Abstract
Background:
Patients presenting with a sinus tract over total knee arthroplasty (TKA) are challenging cases of periprosthetic joint infection (PJI). A 2-stage revision TKA has long been considered the gold standard for the management of PJI. At our institution, approximately 85% of patients with PJI, including patients with a sinus tract, undergo 1-stage revision TKA.
Purpose:
We sought to evaluate rates of reinfection and reoperation and predictors of failure of 1-stage revision TKA in patients with a concomitant sinus tract.
Methods:
We retrospectively reviewed patients with PJI and a sinus tract overlying TKA who underwent 1-stage revision TKA following a well-defined surgical protocol at our institution between January 2001 and December 2018. Of 170 patients included, 69 patients (40.6%) had a sinus tract overlying TKA; 101 patients without a sinus were the propensity-matched control group.
Result:
The success rate of controlling reinfection with 1-stage revision TKA with a concomitant sinus was 78.3% with a mean follow-up of 4.8 years. The most common intraoperatively isolated organisms in patients with a sinus tract were coagulase-negative Staphylococcus in 28 patients (40.6%), Staphylococcus aureus in 12 patients (17.2%), and polymicrobial infection in 14 patients (20.3%). A sinus tract in line with the surgical wound was associated with a higher risk of reoperation than a sinus tract away from the wound.
Conclusion:
Our retrospective study suggests that 1-stage revision TKA may be a viable treatment option for patients presenting with a sinus tract. A sinus in line with the former incision was associated with a higher rate of revision. Surgeons should take into consideration this risk for revision before performing a 1-stage exchange surgery.
Keywords: sinus tract, periprosthetic joint infection, 1-stage revision, revision total knee arthroplasty, PJI, TKA
Introduction
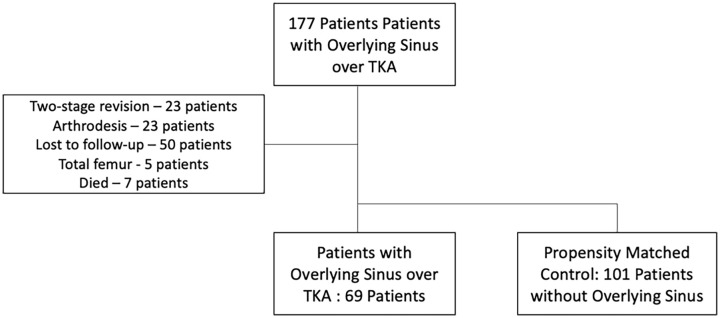
The incidence of periprosthetic joint infection (PJI) in primary and revision total knee arthroplasty (TKA) is increasing along with the rising numbers of TKA being performed [7]. A sinus tract overlying TKA is one of the most challenging revision arthroplasty scenarios (Fig. 1). Managing PJI in patients with TKA and a concomitant sinus tract requires careful consideration of the overlying soft tissues and either 1-stage or 2-stage exchange arthroplasty [6].
Fig. 1.
Picture of a patient with 2 overlying sinuses in the area of the scar.
According to the International Consensus Meeting (ICM) 2018 definition, a sinus tract is an abnormal channel through soft tissue that directly communicates between the joint prosthesis and the outside environment; this can be detected via visualization of the prosthesis through the sinus tract or diagnostic imaging studies such as ultrasound, computed tomography (CT), or magnetic resonance imaging (MRI) [3]. The presence of a sinus tract overlying a prosthetic joint is 1 of the 2 major criteria for diagnosing PJI. This criterion is concordant with the definition for PJI of the European Bone and Joint Infection Society [11] and the Infectious Diseases Society of America [5].
Two-stage revision TKA has long been considered the gold standard for the management of PJI with an overlying sinus tract as this allows debridement of compromised periarticular tissues and convalescence of wounds before proceeding with definitive implantation of the prosthesis [16]. Therefore, the presence of a sinus tract was regarded as a contraindication for 1-stage revision TKA in previous studies [8,10]. At our institution, approximately 85% of all patients with PJI of the hip and knee are managed with 1-stage revision [4].
To perform a 1-stage revision for PJI, a strict protocol is followed. This includes preoperative diagnosis of PJI as per the ICM criteria, identification of the causative organism, systematic and radical intraoperative debridement of the compromised periarticular tissues and use of a cemented prosthesis with antibiotic-loaded bone cement that is sensitive to the isolated organism [1,5]. The presence of a sinus tract is not a contraindication to performing 1-stage revision for PJI at our institution if primary wound closure is possible. The advantages of 1-stage revision for knee PJI include earlier return to function, shorter hospitalization, reduced morbidity, and lower costs associated with avoiding a second operative intervention [4].
The aim of this study was to review outcomes after 1-stage revision TKA for patients with an overlying sinus tract and identify risk factors associated with reoperation or reinfection.
Methods
Institutional review board approval was obtained prior to the commencement of this study. A retrospective review was undertaken of patients who underwent 1-stage revision TKA with an overlying sinus tract between January 2001 and December 2018. The inclusion criteria were patients who presented with a sinus tract overlying TKA and underwent 1-stage revision TKA. This included patients with primary and revision TKA. We excluded patients managed with 2-stage revision TKA for PJI and patients who had total femur replacement and knee arthrodesis. Patients with inadequate documentation or unable to be followed up during the study period were also excluded.
A control group of patients who underwent 1-stage revision TKA for PJI without a sinus tract were selected from our database during same time interval as those patients with a sinus. The groups were matched by age, sex, and date of the surgical procedure. This control group had the same inclusion and exclusion criteria without the presence of a sinus tract overlying the joint.
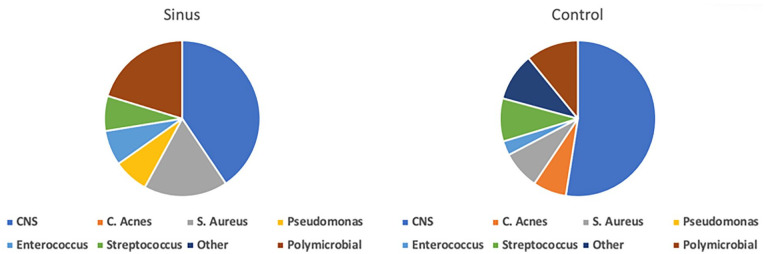
There were 177 patients with a sinus tract overlying TKA during the study period. Fifty-one patients were excluded as they were treated with a different surgical technique (23 with 2-stage exchange, 23 with arthrodesis, 5 with total femur replacement), 50 patients were lost to follow up, and 7 patients had died at the time of data collection. Therefore, 69 patients were included in the sinus cohort. A cohort of 101 patients who underwent 1-stage revision TKA for PJI without a sinus tract in the same time interval was selected as a control group (Fig. 2). The average age of patients in the sinus cohort was 74.3 years, with a mean follow-up period of 58.8 months (0–208). Demographic characteristics of the sinus and control group were comparable (Table 1).
Fig. 2.
Patient selection flow chart.
TKA total knee arthroplasty.
Table 1.
Demographics of study cohort.
| Sinus (n=69) | Control (n=101) | P value | |
|---|---|---|---|
| Age (mean) | 74.3 | 74.7 | .745 |
| Gender (F/M) | 38/31 | 49/52 | .401 |
| Site (left/right) | 34/35 | 45/56 | .544 |
| BMI (kg/m2) | 30.55 ± 5.31 | 29.62 ± 4.08 | .282 |
| Follow-up (months) | 58.8 | 53.2 | .917 |
| Operative Interventions prior to Single-Stage revision for PJI | 1–2 (2.9%) | 1–24 (23.8%) | <.001 |
| 2–5 (7.2%) | 2–11 (10.9%) | ||
| 3–10 (14.5%) | 3–25 (24.8%) | ||
| 4–11 (15.9%) | 4–10 (9.9%) | ||
| ≥5–41 (59.4%) | ≥5–31 (30.7%) | ||
| Operative Interventions for PJI Prior to Single-Stage | 0–12 (17.4%) | 0–41 (30.7%) | .001 |
| 1–18 (26.1%) | 1–28 (10.9%) | ||
| 2–14 (20.3%) | 2–16 (24.8%) | ||
| ≥3–25 (36.2%) | ≥3–15 (9.9%) |
BMI body mass index, PJI periprosthetic joint infection.
Multiple patient-related risk factors were analyzed, including age, sex, body mass index (BMI), history of sepsis, and selected comorbidities (diabetes mellitus, rheumatic disorders, and renal failure). Procedure-related factors were also collated, including the number of interventions prior to the 1-stage revision, number of interventions specifically for the management of PJI, number of sinus tracts, and the location of sinus tract in relation to the surgical wound. Microbial results from preoperative joint aspirate and intraoperative tissues were also obtained.
The follow-up of patients in the study was performed via mailed questionnaires. If the patient did not respond by mail, telephone follow-up was conducted to ascertain whether reoperation was required after the 1-stage revision and if so, the cause of reoperation. The study’s primary endpoints were reinfection, aseptic revision, or wound complications.
All patients had a preoperative aspiration performed at our institution to identify the organism. In addition, multiple intraoperative deep tissues were sent for culture. No microbial swabs were obtained from the sinus tract as this has low correlation to the intra-articular organism [15]. All patients with a sinus tract overlying TKA were classified as infected.
The surgical protocol consisted of complete excision of the old scar and sinus tract if the sinus tract was in-line with the incision. If the sinus was not along the course of the incision, a second incision was made to debride the sinus tract and was closed by sutures at the end of the surgery. A sufficient distance of at least 3 cm between the skin incisions must be maintained to avoid wound necrosis. The sinus tract should be excised down to the joint capsule. All suspicious infected periarticular tissues were excised, including collateral ligaments if necessary. At least 6 microbial and 2 histological tissue samples were taken for culture. The tissue culture results were compared with the preoperative aspiration culture results. All foreign material was removed completely, followed by a radical debridement of the infected joint. Debridement of the posterior capsule was completed after removal of the prosthesis. Subsequently, the surgical site was packed with polyhexanide-soaked gauze sponges, and intravenous antibiotic therapy was commenced based on the preoperative microbial findings. The surgical area was re-draped and a new, sterile set of surgical trays was used.
Antibiotic-loaded bone cement sensitive to the preoperatively identified organism is used to implant a revision prosthesis. A higher constraint implant, such as the cemented Endo-Model hinged knee system (Waldermar Link GmbH & Co) is used after debridement of the compromised periarticular tissues. In cases of severe bone loss, femoral and tibial cones are utilized. One drain is inserted into the joint and removed on the second postoperative day. Intravenous antibiotics are routinely administered for 12 to 14 days, followed by oral antibiotics for at least 2 weeks.
Statistical Analysis
Differences in patient characteristics for continuous variables were initially analyzed using the Shapiro-Wilk test to assess distribution. The comparison of continuous data with Gaussian distribution was performed using a 2-tailed t-test; otherwise, the Mann-Whitney U test was utilized. The distribution of categorical variables was compared using the χ2 test or the Fisher exact test according to the data frequency. Statistical significance was defined as P < .05. The statistical software used was SAS 9.4 for windows. Patients with and without a sinus tract were compared according to aseptic revision, reinfection, and wound healing problems.
Results
There was a significant difference in the rate of patients who required reoperation between the sinus and control cohorts (P = .04). In the sinus cohort, 33 (47.8%) patients did not require reoperation following 1-stage revision. The reasons for reoperation in the sinus cohort included aseptic revision in 12 (17.4%), reinfection in 15 (21.7%), and wound complication in 9 (13%) patients. From the control cohort, 62 (61.4%) patients did not require reoperation after 1-stage revision TKA for PJI. Reasons for reoperation included reinfection in 15 (14.9%), aseptic revision in 21 (20.8%), and wound complications in 3 (3%) patients. None of our patients in the sinus cohort required plastic surgical intervention for soft-tissue coverage (Table 2).
Table 2.
Perioperative profile.
| Sinus (n=69) | Control (n=101) | P value | |
|---|---|---|---|
| Location of sinus | Unknown—10 (14.5%) | Nil–101 | |
| Along incision—24 (34.8%) | |||
| Outside incision—33 (47.8%) | |||
| Both—2 (2.09%) | |||
| Number of sinus tract | Unknown—4 (5.8%) | Nil–101 | |
| 1–47 (68.1%) | |||
| 2–11 (15.9%) | |||
| ≥3–7 (10.1%) | |||
| Positive intraoperative tissue culture | 57 (82.6%) | 76 (75.2%) | .253 |
| Revision after single-stage | 36 (52.2%) | 39 (38.6%) | .08 |
| Reason for revision after single-stage | Aseptic revision—12 (17.4%) | Aseptic revision—21 (20.8%) | .035 |
| Re-infection—15 (21.7%) | Re-infection—15 (14.9%) | ||
| Wound revision—9 (13%) | Wound revision—3 (3%) | ||
| No revision—33 (47.8%) | No revision—62 (61.4%) |
When bivariate analysis was performed with reinfection as an outcome, the number of operations prior to 1-stage revision TKA or the location of the sinus tract did not reach statistical significance as a risk factor for predicting reinfection (Table 3). There was no correlation found between specific germ and reinfection. No case of methicillin-resistant Staphylococcus aureus (MRSA) was included in the study population, but MRSA was not considered as contraindication. Seventeen patients required reoperation for infection in the sinus cohort. Reinfection with the same organism occurred in 2 patients in the study cohort. One patient had a reinfection with Streptococcus pneumoniae, and the other patient with Staphylococcus aureus.
Table 3.
Reinfection after 1-stage revision.
| No reinfection (n=136) | Reinfection (n=34) | P value | |
|---|---|---|---|
| Operative interventions prior to single-stage revision for PJI | 1–21 (15.4%) | 1–5 (14.7%) | .15 |
| 2–16 (11.8%) | 2–0 (0%) | ||
| 3–30 (22.1%) | 3–5 (14.7%) | ||
| 4–16 (11.8%) | 4–5 (14.7%) | ||
| ≥5–53 (39.0%) | ≥5–19 (55.9%) | ||
| Location of sinus | Nil/unknown—94 (69.1%) | Nil/unknown—17 (50%) | .502 |
| Along incision—16 (11.8%) | Along incision—8 (23.5%) | ||
| Outside incision—25 (18.4%) | Outside incision—8 (23.5%) | ||
| Both—1 (0.7%) | Both—1 (2.9%) |
PJI periprosthetic joint infection.
When reoperation following 1-stage revision TKA was considered as an outcome, a sinus tract in line with the surgical wound was associated with a higher risk of reoperation than patients who had the sinus tract away from the wound (P = .047) The number of operations prior to the 1-stage revision did not reach statistical significance as a risk factor for requiring reoperation (P = .51) (Table 4).
Table 4.
Reoperation after 1-stage revision.
| No revision (n=95) | Revision (n=75) | P value | |
|---|---|---|---|
| Operative interventions prior to single-stage revision for PJI | 1–14 (14.7%) | 1–12 (16%) | .501 |
| 2–12 (12.6%) | 2–4 (5.3%) | ||
| 3–19 (20.0%) | 3–16 (21.3%) | ||
| 4–13 (13.7%) | 4–8 (10.7%) | ||
| ≥5–37 (38.9%) | ≥5–35 (46.7%) | ||
| Location of sinus | Nil/unknown—66 (69.5%) | Nil/unknown—45 (60%) | .047 |
| Along incision/both—9 (9.5%) | Along incision/both—17 (22.7%) | ||
| Outside incision—20 (21.1%) | Outside incision—13 (17.3%) |
PJI periprosthetic joint infection.
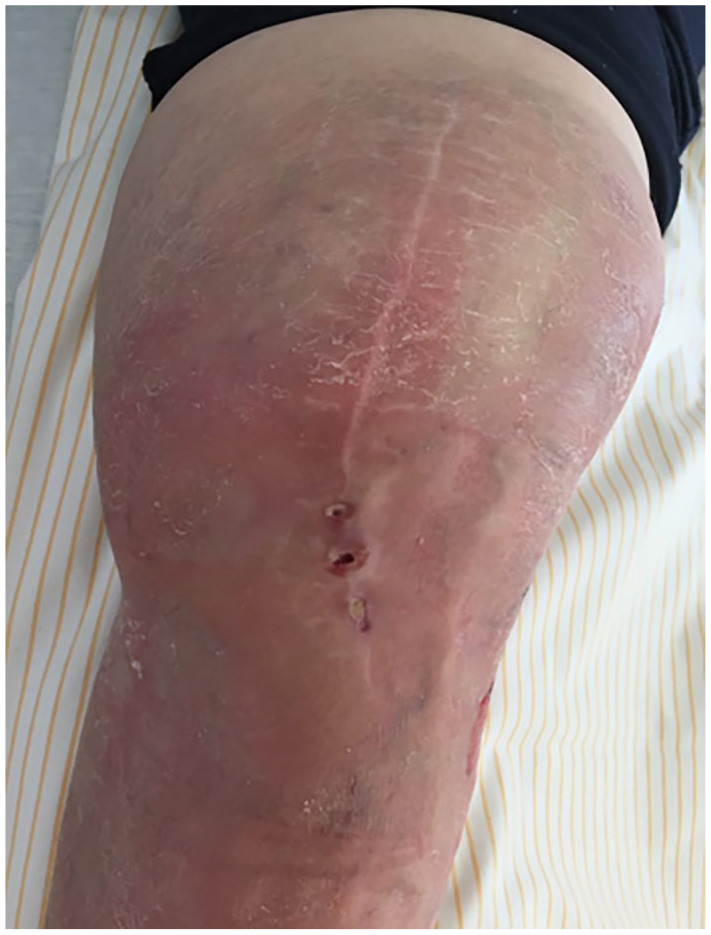
The most common organism isolated from intraoperative tissue samples in patients with a sinus tract was coagulase-negative Staphylococcus in 28 patients (40.6%) and Staphylococcus aureus in 12 patients (17.4%). Polymicrobial infection occurred in 14 (20.3%) in the sinus cohort and 11 patients (10.9%) in the control cohort (Fig. 3) The organism isolated from the tissue culture correlated to the organism isolated from preoperative joint aspirate in 46 (66.7%) patients in the sinus cohort. A positive deep tissue culture with Pseudomonas was significantly associated with presence of a sinus tract (P = .03). The most common germ in the group without a sinus was coagulase-negative Staphylococcus (Fig. 3).
Fig. 3.
Microbial characteristics in the 2 groups.
CNS Coagulase-negative Staphylococcus, C. Acnes Cutibacterium acnes, S. Aureus Staphylococcus aureus.
Discussion
A sinus tract overlying TKA presents a management dilemma, even for an experienced arthroplasty surgeon. Although studies examining the use of 1-stage revision TKA with concomitant sinus tract are lacking in the literature, studies have evaluated the use of 1-stage revision total hip arthroplasty (THA) in patients who presented with a sinus tract overlying THA. The outcomes after 1-stage revision THA with a sinus tract are favorable with reoperation rates of 4.7% to 14% [9,12]. In our study, we found a small but statistically significant increased need for all-cause revision (52% vs 39%) and revision for recurrent sepsis (22% vs 15%) in the cohort with a sinus tract.
The limitations of this study include those inherent to a retrospective design. Since we perform 1-stage revision TKA in most of our patients with PJI, we could not compare, without bias, the results of 1-stage vs 2-stage revision TKA in patients with a sinus tract overlying TKA. Due to the rather small sample size, the results of multivariate analyses are limited. Furthermore, we lost a significant number of patients to follow-up owing to the long study period (beginning in 2001) and the senior age at which patients underwent the operations. Finally, we excluded patients for whom we could not achieve primary wound closure. The proportion of patients who required advanced soft-tissue management was small and managed within a multidisciplinary team.
Razii et al [13] analyzed outcomes after 1-stage revision TKA and included patients with a sinus tract; although they did not quantify the number of patients who had a sinus tract prior to 1-stage revision, they reported a success rate at 5 years of 83.5%. The results from our institution with 1-stage revision TKA without excluding patients with a sinus tract was 93% for 10-year infection-free survival [17]. When we specifically examined patients with a sinus tract overlying TKA, 78.3% of patients from the sinus cohort were successfully managed with 1-stage revision TKA with a mean follow-up of 4.8 years.
Our study suggests that a sinus tract in-line with the surgical incision is associated with a higher risk of reoperation than a sinus tract away from the incision. We recognize that excluding patients who could not have primary wound closure from the cohort is a confounding factor. Nevertheless, this is an unexpected result as the difficulty of the soft-tissue closure would be more significant, and thus the risk of complications is higher if the sinus tract is away from the original surgical wound.
Davis et al [2] demonstrated that patients who present with a sinus tract overlying TKA had 1 or more non-definitive procedures (radiology drain placement, debridement of the infected joint) prior to definitive revision TKA. Our study demonstrated a similar finding where patients undergoing multiple procedures prior to definitive management of PJI were at a higher risk of developing a sinus tract (P = .001). However, our study could not correlate the number of prior procedures to the risk of failure after 1-stage revision TKA.
A draining sinus appears to be a risk factor for polymicrobial PJI, which can increase the risk of amputation, arthrodesis, or death [14]. Tetreault et al [15] reported polymicrobial infection in 11.8% of deep cultures in patients with a sinus tract over hip or knee arthroplasty. This study identified polymicrobial organisms in 20.3% of patients in the sinus group, although this was not a significant risk factor for reoperation. Similar to 2-stage revision TKA, higher risk of failure is reported when 1-stage revision TKA is performed for patients with polymicrobial PJI [13]. In this study, we did not obtain superficial cultures in our sinus cohort as there is poor correlation between superficial culture results to intraoperative tissue cultures, thus potentially complicating antimicrobial treatment [15]. Finally, 66.7% of patients from the sinus cohort had the same organism from intraoperative tissue cultures and preoperative aspirate, but it was not a significant risk factor for reinfection. Antibiotics were modified during the postoperative period, with advice from a multidisciplinary team, in cases where there was a discrepancy between the tissue and aspirate culture results.
In conclusion, this retrospective study suggests that 1-stage revision TKA may be a viable management option in patients with a sinus tract overlying TKA. We found that a sinus tract in line with the surgical incision showed a higher rate of reoperation than a sinus tract away from the wound. This risk for revision should be taken into consideration by surgeons planning a 1-stage septic exchange.
Supplemental Material
Supplemental material, sj-docx-1-hss-10.1177_15563316241228267 for Mid-term Results of 1-stage Revision Total Knee Arthroplasty for Periprosthetic Joint Infection With a Sinus Tract by Christian Lausmann, Anne Wollny, Mustafa Citak, Thorsten Gehrke, Frank Timo Beil, Min-Jae Lee and Niklas Unter Ecker in HSS Journal®
Supplemental material, sj-docx-2-hss-10.1177_15563316241228267 for Mid-term Results of 1-stage Revision Total Knee Arthroplasty for Periprosthetic Joint Infection With a Sinus Tract by Christian Lausmann, Anne Wollny, Mustafa Citak, Thorsten Gehrke, Frank Timo Beil, Min-Jae Lee and Niklas Unter Ecker in HSS Journal®
Supplemental material, sj-docx-3-hss-10.1177_15563316241228267 for Mid-term Results of 1-stage Revision Total Knee Arthroplasty for Periprosthetic Joint Infection With a Sinus Tract by Christian Lausmann, Anne Wollny, Mustafa Citak, Thorsten Gehrke, Frank Timo Beil, Min-Jae Lee and Niklas Unter Ecker in HSS Journal®
Supplemental material, sj-docx-4-hss-10.1177_15563316241228267 for Mid-term Results of 1-stage Revision Total Knee Arthroplasty for Periprosthetic Joint Infection With a Sinus Tract by Christian Lausmann, Anne Wollny, Mustafa Citak, Thorsten Gehrke, Frank Timo Beil, Min-Jae Lee and Niklas Unter Ecker in HSS Journal®
Supplemental material, sj-docx-5-hss-10.1177_15563316241228267 for Mid-term Results of 1-stage Revision Total Knee Arthroplasty for Periprosthetic Joint Infection With a Sinus Tract by Christian Lausmann, Anne Wollny, Mustafa Citak, Thorsten Gehrke, Frank Timo Beil, Min-Jae Lee and Niklas Unter Ecker in HSS Journal®
Supplemental material, sj-docx-6-hss-10.1177_15563316241228267 for Mid-term Results of 1-stage Revision Total Knee Arthroplasty for Periprosthetic Joint Infection With a Sinus Tract by Christian Lausmann, Anne Wollny, Mustafa Citak, Thorsten Gehrke, Frank Timo Beil, Min-Jae Lee and Niklas Unter Ecker in HSS Journal®
Supplemental material, sj-docx-7-hss-10.1177_15563316241228267 for Mid-term Results of 1-stage Revision Total Knee Arthroplasty for Periprosthetic Joint Infection With a Sinus Tract by Christian Lausmann, Anne Wollny, Mustafa Citak, Thorsten Gehrke, Frank Timo Beil, Min-Jae Lee and Niklas Unter Ecker in HSS Journal®
Footnotes
The author(s) declared the following potential conflicts of interest with respect to the research, authorship, and/or publication of this article: MC, MD, PhD, reports a relationship with Waldemar Link GmbH & Co. KG. TG, MD, reports relationships with Waldemar Link GmbH & Co. KG, Zimmer Biomet Inc., Heraeus, and Ceramtec Co. The other authors report no potential conflicts of interest.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Human/Animal Rights: All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2013.
Informed Consent: Informed consent was waived from all patients included in this study.
Level of Evidence: Level III: Retrospective Therapeutic Study
Required Author Forms: Disclosure forms provided by the authors are available with the online version of this article as supplemental material.
ORCID iD: Christian Lausmann  https://orcid.org/0000-0002-8873-8119
https://orcid.org/0000-0002-8873-8119
References
- 1. Citak M, Friedenstab J, Abdelaziz H, et al. Risk factors for failure after 1-stage exchange total knee arthroplasty in the management of periprosthetic joint infection. J Bone Joint Surg Am. 2019;101(12):1061–1069. [DOI] [PubMed] [Google Scholar]
- 2. Davis B, Ford A, Holzmeister AM, Rees HW, Belich PD. Management of periprosthetic hip and knee joint infections with a known sinus tract: a single-center experience. Arthroplast Today. 2021;8:124–127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Elkins JM, Kates S, Lange J, et al. General assembly, diagnosis, definitions: proceedings of international consensus on orthopedic infections. J Arthroplasty. 2019;34(2S):S181–S185. 10.1016/j.arth.2018.09.069. [DOI] [PubMed] [Google Scholar]
- 4. Gehrke T, Zahar A, Kendoff D. 1-stage exchange: it all began here. Bone Joint J. 2013;95-B(11)(suppl A):77–83. [DOI] [PubMed] [Google Scholar]
- 5. International Standardization Organization. ISO 14243-2:2009: implants for surgery—wear of total knee-joint prostheses. 2009. Available at: https://www.iso.org/standard/69851.html. Accessed January 5, 2024.
- 6. Kunutsor SK, Whitehouse MR, Lenguerrand E, Blom AW, Beswick AD. Re-infection outcomes following one- and 2-stage surgical revision of infected knee prosthesis: a systematic review and meta-analysis. PLoS ONE. 2016;11(3):e0151537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Kurtz S, Ong K, Lau E, Mowat F, Halpern M. Projections of primary and revision hip and knee arthroplasty in the United States from 2005 to 2030. J Bone Joint Surg Am. 2007;89(4):780–785. [DOI] [PubMed] [Google Scholar]
- 8. Lichstein P, Gehrke T, Lombardi A, et al. 1-stage versus 2-stage exchange. J Orthop Res. 2014;32(suppl 1):S141–S146. [DOI] [PubMed] [Google Scholar]
- 9. Marmor S, Kerroumi Y, Meyssonnier V, et al. 1-stage exchange arthroplasty for fistulizing periprosthetic joint infection of the hip: an effective strategy. Front Med (Lausanne). 2020;7:540929. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Matar HE, Bloch BV, Snape SE, James PJ. Outcomes of single- and 2-stage revision total knee arthroplasty for chronic periprosthetic joint infection: long-term outcomes of changing clinical practice in a specialist centre. Bone Joint J. 2021;103-B(8):1373–1379. [DOI] [PubMed] [Google Scholar]
- 11. McNally M, Sousa R, Wouthuyzen -Bakker M, et al. The EBJIS definition of periprosthetic joint infection. Bone Joint J. 2021;103-B(1):18–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Raut VV, Siney PD, Wroblewski BM. 1-stage revision of infected total hip replacements with discharging sinuses. J Bone Joint Surg Br. 1994;76(5):721–724. [PubMed] [Google Scholar]
- 13. Razii N, Clutton JM, Kakar R, Morgan-Jones R. Single-stage revision for the infected total knee arthroplasty: the Cardiff experience. Bone Jt Open. 2021;2(5):305–313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Tan TL, Kheir MM, Tan DD, Parvizi J. Polymicrobial periprosthetic joint infections: outcome of treatment and identification of risk factors. J Bone Joint Surg Am. 2016;98(24):2082–2088. [DOI] [PubMed] [Google Scholar]
- 15. Tetreault MW, Wetters NG, Aggarwal VK, et al. Should draining wounds and sinuses associated with hip and knee arthroplasties be cultured? J Arthroplasty. 2013;28(8 suppl):133–136. [DOI] [PubMed] [Google Scholar]
- 16. Tözün IR, Ozden VE, Dikmen G, Karaytuğ K. Trends in the treatment of infected knee arthroplasty. EFORT Open Rev. 2020;5(10):672–683. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Zahar A, Kendoff DO, Klatte TO, Gehrke TA. Can good infection control be obtained in 1-stage exchange of the infected TKA to a rotating hinge design? 10-year results. Clin Orthop Relat Res. 2016;474(1):81–87. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-docx-1-hss-10.1177_15563316241228267 for Mid-term Results of 1-stage Revision Total Knee Arthroplasty for Periprosthetic Joint Infection With a Sinus Tract by Christian Lausmann, Anne Wollny, Mustafa Citak, Thorsten Gehrke, Frank Timo Beil, Min-Jae Lee and Niklas Unter Ecker in HSS Journal®
Supplemental material, sj-docx-2-hss-10.1177_15563316241228267 for Mid-term Results of 1-stage Revision Total Knee Arthroplasty for Periprosthetic Joint Infection With a Sinus Tract by Christian Lausmann, Anne Wollny, Mustafa Citak, Thorsten Gehrke, Frank Timo Beil, Min-Jae Lee and Niklas Unter Ecker in HSS Journal®
Supplemental material, sj-docx-3-hss-10.1177_15563316241228267 for Mid-term Results of 1-stage Revision Total Knee Arthroplasty for Periprosthetic Joint Infection With a Sinus Tract by Christian Lausmann, Anne Wollny, Mustafa Citak, Thorsten Gehrke, Frank Timo Beil, Min-Jae Lee and Niklas Unter Ecker in HSS Journal®
Supplemental material, sj-docx-4-hss-10.1177_15563316241228267 for Mid-term Results of 1-stage Revision Total Knee Arthroplasty for Periprosthetic Joint Infection With a Sinus Tract by Christian Lausmann, Anne Wollny, Mustafa Citak, Thorsten Gehrke, Frank Timo Beil, Min-Jae Lee and Niklas Unter Ecker in HSS Journal®
Supplemental material, sj-docx-5-hss-10.1177_15563316241228267 for Mid-term Results of 1-stage Revision Total Knee Arthroplasty for Periprosthetic Joint Infection With a Sinus Tract by Christian Lausmann, Anne Wollny, Mustafa Citak, Thorsten Gehrke, Frank Timo Beil, Min-Jae Lee and Niklas Unter Ecker in HSS Journal®
Supplemental material, sj-docx-6-hss-10.1177_15563316241228267 for Mid-term Results of 1-stage Revision Total Knee Arthroplasty for Periprosthetic Joint Infection With a Sinus Tract by Christian Lausmann, Anne Wollny, Mustafa Citak, Thorsten Gehrke, Frank Timo Beil, Min-Jae Lee and Niklas Unter Ecker in HSS Journal®
Supplemental material, sj-docx-7-hss-10.1177_15563316241228267 for Mid-term Results of 1-stage Revision Total Knee Arthroplasty for Periprosthetic Joint Infection With a Sinus Tract by Christian Lausmann, Anne Wollny, Mustafa Citak, Thorsten Gehrke, Frank Timo Beil, Min-Jae Lee and Niklas Unter Ecker in HSS Journal®