A 74-year-old man presented to our orthopedic department with pain and swelling in his right hand after falling down a mountainside and landing on his outstretched hand that day. On initial examination, he had tenderness over the carpal bones and restricted wrist movements. Motor and sensory function of the hand were intact, and the radial pulse was palpable. Wrist radiographs showed a perilunate dislocation with a radial styloid fracture (Figure 1). On the same day, we performed a closed reduction of the perilunate dislocation with percutaneous pinning. Postoperative radiographs confirmed alignment (Appendix 1, available at www.cmaj.ca/lookup/doi/10.1503/cmaj.241034/tab-related-content). The patient was immobilized in a cast for 6 weeks, and we removed the K-wires 8 weeks after the operation. At the 3-month follow-up visit, he had nearly normal range of motion in his right hand and reported no pain.
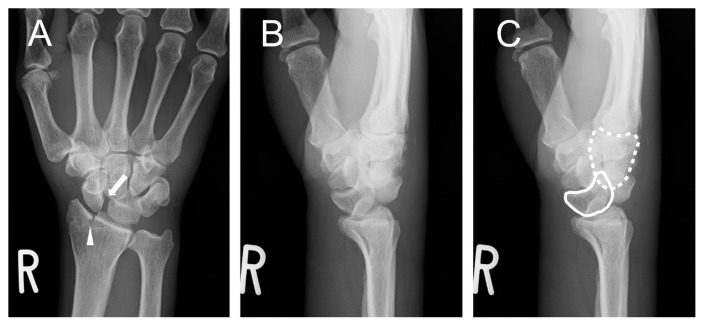
Figure 1:
(A) Radiographs of the right wrist of a 74-year-old man showing an enlarged scapholunate interval of more than 3 mm (arrow) and the radial styloid fracture (arrowhead) on the anteroposterior view. (B, C) The lateral view shows misalignment, with the lunate (solid line) palmarly flexed and not articulated with the capitate (dashed line).
Perilunate dislocation is an uncommon injury that typically results from high-energy falls on an outstretched hand.1–3 It occurs because of ligamentous disruption and may be accompanied by fractures of the scaphoid and the radial styloid, as well as median nerve injuries.1–3 Perilunate dislocation occurs when only the lunate remains within the radiocarpal joint while the other carpal bones dislocate dorsally.1 Lunate dislocation, caused by the disruption of all ligaments surrounding the lunate, results in a palmarly dislocated lunate.1 Given unfamiliarity with perilunate dislocation and misinterpretation of abnormalities on the radiographs, 3 perilunate dislocation is misdiagnosed in around 25% of patients on initial presentation.1–3 Prompt and accurate diagnosis is critical because perilunate dislocations require timely surgical intervention for proper anatomic alignment.1,2 Delayed diagnosis can lead to complications such as median nerve injury and avascular necrosis of the carpal bones, potentially resulting in chronic pain, carpal instability, and joint dysfunction.1,2 In cases of wrist injuries from high-energy trauma, maintaining a high index of suspicion for perilunate dislocation is crucial. Once diagnosed, immediate reduction is essential.
Supplementary Information
Footnotes
Competing interests: None declared.
This article has been peer reviewed.
The authors have obtained patient consent.
References
- 1.Goodman AD, Harris AP, Gil JA, et al. Evaluation, management, and outcomes of lunate and perilunate dislocations. Orthopedics 2019;42:e1–6. [DOI] [PubMed] [Google Scholar]
- 2.Beak P, Umarji S. A traumatic wrist injury. BMJ 2018;361:k2574. [DOI] [PubMed] [Google Scholar]
- 3.Çolak I, Bekler HI, Bulut G, et al. Lack of experience is a significant factor in the missed diagnosis of perilunate fracture dislocation or isolated dislocation. Acta Orthop Traumatol Turc 2018;52:32–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.