Abstract
Exercise is an important physiological activity with several health benefits. In the setting of ischemic heart disease (IHD), the view toward exercise has greatly evolved throughout the years, concurrently to several major advances in the management of this complex entity. Currently, exercise training has broad applications across the IHD continuum as a powerful tool in its overall management, being a core component of comprehensive cardiac rehabilitation programs. Beyond this, exercise has also been incorporated as an integral part of contemporary methodologies aiming to provide diagnostic and prognostic data, such as cardiopulmonary exercise stress testing or stress echocardiography. In this article, we provide a pragmatic overview concerning the role of exercise in IHD, with a focus on its incorporation in cardiac rehabilitation frameworks, while also discussing some of the challenges and unmet needs concerning these interventions.
Keywords: cardiac rehabilitation, exercise, exercise training, ischemic heart disease, preventive cardiology
Introduction
Throughout the ages, physical exercise has played a key role in different civilizations, with its health impact being described across various settings.1 These range from the early depictions attributed to Sushruta in the Indus valley thousands of years ago, to reports from the Yellow river civilizations or those by physicians from ancient Greece such as Hippocrates and Heraclius.1-3 Interestingly, the notion that, in its prescription, factors related to the individual and general setting were to be considered also emerged early on.1,2
Cardiovascular disease is a major cause of morbidity and mortality.4,5 While encompassing a broad and complex group of pathologies, often having intricate links with other entities (such as cancer, autoimmune, or infectious disorders), ischemic heart disease (IHD) has been a particularly relevant health care burden.4-8 Although sometimes referred to as a “modern” disease, namely given the profound influence of lifestyle factors (including dietary patterns, tobacco exposure, or sedentarism) and ensuing cardiovascular risk factors in its expression, studies have progressively shown that this too may have been a challenge since ancient times.9,10 This is elegantly illustrated by data derived from the study of mummies from diverse world regions by computed tomography, showing atherosclerotic disease (in different vascular beds) already in these bygone eras.9
Over the past century, groundbreaking improvements have been made in IHD, across its continuum from acute presentations to chronic settings.11,12 These span its prevention, diagnosis, and treatment and have heralded major reductions in mortality while also greatly affecting morbidity.4,6,8 As detailed below, data have highlighted the importance of exercise in both the prevention and management of IHD.6,8,13 Indeed, exercise training has been incorporated as a core component of cardiac rehabilitation (CR) programs, one of the central strategies in the management of IHD as underscored by current guidelines.6,8,14,15 Furthermore, exercise has also been coupled with various tests (such as the electrocardiogram and echocardiogram), being used for both diagnostic and prognostic assessments (Fig. 1).14,16,17
Figure 1.
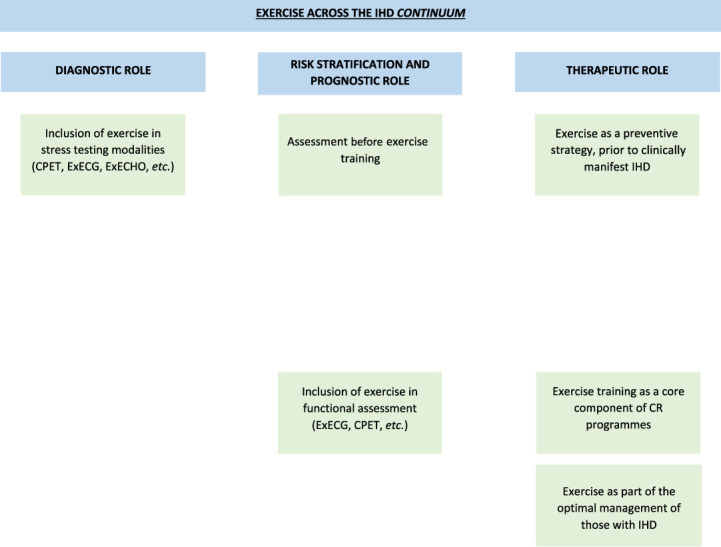
Overview of some of the potential applications of exercise across the continuum of ischemic heart disease. CPET, cardiopulmonary exercise stress testing; CR, cardiac rehabilitation; ExECG, exercise stress testing with electrocardiographic monitoring; ExECHO, exercise stress echocardiography; IHD, ischemic heart disease.
In this review, we present an overview concerning the role of exercise in IHD, while also pragmatically reviewing its incorporation in CR and briefly exploring some of the unmet needs and future challenges concerning these interventions.
A brief review concerning the interplay between exercise and the cardiovascular system
A plethora of pathways have been described when analyzing the benefits of exercise.13,18,19 Although beyond the scope of this article, having been previously extensively explored, different mechanisms have been linked to its positive effects.13,18-20 In this regard, not only effects specifically related to the cardiovascular system but also those in other systems have been under the spotlight.14,18,21,22 Among the former, both structural and functional adaptations (including some assessed by readily available noninvasive tests such as echocardiography and others needing ancillary methodologies to be fully ascertained) are a mainstay of the effects of exercise.14,23,24 These encompass not only the heart but also the peripheral vasculature, with improvements in cardiac contractility, chronotropic reserve, and endothelial function.18,20,21 For the latter, some effects include those elicited in the musculoskeletal system where the release of myokines can modulate the cardiovascular response, as well as in the respiratory and autonomic nervous systems, and overall metabolic response.13,14,21,22,25,26 These far-reaching effects resonate with the manifold components of physical fitness, while concurring with the benefits of exercise beyond cardiovascular disease, where its role has progressively garnered center stage in areas ranging from lung diseases (being incorporated in respiratory rehabilitation programs) to cancer.27-32 Moreover, its place at the intersection between cardiovascular disease and other pathologies should also be considered, as in chronic kidney disease.33,34
Notably, it should be emphasized that although cardiopulmonary function is a critical part of physical fitness, other determinants are also paramount to its overall expression.14 Importantly, data derived from frameworks such as cardiopulmonary exercise stress testing (CPET) can allow a dynamic assessment of several components of the response to exercise (providing relevant data in several scenarios).16,35 Moreover, methodologies such as invasive CPET or exercise magnetic resonance imaging have also been reported, further improving knowledge and perspectives on this complex and expanding field.36,37
Another point worthy of mention relates to the fact that, albeit associated with various benefits, there could also be deleterious effects related to exercise.38,39 Some of those reported range from phenomena such as elevated cardiac biomarkers or increased risk of atrial fibrillation (where long-term high-intensity endurance training has been associated with this arrhythmia, albeit the possible effects of sex, cardiovascular risk factors, and other factors should be considered, namely given that the mechanisms for this finding remain to be fully characterized), to potential adverse effects in terms of plaque remodeling or atherosclerotic burden.38-46 These reinforce the need for a careful risk stratification, particularly when considering exercise in individuals with IHD or at increased risk (including those with more advanced age or with a high cardiovascular risk undergoing high-intensity activities).14,47 Once more, when addressing exercise across the IHD continuum, an integrated view is of pivotal relevance.14
It should also be recalled that, although acknowledging areas of overlap, concepts concerning physical activity and exercise have specificities which should be noted.14,48 As detailed in the European Society of Cardiology (ESC) guidelines, exercise may be defined as physical activity which is structured and performed in a repetitive purposeful manner to maintain or improve one or more components of physical fitness.14 On the other hand, any bodily movement which results in energy expenditure and was produced by skeletal muscle could be within the scope of physical activity.14 These concepts are also relevant when analyzing the settings in which these take place, as data have shown that this may also affect the cardiovascular response.49-51 Some examples encompass changes in atmospheric conditions (such as temperature but also pollution) and differences between occupational and recreational activities, in terms of their cardiovascular profile.19,49-52
Exercise and ischemic heart disease
A journey from the armchair to contemporary guidelines
The interplay between exercise and IHD has been an evolving topic across timeframes.53-56 Although depictions suggesting angina pectoris were already mentioned in the Papyrus Ebers dating back millennia, as well as those of epicardial artery narrowing by renaissance master Leonardo Da Vinci, the portrayal of this entity would be greatly refined in the eighteenth century.57-59 At this point, William Heberden provided a seminal and (especially at a time when much of the pathophysiology of IHD was yet to be unraveled) remarkably eloquent description of the clinical features of angina pectoris, the prototypical manifestation of IHD.57 Of note, he also described an individual who improved his symptoms by exercising (in the case by sawing wood).53,56 Although the depiction of typical anginal symptoms has (with subsequent adaptations) to some extent stood the test of time, the case for exercise in IHD would still be a point of discussion.53,55,56,59
At the dawn of the twentieth century, prolonged bed rest and immobilization were the norm after a myocardial infarction.11,53,54,56 It should be recalled that at this time major leaps were being undertaken into the understanding of some of the mechanisms leading to myocardial infarction, spearheaded by James Herrick's now classical depiction of coronary thrombosis.11,54,60 These initial insights (such as the emphasis on the development of scar tissue), however, coupled with the lack of effective and widespread therapeutic interventions, lead to a restrictive view in terms of exercise (and “stress” in general as recalled years later by Eugene Braunwald, recollecting on what could be described as an “expectant” phase in the management of myocardial infarction).11,56 Nonetheless, already at this time the value of long bed rest periods, as well as their potential adverse effects, would be put into question.54,55 During the first half of the past century, pioneering works such as those by Samuel Levine (who in 1944 expressed several concerns regarding these strict regimens, illustrated by clinical cases) paved the way, in many respects, to deep paradigm shifts in rehabilitation strategies.53,55,61 Among these a special mention should be given to the so-called “armchair” treatment (also recalled as the “cardiac chair treatment”), an approach in which patients were sited with feet dependent early on in their clinical course.54,62 Albeit extraordinarily simple and plain by current standards, this innovation proved central in ushering in an era of early mobilization and rehabilitation.54-56,63 Concurrently to these developments, some the first CR programs were being introduced, a milestone which would profoundly affect the care of myocardial infarction survivors (and several other cardiovascular diseases).64-66 As previously alluded to, when assessing exercise in IHD, careful considerations should be made in terms of the overall context in which it is inserted. In this background, it should be recalled that several strategies, nowadays commonplace, were yet to be developed and generalized, as illustrated by the (at the time) much publicized management of US president Eisenhower's myocardial infarction.56,67
Since the inception of the first CR programs, exercise has been a core component of these interventions.68,69 Although the management of IHD has remarkably evolved (to name a few, with the advent of coronary care units, revascularization strategies including percutaneous coronary intervention, and a myriad of pharmacological agents), CR has along this journey continuously shown its relevance.55,70,71 In this regard, meta-analyses have shown the benefits of CR across several time points and profiles.71,72 Although care should be taken when analyzing and interpreting different studies (namely given the differences in design or patient characteristics), these are reinforced by an updated meta-analysis reporting on the benefits of CR in cardiovascular mortality and recurrent myocardial infarction and hospitalizations.69,72-75 These data have led to the incorporation of CR at the center of IHD management, as illustrated by the high levels of recommendation provided in guidelines by different societies such as the ESC and the American College of Cardiology/American Heart Association (both endorsing CR as a class I, level A recommendation in these settings).6,8,15,76 Of note, these programs can be of interest in a range of patient characteristics.77-81 Albeit different responses have been reported across populations under study, the potential benefits of these interventions reinforce their usefulness.79,80,82-84
Cardiac rehabilitation frameworks
Since its first iterations, CR has matured substantially to provide a comprehensive intervention addressing the many facets of IHD.53,68,69,83,85 Although the multilayered nature of CR should be underscored (encompassing areas such as nutritional counseling, psychological support, smoking cessation, and others), exercise training is an integral component of these programs.68,83 Beyond its therapeutic role, exercise also forms a key part of risk stratification and prescription optimization and in assessing the (functional) impact of the program.14,35,68,86 This concept is clearly displayed by its incorporation in stress testing [such as in exercise stress testing with electrocardiographic monitoring (ExECG) or CPET], providing highly important inputs for these components.17,35,86
Although there are many particularities concerning exercise prescription in IHD, stemming from both patient characteristics (including functional capacity, osteoarticular limitations, and other comorbidities or the presence of risk features such as residual ischemia and left ventricular dysfunction) and availability, an individualized approach is essential to harness the full breadth of this intervention.14,83,86 In parallel to the approach used in pharmacological interventions, an adequate and personalized exercise prescription is paramount.86,87 This notion is expressed for both aerobic and resistance training, where different methodologies may be applied according to specific contexts.83,86,87 In aerobic training, assessing ventilatory thresholds (by CPET) can provide an invaluable window with which to tailor prescription, whereas peak heart rate and maximal load attained, as well as the Borg scale, can also inform on specific regimens.86-88 Notably, beyond continuous moderate training, different modes of exercise training such as those using high-intensity interval training have also been reported.8,83,86,89-91 For resistance training, this too has been shown to be a relevant component of regimens.8,86,92 As for aerobic training, in resistance training an individualized assessment for risk (taking into consideration factors such as diabetes and retinopathy) and aspects such as the type of equipment to be used and intensity to be employed (namely with the definition of repetition maximums) should be considered.92 When structuring the exercise training program, the presence of cardiac implantable electronic devices is another important factor.87,92,93 In these patients, an integrated assessment of not only background disease but also issues related to the device (such as programming or the risk of trauma) should be performed, to appropriately couple safety considerations with optimal benefits.93
Assessing the functional impact of the program is an important part of current CR.68 This can also inform on prognosis, as variations in peak oxygen consumption have been associated with outcomes such as mortality.78,94,95 Thus, from preintervention to training sessions and finally postintervention assessments, exercise (whether with a predominantly therapeutic intent or as a component of tests such as CPET) forms one of the pillars of CR across different moments.35,68,86
Role of exercise beyond therapeutic effects
Beyond its role with a primarily therapeutic intent, exercise can also be a useful tool for diagnostic, risk stratification, and prognostic evaluations (Fig. 1).14,16,17,35,96 Although much research has in recent years focused on settings such as heart failure, cardiomyopathies, and cancer, these capabilities also extend to the global assessment of IHD.14,28,35,96-99 In this capacity exercise has been discussed, although with marked methodological and technical variations, for several decades.17,100,101
As mentioned above, since some of the first descriptions of IHD, exertion has been regarded as having a leading role in eliciting symptoms (whether chest discomfort or dyspnea).8,59,102 Beyond these clinical manifestations, electrocardiographic changes associated with exercise were also reported early on.103 These would lead to the incorporation of exercise as part of the workup of IHD with examples such as the Master two-step test (in which patients climbed two steps, each with 22.86 cm) lavishly illustrating the resourcefulness of some of the early frameworks employed, aiming to standardize its application.103-105 As recalled decades after its inception in a review by Arthur Master (one of its codevelopers and the namesake for the test), its predominant focus, however, was the assessment of myocardial ischemia and not overall fitness.100,106,107 Although with limitations, this was one of the precursors of what would later become the contemporary ExECG.103 This technique would be subsequently refined and streamlined by American cardiologist Robert Bruce, leading to the eponymous and now ubiquitous Bruce protocol.17
As imaging methodologies continue to improve, showing increasing accuracy in the assessment of suspected IHD, the use of the ExECG with a diagnostic aim has progressively been superseded.7,8 However, beyond its role in electrocardiographic changes appraisal with a focus on ischemia assessment for diagnostic purposes, this test can also provide data on several other dimensions such as symptom status, functional capacity, blood pressure, heart rate, rhythm, and conduction disturbances.8,17,108 Indeed, its utility in the assessment of these parameters has been reported in distinct scenarios.17,108 As for additional applications, several of the principles used in ExECG also form a core part of CPET. 16,35 Finally, applying exercise beyond these examples is another hallmark of its resolute enduring relevance.8,102,109,110 This can be distinctly seen in stress echocardiography where exercise has been advised as a first-line stressor in the setting of coronary artery disease but also by its use in modalities such as myocardial perfusion scintigraphy.8,102,109 Concurrently to these, the role of cardiorespiratory fitness as a powerful predictor of events across several populations should also be recalled.94,96,111,112
Future perspectives—cardiac rehabilitation in a changing world
As discussed above, the prominent role of exercise in IHD is currently well established.6,8,68,73 Albeit this, there are still several hindrances concerning its application.69,73 For CR (and secondary prevention in general), a gap between recommendations and overall implementation should be considered as several studies have described suboptimal patient participation in these programs.64,113,114 Many barriers affecting diverse links have been identified, including those related to health care systems as well as patient-specific and clinician-specific issues, reflecting the complex nature of this matter.113 Some of the proposed avenues to address these unmet needs range from strategies such as providing different models of CR (versus classical center-based programs) and incorporating automatic referrals, to improving patient education on this issue and further expanding health care provider training.113,115 In addition, as digital platforms and technological innovations become ever more intertwined with day-to-day activities, their use to leverage CR has also been an area of increasing interest.113,116,117 From possible roles in allowing more individualized regimens (by taking into consideration data on different parameters, namely with inputs derived from devices such as smartwatches or wearable sensors) to their incorporation in home-based or hybrid programs, outlooks on the use of digital technologies have progressively been under the spotlight.116-118 Notwithstanding their major potential in improving CR, pitfalls such as how to best apply different technologies, patient preferences, and selection issues, among others, should still be taken into consideration.53,119
Another point worthy of mention relates to the distinct profiles encompassed by IHD.6,8 These reflect also the progressive shift from the prior classical view of IHD centered on epicardial obstructive disease to one where both macrocirculation and microcirculation (with anatomical and functional specificities) are increasingly recognized as having prominent roles in health and disease.8,59,120,121 This notion, coupled with the multitude of different patient characteristics (in terms of comorbidities, the presence of frailty, prior physical activity, among others) leads to the need to integrate several components when assessing the individual patient.8,14,83,86,87,122,123 As with other areas of cardiology, the possible incorporation of novel and transformative frameworks such as those related to artificial intelligence and machine learning may also improve the application of these interventions.124,125 Beyond this, these could also allow enhancements in the interpretation and scope of tests such as CPET, by providing novel insights and potential applications.82,126,127
Conclusion
Exercise represents a unique and fundamental strategy across the continuum of IHD. Robust data support its role in the management of IHD, namely when incorporated in contemporary CR programs. Moreover, the use of exercise as part of frameworks such as CPET or stress echocardiography provides relevant information for diagnostic purposes, risk stratification, and prognostic assessment. Although having accompanied several major paradigm changes in IHD over the years, exercise has maintained its prominence, having a leading role in this continuously and rapidly evolving field.
References
- [1].Tipton CM. The history of “Exercise Is Medicine” in ancient civilizations. Adv Physiol Educ. 2014;38:109–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Tipton CM. Susruta of India, an unrecognized contributor to the history of exercise physiology. J Appl Physiol (1985). 2008;104:1553–6. [DOI] [PubMed] [Google Scholar]
- [3].Castelletti S, D'Ascenzi F, Papadakis M. Sports cardiology in Europe from the ancient Greek-Roman era to the present. Eur Heart J. 2022;43:2542–4. [DOI] [PubMed] [Google Scholar]
- [4].Martin SS, Aday AW, Almarzooq ZI, et al. 2024 heart disease and stroke statistics: a report of US and global data from the American heart association. Circulation. 2024;149:e347–913. [DOI] [PubMed] [Google Scholar]
- [5].Timmis A, Aboyans V, Vardas P, et al. European society of cardiology: the 2023 atlas of cardiovascular disease statistics. Eur Heart J. 2024;45:4019–62. [DOI] [PubMed] [Google Scholar]
- [6].Byrne RA, Rossello X, Coughlan JJ, et al. 2023 ESC Guidelines for the management of acute coronary syndromes. Eur Heart J. 2023;44:3720–826. [DOI] [PubMed] [Google Scholar]
- [7].Knuuti J, Wijns W, Saraste A, et al. 2019 ESC Guidelines for the diagnosis and management of chronic coronary syndromes. Eur Heart J. 2020;41:407–77. [DOI] [PubMed] [Google Scholar]
- [8].Vrints C, Andreotti F, Koskinas KC, et al. 2024 ESC Guidelines for the management of chronic coronary syndromes. Eur Heart J. 2024;45:3415–537. [DOI] [PubMed] [Google Scholar]
- [9].Thompson RC, Sutherland ML, Allam AH, et al. Atherosclerosis in ancient mummified humans: the global HORUS study. Eur Heart J. 2024;45:2259–62. [DOI] [PubMed] [Google Scholar]
- [10].Vilela E, Fontes-Carvalho R. The heart as a “balance” in everyday and after life: lessons from ancient Egypt. JACC Case Rep. 2023;23:102010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Braunwald E. The treatment of acute myocardial infarction: the Past, the Present, and the Future. Eur Heart J Acute Cardiovasc Care. 2012;1:9–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Montone RA, Rinaldi R, Niccoli G, et al. Optimizing management of stable angina: a patient-centered approach integrating revascularization, medical therapy, and lifestyle interventions. J Am Coll Cardiol. 2024;84:744–60. [DOI] [PubMed] [Google Scholar]
- [13].Tucker WJ, Fegers-Wustrow I, Halle M, Haykowsky MJ, Chung EH, Kovacic JC. Exercise for primary and secondary prevention of cardiovascular disease: JACC focus seminar 1/4. J Am Coll Cardiol. 2022;80:1091–106. [DOI] [PubMed] [Google Scholar]
- [14].Pelliccia A, Sharma S, Gati S, et al. 2020 ESC Guidelines on sports cardiology and exercise in patients with cardiovascular disease. Eur Heart J. 2021;42:17–96. [DOI] [PubMed] [Google Scholar]
- [15].Writing Committee Members, Virani SS, Newby LK, Arnold SV, et al. 2023 AHA/ACC/ACCP/ASPC/NLA/PCNA guideline for the management of patients with chronic coronary disease: a report of the American Heart Association/American College of Cardiology joint committee on clinical practice guidelines. J Am Coll Cardiol. 2023;82:833–955. [DOI] [PubMed] [Google Scholar]
- [16].Chaudhry S, Kumar N, Arena R, Verma S. The evolving role of cardiopulmonary exercise testing in ischemic heart disease—state of the art review. Curr Opin Cardiol. 2023;38:552–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Vilela EM, Oliveira C, Oliveira C, et al. Sixty years of the Bruce protocol: reappraising the contemporary role of exercise stress testing with electrocardiographic monitoring. Porto Biomed J. 2023;8:e235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Fontes-Carvalho R, Vilela EM, Gonçalves-Teixeira P. The effect of exercise training in systolic and diastolic function. In: Watson RR, Zibadi S, eds. Lifestyle in heart health and disease. 1st ed. Amsterdam: Elsevier; 2018:153–62. [Google Scholar]
- [19].Valenzuela PL, Ruilope LM, Santos-Lozano A, et al. Exercise benefits in cardiovascular diseases: from mechanisms to clinical implementation. Eur Heart J. 2023;44:1874–89. [DOI] [PubMed] [Google Scholar]
- [20].Hastings MH, Castro C, Freeman R, et al. Intrinsic and extrinsic contributors to the cardiac benefits of exercise. JACC Basic Transl Sci. 2024;9:535–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Fiuza-Luces C, Santos-Lozano A, Joyner M, et al. Exercise benefits in cardiovascular disease: beyond attenuation of traditional risk factors. Nat Rev Cardiol. 2018;15:731–43. [DOI] [PubMed] [Google Scholar]
- [22].Aimo A, Saccaro LF, Borrelli C, et al. The ergoreflex: how the skeletal muscle modulates ventilation and cardiovascular function in health and disease. Eur J Heart Fail. 2021;23:1458–67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [23].Pelliccia A, Caselli S. Structural and functional adaptations in the athlete’s heart. In: Pellicia A, Heidbuchel H, Corrado D, Borjesson M, Sharma S, eds. ESC textbook sports cardiology. 1st ed. UK: OUP; 2019:9–20. [Google Scholar]
- [24].Sun H, Zhang Y, Shi L. Advances in exercise-induced vascular adaptation: mechanisms, models, and methods. Front Bioeng Biotechnol. 2024;12:1370234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [25].Thyfault JP, Bergouignan A. Exercise and metabolic health: beyond skeletal muscle. Diabetologia. 2020;63:1464–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [26].McKenzie DC. Respiratory physiology: adaptations to high-level exercise. Br J Sports Med. 2012;46:381–4. [DOI] [PubMed] [Google Scholar]
- [27].Holland AE, Cox NS, Houchen-Wolloff L, et al. Defining modern pulmonary rehabilitation. An official American Thoracic Society Workshop report. Ann Am Thorac Soc. 2021;18:e12–29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [28].Gilchrist SC, Barac A, Ades PA, et al. Cardio-Oncology rehabilitation to manage cardiovascular outcomes in cancer patients and survivors: a scientific statement from the American Heart Association. Circulation. 2019;139:e997–1012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [29].Lyon AR, López-Fernández T, Couch LS, et al. 2022 ESC guidelines on cardio-oncology developed in collaboration with the European Hematology Association (EHA), the European Society for Therapeutic Radiology and Oncology (ESTRO) and the International Cardio-Oncology society (IC-OS). Eur Heart J. 2022;43:4229–361. [DOI] [PubMed] [Google Scholar]
- [30].Viamonte SG, Joaquim AV, Alves AJ, et al. Cardio-Oncology rehabilitation for cancer survivors with high cardiovascular risk: a randomized clinical trial. JAMA Cardiol. 2023;8:1119–28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [31].Antunes P, Joaquim A, Sampaio F, et al. Effects of exercise training on cardiac toxicity markers in women with breast cancer undergoing chemotherapy with anthracyclines: a randomized controlled trial. Eur J Prev Cardiol. 2023;30:844–55. [DOI] [PubMed] [Google Scholar]
- [32].Antunes P, Joaquim A, Sampaio F, et al. Exercise training benefits health-related quality of life and functional capacity during breast cancer chemotherapy: a randomized controlled trial. Med Sci Sports Exerc. 2024;56:600–11. [DOI] [PubMed] [Google Scholar]
- [33].Valenzuela PL, Castillo-García A, Saco-Ledo G, Santos-Lozano A, Lucia A. Physical exercise: a polypill against chronic kidney disease. Nephrol Dial Transpl. 2024;39:1384–91. [DOI] [PubMed] [Google Scholar]
- [34].Kouidi E, Hanssen H, Anding-Rost K, et al. The role of exercise training on cardiovascular risk factors and heart disease in patients with chronic kidney disease G3-G5 and G5D: a Clinical Consensus Statement of the European Association of Preventive Cardiology of the ESC and the European Association of Rehabilitation in Chronic Kidney Disease. Eur J Prev Cardiol. 2024;31:1493–515. [DOI] [PubMed] [Google Scholar]
- [35].Dores H, Mendes M, Abreu A, et al. Cardiopulmonary exercise testing in clinical practice: principles, applications, and basic interpretation. Rev Port Cardiol. 2024;43:525–36. [DOI] [PubMed] [Google Scholar]
- [36].Joseph P, Singh I, Oliveira R, et al. Exercise pathophysiology in myalgic encephalomyelitis/chronic fatigue syndrome and postacute sequelae of SARS-CoV-2: more in common than not? Chest. 2023;164:717–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [37].Hooijmans MT, Jeneson JAL, Jørstad HT, Bakermans AJ. Exercise MR of skeletal muscles, the heart, and the brain. J Magn Reson Imaging. Published online May 10, 2024. doi: 10.1002/jmri.29445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [38].Franklin BA, Eijsvogels TMH, Pandey A, Quindry J, Toth PP. Physical activity, cardiorespiratory fitness, and cardiovascular health: a clinical practice statement of the ASPC Part I: bioenergetics, contemporary physical activity recommendations, benefits, risks, extreme exercise regimens, potential maladaptations. Am J Prev Cardiol. 2022;12:100424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [39].De Bosscher R, Dausin C, Claus P, et al. Lifelong endurance exercise and its relation with coronary atherosclerosis. Eur Heart J. 2023;44:2388–99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [40].Aengevaeren VL, Mosterd A, Bakker EA, et al. Exercise volume versus intensity and the progression of coronary atherosclerosis in middle-aged and older athletes: findings from the MARC-2 study. Circulation. 2023;147:993–1003. [DOI] [PubMed] [Google Scholar]
- [41].Shuval K, Leonard D, DeFina LF, et al. Physical activity and progression of coronary artery calcification in men and women. JAMA Cardiol. 2024;9:659–66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [42].Vilela EM, Bastos JC, Rodrigues RP, Nunes JP. High-sensitivity troponin after running--a systematic review. Neth J Med. 2014;72:5–9. [PubMed] [Google Scholar]
- [43].Vilela EM, Bettencourt-Silva R, Nunes JP, Ribeiro VG. BNP and NT-proBNP elevation after running—a systematic review. Acta Cardiol. 2015;70:501–9. [DOI] [PubMed] [Google Scholar]
- [44].Lampert R, Chung EH, Ackerman MJ, et al. 2024 HRS expert consensus statement on arrhythmias in the athlete: evaluation, treatment, and return to play. Heart Rhythm. 2024;21:e151–252. [DOI] [PubMed] [Google Scholar]
- [45].Petek BJ, Chung EH, Kim JH, et al. Impact of sex on cardiovascular adaptations to exercise: JACC review topic of the week. J Am Coll Cardiol. 2023;82:1030–8. [DOI] [PubMed] [Google Scholar]
- [46].Newman W, Parry-Williams G, Wiles J, et al. Risk of atrial fibrillation in athletes: a systematic review and meta-analysis. Br J Sports Med. 2021;55:1233–8. [DOI] [PubMed] [Google Scholar]
- [47].Franklin BA, Thompson PD, Al-Zaiti SS, et al. Exercise-related acute cardiovascular events and potential deleterious adaptations following long-term exercise training: placing the risks into perspective-an update: a scientific statement from the American Heart Association. Circulation. 2020;141:e705–36. [DOI] [PubMed] [Google Scholar]
- [48].Piggin J. What is physical activity? A holistic definition for teachers, researchers and policy makers. Front Sports Act Living. 2020;2:72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [49].Périard JD, Eijsvogels TMH, Daanen HAM. Exercise under heat stress: thermoregulation, hydration, performance implications, and mitigation strategies. Physiol Rev. 2021;101:1873–979. [DOI] [PubMed] [Google Scholar]
- [50].Feng Z, Hu Y, Yu S, et al. Exercise in cold: friend than foe to cardiovascular health. Life Sci. 2023;328:121923. [DOI] [PubMed] [Google Scholar]
- [51].Holtermann A, Schnohr P, Nordestgaard BG, Marott JL. The physical activity paradox in cardiovascular disease and all-cause mortality: the contemporary Copenhagen General Population Study with 104 046 adults. Eur Heart J. 2021;42:1499–511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [52].Hahad O, Kuntic M, Frenis K, et al. Physical activity in polluted air-net benefit or harm to cardiovascular health? A comprehensive review. Antioxidants (Basel). 2021;10:1787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [53].Thomas RJ. Cardiac rehabilitation—challenges, advances, and the road ahead. N Engl J Med. 2024;390:830–41. [DOI] [PubMed] [Google Scholar]
- [54].Leighton LS. The story of the “cardiac chair” and the resistance to its use in patients with acute myocardial infarction, 1950 to 1961. Am J Cardiol. 2017;120:1674–80. [Google Scholar]
- [55].Redfern J, Gallagher R, O'Neil A, et al. Historical context of cardiac rehabilitation: learning from the past to move to the future. Front Cardiovasc Med. 2022;9:842567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [56].Certo CM. History of cardiac rehabilitation. Phys Ther. 1985;65:1793–5. [DOI] [PubMed] [Google Scholar]
- [57].Heusch B, Guth BD, Heusch G. A brief history of angina pectoris: change of concepts and ideas. In: Heusch G, ed. Pathophysiology and Rational Pharmacotherapy of Myocardial Ischemia. 1st ed. Germany: Steinkopff Heidelber; 1990:1–9. [Google Scholar]
- [58].Mitchell JD, Brown DL. Harmonizing the paradigm with the data in stable coronary artery disease: a review and viewpoint. J Am Heart Assoc. 2017;6:e007006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [59].Boden WE, Kaski JC, Berry C. Reprising Heberden's description of angina pectoris after 250 years. Eur Heart J. 2023;44:1684–6. [DOI] [PubMed] [Google Scholar]
- [60].Olszewski TM. James Herrick (1861-1954): consultant physician and cardiologist. J Med Biogr. 2018;26:132–6. [DOI] [PubMed] [Google Scholar]
- [61].Levine SA. Some harmful effects of recumbency in the treatment of heart disease. J Am Med Assoc. 1944;126:80–4. [Google Scholar]
- [62].Levine SA, Lown B. “Armchair” treatment of acute coronary thrombosis. J Am Med Assoc. 1952;148:1365–9. [DOI] [PubMed] [Google Scholar]
- [63].Kavanagh T. Exercise in cardiac rehabilitation. Br J Sports Med. 2000;34:3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [64].Turk-Adawi K, Supervia M, Lopez-Jimenez F, et al. Cardiac rehabilitation availability and density around the globe. EClinicalMedicine. 2019;13:31–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [65].Newman LB, Andrews MF, Koblish MO, Baker LA. Physical medicine and rehabilitation in acute myocardial infarction. AMA Arch Intern Med. 1952;89:552–61. [DOI] [PubMed] [Google Scholar]
- [66].Lara-Vargas JA Ilarraza-Lomelí H García-Saldivia M, et al. Tercer Registro Nacional de Programas de Rehabilitación Cardiaca en México (RENAPREC III-2022) [Third National Registry of Cardiac Rehabilitation Programs in Mexico (RENAPREC III-2022)]. Arch Cardiol Mex. Published online June 6, 2023. doi: 10.24875/ACM.22000235. [DOI] [PubMed] [Google Scholar]
- [67].Messerli FH, Messerli AW, Lüscher TF. Eisenhower's billion-dollar heart attack—50 years later. N Engl J Med. 2005;353:1205–7. [DOI] [PubMed] [Google Scholar]
- [68].Abreu A, Frederix I, Dendale P, et al. Standardization and quality improvement of secondary prevention through cardiovascular rehabilitation programmes in Europe: the avenue towards EAPC accreditation programme: a position statement of the Secondary Prevention and Rehabilitation Section of the European Association of Preventive Cardiology (EAPC). Eur J Prev Cardiol. 2021;28:496–509. [DOI] [PubMed] [Google Scholar]
- [69].Taylor RS, Dalal HM, McDonagh STJ. The role of cardiac rehabilitation in improving cardiovascular outcomes. Nat Rev Cardiol. 2022;19:180–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [70].Salzwedel A, Jensen K, Rauch B, et al. Effectiveness of comprehensive cardiac rehabilitation in coronary artery disease patients treated according to contemporary evidence based medicine: update of the Cardiac Rehabilitation Outcome Study (CROS-II). Eur J Prev Cardiol. 2020;27:1756–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [71].Grace SL. Evidence is indisputable that cardiac rehabilitation provides health benefits and event reduction: time for policy action. Eur Heart J. 2023;44:470–2. [DOI] [PubMed] [Google Scholar]
- [72].Dibben GO, Faulkner J, Oldridge N, et al. Exercise-based cardiac rehabilitation for coronary heart disease: a meta-analysis. Eur Heart J. 2023;44:452–69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [73].Vilela EM, Ladeiras-Lopes R, Joao A, et al. Current role and future perspectives of cardiac rehabilitation in coronary heart disease. World J Cardiol. 2021;13:695–709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [74].Abell B, Zecchin R, Gallagher R. Making sense of the unfavourable systematic review of exercise-based cardiac rehabilitation in the modern era: how should we proceed? Heart Lung Circ. 2019;28:204–6. [DOI] [PubMed] [Google Scholar]
- [75].West RR, Jones DA, Henderson AH. Rehabilitation after myocardial infarction trial (RAMIT): multi-centre randomised controlled trial of comprehensive cardiac rehabilitation in patients following acute myocardial infarction. Heart. 2012;98:637–44. [DOI] [PubMed] [Google Scholar]
- [76].Visseren FLJ, Mach F, Smulders YM, et al. 2021 ESC Guidelines on cardiovascular disease prevention in clinical practice. Eur Heart J. 2021;42:3227–337. [DOI] [PubMed] [Google Scholar]
- [77].Vilela EM, Ladeiras-Lopes R, Joao A, et al. Differential impact of a cardiac rehabilitation program in functional parameters according to patient gender. Am J Cardiovasc Dis. 2020;10:367–75. [PMC free article] [PubMed] [Google Scholar]
- [78].Witvrouwen I, Van Craenenbroeck EM, Abreu A, Moholdt T, Kränkel N. Exercise training in women with cardiovascular disease: differential response and barriers—review and perspective. Eur J Prev Cardiol. 2021;28:779–90. [DOI] [PubMed] [Google Scholar]
- [79].Vilela EM, Ladeiras Lopes R, Torres S, et al. Differential impact of a cardiac rehabilitation program on functional parameters in elderly versus non-elderly myocardial infarction survivors. Cardiology. 2020;145:98–105. [DOI] [PubMed] [Google Scholar]
- [80].Prescott E, Eser P, Mikkelsen N, et al. Cardiac rehabilitation of elderly patients in eight rehabilitation units in Western Europe: outcome data from the EU-CaRE multi-centre observational study. Eur J Prev Cardiol. 2020;27:1716–29. [DOI] [PubMed] [Google Scholar]
- [81].Vilela EM, Ladeiras-Lopes R, Ruivo C, et al. Different outcomes of a cardiac rehabilitation programme in functional parameters among myocardial infarction survivors according to ejection fraction. Neth Heart J. 2019;27:347–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [82].Gevaert AB, Adams V, Bahls M, et al. Towards a personalised approach in exercise-based cardiovascular rehabilitation: how can translational research help? A 'call to action' from the Section on Secondary Prevention and Cardiac Rehabilitation of the European Association of Preventive Cardiology. Eur J Prev Cardiol. 2020;27:1369–85. [DOI] [PubMed] [Google Scholar]
- [83].Ambrosetti M, Abreu A, Corrà U, et al. Secondary prevention through comprehensive cardiovascular rehabilitation: from knowledge to implementation. 2020 update. A position paper from the Secondary Prevention and Rehabilitation Section of the European Association of Preventive Cardiology. Eur J Prev Cardiol. 2021;28:460–95. [DOI] [PubMed] [Google Scholar]
- [84].Pavasini R, Biscaglia S, Kunadian V, Hakeem A, Campo G. Coronary artery disease management in older adults: revascularization and exercise training. Eur Heart J. 2024;45:2811–23. [DOI] [PubMed] [Google Scholar]
- [85].Brown TM Pack QR Aberegg E, et al. Core components of cardiac rehabilitation programs: 2024 update: a scientific statement from the American Heart Association and the American Association of Cardiovascular and Pulmonary Rehabilitation. Circulation. 2024;150:e328–e47. [DOI] [PubMed] [Google Scholar]
- [86].Hansen D, Abreu A, Ambrosetti M, et al. Exercise intensity assessment and prescription in cardiovascular rehabilitation and beyond: why and how: a position statement from the Secondary Prevention and Rehabilitation Section of the European Association of Preventive Cardiology. Eur J Prev Cardiol. 2022;29:230–45. [DOI] [PubMed] [Google Scholar]
- [87].Hansen D, Beckers P, Neunhäuserer D, et al. Standardised exercise prescription for patients with chronic coronary syndrome and/or heart failure: a consensus statement from the expert working group. Sports Med. 2023;53:2013–37. [DOI] [PubMed] [Google Scholar]
- [88].Anselmi F, Cavigli L, Pagliaro A, et al. The importance of ventilatory thresholds to define aerobic exercise intensity in cardiac patients and healthy subjects. Scand J Med Sci Sports. 2021;31:1796–808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [89].Conraads VM, Pattyn N, De Maeyer C, et al. Aerobic interval training and continuous training equally improve aerobic exercise capacity in patients with coronary artery disease: the SAINTEX-CAD study. Int J Cardiol. 2015;179:203–10. [DOI] [PubMed] [Google Scholar]
- [90].McGregor G, Powell R, Begg B, et al. High-intensity interval training in cardiac rehabilitation: a multi-centre randomized controlled trial. Eur J Prev Cardiol. 2023;30:745–55. [DOI] [PubMed] [Google Scholar]
- [91].Yu H, Zhao X, Wu X, Yang J, Wang J, Hou L. High-intensity interval training versus moderate-intensity continuous training on patient quality of life in cardiovascular disease: a systematic review and meta-analysis. Sci Rep. 2023;13:13915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [92].Paluch AE, Boyer WR, Franklin BA, et al. Resistance exercise training in individuals with and without cardiovascular disease: 2023 update: a scientific statement from the American Heart Association. Circulation. 2024;149:e217–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [93].Pedretti RFE, Iliou MC, Israel CW, et al. Comprehensive multicomponent cardiac rehabilitation in cardiac implantable electronic devices recipients: a consensus document from the European Association of Preventive Cardiology (EAPC; Secondary prevention and rehabilitation section) and European Heart Rhythm Association (EHRA). Eur J Prev Cardiol. 2021;28:1736–52. [DOI] [PubMed] [Google Scholar]
- [94].De Schutter A, Kachur S, Lavie CJ, et al. Cardiac rehabilitation fitness changes and subsequent survival. Eur Heart J Qual Care Clin Outcomes. 2018;4:173–9. [DOI] [PubMed] [Google Scholar]
- [95].Carbone S, Kim Y, Kachur S, et al. Peak oxygen consumption achieved at the end of cardiac rehabilitation predicts long-term survival in patients with coronary heart disease. Eur Heart J Qual Care Clin Outcomes. 2022;8:361–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [96].Ross R, Blair SN, Arena R, et al. Importance of assessing cardiorespiratory fitness in clinical practice: a case for fitness as a clinical vital sign: a scientific statement from the American Heart Association. Circulation. 2016;134:e653–99. [DOI] [PubMed] [Google Scholar]
- [97].McDonagh TA, Metra M, Adamo M, et al. 2021 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure. Eur Heart J. 2021;42:3599–726. [DOI] [PubMed] [Google Scholar]
- [98].Guazzi M, Wilhelm M, Halle M, et al. Exercise testing in heart failure with preserved ejection fraction: an appraisal through diagnosis, pathophysiology and therapy—a clinical consensus statement of the Heart Failure Association and European Association of Preventive Cardiology of the European Society of Cardiology. Eur J Heart Fail. 2022;24:1327–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [99].Salvioni E, Bonomi A, Magrì D, et al. The cardiopulmonary exercise test in the prognostic evaluation of patients with heart failure and cardiomyopathies: the long history of making a one-size-fits-all suit. Eur J Prev Cardiol. 2023;30(Suppl 2):ii28–33. [DOI] [PubMed] [Google Scholar]
- [100].Master AM. The two-step test of myocardial function. Am Heart J. 1935;10:495–510. [Google Scholar]
- [101].Barringer TB. Exercise tolerance in heart disease. JAMA. 1922;79:2205–6. [Google Scholar]
- [102].Picano E, Pierard L, Peteiro J, et al. The clinical use of stress echocardiography in chronic coronary syndromes and beyond coronary artery disease: a clinical consensus statement from the European Association of Cardiovascular Imaging of the ESC. Eur Heart J Cardiovasc Imaging. 2024;25:e65–90. [DOI] [PubMed] [Google Scholar]
- [103].Chaitman BR. The changing role of the exercise electrocardiogram as a diagnostic and prognostic test for chronic ischemic heart disease. J Am Coll Cardiol. 1986;8:1195–210. [DOI] [PubMed] [Google Scholar]
- [104].Master AM, Friedman R, Dack S. The electrocardiogram after standard exercise as a functional test of the heart. Am Heart J. 1942;24:777–93. [Google Scholar]
- [105].Datey KK, Misra SN. The evaluation of two-step exercise test in patients with heart disease of different etiologies. Dis Chest. 1968;53:294–300. [DOI] [PubMed] [Google Scholar]
- [106].Master AM. The Master two-step test. Am Heart J. 1968;75:809–37. [DOI] [PubMed] [Google Scholar]
- [107].Wenger NK, Arthur M. Master, 1895-1973. Clin Cardiol. 1988;11:509–12. [DOI] [PubMed] [Google Scholar]
- [108].Sharma K, Kohli P, Gulati M. An update on exercise stress testing. Curr Probl Cardiol. 2012;37:177–202. [DOI] [PubMed] [Google Scholar]
- [109].Pellikka PA, Arruda-Olson A, Chaudhry FA, et al. Guidelines for performance, interpretation, and application of stress echocardiography in ischemic heart disease: from the American Society of Echocardiography. J Am Soc Echocardiogr. 2020;33:1–41.e8. [DOI] [PubMed] [Google Scholar]
- [110].Vilela EM, Fontes-Carvalho R. Blood pressure response and exercise stress echocardiography: new perspectives on a contemporary challenge. Arq Bras Cardiol. 2023;120:e20230737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [111].Lang JJ, Prince SA, Merucci K, et al. Cardiorespiratory fitness is a strong and consistent predictor of morbidity and mortality among adults: an overview of meta-analyses representing over 20.9 million observations from 199 unique cohort studies. Br J Sports Med. 2024;58:556–66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [112].Hung RK, Al-Mallah MH, McEvoy JW, et al. Prognostic value of exercise capacity in patients with coronary artery disease: the FIT (Henry Ford ExercIse Testing) project. Mayo Clin Proc. 2014;89:1644–54. [DOI] [PubMed] [Google Scholar]
- [113].Taylor RS, Fredericks S, Jones I, et al. Global perspectives on heart disease rehabilitation and secondary prevention: a scientific statement from the association of cardiovascular nursing and allied professions, European association of preventive cardiology, and international council of cardiovascular prevention and rehabilitation. Eur Heart J. 2023;44:2515–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [114].Fontes JP, Vilela EM, Durazzo A, Teixeira M. Current state of cardiac rehabilitation in Portugal: results of the 2019 national survey. Rev Port Cardiol (Engl Ed). 2021;40:877–87. [DOI] [PubMed] [Google Scholar]
- [115].Vilela EM, Bento L, Oliveira L, et al. Training and attitudes concerning cardiac rehabilitation in Portugal: a national survey of physician members of the Portuguese Society of Cardiology. Rev Port Cardiol. 2024;43:487–96. [DOI] [PubMed] [Google Scholar]
- [116].Golbus JR, Lopez-Jimenez F, Barac A, et al. Digital technologies in cardiac rehabilitation: a science advisory from the American heart association. Circulation. 2023;148:95–107. [DOI] [PubMed] [Google Scholar]
- [117].Beatty AL, Beckie TM, Dodson J, et al. A new era in cardiac rehabilitation delivery: research gaps, questions, strategies, and priorities. Circulation. 2023;147:254–66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [118].Scherrenberg M, Wilhelm M, Hansen D, et al. The future is now: a call for action for cardiac telerehabilitation in the COVID-19 pandemic from the secondary prevention and rehabilitation section of the European Association of Preventive Cardiology. Eur J Prev Cardiol. 2021;28:524–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [119].Marcin T, Bengel C, Goldberg T, Peterhans J, Eser P, Wilhelm M. Patient interest in mHealth as part of cardiac rehabilitation in Switzerland. Swiss Med Wkly. 2021;151:w20510. [DOI] [PubMed] [Google Scholar]
- [120].Reynolds HR, Bairey Merz CN, Berry C, et al. Coronary arterial function and disease in women with no obstructive coronary arteries. Circ Res. 2022;130:529–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [121].Sidik N, Morrow A, Berry C. Human microcirculation in ischemic heart disease. Arterioscler Thromb Vasc Biol. 2020;40:11–3. [DOI] [PubMed] [Google Scholar]
- [122].Larsen AI, Sæland C, Vegsundvåg J, et al. Aerobic high-intensity interval exercise training in patients with angina and no obstructive coronary artery disease: feasibility and physiological effects. Eur Heart J Open. 2023;3:oead030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [123].Pavasini R, Campo G, Serenelli M, et al. Impact of pre-admission physical activity on benefits of physiology-guided complete revascularization in older patients with myocardial infarction: insights from the FIRE trial. Eur J Prev Cardiol. 2024;31:1451–9. [DOI] [PubMed] [Google Scholar]
- [124].Ciccarelli M, Giallauria F, Carrizzo A, et al. Artificial intelligence in cardiovascular prevention: new ways will open new doors. J Cardiovasc Med (Hagerstown). 2023;24(Suppl 2):e106–15. [DOI] [PubMed] [Google Scholar]
- [125].Sotirakos S, Fouda B, Mohamed Razif NA, et al. Harnessing artificial intelligence in cardiac rehabilitation, a systematic review. Future Cardiol. 2022;18:154–64. [DOI] [PubMed] [Google Scholar]
- [126].Portella JJ, Andonian BJ, Brown DE, et al. Using machine learning to identify organ system specific limitations to exercise via cardiopulmonary exercise testing. IEEE J Biomed Health Inform. 2022;26:4228–37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [127].Watanabe T, Tohyama T, Ikeda M, et al. Development of deep-learning models for real-time anaerobic threshold and peak VO2 prediction during cardiopulmonary exercise testing. Eur J Prev Cardiol. 2024;31:448–57. [DOI] [PubMed] [Google Scholar]


