Abstract
Objective
This study describes recency of suicide attempt (SA) and suicidal ideation (SI) at index emergency department (ED) visit and post‐ED‐discharge reattempt among pediatric patients.
Methods
Secondary analysis from the ED Screen for Teens at Risk for Suicide study included patients ages 12–17 who reported a past SA during screening and received a phone call 3‐month post‐ED‐discharge assessing reattempt. Logistic regressions tested past SA/SI recency as predictors of reattempt. Descriptive statistics on SA/SI recency and reattempt are provided.
Results
Sample included 351 patients reporting a past SA during screening (70% cisgender female, 59% White, 53% psychiatric chief complaint, mean [SD] age = 15.3 [1.5]). 17% (60/351) reattempted suicide post‐ED‐discharge. Compared to patients who attempted over a year ago, patients with recent SA within 3 months, especially 1 week before screening, had greater odds of reattempting (3 months: p < 0.05, adjusted odds ratio [adjOR] = 3.1 [1.1–10.4]; 1 week: p < 0.01, adjOR = 4.8 [1.7–16.2]). Patients with recent SI within 24 h before screening had greater odds of reattempting than those with no recent SI (adjOR = 2.8 [1.1–7.6]; p < 0.05). 94% (64/68) of patients with a SA from over a year ago and no recent SI did not reattempt at follow‐up.
Conclusions
Pediatric ED patients have greater risk of reattempting suicide post‐discharge if their last SA was within the past 3 months−especially 1 week−and when most recent SI occurred within 24 h. Conversely, patients reporting SA over a year ago with no recent SI may require less immediate intervention. Findings support universal suicide risk screening and clinical pathways that use recency of SA to inform disposition.
HIGHLIGHTS
The relationship between suicide attempt (SA) and ideation recency and reattempt has not been examined among pediatric emergency department (ED) patients.
Pediatric ED patients are at greater risk of reattempting suicide if they report a SA from the past 3 months, or suicidal ideation (SI) from the past 24 h.
Pediatric patients with a past SA from over 1 year ago may be considered at lower risk of reattempt if they also deny recent SI.
Findings support universal suicide risk screening and clinical pathways that use recency of SA to inform disposition.
Youth suicide is a national public health crisis. In 2020, suicide claimed the lives of 1592 youth between the ages 12 and 17, accounting for 20% of all deaths in that age group (1). One of the strongest predictors of a suicide attempt (SA) is a past attempt (2), a risk factor shared by up to 40% of suicide decedents (3). Validated suicide risk screening tools used in medical settings often assess a patient's lifetime history of SAs, in addition to recent suicidal ideation (SI) (4, 5, 6). Data from multisite validation studies evaluating the Ask Suicide‐Screening Questionnaire (ASQ) showed up to 60% of youth and adults who screened positive for suicide risk reported a past SA (7).
Prior research has also demonstrated that suicide risk screening tools can predict future SAs (6) and suicide‐related emergency department (ED) visits (8, 9, 10). A SA within the last 6 months and SI within the past week have been identified as predictors of SA post‐ED‐discharge (11, 12). In addition, some studies have found that more recent SAs and ideation are associated with post‐hospitalization attempts among psychiatric inpatient youth (13, 14, 15). However, the relationship between recencies of attempt, ideation, and reattempt have not been specifically examined among pediatric ED patients. Identifying a potentially high‐risk period of recent SI and attempt for pediatric ED patients with a past attempt can inform clinicians in managing their care when they screen positive for suicide risk.
Accordingly, this study aimed to describe the association between the recency of a reported SA and SI (both relative to index ED visit), and reattempt within 3 months post‐ED‐discharge among pediatric ED patients with a past attempt. Clinical implications of findings for universal suicide risk screening are discussed.
METHODS
Setting and Participants
This study is a secondary analysis of the Emergency Department Screen for Teens at Risk for Suicide (ED‐STARS) study that developed the Computerized Adaptive Screen for Suicidal Youth (6). In the primary study, data were collected from pediatric ED patients ages 12–17 between July 2015 and July 2016 in 13 urban teaching hospitals across the United States. At their index ED visit, patients completed a survey that contained the ASQ (5) and Columbia Suicide Severity Rating Scale (C‐SSRS) (16, 17) to assess recent SI and attempt history. An enriched subsample (i.e., contained more patients who were deemed “high risk” based on whether they reported a past attempt or acute ideation) received a follow‐up phone call 3 months post‐ED‐discharge to assess whether they attempted suicide post‐discharge. Institutional Review Board approval and consent was obtained in all sites. More information on the ED‐STARS study is detailed elsewhere (6).
The present study included a subsample of participants who reported a past SA at their index ED visit, the date of their most recent SA, and the recency of their SI. All participants in the present study received a follow‐up call 3 months post‐ED‐discharge assessing reattempt status since being discharged. Patients were excluded if they reported an invalid recency value for their past attempt at their index ED visit. Figure 1 displays the flow of participant selection for the present study.
FIGURE 1.
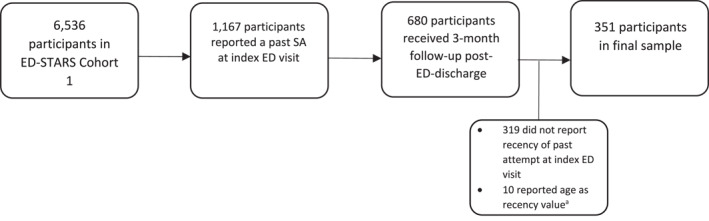
Participant selection flow chart.
aValues for recency of past suicide attempt in the ED‐STARS dataset were recorded as negative numbers to indicate days passed since the last suicide attempt. Ten recency values were nearly equivalent to the patients' age in number of days. ED‐STARS, Emergency Department Screen for Teens at Risk for Suicide; SA, suicide attempt.
Measures
Past SA
At the index ED visit, a past SA was measured by: (1) the ASQ, a validated suicide risk screening tool with four questions that measure recent SI and lifetime SA history (5), and (2) the C‐SSRS, a suicide risk assessment that quantifies severity of SI and behavior, which were embedded into the baseline survey (16). All participants in the present sample reported a past SA on either the ASQ item, “Have you ever tried to kill yourself?” or the C‐SSRS items of “Have you ever in your life made a SA?” or “Have you ever in your life tried to harm yourself because you were at least partly trying to end your life?” Recency of past SA was measured by a C‐SSRS item that measured the number of days between the participant's most recent attempt and their index ED visit. For each participant, recency of past SA relative to index ED visit was categorized into: “Past week,” “1 week to 3 months,” “3 to 6 months,” “6 months to 1 year,” “Over 1 year.”
Recent SI
Recent SI was assessed by binary (Yes/No) responses to items on the C‐SSRS and ASQ and categorized into discrete groups based on their most recent SI, such that there was no overlap of participants across time frames: “No recent SI” (“No” to all SI items), “Within the past 24 h” (“Yes” to C‐SSRS item “In the past 24 h, have you had any thoughts of killing yourself?”), “Between 24 h and 1 month” (“Yes” to ASQ item “In the past week, have you been having thoughts about killing yourself?” or C‐SSRS item “In the past month, have you had any thoughts of killing yourself?”).
Reattempt within 3 months post‐ED‐discharge
All participants had received a 3 months follow‐up phone call assessing whether they attempted suicide post‐ED‐discharge. A reattempt in this study was defined as (1) participant or parent report of a SA‐related ED‐visit or hospitalization in the past 3 months, and/or (2) participant endorsement of adapted C‐SSRS questions assessing SA in the past 3 months (“In the past 3 months, have you made a SA?” or “In the past 3 months, have you tried to harm yourself because you were at least partly trying to end your life?”). Exact dates of reattempts were not collected for the present study.
Statistical Analyses
All analyses were conducted using R Studio version 4.2.2. Descriptive demographic data were reported with means and standard deviations (SDs). Descriptive data were also reported for recency of SI, SA, and reattempt to supplement discussions on clinical implications for suicide risk management. Two logistic regressions, both controlling for age and presenting chief complaint, estimated the adjusted odds ratio (adjOR) and 95% CI of suicide reattempt post‐ED‐discharge associated with different time frames of SA and ideation recency, relative to index ED visit among the sample. An additional logistic regression for SA recency also controlled for past 24 h SI. Participants with reports of past attempts that occurred over a year before index ED visit, and reports of no recent SI, were used as reference groups, respectively.
RESULTS
Of the 6536 participants in the primary ED‐STARS study, 1167 (17.9%) reported a past SA at their index visit and were considered “high risk,” half (680/1167) of whom were selected to receive a follow‐up call 3 months post‐discharge per the study protocol (6). There were 329 participants excluded from the present study (319 did not report the recency of their past attempt, 10 reported invalid recency values). The final analysis included 351 participants who reported a past attempt at their index ED visit and its recency, answered items measuring recent SI, and provided a follow‐up response 3 months post‐ED discharge assessing suicide reattempt status screening (70% cisgender female, 59% White, 53% psychiatric chief complaint at index ED visit, mean [SD] age = 15.3 [1.5]) (Table 1).
TABLE 1.
Demographic and clinical characteristics of participants who endorsed a past attempt and reattempt. a , b
| Total sample (reported a past attempt at index ED visit and received a follow‐up, N = 351) | Participants who reattempted suicide within 3 months post‐ED‐discharge (n = 60; 17%) | |
|---|---|---|
| Age | 15.3 (1.5) | 15.0 (1.6) |
| Gender identity | ||
| Cisgender male | 71 (20.2) | 6 (11.7) |
| Cisgender female | 245 (69.8) | 45 (75.0) |
| Transgender/gender‐diverse | 34 (9.7%) | 8 (13.3) |
| Unavailable | 1 (0.3%) | ‐ |
| Race | ||
| White | 206 (58.7) | 39 (65.0) |
| Black | 69 (19.6) | 12 (20.0) |
| Asian | 1 (0.3) | 1 (1.7) |
| AI/AN | 3 (0.8) | ‐ |
| NH/PI | 2 (0.6) | 1 (1.7) |
| Multiracial | 32 (9.1) | 5 (8.3) |
| Unknown/unavailable | 40 (10.8) | 3 (3.3) |
| Ethnicity | ||
| Hispanic/Latino | 77 (21.9) | 10 (16.7) |
| Not Hispanic/Latino | 245 (69.8) | 45 (75.0) |
| Unknown/unavailable | 29 (8.3) | 5 (8.3) |
| Chief complaint | ||
| Medical/other | 165 (47.0) | 14 (23.3) |
| Psychiatric | 186 (53.0) | 46 (76.7) |
| ED disposition | ||
| Psychiatric admission/transfer c | 139 (39.6) | 36 (60.0) |
| Non‐psychiatric admission | 20 (5.7) | 2 (3.4) |
| Discharged | 188 (53.6) | 21 (35.0) |
| AMA/other | 4 (1.1) | 1 (1.6) |
| Recency of past attempt relative to index ED visit | ||
| Within the past week | 103 (28.8) | 31 (51.7) |
| 1 week to 3 months | 68 (19.0) | 12 (20.0) |
| 3–6 months | 43 (12.3) | 6 (10.0) |
| 6 months to 1 year | 41 (11.5) | 6 (10.0) |
| Over 1 year ago | 96 (27.4) | 5 (8.3) |
| Sole report of past attempt over 1 year ago with no past month SI | 68 (19.4) | 4 (5.9) |
| Recency of SI relative to index ED visit | ||
| No past month SI | 136 (38.7) | 12 (20.0) |
| The last 24 h | 143 (40.7) | 41 (68.3) |
| Between 24 h and 1 month | 72 (20.6) | 7 (11.7) |
AI/AN, American Indian/Alaskan Native; AMA, against medical advice; ED, emergency department; NH/PI, Native Hawaiian/Pacific Islander; SDs, standard deviations; SI, suicidal ideation.
Values are presented as n (%); age is calculated as a mean, so parentheses for the age row contains SDs. Medical/other chief complaint included unintentional injury and intentional injury by other. Psychiatric chief complaint included intentional self‐injury (non‐suicidal), psychiatric (non‐suicidal), SI (no suicide attempt), and suicidal attempt.
All 46 participants in the present sample who were transferred were transferred due to psychiatric reasons.
Recency of Past Attempt Before Index ED Visit, Full Sample
At their index ED visit, all participants reported a SA history: 28.8% (103/351) reported a prior SA that occurred within the week prior to their visit; 19.0% (68/351) between 1 week and 3 months before their visit; 12.3% (43/351) between 3 and 6 months before their visit; 11.5% (41/351) between 6 months and 1 year before their visit; and 27.4% (96/351) over a year before their visit (Table 1).
ED Disposition, Full Sample
Nearly 40% (139/351) of participants who reported a SA history at their visit were admitted or transferred for psychiatric reasons. 53.6% (188/351) were discharged.
Past Attempt and Past Month SI
At their index ED visit, 61.2% (215/351) of participants with SA histories also reported recent SI: 40.7% (143/351) experienced SI within 24 h before their index ED visit; 20.6% (72/351) between 24 h and 1 month before their visit (Table 1). Of the participants who experienced SI within 24 h before their visit, 79.0% (113/143) had attempted suicide in the past 3 months, with 61.5% (88/143) having attempted in the past week.
Past Attempt and No Past Month SI
Thirty‐nine percent (136/351) of participants who reported a past SA at their index ED visit denied recent SI. Half of these participants (68/138) attempted suicide over a year before their index ED visit (Table 1). Of that half, 94% (64/68) did not report reattempting suicide at follow‐up.
Reattempt Post‐ED‐Discharge and Recency of Past Attempt/Ideation
At the 3 months follow‐up, 17.1% (60/351) of the sample reattempted suicide after ED discharge; 76.7% (46/60) had presented to their index ED visit with a psychiatric chief complaint. 92% (55/60) of participants who reattempted during the follow‐up period had made a past SA within 1 year before their index ED visit, with 72% (43/60) occurring in the past 3 months before their index visit and 52% (31/63) occurring in the past week before their index visit. Regarding SI, 68% (41/60) of those who reattempted had reported experiencing SI within 24 h before their index ED visit.
Associations Between Recency of Past Attempt and Reattempt
In logistic regression analyses, those who attempted suicide within 1 week before their index ED visit had 4.8 times greater odds of a reattempt at 3‐month follow‐up compared to those who attempted over a year before their index ED visit (adjOR = 4.8 [95% CI = 1.7–16.2]). Patients whose most recent attempt occurred between 1 week and 3 months before their index ED visit had 3.1 times greater odds of a reattempt compared to those whose most recent attempt was over a year before their index ED visit (adjusted OR = 3.1 [95% CI = 1.1–10.4]). Past attempt recency categories of “3–6 months” and “6 months to 1 year” were not significantly associated with odds of reattempt (Table 2). When controlling for past 24 h SI, logistic regression analyses demonstrated that only patients with a SA from the past week had significantly greater odds of reattempting suicide (Table 2).
TABLE 2.
Recency of suicide attempt by suicide reattempt at 3 months post‐ED‐discharge: logistic regressions. a , b
| Recency of past suicide attempt prior to index ED visit | Adjusted OR (95% CI) | p‐value | Adjusted OR (95% CI) c | p‐value c |
|---|---|---|---|---|
| Past week | 4.8 [1.7–16.2] d | 0.01 | 3.7 [1.3–12.8] e | 0.02 |
| 1 week to 3 months | 3.1 [1.1–10.4] e | 0.04 | 2.8 [1.0–9.6] | 0.07 |
| 3–6 months | 2.6 [0.7–9.8] | 0.13 | 2.6 [0.7–9.6] | 0.14 |
| 6 months to 1 year | 3.0 [0.8–11.0] | 0.08 | 3.0 [0.8–1.0] | 0.09 |
| Over 1 year | Reference | Reference | Reference | Reference |
CI, confidence interval; ED, emergency department; OR, odds ratio.
Regression models are adjusted for age and chief complaint.
Model was also ran controlling for past 24 h suicidal ideation.
p < 0.01.
p < 0.05.
Associations Between Recency of SI and Reattempt
According to logistic regression analyses, patients with a past attempt who also reported experiencing SI within the past 24 h had greater odds of reattempting post‐ED‐discharge compared to those who denied recent SI (adjOR = 2.8 [95% CI = 1.1–7.6]). Past SI recency category of “24 h to 1 month” was not significantly associated with odds of reattempt (Table 3).
TABLE 3.
Recency of suicidal ideation by suicide reattempt at 3 months post‐ED‐discharge: logistic regression. a , b
| Recency of suicidal ideation prior to index ED visit | Adjusted OR (95% CI) | p‐value |
|---|---|---|
| Past 24 h | 2.8 [1.1–7.6] c | 0.04 |
| 24 h to 1 month | 0.9 [0.3–2.5] | 0.90 |
| No past month SI | Reference | Reference |
CI, confidence interval; ED, emergency department; OR, odds ratio.
Regression model is adjusted for age and chief complaint.
p < 0.05.
DISCUSSION
This secondary analysis of the ED‐STARS multisite study examined the association between recency of SA, SI, and suicide reattempt 3 months post‐discharge among a sample of pediatric ED patients with a past attempt. Notably, a SA in the past 3 months or SI within 24 h before the index ED visit was strongly associated with reattempt during the follow‐up period. When controlling for past 24 h SI, analyses revealed that a past week attempt was the only significant predictor for reattempt. Importantly, 94% of patients with a most recent attempt from over a year ago and no recent SI did not report a post‐ED‐discharge reattempt at follow‐up. These novel findings among a general pediatric ED sample of patients reporting a past attempt add to extant research that has primarily examined recency predictors of post‐hospitalization reattempt among psychiatric inpatients (13, 14, 15). Of note, 40% of the present study's sample of patients who reattempted suicide did not have a psychiatric‐related ED disposition. Moreover, nearly a quarter of patients who reattempted suicide post‐ED‐discharge had originally presented to their index ED visit with medical, non‐psychiatric chief complaints, demonstrating the utility of universal suicide risk screening for detecting occult suicide risk.
Clinical Implications: Detecting and Managing Suicide Risk
This study's findings have valuable clinical implications for universal suicide risk screening and suicide intervention in pediatric EDs. When patients screen positive for suicide risk and endorse a prior history of SA, clinicians may probe about the timing of the most recent attempt and SI during triage, which could inform their decision to discharge a patient from the ED. This is especially relevant for effectively managing patients who report a past attempt but deny any recent SI, who accounted for nearly 40% of the present study's sample of patients.
Three‐tiered suicide risk clinical pathways (brief screen, follow‐up safety assessment for patients who screen positive, disposition) are evidence‐based tools that can help clinicians feasibly detect and manage suicide risk in EDs (18, 19). Previous observations of universal screening demonstrated that between 30 and 50% of patients who screened positive for suicide risk reported a past attempt with no recent SI (7, 20). According to the clinical pathway, these patients received a follow‐up safety assessment at every visit, regardless of how long ago their last SA was. To accommodate busy workflows and minimize punitive effects of repeat safety assessments on patients with a past attempt, observational data were used to amend the pathway (20). In the amended pathway, patients with a past attempt and no recent SI may be considered “Lower Risk” if their attempt was over a year before their visit (20). The present findings provide novel empirical support for this clinical pathway amendment: Nearly all (94%) of the patients with no recent SI and a SA from over a year before their index ED visit did not reattempt post‐ED‐discharge.
Since a past attempt is one of the most potent risk factors for future attempt (2), patients with a distant past attempt (i.e., over a year ago) and no recent SI may still benefit from minimal interventions (e.g., providing updated clinical resource information, confirming they have a safety plan). Patients with a recent past attempt (i.e., within the past 3 months) may be considered at imminent risk and require more extensive evaluation and suicide intervention to mitigate risk of reattempt, relative to individuals with an attempt from over a year ago.
In the present study, over 65% of patients who reattempted suicide post‐ED‐discharge had reported SI within 24 h before their index ED visit. Reports of SI within 24 h were significantly associated with reattempt. Nearly 80% of patients who reported past 24‐h SI had a SA in the past 3 months. Findings align with prior research, which demonstrates that acute SI reported at an ED visit can predict future SA post‐discharge (11, 12). Importantly, a landmark adult ED study demonstrated that pairing universal suicide risk screening with a brief intervention (e.g., safety plan and follow‐up phone calls) decreased risk of post‐ED‐discharge SA by 30% (21). Taken together, these findings highlight the need to replicate findings on suicide risk screening and intervention in youth samples. Future research should continue developing brief suicide interventions that can be feasibly administered to high‐risk youth in the ED to mitigate their risk of attempting suicide post‐ED‐discharge (22, 23, 24).
Limitations
This study has the following limitations: First, suicide reattempts at follow‐up may have been underreported, given data was collected by either a guardian or youth. Second, not every participant who reported a past attempt were randomized to receive and return a follow‐up call in the primary study, resulting in possible selection bias and a loss of outcome data, including suicide mortality data. Third, we were unable to conduct any multivariate analyses examining the joint contribution of recent SI and SA on reattempts due to small cell sizes. Nonetheless, descriptive findings provide preliminary support for clinical implications on suicide risk pathways. Lastly, this study did not collect the exact date of reattempt between discharge and follow‐up, which could have provided more nuance to interpretation and clinical implications.
CONCLUSION
Pediatric ED patients who report attempting suicide in the past 3 months, or having SI within 24 h before their ED visit may be at greater risk of reattempting within 3 months post‐ED‐discharge. Pediatric patients with a past SA more than 1 year ago may be considered at lower risk of reattempt if they also deny recent SI. Findings align with existing clinical pathways that guide management of suicide risk as determined by screening. Future research should continue developing interventions that can mitigate risk of SA during the 3 month period following ED‐discharge.
This study was presented as an oral abstract at the Pediatric Academic Societies Meeting, Washington, DC, April 26–May 1, 2023; and in a symposium at the American Academy of Child and Adolescent Psychiatry Meeting, New York, NY, October 23–28, 2023.
This research was supported in part by the Intramural Research Program of the National Institute of Mental Health (Annual Report Number ZIAMH002922).
The authors would like to acknowledge the Pathways and Clinical Care Working Group at the American Academy of Child and Adolescent Psychiatrists (Drs. Khyati Brahmbhatt, Brian Kurtz, Khaled Afzal, Lisa Giles, Kyle Johnson, Elizabeth Kowal) and Dr. Ted Abernethy for their contributions to creating universal suicide risk screening clinical pathways. The authors also thank the Pediatric Emergency Care Applied Research Network (PECARN) Data Coordinating staff at Utah School of Medicine (UTAH), as well as the youth and families who participated in the ED‐STARS study.
All authors report no biomedical financial interests or potential conflicts of interest. This manuscript was prepared using the Emergency Department Screen for Teens at Risk for Suicide (ED‐STARS) Data Set obtained from the University of UTAH, and does not necessarily reflect the opinions or views of the ED‐STARS investigators or the Health Resources Services Administration (HRSA) Maternal Child Health Bureau (MCHB) Emergency Medical Services for Children (EMSC). The Pediatric Emergency Care Applied Research Network (PECARN) was funded by the HRSA/MCHB/EMSC. The information and conclusions in this manuscript are those of the authors and do not necessarily represent the official position of the NIMH, HRSA, HHS, or the U.S. Government.
REFERENCES
- 1. CDC . Web‐based injury statistics query and reporting system. 2023. Available from: https://www.cdc.gov/injury/wisqars/index.html. Accessed 29 Jan 2023.
- 2. Bostwick JM, Pabbati C, Geske JR, McKean AJ. Suicide attempt as a risk factor for completed suicide: even more lethal than we knew. Am J Psychiatr. 2016;173(11):1094–1100. 10.1176/appi.ajp.2016.15070854 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Cavanagh JT, Carson AJ, Sharpe M, Lawrie SM. Psychological autopsy studies of suicide: a systematic review. Psychol Med. 2003;33(3):395–405. 10.1017/s0033291702006943 [DOI] [PubMed] [Google Scholar]
- 4. Boudreaux ED, Jaques ML, Brady KM, Matson A, Allen MH. The patient safety screener: validation of a brief suicide risk screener for emergency department settings. Arch Suicide Res. 2017;21(1):52–61. 10.1080/13811118.2015.1040934 [DOI] [PubMed] [Google Scholar]
- 5. Horowitz LM, Bridge JA, Teach SJ, Ballard E, Klima J, Rosenstein DL, et al. Ask Suicide‐Screening Questions (ASQ): a brief instrument for the pediatric emergency department. Arch Pediatr Adolesc Med. 2012;166(12):1170–1176. 10.1001/archpediatrics.2012.1276 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. King CA, Brent D, Grupp‐Phelan J, Casper TC, Dean JM, Chernick LS, et al. Prospective development and validation of the computerized adaptive screen for suicidal youth. JAMA Psychiatr. 2021;78(5):540–549. 10.1001/jamapsychiatry.2020.4576 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Mournet AM, Bridge JA, Ross A, Powell D, Snyder DJ, Claassen CA, et al. A comparison of suicide attempt histories of pediatric and adult medical inpatients and implications for screening. Arch Suicide Res. 2022;26(3):1541–1555. 10.1080/13811118.2021.1931596 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Ballard ED, Horowitz LM, Jobes DA, Wagner BM, Pao M, Teach SJ. Association of positive responses to suicide screening questions with hospital admission and repeat emergency department visits in children and adolescents. Pediatr Emerg Care. 2013;29(10):1070–1074. 10.1097/pec.0b013e3182a5cba6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. DeVylder JE, Ryan TC, Cwik M, Wilson ME, Jay S, Nestadt PS, et al. Assessment of selective and universal screening for suicide risk in a pediatric emergency department. JAMA Netw Open. 2019;2(10):e1914070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Haroz EE, Kitchen C, Nestadt PS, Wilcox HC, DeVylder JE, Kharrazi H. Comparing the predictive value of screening to the use of electronic health record data for detecting future suicidal thoughts and behavior in an urban pediatric emergency department: a preliminary analysis. Suicide Life‐Threatening Behav. 2021;51(6):1189–1202. 10.1111/sltb.12800 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Arias SA, Miller I, Camargo CA Jr, Sullivan AF, Goldstein AB, Allen MH, et al. Factors associated with suicide outcomes 12 months after screening positive for suicide risk in the emergency department. Psychiatr Serv. 2016;67(2):206–213. 10.1176/appi.ps.201400513 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. King CA, Grupp‐Phelan J, Brent D, Dean JM, Webb M, Bridge JA, et al. Predicting 3‐month risk for adolescent suicide attempts among pediatric emergency department patients. J Child Psychol Psychiatry. 2019;60(10):1055–1064. 10.1111/jcpp.13087 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Goldston DB, Daniel SS, Reboussin DM, Reboussin BA, Frazier PH, Kelley AE. Suicide attempts among formerly hospitalized adolescents: a prospective naturalistic study of risk during the first 5 years after discharge. J Am Acad Child Adolesc Psychiatr. 1999;38(6):660–671. 10.1097/00004583-199906000-00012 [DOI] [PubMed] [Google Scholar]
- 14. Brent DA, Perper JA, Moritz G, Allman C, Friend A, Roth C, et al. Psychiatric risk factors for adolescent suicide: a case‐control study. J Am Acad Child Adolesc Psychiatr. 1993;32(3):521–529. 10.1097/00004583-199305000-00006 [DOI] [PubMed] [Google Scholar]
- 15. King CA, Segal H, Kaminski K, Naylor MW, Ghaziuddin N, Radpour L. A prospective study of adolescent suicidal behavior following hospitalization. Suicide Life‐Threatening Behav. 1995;25(3):327–338. 10.1111/j.1943-278x.1995.tb00955.x [DOI] [PubMed] [Google Scholar]
- 16. Posner K, Brown GK, Stanley B, Brent DA, Yershova KV, Oquendo MA, et al. The Columbia‐Suicide Severity Rating Scale: initial validity and internal consistency findings from three multisite studies with adolescents and adults. Am J Psychiatr. 2011;168(12):1266–1277. 10.1176/appi.ajp.2011.10111704 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Posner K, Brent D, Lucas C, Gould M, Stanley B, Brown G, et al. Columbia‐suicide severity rating scale (C‐SSRS). New York: Columbia University Medical Center; 2008. p. 10. [Google Scholar]
- 18. Blueprint for youth suicide prevention. Available from: https://www.aap.org/en/patient‐care/blueprint‐for‐youth‐suicide‐prevention/. Accessed 29 Jan 2023. [DOI] [PMC free article] [PubMed]
- 19. Brahmbhatt K, Kurtz BP, Afzal KI, Giles LL, Kowal ED, Johnson KP, et al. Suicide risk screening in pediatric hospitals: clinical pathways to address a global health crisis. Psychosomatics. 2019;60(1):1–9. 10.1016/j.psym.2018.09.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Horowitz LM, Bridge JA, Tipton MV, Abernathy T, Mournet AM, Snyder DJ, et al. Implementing suicide risk screening in a pediatric primary care setting: from research to practice. Acad Pediatr. 2022;22(2):217–226. 10.1016/j.acap.2021.10.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Miller IW, Camargo CA, Jr , Arias SA, Sullivan AF, Allen MH, Goldstein AB, et al. Suicide prevention in an emergency department population: the ED‐SAFE study. JAMA Psychiatr. 2017;74(6):563–570. 10.1001/jamapsychiatry.2017.0678 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Asarnow JR, Babeva K, Horstmann E. The emergency department: challenges and opportunities for suicide prevention. Child Adolesc Psychiatr Clin. 2017;26(4):771–783. 10.1016/j.chc.2017.05.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Schleider JL, Dobias ML, Sung JY, Mullarkey MC. Future directions in single‐session youth mental health interventions. J Clin Child Adolesc Psychol. 2020;49(2):264–278. 10.1080/15374416.2019.1683852 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Spirito A, Webb M, Cheek S, Wolff J, Esposito‐Smythers C. An update on the latest treatment approaches with suicidal adolescents. Curr Treat Options Psychiatry. 2021;8(2):64–76. 10.1007/s40501-021-00239-x [DOI] [Google Scholar]


