Abstract
Background:
Worldwide, common mental disorders (CMDs) (depression, anxiety, somatoform disorders) have a high prevalence in the community. About one-third of them experience disability. As the Indian Disability Evaluation and Assessment Scale (IDEAS) was originally designed by the Indian Psychiatric Society to assess disability in severe mental illnesses, it has not been widely used among CMDs. Our objective was to compare and establish a correlation between the level of disability obtained using IDEAS and the Sheehan Disability Scale (SDS) in CMDs.
Methods:
A cross-sectional assessment of disability was performed among 220 consenting patients with CMDs. Disability scores of IDEAS and SDS were compared and correlated across the three varieties of CMDs.
Results:
Age, gender, education, socioeconomic class, duration of illness, and duration of treatment exhibited significant differences among the three CMD groups. Both IDEAS and SDS show a milder level of disability; they did not differ significantly in their scores across CMDs. A strong correlation was seen between SDS and IDEAS across most domains.
Conclusion:
The study revealed strong concurrent validity between the two scales, thus advocating that indigenously designed IDEAS can convincingly assess disability across the CMDs among the Indian population.
Keywords: IDEAS, SDS, correlation, concurrent validity, common mental disorders
Key Messages:
This study highlights the utility of indigenously designed IDEAS in disability assessment of CMDs. This opens up the possibility of the government providing disability benefits for CMDs as well, as is the case in some countries.
Common mental disorders (CMDs) comprise anxiety, nonpsychotic affective, and somatoform disorders and are highly prevalent in the community. Both the National Mental Health Survey (NMHS 2016) of India and the Indian statistics of the World Mental Health Survey reported a CMD prevalence of >5%.1,2 Among the CMDs identified in the NMHS, 37% reported disability in social and family life, and 39% reported disability in work life, as assessed by the Sheehan Disability Scale (SDS). 3 Approximately 50% of these individuals experienced at least a moderate level of disability, indicating a substantial burden. 2 SDS is a globally recognized patient-rated scale that assesses disability in three spheres (work, social life, family life), each scored from 0 to 10 points (0 = no disability, 1–3 = mild disability, 4–6 = moderate disability, 7–9 = marked disability, 10 = extreme disability), with a score of 5 or more in each sphere indicating significant disability. SDS demonstrates reliability and validity in both CMDs and major mental disorders and has versions for both adults and children. 4
Indian Disability Evaluation and Assessment Scale (IDEAS) is an indigenously developed disability assessment tool created in the year 2002 by the Rehabilitation Committee of the Indian Psychiatric Society. 5 It stands as a significant contribution to clinical assessment and disability research in India. The IDEAS measures the disability across the domains of “Self-care,” “Interpersonal Activities,” “Communication and Understanding,” and “Work.” Each domain is scored on a scale of 0–4, with zero indicating “No disability,” one for mild disability, two for moderate, three for severe, and four for “Profound disability.” The scale also scores for the duration of illness (DoI). The Global Disability Score is the total of the four areas mentioned above, plus the DoI score. A global disability score of 40% (8/20) or higher qualifies an individual with mental illness for benefits as per the Rights of Persons with Disabilities Act. 5 While IDEAS has seen limited use in research projects assessing disability related to various psychiatric disorders, 6 it is routinely used in the clinical assessment of major psychiatric disorders like schizophrenia and bipolar disorder, facilitating access to state-sponsored disability benefits. IDEAS is commonly used in severe mental disorders, although it has no defined contraindications for assessing CMDs. On the other hand, SDS was originally designed to assess functional impairment in anxiety disorders. 7 Studies demonstrate its excellent reliability and internal consistency (α = 0.89), sensitivity, and specificity in various psychiatric disorders. With regard to validity, patients who met the criteria for a mental disorder tend to exhibit impairment of a higher degree than those who do not. 8 Given that SDS serves as a gold standard tool for disability assessment, our study aimed to investigate whether IDEAS and SDS could be used interchangeably for assessing disability in CMDs. We compared disability across CMDs using both SDS and IDEAS and examined the concurrent validity of the disability scores from both scales in CMDs. This study is a secondary analysis of data from a larger project focusing on the cost of illness 9 and work productivity 10 related to CMDs.
Materials and Methods
This was a cross-sectional, observational study conducted from April 2018 to January 2019 at a tertiary psychiatric hospital in South India. The study received approval from the institutional ethics committee. Patients diagnosed with one of the three CMDs, visiting the follow-up outpatient unit of the department of psychiatry, were enrolled through purposive sampling after obtaining written informed consent.
Assuming a frequency (P) of 25% for CMDs in the hospital-based population with ±10% confidence limits and a design effect of 1.5, the required sample size at a 95% confidence interval was 110 patients diagnosed with CMDs. However, we recruited 220 study subjects in total, comprising depressive disorder (n = 110), anxiety disorders (n = 58), and somatoform disorders (n = 52). Subjects in the age group of 18–65 years, with a diagnosis of depressive disorder/anxiety disorders/somatoform disorders, as per International Classification of Diseases, Tenth Revision (ICD-10), 11 diagnosed prior by the treating consultant psychiatrist, were enrolled. Severe depression with or without psychotic symptoms or those requiring inpatient care, having other psychiatric co-morbidities or uncontrolled medical disorders, and dependence on drugs except for nicotine dependence were excluded.
We completed all assessments of every patient on the same day. Sociodemographic data were collected using a semi-structured proforma designed specifically for the study. The diagnosis of CMD was confirmed using Mini International Psychiatric Interview Plus version 5.0.0 (MINI Plus 5.0.0), a tool for structured diagnostic psychiatric interviews for research purposes, requiring formal training. 12 The severity of illness was assessed using the Clinical Global Impression-Severity (CGI-S), 13 a clinician-administered tool widely used in psychiatric research to rate illness severity. Disability was assessed using both the SDS 3 and IDEAS. 5 The first author (MBK), proficient in the local language, administered all scales to all study subjects in the vernacular.
Data were analyzed using IBM SPSS Statistics for Windows Version 23. We used Pearson’s chi-square test (or Fisher–Freeman–Halton exact test) and the Kruskal–Wallis test (with post hoc Mann–Whitney U test) to compare the demographic and clinical variables among the three groups of CMDs for discrete and sequential variables, respectively. Disability across the three groups was compared using analysis of variance (ANOVA) with post hoc Tukey Honestly Significant Difference (HSD) to identify significant differences in domains. Pearson’s correlation coefficient test was used to analyze the correlation across the domains of SDS and IDEAS. As age and DoI were different across the three groups, we carried out partial correlation to control these two variables. P values under 0.05 were considered significant.
Results
Our sample size was 220, comprising depression (n = 110), anxiety disorders (n = 58), and somatoform disorders (n = 52). We have presented the sociodemographic and clinical characteristics of the total study sample (n = 220), as well as the different diagnostic subgroups in Table 1. Significant differences were observed in age, gender, education, socioeconomic status, DoI, and duration of treatment. The post hoc analysis showed that patients with somatoform disorder and depression had a significantly longer DoI as well as treatment compared to anxiety disorders. Also, concerning age and gender ratio differences, it was somatoform disorders > depression > anxiety disorders.
Table 1.
Sociodemographic and Select Clinical Variables of the Study Population.
| Variables | Total N = 220 |
Depressive disorder n = 110 |
Anxiety disorder n = 58 |
Somatoform disorder n = 52 |
p-Value |
| Age, M (SD)a | 41.4 (10.2) | 41.6 (9.7) | 36.5 (8.8) | 46.4 (10.4) | <0.001*b |
| Gender, n (%)† Male Female |
82 (37.3) 138 (62.7) |
36 (32.7) 74 (67.3) |
30 (51.7) 28 (48.3) |
16 (30.8) 36 (69.2) |
0.029* |
| Education, n (%)‡ Illiterate Primary High school College Undergraduate Postgraduate |
65 (29.5) 48 (21.8) 51 (23.2) 14 (6.4) 35 (15.9) 7 (3.2) |
33 (30) 27 (24.5) 21 (19.1) 6 (5.5) 19 (17.3) 4 (3.6) |
6 (10.3) 9 (15.5) 21 (36.2) 5 (8.6) 15 (25.9) 2 (3.4) |
26 (50) 12 (23.1) 9 (17.3) 3 (5.8) 1 (1.9) 1 (1.9) |
<0.001* |
| Occupation, n (%)# Unemployed Un/semiskilled Skilled Business Clerical Professional |
4 (1.8) 100 (45.5) 73 (33.2) 15 (6.8) 19 (8.6) 9 (4.1) |
3 (2.7) 51 (46.4) 33 (30) 9 (8.2) 8 (7.3) 6 (5.5) |
0 19 (32.8) 23 (39.7) 4 (6.9) 9 (15.5) 3 (5.2) |
1 (1.9) 30 (57.7) 17 (32.7) 2 (3.8) 2 (3.8) 0 |
0.13 |
| Marital status, n (%)# Single Married Divorced/Separated Widow/Widower |
20 (9.1) 166 (75.5) 6 (2.7) 28 (12.7) |
7 (6.4) 84 (76.4) 5 (4.5) 14 (12.7) |
11 (19) 41 (70.7) 0 6 (10.3) |
2 (3.8) 41 (78.8) 1 (1.9) 8 (15.4) |
0.078 |
| Family type, n (%)† Nuclear Joint |
148 (67.6) 71 (32.4) |
76 (69.1) 34 (30.9) |
43 (74.1) 15 (25.9) |
29 (56.9) 22 (43.1) |
0.14 |
| SES, n (%)† Lower Lower middle Middle and upper |
154 (70) 30 (13.6) 36 (16.4) |
76 (69.1) 15 (13.6) 19 (17.3) |
33 (56.9) 12 (20.7) 13 (22.4) |
45 (86.5) 3 (5.8) 4 (7.7) |
0.02* |
| Duration of illness (in years), M (SD)a | 6.27 (6.39) | 6.63 (6.52) | 4.64 (5.68) | 7.52 (6.67) | 0.009*c |
| Duration of treatment (in years), M (SD)a | 4.07 (5.39) | 4.69 (6.14) | 2.88 (4.99) | 4.27 (3.95) | 0.028*c |
| CGI-S | 3.19 (1.01) | 3.12 (1.08) | 3.35 (0.97) | 3.15 (0.89) | 0.42 |
*p <0.05 (2-tailed); †Pearson’s chi–square test; ‡Likelihood ratio; #Fisher–Freeman–Halton exact test; aKruskal–Wallis test; bPost hoc Mann–Whitney test (Somatoform>Depression>Anxiety); cPost hoc Mann–Whitney test (Somatoform = Depression>Anxiety); CGI-S: Clinical Global Impression-Severity scale; SD, standard deviation.
The mean score on CGI-S for all CMDs was 3, as shown in Table 1. This indicates a mild level of severity for all CMD types. The mean scores on both the IDEAS and SDS also suggest a mild level of disability across all CMDs. Table 2 is a descriptive comparison of disability scores across all domains of SDS and IDEAS. Table 3 shows the disability across the three CMDs on SDS and IDEAS. A significant difference was observed in the domain of DoI on IDEAS. Scores are significantly higher in depression and somatoform disorders compared to anxiety disorders, with no difference between depression and somatoform disorders. A similar trend was seen in the domain of “communication and understanding” of IDEAS.
Table 2.
Scores Across the Domains of IDEAS and SDS (N = 220).
| Domains | Mean (SD) | Median (IQR) | |
| IDEAS | Self-care | 0.77 (0.69) | 1 (1) |
| Interpersonal activities | 1.41 (0.82) | 1 (1) | |
| Communication and understanding | 1.14 (0.73) | 1 (1) | |
| Work | 1.87 (0.96) | 2 (1) | |
| Duration of illness | 2.40 (1.17) | 2 (3) | |
| IDEAS global score | 7.60 (2.92) | 8 (5) | |
| SDS | Work/School | 4.35 (2.49) | 4 (4) |
| Social life | 3.02 (1.982) | 3 (2) | |
| Family life | 2.61 (0.14) | 2 (3) | |
| SDS total | 9.98 (5.57) | 10 (7) |
IDEAS—Indian Disability Evaluation and Assessment Scale; IQR, interquartile range; SDS—Sheehan Disability Scale; SD, standard deviation.
Table 3.
Comparison of Disability Scores Across the Domains of IDEAS and SDS.
| Domains | Depression n = 110 |
Anxiety disorders n = 58 |
Somatoform disorders n = 52 |
F (df = 2,217) |
p-Value | |
| IDEAS | Self-care | 0.81 (0.72) | 0.74 (0.71) | 0.71 (0.57) | 0.41 | 0.661 |
| Interpersonal activities | 1.42 (0.89) | 1.48 (0.80) | 1.27 (0.68) | 0.97 | 0.380 | |
| Communication & understanding | 1.12 (0.71) | 1.29 (0.81) | 0.96 (0.65) | 2.85 | 0.060 | |
| Work | 1.82 (1.02) | 1.89 (0.90) | 1.94 (0.89) | 0.33 | 0.717 | |
| Duration of illness† | 2.47 (1.21) | 1.98 (1.05) | 2.73 (1.10) | 6.19 | 0.002* | |
| IDEAS Global | 7.62 (3.23) | 7.36 (2.94) | 7.62 (2.18) | 0.16 | 0.852 | |
| SDS | Work/School | 4.34 (2.69) | 4.28 (2.26) | 4.33 (2.37) | 0.01 | 0.988 |
| Social life | 3.06 (2.09) | 3.31 (2.03) | 2.50 (1.59) | 2.45 | 0.089 | |
| Family life | 2.78 (2.30) | 2.52 (1.90) | 2.23 (1.91) | 1.23 | 0.293 | |
| SDS total | 10.15 (6.16) | 10.10 (5.03) | 9.06 (5.00) | 0.72 | 0.486 |
ANOVA *p < 0.05 (2-tailed); †Post Hoc Tukey’s Honestly Significant Difference shows scores among depression and somatoform disorder higher than anxiety disorders.
IDEAS—Indian Disability Evaluation and Assessment Scale; SDS—Sheehan Disability Scale.
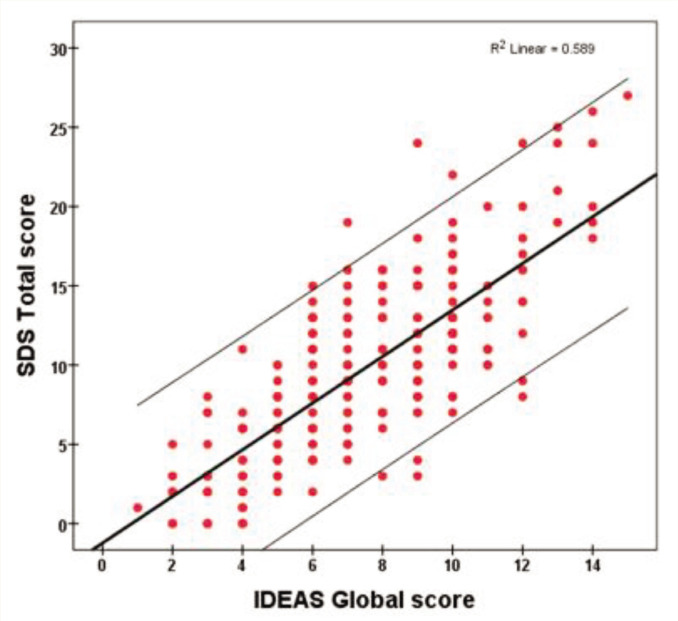
Table 4 shows the correlation scores across the two rating scales. There was a large correlation between SDS and IDEAS in almost all domains. The DoI of IDEAS is the only domain that does not correlate with any of the items on SDS. Most of the correlation values are > 0.5, indicating a strong correlation between the two rating scales. This linear relationship for total scores on both scales is also pictorially represented in the scatterplot (Figure 1). Partial correlation controlling for age and DoI showed that the correlation coefficient remained similarly significant.
Table 4.
Pearson’s Correlation (r) Between Scores Across the Domains of IDEAS and SDS (N = 220).
| SDS | |||||
| Work/ School | Social life | Family life | Total score | ||
| IDEAS | Self-care | 0.53* | 0.57* | 0.51* | 0.63* |
| Interpersonal activities | 0.54* | 0.72* | 0.62* | 0.73* | |
| Communication & understanding | 0.55* | 0.58* | 0.47* | 0.63* | |
| Work | 0.88* | 0.49* | 0.45* | 0.74* | |
| Duration of illness | 0.13 | –0.06 | –0.02 | 0.03 | |
| Global score | 0.76* | 0.62* | 0.55* | 0.77* | |
*p <0.05 (2-tailed).
IDEAS—Indian Disability Evaluation and Assessment Scale; SDS—Sheehan Disability Scale.
Figure 1. Scatterplot Showing a Positive Correlation Between IDEAS Global Score and SDS Total Score (N = 220).
IDEAS—Indian Disability Evaluation and Assessment Scale; SDS—Sheehan Disability Scale.
Discussion
We compared the disability in CMDs, including depression, anxiety disorders, and somatoform disorders, using the scores obtained from SDS and IDEAS. Our findings revealed that none of the domains of SDS differed significantly across the various CMDs. However, on IDEAS, the DoI score was significantly greater in the subgroup of depression and somatoform disorder as compared to anxiety disorder, with a similar trend in the domain of “communication & understanding.” Further, though the mean DoI was fairly longer in all three study groups, as the psychopathology was mild, disability scores also remained low on both SDS and IDEAS. Though the empirical evidence on the course of somatoform disorders is not consistent, a segment of these disorders is said to run a chronic course. 14 As DoI is not a domain in SDS, the possibility of differing significantly if it was an item in SDS can be speculated. However, as far as the areas of functioning are concerned, as per both the tools, the disability across different CMDs is relatively similar.
Upon extensive search, we did not come across other studies that comprehensively assessed and compared disability in CMDs using IDEAS. Notably, epidemiological studies on mental disability employing IDEAS at the community level in India are also scarce, despite it being field-tested in several centers all over the country and gazetted by the Ministry of Human Resources and Empowerment of the Government of India as the endorsed tool to measure psychiatric disability. 15 To provide context, two epidemiological surveys in the general population, conducted in South India approximately a decade apart (in 2008 and 2018) using IDEAS, revealed disability prevalence rates of 2.3 and 7.1%, respectively.6,16 Additionally, there have been numerous studies assessing disability with IDEAS in schizophrenia. These studies typically compared schizophrenia patients, both treated and untreated, with other disorders such as bipolar disorder, alcohol use disorders, obsessive compulsive disorder (OCD), and depression, among others. Understandably, patients with schizophrenia, especially those not receiving treatment, consistently exhibited higher levels of disability. 17 However, in the context of CMDs alone, as mentioned earlier, the utilization of IDEAS has been relatively inconspicuous. Even the NMHS of 2016 18 preferred to administer SDS instead of IDEAS. On the other hand, SDS, as mentioned earlier, has been used extensively and validated for assessing disability in various mental disorders, including CMDs, worldwide. 19 Although we did not find a similar study to ours, our research indicates that disability scores on both SDS and IDEAS across the three CMDs do not significantly differ, except for the DoI scores on IDEAS, as discussed earlier. Furthermore, both scales rated the level of disability as “mild” across all CMDs. This might be because the recruited patients were under treatment for a long time and were in the process of recovery. However, the more important observation here is that the level of severity assessed on IDEAS was not different from that of SDS.
We further examined the correlation between the disability scores measured by IDEAS and SDS. Our results showed a large degree of correlation (r>0.5) between these two instruments. Notably, items with similar functions exhibited a high degree of variance. For example, the variance explained for the “work” domain between the scales was 77%. Similarly, the variance for the “global score” on both scales was 60%, which shows a linear relationship in scores between the two scales. Only the DoI scores are poorly correlated with all the domains of SDS, which is understandable because SDS does not include DoI as a component of disability.
While we did not come across any studies correlating IDEAS with other validated disability scales in CMDs, there was an Indian study that compared the concurrent validity of IDEAS with the Social and Occupational Functioning Scale (SOFS) in patients with schizophrenia. 20 In that study, all IDEAS component scores, including the global score, correlated significantly with the three domains and the total score of SOFS, indicating good concurrent validity with SOFS in patients with residual schizophrenia. Nevertheless, our study is unique in that it comprehensively assessed disability in three CMDs, suggesting that IDEAS could potentially replace the well-validated SDS for assessing disability in CMDs within the Indian population.
Nonetheless, there are some limitations to our study. While we recruited a statistically calculated adequate sample size, it was not evenly distributed across the three CMDs, with depression representing 50% of our study sample. Additionally, we lacked a control group from the general population to compare disability in CMDs against normative data. We also did not quantify the psychopathology of CMDs using suitable rating scales, except for the CGI-S scale. Incorporating psychopathology measurements would have allowed us to explore the correlation between psychopathology and disability. Lastly, a longitudinal study assessing disability at the onset of illness and tracking it over the recovery period would offer a different perspective on the course of disability over time. Nevertheless, this study is one of its kind in demonstrating the utility of IDEAS in assessing disability in CMDs.
Conclusions
In conclusion, our study suggests that IDEAS, the disability assessment tool developed by the Indian Psychiatric Society, is comparable to SDS in assessing the severity of disability in CMDs. We have observed a substantial correlation between these two scales in the assessment of disability in CMDs. Therefore, we propose that these two scales can be used interchangeably for disability assessment in CMDs within the Indian population. We also suggest replication of this study in other populations, overcoming the limitations we have pointed out.
Acknowledgments
Nil.
Footnotes
The authors declared no potential conflicts of interest with respect to the research, authorship and/or publication of this article.
Funding: The authors received no financial support for the research, authorship and/or publication of this article.
The manuscript has been presented for the prestigious Marfatia award during the ANCIPS 2024 at Kochi.
Ethical Approval: Ethical approval was taken from Institutional Ethics Committee Approval No NO.NIMH/DO/IEC (BEH.Sc.DIV)/2017 dtd 31.07.2017
Informed Consent: Written informed consent has been obtained from all the study subjects before enrolling them into the study.
Use of Generative Artificial Intelligence (AI): We, the authors, assume full responsibility for the entire content of the manuscript. We did not use any AI tool in any section of the manuscript.
References
- 1.Sagar R, Pattanayak RD, Chandrasekaran R, et al. Twelve-month prevalence and treatment gap for common mental disorders: Findings from a large-scale epidemiological survey in India. Indian J Psychiatry, 2017; 59: 46–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Jayasankar P, Manjunatha N, Rao GN, et al. Epidemiology of common mental disorders: Results from “National Mental Health Survey” of India, 2016. Indian J Psychiatry, 2022; 64: 13–19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Sheehan DV. Handbook of psychiatric measures. Washington, DC: American Psychiatric Press, 2000, pp. 113–115. [Google Scholar]
- 4.Hodgins DC. Reliability and validity of the Sheehan Disability Scale modified for pathological gambling. BMC Psychiatry, 2013; 13: 177. DOI: 10.1186/1471-244X-13-177 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.The Rehabilitation Committee of the Indian Psychiatric Society. IDEAS (Indian Disability Evaluation and Assessment Scale) - A scale for measuring and quantifying disability in mental disorders. Gurgaon: Indian Psychiatric Society, 2002. [Google Scholar]
- 6.Kumar SG, Premarajan KC, Kattimani S, et al. Epidemiology of mental disability using Indian Disability Evaluation Assessment Scale among general population in an urban area of Puducherry, India. J Postgrad Med, 2018; 64: 16–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Sheehan DV. The anxiety disease. New York: Charles Scribner and Sons, 1983. [Google Scholar]
- 8.Leon AC, Olfson M, Portera L, et al. Assessing psychiatric impairment in primary care with the Sheehan Disability Scale. Int J Psychiatry Med, 1997; 27: 93–105. [DOI] [PubMed] [Google Scholar]
- 9.Kondapura MB, Manjunatha N, Nagaraj AKM, Praharaj SK, Kumar CN. et al. Cost of illness analysis of common mental disorders: a study from an Indian academic tertiary care hospital. Indian J Psychol Med 2023; 45: 519–525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kondapura MB, Manjunatha N, Nagaraj AKM, Praharaj SK, Kumar CN. et al. Work productivity (absenteeism and presenteeism) in persons with common mental disorders: An observational study from South India. Indian J Psychiatry 2023; 65: 412–418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.World Health Organization. The ICD 10 Classification of Mental and Behavioural Disorders. Geneva: World Health Organization, 1992. [Google Scholar]
- 12.Sheehan DV, Lecrubier Y, Sheehan KH, et al. The Mini-International Neuropsychiatric Interview (M. I. N. I.): The development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. J Clin Psychiatry, 1998; 59: 22–33. [PubMed] [Google Scholar]
- 13.Sheehan DV, Harnett‑Sheehan K and Raj BA. The measurement of disability. Int Clin Psychopharmacol, 1996; 11: 89–95. [DOI] [PubMed] [Google Scholar]
- 14.olde Hartman TC, Borghuis MS, Lucassan PLBJ, et al. Medically unexplained symptoms, somatisation disorder and hypochondriasis: course and prognosis, A systematic review. J Psychosom Res, 2009; 66: 363–377. [DOI] [PubMed] [Google Scholar]
- 15.Thara R. Measurement of psychiatric disability. Indian J Med Res, 2005; 121: 723–724. [PubMed] [Google Scholar]
- 16.Kumar SG, Das A, Bhandary PV, et al. Prevalence and pattern of mental disability using Indian disability evaluation assessment scale in a rural community of Karnataka. Indian J Psychiatry, 2008; 50: 21–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Chandrashekar H, Naveen Kumar C, Prashanth NR, et al. Disabilities research in India. Indian J Psychiatry, 2010; 52: 281–285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Gururaj G, Varghese M, Benegal V, et al. National Mental Health Survey of India, 2015–16: Prevalence, patterns and outcomes. Bengaluru, National Institute of Mental Health and Neuro Sciences, NIMHANS Publication No. 129, 2016. [Google Scholar]
- 19.Sheehan DV. The Sheehan Disability Scales. In The Anxiety Disease and How to Overcome It. New York: Charles Scribner and Sons, 1983, p; 151. [Google Scholar]
- 20.Sahoo S, Grover S, Dua D, et al. Concurrent validity of Indian Disability Evaluation and Assessment Scale with socio-occupational functioning scale in patients with schizophrenia. Indian J Psychiatry, 2017; 59: 106–110. [DOI] [PMC free article] [PubMed] [Google Scholar]