Abstract
The presence of the stomach in the thorax is called gastrothorax. If excessive dilatation occurs due to a valve mechanism in the stomach which then is herniated into the thorax, it is called tension gastrothorax and the situation can be life-threatening. In late presentation, congenital diaphragmatic hernias or traumatic diaphragmatic hernias, if the stomach located in the thorax is severely distended, it can be confused with tension pneumothorax or pleural effusion/empyema. We presented tension gastrothorax in two patients with distended stomach in the thorax, in which tension pneumothorax and pleural effusion/empyema-like images were created, based on plain X-rays taken at the first admission in the emergency department, which may cause diagnostic confusion. The tension gastrothorax can cause mediastinal shift, which can lead to respiratory distress and eventually cardiac arrest secondary to obstructive shock. In case of mediastinal shift, it should reduce the tension of the stomach located in the thorax by inserting a nasogastric catheter, and if this fails, by aspiration with a needle.
Keywords: Congenital diaphragmatic hernias, emergency interventions, respiratory distress, tension gastrothorax, traumatic diaphragmatic hernias
Introduction
Most cases of congenital diaphragmatic hernia (CDH) are diagnosed prenatally or in the first 24 h after birth due to severe respiratory distress and are associated with a high mortality rate. In a large systematic review, the overall prevalence of CDH was found to be 2.3 per 10,000 births, and male gender and maternal age over 35 years of age were associated with CDH. Black ethnicity of the mother appeared to be a protective factor.[1,2] 5%–25% of patients with CDH present late and have a much better prognosis due to the absence of significant pulmonary hypoplasia and hypertension.[2,3] The clinical presentation of late-diagnosed CDH includes a broad spectrum, ranging from recurrent pulmonary infection, growth retardation, abdominal pain, vomiting, and chest pain, to respiratory distress, and rarely, cardiac arrest caused by massive distension of the intrathoracic stomach.[2,3] This condition can be confused with tension pneumothorax and pleural effusion or empyema.[4]
Gastrothorax occurs as a result of increased intra-abdominal pressure due to coughing, defecation, blunt trauma to the abdomen, feeding, etc., and when the stomach passes through a congenital or acquired defect in the diaphragm. Then, through a one-way valve mechanism, massive distension of the herniated stomach to the thorax may develop, which is called tension gastrothorax,[4] and it was first described in the literature in 1984 in an adult patient, as a complication of posttraumatic diaphragmatic rupture.[5]
Tension gastrothorax, which is rarely encountered, can be seen at any age, it can be congenital or traumatic and can cause severe respiratory distress and even sudden cardiac arrest. In this article, due to pleural effusion and tension pneumothorax-like images seen in the first chest radiographs taken in the emergency room of two patients who were brought to the emergency room due to respiratory distress, the clues of tension gastrothorax in these radiographs and the initial treatment of tension gastrothorax were discussed.
Case Reports
Case 1
A 16-year-old female was admitted to our emergency department (ED) with chest pain and severe respiratory distress.
In the patient’s medical history, she had epigastric pain intermittently for the last month, she had no chest pain and did not consult a physician with these complaints. In addition, the patient had no history of trauma. The patient had not previously undergone any radiological investigation with the preliminary diagnosis of a congenital diaphragmatic hernia. Then, the family decided to go to the ED after the onset of the patient’s chest pain, which had started the last day, got worse, and respiratory distress eventually developed.
The chest X-ray was taken when the patient was admitted to the emergency room which showed an air–liquid-fluid level, and it was determined that the mediastinum had shifted to the right [Figure 1a], the subsequent thorax computed tomography (CT) revealed that this view was gastrothorax. In addition, colon loops as well as the stomach were observed in the left hemithorax on CT. The patient’s blood gases were within normal limits at the time of admission. A nasogastric catheter could not be placed into the stomach. The patient was operated under emergency conditions. Posterolateral diaphragmatic hernia with a diameter of 4 cm was detected during the operation. The defect was repaired primarily after the stomach and colonic loops were reduced into the abdomen. The patient had an uneventful postoperative period and was discharged on the 4th postoperative day.
Figure 1.
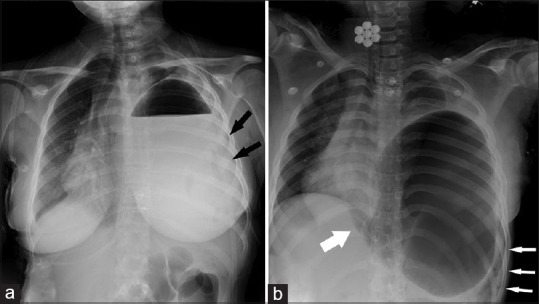
(a) A view showing air-fluid level in the entire left hemithorax, and patchy radiolucent areas are observed in the left lung subzone (black arrows). The diaphragmatic border of the lung on the left, the left cardiophrenic, and costophrenic sinuses are indistinct. While the mediastinal structures are deviated to the right, angulation of the left main bronchus towards the cranial due to being pushed at the level of the hilus, (b) A radiolucent area is observed in the left hemithorax, which causes mediastinal shift and is continuous with the esophagus (thick white arrow). The left main bronchus is angled toward the cranial due to being pushed at the level of the hilum and subsequently loses its radiolucent appearance. In the left hemithorax, the diaphragm lung border, costophrenic, and cardiophrenic sinuses are indistinct. Patchy radiolucent areas are observed in the lower left zone (thin white arrows)
Case 2
A 15-year-old female patient with sudden-onset chest pain and respiratory distress was brought to the ED through ambulance by emergency medical services staff being ventilated all the way with a balloon valve mask.
The patient had no history of trauma, and no information concerning previous similar complaints could be obtained from the family who live in a rural area. The patient was never consulted to a physician before with the aforementioned complaints.
The physical examination was remarkable for central cyanosis, severe intercostal, and suprasternal retractions. Her respiratory rate was 40/min and heart rate was 180/min, and auscultation of the lung revealed diminished breath sound on the left side. Initially, blood gas results were pH 6.9, SO2 39, PO2 45, HCO3 5.5, lactate 21, and PCO2 87, respectively, suggesting respiratory acidosis. The patient was immediately intubated endotracheally.
During this time, a rapid chest X-ray was taken on the bedside in the ED, and the image [Figure 1b] suggested a gastrothorax. Shortly after, cardiopulmonary resuscitation was initiated for the patient who developed cardiac arrest. The nasogastric catheter could not be advanced into the stomach, so immediately a 14-gauge needle was inserted through the 6th intercostal space from the middle axillary line. In addition, the presence of bile content during gas aspiration with a needle suggested that the appearance in the plain X-ray image belonged to an enlarged intrathoracic stomach. In the meantime, cardiopulmonary resuscitation was continued, but the patient did not respond to cardiopulmonary resuscitation despite the reduction of intrathoracic pressure.
There is a limitation in the second case which should be mentioned. Since no autopsy was performed, it is unknown whether the cause of death was due to trauma or CDH.
Discussion
In a healthy child who suddenly develops severe respiratory distress, a pneumothorax with mediastinal shift or a pleural effusion-like appearance on the first plain chest radiograph taken in the ED may be due to gastrothorax. This situation may cause confusion in the diagnosis and may lead to misdiagnosis of the patient and insertion of a thoracic tube.
However, there are some clues in the first plain thorax radiographs. In tension pneumothorax, the diaphragm is depressed and easily identified on plain chest radiographs, while the contours of the diaphragm are not clear in gastrothorax, which can help us in the differential diagnosis.[6] The fact that the radiolucent area in the left hemithorax continues along with the esophagus, which we encountered in our second case, may be a very special finding in recognizing gastrothorax. Moreover, it is stated in the literature that malrotations are mostly present in late-diagnosed cases.[2] The presence of patchy radiolucent areas in the left hemithorax in the direct chest radiographs of our cases suggests that the colon loops pass into the left hemithorax and overlap with the stomach.
In addition, showing the bending of the inserted large-diameter nasogastric or orogastric catheter in the chest cavity on plain X-ray is extremely useful in the diagnosis of tension gastrothorax, and this is also the initial treatment of tension gastrothorax. With this maneuver, gastric decompression is provided, and further tension development is prevented. Definitive diagnosis can be made with contrast studies or thoracic CT. However, the patient’s severe clinical condition may not allow detailed radiological examination in every case. If nasogastric/orogastric catheter placement fails, decompression of the stomach in the lower intercostal space with a transthoracic needle is recommended, so an enlarged stomach will cause a mediastinal shift, which may impair venous return and cause cardiac arrest. Therefore, the treatment of the tension gastrothorax is urgent. At this stage, after excessive distension is prevented and the patient is stabilized, definitive surgical treatment of CDH is planned.[3,4,7,8] However, although needle decompression is recommended as a treatment method in case reports and approach algorithms, there is no scientific evidence regarding the effectiveness and usefulness of this method.
Conclusion
Tension gastrothorax, which is rarely encountered, can be seen at any age, can be congenital or traumatic, and can cause severe respiratory distress and even sudden cardiac arrest.
Because of these two cases, it was emphasized in our article that in patients who were admitted to the ED due to severe respiratory distress, when the first plain chest radiographs showed mediastinal shift and a tension pneumothorax-like appearance or air-fluid level, tension gastrothorax may be present.
For this reason, the emergency physician should be able to distinguish between gastrothorax and tension pneumothorax or pleural effusion. In case of mediastinal shift, it should reduce the tension of the stomach located in the thorax by inserting a nasogastric catheter, and if this fails, by aspiration with a needle, which is the first intervention of tension gastrothorax in emergency conditions.
Conflicts of interest
None Declared.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patients have given their consent for their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Funding
None.
References
- 1.Paoletti M, Raffler G, Gaffi MS, Antounians L, Lauriti G, Zani A. Prevalence and risk factors for congenital diaphragmatic hernia: A global view. J Pediatr Surg. 2020;55:2297–307. doi: 10.1016/j.jpedsurg.2020.06.022. [DOI] [PubMed] [Google Scholar]
- 2.Bagłaj M. Late-presenting congenital diaphragmatic hernia in children: A clinical spectrum. Pediatr Surg Int. 2004;20:658–69. doi: 10.1007/s00383-004-1269-5. [DOI] [PubMed] [Google Scholar]
- 3.Horst M, Sacher P, Molz G, Willi UV, Meuli M. Tension gastrothorax. J Pediatr Surg. 2005;40:1500–4. doi: 10.1016/j.jpedsurg.2005.05.079. [DOI] [PubMed] [Google Scholar]
- 4.Ng J, Rex D, Sudhakaran N, Okoye B, Mukhtar Z. Tension gastrothorax in children: Introducing a management algorithm. J Pediatr Surg. 2013;48:1613–7. doi: 10.1016/j.jpedsurg.2013.05.066. [DOI] [PubMed] [Google Scholar]
- 5.Ordog GJ, Wasserberger J, Balasubramaniam S. Tension gastrothorax complicating post-traumatic rupture of the diaphragm. Am J Emerg Med. 1984;2:219–21. doi: 10.1016/0735-6757(84)90008-1. [DOI] [PubMed] [Google Scholar]
- 6.Zedan M, El-Ghazaly M, Fouda A, El-Bayoumi M. Tension gastrothorax: A case report and review of literature. J Pediatr Surg. 2008;43:740–3. doi: 10.1016/j.jpedsurg.2007.10.072. [DOI] [PubMed] [Google Scholar]
- 7.Azagury DE, Karenovics W, Stähli DM, Mathis J, Schneider R. Management of acute gastrothorax with respiratory distress: Insertion of nasogastric tube as a life saving procedure. Eur J Emerg Med. 2008;15:357–8. doi: 10.1097/MEJ.0b013e32830346c3. [DOI] [PubMed] [Google Scholar]
- 8.Næss PA, Wiborg J, Kjellevold K, Gaarder C. Tension gastrothorax: Acute life-threatening manifestation of late onset congenital diaphragmatic hernia (CDH) in children. Scand J Trauma Resusc Emerg Med. 2015;23:49. doi: 10.1186/s13049-015-0129-8. [DOI] [PMC free article] [PubMed] [Google Scholar]


