we combined results of several various rotating-hinge designs, and therefore, our findings may not extend to other designs. Furthermore, we include the surgical outcomes of multiple surgeons (n = 17), which may introduce some confounding factors. However, these results are perhaps more generalizable than studies that evaluated only 1 implant and 1 surgeon. Third, similar to previous studies, our study is limited by small sample size, given that primary TKA with hinged implants is a relatively rare procedure. Fourth, longer follow-up time is ideal for monitoring survivorship from aseptic loosening; however, we were limited by our retrospective study design. Also, excluding cases with shorter follow-up would have substantially decreased our already small sample size. Instead, we chose to include these cases and use the Kaplan-Meier survivorship method to estimate survivorship, which accounts for differential follow-up time using right censoring [8]. In addition, all procedures were performed at a specialty hospital, making our results less generalizable to all practice settings. Finally, not all patients completed PROMs, with questionnaire completion ranging from 24% to 33% (Table 2); these missing data limit the PROMs assessment of this study.
In this study, 2-year and 5-year survivorship free from any reoperation was 95% (95% CI = 88%-100%) with excellent survivorship free from aseptic loosening at 5 years (100%). Three reoperations were performed, 1 for PJI, 1 for peripatellar fibrosis, and 1 for periprosthetic femur fracture. These results are similar to previously published reports. A recent systematic review and meta-analysis evaluated the performance of rotating-hinge implants in primary TKA for non-tumor indications (N = 1425 TKAs) [1]. Five-year survivorship was 92% with the most common causes of failures being infection, aseptic loosening, dislocation, and periprosthetic fracture [1]. Another multi-center study of 112 TKAs showed survivorship of 91% at 7 years with rates of aseptic loosening at 0% at 5 years [18]. Hintze and colleagues reported on the outcomes of 106 complex primary TKAs performed using a single rotating hinge implant design from 2004 to 2013 [11]. In their study, the 10-year survivorship free from all-cause revision was 92% [11]. Infection has been cited as a common reason for failure in primary rotating-hinge TKAs for non-tumor indications [1]. Rotating-hinge TKA often requires extensive soft tissue dissection and longer operative times, thereby increasing risk of infection [9]. Initial designs of fixed-hinge implants had much higher rates of patellar complications, but the axial rotation and modified patellofemoral joint of newer rotating-hinge designs have resulted in improved patellar tracking and decreased the severity and incidence of these complications [1,21]. Nonetheless, the incidence of patellar tracking complications ranges from 2.5% to 5% in the literature. Myriad contributing factors may explain the high rate of patellar complications, including higher load on the extensor mechanism from increased hinge constraint, unchanged moment arm with flexion, as well as a challenging patient population that in which joint line preservation is difficult and patellar weakness is not uncommon [16,21].
We report modest improvement in a variety of PROMs (Lower Extremity Activity Score, VR-12 MCS and PCS, and KOOS JR) at 1-year and 2-year follow-up. We report a mean 2-year KOOS JR score of 64. The mean 2-year VR-12 PCS was 37, and the mean 2-year VR-12 MCS was 48. In a systematic review by Abdulkarim et al [1], Knee Society Score (KSS) was the main reported functional outcome score. The KSS is divided into clinical score, measuring pain reduction, and function score, measuring functional improvement [6]. Mean postoperative functional score was 68/100 and clinical score was 85/100, emphasizing the pain reduction benefits of rotating-hinge knee implants in this patient population with severe indications [1]. Another study of primary rotating-hinge TKA demonstrated substantial increases in KSS and Western Ontario and McMaster University Arthritis Index (WOMAC) scores along with a decrease in postoperative use of gait aids at 2-month follow-up (92%) [15]. Despite improvement, there is a large variance in PROMs scores for these patients both in our study and others [1,15]. These results emphasize the complexity inherent to this patient population and the importance of setting expectations with patients prior to primary TKA with rotating-hinge implants.
In conclusion, this single-center, multi-surgeon retrospective case series found that patients with contemporary rotating-hinge primary TKAs had few complications, excellent early survivorship, no evidence of loosening on radiographic review, and modest PROMs improvements. There were only 3 reoperations (1 each for PJI, peripatellar fibrosis, and periprosthetic distal femur fracture). These findings suggest that primary TKA with rotating-hinge implants used in well-selected patients for non-tumor indications may have acceptable survival rates and result in reduced pain and improved function. Further study is needed.
Supplemental Material
Supplemental material, sj-docx-1-hss-10.1177_15563316241276869 for Survivorship and Functional Outcomes After Complex Primary Total Knee Arthroplasty With Contemporary Rotating-Hinge Implants by Simarjeet Puri, Troy D. Bornes, Colin C. Neitzke, Agnes D. Jones, Amber A. Hamilton, Ajay Premkumar, Peter K. Sculco and Brian P. Chalmers in HSS Journal®
Supplemental material, sj-docx-2-hss-10.1177_15563316241276869 for Survivorship and Functional Outcomes After Complex Primary Total Knee Arthroplasty With Contemporary Rotating-Hinge Implants by Simarjeet Puri, Troy D. Bornes, Colin C. Neitzke, Agnes D. Jones, Amber A. Hamilton, Ajay Premkumar, Peter K. Sculco and Brian P. Chalmers in HSS Journal®
Supplemental material, sj-docx-3-hss-10.1177_15563316241276869 for Survivorship and Functional Outcomes After Complex Primary Total Knee Arthroplasty With Contemporary Rotating-Hinge Implants by Simarjeet Puri, Troy D. Bornes, Colin C. Neitzke, Agnes D. Jones, Amber A. Hamilton, Ajay Premkumar, Peter K. Sculco and Brian P. Chalmers in HSS Journal®
Supplemental material, sj-docx-4-hss-10.1177_15563316241276869 for Survivorship and Functional Outcomes After Complex Primary Total Knee Arthroplasty With Contemporary Rotating-Hinge Implants by Simarjeet Puri, Troy D. Bornes, Colin C. Neitzke, Agnes D. Jones, Amber A. Hamilton, Ajay Premkumar, Peter K. Sculco and Brian P. Chalmers in HSS Journal®
Supplemental material, sj-docx-5-hss-10.1177_15563316241276869 for Survivorship and Functional Outcomes After Complex Primary Total Knee Arthroplasty With Contemporary Rotating-Hinge Implants by Simarjeet Puri, Troy D. Bornes, Colin C. Neitzke, Agnes D. Jones, Amber A. Hamilton, Ajay Premkumar, Peter K. Sculco and Brian P. Chalmers in HSS Journal®
Supplemental material, sj-docx-6-hss-10.1177_15563316241276869 for Survivorship and Functional Outcomes After Complex Primary Total Knee Arthroplasty With Contemporary Rotating-Hinge Implants by Simarjeet Puri, Troy D. Bornes, Colin C. Neitzke, Agnes D. Jones, Amber A. Hamilton, Ajay Premkumar, Peter K. Sculco and Brian P. Chalmers in HSS Journal®
Supplemental material, sj-docx-7-hss-10.1177_15563316241276869 for Survivorship and Functional Outcomes After Complex Primary Total Knee Arthroplasty With Contemporary Rotating-Hinge Implants by Simarjeet Puri, Troy D. Bornes, Colin C. Neitzke, Agnes D. Jones, Amber A. Hamilton, Ajay Premkumar, Peter K. Sculco and Brian P. Chalmers in HSS Journal®
Supplemental material, sj-docx-8-hss-10.1177_15563316241276869 for Survivorship and Functional Outcomes After Complex Primary Total Knee Arthroplasty With Contemporary Rotating-Hinge Implants by Simarjeet Puri, Troy D. Bornes, Colin C. Neitzke, Agnes D. Jones, Amber A. Hamilton, Ajay Premkumar, Peter K. Sculco and Brian P. Chalmers in HSS Journal®
Footnotes
The author(s) declared the following potential conflicts of interest with respect to the research, authorship, and/or publication of this article: AP, MD, reports relationships with AccuJoint Inc, Azra Care, and Elsevier. PKS, MD, reports relationships with DePuy, EOS Imaging, Intellijoint Surgical, Lima Corporate, and Parvizi Surgical Innovation. BPC, MD, reports relationships with Ortho Development, Smith & Nephew, HSS Journal, and The Journal of Arthroplasty. The other authors report no potential conflicts of interest.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Human/Animal Rights: All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2013.
Informed Consent: Informed consent was waived from all patients included in this study.
Level of Evidence: Level IV: retrospective case series
Required Author Forms: Disclosure forms provided by the authors are available with the online version of this article as supplemental material.
ORCID iD: Brian P. Chalmers  https://orcid.org/0000-0002-2094-3888
https://orcid.org/0000-0002-2094-3888
References
- 1. Abdulkarim A, Keane A, Hu SY, Glen L, Murphy DJ. Rotating-hinge knee prosthesis as a viable option in primary surgery: literature review & meta-analysis. Orthop Traumatol Surg Res. 2019;105(7):1351–1359. 10.1016/j.otsr.2019.08.012. [DOI] [PubMed] [Google Scholar]
- 2. Babazadeh S, Stoney JD, Lim K, Choong PFM. The relevance of ligament balancing in total knee arthroplasty: how important is it? A systematic review of the literature. Orthop Rev. 2009;1(2):e26. 10.4081/or.2009.e26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Bistolfi A, Lustig S, Rosso F, Dalmasso P, Crova M, Massazza G. Results with 98 Endo-Modell rotating hinge prostheses for primary knee arthroplasty. Orthopedics. 2013;36(6):e746–752. 10.3928/01477447-20130523-19. [DOI] [PubMed] [Google Scholar]
- 4. Chalmers BP, Sculco PK, Fehring KA, Trousdale RT, Taunton MJ. A novel percentage-based system for determining aseptic loosening of total knee arthroplasty tibial components. J Arthroplasty. 2017;32(7):2274–2278. 10.1016/j.arth.2017.02.020. [DOI] [PubMed] [Google Scholar]
- 5. Cottino U, Abdel MP, Perry KI, Mara KC, Lewallen DG, Hanssen AD. Long-term results after total knee arthroplasty with contemporary rotating-hinge prostheses. J Bone Joint Surg Am. 2017;99(4):324–330. 10.2106/JBJS.16.00307. [DOI] [PubMed] [Google Scholar]
- 6. Culliton SE, Bryant DM, MacDonald SJ, Hibbert KM, Chesworth BM. Validity and internal consistency of the new knee society knee scoring system. Clin Orthop. 2018;476(1):77–84. 10.1007/s11999.0000000000000014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Efe T, Roessler PP, Heyse TJ, et al. Mid-term results after implantation of rotating-hinge knee prostheses: primary versus revision. Orthop Rev. 2012;4(4):e35. 10.4081/or.2012.e35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Engh GA, Ammeen DJ. Bone loss with revision total knee arthroplasty: defect classification and alternatives for reconstruction. Instr Course Lect. 1999;48:167–175. [PubMed] [Google Scholar]
- 9. Henderson ER, Groundland JS, Pala E, et al. Failure mode classification for tumor endoprostheses: retrospective review of five institutions and a literature review. J Bone Joint Surg Am. 2011;93(5):418–429. 10.2106/JBJS.J.00834. [DOI] [PubMed] [Google Scholar]
- 10. Hernández-Vaquero D, Sandoval-García MA. Hinged total knee arthroplasty in the presence of ligamentous deficiency. Clin Orthop. 2010;468(5):1248–1253. 10.1007/s11999-009-1226-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Hintze J, von Niemeläinen M, Sintonen H, Nieminen J, Eskelinen A. Good mid-term outcome of the rotating hinge knee in primary total knee arthroplasty: results of a single center cohort of 106 knees with a median follow-up of 6.3 years. Knee. 2021;28:273–281. 10.1016/j.knee.2020.12.016. [DOI] [PubMed] [Google Scholar]
- 12. Inglis AE, Walker PS. Revision of failed knee replacements using fixed-axis hinges. J Bone Joint Surg Br. 1991;73(5):757–761. 10.1302/0301-620X.73B5.1894661. [DOI] [PubMed] [Google Scholar]
- 13. Kaplan EL, Meier P. Nonparametric estimation from incomplete observations. In: Kotz S, Johnson NL. eds. Breakthroughs in Statistics: Methodology and Distribution. Springer Series in Statistics. Berlin: Springer; 1992:319–337. 10.1007/978-1-4612-4380-925. [DOI] [Google Scholar]
- 14. Kearns SM, Culp BM, Bohl DD, Sporer SM, Della Valle CJ, Levine BR. Rotating hinge implants for complex primary and revision total knee arthroplasty. J Arthroplasty. 2018;33(3):766–770. 10.1016/j.arth.2017.10.009. [DOI] [PubMed] [Google Scholar]
- 15. Kowalczewski J, Marczak D, Synder M, Sibiński M. Primary rotating-hinge total knee arthroplasty: good outcomes at mid-term follow-up. J Arthroplasty. 2014;29(6):1202–1206. 10.1016/j.arth.2013.12.013. [DOI] [PubMed] [Google Scholar]
- 16. Long R, Gheduzzi S, Bucher TA, Toms AD, Miles AW. A biomechanical evaluation of hinged total knee replacement prostheses. Proc Inst Mech Eng [H]. 2013;227(8):875–883. 10.1177/0954411913488506. [DOI] [PubMed] [Google Scholar]
- 17. Lyman S, Lee Y-Y, Franklin PD, Li W, Cross MB, Padgett DE. Validation of the KOOS, JR: a short-form knee arthroplasty outcomes survey. Clin Orthop Relat Res. 2016;474:1461–1471. 10.1007/s11999-016-4719-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Neri T, Boyer B, Papin PE, et al. Contemporary rotating hinge arthroplasty can safely be recommended in complex primary surgery. Knee Surg Sports Traumatol Arthrosc. 2020;28(6):1780–1788. 10.1007/s00167-019-05589-x. [DOI] [PubMed] [Google Scholar]
- 19. Perrin DL, Turgeon TR. Guided-motion hinged knee replacement prosthesis: early survival rate and postoperative patient function and satisfaction. Can J Surg J Can Chir. 2020;63(3):E196–E201. 10.1503/cjs.002419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Rodríguez-Merchán EC. Total knee arthroplasty using hinge joints: indications and results. EFORT Open Rev. 2019;4(4):121–132. 10.1302/2058-5241.4.180056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Rouquette L, Batailler C, Muller B, Neyret P, Servien E, Lustig S. Early complications and causes of revision after rotating-hinge TKA. Arch Orthop Trauma Surg. 2020;140(1):109–119. 10.1007/s00402-019-03290-9. [DOI] [PubMed] [Google Scholar]
- 22. Sanguineti F, Mangano T, Formica M, Franchin F. Total knee arthroplasty with rotating-hinge Endo-Model prosthesis: clinical results in complex primary and revision surgery. Arch Orthop Trauma Surg. 2014;134(11):1601–1607. 10.1007/s00402-014-2061-1. [DOI] [PubMed] [Google Scholar]
- 23. Schalet BD, Rothrock NE, Hays RD, et al. Linking physical and mental health summary scores from the Veterans RAND 12-Item Health Survey (VR-12) to the PROMIS(®) Global Health Scale. J Gen Intern Med. 2015;30(10):1524–1530. 10.1007/s11606-015-3453-9.a [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-docx-1-hss-10.1177_15563316241276869 for Survivorship and Functional Outcomes After Complex Primary Total Knee Arthroplasty With Contemporary Rotating-Hinge Implants by Simarjeet Puri, Troy D. Bornes, Colin C. Neitzke, Agnes D. Jones, Amber A. Hamilton, Ajay Premkumar, Peter K. Sculco and Brian P. Chalmers in HSS Journal®
Supplemental material, sj-docx-2-hss-10.1177_15563316241276869 for Survivorship and Functional Outcomes After Complex Primary Total Knee Arthroplasty With Contemporary Rotating-Hinge Implants by Simarjeet Puri, Troy D. Bornes, Colin C. Neitzke, Agnes D. Jones, Amber A. Hamilton, Ajay Premkumar, Peter K. Sculco and Brian P. Chalmers in HSS Journal®
Supplemental material, sj-docx-3-hss-10.1177_15563316241276869 for Survivorship and Functional Outcomes After Complex Primary Total Knee Arthroplasty With Contemporary Rotating-Hinge Implants by Simarjeet Puri, Troy D. Bornes, Colin C. Neitzke, Agnes D. Jones, Amber A. Hamilton, Ajay Premkumar, Peter K. Sculco and Brian P. Chalmers in HSS Journal®
Supplemental material, sj-docx-4-hss-10.1177_15563316241276869 for Survivorship and Functional Outcomes After Complex Primary Total Knee Arthroplasty With Contemporary Rotating-Hinge Implants by Simarjeet Puri, Troy D. Bornes, Colin C. Neitzke, Agnes D. Jones, Amber A. Hamilton, Ajay Premkumar, Peter K. Sculco and Brian P. Chalmers in HSS Journal®
Supplemental material, sj-docx-5-hss-10.1177_15563316241276869 for Survivorship and Functional Outcomes After Complex Primary Total Knee Arthroplasty With Contemporary Rotating-Hinge Implants by Simarjeet Puri, Troy D. Bornes, Colin C. Neitzke, Agnes D. Jones, Amber A. Hamilton, Ajay Premkumar, Peter K. Sculco and Brian P. Chalmers in HSS Journal®
Supplemental material, sj-docx-6-hss-10.1177_15563316241276869 for Survivorship and Functional Outcomes After Complex Primary Total Knee Arthroplasty With Contemporary Rotating-Hinge Implants by Simarjeet Puri, Troy D. Bornes, Colin C. Neitzke, Agnes D. Jones, Amber A. Hamilton, Ajay Premkumar, Peter K. Sculco and Brian P. Chalmers in HSS Journal®
Supplemental material, sj-docx-7-hss-10.1177_15563316241276869 for Survivorship and Functional Outcomes After Complex Primary Total Knee Arthroplasty With Contemporary Rotating-Hinge Implants by Simarjeet Puri, Troy D. Bornes, Colin C. Neitzke, Agnes D. Jones, Amber A. Hamilton, Ajay Premkumar, Peter K. Sculco and Brian P. Chalmers in HSS Journal®
Supplemental material, sj-docx-8-hss-10.1177_15563316241276869 for Survivorship and Functional Outcomes After Complex Primary Total Knee Arthroplasty With Contemporary Rotating-Hinge Implants by Simarjeet Puri, Troy D. Bornes, Colin C. Neitzke, Agnes D. Jones, Amber A. Hamilton, Ajay Premkumar, Peter K. Sculco and Brian P. Chalmers in HSS Journal®