Abstract
Objective
Midfoot osteotomy combined with Ilizarov methods of correction is a rarely reported treatment that is particularly well‐suited for severe rigid pes cavus. The study aimed to assess the radiological and clinical results of patients who had been treated for rigid pes cavus using this method.
Methods
The study retrospectively analyzed the clinical and radiological data of 15 pes cavus in 12 patients who were corrected by midfoot osteotomy with Ilizarov external frame in our department from March 2020 to September 2022. Radiologic outcomes were measured using the Meary angle (MA), talus‐first metatarsal angle (TM1A), calcaneal varus angle (CVA) and foot length with weight‐bearing radiographs. Functional assessments were evaluated in terms of pain, function, and quality of life by using the visual analogue scale (VAS), the American Orthopedic Foot and Ankle Society hindfoot scale score (AOFAS), and 36‐item Short Form Health Survey (SF‐36). Additionally, the postoperative satisfaction of patients was investigated by a questionnaire. The clinical and radiological results were evaluated by a paired t‐test.
Results
All patients received plantigrade feet and pain relief. The mean follow‐up was 33.1 ± 5.0 months (range from 25 to 41 months). The etiology included poliomyelitis (4), idiopathic (3), trauma (2), spina bifida (2) and tethered cord syndrome (1). The duration of gradual correction was 30.4 ± 10.6 days, and the external fixation time was 116.3 ± 33.3 days. The bony union rate was 100%. The VAS, AOFAS, and SF‐36 scores significantly improved (p < 0.05). The MA, TM1A, and CVA were close to or reached the normal range postoperative (p < 0.01). The length of each foot was well preserved, which was increased more than 0.8 cm than preoperative. No major complications were reported except two cases of mildly hindfoot varus deformity. The results of the questionnaire showed that patients' satisfaction was 92% (11/12).
Conclusion
Midfoot osteotomy combined with Ilizarov external frame proved to be a reasonable procedure with satisfying mid‐term results for the gradual correction of rigid pes cavus.
Keywords: Ilizarov external frame, midfoot osteotomy, pes cavus, tendon transfer
Midfoot osteotomy combined with Ilizarov distraction is a preferable procedure with satisfying results for the correction of rigid pes cavus with the apex at the midfoot.
Introduction
Pes cavus is a common foot deformity, which was first described by Shaffer in 1885. The main clinical manifestations of pes cavus include the abnormal elevation of medial longitudinal arch, imbalance of the “tripod effect,” reduction of plantar weight‐bearing area and gait disturbances. 1 Severe rigid pes cavus deformity is a challenging problem for orthopedic surgeons. 2 , 3
The etiology remains elusive, which includes genetic, vascular, and trauma factors. 4 The pathogenesis of pes cavus is the imbalance involving both intrinsic and extrinsic muscles of the foot, all of which have been widely recognized. 5
Surgical correction is often required for severe rigid pes cavus, with the goal of obtaining a functional, normal looking, pain‐free, and plantigrade foot. 6 When the apex of pes cavus located in the talon avicular or cuneonavicular joint, midfoot osteotomy may be preferred. 7 Midfoot osteotomy allows for 3D correction of deformities, lowering the medial column and raising the lateral column while correcting the rotation of the forefoot. 8 Among them, the Cole midfoot osteotomy has been widely used in recent years. 9 , 10 Nonetheless, foot shortening and joint sacrifice are two major complications of Coleosteotomy. 11
The Ilizarov method is considered to be a mini‐invasive surgery for rigid pes cavus, which allows for multiplanar correction without bone resection or foot shortening. 12 , 13 , 14 Meanwhile, soft tissue viability can be assessed directly, and the rate of correction can be adjusted accordingly. 15 However, only using the Ilizarov technique, without soft tissue and bone correction, the correction process is painful, the external fixation time is long, and it is easy to relapse. 16 , 17
The combination of the Ilizarov method and midfoot osteotomy may offer more predictable satisfactory results for rigid pes cavus correction to avoid the complications mentioned above. 18 , 19 If limb deformity and foot deformity are present at the same time, this method can exert better correction effect. 20 However, the frame setting of the Ilizarov device is challenging, which involves a great number of connections and adjustments at different levels to realize multiplanar correction. 14
The objective of this retrospective study was: (i) to evaluate the clinical and radiographic results of patients who had undergone the Ilizarov method with midfoot osteotomy for rigid pes cavus correction; and (ii) to introduce our detailed experience on the Ilizarov technique for the correction of complex foot deformities.
Materials and Methods
Patients and Data Collection
With approval from the Ethics Committee of West China Hospital (No. 2024218). The clinical and radiological data of midfoot osteotomy combined with Ilizarov fixation procedures performed in patients for the correction of rigid pes cavus from March 2020 to September 2022 were screened based on the patients' information registration system.
Inclusion Criteria
Symptomatic rigid pes cavus (Meary's angle >10°);
The apex of deformity was at midfoot (the navicular or cuneiform bone).
Exclusion Criteria
Sequela of cerebral palsy with hypermyotonia of lower extremities;
Concurrent skin soft tissue, or bone infection, is not controlled;
Patients with severe neuromuscular disease and in the advanced stage, who are predicted to have poor clinical outcomes even if a successful surgical correction is achieved;
Incomplete clinical data or loss to follow‐up.
According to the inclusion and exclusion criteria, 12 patients (15 feet) with pes cavus who had been undergoing the Ilizarov method with midfoot osteotomy by the same surgical team were enrolled. The cohort comprised of 7 females and 5 males. The mean follow‐up was more than 30 months.
The visual analogue scale (VAS), the American Orthopedic Foot and Ankle Society hindfoot scale score (AOFAS), and 36‐item Short Form Health Survey (SF‐36)were obtained by one experienced foot and ankle surgeon at each follow‐up. All data were recorded in detail.
Pre‐Operative Assessment
A detailed medical history was necessary for surgeons to detect the causes.
Physical examination should be performed by a veteran surgeon, which included the appearance of the foot, muscle strength assessment, joint's range of motion, Coleman block test, and Silfverskiold test.
Radiographs should include standard weight‐bearing foot and ankle views (anteroposterior [AP], lateral). Long‐leg axial calcaneal view helped to identify the alignment of the hindfoot. Full length of lower limbs view helped to rule out any supramalleolar or limbs deformities. The AP view measurements included the talo–first metatarsal angle (TM1 angle). Lateral view measurements included the talo–first metatarsal angle (Meary's angle), which determines the apex of deformity. The long‐leg axial calcaneal view measurement included calcaneus varus angle (CVA angle).
Surgical Technique and Postoperative Care
The treatment of midfoot osteotomy combined with Ilizarov technique was performed for the rigid pes cavus with the apex at the midfoot after adequate preoperative preparation and planning (Figure 1). The procedure was performed with the patient in the supine or lateral position under general anesthesia. A thigh tourniquet was routinely used to achieve hemostasis. Our procedure aimed to archive a painless, plantigrade, and balanced foot.
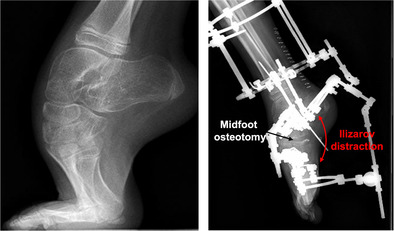
FIGURE 1.
The schematic diagram of midfoot osteotomy combined with Ilizarov technique for rigid pes casvus. (A) A linear osteotomy was performed for a rigid pes cavus when the apex is located in the midfoot. Black dashed line, midfoot osteotomy. White lines, the force line of foot. (B) Excellent correction was achieved without foot shorteningvia gradual distraction by Ilizarov technique. Bidirectional red arrow, Ilizarov distraction.Red area, distraction area.White line, the force line of foot.
Soft‐Tissue Release
In our experience, Achilles tendon lengthening, or gastrocnemius recession was performed firstly according to the result of the Silfverskiöld test. Then, the hindfoot was stabilized by inserting a 3.5‐mm Kirschner wire to maintain approximately 5° of heel valgus and dorsiflexion‐neutral position of ankle. The tendon transfer plans were individually drawn up for each patient. Usually, the posterior tibial or anterior tibial tendon and peroneal longus should be fully dissociated from their insertion, preserving as much length as possible. The releases of deltoid ligament, spring ligament, and the relevant joints capsules should be performed if satisfactory correction was not achieved. Where after, the flexibility of the hindfoot should be assessed once more. If not, the calcaneus osteotomy or subtalar arthrodesis should be done to restore the alignment of the hindfoot. Then, the bony deformity should be reevaluated to minor revision of the bony reconstruction plan after full soft‐tissue releases.
Bony Reconstruction
In this case series, midfoot osteotomy was performed before external fixation was applied. The bilateral approach, where an approximately 5–7‐cm‐long incision was made to expose the medial and lateral cuneiform, navicular, and cuboid. A periosteal elevator is inserted subcutaneous medially at the level of the first cuneiform to the lateral level of the cuboid. The blood vessels and nerves were protected during the dissection process. With the aid of fluoroscopy, the level of the osteotomy was identified on the AP view of the foot and was marked with K‐wires (Figure 2A). Transverse osteotomy from medial cuneiform or navicular to cuboid was performed at the apex of deformity (Figure 2B). Then, the rotation of the forefoot can be corrected immediately. After that, two crossed 1.0 or 1.5 mm K‐wires were inserted from the medial column and the lateral column to fix the dorsal cortex to prevent dorsal displacement of the distal end of the osteotomy during the gradual distraction.
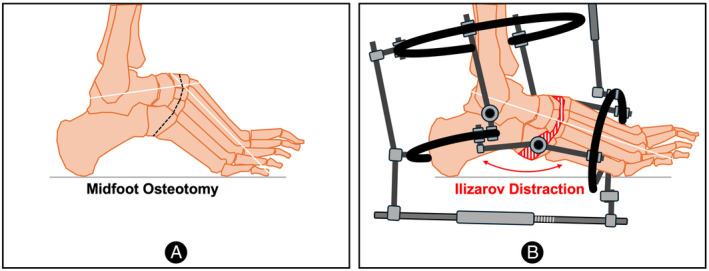
FIGURE 2.
The midfoot osteotomy combined with Ilizarov technique for rigid pes casvus. (A) The anteroposterior (AP) and lateral view of the foot for intraoperatively determining the level of the osteotomy. (B) The transverse midfoot osteotomy was performed after exposing the talar‐navicular joint, cuneiforms and cuboid. (C) The Ilizarov technique was performed to gradually correct the pes cavus.
Tendon Transfer
The tendon transfer procedure plan needed to be customized for each patient due to the variables of muscular forces. The relative overpowering activity of the peroneus longus and the posterior tibialis tendon was usually the main deformity force. The transfer of the peroneus longus to brevis, and the posterior tibialis to lateral seemed to be the most common transfer in those cases of pes cavus.
Application of Ilizarov External Frames
As shown in Figure 2C, the Ilizarov external frames consists of four parts: the tibial frame, the heel frame, the forefoot frame, and the plantar frame. Two parallel rings were fixed perpendicular to the tibia axis by four crossed 2.5 mm K‐wires. A 5‐mm diameter Schantz pin was introduced into the anterior tibia to enhance the stability of the frame. The calcaneus was fixed with two crossed 2.5 mm K wires locked to a half‐ring positioned perpendicular to the longitudinal axis. Two crossed 2.0 mm K wires were passed through the metatarsal and fixed to a half‐ring. The plantar frame consists of two parallel half‐rings and one rod. Each part of the Ilizarov external frames was individually attached to each other by screwed rods and hinges. After this, 110 Kg of tension was applied to the wires of the tibial frame, while 90 Kg of tension was applied to the wires of the heel and forefoot frames. The toes were fixed by 1.0 mm Kwires.
Postoperative Care
The initiation of correction began 3 days after surgery in a progressive manner. The cavus was corrected by distraction of the plantar rod, the adduction was corrected by adjusting the rods on the bilateral between the forefoot and heel, the equinus was corrected by distraction of the rods between the forefoot and tibia, and the hindfoot varus was corrected by adjusting the rods between the heel and tibia. The rate of distraction was usually 1 mm/day for each section, and the extension speed was dynamically adjusted according to the specific situation. During the distraction period, tension in the soft tissues, neurovascular status, pinning site condition, and presence of pain were monitored regularly.
After the correction period, the plantar frames were removed, and bilateral rods were applied to maintain the shape of the arch, while other parts of the frames were held in place for an additional 4 weeks to stabilize the correction. The patients were encouraged to walk with weight‐bearing. When the radiographic union was achieved, the Ilizarov external frame was removed, and the full weight‐bearing tolerance was activated. Follow‐up intervals were 4 weeks, 8 weeks, 12 weeks, 6 months, and every year post‐operation.
The sugical tips and pitfalls of midfoot osteotomy combined with Ilizarov distraction are described in detail in Table 1.
TABLE 1.
Tips and pitfalls of midfoot osteotomy combined with Ilizarov distraction.
| Tips | Pitfalls |
|---|---|
| Perform the procedures of soft tissue release before bony correction. | The bony deformity needs to be re‐evaluated and correction plan may be intraoperatively adjusted after soft tissue release. Otherwise, overcorrection may occur. |
| Midfoot osteotomy should be carefully performed at the apex of deformity under the fluoroscopy according to the correction plan. | During the surgery, preoperative planning should be implemented as much as possible during the operation, and there should be no illusion of resolving residual deformities through postoperative distraction. |
| Tendon transfer procedures are individualized based on preoperative physical examination. | Tendon transfer surgery can only solve the problem of muscle imbalance. Patients with serious dysregulation of the neuromuscular system (e.g., severe spasmatic cerebral palsy) are usually predicted to have poor clinical outcomes.Surgical correction of pes cavus deformity could only be performed for these patients with great caution when their neuromuscular symptoms could be improved by additional management. |
| Intraoperative confirmation of complete osteotomy should be made, and postoperative distraction should be performed promptly.The distraction speed should be controlled between 0.5 and 1 mm per day. | Failure to perform a complete osteotomy, a longer latency period and a slow distraction rate could result in premature consolidation in the distraction gap which needs to be solved by a secondary surgery. But excessive distraction speed can lead to soft tissue injury or neurovascular complications. |
| The toes should be fixed by 1.0 mm K‐wires to avoid the complication of subluxated toe joints. | The importance of postoperative rehabilitation needs to be emphasized, otherwise it will lead to stiff toes. |
Outcome Assessment
Radiological Assessment
Postoperative AP and lateral weight‐bearing x‐ray were analyzed. The radiographic views pre‐ and postoperative were taken by the same radiographic technician according to the same standards. The radiographic angles were measured by two of the authors using standard goniometer techniques. If there was any deviation between the two authors, it would be decided by the senior doctor. The radiographic measurements included the MA, TM1A, CVA, and footlength.
Rating Scale Assessment
All patients completed the VAS, AOFAS, and SF‐36 scores during the follow‐up visits. All data were recorded by the authors mentioned above.
Questionnaire
During follow‐up, patients were asked to fill out satisfaction questionnaires. The results were recorded and statistically analyzed by one of the authors.
Statistics Analysis
Data were analyzed with SPSS statistical software (IBM Statistics 20). The Shapiro–Wilk test was used to establish the normality criteria. The clinical and radiological results were evaluated by a paired t‐test. Continuous data were expressed in terms of the mean and the standard deviation (). A p value of <0.05 was considered significant.
Results
General Information
Midfoot osteotomy combined with Ilizarov external fixation was performed in 15 feet (8 left and 7 right) of 12 patients. Seven patients were male and five were female. The patient's age at the time of surgery was 33.9 ± 11.3 years (range from 16 to 54 years). The duration of clinical and radiographic follow‐up was 33.1 ± 5.0 months (range from 25 to 41 months).The etiology included poliomyelitis (4), idiopathic (3), trauma (2), spina bifida (2), and tethered cord syndrome (1). All patients had rigid pes cavus deformity with MA >10° (33.9° ± 9.2°), while 6 feet were with limb length discrepancies. All patients received additional soft tissue and bony procedure, including posterior tibial tendon transfer (7 feet), anterior tibial tendon transfer (8 feet), peroneus longus tendon transfer (12 feet), Achilles tendon lengthening (13 feet), gastrocnemius release (2 feet), and tibial lengthening (6 legs).
Radiological Outcomes
The duration of gradual correction was 30.4 ± 10.6 days, and the external fixation time was 116.3 ± 33.3 days. At last follow‐up, the bony union rate was 100%. The MA in all patients improved significantly to 7.8° ± 3.7° (p < 0.05), TM1A improved from 22.2° ± 5.8° to 9.2° ± 4.1° (p < 0.05), CVA were close to the normal range from 26.8° ± 8.1° to 8.6° ± 4.0° (p < 0.05).
Clinical Outcomes
All patients received plantigrade feet and pain relief. The VAS scores significantly improved from 5.8 ± 0.8 points to 1.4 ± 1.1 points (p < 0.05); the AOFAS scores improved from 38.7 ± 8.5 points to 88.6 ± 3.9 points (p < 0.05), while SF‐36 scores significantly improved from 78.6 ± 7.9 points to 106.4 ± 6.2 points (p < 0.05). The length of the feet was 23.4 ± 1.5 cm preoperatively, and 24.3 ± 1.7 cm postoperatively.
No major complications were reported except in 2 cases of residual mild hindfoot varus deformity. The results of the questionnaire showed that patients' satisfaction was 92% (11/12). The patients' demographics, surgical, and follow‐up data are summarized in Table 2. Typical cases are illustrated in Figures 3 and 4.
TABLE 2.
Baseline characterization of patients (n = 12).
| Case | Gender | Age (years) | Side | Deformity | Etiology | Procedure | Additional procedure | Correction time(days) | EFT (days) | Follow‐up (months) |
|---|---|---|---|---|---|---|---|---|---|---|
| 1 | M | 27 | L | PECV | Idiopathic | MO, EF | PTT, PL transfer, AT elongation | 21 | 92 | 25 |
| R | PECV | Idiopathic | MO, EF | PTT, PL transfer, AT elongation | 21 | 92 | 25 | |||
| 2 | F | 43 | L | PECV | TCS | MO, EF | ATT, ED, PL transfer, AT elongation | 29 | 100 | 34 |
| R | PECV | TCS | MO, EF | ATT, ED, PL transfer, AT elongation | 29 | 100 | 34 | |||
| 3 | F | 47 | L | PECV | Idiopathic | MO, EF | PTT, PL transfer, AT elongation | 19 | 89 | 41 |
| R | PECV | Idiopathic | MO, EF | PTT, PL transfer, AT elongation | 19 | 89 | 41 | |||
| 4 | M | 16 | R | PECV | Idiopathic | MO, EF | ATT, ED, PL transfer, GM release | 25 | 95 | 32 |
| 5 | M | 41 | L | PECV | Trauma | MO, EF | ATT, ED, PL transfer, AT elongation | 20 | 105 | 29 |
| 6 | F | 23 | L | PECV | Trauma | MO, EF | PTT, PL transfer, GM release | 22 | 90 | 35 |
| 7 | M | 31 | R | PECV, LLD | Poliomyelitis | MO, EF, LLL | ATT, PL transfer, AT elongation | 37 | 120 | 27 |
| 8 | F | 46 | R | PECV, LLD | Poliomyelitis | MO, EF, LLL | ATT transfer, AT elongation | 51 | 185 | 36 |
| 9 | M | 26 | L | PECV, LLD | Poliomyelitis | MO, EF, LLL | ATT, ED transfer, AT elongation | 32 | 119 | 33 |
| 10 | M | 54 | R | PECV, LLD | Poliomyelitis | MO, EF, LLL | ATT transfer, AT elongation | 39 | 115 | 40 |
| 11 | F | 27 | L | PECV, LLD | Spina bifida | MO, EF, LLL | PTT, ED, PL transfer, AT elongation | 44 | 180 | 31 |
| 12 | M | 26 | L | PECV, LLD | Spina bifida | MO, EF, LLL | PTT, ED, PL transfer, AT elongation | 48 | 174 | 34 |
Abbreviations: AT, Achilles's tendon; ATT, anterior tibial tendon; ED, extensor digital; EF, external fixation; EFT, external fixation time; F, female; GM, gastrocnemius; L, left; LLD, leg length discrepancy; LLL, lower limb lengthening; M, male; MO, midfoot osteotomy; PECV, pes equinocavovarus; PL, peroneus longus; PTT, posterior tibial tendon; R, right; TCS, tethered cord syndrome.
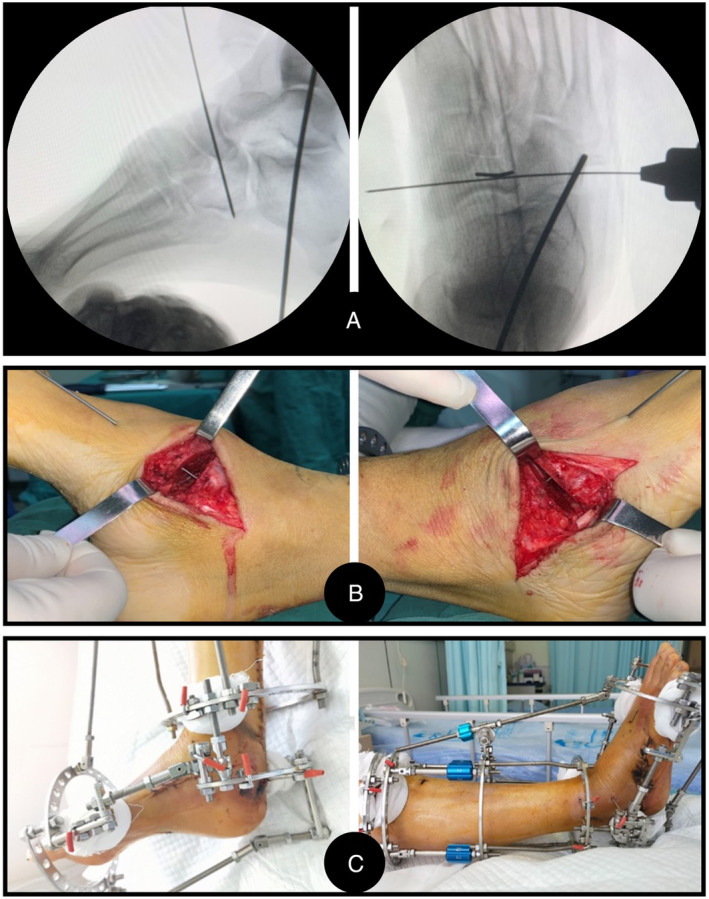
FIGURE 3.
A 16‐year‐old male patient with a congenital pes cavus was successfully treated by midfoot osteotomy combined with Ilizarov technique. (A) The preoperative outlook and (B) X‐ray show a rigid pes cavus. (C) The schematic diagram of preoperatively surgical planning and (D) X‐ray at 7 days after surgery show the midfoot osteotomy combined Ilizarov technique for this patient. White lines, the force line of foot. Red dashed line, midfoot osteotomy. Red area, distraction area. (E) The outlook and (F) X‐ray at 1 year after surgery show an excellent correction was achieved in this patient.
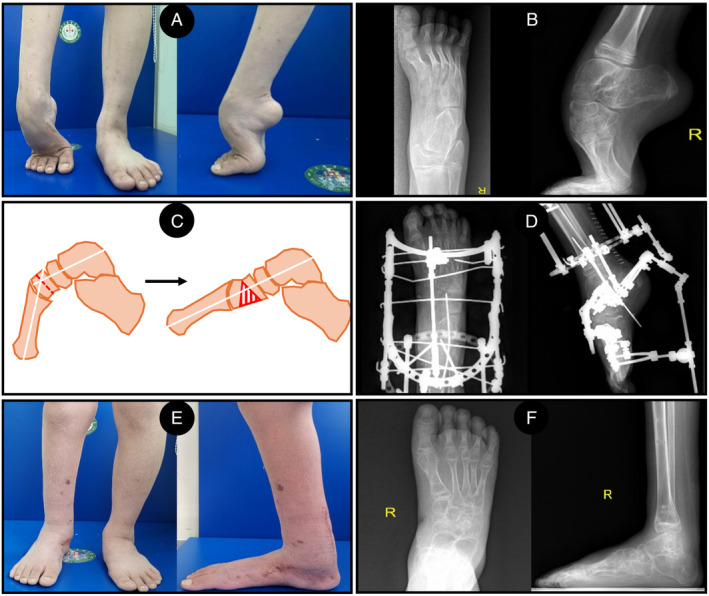
FIGURE 4.
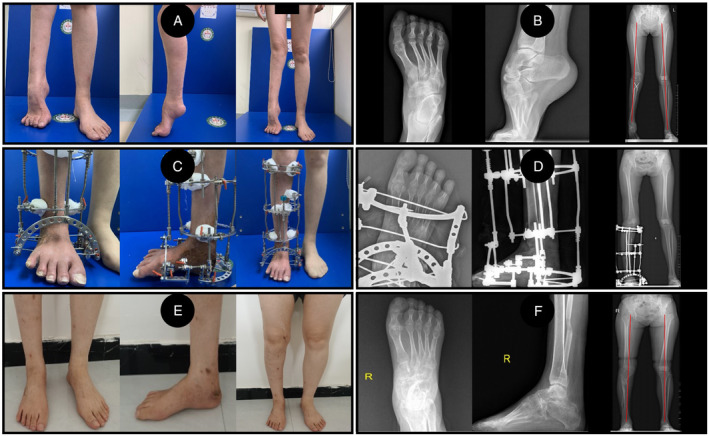
A 46‐year‐old female patient who suffered a rigid pes cavus and a limb deformity from poliomyelitis was successfully treated by midfoot osteotomy combined with Ilizarov technique. (A) The preoperative outlook and (B) X‐ray show a rigid pes cavus and a leg length discrepancy and valgus deformity of the ipsilateral lower extremity. Red lines, the force lines of low limbs. (C) The outlook and (D) X‐ray at 3 months after surgery show midfoot osteotomy combined with Ilizarov technique for this patient. (E) The outlook and (F) X‐ray at 2 years after surgery show excellent correction was achieved in this patient. Red lines, the force lines of low limbs.
Discussion
Main Findings of the Study
Despite the fact that the Cole midfoot osteotomy has been shown to be an effective method of correcting rigid pes cavus deformities, a significant limitation is the technical complexity associated with the multidirectional aspects of the deformity. 21 It requires a successful “one‐time” surgery once acute correction via a midfoot osteotomy with internal fixation is selected. Complications of neurovascular compromise, overcorrection or under correction, and the need for extensive exposure may be unavoidable in this condition. 9 , 10 , 11 , 22 More importantly, the frequent need for bone wedge resection results in the sacrifice of the normal joint and the additional shortening of the foot which seem to be unacceptable for some patients. 23 On the one hand, foot shortening not only affects appearance and walking stability but also causes inconvenience in footwear purchasing. 24 On the other hand, the sacrifice of the normal joint may lead to the loss of the foot's flexibility and adjacent joint degeneration. Here, we reported satisfactory outcomes of midfoot osteotomy combined with Ilizarov methods for correcting rigid pes cavus. All the radiographic parameters of foot improved significantly without the foot shortening and the sacrifice of normal joints after the combined treatment. The AOFAS scores improved from 38.7 ± 8.5 points preoperatively to 88.6 ± 3.9 points at the final follow‐up.
Ilizarov Technique
Gradual correction by Ilizarov technique has been confirmed as an effective and safe method to correct complex deformities in the foot with minimal complications. 25 , 26 The Ilizarov method involves minimally invasive surgery with the lower risk of soft tissue and neurovascular damage. 27 This technique is also forgiving, in that if further adjustment is needed after surgery, postoperative fine tuning could be performed to obtain satisfied correction under supervision. What is more, different from acute correction, distraction histiogenesis by Ilizarov technique makes it possible to maintain the length of the affected foot. The cavus could be corrected and the length of the foot could simultaneously be restored with the distraction of the plantar rod. Furthermore, as shown in this study, 6/12 (50%) of the patients suffered leg length discrepancy (LLD). Additionally, and to avoid foot shortening, correcting LLD in ipsilateral lower limb is also important for these patients. Our previous study has demonstrated that the Ilizarov method could provide a powerful and flexible ability for dynamical 3D correction of foot deformities and simultaneous correction of ipsilateral lower extremity deformities. 20 Also, additionally, the Ilizarov method allows for early weight‐bearing after removing the plantar frames, which is beneficial for bone healing in both foot and limb. 28 Thus, these above advantages make Ilizarov technique a good candidate for corrective pes cavus deformity.
The Methods of Osteotomy
However, it has been recognized that, in pes cavus with severe bony deformity, only distraction of soft tissues without bone correction may often result in joint incongruity or recurrence. Instead, such patients would benefit from osteotomy in combination with soft‐tissue procedures. Up to now, the combination of Ilizarov external fixator and osteotomy has been widely used to correct complex foot deformities, such as U‐osteotomy, 29 , 30 V‐osteotomy, 31 , 32 or Y‐osteotomy. 33 , 34 The U‐osteotomy is mainly used for severe rigid equinus deformity correction which is indicated in patients with preexisting stiffness and/or fusion of the subtalar joint. The V‐osteotomy is the combination of the posterior calcaneus oblique osteotomy and the anterior calcaneal‐talar osteotomy. Similarly, the Y‐osteotomy is also performed between calcaneus and talar. The three branches include the anterior branch of calcaneal‐talar osteotomy, the posterior branch of oblique calcaneus osteotomy, and vertical branch of vertical calcaneus osteotomy. These two osteotomy methods allow reshaping the foot by gradual distraction of the bones and soft tissues to realize the multiplanar correction with lengthening. The advantage of Y‐osteotomy is to avoid the diastasis of the calcaneus‐cuboid joint during distraction. Despite the powerful correction abilities mentioned above, the sacrifice of subtalar joints and residual forefoot deformity were unavoidable. However, when the apex of deformity was focused on the midfoot, the osteotomy methods mentioned before may be unsuitable. Complete correction can only be achieved by osteotomy at the apex of the deformity. However, it should be noted that wedge osteotomy at midfoot could lead to the sacrifice of normal joint and the shortening of foot. 23 In our study, all cases achieved three‐dimensional correction by a linear midfoot osteotomy. This osteotomy could also allow for multiplane correction. Since the osteotomy area is located at the apex of the deformity, usually at the navicular or cuneiform bones, the sacrifice of normal joints can be avoided. Moreover, foot shortening could be effectively avoided by combining this linear osteotomy with the Ilizarov technique.
Prevention of Complication
The goal of rigid pes cavus correction is to achieve a plantigrade, painless, functional, and stable foot. 35 Achieving this treatment goal requires not just a successful surgery but also a careful postoperative management. When Ilizarov distraction osteogenesis has been applied for the correction of bony deformity, failure to perform a complete osteotomy, a longer latency period, and a slow distraction rate could result in premature consolidation in the distraction gap. Bradley M. Lamm et al. 36 reported 3 of 26 feet experienced premature consolidation in their study, while Paley 25 reported premature consolidation in 2 of 4 cases. In our center, several effective measures were performed based on the experience from predecessors and lengthy clinical practices of our team to avoid this complication. Intraoperatively, we confirmed the complete osteotomy by repeated C‐arm fluoroscopy. Postoperatively, the distraction usually began at 3 days after surgery in a rate of 1 mm/day. The speed of distraction was adjusted according to the osteogenesis. X‐rays should be taken regularly to confirm the distraction of osteotomy. As shown in our results, all patients had good correction of foot deformities without premature consolidation by radiology and clinical evaluation.
Kocaoglu et al. 15 reported cases of subluxated toe joints by using the Ilizarov external fixator for foot deformities correction. To avoid this complication, the toes were fixed by 1.0 mm K‐wires during procedure in our study. At the same time, all patients underwent additional soft‐tissue balancing procedures, which aimed to minimize residual deformity and recurrence rates. Soft tissue imbalance played an important role in the occurrence and development of pes cavus. Hence, soft tissue balancing by means of tendon transfers or soft‐tissue release must be combined with bony procedures.
The adjustment of the Ilizarov external fixator is done in a gradual and progressive manner. 37 The adjustment plan for each patient is variable in a personalized manner. In our study, MA, TM1A, and CVA were almost corrected to the normal range by adjusting each part of the frame. Of course, dynamical imaging observations are essential to guide the adjustment procedure.The drawbacks of this technique, however, are the inconvenience and discomfort of patients due to the long duration of the Ilizarov external fixator and the occurrence of pin‐site infection.
Another thing to note is that it is important to capture the patient's expectations. Surgeons should give a realistic explanation of what the deformity correction will accomplish, what the foot will look like in the corrected position, and functional limitations.
Limitations
The limitations of our study are as follows: (1) the small sample size; (2) the retrospective nature with no valid control group; and (3) the short follow‐up period. Therefore, a large‐scale randomized control study with long‐term follow‐up is needed to prove the effectiveness and safety of the strategy proposed by the current study.
Prospects of Clinical Application
It is still a challenge to correct rigid pes cavus. When the apex of pes cavus is located in the midfoot, midfoot osteotomy combined with Ilizarov technique is an effective treatment to obtain a functional, normal‐looking, pain‐free, and plantigrade foot without foot shortening, and the sacrifice of normal joints. However, there are still potential risks requiring great attention to prevention, such as premature consolidation, subluxated toe joints, residual deformities, and so on.
Conclusion
In conclusion, the midfoot osteotomy combined with Ilizarov external frame is a preferable procedure with satisfying results for the correction of rigid pes cavus with the apex at the midfoot. However, high‐quality levels I and II studies with large sample sizes over long follow‐ups are needed to further verify its clinical effects.
Ethics Statement
Each author certifies that his or her institution approved the human protocol for this investigation, and that all investigations were conducted in conformity with ethical principles of research.
Conflict of Interest Statement
The authors declare that they have no conflicts of interest. Ethical approval for all procedures performed in studies involving human participants were in accordance with the ethical standards of institutional and/or national research committee, and with the 1964 Helsinki Declaration, and its later amendments or comparable ethical standards. Informed consent was obtained from all individual participants included in the study.
Author Contributions
Yaxing Li: Project administration; formal analysis; writing–original draft; writing–review & editing. Boquan Qin: Project administration; formal analysis; writing–original draft; writing–review & editing. Shijiu Yin: Formal analysis; writing–review & editing. Jia Li: Formal analysis; writing–review & editing. Yi Ren: Writing–review & editing. Ye Wu: Writing–review & editing. Xiang Fang: Writing–review & editing. Huiqi Xie: Supervision; writing–review & editing. Hui Zhang: Conceptualization; project administration; supervision; writing–review & editing.
Consent for Publication
Each author confirms that this manuscript has not been published elsewhere and is not under consideration by any other journal. All authors have approved the manuscript and agree with submission to Orthopaedic Surgery.
Consent to Participate
All patients included in this study agree to participate in this study.
Acknowledgments
This research was supported by the 1·3·5 project for disciplines of excellence–Clinical Research Incubation Project, West China Hospital, Sichuan University (22HXFH015), the Natural Science Foundation of Tibet Autonomous Region (Grant nos. XZ202201ZR0033G and XZ202201ZY0038G), the Natural Science Foundation of Sichuan Province (Grant no. 2023YFS0014), and the full‐time postdoctoral research and development fund of West China Hospital of Sichuan University (2024HXBH076).
Yaxing Li and Boquan Qin contributed equally to this study.
References
- 1. Akoh CC, Phisitkul P. Clinical examination and radiographic assessment of the Cavus foot. Foot Ankle Clin. 2019;24:183–193. [DOI] [PubMed] [Google Scholar]
- 2. Bai L‐B, Wang Z‐J, Wang Z‐T. Telescopic rod technique to reverse anterior subluxation of the talus during the correction of equinocavovarus deformity with the Ilizarov fixator. J Orthop Transl. 2020;25:43–46. [Google Scholar]
- 3. de la Huerta F. Correction of the neglected clubfoot by the Ilizarov method. Clin Orthop Relat Res. 1994;301:89–93. [PubMed] [Google Scholar]
- 4. Pavone V, Chisari E, Vescio A, Lucenti L, Sessa G, Testa G. The etiology of idiopathic congenital talipes equinovarus: a systematic review. J Orthop Surg Res. 2018;13:206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Sanpera I, Villafranca‐Solano S, Muñoz‐Lopez C, Sanpera‐Iglesias J. How to manage pes cavus in children and adolescents? EFORT Open Rev. 2021;6:510–517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. James Welck M, Haldar A. Hindfoot fusions in the Cavovarus foot: what is the key for a successful outcome? Foot Ankle Clin. 2023;28:805–818. [DOI] [PubMed] [Google Scholar]
- 7. Zide JR, Myerson MS. Arthrodesis for the cavus foot: when, where, and how? Foot Ankle Clin. 2013;18:755–767. [DOI] [PubMed] [Google Scholar]
- 8. Myerson MS, Myerson CL. Managing the complex Cavus foot deformity. Foot Ankle Clin. 2020;25:305–317. [DOI] [PubMed] [Google Scholar]
- 9. Grady JF, Schumann J, Cormier C, LaViolette K, Chinn A. Management of Midfoot Cavus. Clin Podiatr Med Surg. 2021;38:391–410. [DOI] [PubMed] [Google Scholar]
- 10. Ergun S, Yildirim Y. The Cole Midfoot osteotomy: clinical and radiographic retrospective review of five patients (six feet) with different etiologies. J Am Podiatr Med Assoc. 2019;109:180–186. [DOI] [PubMed] [Google Scholar]
- 11. Cole WH. The classic. The treatment of claw‐foot. By Wallace H. Cole. 1940. Clin Orthop Relat Res. 1983;181:3–6. [PubMed] [Google Scholar]
- 12. Ferreira RC, Costa MT, Frizzo GG, Santin RA. Correction of severe recurrent clubfoot using a simplified setting of the Ilizarov device. Foot Ankle Int. 2007;28:557–568. [DOI] [PubMed] [Google Scholar]
- 13. Kucukkaya M, Kabukcuoglu Y, Kuzgun U. Management of the neuromuscular foot deformities with the Ilizarov method. Foot Ankle Int. 2002;23:135–141. [DOI] [PubMed] [Google Scholar]
- 14. Ferreira RC, Costo MT, Frizzo GG, da Fonseca Filho FF. Correction of neglected clubfoot using the Ilizarov external fixator. Foot Ankle Int. 2006;27:266–273. [DOI] [PubMed] [Google Scholar]
- 15. Kocaoğlu M, Eralp L, Atalar AC, Bilen FE. Correction of complex foot deformities using the Ilizarov external fixator. J Foot Ankle Surg. 2002;41:30–39. [DOI] [PubMed] [Google Scholar]
- 16. El‐Mowafi H, El‐Alfy B, Refai M. Functional outcome of salvage of residual and recurrent deformities of clubfoot with Ilizarov technique. Foot Ankle Surg. 2009;15:3–6. [DOI] [PubMed] [Google Scholar]
- 17. El Barbary H, Abdel Ghani H, Hegazy M. Correction of relapsed or neglected clubfoot using a simple Ilizarov frame. Int Orthop. 2004;28:183–186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Oganesyan OV, Istomina IS, Kuzmin VI. Treatment of equinocavovarus deformity in adults with the use of a hinged distraction++ apparatus. J Bone Joint Surg Am. 1996;78:546–556. [DOI] [PubMed] [Google Scholar]
- 19. Kirienko A, Peccati A, Abdellatif I, Elbatrawy Y, Mostaf ZM, Necci V. Correction of poliomyelitis foot deformities with Ilizarov method. Strategies Trauma Limb Reconstr. 2011;6:107–120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Boquan Q, Yi R, Tingjiang G, Xi L, Hui Z. Complex foot deformities associated with lower limb deformities: a new therapeutic strategy for simultaneous correction using Ilizarov procedure together with osteotomy and soft tissue release. J Orthop Surg Res. 2020;15:492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Turco VJ. Surgical correction of the resistant club foot. One‐stage posteromedial release with internal fixation: a preliminary report. J Bone Joint Surg Am. 1971;53:477–497. [PubMed] [Google Scholar]
- 22. Tullis BL, Mendicino RW, Catanzariti AR, Henne TJ. The Cole midfoot osteotomy: a retrospective review of 11 procedures in 8 patients. J Foot Ankle Surg. 2004;43:160–165. [DOI] [PubMed] [Google Scholar]
- 23. Hosny GA. Correction of foot deformities by the Ilizarov method without corrective osteotomies or soft tissue release. J Pediatr Orthop B. 2002;11:121–128. [DOI] [PubMed] [Google Scholar]
- 24. Mun KR, Chun S, Hong J, Kim J. The relationship between foot feature parameters and postural stability in healthy subjects. Hum Factors. 2019;61:1077–1085. [DOI] [PubMed] [Google Scholar]
- 25. Paley D. The correction of complex foot deformities using Ilizarov's distraction osteotomies. Clin Orthop Relat Res. 1993;293:97–111. [PubMed] [Google Scholar]
- 26. Choi IH, Yang MS, Chung CY, Cho TJ, Sohn YJ. The treatment of recurrent arthrogrypotic club foot in children by the Ilizarov method. A preliminary report. J Bone Joint Surg Br. 2001;83:731–737. [DOI] [PubMed] [Google Scholar]
- 27. Paley D, Lamm BM. Correction of the cavus foot using external fixation. Foot Ankle Clin. 2004;9:611–624. x. [DOI] [PubMed] [Google Scholar]
- 28. Birch JG, Samchukov ML. Use of the Ilizarov method to correct lower limb deformities in children and adolescents. J Am Acad Orthop Surg. 2004;12:144–154. [DOI] [PubMed] [Google Scholar]
- 29. Du H, He XT, Yin XH, Gu JM, Zhou YX, Yang J, et al. The gradual correction of adult severe rigid Equinus deformity using minimal invasive U‐osteotomy with Taylor spatial frame. Foot Ankle Int. 2023;44:62–70. [DOI] [PubMed] [Google Scholar]
- 30. Küçükkaya M, Karakoyun O, Armağan R, Kuzgun U. Correction of complex lower extremity deformities with the use of the Ilizarov‐Taylor spatial frame. Acta Orthop Traumatol Turc. 2009;43:1–6. [DOI] [PubMed] [Google Scholar]
- 31. Shalaby H, Hefny H. Correction of complex foot deformities using the V‐osteotomy and the Ilizarov technique. Strategies Trauma Limb Reconstr. 2007;2:21–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Segev E, Ezra E, Yaniv M, Wientroub S, Hemo Y. V osteotomy and Ilizarov technique for residual idiopathic or neurogenic clubfeet. J Orthop Surg (Hong Kong). 2008;16:215–219. [DOI] [PubMed] [Google Scholar]
- 33. Lee K, Cho JH, Lee WC. The indications and technique for surgical correction of pes cavus with external fixation. Foot Ankle Clin. 2013;18:743–753. [DOI] [PubMed] [Google Scholar]
- 34. Kirienko A, Gradov L, Malagoli E, Tacci F, Lucchesi G. Correction of a complex foot deformity with V and Y osteotomy and Ilizarov method. J Foot Ankle Surg. 2022;61:1209–1220. [DOI] [PubMed] [Google Scholar]
- 35. Stapleton JJ, DiDomenico LA, Zgonis T. Corrective midfoot osteotomies. Clin Podiatr Med Surg. 2008;25:681–690, ix. [DOI] [PubMed] [Google Scholar]
- 36. Lamm BM, Gourdine‐Shaw MC, Thabet AM, Jindal G, Herzenberg JE, Burghardt RD. Distraction osteogenesis for complex foot deformities: Gigli saw midfoot osteotomy with external fixation. J Foot Ankle Surg. 2014;53:567–576. [DOI] [PubMed] [Google Scholar]
- 37. Sharma A, Cherian RJ, Pandey RA, Khatter H, Paul R, John B. Clinico‐radiological and functional outcome of difficult Talipes Equinovarus deformity corrected with an Ilizarov fixator. J Foot Ankle Surg. 2022;61:719–725. [DOI] [PubMed] [Google Scholar]


