Abstract
Objective:
To determine the optimal anthropometric cut-off points for predicting the likelihood ratios of hypertension and diabetes in the Peruvian population.
Design:
A cross-sectional study was performed to establish cut-off values for body mass index (BMI), waist circumference (WC), waist:height ratio (WHtR) and Conicity index (C-index) associated with increased risk of hypertension and diabetes. Youden’s index (YIndex), area under the curve (AUC), sensitivity and specificity were calculated.
Setting:
Peruvian households.
Participants:
Peruvian population over the age of 18 years.
Results:
A total of 31 553 subjects were included, 57 % being women. Among the women, 53·06 % belonged to the 25- to 44-year-old age group [mean age: 41·66 in men and 40·02 in women]. The mean BMI, WHtR and C-index values were higher in women 27·49, 0·61, 1·30, respectively, while the mean WC value was higher in men 92·12 cm (sd ± 11·28). The best predictors of hypertension in men were the WHtR (AUC = 0·64) and the C-index (AUC = 0·64) with an optimal cut-off point of 0·57 (YIndex = 0·284) and 1·301 (YIndex = 0·284), respectively. Women showed an AUC of 0·63 and 0·61 in the WHtR and C-index, respectively, with an optimal cut-off of 0·61 (YIndex = 0·236) and 1·323 (YIndex = 0·225). The best predictor for diabetes was the C-index: with an AUC = 0·67 and an optimal cut-off of 1·337 (YIndex = 0·346) for men and an AUC = 0·66 and optimal cut-off of 1·313 (YIndex = 0·319) for women.
Conclusions:
Our findings show that in Peruvian adults, the WHtR and the C-index have the strongest association with hypertension in both sexes. Likewise, the C-index had the strongest association with diabetes.
Keywords: Peru, Anthropometry, BMI, Diabetes Mellitus, Type 2, Hypertension, Risk Factors
Hypertension and diabetes represent a threat to global health due to their growing trend and increased impact in developing countries(1). Hypertension currently affects one billion people, while diabetes affects nearly 500 million people worldwide(2,3). In Peru, the prevalence of hypertension is estimated at 14·8 % and that of diabetes is between 3·6 and 7 %(4,5). The complications of these conditions represent a significant burden of disease in terms of mortality and disability as well as a high economic burden at the country level(6–8). Thus, it is relevant to implement prevention strategies and timely screening in higher risk populations.
Overweight is one of the main risk factors for the onset of hypertension and diabetes. The World Health Organisation (WHO) proposed the use of the body mass index (BMI) for the diagnosis of obesity and waist circumference (WC) for measuring the risk of metabolic complications(9). For this reason, the BMI is currently the most widely used measure in clinical and epidemiological contexts, although there is a concern about its low accuracy in detecting cardiovascular risk in specific populations(10).
Others indices such as the waist:hip ratio (WHR), the waist:height ratio (WHtR) and the conicity index (C-index) are currently performed to provide information about body composition and to predict morbidity and mortality at the population level(11). Some of the indices such as WC, WHtR and WHR are better predictors than BMI of the risk of developing hypertension and type 2 diabetes mellitus in different countries(12–14). However, the WHO concluded that cut-off points for WC and WHR must be identified according to the anthropometric characteristics of specific populations(15). Moreover, others indices such as the C-index are in the exploratory stage, and accurate cut-off points have not yet been defined.
In Peru, through the Ministry of Health, the National Institute of Health has suggested the use of BMI for the detection of obesity and WC for the detection of the risk of hypertension and diabetes(16,17). However, there is controversy about the cut-off points of WC for Latin America, since the cut-off points for the Asian population have been adopted(18). This is relevant because some studies in Latin America show that the internationally proposed cut-off for WC provides a poor estimate of cardiometabolic risk(19–21), thereby demonstrating the need for regional limit values(22).
In contrast to this controversy, there are other anthropometric indicators such as the WHtR that incorporates the size of the individual in the measurement, improving the precision of the estimation of risks(23). This is very important in the Peruvian population because it has one of the lower heights worldwide(24). Furthermore, a genetic variation has even been postulated in a recently published study that would explain the short stature on this population(25). The presence of this genetic variation would produce a reduction of 2·2 to 4·4 cm in height and is more frequent in the population from the coast - one of the three natural regions of Peru which comprises 55·9 % of the total population - than in the highlands or the Jungle.
To date, compared with the BMI, the cut-off points and the level of prediction of risk of hypertension and diabetes of the WC, WHtR and C-index in the Peruvian population are unknown(26,27). Therefore, considering that the last Demographic and Family Health Survey (ENDES, in Spanish) 2018 has incorporated WC measurement, we aimed to determine the optimal cut-off points of the BMI, WC, the WHtR and the C-index to predict the probability rates of hypertension and diabetes in the Peruvian population according to sex and age groups.
Methods
Settings
Peru is a South American country made up of three regions: the Coast, Highlands and Jungle, with 55·9 % of the population residing on the Coast, 29·6 % in the Highlands and 14·5 % in the Jungle(28). Likewise, Peru has a population of more than 35 million inhabitants, among which about 6·5 million live in rural areas of the Peruvian territory, especially in the Highlands and Jungle regions(29). Unlike countries with a marked predominance of a race, such as Caucasian or Asian, these regions have a diversity of mixtures with a series of genotypes and phenotypes that hinder the ethnic classification of the population and explain some nutritional characteristics of these populations(30,31).
Study design and subjects
A cross-sectional study was conducted based on the data obtained by ENDES 2018, which is an annual population-based survey performed by the Demographic and Health Survey Programme that provides information on maternal and child health indicators and communicable and non-communicable diseases(4,32). The survey is supervised by the National Institute of Statistics and Informatics of Peru and contains three questionnaires on households, women’s health and health characteristics. The sampling and analysis units were households and individuals, respectively. A detailed description of the sampling method, enrolment procedure and ENDES objectives has been reported previously(4,32).
A total of 33 794 people over the age of 15 years were interviewed in the ENDES 2018 survey. The sample selected for this study included subjects >18 years of age (31 553). Questionnaires and physical examinations were performed to register socio-demographic and biophysical variables by trained staff according to a standard protocol(33).
Hypertension, diabetes and anthropometric measurements
Individuals were considered to have hypertension if their average (two readings) systolic blood pressure was ≥140 mmHg or diastolic blood pressure was ≥90 mmHg(34) using a digital blood pressure monitor, or a self-reported diagnosis of hypertension by a doctor.
Diabetes was defined through self-reporting of whether an individual had been diagnosed with diabetes mellitus previously by a doctor (Has a physician ever diagnosed you with diabetes or high blood sugar?).
Four anthropometric indices were used in the study: the BMI, WC, the WHtR and the C-index. BMI was calculated according to the Quetelet index as weight (kg) divided by height squared (m2). WC was measured at a midway point between the lower rib margin and the iliac crest. The WHtR was calculated as WC (cm) divided by height (m), and the C-index was determined applying the following formula proposed by Valdez et al.(35)
 |
height and WC should be recorded in metres and the weight in kilograms; the constant of 0·109 is to convert volume and mass to height.
Contrary to the previously mentioned anthropometric indices, the C-index is considered an exploratory measurement, and therefore, its cut-off points have not been accurately defined. However, this index has been developed taking into account that the human body changes from a cylindrical shape (C-index equals 1·0) to a ‘double cone’ (C-index up to 1·73) when adiposity is accumulated in the waist(35). This fact makes this index potentially usable in certain populations, since it takes into account the relationship between weight, height and waist circumference at a time, allowing the comparison of people with different measurements of body weight and height(36).
For analytical purposes, the BMI was classified into four categories: <18·5, 18·5–24·9, 25·0–29·9 and ≥30 kg/m2 according to the WHO classification(37). WC was classified as a risk indicator when ≥90 cm for men and ≥ 80 cm for women according to the International Diabetes Federation of Ethnic South and Central Americans(18). The WHtR was defined as a risk indicator when ≥0·5 for both men and women(38). Currently, the C-index does not have established cut-off points, and therefore, it was classified as a risk indicator when ≥1·29 for men and ≥1·25 for women according to a study conducted in Brazil(39).
Covariates
Sex (male; female) and age groups (18–24, 25–44, 45–64, 65 or more years) were considered to stratify the selected population. To describe the population characteristics, the following variables were reported: current smokers (smoked in the last 30 d) (yes/no), alcohol consumption in the last 12 months for 12 or more days (yes/no) and area of residence (urban/rural).
Data analysis
Continuous variables were presented as means and standard deviations (sd), and categorical variables were expressed as absolute numbers and weighted proportions with 95 % confidence intervals (CI). Prevalence and age-standardised prevalence were estimated based on the WHO reference population(40) for anthropometric measures for hypertension and diabetes. Age-standardised prevalence allows more accurate comparisons between structurally different populations(41). The mean differences between groups (men and women) and age-adjusted proportions were tested by linear combination of weighted means and the χ2 test. In addition, alluvial diagrams to visualise relations among anthropometric indices were also carried out. We included the ENDES 2018 sampling specifications, including stratification, and ponderation factor. The Youden’s index ((sensitivity + specificy) − 1) (YIndex) was used to identify optimal cut-off points according to sex and ages of the BMI, WC, the WHtR and the C-index for the prediction of hypertension and diabetes(42,43). The area under the curve (AUC), sensitivity (S) and specificity (Sp) values were calculated using the cutpt command. CI at 95 % of the AUC were also estimated using bootstrapping with 1000 replications.
All statistical analyses were performed using Stata v14·2 (Stata Corporation). The level of statistical significance was P < 0·05.
Ethical considerations
This study did not require the approval of an ethics committee because it is an analysis of aggregated secondary data that are in the public domain (http://iinei.inei.gob.pe/microdatos/) and does not identify any participants.
Results
Socio-demographic and clinical characteristics of the sample
Of the 31 553 subjects evaluated, 57 % were women. The most frequent age group was 25 to 44 years (51·57 % of men and 53·06 % of women), and the mean age was 41·66 years (sd 15·96) for men and 40·02 years (sd 16·14) for women. The average heights were significantly different according to natural region and were lower, both for men and women, in the rural Highlands. The mean BMI, WHtR and C-index values were higher in women at 27·49 (sd 4·82), 0·61 (sd 0·08), 1·30 (sd 0·08), respectively, while the mean WC was higher in men with 92·12 cm (sd 11·28) (Table 1).
Table 1.
Socio-demographic and clinical characteristics of Peruvian adults, Demographic and Family Health Survey (ENDES) 2018*
| Men (n 13 590) | Women (n 17 963) | |||
|---|---|---|---|---|
| Characteristics | % | 95 % CI | % | 95 % CI |
| Age (years) | ||||
| Mean | 41·66 | 40·02 | ||
| sd | 15·96 | 16·14 | ||
| Age groups | ||||
| 18–24 | 12·69 | 12·14, 13·26 | 15·45 | 14·93, 15·99 |
| 25–44 | 51·57 | 50·73, 52·41 | 53·06 | 52·33, 53·79 |
| 45–64 | 24·48 | 23·77, 25·21 | 21·28 | 20·69, 21·89 |
| 65+ | 11·26 | 10·74, 11·80 | 10·20 | 9·77, 10·66 |
| Level of education | ||||
| No education | 1·60 | 1·33, 1·92 | 6·58 | 6·08, 7·12 |
| Primary | 18·34 | 17·46, 19·26 | 22·98 | 22·09, 23·89 |
| Secondary | 44·03 | 42·65, 45·41 | 37·36 | 36·26, 38·47 |
| Higher | 36·03 | 34·68, 37·41 | 33·08 | 31·97, 34·22 |
| Wealth Index | ||||
| Poorest | 18·65 | 17·84, 19·49 | 18·66 | 17·94, 19·40 |
| Poorer | 21·20 | 20·10, 22·35 | 19·80 | 18·90, 20·73 |
| Middle | 20·41 | 19·39, 21·47 | 21·39 | 20·38, 22·43 |
| Richer | 20·81 | 19·65, 22·02 | 19·71 | 18·71, 20·75 |
| Richest | 18·93 | 17·64, 20·29 | 20·44 | 19·37, 21·56 |
| Urban | 64·22 | 63·41, 65·02 | 66·40 | 65·74, 67·12 |
| Weight (kg) | ||||
| Mean | 71·17 | 63·12 | ||
| sd | 13·61 | 12·24 | ||
| Height (cm) | ||||
| Mean | 163·60 | 151·39 | ||
| sd | 6·69 | 6·09 | ||
| Mean height by natural region and residence area | ||||
| Rural jungle | ||||
| Mean | 161·59 | 149·95 | ||
| sd | 0·16 | 0·14 | ||
| Urban jungle | ||||
| Mean | 163·86 | 152·25 | ||
| sd | 0·15 | 0·12 | ||
| Rural highlands | ||||
| Mean | 160·86 | 149·14 | ||
| sd | 0·12 | 0·10 | ||
| Urban highlands | ||||
| Mean | 164·46 | 151·42 | ||
| sd | 0·15 | 0·11 | ||
| Rural coast | ||||
| Mean | 162·79 | 150·97 | ||
| sd | 0·28 | 0·22 | ||
| Urban coast | ||||
| Mean | 165·52 | 152·76 | ||
| sd | 0·09 | 0·07 | ||
| BMI (kg/m2) | ||||
| Mean | 26·49 | 27·49 | ||
| sd | 4·27 | 4·82 | ||
| WC (cm) | ||||
| Mean | 92·12 | 91·56 | ||
| sd | 11·28 | 11·57 | ||
| WHtR | ||||
| Mean | 0·563 | 0·605 | ||
| sd | 0·067 | 0·078 | ||
| C-index | ||||
| Mean | 1·285 | 1·304 | ||
| sd | 0·074 | 0·079 | ||
| SBP, mmHg | ||||
| Mean | 125·74 | 114·98 | ||
| sd | 15·83 | 16·93 | ||
| DBP, mmHg | ||||
| Mean | 75·48 | 70·77 | ||
| sd | 10·10 | 9·50 | ||
| Smoker | 19·81 | 19·15, 20·49 | 3·25 | 3·00, 3·51 |
| Alcohol drinker | 32·94 | 32·15, 33·73 | 12·50 | 12·03, 13·00 |
WC, waist circumference; WHtR: waist:height ratio; C-index, conicity index; SBP, systolic blood pressure; DBP, diastolic blood pressure.
Weights and sample specifications of the ENDES 2018 were included (except for continuous variables).
Prevalence of obesity, cardiometabolic risk, hypertension and diabetes
The standardised prevalence of obesity calculated with the BMI was 21·05 % in men and 27·78 % in women (P < 0·001). The prevalence of cardiometabolic risk calculated with the WC, WHtR and C-index was statistically higher in women (84·91 %, 92·16 % and 76·93 %) compared with men (60·77 %, 82·78 % and 50·50 %) (P < 0·001), respectively.
In addition, the standardised prevalence of hypertension was 23·15 % in males and 18·41 % in females (P < 0·001), while the prevalence of diabetes was 3·25 % and 4 %, respectively (P = 0·017) (Table 2).
Table 2.
Anthropometric indices and clinical characteristics of Peruvian adults, Demographic and Family Health Survey (ENDES) 2018*
| Men (n 13 590) | Women (n 17 963) | P-value | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Characteristics | Prevalence | 95 % CI | Age-standardised prevalence | 95 % CI | Prevalence | 95 % CI | Age-standardised prevalence | 95 % CI | |
| BMI | |||||||||
| Underweight | 3·04 | 2·65, 3·49 | 3·11 | 2·74, 3·53 | 3·39 | 3·00, 3·82 | 3·24 | 2·90, 3·62 | 0·628 |
| Normal | 36·10 | 34·89, 37·32 | 36·19 | 35·06, 37·34 | 30·15 | 29·08, 31·25 | 30·50 | 29·50, 31·51 | < 0·001 |
| Overweight | 39·74 | 38·45, 41·05 | 39·64 | 38·40, 40·90 | 38·67 | 37·56, 39·80 | 38·48 | 37·42, 39·56 | 0·160 |
| Obese | 21·12 | 20·07, 22·21 | 21·05 | 20·04, 22·10 | 27·79 | 26·72, 28·88 | 27·78 | 26·77, 28·82 | < 0·001 |
| WC (cm) | |||||||||
| Normal | 44·44 | 43·60, 45·27 | 39·23 | 38·11, 40·35 | 15·93 | 15·40, 16·47 | 15·09 | 14·35, 15·87 | < 0·001 |
| At risk (≥90 M, ≥80 W) | 55·56 | 54·73, 56·40 | 60·77 | 59·65, 61·89 | 84·07 | 83·53, 84·60 | 84·91 | 84·13, 85·65 | < 0·001 |
| WHtR | |||||||||
| Normal | 18·32 | 17·68, 18·98 | 17·22 | 16·41, 18·05 | 7·88 | 7·50, 8·29 | 7·84 | 7·29, 8·43 | < 0·001 |
| At risk (≥0·50) | 81·68 | 81·02, 82·32 | 82·78 | 81·95, 83·59 | 92·12 | 91·71, 92·50 | 92·16 | 91·57, 92·71 | < 0·001 |
| C-index | |||||||||
| Normal | 52·41 | 51·57, 53·25 | 49·50 | 48·40, 50·60 | 24·02 | 23·40, 24·65 | 23·07 | 22·21, 23·96 | < 0·001 |
| At risk (≥1·29 M, ≥1·25 W) | 47·59 | 46·75, 48·43 | 50·50 | 49·40, 51·60 | 75·98 | 75·35, 76·60 | 76·93 | 76·04, 77·79 | < 0·001 |
| Hypertension | 21·07 | 20·39, 21·76 | 23·15 | 22·15, 24·18 | 15·38 | 14·86, 15·91 | 18·41 | 17·59, 19·27 | < 0·001 |
| Diabetes | 2·71 | 2·45, 2·99 | 3·25 | 2·83, 3·74 | 2·98 | 2·74, 3·24 | 4·00 | 3·55, 4·51 | 0·017 |
WC, waist circumference; WHtR, waist:height ratio; C-index, conicity index; M, men; W, women.
Weights and sample specifications of the ENDES 2018 were included.
Figure 1a-c shows the differences in risk estimation using the BMI v. the WC, WHtR, and C-index. A considerable group of males and females considered as normal according to the BMI were considered at risk with the WC, WHtR and C-index, respectively.
Fig. 1.
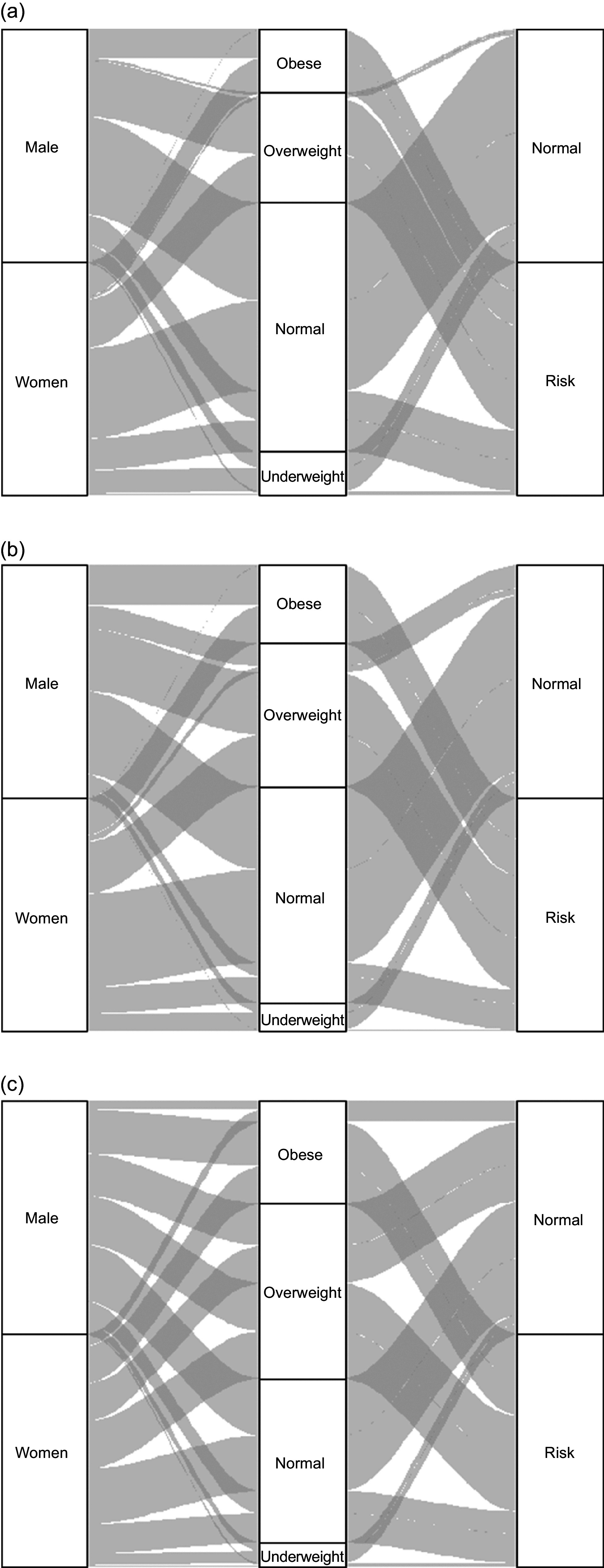
(a) Comparison of the estimation of risk of BMI against WC. (b) Comparison of the estimation of risk of BMI against WHtR. (c) Comparison of the estimation of risk of BMI against C-index
Accuracy and optimal cut-off points of anthropometric indices to predict hypertension and diabetes
Table 3 shows the cut-off points, S, Sp and AUCs estimates. The most accurate indices for predicting hypertension in males were the WHtR (AUC 0·64) and the C-index (AUC 0·64). In addition, the optimal cut-offs for these measures were 0·57 (YIndex 0·284) and 1·301 (YIndex 0·284), respectively. Likewise, the most accurate indices to predict hypertension were the WHtR (AUC 0·63) and the C-index (AUC 0·61) for women, with the optimal cut-off points for these measures being 0·61 (YIndex 0·236) and 1·323 (YIndex 0·225) (Table 3).
Table 3.
Anthropometric indices and hypertension in Peruvian adults, Demographic and Family Health Survey (ENDES) 2018
| Characteristics | n | Optimal cut-off point | AUC | Sensitivity (%) | Specificity (%) | Younden index | 95 % CI |
|---|---|---|---|---|---|---|---|
| Men | 13 593 | ||||||
| BMI (kg/m2) | 27·7 | 0·60 | 51 | 70 | 0·203 | ||
| 18–24 | 1725 | 24·6 | 0·64 | 64 | 63 | 0·271 | 0·199–0·343 |
| 25–44 | 7008 | 27·7 | 0·62 | 57 | 66 | 0·233 | 0·201–0·265 |
| 45–64 | 3327 | 27·8 | 0·61 | 56 | 67 | 0·228 | 0·195–0·261 |
| 65+ | 1533 | 27·2 | 0·59 | 41 | 77 | 0·180 | 0·140–0·221 |
| WC (cm) | 93·3 | 0·62 | 64 | 61 | 0·248 | ||
| 18–24 | 1725 | 87·2 | 0·64 | 56 | 72 | 0·281 | 0·209–0·352 |
| 25–44 | 7008 | 96·2 | 0·61 | 52 | 70 | 0·222 | 0·194–0·250 |
| 45–64 | 3327 | 96·9 | 0·62 | 61 | 63 | 0·236 | 0·199–0·271 |
| 65+ | 1533 | 90·3 | 0·59 | 69 | 49 | 0·182 | 0·142–0·222 |
| WHtR | 0·57 | 0·64 | 64 | 64 | 0·284 | ||
| 18–24 | 1725 | 0·51 | 0·63 | 65 | 60 | 0·256 | 0·175–0·337 |
| 25–44 | 7008 | 0·56 | 0·61 | 70 | 52 | 0·225 | 0·194–0·256 |
| 45–64 | 3327 | 0·57 | 0·62 | 74 | 50 | 0·241 | 0·213–0·270 |
| 65+ | 1533 | 0·58 | 0·61 | 66 | 56 | 0·226 | 0·179–0·274 |
| C-Index | 1·301 | 0·64 | 64 | 64 | 0·284 | ||
| 18–24 | 1725 | 1·245 | 0·60 | 47 | 74 | 0·207 | 0·125–0·289 |
| 25–44 | 7008 | 1·277 | 0·58 | 62 | 54 | 0·165 | 0·130–0·200 |
| 45–64 | 3327 | 1·311 | 0·60 | 71 | 48 | 0·195 | 0·161–0·228 |
| 65+ | 1533 | 1·359 | 0·58 | 55 | 61 | 0·161 | 0·111–0·212 |
| Women | 17 963 | ||||||
| BMI (kg/m2) | 28·6 | 0·58 | 51 | 65 | 0·160 | ||
| 18–24 | 2776 | 23·8 | 0·57 | 73 | 41 | 0·146 | 0·060–0·232 |
| 25–44 | 9531 | 29·7 | 0·60 | 49 | 70 | 0·196 | 0·160–0·231 |
| 45–64 | 3823 | 28·6 | 0·58 | 58 | 58 | 0·162 | 0·129–0·194 |
| 65+ | 1833 | 26·2 | 0·58 | 57 | 59 | 0·160 | 0·120–0·199 |
| WC | 93·3 | 0·60 | 59 | 60 | 0·198 | ||
| 18–24 | 2776 | 81·0 | 0·57 | 76 | 38 | 0·139 | 0·065–0·214 |
| 25–44 | 9531 | 98·1 | 0·60 | 47 | 73 | 0·200 | 0·167–0·233 |
| 45–64 | 3823 | 91·4 | 0·58 | 74 | 42 | 0·160 | 0·133–0·187 |
| 65+ | 1833 | 83·9 | 0·59 | 77 | 41 | 0·177 | 0·138–0·217 |
| WHtR | 0·61 | 0·63 | 64 | 59 | 0·236 | ||
| 18–24 | 2776 | 0·61 | 0·57 | 33 | 80 | 0·136 | 0·061–0·212 |
| 25–44 | 9531 | 0·61 | 0·60 | 62 | 58 | 0·195 | 0·162–0·229 |
| 45–64 | 3823 | 0·65 | 0·58 | 53 | 62 | 0·154 | 0·121–0·188 |
| 65+ | 1833 | 0·58 | 0·59 | 75 | 42 | 0·177 | 0·139–0·215 |
| C-Index | 1·323 | 0·61 | 60 | 62 | 0·225 | ||
| 18–24 | 2776 | 1·237 | 0·59 | 76 | 41 | 0·173 | 0·091–0·255 |
| 25–44 | 9531 | 1·289 | 0·56 | 70 | 43 | 0·129 | 0·095–0·163 |
| 45–64 | 3823 | 1·344 | 0·55 | 54 | 57 | 0·105 | 0·076–0·135 |
| 65+ | 1833 | 1·323 | 0·57 | 68 | 46 | 0·134 | 0·91–0·178 |
WC, waist circumference; WHtR, waist:height ratio; C-index, conicity index.
For diabetes, the C-index showed the highest accuracy in men (AUC 0·67), with an optimal cut-off of 1·337 (YIndex 0·346), compared with women (AUC 0·66), who had an optimal cut-off of 1·313 (YIndex 0·319) (Table 4).
Table 4.
Anthropometric indices and diabetes in Peruvian adults, Demographic and Family Health Survey (ENDES) 2018
| Characteristics | n | Optimal cut-off point | AUC | Sensitivity (%) | Specificity (%) | Younden index | 95 % CI |
|---|---|---|---|---|---|---|---|
| Men | 13 590 | ||||||
| BMI (kg/m2) | 27·3 | 0·61 | 60 | 62 | 0·220 | ||
| 18–24 | 1725 | 26·3 | 0·69 | 64 | 75 | 0·388 | 0·145–0·630 |
| 25–44 | 7008 | 27·4 | 0·64 | 68 | 60 | 0·279 | 0·186–0·373 |
| 45–64 | 3327 | 24·8 | 0·61 | 89 | 33 | 0·215 | 0·170–0·260 |
| 65+ | 1530 | 26·3 | 0·61 | 58 | 63 | 0·213 | 0·130–0·297 |
| WC (cm) | 94·1 | 0·66 | 72 | 60 | 0·320 | ||
| 18–24 | 1725 | 87·7 | 0·72 | 73 | 71 | 0·442 | 0·171–0·712 |
| 25–44 | 7008 | 99·9 | 0·65 | 52 | 78 | 0·298 | 0·194–0·402 |
| 45–64 | 3327 | 94·0 | 0·63 | 80 | 47 | 0·264 | 0·206–0·322 |
| 65+ | 1530 | 97·1 | 0·63 | 61 | 65 | 0·266 | 0·178–0·353 |
| WHtR | 0·58 | 0·66 | 70 | 62 | 0·316 | ||
| 18–24 | 1725 | 0·50 | 0·69 | 82 | 56 | 0·378 | 0·135–0·620 |
| 25–44 | 7008 | 0·58 | 0·64 | 59 | 68 | 0·276 | 0·177–0·375 |
| 45–64 | 3327 | 0·58 | 0·61 | 74 | 49 | 0·225 | 0·165–0·285 |
| 65+ | 1530 | 0·58 | 0·60 | 73 | 46 | 0·191 | 0·106–0·276 |
| C-index | 1·337 | 0·67 | 58 | 77 | 0·346 | ||
| 18–24 | 1725 | 1·194 | 0·66 | 91 | 41 | 0·323 | 0·114–0·533 |
| 25–44 | 7008 | 1·313 | 0·61 | 48 | 75 | 0·229 | 0·132–0·326 |
| 45–64 | 3327 | 1·346 | 0·62 | 58 | 66 | 0·234 | 0·163–0·304 |
| 65+ | 1530 | 1·357 | 0·59 | 65 | 54 | 0·188 | 0·107–0·270 |
| Women | 17 963 | ||||||
| BMI (kg/m2) | 28·3 | 0·59 | 57 | 61 | 0·181 | ||
| 18–24 | 2776 | 25·9 | 0·68 | 75 | 61 | 0·361 | 0·060–0·662 |
| 25–44 | 9531 | 31·4 | 0·59 | 37 | 81 | 0·172 | 0·102–0·242 |
| 45–64 | 3823 | 28·4 | 0·57 | 62 | 53 | 0·143 | 0·092–0·193 |
| 65+ | 1833 | 27·0 | 0·61 | 63 | 59 | 0·221 | 0·152–0·290 |
| WC | 94·2 | 0·63 | 65 | 61 | 0·258 | ||
| 18–24 | 2776 | 90·7 | 0·68 | 63 | 73 | 0·359 | 0·043–0·674 |
| 25–44 | 9531 | 89·3 | 0·61 | 82 | 41 | 0·229 | 0·167–0·290 |
| 45–64 | 3823 | 97·4 | 0·59 | 59 | 59 | 0·183 | 0·124–0·242 |
| 65+ | 1833 | 90·4 | 0·65 | 78 | 51 | 0·291 | 0·239–0·343 |
| WHtR | 0·63 | 0·63 | 64 | 63 | 0·268 | ||
| 18–24 | 2776 | 0·56 | 0·66 | 75 | 56 | 0·311 | 0·044–0·578 |
| 25–44 | 9531 | 0·63 | 0·60 | 56 | 63 | 0·192 | 0·119–0·264 |
| 45–64 | 3823 | 0·66 | 0·60 | 55 | 64 | 0·193 | 0·126–0·260 |
| 65+ | 1833 | 0·58 | 0·63 | 89 | 36 | 0·251 | 0·208–0·295 |
| C-index | 1·313 | 0·66 | 77 | 55 | 0·319 | ||
| 18–24 | 2776 | 1·232 | 0·63 | 88 | 39 | 0·261 | 0·034–0·488 |
| 25–44 | 9531 | 1·276 | 0·60 | 86 | 35 | 0·207 | 0·149–0·264 |
| 45–64 | 3823 | 1·308 | 0·60 | 84 | 35 | 0·189 | 0·142–0·237 |
| 65+ | 1833 | 1·325 | 0·63 | 83 | 43 | 0·256 | 0·199–0·314 |
WC, waist circumference; WHtR, waist:height ratio; C-index, conicity index.
Optimal cut-offs of the anthropometric indices by age group
The optimal cut-offs for the WHtR in men to predict the risk of hypertension ranged from 0·51 (AUC –0·63, S 65, Sp 60) in the 18–24-year-old group to 0·58 (AUC 0·61, S 66, Sp 56) in the 65-year-old group. In relation to the C-index, the optimal cut-offs for predicting hypertension ranged from 1·245 (AUC 0·60, S 47, Sp 74) in 18 to 24 years of age group to 1·359 (AUC 0·58, S 55, Sp 61) in the 65-year-old group. In women, the optimal cut-offs of the WHtR ranged from 0·58 (AUC 0·59, S 75, Sp 42) in the 65-year-old group to 0·65 (AUC 0·58, S 53, Sp 62) in the 45–64-year-old group. In addition, the optimal cut-offs for the C-index were 1·237 (AUC 0·59, S 76, Sp 41) for the 18–24-year-old group and 1·344 (AUC 0·55, S 54, Sp 57) for the 45–64-year-old group (Table 3).
The optimal cut-offs of the C-index to predict the risk of diabetes in men ranged from 1·194 (AUC 0·66, S 91, Sp 41) in the 18–24-year-old group to 1·357 (AUC 0·59, S 65, Sp 54) in the 65-year-old group. In women, the optimal cut-offs for the C-index ranged from 1·232 (AUC 0·63, S 87·5, Sp 38·6) in the group of 18–24 years old to 1·325 (AUC 0·63, S 83·13, Sp 42·5) in the 65-year-old group (Table 4).
Discussion
In this study, we estimated the optimal cut-off points for the BMI, the WC, the WHtR, and the C-index in Peruvian men and women for predicting the development of hypertension and diabetes. We found that in Peruvian adults, the WHtR and the C-index have the strongest association with hypertension in both sexes. Likewise, the C-index had the strongest association with diabetes. To our knowledge, this is the first study to estimate optimal anthropometric cut-off points using representative populational data in Peru.
Several systematic reviews and primary studies have reported better performance of the WHtR to predict hypertension and diabetes compared with other anthropometric indicators such as the BMI and WC(12,23,44–46). In this regard, it should be specified that both the WHtR and WC better identify abdominal obesity than the BMI(47,48), but the better predictive capacity of the WHtR over WC could be explained because WC is a simple measure that does not take into account the size and proportions of the individual, assuming that individuals of short stature have the same risk as subjects of tall stature(49). Unlike other anthropometric indicators, such as the BMI, the WHR, the WHtR and the C-index, which construct ratios, by incorporating height or another dimensions in their formulas(23,50). For this reason, some authors have reported that WC is biased by the height of the individual and that people of short stature with high WC would be more at risk than people with high stature and the same WC(51).
In this regard, the WHtR, by incorporating the patient’s height in the formula, overcomes the limitation of assuming the same cut-off point for individuals with different heights and body proportions(23,51). This fact is important in the Peruvian context since a large proportion of the population of this country have a low height, and a measurement taking into account this characteristic would give a better estimation of risk(25). In addition, an inverse association of height with morbidity and mortality due to CVD has been described(50), which could be explained by adult height reflecting the nutritional situation in early childhood. Thus, inadequate nutrition during pregnancy and during early life stages ‘programme’ a metabolic imprint that predisposes the individual to obesity, resistance to insulin and other cardiovascular risk factors as well as short stature in adulthood(23,52).
Regarding the C-index, our findings may be considered as preliminary, since, to date, no cut-off points to diagnose obesity or risk of metabolic diseases have been defined for this indicator. In our study, we applied the criteria defined by Pitanga et al. in Brazil(52).
The prevalence of cardiometabolic risk and abdominal obesity estimated by the WHtR, WC and the C-index was very high and has not been reported previously in the Peruvian population. Thus, abdominal obesity calculated with the WHtR was 83 % in males and 92 % in females, while the BMI reported overweight and obesity in 61·3 % and 66 % of males and females, respectively. These differences between indicators indicate that the BMI could underestimate the risk of CVD, because it is an indirect measure of obesity, it does not allow assessment of fat distribution in the body(52) and is influenced by body proportions, so that subjects with lower height have a higher BMI(53,54).
The prevalence of self-reported diabetes was low in our study (3·5 % in males and 4 % in females); however, a systematic review by Carrillo-Larco et al. reported that the prevalence of diabetes had risen from 5·1 % to 7 % in national and subnational studies(5). This difference may be due to an underestimation of diabetes in undiagnosed subjects in our study, which is not consistent with the growing trend of diabetes in developing countries(55).
The anthropometric indicators that best predicted hypertension in the Peruvian population were the WHtR and the C-index. However, they are the least used by health care personnel, who routinely perform the BMI and WC as recommended by the WHO. Other studies in Brazil agree with the performance of the WHtR found in our study, as it has been reported as the best predictor for hypertension when compared with other indicators such as the WC, WHR, body fat percentage, BMI and C-index(12,39). However, another study in Nigeria reported BMI as the best predictor of hypertension in the study population when compared with metabolic risk indicators(56). In this regard, it should be taken into account that the average height of the sample in this study was 169·81 cm in men and 162·45 cm in women, which is greater than the Peruvian population, in which the average height was 163·60 cm in men and 151·39 cm in women according to our estimations presented in Table 1. Compared with the Nigerian population, the WC was higher in the Peruvian population for both men (88·37 v. 92·12) and women (90·03 v. 91·56), which suggests a more uniform distribution of body fat in the Nigerian population, making the BMI the best predictor of risk in Nigerians. These results highlight the need for re-evaluation of these indicators in different population groups, as this would allow identification of which indicators best predict the risk of hypertension at clinical and population levels.
The WHtR showed good performance for predicting the risk of hypertension in the Peruvian population as did the C-index for men, being very similar in women. The C-index was also the indicator which best predicted diabetes in men and women in our study. However, as described above, the results of the C-index in our study should be considered with caution, and further studies are needed to validate these findings. In this sense, the use of WHtR would be useful in the clinical and epidemiological setting for the detection of abdominal obesity, since it would substitute the use of two independent risk indicators such as BMI for obesity and WC for hypertension and diabetes. Using a single indicator, which according to our results, has greater precision in detecting cardiovascular risk factors, and by not involving other measurements, it would not generate additional costs for the health system. Likewise, its use would grant greater accuracy than WC for the detection of cardiometabolic risk in the Peruvian population since it incorporates height, considering the great variability of height in our population. In addition, there is a need for further research to investigate the use of the C-index, as although it was the best-performing indicator for predicting the risk of diabetes, it has shown different results in other populations(56–58).
One of the main limitations of this study was its observational design which does not allow causality to be inferred between anthropometric markers and hypertension/diabetes. Furthermore, we considered the diagnosis of hypertension and diabetes through self-reporting the estimates could be underestimated, although self-reporting of both diseases has shown good accuracy compared with clinical measures(59). Moreover, the cut-offs for the C-index were taken from a study in Brazil, without being validated in our country, and therefore, the estimates might have been different if other cut-offs had been applied. Likewise, it should be borne in mind that the prediction of disease risk of some anthropometric measures may be inadequate in populations with a low prevalence of the disease, such as young adults. Also, due to the cross-sectional nature of the study, some individuals with hypertension or diabetes might have improved their lifestyle and reduced weight after diagnosis; therefore, some of the anthropometric indices could actually have been similar or lower than healthy participants. In addition, information bias could happen by pollsters who participated in ENDES 2018, although they were trained to reduce the probability of this bias. Despite these limitations, it is worth highlighting the strengths of the study, such as the representativeness of the results with the use of data from the ENDES survey. In addition, this survey has the technical support of the well-recognised Demographic and Health Survey Programme.
The present study is the first to highlight that the WHtR and the C-index are the best predictors for hypertension and diabetes in the Peruvian population, thereby justifying their use in the health system for health personnel training and for population risk assessment and behaviour changing.
The results of this study show that the WHtR and the C-index were the best predictors for hypertension and diabetes in the Peruvian population. However, given the exploratory nature of the C-index, the use of the WHtR is recommended. Optimal cut-off points were also established to identify the risk of hypertension and diabetes, based on sex and age. According to our results, the WHtR may be considered as the principal indicator for the detection of these conditions in clinical and epidemiological fields in our country. In addition, we encourage the adoption of the optimal cut-off points identified in our study.
Acknowledgements
Acknowledgements: The authors are grateful to Elaine Pringle Donna for reviewing the language and style. Financial support: None. Conflict of interest: None. Authorship: A.H.V. and J.P.A. conceived the idea for the study; A.H.V. and RV.F. collected the data and did the statistical analysis; A.H.V., D.A., R.V.F. and J.P.A. drafted the manuscript; all authors contributed to the interpretation of data, writing and preparation of the manuscript. R.M.C.H. did the technical editing of the manuscript. All authors critically reviewed and approved the final manuscript. Ethics of human subject participation: The study has not required the approval of an ethics committee because it is an analysis of aggregated secondary data that is in the public domain (http://iinei.inei.gob.pe/microdatos/) and does not identify any participants.
References
- 1. NCD Risk Factor Collaboration (NCD-RisC) (2016) Worldwide trends in diabetes since 1980: a pooled analysis of 751 population-based studies with 4.4 million participants. Lancet 387, 1513–1530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. NCD Risk Factor Collaboration (NCD-RisC) (2017) Worldwide trends in blood pressure from 1975 to 2015: a pooled analysis of 1479 population-based measurement studies with 19·1 million participants. Lancet 389, 37–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. World Health Organization (2019) Global Report on Diabetes [Internet] WHO. https://www.who.int/diabetes/global-report/en/ (accessed October 2019).
- 4. National Institute of Statistics and Informatics (2019) Peru: Noncommunicable and Communicable Diseases, 2018 [Internet]. Lima Peru: INEI. https://www.inei.gob.pe/media/MenuRecursivo/publicaciones_digitales/Est/Lib1657/index1.html (accessed October 2020).
- 5. Carrillo-Larco RM & Bernabé-Ortiz A (2019) Type 2 diabetes mellitus in peru: a systematic review of prevalence and incidence in the general population. Rev Peru Med Exp Salud Publica 36, 26–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Mutowo MP, Lorgelly PK, Laxy M et al. (2016) The Hospitalization costs of diabetes and hypertension complications in Zimbabwe: estimations and correlations. J Diabetes Res 2016, 9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Wang G, Zhou X, Zhuo X et al. (2017) Annual total medical expenditures associated with hypertension by diabetes status in US adults. Am J Prev Med 53, S182–S189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. American Diabetes Association (2017) Economic costs of diabetes in the U.S. in 2017. Diabetes Care 41, 917. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. World Health Organization (2019) Waist circumference and waist-hip ratio: report of a WHO Expert Consultation Geneva 2011 [Internet]. WHO. https://www.who.int/nutrition/publications/obesity/WHO_report_waistcircumference_and_waisthip_ratio/en/ (accessed October 2019).
- 10. Wollner M, Paulo Roberto B-B, Alysson Roncally SC et al. (2017) Accuracy of the WHO’s body mass index cut-off points to measure gender- and age-specific obesity in middle-aged adults living in the city of Rio de Janeiro, Brazil. J Public Health Res 6, 904. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Zazai R, Wilms B, Ernst B et al. (2017) Waist circumference and related anthropometric indices are associated with metabolic traits in severely obese subjects. Obes Surg 24, 777–782. [DOI] [PubMed] [Google Scholar]
- 12. Caminha TCS, Ferreira HS, Costa NS et al. (2017) Waist-to-height ratio is the best anthropometric predictor of hypertension: a population-based study with women from a state of northeast of Brazil. Medicine 96, e5874–e5874. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Tran NTT, Blizzard CL, Luong KN et al. (2018) The importance of waist circumference and body mass index in cross-sectional relationships with risk of cardiovascular disease in Vietnam. PLoS One 13, e0198202–e0198202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. de Souza APA, Rodrigues PRM, Muraro AP et al. (2013) Cut-off points of anthropometric markers associated with hypertension in the Brazilian population: national Health Survey Public Health Nutr 22, 2147–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Nishida C, Ko GT & Kumanyika S (2010) Body fat distribution and noncommunicable diseases in populations: overview of the 2008 WHO Expert Consultation on Waist Circumference and Waist-Hip Ratio. Eur J Clin Nutr 64, 2–5. [DOI] [PubMed] [Google Scholar]
- 16. National Institute of Health (2012) Technical guide for nutritional assessment anthropometry of the adult [Internet]. https://repositorio.ins.gob.pe/xmlui/bitstream/handle/INS/225/CENAN-0067.pdf?sequence=1&isAllowed=y (accessed May 2020).
- 17. National Institute of Health (2013) Technical guide for nutritional assessment anthropometric of the elderly person [Internet]. https://bvs.ins.gob.pe/insprint/CENAN/Valoraci%C3%B3n_nutricional_antropom%C3%A9trica_persona_adulta_mayor.pdf (accessed May 2020).
- 18. Alberti KGMM, Zimmet P & Shaw J (2006) Metabolic syndrome – a new world-wide definition. A consensus statement from the international diabetes federation. Diabet Med 23, 469–480. [DOI] [PubMed] [Google Scholar]
- 19. Aschner P, Ruiz A, Balkau B et al. (2009) Association of abdominal adiposity with diabetes and cardiovascular disease in Latin America. J Clin Hypertens 11, 769–774. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Barbosa PJB, Lessa Í, de Almeida Filho N et al. (2006) Critério de obesidade central em população brasileira: impacto sobre a síndrome metabólica [Criteria for central obesity in the Brazilian population. Impact on metabolic syndrome]. Arquivos Brasileiros Cardiologia 87, 407–414. [DOI] [PubMed] [Google Scholar]
- 21. Sánchez-Castillo CP, Velázquez-Monroy O, Berber A et al. (2000) Anthropometric cutoff points for predicting chronic diseases in the Mexican National Health Survey Obes Res 2003, 442–451. [DOI] [PubMed] [Google Scholar]
- 22. Aschner P, Buendía R, Brajkovich I et al. (2011) Determination of the cutoff point for waist circumference that establishes the presence of abdominal obesity in Latin American men and women. Diabetes Res Clin Pract 93 243–247. [DOI] [PubMed] [Google Scholar]
- 23. Ashwell M, Gunn P & Gibson S (2012) Waist-to-height ratio is a better screening tool than waist circumference and BMI for adult cardiometabolic risk factors: systematic review and meta-analysis. Obes Rev 13, 275–286. [DOI] [PubMed] [Google Scholar]
- 24. NCD Risk Factor Collaboration (NCD-RisC) (2016) A century of trends in adult human height. Elife 5, e13410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Asgari S, Luo Y, Akbari A et al. (2020) A positively selected FBN1 missense variant reduces height in Peruvian individuals. Nature 582, 234–239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Ninatanta-Ortiz JA & Romaní FR (2017) Metabolic syndrome and abdominal obesity criteria for andean populations – reply. Rev Peru Med Exp Salud Publica 34, 148–149. [DOI] [PubMed] [Google Scholar]
- 27. Chirinos DA, Morey-Vargas OL, Goldberg RB et al. (2013) Metabolic syndrome in andean populations. Glob Heart 8, 349–354.e1. [DOI] [PubMed] [Google Scholar]
- 28. National Institute of Statistics and Informatics (2020) National Institute of Statistics and Informatics [Internet]. http://m.inei.gob.pe/prensa/noticias/el-peru-tiene-una-poblacion-de-31-millones-488-mil-625-habitantes-9196/ (accessed May 2020).
- 29. National Institute of Statistics and Informatics (2017) Peru: Socio-demographic Profile 2017 [Internet]. https://www.inei.gob.pe/media/MenuRecursivo/publicaciones_digitales/Est/Lib1539/cap01.pdf (accessed July 2020).
- 30. Harris DN, Song W, Shetty AC et al. (2018) Evolutionary genomic dynamics of Peruvians before, during, and after the Inca Empire. Proc Natl Acad Sci USA 115, E6526–E6535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Guio H, Poterico JA, Levano KS et al. (2018) Genetics and genomics in Peru: clinical and research perspective. Mol Genet Genomic Med 6, 873–886. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Hernández-Vásquez A & Chacón-Torrico H (2019) Manipulation, analysis, and visualization of data from the demographic and family health survey with the R program. Rev Peru Med Exp Salud Publica 36, 128–133. [DOI] [PubMed] [Google Scholar]
- 33. National Institute of Statistics and Informatics (2018) Manual from the interviewer [Internet]. https://proyectos.inei.gob.pe/endes/2018/documentos_2018/MANUAL_DE_LA_ENTREVISTADORA_2018_ENERO.pdf (accessed May 2020).
- 34. Chobanian AV, Bakris GL, Black HR et al. (2003) the seventh report of the joint national committee on prevention, detection, evaluation, and treatment of high blood pressure: the JNC 7 report. JAMA 289, 2560–2572. [DOI] [PubMed] [Google Scholar]
- 35. Valdez R (1991) A simple model-based index of abdominal adiposity. J Clin Epidemiol 44, 955–956. [DOI] [PubMed] [Google Scholar]
- 36. Almeida TD, Almeida MGD & Araújo TM (2009) Abdominal obesity and cardiovascular risk: performance of anthropometric indexes in women. Arq Bras Cardiol 92, 375–380. [DOI] [PubMed] [Google Scholar]
- 37. World Health Organization (2020) Obesity: preventing and managing the global epidemic. Report of a WHO consultation. World Health Organ Tech Rep Ser [Internet]. https://www.who.int/nutrition/publications/obesity/WHO_TRS_894/en/ (accessed October 2019). [PubMed]
- 38. Browning LM, Hsieh SD & Ashwell M (2010) A systematic review of waist-to-height ratio as a screening tool for the prediction of cardiovascular disease and diabetes: 0·5 could be a suitable global boundary value. Nutr Res Rev 23, 247–269. [DOI] [PubMed] [Google Scholar]
- 39. Dutra MT, Reis DBV, Martins KG et al. (2018) Comparative evaluation of adiposity indices as predictors of hypertension among Brazilian adults. Int J Hypertens 2018, 8396570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Ahmad OB, Boschi-Pinto C, Lopez AD et al. (2001) Age Standardization of Rates: A New WHO Standard. Geneva: World Health Organization; [Internet]. https://pdfs.semanticscholar.org/7e89/5b230760ac34ce3d5472fb1cbf92b08566cc.pdf (accessed October 2019). [Google Scholar]
- 41. Naing NN (2000) Easy way to learn standardization: direct and indirect methods. Malays J Med Sci 7, 10–5. [PMC free article] [PubMed] [Google Scholar]
- 42. Fluss R, Faraggi D & Reiser B (2005) Estimation of the Youden Index and its associated cutoff point. Biom J 47, 458–472. [DOI] [PubMed] [Google Scholar]
- 43. Clayton P (2013) CUTPT: Stata module for empirical estimation of cutpoint for a diagnostic test. Statistical Software Components [Internet]. https://ideas.repec.org/c/boc/bocode/s457719.html (accessed July 2019).
- 44. Savva SC, Lamnisos D & Kafatos AG (2013) Predicting cardiometabolic risk: waist-to-height ratio or BMI. A meta-analysis. Diabetes Metab Syndr Obes 6, 403–419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Corrêa MM, Thumé E, De Oliveira ERA et al. (2016) Performance of the waist-to-height ratio in identifying obesity and predicting non-communicable diseases in the elderly population: a systematic literature review. Arch Gerontol Geriatr 65, 174–182. [DOI] [PubMed] [Google Scholar]
- 46. Corrêa MM, Tomasi E, Thumé E et al. (2017) Waist-to-height ratio as an anthropometric marker of overweight in elderly Brazilians. Cad Saude Publica 33, e00195315. [DOI] [PubMed] [Google Scholar]
- 47. Després JP, Moorjani S, Lupien PJ et al. (1990) Regional distribution of body fat, plasma lipoproteins, and cardiovascular disease. Arteriosclerosis 10, 497–511. [DOI] [PubMed] [Google Scholar]
- 48. Foster MT & Pagliassotti MJ (2012) Metabolic alterations following visceral fat removal and expansion: beyond anatomic location. Adipocyte 1, 192–199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Han TS, Sattar N & Lean M (2006) ABC of obesity. Assessment of obesity and its clinical implications. BMJ 333, 695–698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Hsieh SD & Yoshinaga H (1999) Do people with similar waist circumference share similar health risks irrespective of height? Tohoku J Exp Med 188, 55–60. [DOI] [PubMed] [Google Scholar]
- 51. Waterland RA & Garza C (1999) Potential mechanisms of metabolic imprinting that lead to chronic disease. Am J Clin Nutr 69, 179–197. [DOI] [PubMed] [Google Scholar]
- 52. Pitanga FJG & Lessa I (2005) Anthropometric indexes of obesity as an instrument of screening for high coronary risk in adults in the city of Salvador--Bahia. Arq Bras Cardiol 85 26–31. [DOI] [PubMed] [Google Scholar]
- 53. Bagust A & Walley T (2000) An alternative to body mass index for standardizing body weight for stature. QJM 93, 589–596. [DOI] [PubMed] [Google Scholar]
- 54. Garn SM, Leonard WR & Hawthorne VM (1986) Three limitations of the body mass index. Am J Clin Nutr 44, 996–997. [DOI] [PubMed] [Google Scholar]
- 55. Krug EG (2016) Trends in diabetes: sounding the alarm. Lancet 387, 1485–1486. [DOI] [PubMed] [Google Scholar]
- 56. Ononamadu CJ, Ezekwesili CN, Onyeukwu OF et al. (2017) Comparative analysis of anthropometric indices of obesity as correlates and potential predictors of risk for hypertension and prehypertension in a population in Nigeria. Cardiovasc J Afr 28, 92–99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Wang H, Liu A, Zhao T et al. (2017) Comparison of anthropometric indices for predicting the risk of metabolic syndrome and its components in Chinese adults: a prospective, longitudinal study. BMJ Open 7, e016062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Wang Z, He S & Chen X (2019) Capacity of different anthropometric measures to predict diabetes in a Chinese population in southwest China: a 15-year prospective study. Diabet Med 36, 1261–1267. [DOI] [PubMed] [Google Scholar]
- 59. Chun H, Kim I-H & Min K-D (2016) Accuracy of self-reported hypertension, diabetes, and hypercholesterolemia: analysis of a representative sample of Korean older adults. Osong Public Health Res Perspect 7, 108–115. [DOI] [PMC free article] [PubMed] [Google Scholar]


