Abstract
Abstract
Background
A decrease in obtaining quality healthcare is a major cause of maternal and newborn deaths in low-income and middle-income countries. Ethiopia has one of the highest neonatal mortality rates. Increasing mothers’ health-seeking practices related to neonatal danger signs is an essential strategy for reducing the death rate of newborns. However, the pooled prevalence of mothers’ health-seeking practices related to neonatal danger signs is not well known in Ethiopia.
Objective
The main aim of this systematic review and meta-analysis is to assess the mothers’ health-seeking practices and associated factors towards neonatal danger signs in Ethiopia.
Design
Systematic review and meta-analysis.
Primary and secondary outcomes
The primary outcome was to assess the mothers’ health-seeking practices towards neonatal danger signs and the secondary outcome was to identify factors associated with health-seeking practices.
Methods
In total, comprehensive literature was searched in the PubMed, Google Scholar, HINARI, Embase and CINAHL databases published up to 30 December 2023. A random effect model was used to estimate the pooled prevalence and adjusted OR (AOR). Stata (V.17.0) was used to analyse the data. I2 statistics were computed to assess heterogeneity among studies. To minimise the underlying heterogeneity, a subgroup analysis was conducted based on the study region and year of publication. To assess publication bias, Egger’s test and funnel plots were used.
Results
Overall, 1011 articles were retrieved, and 11 cross-sectional studies, with a total of 5066 study participants, were included in this systematic review. The overall pooled prevalence of mothers’ health-seeking practices for neonatal danger signs in Ethiopia was 52.15%. Postnatal care follow-up (AOR 2.72; 95% CI 1.62 to 4.56), good maternal knowledge (AOR 3.20, 95% CI 2.24 to 4.56), educational status of secondary school and above (AOR 4.17, 95% CI 2.04 to 8.55), women’s decision-making autonomy (AOR 3.59, 95% CI 1.60 to 8.06) and place of delivery (AOR 2.71, 95% CI 1.21 to 6.04) were significantly associated with mothers’ health-seeking practices for neonatal danger signs.
Conclusion
The maternal health-seeking practices of women towards neonatal danger signs were found to be low in Ethiopia. When barriers to seeking care for newborn danger signs are successfully removed, women’s practices for seeking care for neonatal danger signs could decrease perinatal mortality.
Keywords: Meta-Analysis, Neonatal intensive & critical care, Paediatric intensive & critical care, NEONATOLOGY
STRENGTHS AND LIMITATIONS OF THIS STUDY.
A robust search algorithm to include studies from various databases.
The first prevalence estimates of mothers’ health-seeking practices for newborn danger signs in Ethiopia.
Identifying key factors crucial for maternal and neonatal health prevention.
The inclusion of only English articles and cross-sectional studies with a narrow focus.
Coverage of just three regions, potentially leaving other areas unrepresented.
Introduction
The word ‘neonatal danger signs’ (NDS) refers to clinically recognised markers that could point to a significant risk of newborn morbidity and death as well as the necessity of immediate medical treatment or intervention. Neonates often display non-specific symptoms and indicators of life-threatening illness. These symptoms may manifest in a newborn who presents to the hospital, over the course of a hospital stay or right after birth. Stabilisation and averting further deterioration are the goals of the first care given to a newborn exhibiting these symptoms.1 2 The notifiable causes of NDSs are neonatal jaundice, vomiting, cord sepsis, inability to suck breast milk, convulsions, hyperthermia/hypothermia, no urine in the first 24 hours, no bowel movement in the first 48 hours, a rapid breathing rate over 60 per minute, etc.3
The first 28 days of life remain the most crucial for a newborn’s survival. In 2020, 2.4 million infants worldwide passed away in their first month of life. 667 newborn perish every day, making up 47% of all child mortality. In 2020, sub-Saharan Africa had the highest rate of newborn mortality, with 27 (25–32) deaths per 1000 live births. When compared with developed nations, the number of neonatal deaths in the first month of life is more than 10 times higher in sub-Saharan Africa or southern Asia.4 5 Compared with other developing countries, Ethiopia has one of the highest neonatal mortality rates (29 deaths/1000 live births), Approximately half of the under-5 deaths reported in the 2016 and increasing to 30% of the 1000 live births reported in the 2019 Ethiopian Mini demographic health survey.6 7
Most neonatal deaths (75%) occur during the first week of life, and in 2019, approximately one million newborns died within the first 24 hours.4 80% of newborn deaths are known to be connected to three preventable and treatable disorders: prematurity-associated difficulties, intrapartum-related deaths (including asphyxia at birth) and neonatal infections. We have ways to deal with these problems and avoid long-term impairment.8 Half of maternal deaths and 61% of newborn deaths are attributed to poor quality care and delayed healthcare seeking is a major factor in neonatal mortality.9
The Sustainable Development Goals (SDGs) recognise this and mandate that by 2030, all countries must achieve a neonatal mortality rate—defined as the probability that a newborn will die before turning 28 days old, 12 or fewer deaths per 1000 live births.10 Mothers’ health-seeking practices regarding NDSs are poor in countries with low or middle incomes.11
A woman’s decision to seek care for her newborn may be delayed by a number of factors, including poor recognition of illness signs, a lack of decision-making skills, sociocultural traditions surrounding the seclusion of newborn, distance to a facility or provider, inadequate treatment received at facilities and insufficient funds for transportation or healthcare.11,13
Preventing delayed healthcare-seeking practices from pregnancy to the postnatal period and enhancing the quality of care provided to expectant mothers and newborn will be crucial to achieving the SDGs.9
Several studies on the practice of seeking healthcare for NDSs and the factors that are associated with this practice have been conducted in Ethiopia. The majority of the currently available studies are cross-sectional in design, have a narrow scope and are unable to address all regions of the country, we are unable to more precisely identify mothers’ health-seeking practices for NDSs and associated factors at the national level.
However, the pooled prevalence of mothers’ health-seeking practices related to NDSs is not well known in Ethiopia. Therefore, the main purpose of this systematic review was to determine the extent to which Ethiopian women practice seeking healthcare for NDSs and associated factors to provide reliable data that can support policy formulation and evidence-based decision-making.
Methods
A systematic review and meta-analysis was also conducted to estimate the pooled prevalence of mothers’ health-seeking practices for NDSs and their associated factors in Ethiopia. The Preferred Reporting Items for Systematic Review and Meta-Analysis guidelines were used to report the results14 (online supplemental information 1). Ethiopia is a country in the Horn of Africa that can be classified as low income. Ethiopia is split into 12 administrative regional states and 2 city administrations from an administrative standpoint.
Search strategies
The search strategy included international databases (ie, PubMed, Web of Science, Google Scholar and HINARI). This systematic review and meta-analysis included studies published up to 30 December 2023.
Our search terms used were “delivery of health care”[MeSH Terms] OR (“delivery”[All Fields] AND “health”[All Fields] AND “care”[All Fields]) OR “delivery of health care”[All Fields] OR “health”[All Fields] AND “care”[All Fields]) OR “health care”[All Fields]) AND seeking[All Fields] AND “behaviours”[All Fields] OR “behaviours”[MeSH Terms] OR “behaviour”[All Fields] OR “behaviours”[All Fields]) AND “practice”[All Fields] AND “infant, newborn”[MeSH Terms] OR (“infant”[All Fields] AND “newborn”[All Fields]) OR “newborn infant”[All Fields] OR “neonatal”[All Fields]) AND danger[All Fields] AND “diagnosis”[Subheading] OR “diagnosis”[All Fields] OR “signs”[All Fields] OR “diagnosis”[MeSH Terms]) AND “mothers”[MeSH Terms] OR “mothers”[All Fields]) AND “Ethiopia”[MeSH Terms] OR “Ethiopia”[All Fields]) (online supplemental additional file 1).
Inclusion criteria
Studies on mothers’ health-seeking practices towards NDSs published up to 30 December 2023 were included.
Exclusion
Studies that did not include qualitative research and studies with insufficient data were excluded from the study of mothers’ health-seeking practices for NDSs.
Data extraction
The datasets were exported to EndNote V.X8, after which the sequences were transferred to a Microsoft Excel spreadsheet for further analysis. The first step in the analysis involved removing any duplicate data from the review. To ensure accurate data extraction, three authors (WYF, BBE and TSY) independently extracted all the relevant data. In cases where there were disagreements between the reviewers, a second team of reviewers (MM, SBZ and EDY) was involved to resolve the discrepancies. The resolution process involved critical discussions and evaluations of the articles by an independent group of reviewers. The following information was extracted from the articles: author name, sample size, publication year, study area, region, study design, prevalence of mothers’ health-seeking practices for NDSs and adjusted ORs with 95% CIs for factors associated with mothers’ health-seeking practices for NDSs. By following this systematic data extraction process, the study aimed to ensure consistency and accuracy in capturing the relevant information from the selected articles.
Quality assessment
The quality of the studies was assessed using the Newcastle-Ottawa Quality Assessment Scale15 (online supplemental information 2). Three authors (WYF, BBE and TSY) independently assessed the quality of each study, covering various aspects such as methodological quality, sample selection, sample size, comparability, outcome assessment and statistical analysis. In cases of disagreement among the three authors during the quality assessment, three additional authors (MM, SBZ and EDY) were involved. Primary studies were considered to be of excellent quality if they had a score of 8 or higher. On the other hand, studies scoring between 6 and 7 points were considered to be of moderately high quality and were included in the meta-analysis and systematic review.
Measurement of outcome variables
The primary outcome examined in this systematic review and meta-analysis was the prevalence of mothers’ health-seeking practices for NDSs. Identifying factors associated with mothers’ health-seeking practices regarding NDSs was the second outcome of this study.
Data analysis
The data were entered into Microsoft Excel and subsequently exported to STATA V.17 statistical software for analysis.16 Heterogeneity between mothers’ health-seeking practices for NDSs was assessed by calculating the p values of I2 statistics.17
Heterogeneity was observed among the studies assessing the polled prevalence of maternal health-seeking practices related to NDSs in Ethiopia (I2=97.36%, p≤0.01). Therefore, random effect models were used to assess the pooled prevalence of mothers’ health-seeking practices for NDSs in Ethiopia. Subgroup analysis was performed to identify possible source heterogeneity according to the year of publication, sample size and region where the studies were conducted. Funnel plots and Egger regression tests were used to assess publication bias between the studies.18 Egger’s test was used to determine the statistical significance of publication bias, and a p value of less than 0.05 was used to declare the statistical significance of publication bias.19 In research where publication bias was detected, the Duval and Tweedie’s non-parametric trim-and-fill analysis was employed to adjust for publication bias.
Patient and public involvement
Patients and the public were not involved in the planning and design of the study.
Result
Characteristics of the included studies
This research has revealed how common mothers’ health-seeking practices for NDSs are in Ethiopia, as well as the factors that influence their use. PubMed, Google Scholar, HINARI, Embase, CINAHL and other sources described previously. A total of 1011 main studies were identified, with 342 articles remaining after eliminating 659 duplicates. 291 articles were excluded based on a review of their title and abstract, and the remaining articles underwent a full-text evaluation for inclusion criteria, resulting in the exclusion of an additional 61 papers. Ultimately, 11 papers met the eligibility criteria and were included in the final systematic review and meta-analysis (online supplemental figure 1).
Three of the studies included in the analysis were conducted in the Amhara region, four in Oromia and four in the South Nation Nationality and People Region of Ethiopia. All the studies that met the criteria for the meta-analysis and systematic review had a cross-sectional design and were reported in English. These studies collectively involved a total of 5066 participants, with individual sample sizes ranging from 285 to 772 participants. The prevalence of mothers’ health-seeking practices related to NDSs varied between 34.5% and 78.7%. The study with the highest prevalence of these practices was conducted by Kebede et al in the Amhara region, involving a sample size of 772 participants. In contrast, the study with the lowest prevalence was conducted by Abute Idris et al in the South Nation Nationality and People Region of Ethiopia, with a sample size of 421 participants (table 1).
Table 1. Descriptive summary of 11 studies about mothers’ health-seeking practices for neonatal danger signs and associated factors in Ethiopia: meta-analysis.
| Authors | Publication year | Region | Study period | Study design | Sample size | Prevalence (%) |
| Kebede et al13 | 2020 | Amhara | 01 July to 10 August 2019 | Cros-sectional | 772 | 78.7 |
| Gomora Tesfaye et al22 | 2022 | Oromia | 01 June to 27 November 2020 | Cross-section | 400 | 44 |
| Mesele et al21 | 2023 | SNNPR | 01 October to 30 October 2019 | Cross-section | 410 | 47.6 |
| Bulto et al31 | 2019 | Oromia | 01 February to 30 March 2018 | Cross-section | 404 | 60.5 |
| Bekele et al20 | 2020 | Oromia | 01 November 2018 to 30 October 2019 | Cross-section | 360 | 48.9 |
| Abute Idris et al26 | 2022 | SNNPR | 15 June to 16 July 2019 | Cross-section | 421 | 34.5 |
| Habtamu Chanie | 2019 | Amhara | June to September 2016 | Cross-section | 285 | 46.9 |
| Gebeyaw et al24 | 2017 | Amhara | 23 October to 17 November 2015 | Cross-section | 527 | 41.3 |
| T. Getachew et al32 | 2021 | SNNPR | 1 March to 30 March 2019 | Cross-section | 510 | 61 |
| Gomora Tesfaye et al22 | 2022 | Oromia | 1 June to 22 June 2020 | Cross-section | 407 | 57.6 |
| Ezo et al25 | 2023 | SNNPR | 1 February to 30 2020 | Cross-section | 570 | 52.2 |
SNNPRSouth Nation Nationalities and Peoples’ Regional State
Mothers’ health-seeking practices for NDSs in Ethiopia
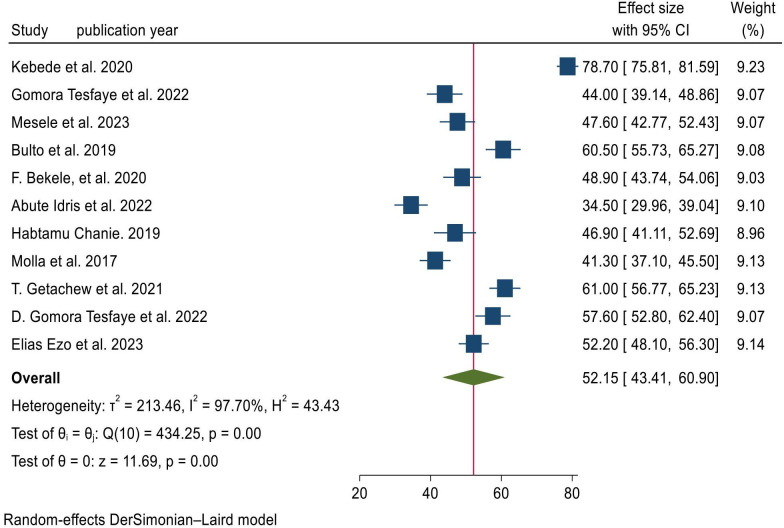
The overall pooled prevalence of mothers’ health-seeking practices for NDSs in Ethiopia was 52.15%, with 95% CI (43.41%, 60.90%). I2 statistics showed significant heterogeneity across the included studies (I2=97.70%, p≤0.001). As a result, random effect models were used to determine the pooled prevalence of mothers’ health-seeking practices for NDSs in Ethiopia. According to the included studies, the highest prevalence of maternal health-seeking practices for NDSs was reported by Kebede et al (78.70%) (75.81%, 81.59%), and the lowest was reported by Abute Idris et al (34.50%) (29.96%, 39.04%) (figure 1).
Figure 1. Forest plot for the pooled prevalence of mothers’ health-seeking practices for neonatal danger in Ethiopia, 2023.
Subgroup analysis of mothers’ health-seeking practices for NDSs in Ethiopia
According to the results of this systematic review and meta-analysis, the subgroup analysis by region showed that the pooled prevalence of health-seeking practices for NDSs was highest in the Amhara region (55.69%; 95% CI 29.23%, 82.15%; I2=99.18%; p=0.00). However, the results of the subgroup analysis were lowest for the South Nation Nationalities and Peoples’ Regional State (SNNPR) (48.85%; 95% CI 38.00%, 59.70%; I2=95.86%; p=0.00) (table 2).
Table 2. Subgroup analysis by region and year of publication on pooled mothers’ health-seeking practices for neonatal danger signs in Ethiopia.
| Subgroup analysis | Characteristics | Number of studies | Sample size | Pooled prevalence of health-seeking practices for neonatal danger signs (95% CI) | Heterogeneity (I2 %) | P value |
| Region | Amhara | 03 | 1584 | 55.69% (29.23%, 82.15%) | 99.18 | <0.001 |
| Oromia | 04 | 1571 | 52.77% (45.22%, 60.33%) | 89.51 | <0.001 | |
| SNNPR | 04 | 1911 | 48.85% (38.00%, 59.70%) | 95.86 | <0.001 | |
| Year of publication | 2019 and before | 03 | 1216 | 49.56% (37.65%, 61.47%) | 94.41 | 0.001 |
| After 2019 | 08 | 3850 | 53.11% (42.09%, 64.14%) | 98.11 | <0.001 | |
| Overall |
SNNPRSouth Nation Nationalities and Peoples’ Regional State
Meta-regression
Meta-regression was conducted to identify the possible source heterogeneity of mothers’ health-seeking practices and associated factors towards NDSs using the publication years and sample size. Of these factors, none of them were statistically significant (online supplemental table 1).
Sensitivity analysis
To identify any reports that are outliers and may have an effect on the pooled prevalence of health-seeking practices on NDSs by providing a wide CI and variance instability, we checked each study’s sensitivity. The results showed that there was no significant influence of individual study on the incidence of pooled health-seeking practices on NDSs (online supplemental figure 2).
Heterogeneity and publication bias
According to the findings of this study, there was markedly high heterogeneity across the studies, as evidenced by the I2 statistics (I2=97.70%, p≤0.001).
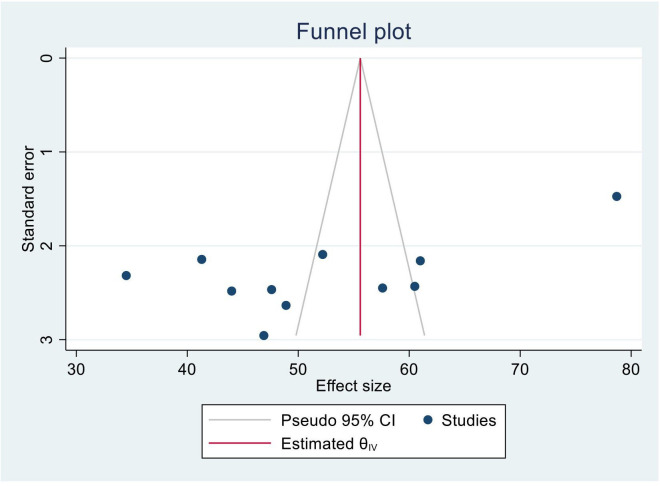
Publication bias among the included studies assessing health-seeking practices related to NDSs was checked using visual inspection of funnel plots and objectively by using Egger’s regression test. Publication bias was assessed using Egger’s test, which revealed statistical significance for estimating the prevalence of health-seeking practices related to NDSs in Ethiopia (p=0.0315), and the shape of the funnel plots was asymmetrical (figure 2). Duval and Tweedie’s non-parametric trim-and-fill analysis was conducted to correct publication bias among the 11 studies reporting on health-seeking practices for NDSs. However, no trimming was performed, indicating that the data were unchanged (online supplemental figure 3).
Figure 2. Funnel plot with a pseudo 95% CI for the pooled prevalence of maternal health-seeking practices towards neonatal danger signs in Ethiopia.
Factors associated with health-seeking practices for NDSs in Ethiopia
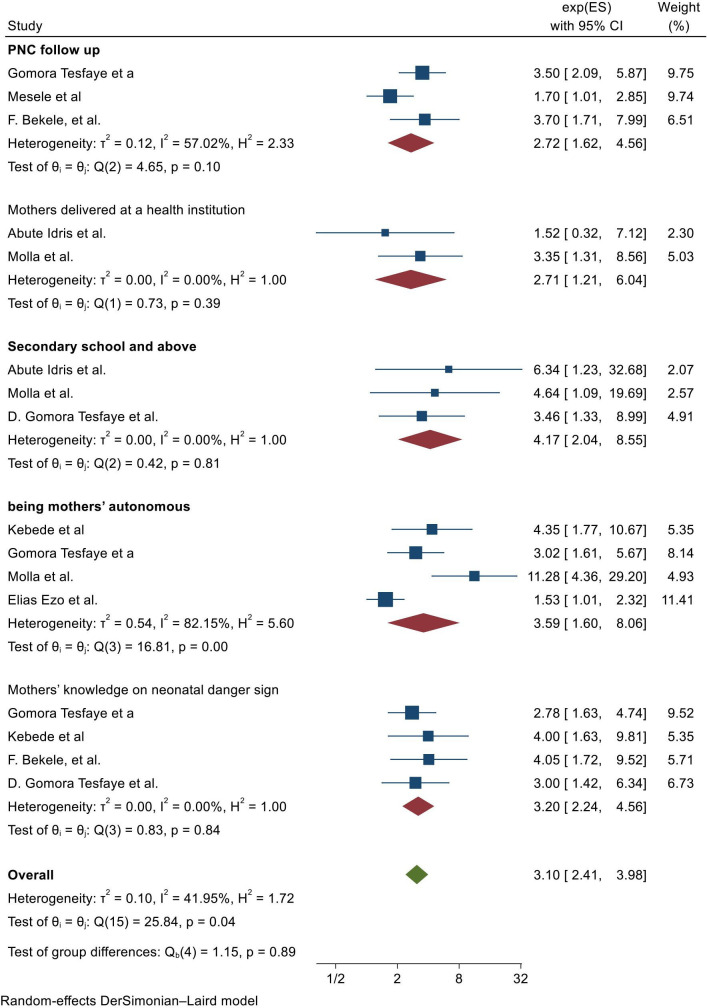
In our systematic review and meta-analysis, several factors were found to be significantly associated with health-seeking practices related to NDSs in Ethiopia. These factors include postnatal care (PNC) follow-up, knowledge of mothers, educational status secondary school and above, mothers’ autonomy and place of delivery.
The association between PNC follow-up and health-seeking practices for NDSs was evaluated in three studies.20,22
Women who had a PNC follow-up were 2.72 times more likely to health-seeking practices for NDSs than were their counterparts (adjusted OR (AOR) 2.72, 95% CI 1.62, 4.56). Heterogeneity was observed across the studies (I2=57.02%). Hence, a random effects model was used to evaluate the associations.
The pooled effect of four studies13 20 22 23 revealed that having good knowledge of NDSs was significantly associated with health-seeking practices. Mothers who had good knowledge of NDSs had health-seeking practices threefold greater than women mothers who had poor knowledge of NDSs (OR 3.20; 95% CI 2.24, 4.56).
Mothers’ decision-making power is another important factor significantly associated with appropriate health-seeking practices for NDSs. The pooled effect of four studies13 22 24 25 revealed that mothers who had full decision-making power were 3.59 times more likely to practice appropriate healthcare seeking for their sick neonates than mothers who had less decision-making power (AOR 3.59, 95% CI 1.60, 8.06).
The pooled effect of three studies23 24 26 also showed that maternal education level was associated with good healthcare-seeking practices; mothers with secondary education and higher were four times more likely than their counterparts to practice these practices (AOR 4.17, 95% CI 2.04, 8.55).
There was a significant association between institutional delivery and mothers’ health-seeking practices for NDSs. The pooled effect of two studies24 26 revealed that mothers who delivered a child at a health institution were 2.71 times more likely to seek neonatal medical care than mothers who delivered at home (AOR 2.71, 95% CI 1.21, 6.04) (figure 3).
Figure 3. Factors associated with mothers’ health-seeking practices towards neonatal danger signs in Ethiopia. PNC, postnatal care.
Discussion
To the best of the author’s knowledge, there is no pooled estimate of maternal health-seeking practices towards NDSs and their associated factors in Ethiopia. Therefore, this systematic review and meta-analysis provide the pooled prevalence of maternal health-seeking practices towards NDSs. A significant number of the world’s health problems could be resolved if children’s healthcare needs were adequately addressed. Improving the healthcare seeking for the health of newborn may avert many avoidable deaths.27 Therefore, this systematic review found it promising to estimate the pooled prevalence of maternal health-seeking practices towards NDSs and their associated factors in Ethiopia.
The pooled prevalence of health-seeking practices for mothers on NDSs in Ethiopia was 52.15%, with 95% CI (43.41, 60.90). This conclusion is consistent with the findings of a systematic review conducted in low-income and middle-income countries, which revealed that 59% of caregivers sought care during newborn illness.11 However, our findings were greater than those of a study conducted in Rajasthan.28 This may be the result of differences in social, cultural and health services factors that influence decisions to seek care and cause delays in seeking healthcare.29
These findings suggest regional variations in the prevalence of health-seeking practices for NDSs in Ethiopia, with higher rates observed in the Amhara region ((55.69%), while the SNNPR region (48.85%) had the lowest prevalence. The differences may reflect variations in healthcare practices, resource availability or other regional factors that influence health-seeking practices for NDSs and outcomes.
Compared with their counterparts, women who had a PNC follow-up were 2.72 times more likely to practice seeking healthcare for NDSs. This may be because postnatal counselling on NDSs is easily accessible and may help mothers become more knowledgeable about newborn illness, which provides a gateway to healthcare-seeking practices.
Mothers who had good knowledge of NDSs had threefold greater health-seeking practices than women mothers who had poor knowledge of NDSs. This could be due to parents’ lack of knowledge about NDSs during the neonatal period, which could cause parents to become confused and provide less quality care, affecting the health of the newborn and increasing the risk of neonatal morbidity and mortality.30
The pooled effect of four studies revealed that mothers who had full decision-making power were 3.59 times more likely to practice seeking appropriate healthcare for their sick neonates than mothers who had less decision-making power. The most significant barrier to seeking care during illnesses has been identified as ineffective or unfair decision-making, particularly regarding decision-making autonomy, which is crucial when seeking healthcare in an institutional setting.29
The pooled effect of three studies also showed that maternal education level was associated with good healthcare-seeking practices; mothers who had a secondary education or above were four times more likely to practice good healthcare-seeking than their counterparts. The rationale could be to educate women in community-based interventions about essential newborn care and birth preparedness, including danger sign recognition, which can increase healthcare seeking for neonatal danger by 40%.11 27
Mothers who gave birth in a hospital were 2.71 times more likely to seek neonatal healthcare than mothers who gave birth at home, according to the combined effect of two studies; therefore, the place of delivery influences maternal healthcare-seeking practices. Therefore, it is feasible that an increase in facility births will result in better newborn danger signs and healthcare seeking in practice.
Our study underscores the significant benefits of healthcare-seeking practices for both women and their newborn. Therefore, it is imperative that public health initiatives and community efforts focus on enhancing maternal health-seeking practices, particularly in response to NDSs.
Strength
First, we employed a robust search algorithm to incorporate studies from various databases. Second, our study offers the first-ever prevalence estimates of mothers’ health-seeking practice for newborn danger signs in Ethiopia. Additionally, we identified the factors influencing these health-seeking practices, which are essential for preventive maternal and neonatal health initiatives.
Limitations
This systematic review and meta-analysis has the following limitations: only articles published in English were included in the analysis. The majority of the currently available studies are cross-sectional in design, have a narrow scope and do not address all regions of the country, as only three regions were included in the analysis, leaving some regions potentially unrepresented.
Conclusion
According to the results of this systematic review and meta-analysis, maternal health-seeking practices involving NDSs were found to be low in Ethiopia. A higher educational status, PNC follow-up, good knowledge of NDSs, decision-making autonomy and giving birth at health institutions were factors associated with the health-seeking practices of women on NDSs.
After adjusting for these factors, women’s barriers to seeking healthcare for newborn danger signs can be effectively addressed, which might improve their healthcare seeking for neonatal illnesses and decrease perinatal mortality.
supplementary material
Acknowledgements
The authors would like to thank all authors and publishers of the original study.
Footnotes
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Prepublication history and additional supplemental material for this paper are available online. To view these files, please visit the journal online (https://doi.org/10.1136/bmjopen-2024-086729).
Provenance and peer review: Not commissioned; externally peer reviewed.
Patient consent for publication: Not applicable.
Data availability free text: Availability of data and materials All data relevant to the study are included in the article or uploaded as online supplemental information.
Patient and public involvement: Patients and/or the public were not involved in the design, or conduct, or reporting, or dissemination plans of this research.
Contributor Information
Wassie Yazie Ferede, Email: wassieyazie@gmail.com.
Tigist Seid Yimer, Email: tigistseid@yahoo.com.
Tiruset Gelaw, Email: tirusetgelaw@gmail.com.
Maru Mekie, Email: maru.mekie1@gmail.com.
Shimeles Biru Zewude, Email: nathanshimeles@gmail.com.
Getachew Mekete, Email: meketegetachew16@gmail.com.
Habtam Desse Alemayehu, Email: Habtamdesse153@gmail.com.
Fillorenes Ayalew Sisay, Email: flornceayalew@gmail.com.
Abeba Belay Ayalew, Email: ayaliew08@gmail.com.
Assefa Kebie Mitiku, Email: kebieassefa@gmail.com.
Enyew Dagnew Yehuala, Email: enydagnew@gmail.com.
Besfat Berihun Erega, Email: berihunbesfat@gmail.com.
Data availability statement
All data relevant to the study are included in the article or uploaded as online supplemental information.
References
- 1.WHO Guidelines Approved by the Guidelines Review Committee . Pocket book of hospital care for children: guidelines for the management of common childhood illnesses. Geneva: World Health Organization; 2013. [PubMed] [Google Scholar]
- 2.Anmut W, Fekecha B, Demeke T. Mother’s knowledge and Practice about Neonatal Danger Signs and Associated Factors in Wolkite Town, Gurage Zone, SNNPR, Ethiopia, 2017. J Biomedical Sci . 2017;06 doi: 10.4172/2254-609X.100077. [DOI] [Google Scholar]
- 3.Nusrat K, Khan MR, Waseem Z, et al. Neonatal danger signs and healthcare seeking behaviours: A cross-sectional study in Karachi amongst pregnant females. J Pak Med Assoc. 2020;70:74–9. doi: 10.5455/JPMA.3145. [DOI] [PubMed] [Google Scholar]
- 4.UNICEF United Nations Inter-agency Group for Child Mortality Estimation (UN IGME) Monit Situat Child Women. 2019;386:2276–86. [Google Scholar]
- 5.UNICEF Levels and trends in child mortality. 2021.
- 6.Ethiopia Demographic and Health Survey, 2016: ICF International, Rockville, Maryland, USA Central Statistical Agency. 2016.
- 7.Sahile A, Bekele D, Ayele H. Determining factors of neonatal mortality in Ethiopia: An investigation from the 2019 Ethiopia Mini Demographic and Health Survey. PLoS One. 2022;17:e0267999. doi: 10.1371/journal.pone.0267999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.World Health Organization Every newborn: an action plan to end preventable deaths. 2014.
- 9.Kruk ME, Gage AD, Arsenault C, et al. High-quality health systems in the Sustainable Development Goals era: time for a revolution. Lancet Glob Health. 2018;6:e1196–252. doi: 10.1016/S2214-109X(18)30386-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Nino FS. Sustainable Development Goals—United Nations. United Nations Sustainable Development. 2015.
- 11.Herbert HK, Lee ACC, Chandran A, et al. Care seeking for neonatal illness in low- and middle-income countries: a systematic review. PLoS Med. 2012;9:e1001183. doi: 10.1371/journal.pmed.1001183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Syed U, Khadka N, Khan A, et al. Care-seeking practices in South Asia: using formative research to design program interventions to save newborn lives. J Perinatol. 2008;28 Suppl 2:S9–13. doi: 10.1038/jp.2008.165. [DOI] [PubMed] [Google Scholar]
- 13.Kebede AA, Cherkos EA, Taye EB. Mother’s Knowledge of Neonatal Danger Signs and Health-Seeking Practices and Associated Factors in Debretabor, Northwest Ethiopia: A Community-Based Cross-Sectional Study. Res Rep Neonatol. 2020:47–58. [Google Scholar]
- 14.Moher D, Shamseer L, Clarke M, et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst Rev. 2015;4:1.:1. doi: 10.1186/2046-4053-4-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Peterson J, Welch V, Losos M, et al. The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. Ottawa: Ottawa Hospital Research Institute; 2011. pp. 1–12. [Google Scholar]
- 16.Ho AT, Huynh KP, Jacho-Chávez DT, et al. Data science in Stata 16: Frames, lasso, and Python integration. J Stat Softw. 2021;98:1–9. doi: 10.18637/jss.v098.s01. [DOI] [Google Scholar]
- 17.DerSimonian R, Kacker R. Random-effects model for meta-analysis of clinical trials: an update. Contemp Clin Trials. 2007;28:105–14. doi: 10.1016/j.cct.2006.04.004. [DOI] [PubMed] [Google Scholar]
- 18.Peters JL, Sutton AJ, Jones DR, et al. Comparison of two methods to detect publication bias in meta-analysis. JAMA. 2006;295:676–80. doi: 10.1001/jama.295.6.676. [DOI] [PubMed] [Google Scholar]
- 19.Sterne JA, Egger M. Funnel plots for detecting bias in meta-analysis: guidelines on choice of axis. J Clin Epidemiol. 2001;54:1046–55. doi: 10.1016/s0895-4356(01)00377-8. [DOI] [PubMed] [Google Scholar]
- 20.Bekele F, Bekele K, Mekonnen M, et al. Mothers’ knowledge and their health seeking behavior about neonatal danger signs and associated factors in Fiche town, Oromia region, Ethiopia. J Neonatal Nurs. 2020;26:324–9. doi: 10.1016/j.jnn.2020.03.001. [DOI] [Google Scholar]
- 21.Mesele M, Abebe K, Dessu S, et al. Mothers’ health care seeking behavior for neonatal danger sign in southern Ethiopia: Community based cross-sectional study. PLoS One. 2023;18:e0280993. doi: 10.1371/journal.pone.0280993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Gomora Tesfaye D, Geta G, Kene C, et al. Maternal Health Care Seeking Behavior for Neonatal Danger Signs and Associated Factors Among Post-Partum Mothers in Southeast Ethiopia: A Cross-Sectional Study. Inquiry. 2022;59 doi: 10.1177/00469580221143629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Gomora Tesfaye D, Dulla Koboto D, Gezahegn H. Maternal knowledge, health care seeking behaviour and associated factors for neonatal danger signs among postpartum mothers in Shashamane Town, Ethiopia: Cross sectional study. Int J Afr Nurs Sci. 2022;17:100438. doi: 10.1016/j.ijans.2022.100438. [DOI] [Google Scholar]
- 24.Gebeyaw M, Alemayehu G, Tefera B, et al. Health Care Seeking Behaviour on Neonatal Danger Signs among Mothers in Tenta District, Northeast Ethiopia: Community based cross- sectional study. Int J Nurs Midwifery. 2017;9:85–93. doi: 10.5897/IJNM2017.0266. [DOI] [Google Scholar]
- 25.Ezo E, Gezimu W. Health Care Seeking Behavior Towards Neonatal Danger Signs and Associated Factors Among Mothers in Kamba Zuria District, South Ethiopia. AJBSR . 2023;20:217–23. doi: 10.34297/AJBSR.2023.20.002694. [DOI] [Google Scholar]
- 26.Abute Idris Z, Tolu Feyissa G, Tesfaye Elilo L, et al. Healthcare-Seeking Behavior and Associated Factors for Newborn Danger Signs among Mothers Who Gave Birth in the Last 12 Months in Anlemo District. Adv Public Health. 2022;2022:1–11. doi: 10.1155/2022/7592832. [DOI] [Google Scholar]
- 27.Lassi ZS, Middleton PF, Bhutta ZA, et al. Strategies for improving health care seeking for maternal and newborn illnesses in low- and middle-income countries: a systematic review and meta-analysis. Glob Health Action. 2016;9:31408. doi: 10.3402/gha.v9.31408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Mohan P, Iyengar SD, Agarwal K, et al. Care-seeking practices in rural Rajasthan: barriers and facilitating factors. J Perinatol. 2008;28 Suppl 2:S31–7. doi: 10.1038/jp.2008.167. [DOI] [PubMed] [Google Scholar]
- 29.Lassi ZS, Middleton P, Bhutta ZA, et al. Health care seeking for maternal and newborn illnesses in low- and middle-income countries: a systematic review of observational and qualitative studies. F1000Res. 2019;8:200. doi: 10.12688/f1000research.17828.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Demis A, Gedefaw G, Wondmieneh A, et al. Women’s knowledge towards neonatal danger signs and its associated factors in Ethiopia: a systematic review and meta-analysis. BMC Pediatr. 2020;20:217. doi: 10.1186/s12887-020-02098-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Bulto GA, Fekene DB, Moti BE, et al. Knowledge of neonatal danger signs, care seeking practice and associated factors among postpartum mothers at public health facilities in Ambo town, Central Ethiopia. BMC Res Notes. 2019;12:549.:549. doi: 10.1186/s13104-019-4583-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Getachew T, Assebe Yadeta T, Gereziher T, et al. Determinants of maternal knowledge on neonatal danger signs and care-seeking practices in a rural area of southeastern Ethiopia. Int Health. 2022;14:610–8. doi: 10.1093/inthealth/ihab084. [DOI] [PMC free article] [PubMed] [Google Scholar]