ABSTRACT
Background:
The mortality risks of children undergoing various cardiac surgeries for congenital heart disease (CHD) in India are not well defined. We conducted a systematic review and meta-analysis to estimate the inhospital mortality of various common CHD surgeries reported in India and compared it to representative data from established Western databases.
Methods and Results:
We searched four bibliographic databases for studies published in India over the last 25 years. In total, 135 studies met the inclusion criteria and included 30,587 patients aged from 1 day to 65 years. The pooled mortality rate of 43 Indian studies reporting multiple CHD surgical outcomes is 5.63% (95% confidence interval [CI]: 4.26–7.16; I2 = 93.9%), whereas the Western data showed a pooled mortality rate of 2.65% (P value for comparison <0.0001). The pooled mortality risk for ventricular septal defect closure and tetralogy of Fallot repair in Indian studies was 2.87% (95% CI: 0.76–5.91; I2 = 62.4%) and 4.61% (95% CI: 2.0–8.02; I2 = 87.4%), respectively. The estimated mortality risk was higher than the Western databases for all subcategories studied except for surgeries in the grown-ups with CHD population and coarctation repair.
Conclusions:
The estimated mortality risks are higher among Indian patients undergoing cardiac surgery for CHD as compared to Western data. We need prospective multicentric data to document whether the observed excess mortality exists after adjusting for various high-risk features and comorbidities in Indian patients. We need systemic measures to improve the outcomes of CHD surgeries in India.
Keywords: Operative mortality, low- and middle-income countries, pooled mortality risk, congenital heart surgery
INTRODUCTION
Across the globe, around 130 million children are born annually, and 4 million are estimated to die during the neonatal period.[1] Seven percent of these deaths are due to congenital abnormalities,[2] with cardiac illness being the most common.[3,4] It is estimated that 90% of children are born in low- and middle-income countries (LMIC). However, <20% of cardiac surgeries happen in these countries.[5,6] A vast majority of children with correctable congenital heart disease (CHD) are not operated on time in the LMIC countries. India’s high birth rate predicts 150,000–200,000 children are born with CHD each year, with at least 50,000 neonates and infants requiring early intervention.[5,7] Currently, less than one-third to one-fourth of these children are operated on. Children undergoing surgery in LMIC countries are often burdened with comorbidities of heart failure, serious infections, prolonged cyanosis, pulmonary vascular disease, and malnutrition.[8]
In India, lower rates of antenatal diagnosis of CHD, delayed diagnosis of CHD, issues related to accessibility and affordability of pediatric cardiac care, and lack of a formal referral system for CHD may lead to inadequate delivery of care. Hence, CHD surgery-related outcomes may be suboptimal in India as compared to the corresponding Western data. However, the magnitude of differences is unknown and could vary for different surgeries and subgroups. Large-scale prospective data from India studying the outcomes of CHD surgeries are limited. In addition, analyses comparing pediatric cardiac surgery outcomes across countries are limited.[9] No formal analysis specifically compares the outcomes of CHD surgeries observed in India with those of developed countries. Hence, we compiled the published data from India over 25 years on CHD surgical outcomes in this systematic review. We intended to estimate the inhospital mortality of cardiac surgeries for CHD reported from India and compare it to the representative data from established Western registries of the developed world, such as the STS (Society of Thoracic Surgeons) Database.
MATERIALS AND METHODS
Search strategy
We searched the electronic databases PubMed, Embase, Web of Science, and Scopus for studies published in India between January 1998 and March 2023. The search terms included “congenital heart disease” OR “congenital heart defect” OR “congenital heart malformation” AND “outcome” OR “surgery.” Our initial searches revealed 46,304 studies, which were narrowed down to 1442 after applying the date range and country filters. We also manually searched the reference lists of relevant articles and review papers.
Study selection
The following steps were taken for study selection: (1) identification of titles of records through database search, (2) removal of duplicates, (3) screening and selection of abstracts, (4) assessment for eligibility through full-text articles, and (5) final inclusion in the study. There were no language restrictions. Two authors (LK and SR) independently screened the titles and abstracts of the identified studies for relevance and then reviewed the full-text articles for inclusion/exclusion. When there was disagreement, a third reviewer (MK) decided to include or exclude the study. Ethical approval did not apply to this study because it consisted of a systematic review with meta-analysis. The study protocol was registered in the PROSPERA database (ID: CRD42023462297).
Inclusion and exclusion criteria
Using the Population, Interventions, Comparison, Outcome, and Study Design strategy, studies were included if the following criteria were fulfilled: (1) Patients who underwent any cardiac surgical procedure for a CHD; (2) Published in the last 25 years (1998–2023), (3) Published from an Indian center, (4) Outcomes studied included hospital mortality, and (5) Studies could be retrospective, prospective, clinical trials, or case series. We excluded studies reporting surgical outcomes of only specific risk-category patients and redo surgery. Case reports and case series with less than five patients were also excluded. We extracted the following data from each included study: total number of patients, age (mean/median and range), gender, type of surgical deaths including operative, inhospital, and 30-day mortality, and preoperative risk scores. Any discrepancies were resolved through discussion. The studies were then divided into overall and lesion-specific groups based on the population studied.
Outcomes
The primary outcome of the meta-analysis is to estimate the inhospital mortality of cardiac surgeries for CHD reported from India and compare it to the representative data from established Western databases. Secondary outcomes included individual surgical mortality of various common lesions reported from India and analysis of the reported Risk Adjustment for Congenital Heart Surgery (RACHS) score-based mortality. We planned to report the outcome of surgery for ventricular septal defect (VSD), aortopulmonary window, and coarctation of the aorta among acyanotic CHD. Tetralogy of Fallot (TOF), transposition of great arteries (TGA), and total anomalous pulmonary venous drainage (TAPVC) outcomes were compared to represent the correctable cyanotic CHD group. Among the palliative surgeries, we compared outcomes of the pulmonary artery banding, Blalock–Taussig–Thomas shunt (BTTS), bidirectional Glenn shunt (BDG), and Fontan surgeries. The outcome of surgeries for grown-ups with congenital heart disease is also compared with the available Western database. We excluded studies reporting other CHD surgery outcomes, including atrial septal defect, atrio-ventricular septal defect, partial venous anomalous venous drainage, double-outlet right ventricle, and congenital valve surgeries.
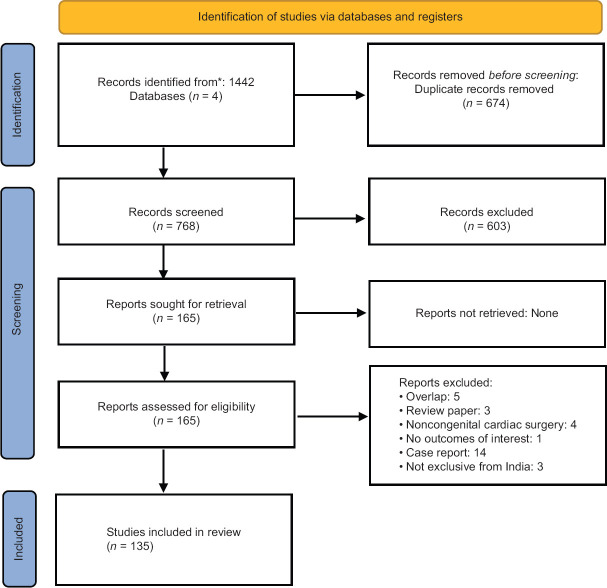
Data extraction
The method is outlined in the PRISMA flow diagram [Figure 1].
Figure 1.
Schematic flow chart showing the selection of studies
Risk-of-bias (quality) assessment
Risk-of-bias assessment was made using the mixed method appraisal tool (MMAT) version 2018 for systematic reviews of studies, including qualitative, quantitative, and mixed methods studies. Sufficient data for analysis were available for 133 studies. The most common category of the studies was quantitative descriptive (126), followed by randomized controlled trials (6), and the remaining one was a nonrandomized clinical trial. The individual study MMAT scoring table and overall category-wise scores are provided in Supplementary Table 1.
Supplementary Table 1.
Overall percentage score of risk-of-bias assessment by mixed method appraisal tool
| Category | Number of studies | Score (%) |
|---|---|---|
| Overall | 42 | 89.05 |
| GUCH | 13 | 84.62 |
| TGA | 10 | 89.09 |
| TAPVC | 9 | 77.78 |
| TOF | 17 | 87.65 |
| PAB | 6 | 73.33 |
| BTTS | 7 | 85.71 |
| BDG | 7 | 81.43 |
| Fontan | 3 | 80 |
| VSD | 8 | 83.75 |
| APW | 7 | 88.57 |
| CoA | 4 | 90 |
MMAT: Mixed method appraisal tool, GUCH: Grown-ups with congenital heart disease, TGA: Transposition of great arteries, TAPVC: Total anomalous pulmonary venous connection, TOF: Tetralogy of Fallot, PAB: Pulmonary artery banding, BTTS: Blalock–Taussig–Thomas shunt, BDG: Bidirectional Glenn shunt, VSD: Ventricular septal defect, APW: Aortopulmonary window, COA: Coarctation of the aorta
Statistical analysis
A pairwise meta-analysis was performed for overall analysis. We used the DerSimonian and Laird random effects model in our study to determine the 95% confidence interval (CI) and pooled risk ratio for each outcome. We utilized the Higgins I2 statistic to compute between-study heterogeneity calculations. Low heterogeneity and high heterogeneity are defined by I2 <25% and >75%, respectively. We also conducted a leave-one-out sensitivity analysis to eliminate the impact of individual studies on our findings. The studies were divided into overall and lesion-specific groups based on the population studied. We used the Chi-square test to compare Indian data with the Western outcome. All tests were 2-tailed with a P < 0.05 considered statistically significant.
Reporting
We reported the results of our meta-analysis using the Preferred Reporting Items for Systematic Reviews and Meta-Analyses guidelines. The estimates of sensitivity and CIs are presented.
RESULTS
Out of the 1442 studies identified, 135 were finally included in the analysis, and the process is summarized in Figure 1. Details of the included Indian studies are presented in Table 1. Most studies were retrospective (73.3%) and single-center (99.3%) studies reporting lesion-specific outcomes. Only one study (Nair et al. 2021) was a multicentric study reporting outcomes among 2059 patients with CHD from Kerala.[10] Only 43 studies reported outcomes of multiple CHD surgeries, and 65.2% of studies were published in the last 10 years. The primary analysis excluded studies reporting data from other LMICs (not exclusively in India).[11,12,13] About 16% of the patients in these analyses were from seven Indian centers. For the comparator, the Western data obtained from reports published in 2021 by the Society of Thoracic Surgery (STS)[14] were multicentric and prospective, while the GUCH data obtained from the European database[15] were retrospective in nature.
Table 1.
Details of the included Indian congenital heart disease surgery outcome studies
| Type of outcome reported | Number of studies | Prospective (%) | In the last 10 years (2012–2023), n (%) |
|---|---|---|---|
| Overall outcome | 43 | 23 (53.5) | 31 (72.1) |
| GUCH population | 13 | 0 | 6 (46.2) |
| Lesion-specific - acyanotic CHD surgeries | |||
| Ventricular septal defect | 8 | 4 (50) | 7 (87.5) |
| Aortopulmonary window | 7 | 0 | 6 (85.7) |
| Coarctation of aorta | 4 | 0 | 3 (75) |
| PA banding | 5 | 0 | 2 (40) |
| Lesion-specific - cyanotic CHD surgeries | |||
| TOF | 19 | 8 (42.1) | 16 (84.2) |
| TGA | 10 | 1 (10) | 7 (70) |
| TAPVC | 10 | 0 | 5 (50) |
| BTTS | 7 | 0 | 1 (14.3) |
| Bidirectional Glenn shunt | 6 | 0 | 2 (33.3) |
| Fontan | 3 | 0 | 2 (66.7) |
CHD: Congenital heart disease, GUCH: Grown-ups with congenital heart disease, PA: Pulmonary artery, TOF: Tetralogy of Fallot, TGA: Transposition of great arteries, TAPVC: Total anomalous pulmonary venous connection, BTTS: Blalock–Taussig–Thomas shunt
We compared the mortality outcomes reported by 135 Indian studies and compared them with the major international multicentric registries. We included 30,587 patients with ages ranging from 1 day to 65 years. The studies were divided based on patient population, either reporting outcomes of lesion-specific studies or varied CHD surgeries. The pooled mortality rate of the 43 studies reporting varied multiple CHD surgical outcomes published in the country from 1998 to 2023 is 5.63% (95% CI: 4.26–7.16; I2 = 93.9%) [Figure 2], whereas the Western data throughout 2016–2021 reported a mortality rate of 2.65%. When we compared the Indian studies published in the last 10 years (after 2012), the pooled mortality is 5.35% (95% CI: 4.46–6.32). We also performed a supplementary analysis, including studies involving other LMICs that included a significant proportion of patients from India (otherwise excluded in the primary analysis). This analysis involving 49 studies (n = 86116) showed a pooled mortality rate of 5.84% (95% CI: 4.93–6.82; I2 = 94.4%).
Figure 2.
Pooled analysis of in-hospital mortality reported by pediatric cardiac surgery studies from India[10,16,17,18,19,20,21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54]
Only a few Indian and LMIC studies reported RACHS classification-based outcomes [Table 2a]. However, more studies reported the distribution of patients in various RACHS classes [Table 2b]. Out of 20,511 patients included in these studies, RACHS scoring could be calculated for 19,606 patients [Table 2b]. The chosen Western databases reported STAT categorization only [Table 3].
Table 2a.
Risk adjustment for congenital heart surgery category-wise mortality reported from the pooled Indian and low- and middle-income countries studies[11,43,44]
| RACHS-1 category | Alam S et al. (2018) | Joshi S et al. (2014) | Jenkins KJ et al. (2014) | Total | Mortality (%) |
|---|---|---|---|---|---|
| 1 | 163 | 224 | 2724 | 3111 | 1.51 |
| 2 | 613 | 797 | 7254 | 8664 | 4.07 |
| 3 | 72 | 111 | 3347 | 3530 | 10.67 |
| 4 | 72 | 5 | 750 | 827 | 17.62 |
| 5+6 | 0 | 0 | 87 | 87 | 51.10 |
RACHS: Risk adjustment for congenital heart surgery
Table 2b.
The Indian and low- and middle-income countries studies that are reporting the risk adjustment for congenital heart surgery score[11,28,43,44,46,55,56]
| Author (year) | Total (n) | Mortality (%) | RACHS 1, n (%) | RACHS 2, n (%) | RACHS 3, n (%) | RACHS 4, n (%) | RACHS 5, n (%) | RACHS 6, n (%) |
|---|---|---|---|---|---|---|---|---|
| Joshi SS et al. (2014) | 1150 | 7.9 | 224 (19.5) | 797 (69.3) | 111 (9.7) | 5 (0.4) | 0 | 0 |
| Jenkins KJ et al. (2014) | 15,049 | 6.3 | 2724 (18.1) | 7254 (48.2) | 3347 (22.2) | 750 (5.0) | 9 (0.1) | 78 (0.5) |
| Reddy et al. (2015) | 1028 | 4.1 | 50 (4.9) | 544 (52.9) | 303 (29.5) | 120 (11.7) | 0 | 11 (1.1) |
| Balachandran R et al. (2015) | 1702 | 3.0 | 230 (13.5) | 815 (47.9) | 510 (30.0) | 129 (7.6) | 2 (0.1) | 11 (0.7) |
| Alam S et al. (2018) | 574 | 3.5 | 51 (8.9) | 407 (70.9) | 62 (10.8) | 54 (9.4) | 0 | 0 |
| Alam S et al. (2018) | 920 | 3.0 | 163 (17.7) | 613 (66.6) | 72 (7.8) | 72 (7.8) | 0 | 0 |
| Karri S et al. (2022) | 88 | 8.0 | 0 | 48 (54.6) | 9 (10.2) | 28 (31.8) | 3 (3.4) | 0 |
| Overall | 19,606 | 5.8 | 3442 (17.6) | 10,478 (53.4) | 4414 (22.5) | 1158 (5.9) | 14 (0.1) | 100 (0.5) |
RACHS: Risk adjustment for congenital heart surgery
Table 3.
Society of Thoracic Surgeons - European Association for Cardio-Thoracic Surgery category-wise mortality reported from the Society of Thoracic Surgeons database[14]
| Database | STAT category | n (%) | Mortality rate (%) |
|---|---|---|---|
| STS (2021) | 1 | 27,163 (28.1) | 0.40 |
| 2 | 33,244 (34.4) | 1.38 | |
| 3 | 11,272 (11.7) | 2.02 | |
| 4 | 21,150 (21.9) | 6.15 | |
| 5 | 3765 (3.9) | 12.23 | |
| Overall | 96,594 (100) | 2.65 |
STS: Society of Thoracic Surgeons, STAT: The STS - European Association for Cardio-Thoracic Surgery
Western data showed the maximum number of patients in STAT category 1. Nearly two-thirds of patients were in categories 1–3, with <4% of patients in category 4 and none in category 5. In contrast, most Indian patients belonged to RACHS category 2, with 6.5% belonging to categories 4–6. Numerically, the observed mortality seems higher in Indian studies across the various classes. However, head-to-head comparison of Indian, other LMICs and Western data were impossible due to significant heterogeneity in reporting preoperative risk classification and outcomes. Similarly, the age and gender distribution of patients also could not be meaningfully analyzed due to significant heterogeneity in reporting.
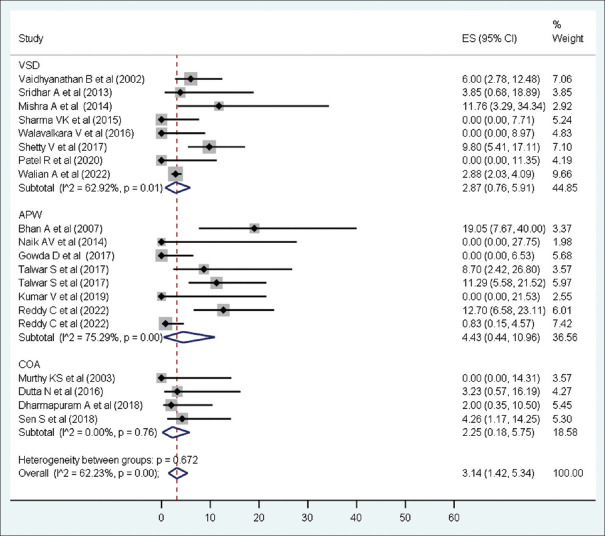
The pooled inhospital mortality of surgery reported by Indian studies for VSD (n = 1400; 8 studies) was 2.87% (95% CI: 0.76–5.91; I2 = 62.4%), coarctation of the aorta (n = 151; 4 studies) was 2.25% (95% CI: 0.18–5.75; I2 = 0%), and APW (n = 368; 7 studies) was 4.43% (95% CI: 0.44–10.96; I2 = 75.29%) [Figure 3].
Figure 3.
Pooled analysis of in-hospital mortality reported by Indian studies – Selected surgeries for acyanotic congenital heart diseases (VSD,[57,58,59,60,61,62,63,64] APW,[65,66,67,68,69,70,71] COA[72,73,74,75]). VSD: Ventricular septal defect, APW: Aortopulmonary window, COA: Coarctation of the aorta. (Reddy C, et al. (2022) Single comparative study of APW simple versus complex groups[69])
Among surgeries for cyanotic CHD, the pooled inhospital mortality of surgery reported by Indian studies for TGA (n = 1069; 10 studies) was 9.2% (95% CI: 4.86–14.6; I2 = 83.19%), TAPVC (n = 1157; 10 studies) was 7.96% (95% CI: 2.54–15.65; I2 = 93%), and TOF (n = 2053; 19 studies) was 4.53% (95% CI: 2.09–7.67; I2 = 86.64%) [Figure 4].
Figure 4.

Pooled analysis of in-hospital mortality reported by Indian studies – Selected surgeries for cyanotic congenital heart diseases. (TGA,[76,77,78,79,80,81,82,83,84,148] TAPVC,[85,86,87,88,89,90,91,92,93,94] TOF[95,96,97,98,99,100,101,102,103,104,105,106,107,108,109,110,111,112]). TGA: Transposition of great arteries, TAPVC: Total anomalous pulmonary venous connection, TOF: Tetralogy of Fallot
The pooled inhospital mortality of palliative surgeries reported by Indian studies were: PA banding (n = 284; 5 studies) 5.82% (95% CI: 0.3–15.87; I2 = 85.69%), blalock-taussig-thomas (BTT) shunt (n = 371; 7 studies) 5.61% (95% CI: 2.31–9.96; I2 = 49.65%), BDG (n = 1116; 6 studies) 4.04% (95% CI: 1.56–7.45; I2 = 81.22%), and Fontan (n = 242; 3 studies) 5.89% (95% CI: 2.19–11.01; I2 = 0%) [Figure 5].
Figure 5.
Pooled analysis of in-hospital mortality reported by Indian studies – Selected palliative surgeries (PAB,[113,114,115,116] BTS,[117,118,119,120,121,122,145] BDG,[123,124,125,126,127,128] Fontan[129,130,131]). PAB: Pulmonary artery banding, BTTS: Blalock-Taussig-Thomas shunt, BDG: Bidirectional Glenn. (Chowdhury et al. (2001)[125] single comparative study of outcomes of BDG based on two groups before and after 2 years of age)
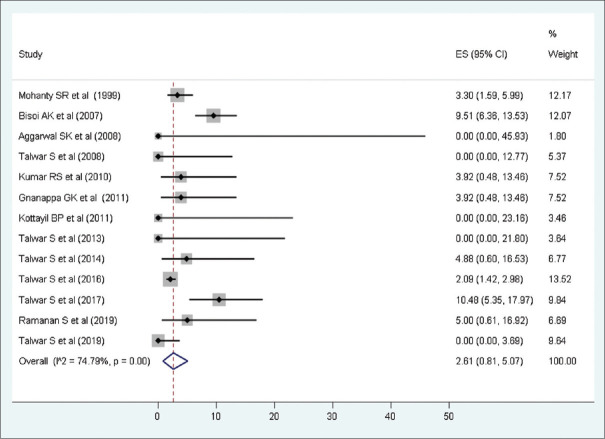
Analysis of cardiac surgery among the GUCH population included 13 Indian studies involving 2467 patients. The pooled mortality was 2.61% (95% CI: 0.81–5.07; I2 = 74.8%) [Figure 6].
Figure 6.
Pooled analysis of in-hospital mortality reported by Indian studies involving the GUCH population[91,130,132,133,134,135,136,137,138,139,140,141,142,143]
We compared the pooled mortality from Indian studies with that from representative Western databases [Table 4].
Table 4.
| Category | Western data | Pooled Indian studies | P | |||
|---|---|---|---|---|---|---|
|
|
|
|||||
| Database | Patients (n) | Mortality (%) | Patients (n) | Pooled mortality (95% CI) | ||
| Overall | STS database | 96,594 | 2.65 | 19,723 | 5.63 (4.26–7.16) | <0.00001 |
| GUCH population | Vida VL et al. (European database) | 20,602 | 3.02 | 2467 | 2.61 (0.81–5.07) | 0.22 |
| TGA | STS database (ASO) | 1876 | 1.90 | 1069 | 9.20 (4.86–14.60) | <0.00001 |
| TGA-VSD | STS database (ASO + VSD) | 849 | 5.30 | |||
| TOF | STS database | 4569 | 1.20 | 2053 | 4.51 (2.0–8.02) | <0.00001 |
| BDG | STS database | 4027 | 2.00 | 1116 | 4.04 (1.56–7.45) | <0.00001 |
| FONTAN | STS database | 3791 | 1.10 | 242 | 5.89 (2.19–11.01) | <0.00001 |
| VSD | STS database | 7161 | 0.43 | 1400 | 2.87 (0.76–5.91) | <0.00001 |
| COA | STS database | 3460 | 1.01 | 151 | 2.25 (0.18–5.75) | 0.06 |
CI: Confidence interval, STS: Society of Thoracic Surgeons, GUCH: Grown-ups with congenital heart disease, ASO: Arterial switch operation, TGA: Transposition of great arteries, VSD: Ventricular septal defect, TOF: Tetralogy of Fallot, BDG: Bidirectional Glenn shunt, COA: Coarctation of aorta, CI: Confidence interval
For studies reporting the outcome of multiple varied CHD surgeries, the pooled mortality of Indian studies was 5.63% compared to 2.65% reported by the STS database (P < 0.00001 for comparison). For surgery among the GUCH population, the mortality reported was 2.61% by Indian studies compared to 3.02% by the European database (P = 0.22). Indian pooled mortality was higher for all the lesion-specific outcomes analyzed except for surgery for coarctation of the aorta (P = 0.06).
DISCUSSION
Our analysis shows that Indian patients have a pooled mortality rate of 5.84% (4.93–6.82) for cardiac surgery for CHD, which is comparable to that reported from other LMIC countries (5.65% [5.0%–6.8%]).[11,12,13] However, it is much higher than the mortality rates reported by Western databases. This remains the only study that cumulatively included representative data from across India, comprising over 30000 surgeries outlined in 135 studies. The mortality ranged widely from 0% to 35%, denoting a heterogeneous pool of studies, as seen from the distribution of I2 values except for VSD closure and BT shunt (I2 values >25–<75). Our lesion-specific mortalities were also significantly higher than the Western data, except for the GUCH population and coarctation of the aorta.
The estimated all-age mortality for CHD in 2019 is 2.80 (2.29–3.38) per 100,000 population, with a 60.4% (41.4–71.9) decrease from 1990, and the estimated age-standardized mortality for CHD is 3.23 (2.64–3.92) per 100,000 population, with a 45.5% (19.5–61.1) decrease from 1990. India remains the most significant contributor, with 38,000 deaths (25,000-56,000).[144] Most of the excess CHD-related mortality in India is due to lack of timely surgery. However, some excess could be related to suboptimal cardiac surgery outcomes.
Among the studies included in this meta-analysis, 14 studies[19,23,26,32,34,35,41,45,79,85,92,120,121,145] reported data exclusively from 2199 neonatal surgeries and reported 155 deaths, with mortality rates ranging from zero to 10.4 percent. Exclusive infant cardiac surgeries were reported by 21[19,23,24,28,32,34,35,37,41,44,45,46,78,80,83,89,120,121,122,145] studies with 4791 patients and 413 deaths, with mortality rates ranging up to 21%. The mortality from CHD surgery in infancy diagnosed either prenatally or through newborn screening from a single center in California, US, is 10.4%.
The developed nations have established databases for prospective recording of CHD surgical outcomes. The IQIC collaborative is another worldwide initiative with over 70 sites in 25 developing countries. The STS database[14] reported outcomes of 96,594 operations in 2021, while data from LMIC countries (including India) reported by the IQIC network in 2019 comprised 54521 operations.[11,12,13] Currently, 17 centers in India are partner centers that share data with the framework.[13] However, some of India’s most populated states with the highest birth rates and lowest GDP (gross domestic product) are not part of the framework. Some of these states do not even have one center capable of providing optimal treatment for neonates and children born with CHD.[7]
Indian children undergoing surgery frequently have advanced heart failure, severe cyanosis, pulmonary vascular disease, and malnutrition.[8] The median weight for age standard score (Z score) of patients undergoing congenital heart surgery reported by George et al. was −3.2.[50] A few studies established a worsening mortality trend with undernutrition severity. Indian population-based studies have shown that the median z score of healthy Indian children is -0.59, with 8% of urban and 42% of rural children being underweight.[146,147] This leaves Indian children of the same age at risk of higher mortality due to lower weight as compared to their Western counterparts.
The surgical mortality for VSDs ranged from zero to 11.8%; however, the eldest patient was 22 years,[64] with the mean age of the studies ranging from 3 months to 3 years. Apart from undernutrition and infection, delayed presentation and advanced pulmonary vascular disease could have contributed to the excess mortality of Indian children with VSD undergoing surgical closure. Of the eight studies assessing VSD surgical outcomes, three studied the role of perioperative intravenous sildenafil.[58,60,62] Two studies specifically looked at outcomes of apical and multiple muscular defects, a rather complicated subset to tackle among various subtypes.[57,64] One study reported outcomes from all children >2 years of age, with two-thirds of patients being nonresponders on preoperative vasoreactivity testing during catheterization.[59] A delayed age at surgery and advanced cyanosis may be the most critical factors contributing to excess mortality in patients with cyanotic CHD undergoing either palliative or corrective surgery in India. The RACHS score, which is widely used for risk stratification, unfortunately, does not consider non-cardiac factors such as malnutrition, preexisting sepsis, and late presentation which have a significant impact on the outcomes of surgery in India and other LMICs.
Our surgical mortality for TGA ranged from none, as reported in atrial switch operations, to nearly 20% in the earliest reported arterial switch series from 2002. Notably, the age of the patients in the study ranged up to adolescence,[148] which remains a rare occurrence in developed nations. Two of these studies specifically report outcomes in late presenters of TGA-IVS beyond 6 weeks,[80,82] while one study reports outcomes in a subset with intramural coronaries.[84] These subgroups are well-established factors for increased mortality following an arterial switch operation. The higher mortality in TGA studies from India is primarily due to late presentation and multiple comorbidities like severe infection and a sicker state at presentation. On the other hand, a survey by Kunde et al. reports the lowest mortality rates of TGA in patients with prenatal detection and planned peripartum care in India.[81]
Ten studies report outcomes of TAPVC repair in 1157 patients, with 107 deaths. A recent study of TAPVC from South India reported outcomes matching those reported from Western countries. In addition, one of the studies reported outcomes beyond infancy,[90] while another reported outcomes beyond 10 years of age.[91] Surprisingly, both these groups have reported no mortality. Among the studies reporting outcomes following surgical repair of TOF, two report outcomes in the absence of a pulmonary valve. At the same time, one mentions outcomes specifically in the anomalous pulmonary branch from the aorta subset. These studies have been excluded from sensitivity analyses.
Lack of organized systems of care, transport systems, trained workforce, referral mechanisms, insurance, and other support systems are some of the significant limitations of Indian pediatric cardiac care systems that contribute to this excess mortality.[149,150,151] In many hospitals, surgeons deal with a huge patient load and often lack the support systems to deliver high-quality care. Despite all these challenges, surgery for CHD in India costs less than a fraction of what it costs in the developing world.[152]
Efforts to improve outcomes– Islands of excellence
Among the studies reporting the overall surgical CHD mortality, 13 studies[10,16,17,21,25,41,42,44,48] have mortality rates equal to or lesser than the STS data. The IQIC analysis from 2019 showed that India, despite having a low GDP per capita income, showed a standardized mortality ratio of <1.[13] According to the GBD (global burden of disease) data in 2017, India has shown a modest reduction in CHD mortality of –1.36% [–1.75 to –0.98] from 1990 to 2019.[144] Hridyam, Kerala state health department’s scheme to check mortality due to CHD has performed over 7000 surgeries. The scheme employs screening of children for CHD at birth, anganwadis, schools, and home visits. A referral system is outlined for further confirmation of diagnosis and management. Various government and private hospitals are empanelled under the scheme for financial support. The Ayushman Bharat Pradhan Mantri Jan Arogya Yojana (PM-JAY) and the various state-sponsored financing schemes are beginning to impact the care of children with CHD in India.[152] Under the West Bengal government-sponsored scheme, 11,483 surgical interventions have been done over 10 years, with an inhospital mortality rate of 5.2%.[153] Three studies identifying the impact of the intrauterine diagnosis of CHD on neonatal surgery have reported mortality rates of 0%, 2%, and 3%, respectively, showcasing the ability of Indian health-care providers to do optimum management when the challenges are preplanned.[35,41,45] In India, maintaining and improving surgical standards and attracting fresh talent to pediatric cardiac surgery are significant challenges in the future.[149,150,151]
Limitations of the study
Most of the studies included in the analysis were retrospective in nature and, hence, are marred by shortcomings. Significant heterogeneity was observed in the studies, so the overall effect may be skewed. The analysis is subject to publication bias, and the actual mortality may be greater than reported numbers. The studies are from a handful of significant centers, which would affect results both ways. Most publications are from academic institutions, whereas most congenital heart surgery in India is done in nonacademic and private institutions, with less compulsion to publish data. The derived results may, therefore, not reflect the situation in the public or private sectors.
We compared our data with the STS 2021 data, which comprises data from July 2016 to June 2022. A comparison with STS data from the corresponding period of Indian studies would have been more accurate. The STS 2016 data,[154] comprising data from 1998 to 2014, reported a mortality rate of 3.4%. The mortality of STS 2016 was significantly higher than the 2021 data (2.65%; P < 0.05 for comparison). However, the cumulative mortality from the Indian studies (mortality-5.63%) is still higher than even the STS 2016 data (P < 0.05). The GUCH data from the Western population included patients with residual lesions and redo sternotomies, whereas corresponding Indian data included predominately unoperated late presenters, making direct comparisons erroneous.
Even though we tried to be meticulous in our search for Indian studies, we could have inadvertently missed a few studies. Furthermore, we could not include the more recent (2024) large series involving over 11,000 Indian children undergoing cardiac surgery.[153] However, the reported mortality in that series (5.2%) was close to our estimate (5.63%). Comprehensive, uniform surgical training and standardized postoperative management may promote better results; however, catering to the most complex versions of the illness and significant delays in surgery due to long waiting lists would affect the outcomes negatively.
CONCLUSIONS
CHD surgical mortality in India is higher than in the developed nations. The estimated lesion-specific mortalities are significantly higher than the Western data, except for the GUCH population and coarctation of the aorta. Factors inherent to socioeconomic status, demographics, and health-care system accessibility are vital in determining outcomes. We must establish prospective multicentric registries to document the quantum and the causes of the observed excess mortality. We need systemic measures to improve the outcomes of CHD surgeries in India.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Hug L, You D, Blencowe H, Mishra A, Wang Z, Fix MJ, et al. Global, regional, and national estimates and trends in stillbirths from 2000 to 2019: a systematic assessment. Lancet. 2021;398:772–85. doi: 10.1016/S0140-6736(21)01112-0. [doi: 10.1016/S0140-6736(21)01112-0] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lawn JE, Cousens S, Zupan J Lancet Neonatal Survival Steering Team. 4 million neonatal deaths: When? Where? Why? Lancet. 2005;365:891–900. doi: 10.1016/S0140-6736(05)71048-5. [DOI] [PubMed] [Google Scholar]
- 3.Saxena A, Mehta A, Sharma M, Salhan S, Kalaivani M, Ramakrishnan S, et al. Birth prevalence of congenital heart disease: A cross-sectional observational study from North India. Ann Pediatr Cardiol. 2016;9:205–9. doi: 10.4103/0974-2069.189122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Vaidyanathan B, Sathish G, Mohanan ST, Sundaram KR, Warrier KK, Kumar RK. Clinical screening for congenital heart disease at birth: A prospective study in a community hospital in Kerala. Indian Pediatr. 2011;48:25–30. doi: 10.1007/s13312-011-0021-1. [DOI] [PubMed] [Google Scholar]
- 5.Saxena A. Congenital heart disease in India: A status report. Indian Pediatr. 2018;55:1075–82. [PubMed] [Google Scholar]
- 6.Vervoort D, Jin H, Edwin F, Kumar RK, Malik M, Tapaua N, et al. Global access to comprehensive care for paediatric and congenital heart disease. CJC Pediatr Congenit Heart Dis. 2023;2:453–63. doi: 10.1016/j.cjcpc.2023.10.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ramakrishnan S. Pediatric cardiology: Is India self-reliant? Ann Pediatr Cardiol. 2021;14:253–9. doi: 10.4103/apc.apc_153_21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Liu J. Challenges and progress of the pediatric cardiac surgery in Shanghai Children's Medical Center: A 25-year solid collaboration with project HOPE. Semin Thorac Cardiovasc Surg Pediatr Card Surg Annu. 2009:12–8. doi: 10.1053/j.pcsu.2009.01.020. [DOI] [PubMed] [Google Scholar]
- 9.Bateson BP, Deng L, Ange B, Austin E, Dabal R, Bowser T, et al. Primary or delayed repair for complete atrioventricular septal defect, tetralogy of fallot, and ventricular septal defect: Relationship to country economic status. World J Pediatr Congenit Heart Surg. 2024;15:11–8. doi: 10.1177/21501351231204333. [DOI] [PubMed] [Google Scholar]
- 10.Nair SM, Zheleva B, Dobrzycka A, Hesslein P, Sadanandan R, Kumar RK. A population health approach to address the burden of congenital heart disease in Kerala, India. Glob Heart. 2021;16:71. doi: 10.5334/gh.1034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Jenkins KJ, Castañeda AR, Cherian KM, Couser CA, Dale EK, Gauvreau K, et al. Reducing mortality and infections after congenital heart surgery in the developing world. Pediatrics. 2014;134:e1422–30. doi: 10.1542/peds.2014-0356. [DOI] [PubMed] [Google Scholar]
- 12.Sen AC, Morrow DF, Balachandran R, Du X, Gauvreau K, Jagannath BR, et al. Postoperative infection in developing world congenital heart surgery programs: Data from the international quality improvement collaborative. Circ Cardiovasc Qual Outcomes. 2017;10:e002935. doi: 10.1161/CIRCOUTCOMES.116.002935. [DOI] [PubMed] [Google Scholar]
- 13.Rahman S, Zheleva B, Cherian KM, Christenson JT, Doherty KE, de Ferranti D, et al. Linking World Bank development indicators and outcomes of congenital heart surgery in low-income and middle-income countries: Retrospective analysis of quality improvement data. BMJ Open. 2019;9:e028307. doi: 10.1136/bmjopen-2018-028307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kumar SR, Mayer JE, Jr, Overman DM, Shashidharan S, Wellnitz C, Jacobs JP. The society of thoracic Surgeons congenital heart surgery database: 2021 update on outcomes and research. Ann Thorac Surg. 2021;112:1753–62. doi: 10.1016/j.athoracsur.2021.10.002. [DOI] [PubMed] [Google Scholar]
- 15.Vida VL, Zanotto L, Torlai Triglia L, Zanotto L, Maruszewski B, Tobota Z, et al. Surgery for adult patients with congenital heart disease: Results from the European database. J Clin Med. 2020;9:2493. doi: 10.3390/jcm9082493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Sahu MK, Das A, Siddharth B, Talwar S, Singh SP, Abraham A, et al. Arrhythmias in children in early postoperative period after cardiac surgery. World J Pediatr Congenit Heart Surg. 2018;9:38–46. doi: 10.1177/2150135117737687. [DOI] [PubMed] [Google Scholar]
- 17.Joshi RK, Aggarwal N, Agarwal M, Dinand V, Joshi R. Assessment of risk factors for a sustainable “on-table extubation” program in pediatric congenital cardiac surgery: 5-year experience. J Cardiothorac Vasc Anesth. 2016;30:1530–8. doi: 10.1053/j.jvca.2016.06.017. [DOI] [PubMed] [Google Scholar]
- 18.Talwar S, Khadgawat R, Sandeep JA, Sreenivas V, Choudhary SK, Gupta N, et al. Cardiopulmonary bypass and serum thyroid hormone profile in pediatric patients with congenital heart disease. Congenit Heart Dis. 2012;7:433–40. doi: 10.1111/j.1747-0803.2012.00667.x. [DOI] [PubMed] [Google Scholar]
- 19.Mohammed S, Menon S, Gadhinglajkar SV, Baruah SD, Ramanan SV, Gopalakrishnan KA, et al. Clinical outcomes of Del Nido cardioplegia and St Thomas blood cardioplegia in neonatal congenital heart surgery. Ann Card Anaesth. 2022;25:54–60. doi: 10.4103/aca.aca_220_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Vasdev S, Chauhan S, Malik M, Talwar S, Velayoudham D, Kiran U. Congenital heart surgery outcome analysis: Indian experience. Asian Cardiovasc Thorac Ann. 2013;21:675–82. doi: 10.1177/0218492312466751. [DOI] [PubMed] [Google Scholar]
- 21.Joshi SS, Keshava M, Murthy KS, Sambandamoorthy G, Shetty R, Shanmugasundaram B, et al. Coronavirus disease 2019 convalescent children: Outcomes after congenital heart surgery. Cardiology in the Young. 2022;32:1469–74. doi: 10.1017/S1047951121004509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Balachandran R, Nair SG, Gopalraj SS, Vaidyanathan B, Kumar RK. Dedicated pediatric cardiac intensive care unit in a developing country: Does it improve the outcome? Ann Pediatr Cardiol. 2011;4:122–6. doi: 10.4103/0974-2069.84648. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Bakshi KD, Vaidyanathan B, Sundaram KR, Roth SJ, Shivaprakasha K, Rao SG, et al. Determinants of early outcome after neonatal cardiac surgery in a developing country. J Thorac Cardiovasc Surg. 2007;134:765–71. doi: 10.1016/j.jtcvs.2007.04.042. [DOI] [PubMed] [Google Scholar]
- 24.Sahu MK, Singal A, Menon R, Singh SP, Mohan A, Manral M, et al. Early enteral nutrition therapy in congenital cardiac repair postoperatively: A randomized, controlled pilot study. Ann Card Anaesth. 2016;19:653–61. doi: 10.4103/0971-9784.191550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Solomon RS, Sasi T, Sudhakar A, Kumar RK, Vaidyanathan B. Early neurodevelopmental outcomes after corrective cardiac surgery in infants. Indian Pediatr. 2018;55:400–4. [PubMed] [Google Scholar]
- 26.Shukla VV, Bobhate P, Mohanty S, Rao S, Joshi P, Joshi V. Early outcomes of neonatal cardiac surgery in India. Indian Pediatr. 2020;57:129–32. [PubMed] [Google Scholar]
- 27.Talwar S, Patel K, Juneja R, Choudhary SK, Airan B. Early postoperative arrhythmias after pediatric cardiac surgery. Asian Cardiovasc Thorac Ann. 2015;23:795–801. doi: 10.1177/0218492315585457. [DOI] [PubMed] [Google Scholar]
- 28.Karri S, Mandal B, Kumar B, Puri G, Thingnam S, Kumar H, et al. Effect of perioperative use of oral triidothyronine for infants undergoing complex congenital cardiac surgeries under cardiopulmonary bypass: A double-blinded randomised controlled study. Ann Card Anaesth. 2022;25:270–8. doi: 10.4103/aca.aca_51_22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Kundan S, Tailor K, Radhakrishnan HB, Mohanty SR, Bhavsar K, Kadam S, et al. Elective delayed sternal closure portends better outcomes in congenital heart surgery: A retrospective observational study. Indian J Thorac Cardiovasc Surg. 2019;35:530–8. doi: 10.1007/s12055-019-00830-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Chauhan S, Malik M, Malik V, Chauhan Y, Kiran U, Bisoi AK. Extra corporeal membrane oxygenation after pediatric cardiac surgery: A 10 year experience. Ann Card Anaesth. 2011;14:19–24. doi: 10.4103/0971-9784.74395. [DOI] [PubMed] [Google Scholar]
- 31.Garg R, Rao S, John C, Reddy C, Hegde R, Murthy K, et al. Extubation in the operating room after cardiac surgery in children: A prospective observational study with multidisciplinary coordinated approach. J Cardiothorac Vasc Anesth. 2014;28:479–87. doi: 10.1053/j.jvca.2014.01.003. [DOI] [PubMed] [Google Scholar]
- 32.Karmegaraj B, Kappanayil M, Sudhakar A, Kumar RK. Impact of transport on arrival status and outcomes in newborns with heart disease: A low-middle-income country perspective. Cardiol Young. 2020;30:1001–8. doi: 10.1017/S1047951120001420. [DOI] [PubMed] [Google Scholar]
- 33.Vaidyanathan B, Nair SB, Sundaram KR, Babu UK, Shivaprakasha K, Rao SG, et al. Malnutrition in children with congenital heart disease (CHD) determinants and short term impact of corrective intervention. Indian Pediatr. 2008;45:541–6. [PubMed] [Google Scholar]
- 34.Gunasekara CM, Moynihan K, Sudhakar A, Sunil GS, Kotayil BP, Bayya PR, et al. Neonatal cardiac surgery in low resource settings: Implications of birth weight. Arch Dis Child. 2020;105:1140–5. doi: 10.1136/archdischild-2020-319161. [DOI] [PubMed] [Google Scholar]
- 35.Colaco SM, Karande T, Bobhate PR, Jiyani R, Rao SG, Kulkarni S. Neonates with critical congenital heart defects: Impact of fetal diagnosis on immediate and short-term outcomes. Ann Pediatr Cardiol. 2017;10:126–30. doi: 10.4103/apc.APC_125_16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Shakya S, Saxena A, Gulati S, Kothari SS, Ramakrishnan S, Gupta SK, et al. Neurodevelopmental outcomes in children with cyanotic congenital heart disease following open heart surgery. Ann Pediatr Cardiol. 2022;15:4–12. doi: 10.4103/apc.apc_149_21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Sharma R, Choudhary SK, Mohan MR, Padma MV, Jain S, Bhardwaj M, et al. Neurological evaluation and intelligence testing in the child with operated congenital heart disease. Ann Thorac Surg. 2000;70:575–81. doi: 10.1016/s0003-4975(00)01397-7. [DOI] [PubMed] [Google Scholar]
- 38.Padhy K, Satyanarayana P, Maharaj TM, Magatapalli K, Babu TK, Swain AK, et al. Normothermic CPB in congenital heart disease – An experience of 653 cases. Indian J Thorac Cardiovasc Surg. 2010;26:235–8. [Google Scholar]
- 39.Talwar S, Bhoje A, Khadagawat R, Chaturvedi P, Sreenivas V, Makhija N, et al. Oral thyroxin supplementation in infants undergoing cardiac surgery: A double-blind placebo-controlled randomized clinical trial. J Thorac Cardiovasc Surg. 2018;156:1209–17.e3. doi: 10.1016/j.jtcvs.2018.05.044. [DOI] [PubMed] [Google Scholar]
- 40.Singh D, Sahu MK, Singh SP, Singh U, Choudhary S, Pandey S. Outcome of ventilator-associated pneumonia in children post cardiac surgery: A prospective observational study. J Card Crit Care TSS. 2022;6:033–9. [Google Scholar]
- 41.Changlani TD, Jose A, Sudhakar A, Rojal R, Kunjikutty R, Vaidyanathan B. Outcomes of infants with prenatally diagnosed congenital heart disease delivered in a tertiary-care pediatric cardiac facility. Indian Pediatr. 2015;52:852–6. doi: 10.1007/s13312-015-0731-x. [DOI] [PubMed] [Google Scholar]
- 42.Shinde S, Golam K, Kumar P, Patil N, Sadacharan K. Perioperative blood lactate levels, pyruvate levels, and lactate-pyruvate ratio in children undergoing cardiopulmonary bypass for congenital heart disease. Indian J Crit Care Med. 2005;9:145–50. [Google Scholar]
- 43.Joshi SS, Anthony G, Manasa D, Ashwini T, Jagadeesh AM, Borde DP, et al. Predicting mortality after congenital heart surgeries: Evaluation of the Aristotle and risk adjustement in congenital heart surgery-1 risk prediction scoring systems: A retrospective single center analysis of 1150 patients. Ann Card Anaesth. 2014;17:266–70. doi: 10.4103/0971-9784.142057. [DOI] [PubMed] [Google Scholar]
- 44.Alam S, Shalini A, Hegde RG, Mazahir R, Jain A. Predictors and outcome of early extubation in infants postcardiac surgery: A single-center observational study. Ann Card Anaesth. 2018;21:402–6. doi: 10.4103/aca.ACA_209_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Vijayaraghavan A, Sudhakar A, Sundaram KR, Kumar RK, Vaidyanathan B. Prenatal diagnosis and planned peri-partum care as a strategy to improve pre-operative status in neonates with critical CHDs in low-resource settings: A prospective study. Cardiol Young. 2019;29:1481–8. doi: 10.1017/S104795111900252X. [DOI] [PubMed] [Google Scholar]
- 46.Reddy NS, Kappanayil M, Balachandran R, Jenkins KJ, Sudhakar A, Sunil GS, et al. Preoperative determinants of outcomes of infant heart surgery in a limited-resource setting. Semin Thorac Cardiovasc Surg. 2015;27:331–8. doi: 10.1053/j.semtcvs.2015.09.008. [DOI] [PubMed] [Google Scholar]
- 47.Murthy KS, Rao SG, Prakash KS, Robert C, Dhinakar S, Cherian KM. Role of inhaled nitric oxide as a selective pulmonary vasodilator in pediatric cardiac surgical practice. Indian J Pediatr. 1999;66:357–61. doi: 10.1007/BF02845523. [DOI] [PubMed] [Google Scholar]
- 48.Lal PS, Chavan B, Devendran VR, Varghese R, Murmu UC, Kumar RS. Surgical outcome of congenital heart disease in Down's syndrome. Asian Cardiovasc Thorac Ann. 2013;21:166–9. doi: 10.1177/0218492312450701. [DOI] [PubMed] [Google Scholar]
- 49.Kumar M, Sharma R, Sethi SK, Bazaz S, Sharma P, Bhan A, et al. Vasoactive inotrope score as a tool for clinical care in children post cardiac surgery. Indian J Crit Care Med. 2014;18:653–8. doi: 10.4103/0972-5229.142174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.George A, Jagannath P, Joshi SS, Jagadeesh AM. Weight-for-age standard score – Distribution and effect on in-hospital mortality: A retrospective analysis in pediatric cardiac surgery. Ann Card Anaesth. 2015;18:367–72. doi: 10.4103/0971-9784.159807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Kuthiroly S. 7th World congress of pediatric cardiology and cardiac surgery. Cardiol Young. 2017;27:S225. doi: 10.1017/S1047951117002219. [DOI] [PubMed] [Google Scholar]
- 52.Parvathy U, Balakrishnan KR, Ranjith MS, Saldanha R, Sai S, Vakamudi M. Surgical experience with congenital heart disease in Down's syndrome. Indian Heart J. 2000;52:438–41. [PubMed] [Google Scholar]
- 53.Kumar J, Agarwal S, Hegde R, Rao S, John C, Reddy C, et al. Extracorporeal membrane oxygenation in postoperative pediatric cardiac surgical cases. Indian Heart J. 2009;61:55–7. [PubMed] [Google Scholar]
- 54.Kapadia N, Russo P, Kumar S, Venkatesh B, Kumar R, Kapadia S, et al. Fast tracking pediatric cardiac surgery in a moderate sized program. Interactive Interact Cardiovasc Thorac Surg. 2010;10:561. [Google Scholar]
- 55.Balachandran R, Kappanayil M, Sen AC, Sudhakar A, Nair SG, Sunil GS, et al. Impact of the international quality improvement collaborative on outcomes after congenital heart surgery: A single center experience in a developing economy. Ann Card Anaesth. 2015;18:52–7. doi: 10.4103/0971-9784.148322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Alam S, Shalini A, Hegde RG, Mazahir R, Jain A. A comparative study of the risk stratification models for pediatric cardiac surgery. Egypt J Crit Care Med. 2018;6:5–8. [Google Scholar]
- 57.Mishra A, Shah R, Desai M, Chourasiya A, Patel H, Oswal N, et al. A simple surgical technique for closure of apical muscular ventricular septal defect. J Thorac Cardiovasc Surg. 2014;148:2576–9. doi: 10.1016/j.jtcvs.2014.02.036. [DOI] [PubMed] [Google Scholar]
- 58.Patel R, Thingnam SK, Mishra AK, Rohit MK, Upadhyay V, Halder V, et al. Benefits of perioperative sildenafil therapy in children with a ventricular septal defect with pulmonary artery hypertension on early surgical outcomes. J Card Surg. 2020;35:3302–9. doi: 10.1111/jocs.15030. [DOI] [PubMed] [Google Scholar]
- 59.Sridhar A, Subramanyan R, Lakshmi N, Farzana F, Tripathi RR, Premsekar R, et al. Do preoperative haemodynamic data and reactivity test predict the postoperative reversibility of pulmonary arterial hypertension in patients with large ventricular septal defect and borderline operability? Heart Asia. 2013;5:182–7. doi: 10.1136/heartasia-2013-010309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Sharma VK, Joshi S, Joshi A, Kumar G, Arora H, Garg A. Does intravenous sildenafil clinically ameliorate pulmonary hypertension during perioperative management of congenital heart diseases in children? – A prospective randomized study. Ann Card Anaesth. 2015;18:510–6. doi: 10.4103/0971-9784.166457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Vaidyanathan B, Roth SJ, Rao SG, Gauvreau K, Shivaprakasha K, Kumar RK. Outcome of ventricular septal defect repair in a developing country. J Pediatr. 2002;140:736–41. doi: 10.1067/mpd.2002.124304. [DOI] [PubMed] [Google Scholar]
- 62.Walavalkar V, Evers E, Pujar S, Viralam K, Maiya S, Frerich S, et al. Preoperative sildenafil administration in children undergoing cardiac surgery: A randomized controlled preconditioning study. Eur J Cardiothorac Surg. 2016;49:1403–10. doi: 10.1093/ejcts/ezv353. [DOI] [PubMed] [Google Scholar]
- 63.Walian A, Kohli JK, Magoon R, Kashav RC, Shri I, Dey S, et al. Retrospective evaluation of platelet-leukocyte indices and cardiac surgical outcomes in acyanotic heart disease patients with pulmonary hypertension (REPLICA-PH) Braz J Cardiovasc Surg. 2022;37:866–74. doi: 10.21470/1678-9741-2020-0648. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Shetty V, Shetty D, Punnen J, Chattuparambil B, Whitlock R, Bohra D. Single-stage repair for multiple muscular septal defects: A single-centre experience across 16 years. Interact Cardiovasc Thorac Surg. 2017;25:422–6. doi: 10.1093/icvts/ivx105. [DOI] [PubMed] [Google Scholar]
- 65.Naik AV, Salvi P, Mhatre A, Soomar SM, Joshi S. Aortopulmonary window: A single institution surgical experience. Asian Cardiovasc Thorac Ann. 2014;22:272–5. doi: 10.1177/0218492313481222. [DOI] [PubMed] [Google Scholar]
- 66.Talwar S, Agarwal P, Choudhary SK, Kothari SS, Juneja R, Saxena A, et al. Aortopulmonary window: Morphology, diagnosis, and long-term results. J Card Surg. 2017;32:138–44. doi: 10.1111/jocs.12936. [DOI] [PubMed] [Google Scholar]
- 67.Talwar S, Siddharth B, Gupta SK, Choudhary SK, Kothari SS, Juneja R, et al. Aortopulmonary window: Results of repair beyond infancy. Interact Cardiovasc Thorac Surg. 2017;25:740–4. doi: 10.1093/icvts/ivx158. [DOI] [PubMed] [Google Scholar]
- 68.Bhan A, Gupta M, Abraham S, Sharma R, Kothari SS, Juneja R. Surgical experience of aortopulmonary window repair in infants. Interact Cardiovasc Thorac Surg. 2007;6:200–3. doi: 10.1510/icvts.2006.138503. [DOI] [PubMed] [Google Scholar]
- 69.Reddy C, Kaskar A, Karthick E, Siddaiah S, Kiran VS, Suresh P. Surgical management of aortopulmonary window and its associated cardiac lesions. World J Pediatr Congenit Heart Surg. 2022;13:334–40. doi: 10.1177/21501351221077888. [DOI] [PubMed] [Google Scholar]
- 70.Gowda D, Gajjar T, Rao JN, Chavali P, Sirohi A, Pandarinathan N, et al. Surgical management of aortopulmonary window: 24 years of experience and lessons learned. Interact Cardiovasc Thorac Surg. 2017;25:302–9. doi: 10.1093/icvts/ivx099. [DOI] [PubMed] [Google Scholar]
- 71.Kumar V, Singh RS, Thingnam SK, Mishra AK, Jaswal V. Surgical outcome in aortopulmonary window beyond the neonatal period. J Card Surg. 2019;34:300–4. doi: 10.1111/jocs.14023. [DOI] [PubMed] [Google Scholar]
- 72.Dharmapuram AK, Ramadoss N, Verma S, Vejendla G, Ivatury RM. Early outcomes of modification of end to side repair of coarctation of aorta with arch hypoplasia in neonates and infants. Ann Pediatr Cardiol. 2018;11:267–74. doi: 10.4103/apc.APC_5_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Sen S, Garg S, Rao SG, Kulkarni S. Native aortic coarctation in neonates and infants: Immediate and midterm outcomes with balloon angioplasty and surgery. Ann Pediatr Cardiol. 2018;11:261–6. doi: 10.4103/apc.APC_165_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Dutta N, Ghosh R, Awasthy N, Girotra S, Radhakrishnan S, Shrivastava S, et al. Off-pump midline repair of coarctation of aorta when associated with intracardiac defects: An alternate approach for single-stage correction. Eur J Cardiothorac Surg. 2016;50:1089–95. doi: 10.1093/ejcts/ezw260. [DOI] [PubMed] [Google Scholar]
- 75.Murthy KS, Coelho R, Roy C, Kulkarni S, Ninan B, Cherian KM. One-stage repair of cardiac and arch anomalies without circulatory arrest. Asian Cardiovasc Thorac Ann. 2003;11:250–4. doi: 10.1177/021849230301100315. [DOI] [PubMed] [Google Scholar]
- 76.Patwary ME, Khan MS, Marwah A, Singh V, Shekhawat S, Sharma R. Arterial switch for transposition of the great arteries with large ventricular septal defect and for Taussig Bing anomaly: Experience from a tertiary care center in the developing world. World J Pediatr Congenit Heart Surg. 2015;6:413–21. doi: 10.1177/2150135115593128. [DOI] [PubMed] [Google Scholar]
- 77.Talwar S, Kumar MV, Bhoje A, Choudhary SK, Kothari SS, Juneja R, et al. Atrial switch procedure in children more than 5 years of age: Mid-term results. Interact Cardiovasc Thorac Surg. 2016;23:694–8. doi: 10.1093/icvts/ivw189. [DOI] [PubMed] [Google Scholar]
- 78.Ramanan S, Sundaram S, Gopalakrishnan A, Anija DV, Sandhya P, Jose DS, et al. Intermediate-term neurodevelopmental outcomes and quality of life after arterial switch operation beyond early neonatal period. Eur J Cardiothorac Surg. 2021;60:1428–36. doi: 10.1093/ejcts/ezab223. [DOI] [PubMed] [Google Scholar]
- 79.Sharma R, Choudhary SK, Bhan A, Kumar RP, Juneja R, Kothari SS, et al. Late outcome after arterial switch operation for complete transposition of great arteries with left ventricular outflow tract obstruction. Ann Thorac Surg. 2002;74:1986–91. doi: 10.1016/s0003-4975(02)04078-x. [DOI] [PubMed] [Google Scholar]
- 80.Bisoi AK, Ahmed T, Malankar DP, Chauhan S, Das S, Sharma P, et al. Midterm outcome of primary arterial switch operation beyond six weeks of life in children with transposition of great arteries and intact ventricular septum. World J Pediatr Congenit Heart Surg. 2014;5:219–25. doi: 10.1177/2150135113515487. [DOI] [PubMed] [Google Scholar]
- 81.Kunde F, Thomas S, Sudhakar A, Kunjikutty R, Kumar RK, Vaidyanathan B. Prenatal diagnosis and planned peripartum care improve perinatal outcome of fetuses with transposition of the great arteries and intact ventricular septum in low-resource settings. Ultrasound Obstet Gynecol. 2021;58:398–404. doi: 10.1002/uog.23146. [DOI] [PubMed] [Google Scholar]
- 82.Bisoi AK, Sharma P, Chauhan S, Reddy SM, Das S, Saxena A, et al. Primary arterial switch operation in children presenting late with d-transposition of great arteries and intact ventricular septum. When is it too late for a primary arterial switch operation? Eur J Cardiothorac Surg. 2010;38:707–13. doi: 10.1016/j.ejcts.2010.03.037. [DOI] [PubMed] [Google Scholar]
- 83.Sharma R, Bhan A, Nautiyal A, Mittal A, Akole R, Malhotra N, et al. Renal outcomes in neonates and infants with transposition physiology undergoing arterial switch procedure. Pediatr Cardiol. 2022;43:1770–83. doi: 10.1007/s00246-022-02914-z. [DOI] [PubMed] [Google Scholar]
- 84.Mishra A, Jain A, Hinduja M, Wadhawa V, Patel R, Vaidhya N, et al. Transposition of great arteries with intramural coronary artery: Experience with a modified surgical technique. Braz J Cardiovasc Surg. 2016;31:15–21. doi: 10.5935/1678-9741.20160003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Tailor KB, Dharmani KH, Kadam SV, Kattana HB, Rao SG. A single center, retrospective analysis of total anomalous pulmonary venous connection repair early outcome at a tertiary care center in India. Ann Card Anaesth. 2021;24:333–8. doi: 10.4103/aca.ACA_123_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Chowdhury U. Adjustable vertical vein ligation in supracardiac totally anomalous pulmonary venous connection: A clinical report of 99 patients. Clin Cardiol Cardiovasc Interv. 2020;3:2641–0419. [Google Scholar]
- 87.Chowdhury UK, Airan B, Malhotra A, Bisoi AK, Saxena A, Kothari SS, et al. Mixed total anomalous pulmonary venous connection: Anatomic variations, surgical approach, techniques, and results. J Thorac Cardiovasc Surg. 2008;135:106–16. doi: 10.1016/j.jtcvs.2007.08.028. [DOI] [PubMed] [Google Scholar]
- 88.Chowdhury UK, Subramaniam KG, Joshi K, Varshney S, Kumar G, Singh R, et al. Rechanneling of total anomalous pulmonary venous connection with or without vertical vein ligation: Results and guidelines for candidate selection. J Thorac Cardiovasc Surg. 2007;133:1286–94.e4. doi: 10.1016/j.jtcvs.2006.08.010. [DOI] [PubMed] [Google Scholar]
- 89.Choudhary SK, Bhan A, Sharma R, Mathur A, Airan B, Saxena A, et al. Repair of total anomalous pulmonary venous connection in infancy: Experience from a developing country. Ann Thorac Surg. 1999;68:155–9. doi: 10.1016/s0003-4975(99)00375-6. [DOI] [PubMed] [Google Scholar]
- 90.Reddy KP, Nagarajan R, Rani U, Prasad S, Chakravarthy S, Rao IM, et al. Total anomalous pulmonary venous connection beyond infancy. Asian Cardiovasc Thorac Ann. 2011;19:249–52. doi: 10.1177/0218492311409570. [DOI] [PubMed] [Google Scholar]
- 91.Talwar S, Arora Y, Gupta SK, Kothari SS, Ramakrishnan S, Saxena A, et al. Total anomalous pulmonary venous connection beyond the first decade of life. World J Pediatr Congenit Heart Surg. 2019;10:185–91. doi: 10.1177/2150135118822792. [DOI] [PubMed] [Google Scholar]
- 92.Bayya PR, Varghese S, Jayashankar JP, Sudhakar A, Balachandran R, Kottayil BP, et al. Total anomalous pulmonary venous connection repair: Single-center outcomes in a lower-middle income region. World J Pediatr Congenit Heart Surg. 2022;13:458–65. doi: 10.1177/21501351221103492. [DOI] [PubMed] [Google Scholar]
- 93.Katewa A, Sahu B, Prabhu A, Haranal M. Total anomalous pulmonary venous connection with another major congenital cardiac defect in biventricular hearts. Asian Cardiovasc Thorac Ann. 2023;31:97–101. doi: 10.1177/02184923221142378. [DOI] [PubMed] [Google Scholar]
- 94.Choudhary SK, Bhan A, Sharma R, Airan B, Devagourou V, Saxena A, et al. Total anomalous pulmonary venous connection: Surgical experience in Indians. Indian Heart J. 2001;53:754–60. [PubMed] [Google Scholar]
- 95.Damodaran S, Ganesan R, Munirathinam G, Puri G. Early surgical outcome of pediatric tetrology of fallot surgery in indian population;a single centre analysis. Cardiology in the Young. 2017;27:192. [Google Scholar]
- 96.Talwar S, Meena A, Choudhary SK, Kothari SS, Gupta SK, Saxena A, et al. Anomalous branch of pulmonary artery from the aorta and tetralogy of fallot: Morphology, surgical techniques and results. Eur J Cardiothorac Surg. 2014;46:291–6. doi: 10.1093/ejcts/ezt632. [DOI] [PubMed] [Google Scholar]
- 97.Kapoor PM, Subramanian A, Malik V, Kiran U, Velayoudham D. B-type natriuretic peptide as prognostic marker in tetralogy of fallot surgery. Asian Cardiovasc Thorac Ann. 2015;23:146–52. doi: 10.1177/0218492314534247. [DOI] [PubMed] [Google Scholar]
- 98.Talwar S, Chatterjee S, Sreenivas V, Makhija N, Kapoor PM, Choudhary SK, et al. Comparison of del Nido and histidine-tryptophan-ketoglutarate cardioplegia solutions in pediatric patients undergoing open heart surgery: A prospective randomized clinical trial. J Thorac Cardiovasc Surg. 2019;157:1182–92.e1. doi: 10.1016/j.jtcvs.2018.09.140. [DOI] [PubMed] [Google Scholar]
- 99.Sasikumar D, Sasidharan B, Tharakan JA, Dharan BS, Mathew T, Karunakaran J. Early and 1-year outcome and predictors of adverse outcome following monocusp pulmonary valve reconstruction for patients with tetralogy of fallot: A prospective observational study. Ann Pediatr Cardiol. 2014;7:5–12. doi: 10.4103/0974-2069.126538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Dharmapuram AK, Ramadoss N, Goutami V, Verma S, Pande S, Devalaraja S. Early experience with surgical strategies aimed at preserving the pulmonary valve and annulus during repair of tetralogy of fallot. Ann Pediatr Cardiol. 2021;14:315–22. doi: 10.4103/apc.APC_166_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Talwar S, Divya A, Choudhary SK, Gupta SK, Ramakriahnan S, Kothari SS, et al. Mid-term results of correction of tetralogy of fallot with absent pulmonary valve. Indian Heart J. 2017;69:767–71. doi: 10.1016/j.ihj.2017.04.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Raja J, Menon S, Sameer Mohammed, Ramanan S, Baruah SD, Gopalakrishnan A, et al. Midterm results of homografts in pulmonary position: A retrospective single-center study. Indian J Thorac Cardiovasc Surg. 2021;37:129–37. doi: 10.1007/s12055-020-01065-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Raj R, Puri GD, Jayant A, Thingnam SK, Singh RS, Rohit MK. Perioperative echocardiography-derived right ventricle function parameters and early outcomes after tetralogy of fallot repair in mid-childhood: A single-center, prospective observational study. Echocardiography. 2016;33:1710–7. doi: 10.1111/echo.13333. [DOI] [PubMed] [Google Scholar]
- 104.Kapoor PM, Subramanian A, Malik V, Devagorou V. Perioperative endothelin levels in patients undergoing intracardiac repair for tetralogy of fallot. J Card Surg. 2014;29:670–7. doi: 10.1111/jocs.12394. [DOI] [PubMed] [Google Scholar]
- 105.Dharmapuram A, Ramadoss N, Verma S, Gouthami V, Rao I. Preliminary experience with the use of an extracellular matrix to augment the native pulmonary valve during repair of tetralogy of fallot. World J Pediatr Congenit Heart Surg. 2017;8:174–81. doi: 10.1177/2150135116682450. [DOI] [PubMed] [Google Scholar]
- 106.Sasikumar N, Ramanan S, Rema KM, Kumar RS, Subramanyan R, Cherian KM. Prosthetic reconstruction of bicuspid pulmonary valve in tetralogy of fallot. Asian Cardiovasc Thorac Ann. 2014;22:436–41. doi: 10.1177/0218492313496416. [DOI] [PubMed] [Google Scholar]
- 107.Wankhade PR, Aggarwal N, Joshi RK, Agarwal M, Joshi R, Mehta A, et al. Short-term clinical and echocardiographic outcomes after use of polytetrafluoroethylene bicuspid pulmonary valve during the repair of tetralogy of fallot. Ann Pediatr Cardiol. 2019;12:25–31. doi: 10.4103/apc.APC_51_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Kaushal SK, Radhakrishanan S, Dagar KS, Iyer PU, Girotra S, Shrivastava S, et al. Significant intraoperative right ventricular outflow gradients after repair for tetralogy of fallot: To revise or not to revise? Ann Thorac Surg. 1999;68:1705–12. doi: 10.1016/s0003-4975(99)01069-3. [DOI] [PubMed] [Google Scholar]
- 109.Ladha S, Kapoor PM, Singh SP, Kiran U, Chowdhury UK. The role of blood lactate clearance as a predictor of mortality in children undergoing surgery for tetralogy of fallot. Ann Card Anaesth. 2016;19:217–24. doi: 10.4103/0971-9784.179589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Airan B, Choudhary SK, Kumar HV, Talwar S, Dhareshwar J, Juneja R, et al. Total transatrial correction of tetralogy of fallot: No outflow patch technique. Ann Thorac Surg. 2006;82:1316–21. doi: 10.1016/j.athoracsur.2006.03.115. [DOI] [PubMed] [Google Scholar]
- 111.Chowdhury UK, Airan B, Kumar AS, Sharma R, Bhan A, Kothari SS, et al. Management of tetralogy of fallot with absent pulmonary valve: Early and mid-term results of a uniform approach. Indian Heart J. 2000;52:54–9. [PubMed] [Google Scholar]
- 112.Haribabu, Kumar B, Asha KR. To study the efficacy of right ventricular isovolumic acceleration by 2D-echo in evaluating post operative outcomes in tetrology of fallot. Indian Heart J. 2014;66:S56. [Google Scholar]
- 113.Choudhary SK, Talwar S, Airan B, Mohapatra R, Juneja R, Kothari SS, et al. A new technique of percutaneously adjustable pulmonary artery banding. J Thorac Cardiovasc Surg. 2006;131:621–4. doi: 10.1016/j.jtcvs.2005.10.037. [DOI] [PubMed] [Google Scholar]
- 114.Talwar S, Choudhary SK, Mathur A, Airan B, Singh R, Juneja R, et al. Changing outcomes of pulmonary artery banding with the percutaneously adjustable pulmonary artery band. Ann Thorac Surg. 2008;85:593–8. doi: 10.1016/j.athoracsur.2007.07.057. [DOI] [PubMed] [Google Scholar]
- 115.Talwar S, Kamat NA, Choudhary SK, Ramakrishnan S, Saxena A, Juneja R, et al. Mid-term outcomes of patients undergoing adjustable pulmonary artery banding. Indian Heart J. 2016;68:72–6. doi: 10.1016/j.ihj.2015.06.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Sasikumar N, Ramanan S, Rema KM, Subramanyan R, Kumar RS, Cherian KM. Pulmonary artery banding for univentricular heart beyond the neonatal period. Asian Cardiovasc Thorac Ann. 2014;22:660–6. doi: 10.1177/0218492313503640. [DOI] [PubMed] [Google Scholar]
- 117.Chowdhury UK, Venugopal P, Kothari SS, Saxena A, Talwar S, Subramaniam G, et al. Criterions for selection of patients for, and results of, a new technique for construction of the modified Blalock-Taussig shunt. Cardiol Young. 2006;16:463–73. doi: 10.1017/S1047951106000631. [DOI] [PubMed] [Google Scholar]
- 118.Sahoo TK, Chauhan S, Sahu M, Bisoi A, Kiran U. Effects of hemodilution on outcome after modified Blalock-Taussig shunt operation in children with cyanotic congenital heart disease. J Cardiothorac Vasc Anesth. 2007;21:179–83. doi: 10.1053/j.jvca.2006.01.029. [DOI] [PubMed] [Google Scholar]
- 119.Singh SP, Chauhan S, Choudhury M, Malik V, Talwar S, Hote MP, et al. Modified Blalock Taussig shunt: Comparison between neonates, infants and older children. Ann Card Anaesth. 2014;17:191–7. doi: 10.4103/0971-9784.135847. [DOI] [PubMed] [Google Scholar]
- 120.Rao MS, Bhan A, Talwar S, Sharma R, Choudhary SK, Airan B, et al. Modified Blalock-Taussig shunt in neonates: Determinants of immediate outcome. Asian Cardiovasc Thorac Ann. 2000;8:339–43. [Google Scholar]
- 121.Swain SK, Dharmapuram AK, Reddy P, Ramdoss N, Raghavan SS, Kona SM. Neonatal Blalock-Taussig shunt: Technical aspects and postoperative management. Asian Cardiovasc Thorac Ann. 2008;16:7–10. doi: 10.1177/021849230801600103. [DOI] [PubMed] [Google Scholar]
- 122.Kandakure PR, Dharmapuram AK, Ramadoss N, Babu V, Rao IM, Murthy KS. Sternotomy approach for modified Blalock-Taussig shunt: Is it a safe option? Asian Cardiovasc Thorac Ann. 2010;18:368–72. doi: 10.1177/0218492310375856. [DOI] [PubMed] [Google Scholar]
- 123.Naik RB, Srivastava CP, Arsiwala S, Mathur A, Sharma S. Early outcomes after the on pump bidirectional Glenn procedure: A single center experience. J Card Surg. 2021;36:3207–14. doi: 10.1111/jocs.15719. [DOI] [PubMed] [Google Scholar]
- 124.Talwar S, Sandup T, Gupta S, Ramakrishnan S, Kothari SS, Saxena A, et al. Factors determining early outcomes after the bidirectional superior cavopulmonary anastomosis. Indian J Thorac Cardiovasc Surg. 2018;34:457–67. doi: 10.1007/s12055-017-0571-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Chowdhury UK, Airan B, Sharma R, Bhan A, Kothari SS, Saxena A, et al. One and a half ventricle repair with pulsatile bidirectional Glenn: Results and guidelines for patient selection. Ann Thorac Surg. 2001;71:1995–2002. doi: 10.1016/s0003-4975(01)02517-6. [DOI] [PubMed] [Google Scholar]
- 126.Hussain ST, Bhan A, Sapra S, Juneja R, Das S, Sharma S. The bidirectional cavopulmonary (Glenn) shunt without cardiopulmonary bypass: Is it a safe option? Interact Cardiovasc Thorac Surg. 2007;6:77–82. doi: 10.1510/icvts.2006.133710. [DOI] [PubMed] [Google Scholar]
- 127.Kandakure PR, Dharmapuram AK, Kale SB, Babu V, Ramadoss N, Shastri R, et al. Veno-venous shunt-assisted cavopulmonary anastomosis. Ann Pediatr Cardiol. 2010;3:8–11. doi: 10.4103/0974-2069.64361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Kandakure PR, Dharmapuram AK, Kale SB, Babu V, Ramadoss N, Rao IM, et al. Venoatrial shunt-assisted cavopulmonary anastomosis. Asian Cardiovasc Thorac Ann. 2010;18:569–73. doi: 10.1177/0218492310388459. [DOI] [PubMed] [Google Scholar]
- 129.Talwar S, Divya A, Makhija N, Choudhary SK, Airan B. Immediate and early post-operative sequelae of off-pump total cavopulmonary connection. Indian J Thorac Cardiovasc Surg. 2018;34:468–75. doi: 10.1007/s12055-017-0638-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Talwar S, Singh S, Sreenivas V, Kapoor KS, Gupta SK, Ramakrishnan S, et al. Outcomes of patients undergoing primary fontan operation beyond first decade of life. World J Pediatr Congenit Heart Surg. 2017;8:487–94. doi: 10.1177/2150135117713696. [DOI] [PubMed] [Google Scholar]
- 131.Chowdhury UK, Airan B, Kothari SS, Talwar S, Saxena A, Singh R, et al. Specific issues after extracardiac fontan operation: Ventricular function, growth potential, arrhythmia, and thromboembolism. Ann Thorac Surg. 2005;80:665–72. doi: 10.1016/j.athoracsur.2005.02.024. [DOI] [PubMed] [Google Scholar]
- 132.Mohanty SR, Airan B, Bhan A, Sharma R, Kumar AS, Kothari SS, et al. Adult cyanotic congenital heart disease: surgical experience. Indian Heart J. 1999;51:186–92. [PubMed] [Google Scholar]
- 133.Ramanan S, Sasikumar N, Manohar K, Ramani SS, Kumar RS, Agarwal R, et al. Adult tetralogy repair: Factors affecting early outcome in the current era. Asian Cardiovasc Thorac Ann. 2019;27:731–7. doi: 10.1177/0218492319882870. [DOI] [PubMed] [Google Scholar]
- 134.Aggarwal SK, Mishra J, Sai V, Iyer VR, Panicker BK. Aortopulmonary window in adults: Diagnosis and treatment of late-presenting patients. Congenit Heart Dis. 2008;3:341–6. doi: 10.1111/j.1747-0803.2008.00210.x. [DOI] [PubMed] [Google Scholar]
- 135.Talwar S, Kumar MV, Sreenivas V, Choudhary SK, Sahu M, Airan B. Factors determining outcomes in grown up patients operated for congenital heart diseases. Ann Pediatr Cardiol. 2016;9:222–8. doi: 10.4103/0974-2069.189113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Talwar S, Ahmed T, Saxena A, Kothari SS, Juneja R, Airan B. Morphology, surgical techniques, and outcomes in patients above 15 years undergoing surgery for congenitally corrected transposition of great arteries. World J Pediatr Congenit Heart Surg. 2013;4:271–7. doi: 10.1177/2150135113476717. [DOI] [PubMed] [Google Scholar]
- 137.Gnanappa GK, Ganigara M, Prabhu A, Varma SK, Murmu U, Varghese R, et al. Outcome of complex adult congenital heart surgery in the developing world. Congenit Heart Dis. 2011;6:2–8. doi: 10.1111/j.1747-0803.2010.00479.x. [DOI] [PubMed] [Google Scholar]
- 138.Talwar S, Meena A, Choudhary SK, Saxena A, Kothari SS, Juneja R, et al. Repair of tetralogy of fallot in or beyond the fourth decade of life. Congenit Heart Dis. 2014;9:424–32. doi: 10.1111/chd.12162. [DOI] [PubMed] [Google Scholar]
- 139.Kottayil BP, Dharan BS, Pillai VV, Panicker VT, Gopalakrishnan SK, Jayakumar K. Surgical repair of double-chambered right ventricle in adulthood. Asian Cardiovasc Thorac Ann. 2011;19:57–60. doi: 10.1177/0218492310395955. [DOI] [PubMed] [Google Scholar]
- 140.Bisoi AK, Murala JS, Airan B, Chowdhury UK, Kothari SS, Pal H, et al. Tetralogy of fallot in teenagers and adults: Surgical experience and follow-up. Gen Thorac Cardiovasc Surg. 2007;55:105–12. doi: 10.1007/s11748-006-0087-1. [DOI] [PubMed] [Google Scholar]
- 141.Talwar S, Choudhary SK, Reddy S, Saxena A, Kothari SS, Juneja R, et al. Total anomalous pulmonary venous drainage beyond childhood. Interact Cardiovasc Thorac Surg. 2008;7:1058–61. doi: 10.1510/icvts.2008.186734. [DOI] [PubMed] [Google Scholar]
- 142.Kumar R, Varghese R, Kumar G, Varma S, Vimala J, Selvakumar G, et al. Surgical outcome of major open heart surgery in adults with congenital heart disease. Cardiology in the Young. 2010;10:355. [Google Scholar]
- 143.Mohanty SR, Airan B, Bhan A, Sharma R, Kumar AS, Kothari SS, et al. Adult cyanotic congenital heart disease: Surgical experience. Indian Heart J. 1999;51:186–92. [PubMed] [Google Scholar]
- 144.Su Z, Zou Z, Hay SI, Liu Y, Li S, Chen H, et al. Global, regional, and national time trends in mortality for congenital heart disease, 1990-2019: An age-period-cohort analysis for the global burden of disease 2019 study. EClinicalMedicine. 2022;43:101249. doi: 10.1016/j.eclinm.2021.101249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Sivakumar K, Shivaprakasha K, Rao SG, Kumar RK. Operative outcome and intermediate term follow-up of neonatal Blalock-Taussig shunts. Indian Heart J. 2001;53:66–70. [PubMed] [Google Scholar]
- 146.Ramachandran P, Gopalan HS. Assessment of nutritional status in Indian preschool children using WHO 2006 growth standards. Indian J Med Res. 2011;134:47–53. [PMC free article] [PubMed] [Google Scholar]
- 147.Khadilkar VV, Khadilkar AV, Chiplonkar SA. Growth performance of affluent Indian preschool children: A comparison with the new WHO growth standard. Indian Pediatr. 2010;47:869–72. doi: 10.1007/s13312-010-0147-6. [DOI] [PubMed] [Google Scholar]
- 148.Sharma R, Bhan A, Choudhary SK, Kumar RP, Juneja R, Kothari SS, et al. Ten-year experience with the arterial switch operation. Indian Heart J. 2002;54:681–6. [PubMed] [Google Scholar]
- 149.Ramakrishnan S, Maheshwari S. Being a pediatric cardiologist in India – A clarion call. Ann Pediatr Cardiol. 2023;16:389–92. doi: 10.4103/apc.apc_62_24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Ramakrishnan S. Being a young pediatric cardiologist in India: Aspirations versus reality. Ann Pediatr Cardiol. 2023;16:163–7. doi: 10.4103/apc.apc_127_23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Tharakan JA, Sharma R, Subramanyan R, Saxena A, Kulkarni S, Relan J, et al. Being a pediatric cardiologist in India – In search of a holistic solution. Ann Pediatr Cardiol. 2023;16:448–54. doi: 10.4103/apc.apc_58_24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Faisal NV, Handa A, Ramakrishnan S. Pediatric cardiac procedures in India: Who bears the cost? Ann Pediatr Card. 2024;17:1–12. doi: 10.4103/apc.apc_67_24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Das D, Dutta N, Das S, Sharma MK, Chattopadhyay A, Ghosh S, et al. Public-private partnership for treatment of congenital heart diseases: Experiences from an Indian state. World J Pediatr Congenit Heart Surg. 2024 doi: 10.1177/21501351231215257. 21501351231215257. [DOI] [PubMed] [Google Scholar]
- 154.Jacobs JP, He X, Mayer JE, Jr, Austin EH, 3rd, Quintessenza JA, Karl TR, et al. Mortality trends in pediatric and congenital heart surgery: An analysis of the society of thoracic Surgeons congenital heart surgery database. Ann Thorac Surg. 2016;102:1345–52. doi: 10.1016/j.athoracsur.2016.01.071. [DOI] [PubMed] [Google Scholar]