Summary
We report the airway management of an 11‐year‐old boy with Treacher Collins syndrome. In three instances under general anaesthesia, ventilation via either anaesthesia facemask or supraglottic airway device proved virtually impossible except when the neck was flexed, which runs counter to what is typically observed during routine anaesthetic care. In this report, the impact of neck flexion on the patient's airway is demonstrated with images obtained on videolaryngoscopy and flexible endoscopy. It is prudent to manage airways using validated techniques and established algorithms. Nonetheless, airway management can benefit from atypical measures.
Keywords: paediatric anaesthesia, paediatric difficult airway, Treacher Collins syndrome
Introduction
Treacher Collins syndrome is a rare genetic disorder associated with abnormalities of the first and second branchial arches, resulting in mandibular and maxillary hypoplasia, high arched palate, retrognathia and retroposition of the tongue [1]. Traditional airway manoeuvres such as neck extension and jaw thrust may not yield adequate glottic opening for effective facemask ventilation or glottic exposure. Additionally, the anatomical features which make airways difficult to manage in this condition may become more pronounced with age [2, 3, 4, 5]. Anecdotally, we have observed that atlanto‐occipital flexion may allow better opening of the glottis and can improve ventilation through a supraglottic airway device. There is evidence in adults sedated with propofol that head elevation and neck flexion, in the setting of centric occlusion – that is bringing the chin forward and closing the mouth so that the central incisors make maximal contact – may reduce pharyngeal collapsibility and improve ventilation [6]. We report a case where atlanto‐occipital flexion improved glottic opening and visualisation in a patient with Treacher Collins syndrome.
Report
An 11‐year‐old boy weighing 32 kg, with Treacher Collins syndrome presented for bilateral eye surgery. He was alert, interactive and developmentally normal. His past medical history included mild asthma and eczema. His cardiovascular function was normal. He exhibited facial features typical of Treacher Collins syndrome, with downward sloping palpebral fissures, profound retrognathia and mandibular hypoplasia.
The patient's anaesthetic history was notable for difficult airway management. Twenty‐one months prior to this admission, the patient attended for diagnostic microlaryngoscopy. Ventilation was not possible via facemask under anaesthesia and neuromuscular blockade was not administered as this procedure required spontaneous ventilation for airway examination; additionally, the patient's limited mouth opening and retrognathia had progressed so that his mouth could no longer accommodate an 80 mm green oropharyngeal airway. However, ventilation was effective through a supraglottic airway device (Ambu AuraOnce disposable laryngeal mask airway, size 3, Ballerup, Denmark) when the neck was flexed (but not with the neck neutral or extended). A paediatric otolaryngologist with a subspecialist interest in airway conditions was unable to obtain a direct view of the glottis. Only 10% of the glottic opening could be visualised on videolaryngoscopy using a disposable Glidescope LoPro S2 (hyperangulated) blade (Verathon, Bothell, Washington, USA) when performed by both the anaesthetist and surgeon. When the patient attended for further eyelid surgery 12 months prior to this admission, ventilation via facemask and supraglottic airway device proved difficult again, including after 1 mg.kg−1 of suxamethonium had been administered. Ventilation was then successful via the supraglottic airway device (Ambu AuraOnce disposable laryngeal mask airway, size 4, Ballerup, Denmark) when the neck was flexed.
On this admission, the patient's parents permitted anaesthetists to obtain images of this patient's airway with the neck in flexed and neutral positions under general anaesthesia. Intravenous access was secured in the preoperative area and midazolam 2 mg was administered intravenously for anxiolysis. Monitoring was commenced, including pulse oximetry, ECG, non‐invasive blood pressure measurement and end‐tidal gas monitoring via the Apollo anaesthesia circuit (Dräger, Lübeck, Germany). Anaesthesia was induced via facemask with sevoflurane 8% and ketamine in 2.5 mg.kg−1 increments with the aim of maintaining spontaneous ventilation.
A 20 Fr (6.7 mm) nasopharyngeal airway was placed in the right naris and attached to the anaesthesia circuit via a tracheal tube adapter to allow for the delivery of oxygen and sevoflurane and monitoring of end‐tidal carbon dioxide. Once an adequate depth of anaesthesia was achieved, videolaryngoscopy was performed using a disposable Glidescope LoPro S2 (hyperangulated) blade (Verathon, Bothell, Washington, USA). A 2.8 mm flexible bronchoscope, loaded with a 5.0‐mm ID tracheal tube, was then passed via the left naris. With the neck in a neutral to slightly flexed position, only 5% of the glottic opening was visualised with videolaryngoscopy (Fig. 1a). When the neck was placed in a flexed position, 90% of the glottic opening could be visualised (Fig. 1b). When attempts were made to put his neck into a truly neutral or extended position, the patient's airway was completely obstructed but no photographs were taken in these positions.
Figure 1.
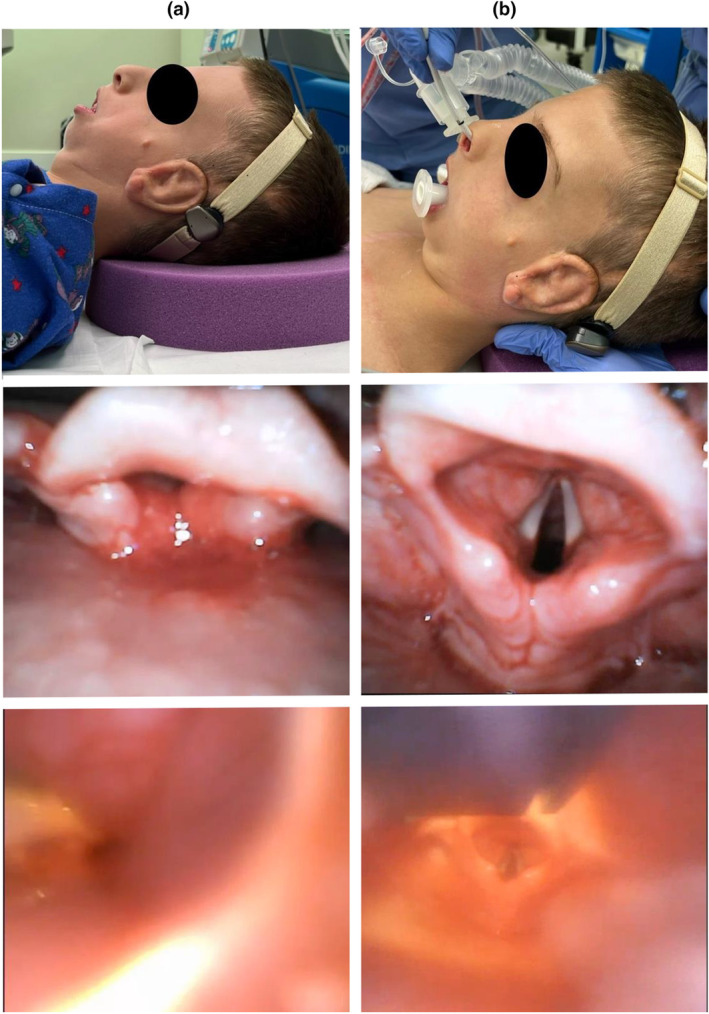
Findings on videolaryngoscopy and flexible endoscopy when the neck is in neutral and flexed positions are shown in (a) and (b), respectively.
Following image capture, the bronchoscope was advanced past the vocal cords into the trachea and vecuronium 0.1 mg.kg−1 was administered prior to advancement of the tracheal tube over the bronchoscope into the trachea. Anaesthesia was maintained with sevoflurane and fentanyl 1.5μg.kg−1 was administered for analgesia. At the conclusion of surgery, neuromuscular blockade was reversed with neostigmine 0.07 mg.kg−1 and glycopyrrolate 0.01 mg.kg−1. Tracheal extubation was performed once the patient was awake, breathing tidal volumes greater than 5 ml.kg−1 and able to protect his own airway.
Discussion
This case is an important reminder that patients with syndromes which associated with difficult airway management may become more difficult to manage with age, and that previous success is not an indicator of subsequent ease. Sometimes, atypical airway anatomy calls for atypical airway management. The interventions which increase exposure of the glottis for successful tracheal intubation can also improve ventilation via facemask and supraglottic airway device [7]. These techniques include atlanto‐occipital extension (sniffing position), chin lift and a jaw thrust to optimise pharyngeal tissue opening [8, 9]. However, in a patient with retrognathia, mandibular hypoplasia and posterior tongue position, manoeuvres to open the glottis and pharynx by bringing the mandible and soft tissues anteriorly may be of limited utility given the relatively fixed and posterior position of the mandible and retrograde anatomy of the tongue. Atlanto‐occipital neck flexion may limit posterior tongue displacement and shift the retrognathic and somewhat fixed mandible anteriorly. This flexion manoeuvre could therefore facilitate ventilation and glottic exposure despite being counter to standard paediatric airway management [9]. It is worth mentioning that sometimes the best management of a difficult airway is to do the least manipulation. In our case, we considered the possibility of conducting the case with a supraglottic airway device rather than pursuing tracheal intubation. However, the patient was not able to be effectively ventilated with a supraglottic airway device without the neck held in flexion, which would have been at odds with ideal operative positioning, which called for a more neutral position and the possibility of inadvertent intra‐operative positional manipulation by the surgeon. Additionally, the head of the bed would be turned away from the anaesthetist and the risk of losing the ability to ventilate due to supraglottic airway device dislodgement was deemed unacceptable.
Lessons from this patient's airway management include: (1) Mastery of airway management requires meticulous understanding of traditional airway techniques and tools; the importance of this knowledge is paramount in the rare instance when an atypical situation requires deviation from standard teaching; (2) Combined use of videolaryngoscopy and flexible bronchoscopy can be a great asset in managing the anatomically challenging airway [10].
Acknowledgements
This case report was published with the written consent of the patient's parents. R. Daly Guris is an editor of Anaesthesia Reports.
1 Attending Anaesthesiologist, Department of Anesthesiology and Critical Care Medicine, Children's Hospital of Philadelphia, Philadelphia, PA, USA
2 Assistant Professor, Department of Anesthesiology and Critical Care Medicine, University of Pennsylvania, Perelman School of Medicine, Philadelphia, PA, USA
3 Attending Anaesthesiologist, Department of Anesthesiology, Westchester, NY, USA
4 Associate Professor, Department of Anesthesiology and Critical Care Medicine, University of Pennsylvania, Perelman School of Medicine, Philadelphia, PA, USA
5 Anaesthesiologist, Princeton Medical Center, Envision Physician Services, Plainsboro, NJ, USA
6 Researcher, Resuscitation Science Center, Children's Hospital of Philadelphia, Philadelphia, PA, USA
References
- 1. Harless J, Ramaiah R, Bhananker SM. Pediatric airway management. Int J Crit Illn Inj Sci 2014; 4: 65–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. de Beer D, Bingham R. The child with facial abnormalities. Curr Opin Anaesthesiol 2011; 24: 282–288. [DOI] [PubMed] [Google Scholar]
- 3. Hosking J, Zoanetti D, Carlyle A, Anderson P, Costi D. Anesthesia for Treacher Collins syndrome: a review of airway management in 240 pediatric cases. Paediatr Anaesth 2012; 22: 752–758. [DOI] [PubMed] [Google Scholar]
- 4. Ross ED. Treacher Collins syndrome. An anaesthetic hazard. Anaesthesia 1963; 18: 350–354. [DOI] [PubMed] [Google Scholar]
- 5. Huang AS, Hajduk J, Rim C, Coffield S, Jagannathan N. Focused review on management of the difficult paediatric airway. Ind J Anaesth 2019; 63: 428–436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Kobayashi M, Ayuse T, Hoshino Y, et al. Effect of head elevation on passive upper airway collapsibility in normal subjects during propofol anesthesia. Anesthesiology 2011; 115: 273–281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Hiremath AS, Hillman DR, James AL, Noffsinger WJ, Platt PR, Singer SL. Relationship between difficult tracheal intubation and obstructive sleep apnoea. Bri J Anaesth 1998; 80: 606–611. [DOI] [PubMed] [Google Scholar]
- 8. Roth B, Magnusson J, Johansson I, Holmberg S, Westrin P. Jaw lift – a simple and effective method to open the airway in children. Resuscitation 1998; 39: 171–174. [DOI] [PubMed] [Google Scholar]
- 9. von Ungern‐Sternberg BS, Erb TO, Reber A, Frei FJ. Opening the upper airway – airway maneuvers in pediatric anesthesia. Paediatric Anaesth 2005; 15: 181–189. [DOI] [PubMed] [Google Scholar]
- 10. Stein ML, Park RS, Kiss EE, et al. Efficacy of a hybrid technique of simultaneous videolaryngoscopy with flexible bronchoscopy in children with difficult direct laryngoscopy in the Pediatric Difficult Intubation Registry. Anaesthesia 2023; 78: 1093–1101. [DOI] [PubMed] [Google Scholar]


