Abstract
China’s “three-child policy”, implemented in response to population aging, has made the protection of maternal and infant health an urgent priority. In this environmental and medical big-data era, the Zhejiang Environmental and Birth Health Research Alliance (ZEBRA) maternity cohort was established with the aim of identifying risk factors for perinatal morbidity and mortality from the perspectives of both observational epidemiology and experimental etiology. Compared with conventional birth cohorts, the inclusion of a maternity cohort allows greater scope for research and places an emphasis on maternal health. In particular, it allows us to focus on pregnant women with a history of pregnancy-related illnesses and those planning to have a second or third child. There are currently many pressing issues in perinatal health, including the risk associations between exogenous together with endogenous factors and the occurrence of perinatal abnormalities, pregnancy complications, and adverse pregnancy outcomes. It is crucial to explore the interaction between environmental exposures and genetic factors affecting perinatal health if we are to improve it. It is also worthwhile to assess the feasibility of the early stage prediction of major perinatal abnormalities. We hope to study this in the ZEBRA cohort and also seek nationwide and international collaborations to establish a multicenter cohort consortium, with the ultimate goal of contributing epidemiological evidence to literature and providing evidence-based insights for global maternal and child healthcare.
Keywords: cohort profile, prospective maternity cohort, perinatal health, pre-eclampsia, preterm birth, low birth weight, environmental exposure
Introduction
Before the advent of modern medicine, childbirth carried an extremely high risk of maternal and perinatal morbidity and mortality. Fortunately, with advances in prenatal healthcare, the prevalence of maternal and perinatal adverse events has significantly decreased. However, gestational hypertension, postpartum hemorrhage, maternal infection, and other antepartum complications remain substantial health risks for pregnant women. Preterm birth, birth asphyxia, and congenital abnormalities still affect many babies all over the world. Under these circumstances, there is an urgent need to implement pragmatic measures to ensure the health of women during and after pregnancy and of children after birth.
Faced with the challenge of an aging population in China, the central government has advocated the “three-child policy” since 2021 to optimize population demographics and structure.1 This policy stresses the importance of maintaining optimal maternal health and screening during pregnancy. With these measures, the incidence of congenital anomalies such as Down syndrome, neural tube malformation, and congenital heart disease has been effectively reduced with new-generation high-sensitivity prenatal screening tools, including the “double-index method” for investigating cardiac murmurs and transcutaneous oxygen saturation for the timely detection of congenital heart disease.2 However, other perinatal issues such as preterm births (approximately 7.8% in China and approximately 5.9% in Zhejiang, a province in China) are still a concern.3,4 Preterm labor increases the risks of low birth weight,5 immature organ development,6 cerebral palsy,7 and cognitive impairment.8
Recent literature has highlighted the impacts of environmental exposures such as air pollution,9 proximity to green spaces,10 and extreme temperatures11 on maternal and child health. To understand the effects of such exogenous exposures as well as endogenous physiological factors on maternal and child health in Zhejiang, our investigators have been recruiting a comprehensive maternity cohort in this province since 2013. Recruitment was expanded to neighboring provinces over time, with the ultimate aim of nationwide coverage. This collaborative research network was formally named the “Zhejiang Environmental and Birth Health Research Alliance (ZEBRA)” in 2022 under the leadership of the Health Commission of Zhejiang Province. We have been able to recruit from pregnancies across the provinces from the electronic medical archiving system, as the cases of in-hospital births have increased tremendously. Over the past few decades, the rate of in-hospital births in China has surged from 60.7% in 1996 to 99.7% in recent years.12,13 In Zhejiang, that rate had already surpassed 99% in 200214 due to a developed healthcare system, abundant public health resources, presence of multilevel medical units in townships, and a strong emphasis on the health of the general population. We were thus able to recruit a longitudinal cohort with extensive information on both mothers and babies.
ZEBRA aims to investigate the associations between endogenous physiological factors and exogenous environmental factors with maternal and child health.15 Zhejiang is well-suited to lead this pioneering effort for several reasons. First, it is one of the most socioeconomically developed provinces in China, with low perinatal and neonatal mortality rates, allowing for a shift in research focus from individual-level clinical treatment to population-level risk prevention. Second, Zhejiang is a leader in cutting-edge interdisciplinary research with access to resources such as the Alibaba Cloud Intelligence Laboratory and the DAMO Academy (Academy for Discovery, Adventure, Momentum, and Outlook), which enable the storage and efficient cloud computing of vast medical records and genetic data. Further considerations are detailed in the Content S1. The first phase of ZEBRA’s research (2022–2026) focuses on screening risk factors, both endogenous and exogenous, and exploring the potential of early stage prediction for various types of perinatal adverse events.
Research Questions to Address
Perinatal complications include a range of maternal conditions such as gestational diabetes mellitus and pre-eclampsia16,17 as well as adverse pregnancy outcomes like stillbirth,18 preterm birth,19 and low birth weight.20 The pathogenesis of perinatal complications is complex and requires further exploration, making population-based cohort studies critical in this endeavor. These studies can identify wide-ranging risk factors that contribute to perinatal complications, such as insufficient nutrition intake during pregnancy,19,21,22 multiple gestation,23,24 short interval between pregnancies25 excessive workload,26 antepartum complications,27 psychological stress or depression,28,29 and hazardous environmental exposures (including both exposure to air pollutants and insufficient exposure to protective environmental factors).20,30−32 The findings from large cohort studies will have implications for screening high-risk pregnant women and reducing perinatal complications, major commitments made by ZEBRA upon its establishment.
Perinatal health protection necessitates collaborative efforts from both families and society. The well-being of women and children is indicative of a civilized society, promoting gender equality and protection for the vulnerable. ZEBRA seeks to foster ongoing advancements in clinical obstetric medicine and public health research and addresses several key scientific questions as follows:
First, are endogenous maternal physiological characteristics and exogenous environmental exposures associated with the occurrence of various perinatal complications? Also, can endogenous and exogenous risk factors interact to alter their impact on maternal and neonatal health?
Second, can detectable longitudinal changes in physiological characteristics and biomarkers of pregnant mothers serve as early indicators of potential perinatal health?
Third, is it possible to predict the risks of gestational complications during the middle or even early stages of pregnancy using routine clinical tests? Additionally, is it feasible to achieve rapid risk prediction with noninvasive tests that do not require cumbersome antenatal visits (e.g., attributes that can be easily collected on a smartphone), even among under-educated populations?
For a start, ZEBRA will work to establish multicohort collaboration and share findings within the China Cohort Consortium (CCC).33 We will assess the validity of our findings with other Chinese cohorts and study suitable interventions within the current Chinese economy and culture. In time, we hope to see whether our findings can be generalized to different populations and environments.
Cohort Profile in Brief
The ZEBRA Maternity Cohort is an open cohort designed to recruit pregnant women and follow them throughout pregnancy until 6 months after delivery, at which point the follow-up will end if no maternal or neonatal health issues are observed. All pregnant women who choose to give birth at any hospitals in cooperation and under the guidance agreement with Women’s Hospital, Zhejiang University School of Medicine are approached for inclusion in the ZEBRA Maternity Cohort, and consent is obtained for those willing to join the study. Across all 11 hospitals, the same diagnostic criteria and record-keeping is applied to ensure homogeneity in information collection and intercenter comparability. On 9 December 2021, the Health Commission of Zhejiang Province held a Press Conference on the standardization of medical records, which hopefully will allow us to include all pregnancies in Zhejiang. We are optimistic that this archiving standardization will spread to more provinces and that more records of pregnant women will become eligible for cohort inclusion in future years.
During the pilot study conducted from 2013 to 2016, 6,275 participants randomly selected from the scanned copy of handwritten medical documents were analyzed due to the lack of interactive data archiving techniques (otherwise, all medical records can be retrieved for cohort recruitment). Since 2017, Zhejiang has implemented a systematic electronic medical records system, and as of 31 December 31, 2022, a total of 118,689 pregnant women were enrolled in the ZEBRA Maternity Cohort (Figure 1). Among all the recruited participants, 63,887 (53.8%) underwent a 75 g oral glucose tolerance test (OGTT) at 24–28 weeks of gestation in hospitals using the same diagnostic standard. Cohort participants are mainly from Zhejiang, but with the recent expansion of research and medical collaboration, currently, 15.2% of the recruited pregnant women are from outside Zhejiang (Table S1). As ZEBRA is an observational cohort, no additional tests are required for participation.3 Detailed follow-up schedules are listed in Content S2.
Figure 1.
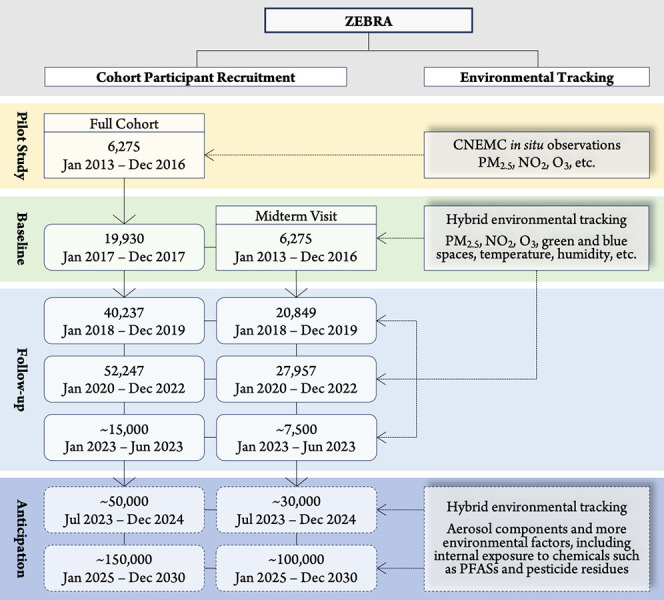
Flow diagram of pilot study, baseline recruitment, and follow-up for the Zhejiang Environmental and Birth Health Research Alliance (ZEBRA) maternity cohort study. ZEBRA was established in late 2022 when the design of the Maternity Cohort was completed; the information collection for newly recruited participants since 2023 is still ongoing, so approximate sample sizes are used to represent expectations. CNEMC, China National Environmental Monitoring Centre.
The sociodemographic characteristics collected include maternal age at delivery, ethnicity (Han or other minorities), occupation, educational attainment (graduate or above, undergraduate, college education, high school or below), place of residence (urban or rural), medical insurance type (New Rural Cooperative Medical Scheme, Urban Resident Basic Medical Insurance, and Urban Employee Basic Medical Insurance), and history of alcohol consumption and smoking, as summarized in Table 1.
Table 1. Statistics of Sociodemographic Features of ZEBRA Maternity Cohort Participants, 2013–2022.
| Feature | Mean (SD) or Count (%) | |
|---|---|---|
| Maternal Age at Delivery | 30.9 (4.3) | |
| Height (meter) | 1.6 (0.1) | |
| Prepregnancy BMI | 26.4 (3.1) | |
| Ethnicity (Han) | 116,671 (98.3%) | |
| Occupation | Office Staff | 94,494 (79.6%) |
| Worker | 13,929 (11.7%) | |
| Professional and Specialist | 2,879 (2.4%) | |
| Farmer | 1,045 (0.9%) | |
| Medical Staff | 364 (0.3%) | |
| Student | 157 (0.1%) | |
| Others | 5,821 (4.9%) | |
| Education Attainment | High School or below | 19,109 (16.1%) |
| College Education | 23,263 (19.6%) | |
| Undergraduate | 60,175 (50.7%) | |
| Graduate or above | 16,142 (13.6%) | |
| Type of Residence | Urban | 89,227 (75.2%) |
| Rural | 29,462 (24.8%) | |
| Type of Medical Insurancea | NCMS | 8,730 (7.4%) |
| URBMI | 7,450 (6.3%) | |
| UEBMI | 102,509 (86.4%) | |
| Alcohol or Smoking History | 112 (0.1%) |
Medical insurance include three types: New Rural Cooperative Medical Scheme (NCMS) for rural residents, Urban Resident Basic Medical Insurance (URBMI) for nonemployed urban residents, and Urban Employee Basic Medical Insurance (UEBMI) for employees.
The electronic medical record system collects a total of over 300 prepregnancy diseases and medical treatment items, among which 70 items have been empirically recognized to be associated with reproductive health with prevalence rates higher than 0.05% (diseases with occurrence rates below 0.05% are defined as rare diseases and are excluded from gestation-oriented epidemiological studies). Table 2 provides an overview of the prevalence rates of the 20 most common prepregnancy diseases and previous surgeries, while Table 3 lists 22 representative obstetric-relevant diagnoses, including gestational weight gain, gestational age in days, history of live birth, stillbirth, miscarriage, menarche age, neonate birth weight, and Apgar scores at 1 and 5 min. A full list of prepregnancy and gestational diagnostic items is detailed in Tables S2 and S3, respectively. A comprehensive array of 60 physiological and biochemical indices were examined during the parturient period and during OGTT, as outlined in Table S4. ZEBRA is currently preparing to collect genetic information from cohort participants for subsequent in-depth research from epigenetic and etiological perspectives.
Table 2. Cases and Prevalence Rates of 20 Representative Prepregnancy Diseases and History of Surgeriesa.
| Diseases or Surgeries | Cases (Prevalence, %) |
|---|---|
| Anemia | 20,084 (16.9%) |
| Assisted Reproduction Technology (ART) | 8,194 (6.9%) |
| Uterine Leiomyomas | 7,393 (6.2%) |
| Carrier of Hepatitis B Virus | 6,645 (5.6%) |
| History of Hepatitis B Infection | 5,129 (4.3%) |
| Liver Diseases | 2,070 (1.7%) |
| Cervical Incompetence | 1,413 (1.2%) |
| Hematopathy | 1,142 (1.0%) |
| History of Cervical Surgery | 968 (0.8%) |
| Thrombocytopenia | 690 (0.6%) |
| Cardiac Arrhythmia | 538 (0.5%) |
| Pelvic Inflammation | 466 (0.4%) |
| History of Syphilis | 434 (0.4%) |
| Cervical Polyps | 428 (0.4%) |
| Congenital Uterine Malformation | 351 (0.3%) |
| History of Intrahepatic Cholestasis of Pregnancy (ICP) | 313 (0.3%) |
| Cervical Conization (Cone Biopsy) and LEEPb | 303 (0.3%) |
| History of Hypertension | 277 (0.2%) |
| Nongestational Diabetes Mellitus | 242 (0.2%) |
| Depression | 180 (0.2%) |
“Prepregnancy diseases and history of surgeries” refer to the pre-existing maternal health conditions or diagnoses present before the current pregnancy, including surgeries undertaken for the purpose of the current pregnancy, such as the assisted reproduction technology (ART) for in vitro fertilization. Items are listed in descending sequence of prevalence rate.
LEEP: loop electrosurgical excision procedure.
Table 3. Statistics of Obstetric-Relevant Diagnoses Commonly Used in Clinical Practicea.
| Obstetric-Relevant Indicators | Mean (SD) or Count (%) |
|---|---|
| Gravidity | 2.1 (1.2) |
| Parity | 1.5 (0.6) |
| Abortion(s) or Miscarriage(s) | |
| 0 | 69,065 (58.2%) |
| 1 to 2 | 44,282 (37.3%) |
| 3 to 5 | 5,173 (4.4%) |
| above 5 | 169 (0.1%) |
| Live Birth(s) | |
| 0 | 66,803 (56.3%) |
| 1 | 48,994 (41.3%) |
| 2 | 2,707 (2.3%) |
| 3 or above | 186 (0.2%) |
| Spontaneous Singleton Delivery | 62,818 (52.9%) |
| Caesarean Singleton Delivery | 51,506 (43.4%) |
| Stillbirth | 1,605 (1.4%) |
| Gestational Age (in Days) | 271 (18) |
| Preterm Birth | 12,386 (10.4%) |
| Singleton Preterm Birth | 11,385 (9.6%) |
| Twins or Multiple Pregnancy | 4,926 (4.2%) |
| Spontaneous Preterm Birth | 6,738 (5.7%) |
| Singleton Spontaneous Preterm Birth | 5,332 (4.5%) |
| Singleton Medical Indicated Preterm Birth | 6,053 (5.1%) |
| Menarche Age (Years) | 13.9 (1.4) |
| Gestational Weight Gain (kg) | 13.5 (6.0) |
| Gestational Diabetes Mellitus | 22,393 (18.9%) |
| Gestational Hypertension | 2,465 (2.1%) |
| Pre-eclampsia | 6,553 (5.5%) |
| Severe Pre-eclampsia | 4,342 (3.7%) |
| Single-Symptom Intrahepatic Cholestasis of Pregnancy (ICP) | 2,872 (2.4%) |
| Multisymptomatic ICP | 724 (0.6%) |
| Birth Weight, Singleton (g) | 3,195 (580) |
| Low Birth Weight Infants, Singleton | 8,365 (7.0%) |
| Apgar Score, Singleton, 1 min | 9.7 (1.3) |
| Apgar Score, Singleton, 5 min | 9.9 (0.5) |
“Obstetric-relevant diagnoses” refer to all maternal and neonatal conditions related to the current pregnancy and childbirth, primarily including obstetric history (both times of pregnancy and delivery), severe maternal diseases during pregnancy, adverse pregnancy outcomes, and neonatal health status.
Tracking of Exogenous Risk Factors
The establishment of highly spatiotemporal-resolved databases has enabled the individual-level exposure tracking to air pollutants, including but not limited to particulate matters (i.e., PM2.5),34,35 nitrogen dioxide,36 and ozone.37−39 We are also able to track exposure to green space,40 humidity, and extreme temperatures41 through geospatial projection based on residential location. Any changes in the residential address will be updated along the way by trained investigators.
The current major challenge for accurate tracking of environmental exposures is achieving high temporal resolution and real-time tracking. Paradigmatic studies widely accept tracking short-term exposures to daily average precision42 and long-term tracking to monthly43 or yearly average precision.44 Intraday exposure variations are often not adequately captured, and a major reason for this is the limited ability of current-stage portable monitoring technologies in identifying high temporal-resolution microenvironment and physical activity changes.45 Additionally, requiring pregnant women to carry portable devices would impose an additional burden. Therefore, an important direction for future exploration is the development of wearable devices integrated with chemical and optical probes, pedometers, and GPS to enable high-resolution time-series tracking of close-to-person environmental exposures while simultaneously minimizing the physical burden on volunteers.
In the future, with the full operation of the Cloud Medicine platform, we propose to collect behavioral and lifestyle information such as dietary habits, physical exercise intensity and frequency, screen exposure, sleeping patterns, and mental conditions, together with behavioral changes for climate adaptation, history of medicine, and supplement use through smartphone applications (further details are provided in Content S3). For participants willing to provide biological samples, exposure levels to heavy metals (e.g., Pb and As) and organic chemical pollutants (e.g., perfluoroalkyl and polyfluoroalkyl substances and pesticide residue) will also be determined from various tissue samples.
Environmental Epidemiological Findings
ZEBRA has played a critical role in addressing research gaps related to screening for risk factors associated with maternal, perinatal, and neonatal diseases among Chinese females (see summaries in Content S4).3,15,46−60 Among the long-time studies, findings in the field of environmental epidemiology warrant highlighting.
Air pollution has been identified as a critical risk factor for pregnancy complications such as miscarriage, preterm birth, and stillbirths as reported in literature.18,61,62 In the pilot study of ZEBRA with a sampled preterm birth prevalence rate of 5.5%,3 we estimated that the risk of preterm birth would increase by 13% (95% confidence interval, CI: 3–25%) and 12% (95% CI: 5–19%) with every 10 μg/m3 increased exposure to PM2.5 and ozone, respectively. Additionally, we found that low body mass index (BMI), multiple gravidity, and hypertension in pregnancy (regardless of whether it was primary or pregnancy-induced) also contributed to the risk of preterm labor. These findings were further confirmed in our subsequent comprehensive study with over 100,000 participants, yielding more robust statistical results.60 Furthermore, we discovered synergistic effects of combined risks among air pollutants, while exposure to green spaces exhibits antagonistic effects on the hazards of air pollution exposure. The environmental exposure window also includes the prepregnancy year, indicating the importance of planned conception to avoid risky environmental exposures at an earlier phase.
ZEBRA also found that maternal gestational diseases can be associated with environmental exposures to varying degrees.60 Focusing on intrahepatic cholestasis of pregnancy (ICP), the risk of multisymptomatic ICP, as per strict diagnostic criteria, is significantly associated with maternal exposure to PM2.5 (RR = 1.070, 95% CI: 1.012–1.131) and ozone (RR = 1.064, 95% CI: 1.021–1.108), whereas the associations are comparatively lower for single-symptom ICP. Additionally, gestational morbidity, particularly cardiovascular diseases, can aggravate the risk associations between air pollution exposure and adverse pregnancy outcomes.63 These epidemiological findings enable us to generate hypotheses from observational risk associations and encourage causal inquiries into the etiology of various perinatal complications, which highlight the importance of disciplines such as environmental epidemiology and epigenetics. From a macro-perspective of risk intervention, identifying statistically significant risk factors before the confirmation of causality can facilitate risk control to achieve wider population health protection.
Prospects for the Future
Numerous birth cohorts have been established in China.64−75 Among them, the representative ones include the China National Birth Cohort (CNBC), which has the largest participant coverage in China, the Shanghai Birth Cohort (SBC) with the most comprehensive research themes (aiming to study the effects of genetic, environmental, and behavioral factors on fertility, pregnancy outcomes, child growth and development, and disease risk),68 and the Born in Guangzhou Cohort Study (BIGCS), targeting in-depth exploration from the genetic perspective.66,67 In general, the common characteristic of China’s current birth cohorts is to focus research on birth defects and growth abnormalities in newborns. Conversely, our established cohort, while retaining the main features of traditional birth cohorts, pays special attention to maternal health. Because previous research was based on the background of China’s “one-child family planning” policy,76 equal weight was given to the health of pregnant mothers and newborns. However, with the implementation of the “three-child policy”,1 it is anticipated that there will be an increase in the number of women expecting more children, which drives the need for more research attention to shift toward pregnant women, especially those with multiple children.
However, the present stage of the ZEBRA maternity cohort design still has limitations. First, during the pilot study conducted from 2013–2017, the estimated relative risk values between preterm birth and maternal exposure to air pollutants were highly uncertain due to the small sample size and the lack of effective adjustment for multipollutant cross-confounding effects. The risk estimations will be updated in subsequent comprehensive epidemiological studies involving a wider cohort. Second, the current ZEBRA cohort study considers relatively few variables related to behavioral characteristics, which are theoretically only obtainable through self-reporting by participants and thus often have lower credibility. The “Cloud Healthcare” platform is anticipated to enhance the client-based questionnaire survey through artificial-intelligence-driven optimization in the next 2 years. Improvements in the frequency and capacity of data collection and the implementation of double verification are among the goals for achieving more reliable self-reported indicators by 2026.
Lastly, while the current data structure used for analysis categorizes populations based on physiological and biochemical indicators and medical history, genetic factors are theoretically the primary method for distinguishing endogenous differences. However, due to ethical requirements, national-level genetic research control, limitations in efficient detection technology, and lower willingness of pregnant women to share genetic information, genetic-level cohort studies are not scheduled to be fully implemented before 2025. Moreover, the number of newborns in Zhejiang was at a high of 434,433 for 2021, whereas comparatively, participants currently enrolled in the ZEBRA Maternity Cohort are still rather inadequate for full representativeness. This compromise was made to ensure that the assessment of the recruited participants had the same quality control standards and criteria. To enhance the generalizability of research findings, it is advisable for cohorts to include broader populations.
Therefore, ZEBRA is planning to establish long-term collaborations with cohorts from other countries with participants of Chinese ethnicity such as Singapore. The Singaporean Growing Up in Singapore Toward Healthy Outcomes (GUSTO)77 and Singapore Preconception Study of Long-Term Maternal and Child Outcomes (S-PRESTO)78 cohorts have collected comprehensive genetic and behavioral information and have been continuously tracking the growth and development of children since birth. In addition, S-PRESTO has collected information on women’s health since preconception, and this allows the earliest precursors of disease development to be determined. Follow up of these cohorts is still ongoing, and there is potential to harmonize the data as well as implement similar assessments in ZEBRA, GUSTO, and S-PRESTO. China-Singapore collaborations can extend the research scale from preconception until the end of child development and assess genetic, physiological, and sociological multidimensional risk factors.
ZEBRA has pledged to provide evidence-based research conclusions on maternal health for the Chinese population, considering that a majority of high-quality cohort studies has been established in Western countries. ZEBRA aims to set an example in the standardized management of electronic medical records for mother-child pairs at the provincial and national level. Optimized algorithmic models for screening risk prediction and identification of risk factors using data mining techniques can be promptly applied to pregnant women in the first trimester. This approach will improve maternal health risk assessment and continually improve as information is updated dynamically with the inclusion of new cohort participants. Moreover, ZEBRA will take on the responsibility of disseminating research findings to the general public, aiming to enhance public awareness of risks and effectively implement self-directed risk control measures.
Healthcare workers, whether gynecologists, physicians, nurses, or medical students, remain dedicated to providing the most professional and comprehensive healthcare service for women who wish to give birth. The medical and research community is committed to leaving no one behind. Currently, various factors influence birth rates among young people. By establishing the ZEBRA cohort, we aim to publish high-quality research reports and provide epidemiological evidence for global maternal and child healthcare. In this way, Zhejiang will contribute to the achievement of the “Healthy China 2030” vision and the United Nations’ Sustainable Development Goals, including SDG3 in maternal and child health.
Acknowledgments
The authors wish to extend their appreciation to several entities for their contributions in the establishment of ZEBRA. Special appreciation is given to Professor Weiguo Lu, the chief director of the Key Laboratory of Women’s Reproductive Health, located in Hangzhou, Zhejiang. Specifically, (1) the Department of Maternal Healthcare at Women’s Hospital, School of Medicine, Zhejiang University, and (2) the Maternal and Child Health Division at the Health Commission of Zhejiang Province are acknowledged for providing comprehensive support. In addition, (3) the TAP (Tracking Air Pollution in China) team at Tsinghua University, (4) the Institute of Reproductive and Child Health, National Health Commission Key Laboratory of Reproductive Health, and the Department of Epidemiology and Biostatistics at the School of Public Health, Peking University Health Science Centre, (5) the School of Atmospheric Sciences at Nanjing University, (6) the Vanke School of Public Health at Tsinghua University, and (7) the School of Public Health and Preventive Medicine at Monash University (Australia) are also acknowledged for their technical assistance. Finally, the authors express gratitude to all ZEBRA cohort participants, as well as the coordinators, administrative and technical staff, and participant interviewers who have made valuable contributions to the cohort study.
Biography
Xiaoxia Bai, Ph.D. Senior Consultant, Principal Investigator of Obstetrics, Women’s Hospital, Zhejiang University School of Medicine. Doctor Bai has been devoted to studies of maternal and fetal medicine, skilled in the treatment of critically ill pregnant women and the impact of environmental exposure on maternal and fetal health. Currently, she serves as an Executive Committee Member of the Obstetrics and Gynecology Branch of the China Healthcare Promotion Association, Executive Committee Member of the Perinatal Medicine Special Committee of the China Association of Traditional Chinese and Western Medicine, Chair of the Perinatal Medicine Special Committee of the Zhejiang Medical Association, and Chair of the Early Life Development and Disease Prevention and Control Special Committee of the Zhejiang Association of Preventive Medicine.
Data Availability Statement
ZEBRA is a valuable resource for the research community, offering a wide range and depth of clinical diagnostic information and individual-level tracking of environmental exposure (e.g., PM2.5, ozone, green space, and abnormal temperature). While the study database is not publicly available, ZEBRA warmly welcomes potential collaborations, and such requests are considered on a case-by-case basis. Progress of the cohort will be updated on MedRxiv: 10.1101/2023.02.21.23286173. Researchers seeking access to the data set are required to obtain approval from the designated ZEBRA research proposal review committee, comprising members of the School of Medicine at Zhejiang University and the Maternal and Child Health Division of the Health Commission of Zhejiang Province. International researchers seeking additional information regarding collaboration and data access are encouraged to contact the lead authors, Dr. Xiaoxia Bai (baixiaoxia@zju.edu.cn) and Dr. Haitong Zhe Sun (ht.sun@nus.edu.sg).
Supporting Information Available
The Supporting Information is available free of charge at https://pubs.acs.org/doi/10.1021/envhealth.4c00104.
Detailed reasons for choosing Zhejiang province as pilot site; cohort follow-up design; questionnaire-based lifestyle and behavioral pattern collection; overview of published studies based on ZEBRA maternity cohort; provincial distribution of ZEBRA maternity cohort participants; full list of cases and prevalence of prepregnancy diseases and histories of surgeries; full list of statistics on obstetric-relevant diagnostic indicators; full list of biochemical indices at parturient period and oral glucose tolerance test in second trimester, 24–28th gestational week (PDF)
Author Contributions
⊥ H.Z.S. and H.T. contributed equally. Haitong Zhe Sun: Conceptualization, Formal Analysis, Methodology, Software, Investigation, Writing - Original Draft, Writing - Review & Editing, Visualization, Supervision, Project Administration, Funding Acquisition; Xiaoxia Bai: Conceptualization, Methodology, Resources, Investigation, Data Curation, Validation, Supervision, Project Administration, Funding Acquisition; Yuming Guo: Methodology, Software, Supervision, Funding Acquisition; Wei Xu: Investigation, Supervision, Project Administration; Haiyang Tang: Formal Analysis, Methodology, Resources, Data Curation, Writing - Original Draft, Writing - Review & Editing; Qingyi Xiang, Siyuan Xu, Yijia Tian, Huan Zhao, Jing Fang, Haizhen Dai, Rui Shi, Yuxia Pan, Ting Luo, Hangbiao Jin, Chenyang Ji, Yuanchen Chen, Meirong Zhao, and Kun Tang: Methodology, Resources, Data Curation; Sheena Nishanti Ramasamy, Evelyn Xiu-Ling Loo, and Lynette P. Shek: Writing - Review & Editing; Hengyi Liu: Resources, Data Curation. All authors have read and approved the final manuscript.
The research has received funding from various sources, including the Zhejiang Province Health Innovative Talent Project (A0466), the International Cooperation Seed Program of Women’s Hospital, Zhejiang University (GH2022B008-01 and GH2024005), the Australian Research Council (DP210102076), the Australian National Health and Medical Research Council (APP2000581), the UK Research and Innovation (UKRI) Centre for Application of Artificial Intelligence to the Study of Environmental Risks (AI4ER, EP/S022961/1), the Start-up Grant from Yong Loo Lin School of Medicine, National University of Singapore (NUHSRO/2024/045/Startup/06), and the US-China Fulbright Program.
The authors declare no competing financial interest.
Notes
The study obtained written informed consent from all participants, and the research involves the use of deidentified personal information for scientific purposes. The ZEBRA cohort study is approved by the ethics committee of the Women’s Hospital, School of Medicine, Zhejiang University (IRB-20220189-R).
Supplementary Material
References
- Tatum M. China’s three-child policy. Lancet 2021, 397 (10291), 2238. 10.1016/S0140-6736(21)01295-2. [DOI] [PubMed] [Google Scholar]
- Wang D.; Zhang Y.; Jiang Y.; Ye Y.; Ji M.; Dou Y.; Chen X.; Li M.; Ma X.; Sheng W.; Huang G.; Yan W. Shanghai Preconception Cohort (SPCC) for the association of periconceptional parental key nutritional factors with health outcomes of children with congenital heart disease: a cohort profile. BMJ. open 2019, 9 (11), e031076 10.1136/bmjopen-2019-031076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sun Z.; Yang L.; Bai X.; Du W.; Shen G.; Fei J.; Wang Y.; Chen A.; Chen Y.; Zhao M. Maternal ambient air pollution exposure with spatial-temporal variations and preterm birth risk assessment during 2013–2017 in Zhejiang Province, China. Environ. Int. 2019, 133 (Pt B), 105242. 10.1016/j.envint.2019.105242. [DOI] [PubMed] [Google Scholar]
- Qiao J.; Wang Y.; Li X.; Jiang F.; Zhang Y.; Ma J.; Song Y.; Ma J.; Fu W.; Pang R.; Zhu Z.; Zhang J.; Qian X.; Wang L.; Wu J.; Chang H.-M.; Leung P. C. K.; Mao M.; Ma D.; Guo Y.; Qiu J.; Liu L.; Wang H.; Norman R. J.; Lawn J.; Black R. E.; Ronsmans C.; Patton G.; Zhu J.; Song L.; Hesketh T. A Lancet Commission on 70 years of women’s reproductive, maternal, newborn, child, and adolescent health in China. Lancet 2021, 397 (10293), 2497–2536. 10.1016/S0140-6736(20)32708-2. [DOI] [PubMed] [Google Scholar]
- Goldenberg R. L.; Culhane J. F. Low birth weight in the United States. Am. J. Clin. Nutr. 2007, 85 (2), 584S–590S. 10.1093/ajcn/85.2.584S. [DOI] [PubMed] [Google Scholar]
- Steer P. The epidemiology of preterm labour. BJOG 2005, 112 (Suppl 1), 1–3. 10.1111/j.1471-0528.2005.00575.x. [DOI] [PubMed] [Google Scholar]
- Mallard C.; Davidson J. O.; Tan S.; Green C. R.; Bennet L.; Robertson N. J.; Gunn A. J. Astrocytes and microglia in acute cerebral injury underlying cerebral palsy associated with preterm birth. Pediatr. Res. 2014, 75 (1–2), 234–40. 10.1038/pr.2013.188. [DOI] [PubMed] [Google Scholar]
- Moster D.; Lie R. T.; Markestad T. Long-term medical and social consequences of preterm birth. N Engl J. Med. 2008, 359 (3), 262–73. 10.1056/NEJMoa0706475. [DOI] [PubMed] [Google Scholar]
- Bekkar B.; Pacheco S.; Basu R.; DeNicola N. Association of Air Pollution and Heat Exposure With Preterm Birth, Low Birth Weight, and Stillbirth in the US: A Systematic Review. JAMA Netw Open 2020, 3 (6), e208243 10.1001/jamanetworkopen.2020.8243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang L.; Shi S.; Wu S.; Yang Y.; Xu J.; Zhang Y.; Wang Q.; Shen H.; Zhang Y.; Yan D.; Peng Z.; Liu C.; Wang W.; Jiang Y.; Shi S.; Chen R.; Kan H.; He Y.; Meng X.; Ma X. Effects of greenness on preterm birth: A national longitudinal study of 3.7 million singleton births. Innovation 2022, 3 (3), 100241. 10.1016/j.xinn.2022.100241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ren M.; Wang Q.; Zhao W.; Ren Z.; Zhang H.; Jalaludin B.; Benmarhnia T.; Di J.; Hu H.; Wang Y.; Ji J. S.; Liang W.; Huang C. Effects of extreme temperature on the risk of preterm birth in China: A population-based multi-center cohort study. Lancet Reg Health West Pac 2022, 24, 100496. 10.1016/j.lanwpc.2022.100496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Health Commission of the People’s Republic of China. Report on the development of maternal and child health in China; Department of Maternal and Child Health: Beijing, 2019. [Google Scholar]
- Zhang Y.; Zhou Y. B.; Li H. T.; Gao Y. Q.; Zhang Y. L.; Luo S. S.; Kang C. Y.; Liu J. M. Secular trends of institutional delivery rate in China from 1996 to 2015. Chinese Medical Journal 2017, 97 (17), 1337–1342. 10.3760/cma.j.issn.0376-2491.2017.17.014. [DOI] [PubMed] [Google Scholar]
- National Bureau of Statistics of China. Development of children health career in Zhejiang; Zhejiang Provincial Bureau of Statistics: Zhejiang Province, 2003. [Google Scholar]
- Sun H. Z.; Xiang Q.; Xu S.; Dai H.; Fang J.; Tang H.; Xue T.; Wang H.; Tang K.; Guo Y.; Bai X. China’s unwavering determination in protecting pregnancy and perinatal health. Innovation 2022, 3 (6), 100336. 10.1016/j.xinn.2022.100336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davenport M. H.; Ruchat S. M.; Poitras V. J.; Jaramillo Garcia A.; Gray C. E.; Barrowman N.; Skow R. J.; Meah V. L.; Riske L.; Sobierajski F.; James M.; Kathol A. J.; Nuspl M.; Marchand A. A.; Nagpal T. S.; Slater L. G.; Weeks A.; Adamo K. B.; Davies G. A.; Barakat R.; Mottola M. F. Prenatal exercise for the prevention of gestational diabetes mellitus and hypertensive disorders of pregnancy: a systematic review and meta-analysis. Br J. Sports Med. 2018, 52 (21), 1367–1375. 10.1136/bjsports-2018-099355. [DOI] [PubMed] [Google Scholar]
- Villar J.; Carroli G.; Wojdyla D.; Abalos E.; Giordano D.; Ba’aqeel H.; Farnot U.; Bergsjo P.; Bakketeig L.; Lumbiganon P.; Campodonico L.; Al-Mazrou Y.; Lindheimer M.; Kramer M.; World Health Organization Antenatal Care Trial Research Group Preeclampsia, gestational hypertension and intrauterine growth restriction, related or independent conditions?. Am. J. Obstet Gynecol 2006, 194 (4), 921–931. 10.1016/j.ajog.2005.10.813. [DOI] [PubMed] [Google Scholar]
- Xue T.; Tong M.; Li J.; Wang R.; Guan T.; Li J.; Li P.; Liu H.; Lu H.; Li Y.; Zhu T. Estimation of stillbirths attributable to ambient fine particles in 137 countries. Nat. Commun. 2022, 13 (1), 6950. 10.1038/s41467-022-34250-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hendler I.; Goldenberg R. L.; Mercer B. M.; Iams J. D.; Meis P. J.; Moawad A. H.; MacPherson C. A.; Caritis S. N.; Miodovnik M.; Menard K. M.; Thurnau G. R.; Sorokin Y. The Preterm Prediction Study: association between maternal body mass index and spontaneous and indicated preterm birth. Am. J. Obstet Gynecol 2005, 192 (3), 882–6. 10.1016/j.ajog.2004.09.021. [DOI] [PubMed] [Google Scholar]
- Luo S.; Wang Y.; Mayvaneh F.; Relvas H.; Baaghideh M.; Wang K.; Yuan Y.; Yin Z.; Zhang Y. Surrounding greenness is associated with lower risk and burden of low birth weight in Iran. Nat. Commun. 2023, 14 (1), 7595. 10.1038/s41467-023-43425-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tamura T.; Goldenberg R. L.; Freeberg L. E.; Cliver S. P.; Cutter G. R.; Hoffman H. J. Maternal serum folate and zinc concentrations and their relationships to pregnancy outcome. Am. J. Clin. Nutr. 1992, 56 (2), 365–70. 10.1093/ajcn/56.2.365. [DOI] [PubMed] [Google Scholar]
- Scholl T. O. Iron status during pregnancy: setting the stage for mother and infant. Am. J. Clin. Nutr. 2005, 81 (5), 1218S–1222S. 10.1093/ajcn/81.5.1218. [DOI] [PubMed] [Google Scholar]
- Fuchs F.; Senat M. V. Multiple gestations and preterm birth. Semin Fetal Neonatal Med. 2016, 21 (2), 113–20. 10.1016/j.siny.2015.12.010. [DOI] [PubMed] [Google Scholar]
- Romero R.; Espinoza J.; Kusanovic J. P.; Gotsch F.; Hassan S.; Erez O.; Chaiworapongsa T.; Mazor M. The preterm parturition syndrome. BJOG 2006, 113 (Suppl 3), 17–42. 10.1111/j.1471-0528.2006.01120.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith G. C.; Pell J. P.; Dobbie R. Interpregnancy interval and risk of preterm birth and neonatal death: retrospective cohort study. BMJ. 2003, 327 (7410), 313. 10.1136/bmj.327.7410.313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saurel-Cubizolles M. J.; Zeitlin J.; Lelong N.; Papiernik E.; Di Renzo G. C.; Breart G.; Europop G. Employment, working conditions, and preterm birth: results from the Europop case-control survey. J. Epidemiol Community Health 2004, 58 (5), 395–401. 10.1136/jech.2003.008029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldenberg R. L.; Culhane J. F.; Iams J. D.; Romero R. Epidemiology and causes of preterm birth. Lancet 2008, 371 (9606), 75–84. 10.1016/S0140-6736(08)60074-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoffman S.; Hatch M. C. Stress, social support and pregnancy outcome: a reassessment based on recent research. Paediatr Perinat Epidemiol 1996, 10 (4), 380–405. 10.1111/j.1365-3016.1996.tb00063.x. [DOI] [PubMed] [Google Scholar]
- Orr S. T.; Miller C. A. Maternal depressive symptoms and the risk of poor pregnancy outcome. Review of the literature and preliminary findings. Epidemiol Rev. 1995, 17 (1), 165–71. 10.1093/oxfordjournals.epirev.a036172. [DOI] [PubMed] [Google Scholar]
- Shah P. S.; Balkhair T. Knowledge Synthesis Group on Determinants of Preterm, L. B. W. b., Air pollution and birth outcomes: a systematic review. Environ. Int. 2011, 37 (2), 498–516. 10.1016/j.envint.2010.10.009. [DOI] [PubMed] [Google Scholar]
- Akaraci S.; Feng X.; Suesse T.; Jalaludin B.; Astell-Burt T. A Systematic Review and Meta-Analysis of Associations between Green and Blue Spaces and Birth Outcomes. Int. J. Environ. Res. Public Health 2020, 17 (8), 2949. 10.3390/ijerph17082949. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chersich M. F.; Pham M. D.; Areal A.; Haghighi M. M.; Manyuchi A.; Swift C. P.; Wernecke B.; Robinson M.; Hetem R.; Boeckmann M.; Hajat S. Climate Change and Heat-Health Study Group, Associations between high temperatures in pregnancy and risk of preterm birth, low birth weight, and stillbirths: systematic review and meta-analysis. BMJ. 2020, 371, m3811. 10.1136/bmj.m3811. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sun Y.; Pei Z.; Zhao H.; Li L.; Hu Y.; Zhang L.; Wang L.; Yang Y.; Huang T.; Zhan S. China Cohort Consortium Study Group, Data Resource Profile: China Cohort Consortium (CCC). Int. J. Epidemiol 2020, 49 (5), 1436–1436m. 10.1093/ije/dyaa102. [DOI] [PubMed] [Google Scholar]
- Geng G.; Xiao Q.; Liu S.; Liu X.; Cheng J.; Zheng Y.; Tong D.; Zheng B.; Peng Y.; Huang X. Tracking Air Pollution in China: Near Real-Time PM2.5 Retrievals from Multiple Data Sources. Environ. Sci. Technol. 2021, 55 (17), 12106–12115. 10.1021/acs.est.1c01863. [DOI] [PubMed] [Google Scholar]
- Wei J.; Li Z. Q.; Lyapustin A.; Sun L.; Peng Y. R.; Xue W. H.; Su T. N.; Cribb M. Reconstructing 1-km-resolution high-quality PM2.5 data records from 2000 to 2018 in China: spatiotemporal variations and policy implications. Remote Sensing of Environment 2021, 252, 112136. 10.1016/j.rse.2020.112136. [DOI] [Google Scholar]
- Wei J.; Liu S.; Li Z.; Liu C.; Qin K.; Liu X.; Pinker R. T.; Dickerson R. R.; Lin J.; Boersma K. F.; Sun L.; Li R.; Xue W.; Cui Y.; Zhang C.; Wang J. Ground-Level NO2 Surveillance from Space Across China for High Resolution Using Interpretable Spatiotemporally Weighted Artificial Intelligence. Environ. Sci. Technol. 2022, 56 (14), 9988–9998. 10.1021/acs.est.2c03834. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xue T.; Zheng Y.; Geng G.; Xiao Q.; Meng X.; Wang M.; Li X.; Wu N.; Zhang Q.; Zhu T. Estimating Spatiotemporal Variation in Ambient Ozone Exposure during 2013–2017 Using a Data-Fusion Model. Environ. Sci. Technol. 2020, 54 (23), 14877–14888. 10.1021/acs.est.0c03098. [DOI] [PubMed] [Google Scholar]
- Sun H.; Shin Y. M.; Xia M.; Ke S.; Wan M.; Yuan L.; Guo Y.; Archibald A. T. Spatial Resolved Surface Ozone with Urban and Rural Differentiation during 1990–2019: A Space-Time Bayesian Neural Network Downscaler. Environ. Sci. Technol. 2022, 56 (11), 7337–7349. 10.1021/acs.est.1c04797. [DOI] [PubMed] [Google Scholar]
- Sun Z.; Archibald A. T. Multi-stage ensemble-learning-based model fusion for surface ozone simulations: A focus on CMIP6 models. Environ. Sci. Ecotechnol 2021, 8, 100124. 10.1016/j.ese.2021.100124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huete A.; Didan K.; Miura T.; Rodriguez E. P.; Gao X.; Ferreira L. G. Overview of the radiometric and biophysical performance of the MODIS vegetation indices. Remote Sensing of Environment 2002, 83 (1–2), 195–213. 10.1016/S0034-4257(02)00096-2. [DOI] [Google Scholar]
- Hersbach H.; Bell B.; Berrisford P.; Hirahara S.; Horanyi A.; Munoz-Sabater J.; Nicolas J.; Peubey C.; Radu R.; Schepers D.; Simmons A.; Soci C.; Abdalla S.; Abellan X.; Balsamo G.; Bechtold P.; Biavati G.; Bidlot J.; Bonavita M.; De Chiara G.; Dahlgren P.; Dee D.; Diamantakis M.; Dragani R.; Flemming J.; Forbes R.; Fuentes M.; Geer A.; Haimberger L.; Healy S.; Hogan R. J.; Holm E.; Janiskova M.; Keeley S.; Laloyaux P.; Lopez P.; Lupu C.; Radnoti G.; de Rosnay P.; Rozum I.; Vamborg F.; Villaume S.; Thepaut J. N. The ERA5 global reanalysis. Quarterly Journal of the Royal Meteorological Society 2020, 146 (730), 1999–2049. 10.1002/qj.3803. [DOI] [Google Scholar]
- Wu Y.; Li S.; Zhao Q.; Wen B.; Gasparrini A.; Tong S.; Overcenco A.; Urban A.; Schneider A.; Entezari A.; Vicedo-Cabrera A. M.; Zanobetti A.; Analitis A.; Zeka A.; Tobias A.; Nunes B.; Alahmad B.; Armstrong B.; Forsberg B.; Pan S. C.; Iniguez C.; Ameling C.; De la Cruz Valencia C.; Astrom C.; Houthuijs D.; Van Dung D.; Roye D.; Indermitte E.; Lavigne E.; Mayvaneh F.; Acquaotta F.; de’Donato F.; Rao S.; Sera F.; Carrasco-Escobar G.; Kan H.; Orru H.; Kim H.; Holobaca I. H.; Kysely J.; Madureira J.; Schwartz J.; Jaakkola J. J. K.; Katsouyanni K.; Hurtado Diaz M.; Ragettli M. S.; Hashizume M.; Pascal M.; de Sousa Zanotti Stagliorio Coelho M.; Ortega N. V.; Ryti N.; Scovronick N.; Michelozzi P.; Correa P. M.; Goodman P.; Nascimento Saldiva P. H.; Abrutzky R.; Osorio S.; Dang T. N.; Colistro V.; Huber V.; Lee W.; Seposo X.; Honda Y.; Guo Y. L.; Bell M. L.; Guo Y. Global, regional, and national burden of mortality associated with short-term temperature variability from 2000–19: a three-stage modelling study. Lancet Planet Health 2022, 6 (5), e410–e421. 10.1016/S2542-5196(22)00073-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sun H. Z.; Zhao J.; Liu X.; Qiu M.; Shen H.; Guillas S.; Giorio C.; Staniaszek Z.; Yu P.; Wan M. W. L.; Chim M. M.; Daalen K. R. v.; Li Y.; Liu Z.; Xia M.; Ke S.; Zhao H.; Wang H.; He K.; Liu H.; Guo Y.; Archibald A. T. Antagonism between ambient ozone increase and urbanization-oriented population migration on Chinese cardiopulmonary mortality. Innovation 2023, 4 (6), 100517. 10.1016/j.xinn.2023.100517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luo Z.; Lv Z.; Zhao J.; Sun H.; He T.; Yi W.; Zhang Z.; He K.; Liu H. Shipping-related pollution decreased but mortality increased in Chinese port cities. Nature Cities 2024, 1 (4), 295–304. 10.1038/s44284-024-00050-8. [DOI] [Google Scholar]
- Chan K. H.; Xia X.; Ho K. F.; Guo Y.; Kurmi O. P.; Du H.; Bennett D. A.; Bian Z.; Kan H.; McDonnell J.; Schmidt D.; Kerosi R.; Li L.; Lam K. B. H.; Chen Z. Regional and seasonal variations in household and personal exposures to air pollution in one urban and two rural Chinese communities: A pilot study to collect time-resolved data using static and wearable devices. Environ. Int. 2021, 146, 106217. 10.1016/j.envint.2020.106217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhao P.; Su C.; Wang C.; Xu J.; Bai X. Clinical characteristics of uterine rupture without previous Cesarean section: A 25-year retrospective study. J. Obstet Gynaecol Res. 2021, 47 (6), 2093–2098. 10.1111/jog.14761. [DOI] [PubMed] [Google Scholar]
- Liu Y.; Liu K.; Zheng P.; Yin S.; Jin H.; Bai X.; Li Y.; Zheng J.; Dai Y.; Zhao M.; Liu W. Prenatal exposure and transplacental transfer of perfluoroalkyl substance isomers in participants from the upper and lower reaches of the Yangtze River. Environ. Pollut. 2021, 270, 116202. 10.1016/j.envpol.2020.116202. [DOI] [PubMed] [Google Scholar]
- Chen F.; Yin S.; Kelly B. C.; Liu W. Chlorinated Polyfluoroalkyl Ether Sulfonic Acids in Matched Maternal, Cord, and Placenta Samples: A Study of Transplacental Transfer. Environ. Sci. Technol. 2017, 51 (11), 6387–6394. 10.1021/acs.est.6b06049. [DOI] [PubMed] [Google Scholar]
- Chen F.; Yin S.; Kelly B. C.; Liu W. Isomer-Specific Transplacental Transfer of Perfluoroalkyl Acids: Results from a Survey of Paired Maternal, Cord Sera, and Placentas. Environ. Sci. Technol. 2017, 51 (10), 5756–5763. 10.1021/acs.est.7b00268. [DOI] [PubMed] [Google Scholar]
- Liu Y. X.; Li A.; An Q.; Liu K.; Zheng P.; Yin S. S.; Liu W. P. Prenatal and postnatal transfer of perfluoroalkyl substances from mothers to their offspring. Crit Rev. Env Sci. Tec 2022, 52 (14), 2510–2537. 10.1080/10643389.2021.1886556. [DOI] [Google Scholar]
- Liu Y.; Li A.; Buchanan S.; Liu W. Exposure characteristics for congeners, isomers, and enantiomers of perfluoroalkyl substances in mothers and infants. Environ. Int. 2020, 144, 106012. 10.1016/j.envint.2020.106012. [DOI] [PubMed] [Google Scholar]
- Liu Y.; Zhou X.; Wu Y.; Yang X.; Wang Y.; Li S.; Bai X.; Schlenk D.; Liu W. Exposure and Blood-Cerebrospinal Fluid Barrier Permeability of PFASs in Neonates. Environ. Sci. Tech Let 2022, 9 (1), 64–70. 10.1021/acs.estlett.1c00862. [DOI] [Google Scholar]
- Bai X.; Ran J.; Zhao X.; Liang Y.; Yang X.; Xi Y. The S100A10-AnxA2 complex is associated with the exocytosis of hepatitis B virus in intrauterine infection. Lab Invest 2022, 102 (1), 57–68. 10.1038/s41374-021-00681-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhao P.; Wen J.; Qian L.; Zhu X.; Wang H.; Bai X. Expression of S100 proteins is associated with HBV intrauterine transmission. Arch Gynecol Obstet 2020, 302 (6), 1389–1399. 10.1007/s00404-020-05753-6. [DOI] [PubMed] [Google Scholar]
- Ji C.; Zhang G.; Xu S.; Xiang Q.; Huang M.; Zhao M.; Bai X. Antibiotic treatments to mothers during the perinatal period leaving hidden trouble on infants. Eur. J. Pediatr 2022, 181 (9), 3459–3471. 10.1007/s00431-022-04516-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen H.; Li H.; Cao Y.; Qi H.; Ma Y.; Bai X.; Zhao Y.; Wu L.; Liu C.; Wei J.; Wang H.; Jin Y.; Wang Z.; Zhu Y. Food Intake and Diet Quality of Pregnant Women in China During the COVID-19 Pandemic: A National Cross-Sectional Study. Front Nutr 2022, 9, 853565. 10.3389/fnut.2022.853565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tu X.; Chen R.; Huang G.; Lu N.; Chen Q.; Bai X.; Li B. Factors Predicting Severe Myelosuppression and Its Influence on Fertility in Patients with Low-Risk Gestational Trophoblastic Neoplasia Receiving Single-Agent Methotrexate Chemotherapy. Cancer Manag Res. 2020, 12, 4107–4116. 10.2147/CMAR.S252664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wen J.; Bai X. X. miR-520h Inhibits cell survival by targeting mTOR in gestational diabetes mellitus. Acta Biochim Pol 2021, 68 (1), 65–70. 10.18388/abp.2020_5389. [DOI] [PubMed] [Google Scholar]
- Shen J.; Chen Q.; Li N.; Bai X.; Wang F.; Li B. TWIST1 expression and clinical significance in type I endometrial cancer and premalignant lesions: A retrospective clinical study. Medicine 2020, 99 (48), e23397 10.1097/MD.0000000000023397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sun H. Z.; Tang H.; Fang J.; Dai H.; Zhao H.; Xu S.; Xiang Q.; Tian Y.; Jiao Y.; Luo T.; Huang M.; Shu J.; Zang L.; Liu H.; Guo Y.; Xu W.; Bai X. A Chinese longitudinal maternity cohort study (2013–2021) on intrahepatic cholestasis phenotypes: Risk associations from environmental exposure to adverse pregnancy outcomes. J. Hazard Mater. 2024, 463, 132915. 10.1016/j.jhazmat.2023.132915. [DOI] [PubMed] [Google Scholar]
- Zhang L. Q.; Liu W. W.; Hou K.; Lin J. T.; Zhou C. H.; Tong X. H.; Wang Z. Y.; Wang Y. B.; Jiang Y. X.; Wang Z. W.; Zheng Y. B.; Lan Y. L.; Liu S. H.; Ni R. J.; Liu M. Y.; Zhu P. P. Air pollution-induced missed abortion risk for pregnancies. Nat. Sustain 2019, 2 (11), 1011–1017. 10.1038/s41893-019-0387-y. [DOI] [Google Scholar]
- Fleischer N. L.; Merialdi M.; van Donkelaar A.; Vadillo-Ortega F.; Martin R. V.; Betran A. P.; Souza J. P. Outdoor air pollution, preterm birth, and low birth weight: analysis of the world health organization global survey on maternal and perinatal health. Environ. Health Persp 2014, 122 (4), 425–30. 10.1289/ehp.1306837. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sun H. Z.; Tang H.; Zhao H.; Xiang Q.; Tian Y.; Daalen K. R. v.; Tang K.; Loo E. X.-L.; Shek L. P.-C.; Archibald A. T.; Xu W.; Guo Y.; Bai X.. Maternal cardiovascular and haematological complications alter the risk associations between environmental exposure and adverse pregnancy outcomes. medRxiv 2023, 10.1101/2023.11.15.23298338. [DOI] [Google Scholar]
- Jiang Y. Q.; Hu Z. B.; Du J. B.; Lin Y.; Ma H. X.; Jin G. F.; Li R.; Yan J. H.; Liu Z. W.; Lin G.; Zhou C. Q.; Xia Y. K.; Shen H. B. Baseline characteristics of the participants of China National Birth Cohort (in Chinese language). Chinese Journal of Epidemiology 2021, 42 (4), 579–585. 10.3760/cma.j.cn112338-20201231-01455. [DOI] [PubMed] [Google Scholar]
- Hu Z. B.; Du J. B.; Xu X.; Lin Y.; Ma H. X.; Jin G. F.; Li R.; Yan J. H.; Liu Z. W.; Lin G.; Zhou C. Q.; Xia Y. K.; Shen H. B. Profile of China National Birth Cohort (in Chinese language). Chinese Journal of Epidemiology 2021, 42 (4), 569–574. 10.3760/cma.j.cn112338-20201211-01402. [DOI] [PubMed] [Google Scholar]
- Huang S.; Liu S.; Huang M.; He J. R.; Wang C.; Wang T.; Feng X.; Kuang Y.; Lu J.; Gu Y.; Xia X.; Lin S.; Zhou W.; Fu Q.; Xia H.; Qiu X. The Born in Guangzhou Cohort Study enables generational genetic discoveries. Nature 2024, 626 (7999), 565–573. 10.1038/s41586-023-06988-4. [DOI] [PubMed] [Google Scholar]
- Qiu X.; Lu J. H.; He J. R.; Lam K. H.; Shen S. Y.; Guo Y.; Kuang Y. S.; Yuan M. Y.; Qiu L.; Chen N. N.; Lu M. S.; Li W. D.; Xing Y. F.; Zhou F. J.; Bartington S.; Cheng K. K.; Xia H. M. The Born in Guangzhou Cohort Study (BIGCS). Eur. J. Epidemiol 2017, 32 (4), 337–346. 10.1007/s10654-017-0239-x. [DOI] [PubMed] [Google Scholar]
- Zhang J.; Tian Y.; Wang W.; Ouyang F.; Xu J.; Yu X.; Luo Z.; Jiang F.; Huang H.; Shen X.; Shanghai Birth C. Cohort Profile: the Shanghai Birth Cohort. Int. J. Epidemiol 2019, 48 (1), 21–21g. 10.1093/ije/dyy277. [DOI] [PubMed] [Google Scholar]
- Lv H.; Diao F.; Du J.; Chen T.; Meng Q.; Ling X.; Li H.; Song C.; Xi Q.; Jiang Y.; Xu Y.; Tao S.; Huang L.; Wen M.; Peng M.; Liu C.; Lu Q.; He Y.; Yin Y.; Liu X.; Xu B.; Han X.; Zhou K.; Jiang T.; Zhao Y.; Ma H.; Jin G.; Xia Y.; Liu J.; Lin Y.; Hu Z.; Shen H. Assisted reproductive technology and birth defects in a Chinese birth cohort study. Lancet Reg Health West Pac 2021, 7, 100090. 10.1016/j.lanwpc.2020.100090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tao F. B.; Hao J. H.; Huang K.; Su P. Y.; Cheng D. J.; Xing X. Y.; Huang Z. H.; Zhang J. L.; Tong S. L. Cohort Profile: the China-Anhui Birth Cohort Study. Int. J. Epidemiol 2013, 42 (3), 709–21. 10.1093/ije/dys085. [DOI] [PubMed] [Google Scholar]
- Qian Z.; Liang S.; Yang S.; Trevathan E.; Huang Z.; Yang R.; Wang J.; Hu K.; Zhang Y.; Vaughn M.; Shen L.; Liu W.; Li P.; Ward P.; Yang L.; Zhang W.; Chen W.; Dong G.; Zheng T.; Xu S.; Zhang B. Ambient air pollution and preterm birth: A prospective birth cohort study in Wuhan, China. Int. J. Hyg Envir Heal 2016, 219 (2), 195–203. 10.1016/j.ijheh.2015.11.003. [DOI] [PubMed] [Google Scholar]
- Dou Y.; Yin Y.; Li Z.; Du J.; Jiang Y.; Jiang T.; Guo W.; Qin R.; Li M.; Lv H.; Lu Q.; Qiu Y.; Lin Y.; Jin G.; Lu C.; Ma H.; Hu Z. China National Birth Cohort, Maternal exposure to metal mixtures during early pregnancy and fetal growth in the Jiangsu Birth Cohort, China. Environ. Res. 2022, 215 (Pt 2), 114305. 10.1016/j.envres.2022.114305. [DOI] [PubMed] [Google Scholar]
- Wang Y. Y.; Li Q.; Guo Y.; Zhou H.; Wang Q. M.; Shen H. P.; Zhang Y. P.; Yan D. H.; Li S.; Chen G.; Zhou S.; He Y.; Yang Y.; Peng Z. Q.; Wang H. J.; Ma X. Ambient temperature and the risk of preterm birth: A national birth cohort study in the mainland China. Environ. Int. 2020, 142, 105851. 10.1016/j.envint.2020.105851. [DOI] [PubMed] [Google Scholar]
- Shao Y.; Qiu J.; Huang H.; Mao B.; Dai W.; He X.; Cui H.; Lin X.; Lv L.; Wang D.; Tang Z.; Xu S.; Zhao N.; Zhou M.; Xu X.; Qiu W.; Liu Q.; Zhang Y. Pre-pregnancy BMI, gestational weight gain and risk of preeclampsia: a birth cohort study in Lanzhou, China. BMC Pregnancy Childbirth 2017, 17 (1), 400. 10.1186/s12884-017-1567-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu X.; Xiao J.; Sun X.; Chen Q.; Yao Z.; Feng B.; Cao G.; Guo L.; He G.; Hu J.; Zeng W.; Rong Z.; Wang Q.; Zhang B.; Dong M.; Wang J.; Chen D.; Ma W.; Liu T. Associations of maternal ambient temperature exposures during pregnancy with the risk of preterm birth and the effect modification of birth order during the new baby boom: A birth cohort study in Guangzhou, China. Int. J. Hyg Envir Heal 2020, 225, 113481. 10.1016/j.ijheh.2020.113481. [DOI] [PubMed] [Google Scholar]
- Hesketh T.; Lu L.; Xing Z. W. The effect of China’s one-child family policy after 25 years. N Engl J. Med. 2005, 353 (11), 1171–6. 10.1056/NEJMhpr051833. [DOI] [PubMed] [Google Scholar]
- Soh S. E.; Tint M. T.; Gluckman P. D.; Godfrey K. M.; Rifkin-Graboi A.; Chan Y. H.; Stunkel W.; Holbrook J. D.; Kwek K.; Chong Y. S.; Saw S. M.; Group G. S. Cohort profile: Growing Up in Singapore Towards healthy Outcomes (GUSTO) birth cohort study. Int. J. Epidemiol 2014, 43 (5), 1401–1409. 10.1093/ije/dyt125. [DOI] [PubMed] [Google Scholar]
- Loo E. X. L.; Soh S. E.; Loy S. L.; Ng S.; Tint M. T.; Chan S. Y.; Huang J. Y.; Yap F.; Tan K. H.; Chern B. S. M.; Tan H. H.; Meaney M. J.; Karnani N.; Godfrey K. M.; Lee Y. S.; Chan J. K. Y.; Gluckman P. D.; Chong Y. S.; Shek L. P.; Eriksson J. G.; Group S. P. S.; Chia A.; Fogel A. M.; Goh A. E. N.; Chu A. H. Y.; Rifkin-Graboi A.; Qiu A.; Lee B. W.; Cheon B. K.; Vaz C.; Henry C. J.; Forde C. G.; Chi C.; Koh D. X. P.; Phua D. Y.; Loh D. N. L.; Quah E. P. L.; Tham E. H.; Law E. C. N.; Magkos F.; Mueller-Riemenschneider F.; Yeo G. S. H.; Yong H. E. J.; Chen H. Y.; Tan H. H.; Pan H.; Bever H.; Tan H. M.; Aris I. B. M.; Tay J.; Chan J. K. Y.; Xu J.; Yoong J. S.; Eriksson J. G.; Choo J. T. L.; Bernard J. Y.; Huang J. Y.; Lai J. S.; Tan K. M. L.; Godfrey K. M.; Kwek K. Y. C.; McCrickerd K.; Narasimhan K.; Chong K. W.; Lee K. J.; Chen L.; Ling L. H.; Chen L. W.; Daniel L. M.; Shek L. P.; Fortier M. V.; Chong M. F.; Chua M. C.; Leow M. K.; Kee M. Z. L.; Gong M.; Tint M. T.; Michael N.; Lek N.; Teoh O. H.; Mishra P.; Li Q. L. J.; Velan S. S.; Ang S. B.; Cai S.; Goh S. H.; Lim S. B.; Tsotsi S.; Hsu S. C.; Toh S. E. S.; Sadananthan S. A.; Tan T. H.; Yew T. W.; Gupta V.; Rajadurai V. S.; Han W. M.; Pang W. W.; Yuan W. L.; Zhu Y.; Cheung Y. B.; Chan Y. H.; Cheng Z. R. Cohort profile: Singapore Preconception Study of Long-Term Maternal and Child Outcomes (S-PRESTO). Eur. J. Epidemiol 2021, 36 (1), 129–142. 10.1007/s10654-020-00697-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
ZEBRA is a valuable resource for the research community, offering a wide range and depth of clinical diagnostic information and individual-level tracking of environmental exposure (e.g., PM2.5, ozone, green space, and abnormal temperature). While the study database is not publicly available, ZEBRA warmly welcomes potential collaborations, and such requests are considered on a case-by-case basis. Progress of the cohort will be updated on MedRxiv: 10.1101/2023.02.21.23286173. Researchers seeking access to the data set are required to obtain approval from the designated ZEBRA research proposal review committee, comprising members of the School of Medicine at Zhejiang University and the Maternal and Child Health Division of the Health Commission of Zhejiang Province. International researchers seeking additional information regarding collaboration and data access are encouraged to contact the lead authors, Dr. Xiaoxia Bai (baixiaoxia@zju.edu.cn) and Dr. Haitong Zhe Sun (ht.sun@nus.edu.sg).


